Abstract
Therapeutic patient education (TPE) aims to empower the patients and their caregivers to effectively care for and manage their conditions. Such educational programs have been shown to improve health behaviors, disease outcomes, and quality of life among different patient populations. The field of TPE has evolved extensively over decades, owing to interdisciplinary research. No study so far has been done to map this field, to identify the stakeholders and gaps requiring future research. By leveraging the theory of co-citation, CiteSpace was used to visualize the bibliographic data pertaining to TPE research. A total of 54,533 articles published in English language were analyzed to identify influential funders, regions, and institutes contributing to this field. Besides these, significant theoretical and empirical contributions that shaped this field were mapped. Our analysis revealed several important insights. Most of the important theories that helped shape TPE were inspired from the social sciences. Five important research themes were identified: disorders, study designs utilized in TPE research, the scope of the TPE literature and outcomes, and populations. The research focused on improving perceptions, behaviors, and attitudes toward health promotion, reducing stigma, self-management and medication adherence. Most of the research was developed in the context of high-income countries. Future research should involve patients and use digital technology. Meta-analytical studies need to be done to identify the effectiveness and moderators of TPE interventions across different disorders. Further research should involve low and middle-income countries (LMIC) to ensure knowledge and technology transfer.
Keywords: patient education, health literacy, scientometric analysis
1. Introduction
Therapeutic patient education (TPE) helps patients, and their caregivers understand and effectively manage their chronic disorders [1,2]. These programs have been shown to alter health behaviors positively, and thus improve biological, psychological, and quality of life outcomes for many chronic disorders [3,4,5,6]. Several stakeholders and international medical organizations have recommended their use in routine patient care [4,5,7].
The field of patient education and health literacy is interdisciplinary, underpinned by frameworks derived from disciplines such as psychology and education [8,9]. It is essential to identify significant theories and empirical works on TPE, to understand how this field has evolved over the years [10]. This has become possible in recent years due to developments in the field of scientometrics (analyzing scholarly literature) and the availability of electronic bibliographic databases [11]. By utilizing statistical and machine learning approaches, analyses of bibliographic databases can yield insights about the field-specific impact of scientists, collaborative networks, institutes, and significant scholarly works [12,13]. Moreover, such exercises not only help map the scholarly contributions in a discipline but also identify gaps or areas that require more effort [14]. Thus, using these techniques, all stakeholders in the research and development process, including researchers, policymakers, and funding agencies, can determine areas where more infrastructure and human resource personnel and funding is required [13].
As previously noted, the discipline of TPE is a broad one, owing its evolution to interdisciplinary collaborative networks. Therefore, it is important to identify those influential theoretical and empirical works, which underpin this discipline. It is also essential to identify the areas where research in this field is most concentrated and the gaps where more resources are required. To our knowledge, there is a paucity of such literature in patient education. This investigation addresses this paucity, and aims to (i) quantize the research output, (ii) identify significant stakeholders, and (iii) map the influential works that have contributed to this field.
2. Methods
We searched the Web of Science (WoS) core database for literature on health literacy and TPE, using a pretested search strategy, from inception to May 2021 (Table 1). The present mapping study is a broad overview of the domain of TPE. In line with our research aims, we adopted a broader definition of TPE, which spans the dimensions of health promotion, prevention (selective/indicated), and treatment. It is also acknowledged that stakeholders often define TPE in a narrow context of self-management, and ongoing treatment and prevention of complications of chronic disorders [2]. We did not restrict ourselves to a particular discipline to delineate the interdisciplinary nature of the scholarly work published in this area.
Table 1.
Search strategy to identify studies pertaining to patient education research.
| Scope | Details |
|---|---|
| Terms | (“Health education*” OR “patient education*” OR psychoeducation* OR “therapeutic education*” OR “consumer health information*” OR “health knowledge” OR “health literacy”) |
| Scope of search | TS: Topic, Title, Abstract, Author Keywords and Keywords Plus® |
| Period | Through 17 May 2021 |
| Filters | Articles published in English language |
| Total search results | 54,533 |
WoS yielded 54,533 articles published in the English language. Bibliographic characteristics of these articles, along with their citing references, were downloaded. This database was chosen for this investigation [11] because of its multidisciplinary coverage spanning over 20,000 journals and over 79 million reference records. It also allows advanced scientometric analyses due to the availability of cited references for each article [15].
For scientometric analyses, we utilized the CiteSpace software (v 5.7.R5W, Drexel University, Philadelphia, PA, USA), a Java-based platform for visualizing bibliographic data [16]. An excellent feature of this software is conducting co-citation analyses to reveal the collaborative networks in bibliographic data. It is based on the theory of co-citation, which posits that two studies are related when one or more studies cite them together [10,17].
We analyzed the whole dataset (without restriction to the year of publication) to quantify the trends in the research output and significant players in TPE research. However, co-citation analyses were only conducted for bibliographic records from 1990 to 2021. These records were divided into one-year periods using time-slicing methods, with each time slice represented by top 100 articles published in that period. This analytical strategy was employed for identifying top keywords, and elucidating networks of countries, institutions, research categories, and funding organizations.
Furthermore, we sought to identify influential studies in TPE research. By doing this, we envisioned constructing the roadmap presenting the evolution of the field of TPE over time. For this purpose, we divided the bibliographic records into six time periods from 1922 to 2021: pre-1985; 1985 to 1996; 1997 to 2006; 2007 to 2011; 2012 to 2016; 2017 to 2021. We chose the top 50 cited articles per one-year slice within each time-period.
Separate network graphs were created for each time-period, which visualized different studies as nodes and links between them as lines or edges [14]. These influential studies yielded high centrality values (≥0.1) and were visualized as either a purple ring, a red ring, or a citation tree [15]. Purple rings reflect a study with a high betweenness centrality representing a new theory or concept. Red rings represent citation bursts, i.e., hot topics of research attracting high research activity in a short time. The citation tree presents the volume of citations accrued by each study, with each concentric ring corresponding to a year. The parsimony of the network was assessed using the value of modularity (Q). A high value of Q (ranging from −1 to +1) corresponds to more parsimonious networks. The influential studies identified during each period may also include studies from previous periods that may have influenced their collaborative networks [15].
These network analyses were run using the link reduction method with the pathfinder network scaling method. The strengths between links were estimated within slices using the Cosine index. Cluster analyses were then utilized to identify clusters of research in each time-period, where each cluster was named by processing titles of articles by employing two algorithms: log-likelihood ratio (LLR) and TF*IDF [15]. The LLR method chooses the most appropriate terms to name a cluster of research by quantifying the relationship between a term and the cluster. The TF*IDF method delineates names of clusters that are weighted by term frequencies (TF) multiplied by inverted document frequencies (IDF) [14,15,16]. The parsimony of each cluster was assessed by the number of articles in each cluster and the corresponding silhouette value. This value measures homogeneity and cohesion among nodes (studies) within a cluster and heterogeneity across different clusters [15,16,17].
3. Results and Discussion
Publication Trends and Stakeholders on TPE
Overall, publication trends in TPE research revealed an increasing exponential trend (Figure 1). So far, 54,533 research articles have been indexed in WoS. The earliest research study on TPE indexed in the WoS was published in the year 1922, with publications increasing exponentially after the year 1990. The research output increased from 112 in 1990 to 6004 in 2020.
Figure 1.
Trends of publications in patient education research.
Various disciplines published TPE research on public, environmental, and occupational health, yielding both the highest number of citations (n = 12,671) and centrality (0.22). In terms of citations, it was followed by health services research, general and internal medicine; nursing, psychology, psychiatry, education, and health policy, and oncology. In terms of innovation, however, research published in the disciplines of pharmacology and pharmacy, (bio)engineering, and economics yielded the highest centrality values (>0.10) (Supplementary Figure S1).
There were 159 nodes and 1217 edges in the network graph of countries. Authors from high-income countries contributed to 97.82% of research studies published on TPE, followed by upper-middle-income countries (15.44%), low-middle-income (8.41%), and low-income countries (2.31%) (Figure 2). The USA was the single largest contributor to TPE research, accounting for 44.05% of all published research studies. It was followed by England (8.01%), Australia (7.75%), Canada (5.85%), and the People’s Republic of China (4.65%) (Table 2). Despite being upper- and lower-middle-income countries, Brazil and India were among the top-ten contributors of research in this domain. Four of the countries not only contributed to innovations in TPE research, but were also highly collaborative, as visualized by the purple rings in Supplementary Figures S2 and S3 and high centrality values (≥0.10).
Figure 2.
Regional contributors of patient education research (includes multi-authored studies).
Table 2.
Top-five stakeholders in patient education research.
| Institutes | Countries | Journals |
|---|---|---|
| University of California System (n = 2215) | USA (n = 24,021) | Patient Education and Counseling (n = 1109) |
| Harvard University (n = 1363) | England (n = 4367) | BMC Public Health (n = 666) |
| University of London (n = 1256) | Australia (n = 4226) | PloS One (n = 619) |
| University of North Carolina (n = 1086) | Canada (n = 3188) | Journal of School Health (n = 586) |
| University of Texas System (n = 1084) | Peoples Republic of China (n = 2537) | International Journal of Environmental Research & Public Health (n = 525) |
The top 25 funding agencies (Supplementary Table S2) were in high-income countries, except for China’s National Natural Science Foundation (NSF). National Institutes of Health in USA accounted for the highest proportion of funding at 23.75% of funded research projects. Only two countries from Asia contributed to the funding of TPE research, including NSF China (0.68%), the Ministry of Education Culture Sports Science and Technology Japan MEXT (0.53%), and the Japan Society for Promotion of Science (0.45%). The European Commission ranked fourth overall (2.12%).
4. Keywords
Top keywords were analyzed to yield two important insights; (a) central and most cited keywords to identify essential themes of research and (b) burst words to identify hotspots of research in different time-periods. First, a critical appraisal of central and keywords accruing > 300 citations was conducted to analyze themes of research that have most frequently been researched in TPE. There were 413 nodes and 2455 edges in this network graph. It revealed five important research themes including different chronic disorders, study designs, scope, outcomes, and populations (Supplementary Figure S4). Table 3 presents important chronic disorders exhibiting substantial research activity (citation bursts) during specific time-periods.
Table 3.
Keyword bursts for disorders explored in patient education research.
| Keywords | Strength | Begin | End | 1990–2021 |
|---|---|---|---|---|
| Alcohol | 34.6 | 1991 | 2006 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Arthritis | 30.51 | 1991 | 2002 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Asthma | 103.39 | 1991 | 2013 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂ |
| Blood pressure | 53.05 | 1991 | 2008 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Cardiovascular disease | 20.76 | 2005 | 2008 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Childhood asthma | 5.82 | 1992 | 1998 | ▂▂ ▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Cholesterol | 18.22 | 1991 | 1997 | ▂ ▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Cigarette smoking | 23.95 | 1992 | 1998 | ▂▂ ▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Coronary heart disease | 20.72 | 2005 | 2007 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Dental caries | 8.37 | 1990 | 2002 | ▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Diabetes | 31.4 | 2015 | 2017 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃ ▂▂▂▂ |
| Diabetes mellitus | 28.53 | 1995 | 2007 | ▂▂▂▂▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Diarrhea | 6.59 | 1991 | 1996 | ▂ ▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Heart disease | 9.17 | 1992 | 1997 | ▂▂ ▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| HIV infection | 20.02 | 1992 | 2000 | ▂▂ ▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Hospitalization | 4.76 | 1991 | 1993 | ▂ ▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Human immunodeficiency virus | 12.01 | 1991 | 1995 | ▂ ▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Hypertension | 12.17 | 2011 | 2013 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃ ▂▂▂▂▂▂▂▂ |
| Immunization | 4.65 | 1992 | 1996 | ▂▂ ▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Infection | 7.86 | 2010 | 2011 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃ ▂▂▂▂▂▂▂▂▂▂ |
| Low birth weight | 4.07 | 1992 | 1994 | ▂▂ ▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Malignant melanoma | 7.16 | 1995 | 1999 | ▂▂▂▂▂ ▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Mammography | 12.54 | 1991 | 2004 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Mental health | 44.63 | 2019 | 2021 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃ |
| Mortality | 4.72 | 1994 | 1995 | ▂▂▂▂ ▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Myocardial infarction | 12.93 | 1992 | 1998 | ▂▂ ▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Oral health | 39.24 | 2014 | 2018 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃▃▃ ▂▂▂ |
| Pain | 18.58 | 2013 | 2014 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃ ▂▂▂▂▂▂▂ |
| Relapse | 66.57 | 1991 | 2006 | ▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Rheumatoid arthritis | 48.38 | 1992 | 2003 | ▂▂ ▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Schizophrenia | 4.21 | 1996 | 1998 | ▂▂▂▂▂▂ ▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Schizophrenic patient | 16.54 | 1992 | 1999 | ▂▂ ▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Sexual behavior | 4.55 | 1991 | 1997 | ▂ ▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Sexually transmitted disease | 8.53 | 1991 | 2001 | ▂ ▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Smoking | 15.08 | 2009 | 2010 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃ ▂▂▂▂▂▂▂▂▂▂▂ |
| Smoking cessation | 45.33 | 1994 | 2006 | ▂▂▂▂ ▃▃▃▃▃▃▃▃▃▃▃▃▃ ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| Stress | 62.87 | 2019 | 2021 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ ▃▃▃ |
The blue bar presents the time-period from the year 1990 to 2021, while the overlapping red color exhibits the period with citation burst activity.
TPE research was focused on improving perceptions, behaviors, and attitudes for health promotion, self-management, and medication adherence, and reducing stigma. In addition, knowledge- and awareness-related outcomes, quality of life, and decision making for patients were frequently cited outcomes. From 2020 to 2021 specifically, keywords showed social media, health communication, and coronavirus as the top-cited keywords, indicating a shift in research to these important topics (Supplementary Table S3). Significant study design related keyword exhibiting a burst of research activity was controlled trial (1991 to 2009), while the top-five chronic conditions exhibiting the most robust research activity were asthma (the year 1991 to 2013), diabetes mellitus (1991 to 2004), hypertension (1991 to 2008), rheumatoid arthritis (1992 to 2003), and smoking cessation (1991 to 2006).
4.1. Clusters and Influential Publications in TPE Research
To examine clusters of research in TPE, the research literature was divided into two timeframes: pre-1985 and post-1985. Due to the extent of literature, the bibliographic dataset of literature published after 1986 was divided into seven, five-yearly time slices. This strategy allowed us to get a dynamic snapshot of changing research themes over time. This also allowed us to identify important pieces of work published during each time slice, thus, identifying the evolution and complexity of TPE research over time (Table 4 and Supplementary Table S4).
Table 4.
Theories in patient education research yielding the highest centrality values (≥0.1).
| Author, Year | Theory | Comment |
|---|---|---|
| Lazarus and Folkman (1984) [18] | Stress, Appraisal and Coping | A detailed theory of psychological stress, building on the concepts of cognitive appraisal and coping |
| Bandura A (1986) [19] | Social Foundations of Thought and Action: A Social Cognitive Theory | An influential piece of work in psychology that presented a comprehensive theory of human motivation and action. It explores the role of cognition, self-regulation, and self-reflective processes in improving psychosocial functioning |
| Ajzen (1991) [8] | Ajzen’s theory of planned behavior | Behavioral intentions and actions result due to interplay of three components: attitudes, subjective norms, and perceived behavioral control |
| Marlatt GA (1985) [20] | CB model of the relapse process | It challenged the then notions of viewing relapse as “treatment failure” |
| Woodcock (1990) [21] and McGrew (1991) [22] | Measures of Cognitive Ability | Laid down the theoretical foundations of -R measures of cognitive ability |
| David Baker (2006) [23] | Meaning and the measure of health literacy | Defining health literacy. |
4.2. Analysis of the Literature Published before 1985
Before the year 1985, 1942 research studies accounting for 3.57% of the total research output in TPE were published. The earliest study indexed in WoS was published in the year 1922. In the resulting network, there were 320 nodes and 881 edges, with a density of 0.0173.
Five research clusters with a silhouette value > 0.9 were identified (Figure 3). The largest research cluster comprised of 47 studies focused on program planning (ID # 0, LLR), and included studies on program planning, cost-benefit, and impact evaluation of health education programs. The first cluster comprised 38 studies and was termed behavioral pediatrics, which included research on school health education programs. The second cluster consumer health education included studies focused on TPE in chronic disorders, aging and hypertension in the elderly. Cluster # 3 HMO environment predominantly comprised of health education and health promotion among individuals living in houses with multiple occupancies. The last cluster ID # 5 comprised 15 studies, termed the organized patient education program.
Figure 3.
Top clusters of research in patient education research before 1985.
Only one study during this period yielded a high centrality score of 0.21. In this study, Farquhar et al. tested the effectiveness of a novel community education intervention to improve cardiovascular health [24]. This novel intervention was a combination of an extensive mass-media campaign plus face-to-face instruction comprised of information and behavioral skills to affect attitude and motivation [25]. It also attracted a significant research burst for 4.28 years. During this period, the works of Green LW attracted significant research activity, albeit without yielding a high centrality score [26]. Notable works focused on frameworks for studying the impact and cost-effectiveness evaluations of TPE programs.
4.3. Analysis of the Literature Published from 1985 to 1996
From 1985 to 1996, a total of 3026 studies were published. There were 608 nodes and 1362 edges in the network, yielding an adequate modularity (0.87) and mean silhouette value (0.96). Several innovative and central works were published during this period, indicating rapid scholarly progress in TPE research (Supplementary Figure S5). These influential research studies were diverse and employed rigorous study designs. All the influential works were published from high-income western nations.
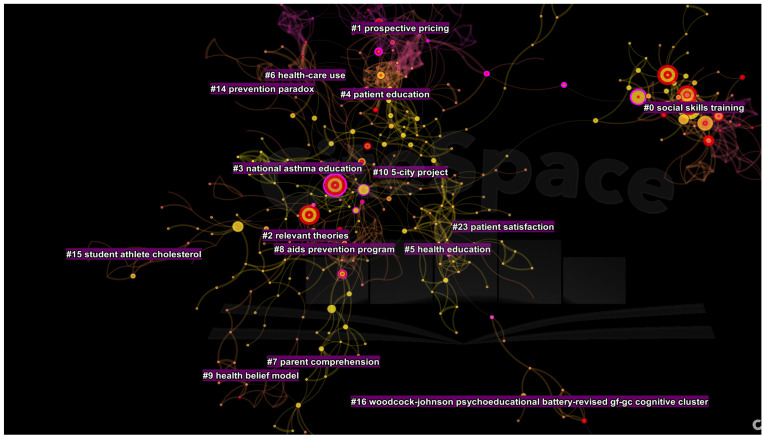
There were sixteen parsimonious clusters of research (Figure 4), represented by at least ten studies published during this period. The cluster (#0) comprised of 69 studies with a mean silhouette value of 0.99. It was termed as social skills training (LLR) and schizophrenia (LSI). It was followed by clusters entitled development, reliability, and prospective pricing (#1); relevant theories (cluster #2), national asthma education (#3), therapeutic potential and rheumatoid arthritis (#4), diabetes, brief-office based intervention and dietary management (#5), asthma and school setting (#6); polio vaccine information and mammography usage (#7), AIDS prevention program (#8), health belief model (#9), and five city project and Stanford (#10). The following two clusters were entitled adolescents (#11) and learning disabilities (#12).
Figure 4.
Top clusters of research in patient education from 1985 to 1996.
Several important works in psychology that underpinned the philosophical and conceptual foundations of TPE were published during this period. Lazarus and Folkman (1984) presented an integrative theoretical analysis entitled Stress, Appraisal and Coping, as a detailed theory of psychological stress which built on the concepts of cognitive appraisal and coping. These have since become major themes of theory and investigation [18]. Bandura A (1986) published their seminal work Social Foundations of Thought and Action: A Social Cognitive Theory, an influential piece of work in psychology, which presented a comprehensive theory of human motivation and action [19]. It analyzed the role of cognition, self-regulation, and self-reflective processes in improving psychosocial functioning. Another critical insight during this period was the concept of self-efficacy and its application in bringing about a sustained behavior change. This was elaborated by Strecher et al. (1986), who examined its utility in several domains, including cigarette smoking, obesity, contraception, alcohol use, and physical activity. Extending upon the cognitive behavioral model [27], Marlatt GA (1985) presented their breakthrough CB model of the relapse process. This work was seminal because it challenged the notions of viewing relapse as a “treatment failure” [20]. The field of TPE was also developed further based on Ajzen’s theory of planned behavior, which emphasized that behavioral intentions and actions result from the interplay of three components: attitudes, subjective norms, and perceived behavioral control [8]. Using path analysis techniques, Rippetoe and Rogers (1987) described the utility of protection-motivation theory on adaptive and maladaptive coping skills to manage health threats [28].
A significant body of work focused on developing psychological constructs and testing measures for utilization in TPE research. The Diagnostic and Statistical Manual (3rd edition) proved to be a major work in guiding psychoeducation programs for people with chronic mental illnesses [29]. Woodcock (1990) and McGrew (1991) laid down the theoretical foundations of -R Measures of Cognitive Ability and Anastasi A (1986) published an easy to understand book on psychological testing [21,22,30].
A body of work focused on understanding processes to improve patient participation in clinical care. However, most of these research studies focused on either cardiovascular diseases or post-surgical recovery. For instance, Davis et al. (1990) emphasized the importance of designing patient reading material with better readability [31], and Greenfield et al. (1988) tested the utility of algorithmic prompts to encourage patients to negotiate medical decisions [32]. Morisky et al. (1983) yielded the highest centrality (0.28) during this period, demonstrating the high effectiveness of the TPE program in improving pressure control and mortality among hypertensive patients belonging to poor urban households [33]. Devine et al. (1986) presented a meta-analysis of 102 studies to demonstrate the clinical effectiveness and cost-saving benefits of psychoeducational interventions among surgical patients to improve recovery, pain, satisfaction, and psychological well-being [34]. In 1983, Devine and Cook used meta-analytical methods to demonstrate lower post-surgical hospital stays among surgical patients [35]. Mullen et al. (1985) presented another meta-analysis comparing the effectiveness of educational programs for people with long-term health problems, focusing on moderators of treatment [36]. Faraquhar (1990) led the Stanford five-city project and demonstrated the effectiveness of low-cost, community-wide TPE programs in improving outcomes in stroke and coronary heart disease [25].
Only one study on a psychiatric disease yielded significance during this period. In 1986, Hogarty et al., published a landmark study combining a patient-centered behavioral treatment and a psychoeducational family intervention to reduce relapse rates in patients with schizophrenia [37].
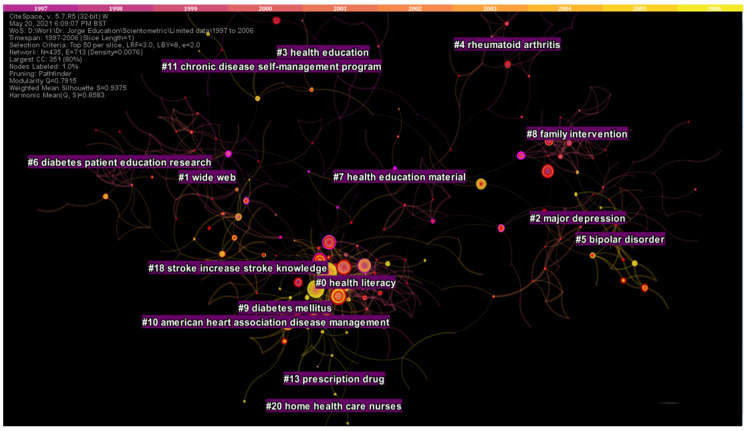
4.4. Analysis of the Literature Published from 1997 to 2006
From 1997 to 2006, a total of 7370 records were analyzed. The resulting network graph comprised of 435 nodes and 713 edges: with a modularity of 0.79 and silhouette value of 0.94 (Supplementary Figure S6). Eleven research clusters comprising at least ten studies and adequate silhouette values were identified. The largest health cluster (#0) focused on functional health literacy, comprising of 63 studies. Cluster #1 comprising of 50 studies focused on digital interventions. The rest of the clusters were entitled major depression (#2), health education and health promotion (#3), rheumatoid arthritis and educational-behavioral joint protection program (#4), bipolar disorder (#5), diabetes TPE research (#6 and #9), health education material and physical activity (#7), family intervention and schizophrenic patient (#8), and the American Heart Association Disease Management (#10) (Figure 5).
Figure 5.
Top clusters of research from 1997 to 2006.
Most of the influential articles on TPE reported findings from controlled trials and impact assessments of TPE interventions in Western countries. However, Campbell and colleagues (2000), building on a more extensive report of the Medical Research Council, published a debate to attract the research community to go beyond RCT and focus on the design, evaluation, and implementation of complex TPE interventions [38]. In addition, three works of note focused on measuring patients’ literacy skills and designing health communication strategies for patients with low literacy levels [39,40,41,42].
Two critical pieces of legislation and policy documents provided an impetus to TPE research during this period and beyond. The guide to clinical and preventive services published by the US Preventive Services Task Force (1996), endorsed counseling interventions for prevention and clinical services including counselling for substance misuse, diet, and exercise, injury prevention, sexual behavior, and dental health [43]. While in the UK, an expenditure and funding report published by Health and Personal Social Services Programmes placed much emphasis on TPE and counseling services [44].
In mental health, the most influential work comprised two reviews of research evidence on social skills training, family interventions, cognitive rehabilitation, and coping with residual positive symptoms among patients with schizophrenia [45,46]. In addition, four studies explored multidisciplinary interventions to prevent the readmission of elderly patients with congestive heart failure [47]; quality of life in asthma and chronic obstructive pulmonary disease [48]; and type 2 diabetes mellitus [49]. This period also saw two central works utilizing a digital platform to reduce hospital admission through computer supported education for patients with asthma and to improve dietary behavior in primary care [50,51].
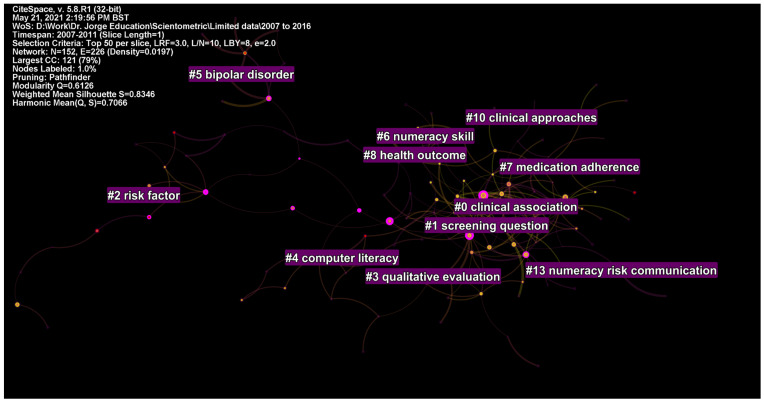
4.5. Analysis of the Literature Published from 2007 to 2011
From 2007 to 2011, a total of 7517 records were published during this period. As a result, there were 152 nodes and 226 edges in the network graph, with a mean modularity of 0.61 and silhouette value of 0.81 (Supplementary Figure S7).
Two studies focused on theoretical developments in the field of TPE. The narrative during this period shifted to health literacy, emphasizing the need to understand this complex construct. In this context, David Baker’s (2006) perspective on the meaning and the measure of health literacy yielded much significance in this field [23]. An influential review during this period by DeWalt and colleagues (2004) showed that the patients with low literacy scored poorer on several psychosocial and biological health outcomes [52].
These theoretical works aided in several empirical investigations. For example, Davis et al. (2006) demonstrated a poorer understanding of dosage labels to be a major factor for non-adherence [53]. Lower use of preventive services was also evident in people with low literacy levels [54]. Other hazards of low literacy levels were also demonstrated in people with diabetes and cancer patients [55], where a poorer understanding of cancer screening and cancer symptoms adversely affects the stage of cancer at diagnosis. The most central intervention-focused reviews and trials during this period researched bipolar disorder [56], type 2 diabetes [57], and chronic conditions [58].
Computer-assisted interventions and health informatics began to emerge as a central field of study during this period. Three significant studies were published during this period. Berland et al. (2001) demonstrated that most of the information provided on the internet might be accurate but lacks good coverage and readability [59]. Deborah et al. (2003) reported computer-delivered TPE to be effective [60]. There were barriers to its access, but generally, no socioeconomic disparities in its usage were evident. Ziebland et al. (2004) conducted a qualitative study among patients with cancer and explored their internet usage in context of their illnesses [61].
There were five clusters with ≥10 studies and adequate silhouette values. Cluster #0 comprised 22 studies and was labelled as clinical association and health literacy. Cluster #1 was labelled as screening question and health literacy, cluster #2 as risk factor, self-management, and controlled trial, cluster #3 as qualitative evaluation and controlled trial, cluster #4 as computer literacy, and cluster #5 as bipolar disorder and psychosocial treatment (Figure 6).
Figure 6.
Top clusters of research from 2007 to 2011.
4.6. Analysis of the Literature Published from 2012 to 2016
From 2012 to 2016, a total of 13,746 studies were published. There were 150 nodes and 195 edges in the network graph, yielding a modularity of 0.63 and silhouette value of 0.85 (Supplementary Figure S8). Research during this period diversified in terms of populations (Figure 7). In contrast to previous periods, an emphasis on racial disparities, non-Caucasians, and ethnic minorities was evident. The largest cluster (#0) comprising 20 studies pertained to health literacy decline and health disparities. The second cluster (#1) focused on readability assessment of internet-based education material. The third cluster (#2) was on oral health and mental health literacy. It was followed by health literacy questionnaire (#3), health literacy (#4), medication adherence (#5), ethnic group (#6), cohort study (#7), and health outcome (#8) (Figure 7).
Figure 7.
Top clusters of research published from 2012 to 2016.
By examining the most central works on TPE during this period, three major themes of research studies emerged. The first body of central works focused on the evolving concept of health literacy, its definitions, and its measurement methods. Don Nutbeam (2008) emphasized the evolving concept of health literacy by dividing it into two disciplines: (i) a measure of clinical risk emphasized in public health and (ii) as an asset emphasized in education research into adult learning and health promotion [62]. The Newest Vital Sign emerged as a widely used short tool for the measurement of health literacy [63,64]. Further conceptual work on health literacy was conducted by Sørensen et al. (2012), who put forward an influential integrative model for health literacy to aid in the development of health-promotion interventions [65]. Finally, Jordan et al. (2010) summarized the evidence for health literacy scales and reported inconsistencies in concepts and measurements underpinning these scales [66].
This period also recognized patient activation as a measure for health-related outcomes and as a component of TPE interventions [9]. TPE intervention for diverse populations gained momentum including child-related outcomes [67], and geriatric populations [68,69]. The seminal work by Osborn et al. (2011) emphasized that health literacy explains racial disparities in health outcomes [70].
4.7. Analysis of the Literature Published from 2017 to 2021
From 2017 to 2021, a total of 21,185 articles were published. The resulting network had 194 nodes and 288 edges. The modularity of the network was 0.66 and silhouette value 0.89 (Supplementary Figure S9). Nine parsimonious clusters with >10 studies and adequate silhouette values were identified during this period. Cluster (#0) was entitled pragmatic randomized controlled trial, followed by e-health literacy scale (#1), COVID-19 pandemic (#2), health literacy questionnaire (#3), study design and latent trait (#4), mixed methods study (#5), health literacy and decision aid (#6), mental health literacy (#7), and diabetes mellitus (#8) (Figure 8).
Figure 8.
Top clusters published from 2017 to 2021.
A total of 19 studies yielded a centrality value > 0.10 during this period. Three policy documents in this period attracted research on TPE. The diabetes atlas (IDF, 2017) published by the International Diabetes Federation and the WHO’s Global Report on Diabetes (2016) yielded much significance among TPE researchers, and introduced several initiatives and calls for TPE programs targeting people with diabetes mellitus [71,72]. Among the research community, a focus was observed on measuring health literacy in different regions by conducting extensive surveys. Sorensen et al. (2015) published the European Health Literacy Survey to report literacy levels in eight European countries [73]. They reported a social gradient in health literacy levels with poorer literacy observed among people with financial deprivation, low social status, low education, and old age. These findings were also corroborated by Rikard et al. (2016), who reported health literacy disparities in the US [74], Levin-Zamir et al. (2016) in Israel [75], and Duong et al. in Taiwan [76]. During this period, Duong et al. (2015) also validated the European health literacy questionnaire (HLS-EU-Q47) in six Asian countries [77].
This period also saw the publication of several influential articles on health literacy assessment tools. An influential review by Altin et al., reported that there was a lack of clear consensus on health literacy measurements [78]. In a similar context, a review of 51 instruments for measuring health literacy [79] highlighted that these tools represent only a narrow set of conceptual dimensions, limited modes of administration, and lack information on their reliability and validity. Meta-analytical studies published during this period investigated the negative association between health literacy and the ability to evaluate online health information (Divani et al., 2015); self-management skills in chronic disease management [80]; medication adherence [81,82]; and the role of decision aids in choosing health treatments or making screening decisions [83].
Only one study on mental health gained adequate centrality during this period. However, in contrast to previous interventions, it was focused on mental health first aid to empower the public to approach, support, and refer individuals in distress [84].
The year 2020 to 2021 was unique because the research focus shifted to the COVID-19 pandemic. There was a mushroom growth in publications during this period. After the WHO declared the COVID-19 as a pandemic, a lot of researchers strived to work for solutions. Three articles of interest were published during this period. Nguyen et al. (2020) reported that people with suspected COVID-19 symptoms reported a higher likelihood of depression and quality of life. However, this effect was moderated by health literacy levels [85]. Wang et al. (2020) reported the psychological impact of COVID-19 in 194 cities in China. A high proportion of Chinese people reported moderate to severe psychological impact from the COVID-19 pandemic and one-third reported moderate to severe symptoms of anxiety [86]. Finally, Brooks et al. (2020) published a rapid review on the psychological impact of quarantine and recommended that officials should quarantine individuals for no longer than required, provide clear rationale for quarantine and information about protocols, and ensure sufficient supplies are provided [87].
5. Discussion
The present scientometric analysis is part of a larger project the research team is leading to evaluate the state of research in patient education and its effectiveness in managing chronic disorders. We found that much significant research works in TPE and outcomes tested, lacked the involvement of patients. Patient and lay public involvement in health research is a vast field at present. Just as they are important stakeholders in clinical decision-making, their involvement in the design of TPE interventions should be ensured. This can lead to more feasible, acceptable, sustainable, and transparent interventions [88].
More recently, much focus has been put on the use of digital technology in the provision of healthcare [89]. The adoption of digital technology is a massive breakthrough in population health because it can ensure equitable health access to specialized resources [90,91]. Although digital health has been tested in several facets of healthcare, including access to specialized clinical help [89], more research is needed in providing TPE. Currently a lot of research is going on in the provision of TPE using web platforms, which needs to be streamlined by government stakeholders to prevent content that may cause harm. The recent COVID-19 infodemic of hoaxes and conspiracy theories is an excellent example in this context [92].
Although the publication trends in TPE seem satisfactory, a considerable research deficit was seen in low- to middle-income countries (LMIC). This may be partly explained by a lack of clinical resources, including healthcare personnel (HCP) and medications [93,94]. The shortage of HCPs is far below the recommended numbers by the WHO, leading to short consultation times, and therefore, patients with chronic disorders usually get poorer (if any) TPE [95,96]. The world, therefore, is far from achieving equitable health access as declared in the Alma Ata declaration four decades ago [97]. To counter this inequity in resources, multidisciplinary research is required in these countries to develop culture-sensitive theories and intervention programs and innovations for equitable delivery. Researchers based in high-income countries should collaborate with those in LMICs to ensure knowledge and technology transfer. The knowledge transfer activities could range from training and education of scholars, assistance in the development of interventions, and cross-cultural adaptations of important theories for conceptual advances.
The advances in research in TPE should be centralized on a single platform, gathering researchers and stakeholders from around the globe. Priority setting should be done for the gaps identified to yield maximum benefits. This centralized platform could be housed as a collaboration between different international societies on TPE. An important example to emulate could be the James Lind Alliance for priority setting in clinical trials, which involves patients and physicians setting priorities for research in different disorders. By using Delphi study methods, a stakeholder consensus could be achieved in TPE research. Another critical task for this consensus committee should be the standardization of definitions and terminologies across the TPE field. This would allow the harmonization of literature and concepts across different study disciplines.
Meta-analytical studies need to be done to identify the effectiveness of TPE interventions across different disorders and define their moderators. For instance, it is important to identify in which conditions, modalities of delivery and for whom these TPE interventions work the best. This is indeed possible by using meta-analytical methods. In addition, research is required on large-scale implementation aspects of TPE interventions. Many clinical trials and meta-analyses have been conducted to prove the effectiveness of these interventions across a variety of biological and psychosocial outcomes. However, the real-life implementation of any intervention and its feasibility and uptake are determined by various forces, which could be identified with implementation-driven studies.
6. Conclusions
The present scientometric analyses reveal several essential insights into TPE research. First, research in TPE is very diverse, with research topics ranging from the development of theories and interventions, development and testing of tools to measure outcomes and tailoring and testing of TPE interventions. Second, TPE is a highly interdisciplinary area, with various interventions underpinned by theories from intelligence research, education, and psychology and public health. Third, restricted research interests on specific chronic disorders were evident in this scientometric analysis. A satisfactory trend in research activity was observed over the years; however, most of this activity was focused on high-income countries. Low- to middle-income countries only account for a small proportion of this research activity.
There are several strengths of this study. Firstly, using reproducible and robust scientometric techniques, it provides a thorough overview of the influential stakeholders in TPE research. In addition, a summary of landmark scholarly works which have contributed to the progress of this field has been provided for the readers. Another strength of this study is the use of an elaborate search strategy using bibliographic data from the Web of Science database, which allowed us to visualize the interdisciplinary nature of the field of TPE. This is important to identify the theories and empirical works cited in TPE that have been borrowed from other disciplines and thus, act as “bridging nodes” between different disciplines.
An important limitation of this study is the restriction to peer-reviewed publications published in the English language. Analysis was restricted to the English language to avoid computational errors in the scientometric analyses. However, this may have resulted in some degree of information bias where landmark studies published in languages other than English may have been omitted. Besides, restricting our analyses to peer-reviewed publications may have led to omissions of landmark non-peer-reviewed working papers commissioned by stakeholders such as the World Health Organization. Therefore, we encourage researchers to consider these limitations in designing future investigations.
Acknowledgments
This scientometric review is part of a larger project PARTNERSHIP (putting the patient first: management of chronic diseases by therapeutic patient education), leading a series of evidence synthesis studies on the role of therapeutic patient education in the management of chronic disorders.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19106128/s1, Figure S1: Disciplines of research central in patient education research. Figure S2: Collaborative network of countries in patient education research. Figure S3: Top institutions contributing to patient education research. Figure S4: Keywords corresponding to central topics in patient education research. Figure S5: Top research articles published from 1985 to 1996. Figure S6: Top articles in patient education research from 1997 to 2006. Figure S7: Top articles published from 2007 to 2011. Figure S8: Top articles published from 2012 to 2016. Figure S9: Top articles published from 2017 to 2021. Table S1: Top cited keywords in patient education research (>300 citations). Table S2: Top funders contributing to the field of patient education. Table S3: Top keywords presented as citation bursts. Table S4: References yielding high centrality values in patient education research from 1922 to 2020.
Author Contributions
J.C.C. developed the conception of the study, contributed to the interpretation of the data, revised and finalized the manuscript; A.W. contributed to the statistical analysis and interpretation of the data and drafted the manuscript; I.A., M.J.D., J.-P.A. and A.G. contributed to drafting and revising the article; Z.P. contributed to the study design, supervised the data interpretation, and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All of the data supporting the findings of this review are included in this published article and Supplementary Materials Files.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Falvo D. Effective Patient Education: A Guide to Increased Compliance. Jones & Bartlett Learning; Burlington, MA, USA: 2004. [Google Scholar]
- 2.World Health Organization . Therapeutic Patient Education: Continuing Education Programmes for Health Care Providers in the Field of Prevention of Chronic Diseases: Report of a WHO Working Group. WHO Regional Office for Europe; Geneva, Switzerland: [Google Scholar]
- 3.Ellis S.E., Speroff T., Dittus R.S., Brown A., Pichert J.W., Elasy T.A. Diabetes patient education: A meta-analysis and meta-regression. Patient Educ. Couns. 2004;52:97–105. doi: 10.1016/S0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 4.Anderson L., Brown J.P., Clark A.M., Dalal H., Rossau HK K., Bridges C., Taylor R. Patient education in the management of coronary heart disease. Cochrane Database Syst. Rev. 2017;6:CD008895. doi: 10.1002/14651858.CD008895.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zangi H.A., Ndosi M., Adams J., Andersen L., Bode C., Boström C., Van Eijk-Hustings Y., Gossec L., Korandová J., Mendes G., et al. EULAR recommendations for patient education for people with inflammatory arthritis. Ann. Rheum. Dis. 2015;74:954–962. doi: 10.1136/annrheumdis-2014-206807. [DOI] [PubMed] [Google Scholar]
- 6.West-Pollak A., Then E.P., Podesta C., Hedelt A., Perry M.L., Izarnotegui W.V., Perez M., Villegas A., Baez N.I., Bassa R., et al. Impact of a novel community-based lifestyle intervention program on type 2 diabetes and cardiovascular risk in a resource-poor setting in the Dominican Republic. Int. Health. 2014;6:118–124. doi: 10.1093/inthealth/iht039. [DOI] [PubMed] [Google Scholar]
- 7.Barbarot S., Bernier C., Deleuran M., De Raeve L., Eichenfield L., El Hachem M., Gelmetti C., Gieler U., Lio P., Marcoux D., et al. Therapeutic patient education in children with atopic dermatitis: Position paper on objectives and recommendations. Pediatr. Dermatol. 2013;30:199–206. doi: 10.1111/pde.12045. [DOI] [PubMed] [Google Scholar]
- 8.Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50:179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 9.Greene J.A., Hibbard J. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012;27:520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen C. The centrality of pivotal points in the evolution of scientific networks; Proceedings of the 10th International Conference on Intelligent User Interfaces—IUI 05; San Diego, CA, USA. 9–12 January 2005. [Google Scholar]
- 11.Clarivate Analytics. Web of Science Platform [Internet] [(accessed on 8 May 2022)]. Available online: https://clarivate.libguides.com/webofscienceplatform/alldb.
- 12.Naveed S., Waqas A., Majeed S., Zeshan M., Jahan N., Sheikh M.H. Child psychiatry: A scientometric analysis 1980–2016. F1000Research. 2017;6:1293. doi: 10.12688/f1000research.12069.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hess D. Science Studies: An Advanced Introduction. New York University Press; New York, NY, USA: 1997. [Google Scholar]
- 14.Synnestvedt M.B., Chen C., Holmes J.H. AMIA Annual Symposium Proceedings. Volume 2005. American Medical Informatics Association; Bethesda, MD, USA: 2005. CiteSpace II: Visualization and knowledge discovery in bibliographic databases; p. 724. [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C. The CiteSpace Manual v1.05. Drexel University College of Computing & Informatics; Philadelphia, PA, USA: 2015. [Google Scholar]
- 16.Chen C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. 2006;57:359–377. doi: 10.1002/asi.20317. [DOI] [Google Scholar]
- 17.Small H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. 1973;24:265–269. doi: 10.1002/asi.4630240406. [DOI] [Google Scholar]
- 18.Lazarus R., Folkman S. Stress, Appraisal and Coping. Springer; New York, NY, USA: 1984. [Google Scholar]
- 19.Bandura A. Social Foundations of Thought and Action. Prentice-Hall, Inc.; Englewood Cliffs, NJ, USA: 1986. pp. 23–28. [Google Scholar]
- 20.Marlatt G.A. Relapse prevention: Theoretical rationale and overview of the model. In: Marlatt G.A., Gordon J.R., editors. Relapse Prevention. 1st ed. Guilford Press; New York, NY, USA: 1985. pp. 250–280. [Google Scholar]
- 21.Woodcock R.W. Theoretical Foundations of the Wj-R Measures of Cognitive Ability. J. Psychoeduc. Assess. 1990;8:231–258. doi: 10.1177/073428299000800303. [DOI] [Google Scholar]
- 22.McGrew K.S., Werder J.K., Woodcock R.W. WJ-R Technical Manual. Riverside Publishing; Itasca, IL, USA: 1991. [Google Scholar]
- 23.Baker D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farquhar J., Wood P., Breitrose H., Haskell W., Meyer A., Maccoby N., Alexander J., Brown B., Mcalister A., Nash J., et al. Community education for cardiovascular health. Lancet. 1977;309:1192–1195. doi: 10.1016/S0140-6736(77)92727-1. [DOI] [PubMed] [Google Scholar]
- 25.Farquhar J.W. Effects of Communitywide Education on Cardiovascular Disease Risk Factors. JAMA. 1990;264:359. doi: 10.1001/jama.1990.03450030083037. [DOI] [PubMed] [Google Scholar]
- 26.Green L.W., Figá-Talamanca I. Suggested Designs for Evaluation of Patient Education Programs. Health Educ. Monogr. 1974;2:54–71. doi: 10.1177/109019817400200109. [DOI] [Google Scholar]
- 27.Strecher V.J., McEvoy DeVellis B., Becker M.H., Rosenstock I.M. The Role of Self-Efficacy in Achieving Health Behavior Change. Health Educ. Q. 1986;13:73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 28.Rippetoe P.A., Rogers R.W. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J. Pers. Soc. Psychol. 1987;52:596–604. doi: 10.1037/0022-3514.52.3.596. [DOI] [PubMed] [Google Scholar]
- 29.Frances A., Pincus H.A., First M.B. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association; Washington, DC, USA: 1994. [Google Scholar]
- 30.Anastasi A. Psychological Testing. 6th ed. Macmillan Publishing Co., Inc.; New York, NY, USA: 1988. [Google Scholar]
- 31.Davis T.C., Crouch M.A., Wills G., Miller S., Abdehou D.M. The gap between patient reading comprehension and the readability of patient education materials. J. Fam. Pract. 1990;31:533–538. [PubMed] [Google Scholar]
- 32.Greenfield S., Kaplan S.H., Ware J.E., Yano E.M., Frank H.J.L. Patients’ participation in medical care. J. Gen. Intern. Med. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 33.Morisky D.E., Levine D.M., Green L.W., Shapiro S., Russell R.P., Smith C.R. Five-year blood pressure control and mortality following health education for hypertensive patients. Am. J. Public Health. 1983;73:153–162. doi: 10.2105/AJPH.73.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Devine E.C., Cook T.D. Clinical and cost-saving effects of psychoeducational interventions with surgical patients: A meta-analysis. Res. Nurs. Health. 1986;9:89–105. doi: 10.1002/nur.4770090204. [DOI] [PubMed] [Google Scholar]
- 35.Devine E.C., Cook T.D. A Meta-Analytic Analysis of Effects of Psychoeducational Interventions on Length of Postsurgical Hospital Stay. Nurs. Res. 1983;32:267–274. doi: 10.1097/00006199-198309000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Mullen P.D., Green L.W., Persinger G.S. Clinical trials of patient education for chronic conditions: A comparative meta-analysis of intervention types. Prev. Med. 1985;14:753–781. doi: 10.1016/0091-7435(85)90070-2. [DOI] [PubMed] [Google Scholar]
- 37.Hogarty G.E. Family Psychoeducation, Social Skills Training, and Maintenance Chemotherapy in the Aftercare Treatment of Schizophrenia. Arch. Gen. Psychiatry. 1986;43:633. doi: 10.1001/archpsyc.1986.01800070019003. [DOI] [PubMed] [Google Scholar]
- 38.Campbell M., Fitzpatrick R., Haines A., Kinmonth A.L., Sandercock P., Spiegelhalter D., Tyrer P. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker R.M., Baker D.W., Williams M.V., Nurss J.R. The test of functional health literacy in adults. J. Gen. Intern. Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 40.Doak C.C., Doak L.G., Root J.H. Teaching Patients with Low Literacy Skills. Am. J. Nurs. 1996;96:16M. doi: 10.1097/00000446-199612000-00022. [DOI] [Google Scholar]
- 41.Hjern A. Chapter 7: Children’s and young people’s health. Scand. J. Public Health. 2006;34:165–183. doi: 10.1080/14034950600677238. [DOI] [PubMed] [Google Scholar]
- 42.Baker D.W., Parker R.M., Williams M.V., Clark W.S. Health literacy and the risk of hospital admission. J. Gen. Intern. Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.US Preventive Services Task Force, United States. Office of Disease Prevention, Health Promotion . Guide to Clinical Preventive Services: Report of the US Preventive Services Task Force. US Department of Health and Human Services, Office of Public Health and Science, Office of Disease Prevention and Health Promotion; Washington, DC, USA: 1996. [Google Scholar]
- 44.Department of Health . The Government’s Expenditure Plans 2001–2002 to 2003–2004 and Main Estimates 2001–2002. The Stationary Office; London, UK: 2001. The Health and Personal Social Services Programmes. [Google Scholar]
- 45.Penn D.L., Mueser K.T., Spaulding W. Information processing, social skill, and gender in schizophrenia. Psychiatry Res. 1996;59:213–220. doi: 10.1016/0165-1781(95)02768-8. [DOI] [PubMed] [Google Scholar]
- 46.Dixon L., Adams C., Lucksted A. Update on Family Psychoeducation for Schizophrenia. Schizophr. Bull. 2000;26:5–20. doi: 10.1093/oxfordjournals.schbul.a033446. [DOI] [PubMed] [Google Scholar]
- 47.Rich M.W., Beckham V., Wittenberg C., Leven C.L., Freedland K.E., Carney R.M. A Multidisciplinary Intervention to Prevent the Readmission of Elderly Patients with Congestive Heart Failure. N. Engl. J. Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 48.Gallefoss F., Bakke P.S., Rsgaard P.Å.L.K. Quality of Life Assessment after Patient Education in a Randomized Controlled Study on Asthma and Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 1999;159:812–817. doi: 10.1164/ajrccm.159.3.9804047. [DOI] [PubMed] [Google Scholar]
- 49.Litzelman D.K. Reduction of Lower Extremity Clinical Abnormalities in Patients with Non-Insulin-Dependent Diabetes Mellitus. Ann. Intern. Med. 1993;119:36. doi: 10.7326/0003-4819-119-1-199307010-00006. [DOI] [PubMed] [Google Scholar]
- 50.Osman L.M., Abdalla M.I., Beattie J.A., Ross S.J., Russell I.T., Friend J.A., Legge J.S., Douglas J.G., Grampian Asthma Study of Integrated Care (GRASSIC) Reducing hospital admission through computer supported education for asthma patients. BMJ. 1994;308:568–571. doi: 10.1136/bmj.308.6928.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Campbell M.K., DeVellis B.M., Strecher V.J., Ammerman A.S., DeVellis R.F., Sandler R.S. Improving dietary behavior: The effectiveness of tailored messages in primary care settings. Am. J. Public Health. 1994;84:783–787. doi: 10.2105/AJPH.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dewalt D.A., Berkman N.D., Sheridan S., Lohr K.N., Pignone M.P. Literacy and health outcomes: A systematic review of the literature. J. Gen. Intern. Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davis T.C., Wolf M.S., Bass P.F., Thompson J.A., Tilson H.H., Neuberger M., Parker R.M. Literacy and Misunderstanding Prescription Drug Labels. Ann. Intern. Med. 2006;145:887. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- 54.Scott T.L., Gazmararian J.A., Williams M.V., Baker D.W. Health Literacy and Preventive Health Care Use Among Medicare Enrollees in a Managed Care Organization. Med. Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Davis T.C., Williams M.V., Marin E., Parker R.M., Glass J. Health Literacy and Cancer Communication. CA Cancer J. Clin. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 56.Colom F., Vieta E., Martínez-Arán A., Reinares M., Goikolea J.M., Benabarre A., Torrent C., Comes M., Corbella B., Parramon G., et al. A Randomized Trial on the Efficacy of Group Psychoeducation in the Prophylaxis of Recurrences in Bipolar Patients Whose Disease Is in Remission. Arch. Gen. Psychiatry. 2003;60:402. doi: 10.1001/archpsyc.60.4.402. [DOI] [PubMed] [Google Scholar]
- 57.Norris S.L., Lau J., Smith S.J., Schmid C.H., Engelgau M.M. Self-Management Education for Adults With Type 2 Diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 58.Barlow J., Wright C., Sheasby J., Turner A., Hainsworth J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Couns. 2002;48:177–187. doi: 10.1016/S0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 59.Berland G.K., Elliott M.N., Morales L.S., Algazy J.I., Kravitz R.L., Broder M.S., Kanouse D.E., Muñoz J.A., Puyol J.-A., Lara M., et al. Health Information on the Internet. JAMA. 2001;285:2612. doi: 10.1001/jama.285.20.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.LEWIS D. Computers in Patient Education. CIN Comput. Inform. Nurs. 2003;21:88–96. doi: 10.1097/00024665-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 61.Ziebland S., Chapple A., Dumelow C., Evans J., Prinjha S., Rozmovits L. How the internet affects patients’ experience of cancer: A qualitative study. BMJ. 2004;328:564. doi: 10.1136/bmj.328.7439.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nutbeam D. The evolving concept of health literacy. Soc. Sci. Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 63.Osborn C.Y., Weiss B.D., Davis T.C., Skripkauskas S., Rodrigue C., Bass P.F., Wolf M.S. Measuring Adult Literacy in Health Care: Performance of the Newest Vital Sign. Am. J. Health Behav. 2007;31:36–46. doi: 10.5993/AJHB.31.s1.6. [DOI] [PubMed] [Google Scholar]
- 64.Weiss B.D., Mays M.Z., Martz W., Castro K.M., DeWalt D.A., Pignone M.P., Mockbee J., Hale F.A. Quick assessment of literacy in primary care: The newest vital sign. Ann. Fam. Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sørensen K., Van den Broucke S., Fullam J., Doyle G., Pelikan J., Slonska Z., Brand H. European, (HLS-EU) Consortium Health Literacy Project Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jordan J.E., Osborne R.H., Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J. Clin. Epidemiol. 2011;64:366–379. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 67.DeWalt D.A., Hink A. Health Literacy and Child Health Outcomes: A Systematic Review of the Literature. Pediatrics. 2009;124:S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 68.Baker D.W. Health Literacy and Mortality Among Elderly Persons. Arch. Intern. Med. 2007;167:1503. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 69.Bennett I.M., Chen J., Soroui J.S., White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann. Fam. Med. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Osborn C.Y., Cavanaugh K., Wallston K.A., Kripalani S., Elasy T.A., Rothman R.L., White R.O. Health literacy explains racial disparities in diabetes medication adherence. J. Health Commun. 2011;16((Suppl. 3)):268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.International Diabetes Federation . IDF Diabetes Atlas. Brussels: International Diabetes Federation. IDF; Brussels, Belgium: 2013. [Google Scholar]
- 72.World Health Organization . World Health Organization Global Report on Diabetes. World Health Organization; Geneva, Switzerland: 2016. [Google Scholar]
- 73.Sørensen K., Pelikan J.M., Röthlin F., Ganahl K., Slonska Z., Doyle G., Fullam J., Kondilis B., Agrafiotis D., Uiters E., et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU) Eur. J. Public Health. 2015;25:1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rikard R.V., Thompson M.S., McKinney J., Beauchamp A. Examining health literacy disparities in the United States: A third look at the National Assessment of Adult Literacy (NAAL) BMC Public Health. 2016;16:975. doi: 10.1186/s12889-016-3621-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Levin-Zamir D., Baron-Epel O.B., Cohen V., Elhayany A. The Association of Health Literacy with Health Behavior, Socioeconomic Indicators, and Self-Assessed Health From a National Adult Survey in Israel. J. Health Commun. 2016;21:61–68. doi: 10.1080/10810730.2016.1207115. [DOI] [PubMed] [Google Scholar]
- 76.Duong V.T., Lin I.-F., Sorensen K., Pelikan J.M., Van Den Broucke S., Lin Y.-C., Chang P.W. Health Literacy in Taiwan. Asia Pac. J. Public Health. 2015;27:871–880. doi: 10.1177/1010539515607962. [DOI] [PubMed] [Google Scholar]
- 77.Duong T.V., Aringazina A., Kayupova G., Nurjanah, Pham T.V., Pham K.M., Truong T.Q., Nguyen K.T., Oo W.M., Su T.T., et al. Development and Validation of a New Short-Form Health Literacy Instrument (HLS-SF12) for the General Public in Six Asian Countries. HLRP Health Lit. Res. Pract. 2019;3:90–102. doi: 10.3928/24748307-20190225-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Altin S.V., Finke I., Kautz-Freimuth S., Stock S. The evolution of health literacy assessment tools: A systematic review. BMC Public Health. 2014;14:1207. doi: 10.1186/1471-2458-14-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Haun J.N., Valerio M.A., McCormack L.A., Sørensen K., Paasche-Orlow M.K. Health Literacy Measurement: An Inventory and Descriptive Summary of 51 Instruments. J. Health Commun. 2014;19:302–333. doi: 10.1080/10810730.2014.936571. [DOI] [PubMed] [Google Scholar]
- 80.Mackey L.M., Doody C., Werner E.L., Fullen B. Self-Management Skills in Chronic Disease Management. Med. Decis. Mak. 2016;36:741–759. doi: 10.1177/0272989X16638330. [DOI] [PubMed] [Google Scholar]
- 81.Zhang Q., Liang Y.-J., Sun X.-L., You G.-Y., Chen Y.-C., Zeng Z., Li X., Gao X.-L., Jiang J., Chen X.-J. Higher blood pressure control rate in a real life management program provided by the community health service center in China. BMC Public Health. 2014;14:801. doi: 10.1186/1471-2458-14-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Miller T.A. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ. Couns. 2016;99:1079–1086. doi: 10.1016/j.pec.2016.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stacey D., Légaré F., Lewis K., Barry M.J., Bennett C.L., Eden K.B., Holmes-Rovner M., Llewellyn-Thomas H., Lyddiatt A., Thomson R., et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hadlaczky G., Hökby S., Mkrtchian A., Carli V., Wasserman D. Mental Health First Aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: A meta-analysis. Int. Rev. Psychiatry. 2014;26:467–475. doi: 10.3109/09540261.2014.924910. [DOI] [PubMed] [Google Scholar]
- 85.Nguyen H.C., Nguyen M.H., Do B.N., Tran C.Q., Nguyen T.T.P., Pham K.M., Pham L.V., Tran K.V., Duong T.T., Tran T.V., et al. People with Suspected COVID-19 Symptoms Were More Likely Depressed and Had Lower Health-Related Quality of Life: The Potential Benefit of Health Literacy. J. Clin. Med. 2020;9:965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Skovlund P.C., Nielsen B.K., Thaysen H.V., Schmidt H., Finset A., Hansen K.A., Lomborg K. The impact of patient involvement in research: A case study of the planning, conduct and dissemination of a clinical, controlled trial. Res. Involv. Engagem. 2020;6:43. doi: 10.1186/s40900-020-00214-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Waqas A., Teoh S.H., Lapão L.V., Messina L.A., Correia J. Harnessing Telemedicine for the Provision of Health Care: Bibliometric and Scientometric Analysis. J. Med. Internet Res. 2020;22:e18835. doi: 10.2196/18835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Adeloye D., Adigun T., Misra S., Omoregbe N. Assessing the coverage of e-Health services in sub-Saharan Africa: A systematic review and analysis. Methods Inf. Med. 2017;56:189–199. doi: 10.3414/ME16-05-0012. [DOI] [PubMed] [Google Scholar]
- 91.World Health Organization . Atlas of eHealth Country Profiles. The Use of eHealth in Support of Universal Health Coverage. WHO; Geneva, Switzerland: 2016. p. 392. [Google Scholar]
- 92.Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.World Health Organization . Access to Medicines: Making Market Forces Serve the Poor. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 94.Ozawa S., Shankar R., Leopold C., Orubu S. Access to medicines through health systems in low-and middle-income countries. Health Policy Plan. 2019;34:III1–III3. doi: 10.1093/heapol/czz119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Alberti H., Boudriga N., Nabli M. Primary care management of diabetes in a low/middle income country: A multi-method, qualitative study of barriers and facilitators to care. BMC Fam. Pract. 2007;8:63. doi: 10.1186/1471-2296-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shabila N.P., Al-Tawil N.G., Al-Hadithi T.S., Sondorp E., Vaughan K. Iraqi primary care system in Kurdistan region: Providers’ perspectives on problems and opportunities for improvement. BMC Int. Health Hum. Rights. 2012;12:21. doi: 10.1186/1472-698X-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chowdhury S., Chakraborty P. Pratim Universal health coverage—There is more to it than meets the eye. J. Fam. Med. Prim. Care. 2017;6:169–170. doi: 10.4103/jfmpc.jfmpc_13_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All of the data supporting the findings of this review are included in this published article and Supplementary Materials Files.