Abstract
(1) Background: The COVID-19 pandemic has indirect consequences for healthcare for other diseases, known as collateral damage. This situation heavily affects healthcare systems, causing changes in patterns of hospital admission. During the peak of the coronavirus disease 2019 pandemic, numerous studies reported a reduction in admissions for acute coronary syndrome. The aim of this study was to evaluate the incidence of admissions for cardiovascular diseases in Abruzzo, a region of Southern Italy, in the year 2020 and compare it to the two previous years (2018–2019). (2) Methods: This retrospective study was conducted in Abruzzo, Italy. The monthly number of admissions in the year 2020 was compared to a control period made from the average number of events that occurred in the previous two years (2018–2019). (3) Results: A global reduction in hospital admissions for all the cardiovascular diseases (CVDs) considered was observed. In particular, compared to the control period, in 2020, the number of admissions for ST-segment elevation myocardial infarction (STEMI) was lower by 34 (hospitalization rate ratio, HRR, 0.93; p < 0.001), the number of non-ST-segment-elevation myocardial infarctions (N-STEMI) was lower by 154.5 (HRR 0.89; p < 0.001), the number for acute coronary syndrome (ACS) was 340 lower (HRR 0.90; p < 0.001) and the number for heart failure (HF) was 1424.5 lower than during the control period (HRR 0.73; p < 0.001). (4) Conclusions: The results of this study show the impact of COVID-19 on admissions for CVDs, suggesting the need for strategic measures to overcome the burden of hospitalizations in future years.
Keywords: COVID-19, cardiovascular disease, hospital admission, healthcare services, HDR, Italy
1. Introduction
From December 2019, an emerging infectious disease caused by coronavirus disease 2019 (COVID-19) rapidly spread around the globe [1,2]. It was subsequently classified as a pandemic by the World Health Organization (WHO) [3]. The pandemic heavily affected health systems, with high hospitalizations and fatality rates. In addition to the direct impact of COVID-19 on morbidity and mortality, the pandemic had indirect effects on healthcare for other diseases, known as collateral damage [4]. In Italy, after the infectious disease spread, the government adopted a state-wide lockdown. This measure, along with the conversion of several hospitals in specific centers to treat only COVID-19 patients, led to a drastic reduction in non-COVID-19 specialist outpatient performances. This situation heavily affected the healthcare system, causing changes in patterns of hospital admission [4,5]. Routine diagnostic procedures and elective admissions were cancelled or postponed due to the focus on the care of patients with COVID-19 [6]. During the peak of the COVID-19 pandemic, numerous hospitals across Europe and the United States of America (USA) reported a reduction in admissions for acute coronary syndrome (ACS), which correlates with higher case fatality and complication rates [4,5,7]. These situations cause concern among physicians and public health authorities about the prognosis of patients with ACS and other cardiovascular diseases (CVDs) because the outcomes of these events depend largely on rapid diagnosis and therapy [7]. Previous studies reported a reduction in admissions for CVDs in several hospitals in Europe [8] and Italy [5], but none of these reported data from an entire region through comparison with two previous years from pandemic. The aim of this study was to evaluate the incidence of admissions for CVDs in a Southern Italian Southern region in the year 2020 and compare it to the two previous years (2018–2019).
2. Materials and Methods
2.1. Study Design
This retrospective study was conducted in Abruzzo, a region of Southern Italy with about 1.3 million inhabitants. The number of CVD admissions (as indicated below) that occurred in the year 2020 was studied and compared to the average number of the same events that occurred in the previous two years (2018–2019) [9,10]. Data were collected from hospital discharge records (HDR), which included information on patients’ demographic characteristics, the diagnosis-related group (DRG) used to classify the admission and a maximum of six diagnoses (one principal diagnosis and up to five comorbidities) and six procedures that occurred during the hospitalization. Diagnoses and procedures were coded according to the International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM), the National Center for Health Statistics (NCHS) and the Centers for Medicare and Medicaid Services External, Atlanta, GA, USA. The study considered cardiovascular hospitalizations concerning the following categories and through the following coding:
Acute coronary syndrome (ACS): discharge with a principal diagnosis of ICD-9-CM 410.xx, 411.xx, or 413.xx
ST-segment elevation myocardial infarction (STEMI): discharge with a principal or secondary diagnosis of ICD-9-CM 410.xx, excluding those with principal or secondary diagnosis of 410.7x or 410.9x
Non-ST-segment elevation myocardial infarction (N-STEMI): discharge with principal or secondary diagnosis of ICD-9-CM 410.7x, excluding those with a principal or secondary diagnosis of 410.9x
Heart failure (HF): discharge with a principal diagnosis of ICD-9-CM 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.0, 428.1, 428.2x, 428.3x, 428.4x, or 428.9.
Monthly number of admissions in the year 2020 was compared to the equivalent value for a control period comprising the average number of events that occurred in the previous two years (2018–2019).
2.2. Statistical Analysis
Quantitative variables were summarized as mean and standard deviation (SD) or median and interquartile range (IQR), according to their distribution. Qualitative variables were summarized as frequency and percentage. Incidence rate ratios comparing the study period with each of the control periods were expressed as Hospital Rate Ratio (HRR) with a 95% confidence interval (95% CI) and were calculated using the Poisson regression, adjusted for age, gender and hospital. For all analyses, a p-value ≤ 0.05 was assumed to be statistically significant (two-tailed). Statistical analyses were performed using STATA v14 software (StataCorp LLC, College Station, TX, USA).
3. Results
During the study period in the Abruzzo region, 1019 patients were admitted for STEMI, 1248 patients were admitted for N-STEMI, 3809 patients were admitted for ACS and 3736 patients were admitted for HF, as reported in Table 1.
Table 1.
Comparison of admissions that occurred between 2020 and the mean of the years 2018–2019.
| 2018 | 2019 | Mean between 2018–2019 (SD) | 2020 | Diff. | p-Value * | |
|---|---|---|---|---|---|---|
| STEMI | ||||||
| Admissions | 1096 | 1010 | 1053 (11.7) | 1019 | −34.0 | |
| Age | ||||||
| 18–44 | 35 | 168 | 101.5 (8.7) | 37 | −64.5 | <0.001 |
| 45–74 | 669 | 492 | 580.5 (8.9) | 653 | 72.5 | |
| ≥75 | 392 | 350 | 371 (16.7) | 329 | −42.0 | |
| LOS median (IQR) | 6.5 (5–10) | 6 (5–9) | 6 (5–10) | 6 (5–9) | 0.146 | |
| Death (N%) | 115 | 112 | 113.5(10.8) | 107(10.5) | −6.5 | 0.808 |
| N-STEMI | ||||||
| Admissions | 1.512 | 1.293 | 1402.5 (20.8) | 1248 | −154.5 | |
| Age | ||||||
| 18–44 | 38 | 217 | 127.5 (18.2) | 19 | −108.5 | <0.001 |
| 45–74 | 776 | 627 | 701.5 (18.3) | 687 | −14.5 | |
| ≥75 | 698 | 449 | 573.5 (26.1) | 542 | −31.5 | |
| LOS median (IQR) | 6 (4–10) | 6 (4–9) | 4 (2–10) | 6 (4–9) | 0.444 | |
| Death (N%) | 79 | 80 | 79.5 (5.7) | 62 (5) | −17.5 | 0.546 |
| ACS | ||||||
| Admissions | 4489 | 3809 | 4149 (26.2) | 3809 | −340.0 | |
| Age | ||||||
| 18–44 | 103 | 622 | 362.5 (25.3) | 77 | −285.5 | <0.001 |
| 45–74 | 20,794 | 1929 | 2361.5 (25.6) | 2407 | 45.5 | |
| ≥75 | 1592 | 1258 | 1425 (61.2) | 1325 | −100.0 | |
| LOS median (IQR) | 5 (2–8) | 5 (2–8) | 5 (2–8) | 5 (2–8) | 0.009 | |
| Death (N%) | 200 | 199 | 199.5 (4.8) | 161 (4.2) | −38.5 | 0.382 |
| HF | ||||||
| Admissions | 5738 | 4583 | 5160.5 (78.6) | 3736 | −1424.5 | |
| Age | ||||||
| 18–44 | 31 | 763 | 397 (69.8) | 28 | −369.0 | <0.001 |
| 45–74 | 1.296 | 1.925 | 1610.5 (68.5) | 1047 | −563.5 | |
| ≥75 | 4.411 | 1.895 | 3153 (96.9) | 2661 | −492.0 | |
| LOS median (IQR) | 8 (5–12) | 8 (5–12) | 8 (5–12) | 8 (5–12) | 0.615 | |
| Death (N%) | 536 | 426 | 481 (9.32) | 321 (8.59) | −160.0 | 0.482 |
* Absolute difference between year 2020 and the mean of years 2018–2019. STEMI: ST-segment-elevation myocardial infarction; N-STEMI: non-ST-segment-elevation myocardial infarction; ACS: acute coronary syndrome; HF: Heart failure; LOS: length of stay; IQR: interquartile range.
A global reduction in hospital admissions for all the CVDs considered was observed, as reported in Table 2. In particular, compared to the control period, in 2020, there were 34 fewer admissions for STEMI (HRR 0.93; 95% CI 0.92–0.94; p < 0.001), the value for N-STEMI was lower by 154.5 (HRR 0.89; 95% CI 0.88–0.90; p < 0.001) and the value for ACS was lower by 340 (HRR 0.90; 95% CI 0.89–0.90; p < 0.001). The main reduction was observed for the HF admissions, which were lower by 1424.5 than during the control period (HRR 0.73; 95% CI 0.73–0.73; p < 0.001).
Table 2.
Hospitalization rate ratios of CVDs in 2020 compared to the two-year period of 2018–2019.
| HRR (95% CI) | p-Value * + | |
|---|---|---|
| STEMI | ||
| 2020 vs. 2018–2019 | 0.93 (0.92–0.94) | <0.001 |
| Male vs. female | 0.99 (0.98–1.00) | 0.331 |
| Age | ||
| 18–44 | Ref. | |
| 45–74 | 0.99 (0.98–1.00) | 0.523 |
| ≥75 | 0.99 (0.98–1.01) | 0.948 |
| N-STEMI | ||
| 2020 vs. 2018–2019 | 0.89 (0.88–0.90) | <0.001 |
| Male vs. female | 1.00 (0.99–1.00) | 0.338 |
| Age | ||
| 18–44 | Ref. | |
| 45–74 | 0.99 (0.97–1.00) | 0.062 |
| ≥75 | 0.98 (0.97–0.99) | 0.015 |
| ACS | ||
| 2020 vs. 2018–2019 | 0.90 (0.89–0.90) | <0.001 |
| Male vs. female | 1.00 (1.00–1.00) | 0.003 |
| Age | ||
| 18–44 | Ref. | |
| 45–74 | 0.99 (0.99–1.00) | 0.925 |
| ≥75 | 1.00 (0.89–0.90) | 0.978 |
| HF | ||
| 2020 vs. 2018–2019 | 0.73 (0.73–0.73) | <0.001 |
| Male vs. female | 1.00 (0.99–1.00) | 0.073 |
| Age | ||
| 18–44 | Ref. | |
| 45–74 | 1.00 (0.99–1.00) | 0.312 |
| ≥75 | 1.00 (0.99–1.00) | 0.186 |
* All models were adjusted for hospital. + Poisson regression. STEMI: ST-segment-elevation myocardial infarction; N-STEMI: non-ST-segment-elevation myocardial infarction; ACS: acute coronary syndrome; HF: Heart failure; LOS: length of stay; 95% CI: 95% confidence interval; IQR: interquartile range.
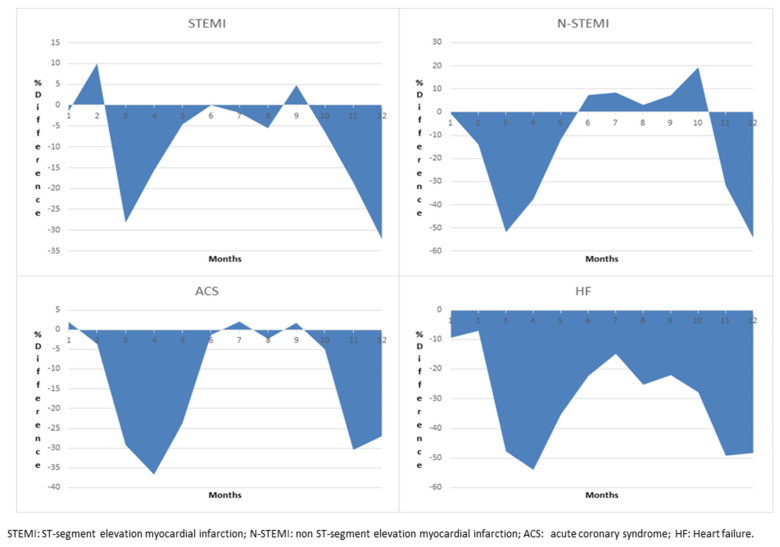
No differences were found in terms of length of stay (LOS) or in-hospital mortality during the study periods (Table 1). At the same time, a significant difference was found in the patients’ age, with a reduction in hospitalization, particularly for patients aged less than 75 years. According to the monthly incidence of CVD admissions, the strong reduction was observed between February and June 2020 and during the last three months of the year, as shown in Figure 1.
Figure 1.
Monthly differences in CVD admissions by month in 2020.
4. Discussion
The COVID-19 pandemic has placed a heavy burden on hospitals across the world. This study assessed hospital admissions for CVDs using HDR in a region of Southern Italy, in comparison with two previous years. During the COVID-19 pandemic in 2020, there was a significant decrease in hospital admissions for CVDs compared to the previous two years in the Abruzzo region, in Italy. This result is in line with the previous literature, confirming findings from across Italy and Europe [4,5,11]. There was a clear impact at the start of the lockdown, with no patients with CVDs being admitted to hospital during the first period of the year. This can be explained by the presence of a state lockdown in Italy, reflecting the general population’s fear of using emergency services [12]. In order to explain these decreases, it should be considered that patients might be reluctant to seek hospital care for fear of infection or contagion [13,14]. A previous cross-sectional study conducted in the United Kingdom showed that patients were afraid of being exposed to COVID-19 and were worried of about increasing the pressure on the United Kingdom’s already overburdened healthcare system [15,16]. The reluctance to seek emergency care seems to be more prevalent in less severe cases [17]. The observed reduction in admissions could be also explained by the adaptation of the healthcare system to the pandemic. Higher limits for referrals to hospitals or emergency departments, lower intensive care unit (ICU) capacity, declines in ambulatory cardiovascular visits, or delays in the treatment of less urgent cases can all cause an overall reduction in hospital admissions [7,18]. On the other hand, previous studies suggested the presence of an increased severity of COVID-19-related symptoms in patients with CVDs [18]. This is also supported by the findings of a study from China, where COVID-19 patients who required intensive care admissions were more likely to suffer from CVDs than non-ICU patients [19]. As consequence, this could increase the risk of patients admitted for COVID-19 symptoms being undiagnosed due to the medical focus on COVID-19. With regard to gender, several studies investigated the sex differences in the impact of COVID-19 on the care and management of ACS [5,20,21,22,23,24,25,26], observing no difference between genders, whereas two studies reported a reduction in STEMI-related admissions among women compared to men [5,22]. Clinicians raised a significant concern about the increased number of cardiovascular cases in hospitals in the future due the presentations that were previously hidden or stable during the pandemic period. In addition, as a consequence of this crisis, in the immediate future, there could be a surge of patients with delayed complications of ACS and reinfarctions [27]. The impact of COVID-19 also affected other conditions, such as strokes [28] and kidney disease [29]. In addition, the social distancing policy caused a lower number of admissions for injuries and traffic accidents [30].
The strength of this study is the large sample analyzed and the long study period considered. This is the first study to have been conducted in Italy considering all the hospital admissions occurring in an entire region. In addition, this study compared the incidence in 2020 with those of two different control years. In comparison with previous studies conducted in Italy and the UK [26], this study confirmed the reduction in both STEMI and non-STEMI admissions. In addition, this is one of first studies to also investigate HF admissions.
However, the results of this study should be considered in the light of the following limitations. Firstly, the selection of the diagnoses was based on ICD-9-CM codes that did not consider the severity of the diseases. Second, the use of administrative data may have been limited by the lack of some clinical information, while some diagnostic codes could have been under-reported or incorrect. Third, information about out-of-hospital mortality was lacking, so the excess mortality during the study period cannot be calculated.
5. Conclusions
The results of this study have immediate relevance for cardiovascular clinicians and public health authorities. They showed the impact of the COVID-19 pandemic on admissions for CVDs, highlighting the need for strategic measures to overcome the burden of hospitalizations future years, especially in the event of future lockdowns, in order to raise the awareness of health professionals and educate patients to call the emergency services if cardiac symptoms occur.
Acknowledgments
The authors are very grateful to the Department of Health and Welfare of the Abruzzo Region (Servizio Governo Dati e Flussi Informativi) for providing the data.
Author Contributions
Conceptualization, F.C., G.D.M., F.R. and T.S.; methodology, G.D.M. and F.C.; software, F.C. and P.D.G.; validation, G.D.M., E.G. and E.T.; formal analysis, F.C. and G.D.M.; data curation, F.C., E.T. and G.D.M.; writing—original draft preparation, G.D.M., F.C. and P.D.G.; writing—review and editing, E.G., E.T., F.R., P.D.G. and T.S.; supervision, F.R. and T.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in conformity with the regulations on data management of the Regional Health Authority of Abruzzo and with the Italian Law on privacy (Art. 20–21 DL 196/2003), published in the Official Journal, n. 190, on 14 August 2004. The data were encrypted prior to the analysis at the regional statistical office, where each patient was assigned a unique identifier. The identifiers eliminated the possibility of tracing the patients’ identities. According to Italian legislation, the use of administrative data does not require any written informed consent from patients.
Informed Consent Statement
The use of administrative data did not require specific written informed consent from the patients.
Data Availability Statement
Data available on request due to privacy and ethical restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–773. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. [(accessed on 1 October 2021)]. Available online: https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audioemergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf.
- 4.De Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A., Secco G.G., Campo G., Gallone G., Verardi R., et al. Reduced Rate of Hospital Admissions for ACS during COVID-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P., Mancone M., Mercuro G., Muscoli S., Nodari S., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) [(accessed on 1 October 2021)];2020 Available online: https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- 7.Kiss P., Carcel C., Hockham C., Peters S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: A systematic review. Eur. Heart J.—Qual. Care Clin. Outcomes. 2020;7:18–27. doi: 10.1093/ehjqcco/qcaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.König S., Ueberham L., Pellissier V., Hohenstein S., Meier-Hellmann A., Thiele H., Ahmadli V., Borger M.A., Kuhlen R., Hindricks G., et al. Hospitalization deficit of in- and outpatient cases with cardiovascular diseases and utilization of cardiological interventions during the COVID-19 pandemic: Insights from the German-wide helios hospital network. Clin. Cardiol. 2021;44:392–400. doi: 10.1002/clc.23549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Di Martino G., Di Giovanni P., Cedrone F., Meo F., Scampoli P., Romano F., Staniscia T. Hospitalization for Short-Term Diabetes-Related Complications: Focus on Patients Aged over 85 Years. Healthcare. 2021;9:460. doi: 10.3390/healthcare9040460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Martino G., Di Giovanni P., Cedrone F., D’Addezio M., Meo F., Scampoli P., Romano F., Staniscia T. The Burden of Diabetes-Related Preventable Hospitalization: 11-Year Trend and Associated Factors in a Region of Southern Italy. Healthcare. 2021;9:997. doi: 10.3390/healthcare9080997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiong T.-Y., Redwood S., Prendergast B., Chen M. Coronaviruses and the cardiovascular system: Acute and long-term implications. Eur. Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez-Marco A., Rosser B., Harky A., Verdichizzo D., McPherson I., Hope E., Qadri S., Oo A., Tsang G., Cale A., et al. The fate of patients with acute aortic syndrome during the coronavirus (COVID-19) pandemic: A UK multicenter study. JTCVS Open. 2021;5:17–25. doi: 10.1016/j.xjon.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wessler B., Kent D.M., Konstam M.A. Fear of Coronavirus Disease 2019—An Emerging Cardiac Risk. JAMA Cardiol. 2020;5:981–998. doi: 10.1001/jamacardio.2020.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moroni F., Gramegna M., Ajello S., Beneduce A., Baldetti L., Vilca L.M., Cappelletti A., Scandroglio A.M., Azzalini L. Collateral damage: Medical care avoidance behavior among patients with acute coronary syndrome during the COVID-19 pandemic. JACC Case Rep. 2020;2:1620–1624. doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.British Heart Foundation [(accessed on 12 August 2020)]. Available online: https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-outbreak.
- 16.Wright J. Coronavirus Doctor’s Diary: Is Lock down Good for Your Heart? [(accessed on 12 August 2020)]. Available online: https://www.bbc.co.uk/news/health-52535044.
- 17.Baracchini C., Pieroni A., Viaro F., Cianci V., Cattelan A.M., Tiberio I., Munari M., Causin F. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol. Sci. 2020;41:1003–1005. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., Brown T.S., Der-Nigoghossian C., Zidar D.A., Haythe J., et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., Bi Z., Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Popovic B., Varlot J., Metzdorf A.P., Jeulin H., Goehringer F., Camenzind E. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter. Cardiovasc. Interv. 2021;97:E319–E326. doi: 10.1002/ccd.29114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reinstadler S.J., Reindl M., Lechner I., Holzknecht M., Tiller C., Roithinger F.X., Frick M., Hoppe U.C., Jirak P., Berger R., et al. Effect of the COVID-19 Pandemic on Treatment Delays in Patients with ST-Segment Elevation Myocardial Infarction. J. Clin. Med. 2020;9:2183. doi: 10.3390/jcm9072183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salarifar M., Ghavami M., Poorhosseini H., Masoudkabir F., Jenab Y., Amirzadegan A., Alidoosti M., Aghajani H., Bozorgi A., Hosseini K., et al. Management and outcomes of ST-segment elevation myocardial infarction during coronavirus 2019 pandemic in a center with 24/7 primary angioplasty capability: Should we change our practice during outbreak? MedRxiv. 2020 doi: 10.1101/2020.05.02.20088302. [DOI] [Google Scholar]
- 23.Gitt A.K., Karcher A.K., Zahn R., Zeymer U. Collateral damage of COVID-19-lockdown in Germany: Decline of NSTE-ACS admissions. Clin. Res. Cardiol. 2020;109:1585–1587. doi: 10.1007/s00392-020-01705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gluckman T.J., Wilson M.A., Chiu S.-T., Penny B.W., Chepuri V.B., Waggoner J.W., Spinelli K.J. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020;5:1419. doi: 10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammad T.A., Parikh M., Tashtish N., Lowry C.M., Gorbey D., Forouzandeh F., Filby S.J., Wolf W.M., Costa M.A., Simon D.I., et al. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID -19 epicenter. Catheter. Cardiovasc. Interv. 2020;97:208–214. doi: 10.1002/ccd.28997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mafham M.M., Spata E., Goldacre R., Gair D., Curnow P., Bray M., Hollings S., Roebuck C., Gale C.P., Mamas M.A., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kulkarni P., Mahadevappa M. COVID-19 pandemic and the reduction in ST-elevation myocardial infarction admissions. Postgrad. Med. J. 2020;96:436–437. doi: 10.1136/postgradmedj-2020-137895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ackah M., Salifu M.G., Ameyaw L., Boakye H., Yeboah C.O. Impact of COVID-19 pandemic on acute stroke admissions and case-fatality rate in lower-income and middle-income countries: A protocol for systematic review and meta-analysis. BMJ Open. 2022;12:e057893. doi: 10.1136/bmjopen-2021-057893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmidt-Lauber C., Günster C., Huber T.B., Spoden M., Grahammer F. Collateral effects and mortality of kidney transplant recipients during the COVID-19 pandemic. Kidney360. 2021;3:325–336. doi: 10.34067/KID.0006472021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cho Y.S., Ro Y.S., Park J.H., Moon S. Effect of social distancing on injury incidence during the COVID-19 pandemic: An interrupted time-series analysis. BMJ Open. 2022;12:e055296. doi: 10.1136/bmjopen-2021-055296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy and ethical restrictions.