Abstract
Studies on Kawasaki disease (KD) in Arab countries are scarce, often providing incomplete data. This along with the benefits of multicenter research collaboratives led to the creation of the KD Arab Initiative [Kawarabi] consortium. An anonymous survey was completed among potential collaborative Arab medical institutions to assess burden of KD in those countries and resources available to physicians. An online 32-item survey was distributed to participating institutions after conducting face validity. One survey per institution was collected. Nineteen physicians from 12 countries completed the survey representing 19 out of 20 institutions (response rate of 95%). Fifteen (79%) institutions referred to the 2017 American Heart Association guidelines when managing a patient with KD. Intravenous immunoglobulin (IVIG) is not readily available at 2 institutions (11%) yet available in the country. In one center (5%), IVIG is imported on-demand. The knowledge and awareness among countries’ general population was graded (0 to 10) at median/interquartiles (IQR) 3 (2–5) and at median/IQR 7 (6–8) in the medical community outside their institution. Practice variations in KD management and treatment across Arab countries require solid proactive collaboration. The low awareness and knowledge estimates about KD among the general population contrasted with a high level among the medical community. The Kawarabi collaborative will offer a platform to assess disease burden of KD, among Arab population, decrease practice variation and foster population-based knowledge.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00246-022-02844-w.
Keywords: Kawasaki disease, Arab, Multicenter collaborative, Registry, Cardiac complications, Survey
Introduction
Kawasaki disease (KD) is the most common acquired heart disease in children in most socioeconomically developed countries [1]. The prevalence, clinical findings and cardiac complications are well studied in western countries and Japan [2, 3]. The disease affects children of different ethnicities at different rates due to genetic factors [1, 4, 5]. The clinical findings and cardiac complications have been well described for children with KD in Eastern Asian and in western nations [6]. Data on KD in the Arab countries are limited to case reports and small single-center studies [7, 8]. KD prevalence among Arab descents appears to be higher in North America compared to the countries of origin. In a Canadian multicenter collaborative study of the annual prevalence and complication rates of KD among Arabic community living in the province of Quebec, the prevalence was 4 to 12 times higher than in their countries of origin [9]. The rates of consanguinity in the Arab world are high. Consanguineous marriages constitute 20–50% of all marriages across Arabic countries, including first-cousin unions [10, 11]. This may help understand the genetic factors influencing children affected by KD.
The recent emergence of 2019 coronavirus disease (COVID-19) and the similarity between KD and the Multi-System Inflammatory Syndrome in Children (MIS-C) brought to the stage the importance of studying KD globally [12–20]. Through professional and personal communications among peers in Middle Eastern countries, a growing concern and awareness toward KD was a recurrent theme. A need for a better understanding of each country’s KD status led to a collaborative effort to address unanswered questions. Thus, KD Arab Initiative [Kawarabi] was established with a vision to improve diagnosis, care and outcome of children and adults with KD across different Arab nations and ethnicities by fostering research and multicenter collaboration. Kawarabi strives to improve accurate diagnosis, timely therapy and reduce morbidity and associated mortality. It also plans to improve population-based education on KD, to optimize patient timely access to therapy, and to emphasize cardiovascular surveillance and management of KD patients with coronary artery complications from onset throughout adult life. Ultimately, the goal would be to raise awareness of KD among healthcare providers, in both urban and the rural setting. Improved level of clinical suspicion of KD is a corner stone in identifying cases and providing proper therapy and long-term management [1].
The first goal of Kawarabi was to better understand the burden of KD in Arabic countries and resources available at participating institutions. The objectives of this article were to introduce the Kawarabi to the medical community and to discuss the results of an online survey among Kawarabi’s participating institutions.
Methods
We surveyed all cardiologists, pediatricians, rheumatologists, and any other specialists caring for children and adults with KD in participating Arab institutions. Each institution identified a physician to represent it at Kawarabi and to serve as its principal investigator (PI). PIs were asked to reflect on their care of children with KD and complete a 32-item survey. The survey questions tackled the demographic and geographic profiles of participating countries and institutions, and their approach to acute and long-term management of KD patients. An overview of the KD knowledge level among practicing physicians and general population was also drawn from the survey. (Supplemental Box 1).
The survey was conducted between April, 2021 and October, 2021. The questionnaire was sent to Kawarabi steering committee members for face validity and piloted prior to full launch [21]. PIs were contacted via email and provided with a link to access the survey online. The providers were asked to fill out the survey after obtaining their consent using a web-based standardized survey tool (forms.office Microsoft ®). One survey per institution was collected. The survey took approximately 15 min to complete. Data were collected anonymously and was based on the respondent best estimate. Reminders via email were sent multiple times to participating physicians to fill out the questionnaire and therefore increase the sample size [22]. The survey study was approved by the Institutional Review Board of CHU Sainte-Justine.
Data were summarized as median (interquartiles) for continuous variables, and frequencies and percentages for categorical variables.
Results
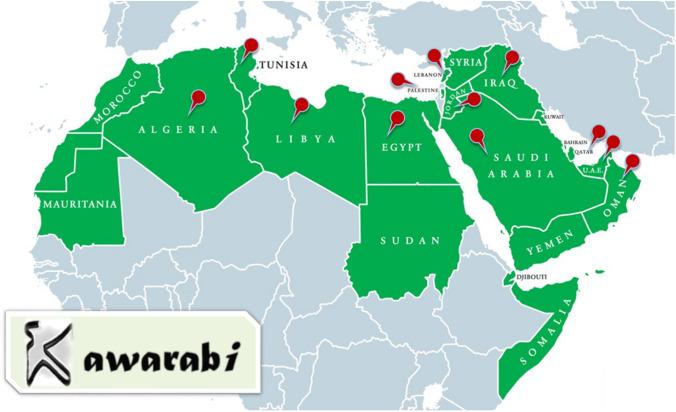
Nineteen physicians from 12 countries participated anonymously in this survey representing 19 out of 20 participating institutions (response rate of 95%). (Fig. 1) Ten (53%) respondents identified as men, 7 (37%) as women and 2 (11%) preferred not to answer. Eighteen (95%) out of nineteen respondents were principal investigators. The reporting physicians had a median of 14 (9–23) years of practice in their current specialty. Fifteen (79%) obtained specialty or sub-specialty training outside the country where they currently practice, while 4 (21%) obtained it in their country of practice. Eight (42%) received a board certification from their own country only, 5 (26%) received a European certificate of Pediatric sub-specialty and 1 (5%) received a European certificate of Pediatrics. Two (11%) received a certification from the American board of Pediatrics, one of these two also received a certificate of the Canadian board of pediatric cardiology. One (5%) physician received a certificate in pediatric cardiac intervention from McGill University. One (5%) completed a Canadian fellowship in pediatric rheumatology. Finally, one (5%) physician received a master’s degree. On a scale from 0 to 5, responders rated their interest to contribute and collaborate with the “Kawarabi project” at 5 (5–5). Fourteen (74%) practiced in centers affiliated with universities, 2 (11%) worked in private clinics, 2 (11%) in government hospitals, and 1 (5%) in a university hospital. Nine (47%) admitted their KD patients to pediatric units within general hospitals and 10 (53%) admitted their patients to free-standing children’s hospitals. The median number of pediatric beds in their primary setting of practice where KD patients were admitted was 52 (23–237). The median number of annual pediatric admissions at the centers was 2500 (1000–5000). The median population size of the city (including close suburbs) where centers were located was 3 (2–5) millions.
Fig. 1.
Countries that participated in the survey. The 12 participating countries are labeled by a red pin
Over the last 10 years, a median 75 (24–105) of children with new onset KD were admitted at the participating centers. Over that same time period a median of 1 (0–3) cases had KD shock syndrome (stated as, requiring admission to intensive care for the management of shock or pre-shock, not related to myocardial ischemia or infarction), a median of 5 (1–6) children with KD who developed giant coronary artery aneurysms (CAAs), and a median of 1 (0–3) cases had or were suspected to have myocardial ischemia/acute coronary syndrome. In the past 10 years, 5 (26%) physicians encountered at least one KD patient who required CA intervention (CA bypass surgery or percutaneous coronary intervention with or without pharmacological thrombolysis). In 2020, respondents encountered 15 (5–29) cases of MIS-C.
Fifteen (79%) centers referred to the 2017 American Heart Association guidelines when managing a patient with KD [1]. Two (11%) referred to 2019 European consensus-based recommendations and the other 2 (11%) used their own adapted institutional consensus guidelines [23].
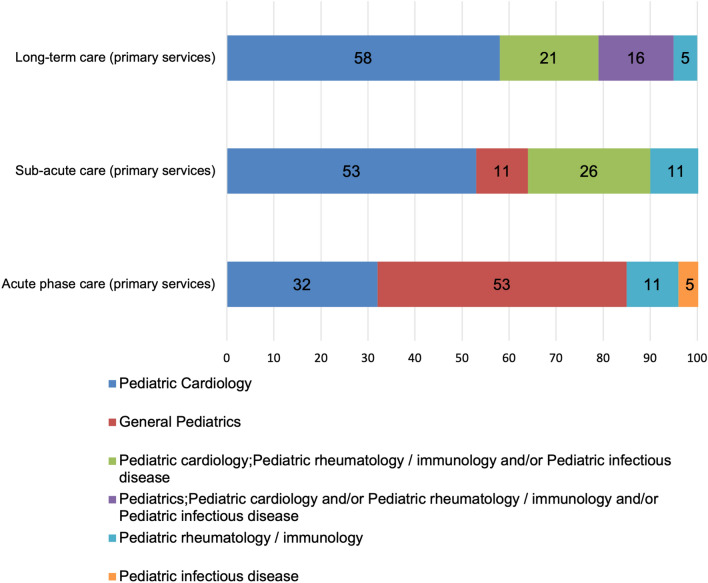
General pediatrics was the primary service managing acute KD in 53% of institutions and pediatric cardiology in 32% (Fig. 2). Also, pediatric cardiology was the service consulted in addition to the primary service during the acute phase admission in 37% of institutions (Fig. 3).
Fig. 2.
Distribution of primary services in charge of the acute, sub-acute and long-term care for KD patients. The data shown are in percentages
Fig. 3.
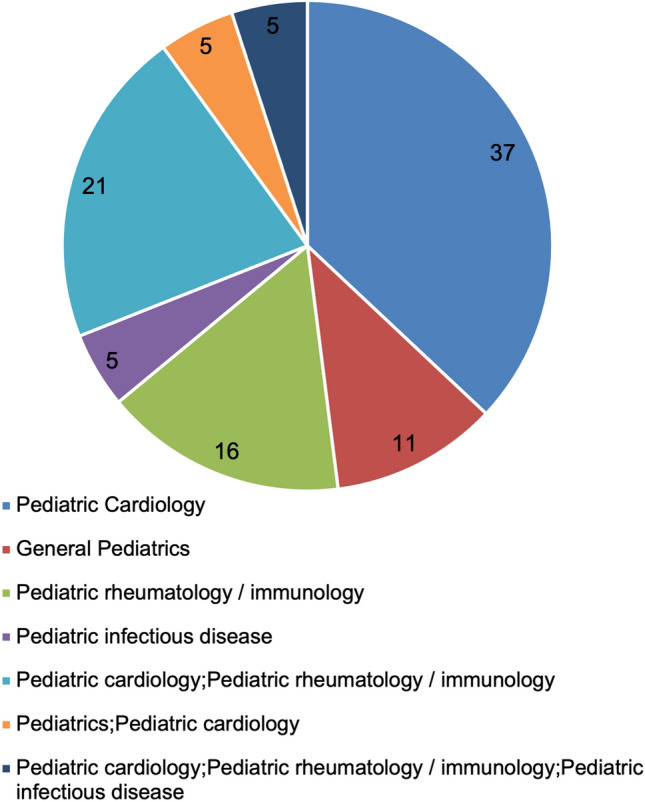
Distribution of services that are consulted in addition to the primary services during the acute phase for KD patients. The data shown are in percentages
Ten (53%) reported that pediatric cardiology was the service in charge of follow-up during the sub-acute phase (first 2 to 3 months) at their center, 4 (21%) responded that it was the pediatric cardiology along with the pediatric rheumatology/immunology services that were responsible for the follow-up, and finally, one reported that pediatric cardiology along with pediatric infectious disease were responsible for the follow-up (Fig. 2).
Eleven (58%) responded that pediatric cardiology was the primary service in charge of long-term follow-up of children with KD, followed by pediatric cardiology along with pediatric rheumatology/immunology in 3 institutions (16%), and pediatric cardiology along with pediatrics in 2 (11%) (Fig. 2).
All the institutions reported using intravenous immunoglobulin (IVIG) 2 g/Kg as first-line therapy when encountering a patient with new onset of KD. Sixteen (84%) reported that IVIG is available in their country and in their institution, 2 (11%) reported that IVIG is available in their country but not available at their center, and one (5%) declared that IVIG is not readily available in their country, but it could be imported on-demand. High-dose Aspirin 70–100 mg/kg/day was the dose used during the acute phase by 10 (53%), followed by medium-dose aspirin 30–50 mg/kg/day used by 7 (37%) and low-dose Aspirin 2–5 mg/kg/day used by one (5%) institution. One (5%) reported that they do not give aspirin for a new onset KD patient.
Physicians were asked to grade the level of knowledge and awareness about KD in their country/city among the general population. The median grade (0 to 10) reported was 3 (2–5). Physicians also graded the knowledge and awareness among the medical community outside their institution at a median of 7 (6–8) and at 8 (7–10) at their institutions.
Discussion
The Kawasaki Disease Arab Initiative (Kawarabi) collaborative is the first multicenter collaborative established in the Middle East to understand the unique aspects of KD in the Arab world to address the challenges the physicians in the region face in managing children with KD. This effort was established to address unanswered questions and missing data in the Arab countries and to ultimately improve the outcome of patients with KD in the Arab region. The establishment of Kawarabi collaborative was based on the objective that multicenter collaboration should improve patient care by the means of networking, educational exchange, and standardizing patient care [24]. Standardization of patient care has previously been shown to improve patient care [22, 25, 26]. Case in point, the National Pediatric Cardiology Quality Improvement Collaborative succeeded in reducing the interstage mortality of children born with hypoplastic left heart syndrome in half [25].
Intravenous immunoglobulins (IVIG) 2 g/kg were unanimously reported as first-line therapy. However, the accessibility varied depending on the institutions. In some institutions, IVIG was not readily available, which means that a KD patient in some Arab countries runs a higher risk of developing CAA. Indeed, timely administrating IVIG is the standard of care and has been associated with a reduction in development of CA abnormalities from 25 to 4% [1]. Advocating for timely therapy is a core principle in the mission of Kawarabi and engagement of stake holders to ensure availability of IVIG across participating centers is vital.
KD remains a rare disease. The annual incidence rate of KD in Northern Africa Arabic countries is low compared to the relative incidence of KD among descents of the same nations living in the province of Quebec, Canada. The relative incidence of KD in Morocco is 3.15/100,000 children < 5 years old, 4.52 in Algeria and 0.95 in Tunisia. In Quebec, data show that relative incidence in children of Moroccan origin is 20.14, 18.31 for the children of Algerian origin and 11.8 for children of Tunisian origin. Thus, compared to countries of origin, the relative incidence of KD in Quebec varies between 4- and 12-folds [9]. When studying rare diseases like KD, there is a benefit from multicenter research and quality improvement collaboratives [27–29]. The International Kawasaki disease registry (IKDR) is a perfect example with more than 34 participating centers before the COVID-19 pandemic (and over 100 centers since, unpublished) [6, 30]. Similar to our efforts, other regional multicenter KD collaboratives were established including Japan, South America, and Europe [3, 31, 32]. To our knowledge, Kawarabi is the first multicenter collaborative to cover patients with KD in the Arabic region. It is expected that the Kawarabi collaboration will result in a future increase of yearly diagnosed cases by the means of increased awareness in general. Increased rate of diagnosis is also enhanced by improving diagnosis of children who present with incomplete clinical criteria of KD [33]. Knowing that children with incomplete clinical criteria are often missed or diagnosed with prejudicial delay, early recognition and administration of proper therapy should result in improved outcome [34]. The high prevalence of consanguinity in Kawarabi collaborating countries could also result in increased clusters of family members of children diagnosed with KD. The 2.1% rate of KD among siblings in Japan is 10 folds higher than the general population [5], and up to 13%, among identical twins [5, 35, 36]. North American genetic studies were limited by the low rate of familial cases of KD due to scarcity of such occurrences in a low consanguinity related offspring society [37]. In contrast, the high consanguinity rate in Arab nations is prone to better identification of clusters of KD relatives in higher proportions. This factor should aid KD genetic research since genetic discoveries in rare diseases are highly powered by substantial numbers of family cases as opposed to clustering sporadic cases [38–40].
Delay in diagnosis of KD contributes to development of cardiac complications [1]. This is of importance as delayed diagnoses were reported in 30 to 62% of children living in northern African Arabic countries [9]. The previously observed delayed diagnosis in Arabic countries highlights the need of national awareness and epidemiological studies. In fact, previous papers have suggested increased awareness might be associated with prompter diagnosis of KD [41]. The current survey showed that the awareness and knowledge about KD among the general population is low despite having a high level of awareness among the medical community. This demonstrates the importance of educating the general population in Arab countries about this disease and how it is treated which is an objective of Kawarabi.
Future Directions for Kawarabi
Kawarabi holds webinars throughout the year on a quarterly basis for the participating physicians to present and discuss relevant topics related to KD and MIS-C in Arabic countries. Also, by creating a discussion group, Kawarabi provides a forum for interprofessional communication where physicians can discuss KD cases. As far as awareness is concerned, the Kawarabi group plans to create a web page accessible to patients, families, and general population to improve their understanding of the disease and have access to different resources in their local language. The organization of conferences and symposia with segments that are dedicated to patients, families and general population is also an objective of Kawarabi.
Limitation
The limitation of the survey was that it covers 50% of all Arab nations. Continued efforts are in place to increase the inclusion of the remaining countries. Knowing that the main obstacles in including the remaining 50% of the Arab nations at this stage is related to the difficulty in identifying physicians with interest or expertise in KD on one hand. On the other hand, some of the non-included nations are stricken with political unrest, low economic status, and limited access to advanced health care, which further underestimates gaps of knowledge across. However, the survey has the strength of covering nearly all Kawarabi participating institutions. Finally, the results of the survey were based on estimates and are not yet linked to the newly established Kawarabi’s multicenter patient registry. In the future we plan to utilize the Kawarabi’s multicenter patient registry to establish prevalence of KD complications in the Arab nations.
Conclusion
The variations in KD management and treatment across Arab countries require solid proactive collaboration. The low awareness and knowledge estimates about KD among the general population contrasted with a high level among the medical community. Projected studies utilizing the Kawarabi collaborative consortium should assess disease burden, complications, and response to treatment among Arab population, foster population-based knowledge, and foster networks to enhance accessibility to expert healthcare providers.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful for Angela J. Doty, MD for her editorial assistance and for all those who contributed to the submission of the surveys including Dr Nassiba Benalikhoudja.
Author Contributions
YA was involved in study design, analysis of data, and drafting the manuscript. NC was involved in study design, analysis of data, and revising the manuscript. ND was involved in study design, analysis of data, and revising the manuscript. NE-K was involved in study design, analysis of data, and revising the manuscript. SYAA was involved in gathering data and revising the manuscript. MEA-S was involved in gathering data and revising the manuscript. HMA was involved in gathering data and revising the manuscript. HA-S was involved in gathering data and revising the manuscript. KSAS was involved in gathering data and revising the manuscript. RA was involved in gathering data and revising the manuscript. AB was involved in gathering data and revising the manuscript. RB was involved in gathering data and revising the manuscript. MMEG was involved in gathering data and revising the manuscript. HME was involved in gathering data and revising the manuscript. NE was involved in gathering data and revising the manuscript. ZF was involved in gathering data and revising the manuscript. MSL was involved in gathering data and revising the manuscript. PM was involved in gathering data and revising the manuscript. AFS was involved in gathering data and revising the manuscript. RGR was involved in gathering of data and revising the manuscript. ASH was involved in study design, analysis of data, and drafting the manuscript. This submission is with the full knowledge and approval of the listed coauthors.
Funding
Fonds BoBeau Coeur, Division of Pediatric Cardiology, CHU Sainte-Justine. Dr. Harahsheh is supported by a Sub-agreement from the Johns Hopkins University with funds provided by Grant No. R61HD105591 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the Office of the Director, National Institute of Health (OD). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development, the Office of the Director, National Institute of Health (OD), the National Institute of Health, the NIBIB, the NHLBI, or the Johns Hopkins University. Non-financial interest: Dr. Harahsheh serves as a scientific advisory board member of OP2 DRUGS (“OP2”). This advisory position has no relevant disclosures for this manuscript.
Availability of Data and Material
Data will be available upon a reasonable request.
Declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
The survey study was approved by the Institutional Review Board of CHU Sainte-Justine. Informed consent was obtained from survey participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yousra Arab, Email: yousra.arab@usherbrooke.ca.
Nadine Choueiter, Email: nchoueit@montefiore.org.
Nagib Dahdah, Email: Nagib.dahdah.hsj@ssss.gouv.qc.ca.
Nermeen El-Kholy, Email: nermeen.elkholy78@gmail.com.
Sima Y. Abu Al-Saoud, Email: simaabualsaoud@yahoo.com
Mohammed E. Abu-Shukair, Email: mabushukair@yahoo.com
Hala M. Agha, Email: halaazza@gmail.com
Hesham Al-Saloos, Email: halsaloos@sidra.org.
Khalfan Salim Al Senaidi, Email: alsineidiksk@hotmail.com.
Raed Alzyoud, Email: raedalzyoud@gmail.com.
Asma Bouaziz, Email: asma.bouaziz@rns.tn.
Rachida Boukari, Email: rachida_boukari@yahoo.fr.
Mona M. El Ganzoury, Email: monaelganzoury@yahoo.com
Hala M. Elmarsafawy, Email: halamarsafawy@gmail.com
Najat ELrugige, Email: najatrugige@gmail.com.
Zohra Fitouri, Email: drzohrafitouri@gmail.com.
Mohamed S. Ladj, Email: samirladj64@yahoo.fr
Pierre Mouawad, Email: pamouawad@stgeorgehospital.org.
Aso F. Salih, Email: aso.salih@univsul.edu.iq
Rocio G. Rojas, Email: rocio.rojas.hsj@ssss.gouv.qc.ca
Ashraf S. Harahsheh, Email: aharahsh@childrensnational.org
References
- 1.McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 2.Zhang MM, Shi L, Li XH, Lin Y, Liu Y. Clinical analysis of Kawasaki disease shock syndrome. Chin Med J. 2017;130(23):2891–2892. doi: 10.4103/0366-6999.219151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yanagawa H, Nakamura Y, Yashiro M, et al. Results of the nationwide epidemiologic survey of Kawasaki disease in 1995 and 1996 in Japan. Pediatrics. 1998;102(6):E65. doi: 10.1542/peds.102.6.e65. [DOI] [PubMed] [Google Scholar]
- 4.Davies HD, Kirk V, Jadavji T, Kotzin BL. Simultaneous presentation of Kawasaki disease and toxic shock syndrome in an adolescent male. Pediatr Infect Dis J. 1996;15(12):1136–1138. doi: 10.1097/00006454-199612000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Fujita Y, Nakamura Y, Sakata K, et al. Kawasaki disease in families. Pediatrics. 1989;84(4):666–669. doi: 10.1542/peds.84.4.666. [DOI] [PubMed] [Google Scholar]
- 6.McCrindle BW, Manlhiot C, Newburger JW, et al. Medium-term complications associated with coronary artery aneurysms after Kawasaki disease: a study from the International Kawasaki Disease Registry. J Am Heart Assoc. 2020;9(15):e016440. doi: 10.1161/JAHA.119.016440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Ammouri I, Al-Wahsh S, Khuri-Bulos N. Kawasaki disease in Jordan: demographics, presentation, and outcome. Cardiol Young. 2012;22(4):390–395. doi: 10.1017/S1047951111001818. [DOI] [PubMed] [Google Scholar]
- 8.Majeed HA, Olson IA. Kawasaki disease in Kuwait. A report of two cases. Acta Paediatr Scand. 1978;67(4):525–528. doi: 10.1111/j.1651-2227.1978.tb16364.x. [DOI] [PubMed] [Google Scholar]
- 9.Gorrab AA, Fournier A, Bouaziz AA, et al. Incidence rate and epidemiological and clinical aspects of Kawasaki disease in children of Maghrebi origin in the province of Quebec, Canada, compared to the country of origin. Glob Pediatr Health. 2016;3:2333794X16630670. doi: 10.1177/2333794X16630670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Gazali L, Hamamy H. Consanguinity and dysmorphology in Arabs. Hum Hered. 2014;77(1–4):93–107. doi: 10.1159/000360421. [DOI] [PubMed] [Google Scholar]
- 11.Tadmouri GO, Nair P, Obeid T, Al Ali MT, Al Khaja N, Hamamy HA. Consanguinity and reproductive health among Arabs. Reprod Health. 2009;6:17. doi: 10.1186/1742-4755-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elias MD, McCrindle BW, Larios G, et al. Management of multisystem inflammatory syndrome in children associated with COVID-19: a survey from the International Kawasaki Disease Registry. CJC Open. 2020;2(6):632–640. doi: 10.1016/j.cjco.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loke YH, Berul CI, Harahsheh AS. Multisystem inflammatory syndrome in children: is there a linkage to Kawasaki disease? Trends Cardiovasc Med. 2020;30(7):389–396. doi: 10.1016/j.tcm.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harahsheh AS, Dahdah N, Newburger JW, et al. Missed or delayed diagnosis of Kawasaki disease during the 2019 novel coronavirus disease (COVID-19) pandemic. J Pediatr. 2020;222:261–262. doi: 10.1016/j.jpeds.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeBiasi RL, Harahsheh AS, Srinivasalu H, et al. Multisystem inflammatory syndrome of children: sub-phenotypes, risk factors, biomarkers, cytokine profiles and viral sequencing. J Pediatr. 2021;237:125–135. doi: 10.1016/j.jpeds.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Harahsheh AS, Dahdah N, Newburger JW, et al. Reply. J Pediatr. 2020;224:184–185. doi: 10.1016/j.jpeds.2020.06.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harahsheh AS, Sharron MP, Bost JE, et al. Comparison of first and second wave cohorts of multisystem inflammatory disease syndrome IN children. Pediatr Infect Dis J. 2022;41(1):e21–e25. doi: 10.1097/INF.0000000000003388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hejazi OI, Loke YH, Harahsheh AS. Short-term cardiovascular complications of multi-system inflammatory syndrome in children (MIS-C) in adolescents and children. Curr Pediatr Rep. 2021;9:93–103. doi: 10.1007/s40124-021-00258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kline JN, Isbey SC, McCollum NL, et al. Identifying pediatric patients with multisystem inflammatory syndrome in children presenting to a pediatric emergency department. Am J Emerg Med. 2022;51:69–75. doi: 10.1016/j.ajem.2021.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Harahsheh AS, Krishnan A, DeBiasi RL, et al. Cardiac echocardiogram findings of severe acute respiratory syndrome coronavirus-2-associated multi-system inflammatory syndrome in children. Cardiol Young. 2021 doi: 10.1017/S1047951121003024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harahsheh AS, Ottolini M, Lewis K, Blatt B, Mitchell S, Greenberg L. An innovative pilot curriculum training pediatric residents in referral and communication skills on a cardiology rotation. Acad Pediatr. 2016;16(7):700–702. doi: 10.1016/j.acap.2016.05.146. [DOI] [PubMed] [Google Scholar]
- 22.Harahsheh AS, Hom LA, Clauss SB, et al. The impact of a designated cardiology team involving telemedicine home monitoring on the care of children with single-ventricle physiology after norwood palliation. Pediatr Cardiol. 2016;37(5):899–912. doi: 10.1007/s00246-016-1366-y. [DOI] [PubMed] [Google Scholar]
- 23.de Graeff N, Groot N, Ozen S, et al. European consensus-based recommendations for the diagnosis and treatment of Kawasaki disease—the SHARE initiative. Rheumatology. 2019;58(4):672–682. doi: 10.1093/rheumatology/key344. [DOI] [PubMed] [Google Scholar]
- 24.Harahsheh AS, Kipps AK, Hart SA, et al. High acuity therapy variation across pediatric acute care cardiology units: results from the pediatric acute care cardiology collaborative hospital surveys. Pediatr Cardiol. 2021;42(5):1074–1081. doi: 10.1007/s00246-021-02584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson JB, Beekman RH, 3rd, Kugler JD, et al. Improvement in interstage survival in a national pediatric cardiology learning network. Circ Cardiovasc Qual Outcomes. 2015;8(4):428–436. doi: 10.1161/CIRCOUTCOMES.115.001956. [DOI] [PubMed] [Google Scholar]
- 26.Clauss SB, Anderson JB, Lannon C, et al. Quality improvement through collaboration: the National Pediatric Quality improvement Collaborative initiative. Curr Opin Pediatr. 2015;27(5):555–562. doi: 10.1097/MOP.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 27.Hoggart C, Shimizu C, Galassini R, et al. Identification of novel locus associated with coronary artery aneurysms and validation of loci for susceptibility to Kawasaki disease. Eur J Hum Genet. 2021;29:1734–1744. doi: 10.1038/s41431-021-00838-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teitel DF, Newburger JW, Sutton N, et al. Development and utility of quality metrics for ambulatory pediatric cardiology in Kawasaki disease. Clin Pediatr. 2020;59(3):245–251. doi: 10.1177/0009922819896098. [DOI] [PubMed] [Google Scholar]
- 29.Osborne J, Friedman K, Runeckles K, et al. Comparison between currently recommended long-term medical management of coronary artery aneurysms after Kawasaki disease and actual reported management in the last two decades. Pediatr Cardiol. 2021;42(3):676–684. doi: 10.1007/s00246-020-02529-2. [DOI] [PubMed] [Google Scholar]
- 30.Manlhiot C, Newburger JW, Low T, et al. Low-molecular-weight heparin vs warfarin for thromboprophylaxis in children with coronary artery aneurysms after Kawasaki disease: a pragmatic registry trial. Can J Cardiol. 2020;36(10):1598–1607. doi: 10.1016/j.cjca.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Mata A, Ulloa-Gutierrez R, Brea J, Soza G, Tremoulet AH. Origin and importance of the Latin American Kawasaki Disease Network (REKAMLATINA) Rev Chilena Infectol. 2014;31(3):330–332. doi: 10.4067/S0716-10182014000300012. [DOI] [PubMed] [Google Scholar]
- 32.Salo E, Griffiths EP, Farstad T, et al. Incidence of Kawasaki disease in northern European countries. Pediatr Int. 2012;54(6):770–772. doi: 10.1111/j.1442-200X.2012.03692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yellen ES, Gauvreau K, Takahashi M, et al. Performance of 2004 American Heart Association recommendations for treatment of Kawasaki disease. Pediatrics. 2010;125(2):e234–241. doi: 10.1542/peds.2009-0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Minich LL, Sleeper LA, Atz AM, et al. Delayed diagnosis of Kawasaki disease: what are the risk factors? Pediatrics. 2007;120(6):e1434–1440. doi: 10.1542/peds.2007-0815. [DOI] [PubMed] [Google Scholar]
- 35.Harada F, Sada M, Kamiya T, Yanase Y, Kawasaki T, Sasazuki T. Genetic analysis of Kawasaki syndrome. Am J Hum Genet. 1986;39(4):537–539. [PMC free article] [PubMed] [Google Scholar]
- 36.Kottek A, Shimizu C, Burns JC. Kawasaki disease in monozygotic twins. Pediatr Infect Dis J. 2011;30(12):1114–1116. doi: 10.1097/INF.0b013e31822ac4ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dergun M, Kao A, Hauger SB, Newburger JW, Burns JC. Familial occurrence of Kawasaki syndrome in North America. Arch Pediatr Adolesc Med. 2005;159(9):876–881. doi: 10.1001/archpedi.159.9.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uehara R, Yashiro M, Nakamura Y, Yanagawa H. Clinical features of patients with Kawasaki disease whose parents had the same disease. Arch Pediatr Adolesc Med. 2004;158(12):1166–1169. doi: 10.1001/archpedi.158.12.1166. [DOI] [PubMed] [Google Scholar]
- 39.Onouchi Y. Genetics of Kawasaki disease: what we know and don't know. Circ J. 2012;76(7):1581–1586. doi: 10.1253/circj.CJ-12-0568. [DOI] [PubMed] [Google Scholar]
- 40.Sham PC, Purcell SM. Statistical power and significance testing in large-scale genetic studies. Nat Rev Genet. 2014;15(5):335–346. doi: 10.1038/nrg3706. [DOI] [PubMed] [Google Scholar]
- 41.Pascall B, Thakker A, Foo Y, Thakker P. Immunoglobulin for Kawasaki disease: a 3-year retrospective audit. BMJ Paediatr Open. 2019;3(1):e000451. doi: 10.1136/bmjpo-2019-000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be available upon a reasonable request.