Abstract
Chronic rhinosinusitis is a chronic inflammatory disease of the upper airways, for which treatment options include medical or surgical therapy. However, there are limitations to conservative treatment strategies, such as the relapse of nasal polyps. In this review, we discuss the rising role of biomolecular mechanisms associated with various biologics that have been approved or are undergoing clinical trials to treat chronic rhinosinusitis. We also highlight the potential molecular therapeutic targets for managing and treating chronic rhinosinusitis.
Keywords: chronic rhinosinusitis, biologics, therapeutic strategy, immunity, monoclonal antibody
1. Introduction
Chronic rhinosinusitis (CRS) can be diagnosed based on the presence of more than two of the following four symptoms for at least 12 weeks: anterior/posterior rhinorrhea, nasal congestion, facial pain or pressure, and olfactory dysfunction. At least one such symptom must be anterior/posterior rhinorrhea or nasal congestion for CRS diagnosis. Depending on the presence or absence of nasal polyps (NPs), CRS can be classified as CRS with NPs (CRSwNP) or CRS without NPs (CRSsNP) [1]. Based on the differences in immune responses between type 1 helper T (Th1)/type 17 helper T (Th17) and type 2 helper T cells (Th2), CRS can also be divided into eosinophilic and non-eosinophilic CRS [2].
CRS affects patients worldwide, with a prevalence rate of 6.95–13% [3,4,5,6]. The burden of medical expenses caused by CRS is exceptionally high. In the United States, the cost of CRS-related diseases is estimated to be between billions and tens of billions of dollars, including outpatient and emergency expenses, drug expenses, nursing expenses, and surgical expenses [7]. Patients with CRS usually receive drug treatment. If the disease persists, the patient can choose to undergo surgery. However, the situation can differ among patients with CRS. Some patients with CRS can be cured by drug treatment only; some patients with CRS require surgery and drug treatment, and others cannot achieve satisfactory curative effects despite trying various treatment schemes [8].
Recently, researchers have made strides to understand different inflammatory mechanisms, which has led to encouraging the development of targeted biological drug therapies. However, owing to the lack of clear treatment guidance and evidence of large-scale use, biologics have not yet become a clinical standard in CRS treatment [9]. Nevertheless, the potential for personalized, targeted therapy for CRS is becoming apparent. Biological therapies are different from traditional therapies. They are aimed at specific immune cells or inflammatory pathways in the disease development and progression. Therefore, they can improve drug efficacy and reduce the incidence of complications [10]. Several biotherapeutics have been developed and approved for patients with CRS. For example, dupilumab is an anti-interleukin (IL)4Rα antagonist that prevents IL-4 and IL-13 from binding to their receptors and blocks the downstream signal transduction of the Th2 inflammatory pathway, and can be used to treat refractory CRSwNP [11].
Based on the increasingly urgent need for new treatment strategies for patients with CRS, remarkable progress has been made in investigating and developing biological therapies. This review summarizes the current and in-development therapeutic strategies of biologics for CRS treatment, and it aims to provide doctors in relevant fields with the latest information concerning biologics.
2. Biologics in CRSwNP
Most biological agents for CRSwNP were originally biological agents for asthma because the pathophysiology of CRSwNP is similar to that of asthma [12]. Biological agents approved by the US Food and Drug Administration (FDA) for CRS include dupilumab, omalizumab, and mepolizumab, whereas benralizumab and reslizumab are in clinical trials [13]. Table 1 lists the names and brands of commercial biological agents approved or in clinical trials for the treatment of CRSwNP, the reduced biomarkers in subjects after their treatment, and their common side effects (Table 1).
Table 1.
Biological agents approved or in clinical trials for CRSwNP.
| Target | Drug | Brand | Approval or Development Status for CRS | Decreased Biomarker after Treatment | Side Effects |
|---|---|---|---|---|---|
| IL-4Rα | Dupilumab | Dupixent® | FDA approved for CRSwNP | Blood thymus and activation-regulated chemokine | Injection site reaction and conjunctivitis |
| IgE | Omalizumab | Xolair® | FDA approved for CRSwNP | Blood Periostin | Injection site reactions |
| IL-5 | Mepolizumab | Nucala® | FDA approved for CRSwNP | Blood Eosinophil | Headache and injection site reaction |
| IL-5 | Reslizumab | CINQAIR® | Phase 2 trials concluded | Blood Eosinophil | Nasopharyngitis |
| IL-5Rα | Benralizumab | Fasenra® | Phase 3 trials concluded | Blood Eosinophil | Nasopharyngitis |
2.1. Dupilumab
IL-4 and IL-13 are key cytokines involved in the pathogenesis of CRSwNP [14]. IL-4 promotes the differentiation of Th0 cells into Th2 cells and is involved in mast cell activation [15]. IL-13 contributes to eosinophil migration, mucinous gland hyperplasia, and mucus hypersecretion [16]. Because of these effects, these two cytokines play a crucial role in tissue remodeling and NP formation in CRS [17]. Dupilumab (Dupixent®) is a humanized monoclonal antibody that targets the IL-4 receptor α-subunit, which is shared by IL-4 and IL-13 receptors. It effectively regulates Th2 inflammation by inhibiting IL-4 and IL-13 signal transduction. The dual inhibition of IL-4 and IL-13 signaling may be an essential strategy for treating CRSwNP [18]. The FDA approved dupilumab for moderate-to-severe atopic dermatitis (AD) and moderate-to-severe asthma in 2017 and 2018, respectively. After Bachert et al. [19] published the results of two phase 3 clinical studies, dupilumab was approved for CRSwNP in 2019. Their results showed that, compared with placebo, dupilumab significantly reduced the levels of blood thymus and activation of regulatory chemokines and other cytokines related to Th2 inflammation. Another randomized controlled trial of 724 patients revealed that dupilumab improved the quality of life of patients with CRSwNP complicated by asthma [20]. The experimental group with a subcutaneous injection of 300 mg dupilumab every 2 weeks had better nasal congestion scores, Lund Mackay computed tomography scores, and 22-item sinonasal outcome test scores than the control group with placebo. The scores for 6-item asthma control were also significantly improved. As the first biotherapeutic drug approved by the FDA for CRSwNP, it can be used for patients with routine treatment failure, but it causes a certain economic burden for patients with CRSwNP because of its high price. As a biological agent approved for clinical use in recent years, the side effects of dupilumab have attracted attention. An observational study indicated that dupilumab is also related to herpes simplex virus reactivation and conjunctivitis, and common drug injection site reactions [21].
2.2. Omalizumab
Immunoglobulin E (IgE) is an effective inflammatory mediator that activates mast cells and aggravates inflammatory signal transduction [22]. When the human body is exposed to allergens, IgE is produced in large quantities. However, the specific role of IgE in the pathophysiology of CRSwNP remains unclear. Elevated IgE levels were measured in patients with CRSwNP with AD and eosinophilia [23]. Omalizumab is a monoclonal anti-IgE antibody that can prevent IgE from interacting with receptors on the cell surface and prevent the activation of basophils and mast cells by binding to Fc receptors on various inflammatory cells [24]. It is sold under the brand name Xolair® and was originally approved by the FDA to treat chronic idiopathic urticaria and allergic asthma [25,26]. The pathophysiological mechanism related to the production of local intranasal IgE leads to an inflammatory cascade and perhaps to the occurrence of CRSwNP [27]. The results of two randomized phase 3 clinical trials showed that omalizumab significantly improved the indicators and symptoms of patients with severe CRSwNP with insufficient intranasal corticosteroid response and was officially approved by the FDA in 2020 for the treatment of adult refractory CRSwNP [28]. Bidder et al. evaluated the efficacy of omalizumab in patients with CRSwNP complicated with asthma in a 16-week study and found that the nasal symptoms of the experimental group were improved compared with those of the control group [29]. A retrospective study showed that serum IgE levels and tissue eosinophils did not decrease in patients with CRSwNP after omalizumab [30]. Similarly, another study showed that treatment with omalizumab did not reduce total IgE levels in patients with CRSwNP and asthma [31]. Only one study has reported that omalizumab reduced serum periostin levels in patients with CRSwNP [32]. The primary adverse reaction to omalizumab is injection site reactions [33]. Other adverse reactions, including anaphylaxis and headaches, are like those associated with other biological agents [34]. The economic burden of omalizumab was the same as that of dupilumab. Patients need approximately USD 10,000 to 30,000 for omalizumab treatment every year, which is difficult for most patients to bear [35].
2.3. Mepolizumab
IL-5, produced by group 2 innate lymphoid cells (ILC2s) or mast cells, plays an important role in Th2 CRSwNP. It mainly involves eosinophilia and plasma cell activation in NPS [36]. Mepolizumab (Nucala®) is an anti-IL-5 monoclonal antibody. Several studies have reported the effects of drugs on CRSwNP. It inhibits eosinophilic inflammation by interfering with the binding of IL-5 to receptors expressed on eosinophils and basophils [37]. In 2015, the FDA first approved mepolizumab as an additional maintenance treatment for patients with severe asthma [38]. In 2021, the FDA approved mepolizumab for the treatment of CRSwNP. It was the first anti-IL-5 biological agent approved by the FDA for adult patients with CRSwNP. A 2011 study evaluated the efficacy of mepolizumab in 30 patients with severe CRSwNP, all of whom showed poor drug control. The patients were treated twice with 1500 mg of mepolizumab for 8 weeks. Compared to the control group treated with placebo, the nasal polyp size of patients in the mepolizumab treatment group was significantly reduced, and the score was significantly improved, showing a good curative effect [39]. Another phase 2 clinical trial in 2017 evaluated whether 105 patients with CRSwNP requiring surgery could avoid surgery after receiving mepolizumab. All patients received 750 mg mepolizumab every 4 weeks for 25 weeks. Although the symptoms of sinusitis and the size of NPs in the drug treatment group were reduced compared to those in the control group, 70% of patients still needed surgical treatment [40]. A phase 3 clinical study of mepolizumab was conducted between May 2017 and December 2018. A total of 407 patients with CRSwNP [41] were included. Compared with the control group, treatment with mepolizumab reduced the size of NPs and nasal congestion symptoms, showing the possibility of its use in patients with refractory severe chronic sinusitis with NPs. Common adverse reactions of mepolizumab include headache and injection site reactions, and there are no reported cases of allergic reactions. Although several studies have reported death cases, there is no strong evidence of a causal relationship with the use of mepolizumab [42]. The efficacy of mepolizumab is good and is associated with fewer side effects. However, its cost-effectiveness exceeded the value threshold. To reach these thresholds, a price discount of more than 60% from the current list price is required. Thus, relevant personnel must negotiate with drug manufacturers; otherwise, it is difficult to apply to most patients [43].
2.4. Reslizumab
Reslizumab is also a humanized anti-IL-5 antibody that can prevent IL-5 from binding to IL-5 receptors and reduce eosinophil differentiation, similar to mepolizumab [44]. Reslizumab (CINQAIR®) was approved in the United States as an additional maintenance treatment for severe asthma with an eosinophilic phenotype in 2016. However, it has not been approved for the treatment of CRSwNP [45]. Gevaert et al. evaluated the safety, efficacy, and biological activity of reslizumab using parameters such as NP size, sinusitis symptoms, and local IL-5 levels. Their results showed that a 3 mg/kg dose of reslizumab was completely safe in a single injection. A single reslizumab injection improved the nasal polyp score in half of the patients with CRSwNP, and the number of eosinophils in the serum and nasal secretions decreased significantly within 8 weeks after treatment. Although there has been no trial of reslizumab for nasal polyposis, a phase III trial of reslizumab for CRS is currently in the recruitment stage [46].
2.5. Benralizumab
Benralizumab is a monoclonal antibody that binds to the IL-5 receptor on the surface of eosinophils to activate the anti-IL-5 receptor α-subunit. It binds to the IL-5 receptor, resulting in signal transduction degradation and strong apoptosis of eosinophils [47]. Benralizumab (Fasenra®) was approved by the FDA to treat severe asthma in 2017 and has been approved in the European Union, Canada, Australia, and several other countries [48]. The results of a phase III-B clinical trial involving 153 patients with CRSwNP by Canonica et al. showed that benralizumab significantly improved nasal symptoms, and other clinical symptoms related to CRSwNP improved to varying degrees without changing over time [18]. A randomized controlled trial evaluating benralizumab in the treatment of CRSwNP involving more than 300 people is currently underway [49], and a phase III clinical trial of benralizumab in the treatment of severe nasal polyposis is currently recruiting subjects. These results indicate that benralizumab for CRSwNP is expected to obtain FDA approval over the next few years. This will make benralizumab a new CRS biological agent after dupilumab, omalizumab, and mepolizumab; reslizumab will compete for this position.
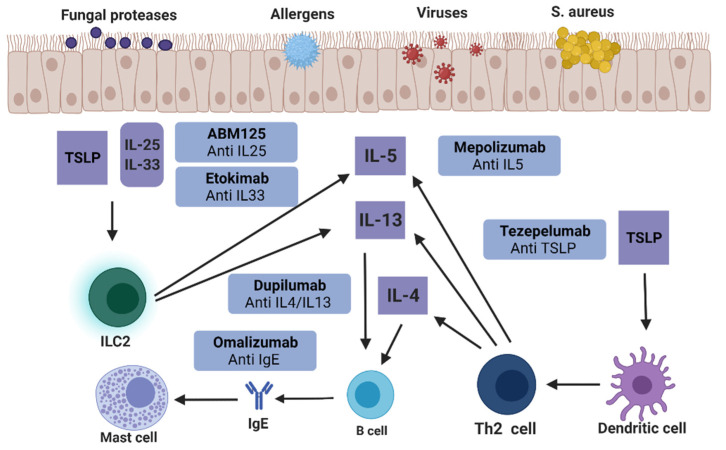
2.6. Anti-IL-25/33 and Anti-TSLP
Thymic stromal lymphopoietin (TSLP), IL-25, and IL-33 are key regulators of the immune pathogenesis of CRS [50]. The activation of epithelial cells stimulated by allergens and pathogens releases TSLP, IL-25, and IL-33, resulting in the activation of Th2, ILC2, and dendritic cells (DCs). The overproduction of inflammatory factors, such as IL-4, IL-5, and IL-13, from these cells leads to an increase in tissue eosinophils and the production of local IgE (Figure 1). In addition to the above biological agents targeting IL-4, IL-5, IL-13, and IgE, biological agents targeting IL-25, IL-33, and TSLP have also been studied. Shin et al. reduced the number of polyps, mucosal edema thickness, and inflammatory cell infiltration through anti-IL-25 treatment and inhibited the expression of local inflammatory cytokines, such as IL-4 and interferon (IFN)-γ, indicating the possibility of treating NPs with anti-IL-25 therapy [51]. IL-33 plays a role in the pathogenesis of allergic diseases and functions as a neutrophil activator. The monoclonal antibody etokimab targeting IL-33 will be evaluated in the upcoming phase 2 trials for adult controlled trials with CRSwNP [52]. Tezepelumab is a monoclonal antibody targeting TSLP. In a phase 2 clinical trial, after 52 weeks of treatment, the efficacy of subcutaneous injection of tezepelumab was compared with that of the control group. Tezepelumab can significantly reduce the incidence of asthma in patients and has considerable potential as a therapeutic agent for CRSwNP [53].
Figure 1.
Biologics for treating CRSwNP.
As shown above, biological agents have shown potential for the treatment of CRSwNP. Currently, three biological agents have been approved by the FDA for refractory CRSwNP, and an increasing number of biological agents are undergoing clinical trials. Although several influential clinical trials have proven preliminary efficacy and safety, when the treatment time is prolonged, the new treatment has a high risk of unknown long-term side effects.
2.7. Uncontrolled CRSwNP
At the European Forum for Research and Education in Allergy and Airway Diseases (EUFOREA) held in Belgium in 2020 [54], the committee of experts defined uncontrolled CRSwNP as “persistent or recurrent despite long-term intranasal steroid treatment and at least one course of systemic corticosteroid treatment and/or nasal surgery in the past two years”. Current research has not shown that biological agents can replace surgical therapies. Therefore, biological agents should be used as another treatment for uncontrolled CRSwNP or as an option for patients who cannot undergo surgical treatment rather than completely replacing the traditional treatment. The EUFOREA expert group proposed five criteria: evidence of type 2 inflammation, the need for systemic corticosteroids in the past two years, significant impairment of quality of life, significant loss of smell, and the diagnosis of asthma. Their research concluded that biological agents like dupilumab, omalizumab, and benralizumab are suitable for patients with bilateral nasal polyps who have previously undergone sinus surgery and meet the above three criteria. However, if patients have never received surgical treatment, they need to meet at least the above four criteria before they can consider receiving biological treatment [55]. The approach based on biomarker-defined clusters would identify responders to biologics [27], for example, in a study of the anti-IL-5 biological agent reslizumab, it was found that in the patients with bilateral nasal polyps, only elevated IL-5 levels (>40 pg/mL) in nasal secretions before treatment benefited from anti-IL-5 treatment [56]. Different biologics should be selected according to the molecular markers of each patient, including anti-IL-4 receptor α (dupilumab), anti-IgE (omalizumab), and anti-IL-5/RA (mepolizumab and benralizumab).
3. Biologics in CRSsNP
Although many studies on the efficacy of biological agents have been conducted in CRSwNP, the exploration of the efficacy of biological agents in CRSsNP is still in the theoretical stage, lacking attention and research. CRSsNP differs pathophysiologically from asthma, which is a type 2 inflammatory disease; instead, CRSsNP is a type 1 inflammatory disease [57]. Therefore, CRSsNPs are generally not considered the focus of type 2 targeted biological agents. However, increasing evidence indicates that it may be wrong to roughly classify CRSwNP and CRSsNP into type 2 and non-type 2 inflammatory diseases. In the United States and Europe, the most common inflammatory endotype of CRSwNP is type 2 CRSwNP. However, in Asia, patients with CRSwNP in some regions mainly show a mixed pattern of type 2 and non-type 2, whereas patients with CRSwNP in other regions show lower Th2 expression levels [58,59]. At present, no biotherapy for non-type 2 mediated CRS inflammation is under study; however, the above research results suggest that if biological agents for non-type 2 CRS can be developed, it may be a meaningful achievement for many patients with CRS in Asia.
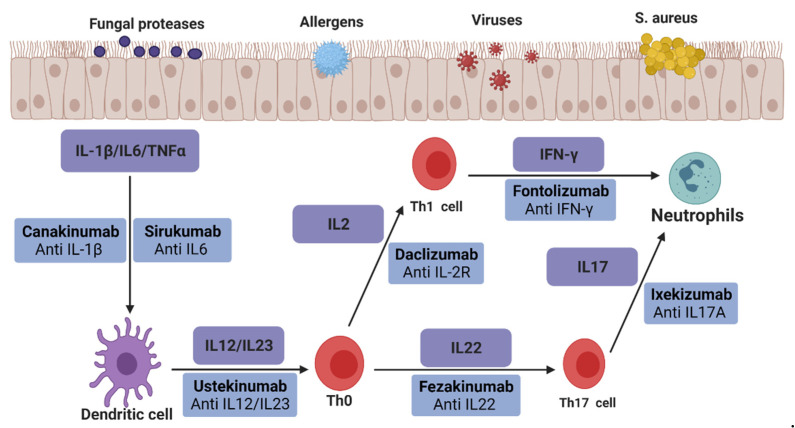
Figure 2 shows various biological therapies for non-type 2 inflammatory diseases, which may be applied to CRSsNP in the future. The biological agent ustekinumab, anti-IL-12/23, has shown good efficacy in joint pain and psoriatic arthritis in clinical studies involving more than 150 patients. It showed high sensitivity to pyoderma gangrenosum and erythema nodosum in seven studies, including 65 patients [60]. In a controlled study involving 230 patients with multiple sclerosis, the lesion site in the daclizumab group targeting IL-2R was more than 70% less than that in the placebo group. The incidence of side effects in the two groups was the same, such as skin rash and infection [61]. A randomized study evaluated the safety and efficacy of fontolizumab, an antibody targeting IFN-γ, in 135 patients with Crohn’s disease. The results showed that the C-reactive protein level in the treatment group decreased significantly and was well tolerated without severe side effects [62]. Canakinumab is a biological agent targeting IL-1 β. In a clinical study evaluating whether canakinumab can be used to treat autoimmune recurrent fever syndrome, the results showed that canakinumab could effectively control and prevent attacks in patients with various autoimmune diseases, with an effective rate of more than 70% [63]. A phase III clinical study reported the efficacy of sirukumab targeting IL-6 in treating rheumatoid arthritis. This 2-year study involving more than 1000 patients showed that sirukumab treatment reduced the clinical signs and symptoms of patients with rheumatoid arthritis and minimized the progress of radiographic damage [64]. Ixekizumab, an antagonist of IL-17A, can disrupt the inflammatory cascade in psoriasis [65]. The phase III clinical trial results showed that nearly 90% of patients treated with ixekizumab for 12 weeks showed efficacy, and the area severity index of psoriasis decreased by 75% [66]. The efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in patients with moderate-to-severe AD were evaluated in a phase 2 clinical trial [67]. After 10 weeks of treatment, the AD score of patients treated with fezakinumab was lower than that of patients treated with the placebo. None of the above drugs have been clinically evaluated in patients with CRS, but these studies may lead to studies related to non-type 2 CRS.
Figure 2.
Possible biologics for treating CRSsNP.
4. Future Targets of Biologics in CRS
Just as the application of biological agents in CRSwNP is inspired by the use of biological agents in asthma [68], research on biological agents for Th1 and Th17 inflammatory pathway-mediated CRS will also be inspired by the evaluation or approval for the treatment of inflammatory diseases with overlapping pathophysiology with CRS, such as psoriatic arthritis, Crohn’s disease, and AD. The main inflammatory pathways related to CRS include the Th1, Th2, and Th17 mediated inflammatory pathways [69], and different targets in these pathways will become the focus of research on new biological agents targeting CRS in the future.
IFN-γ inducible protein 10 (CXCL10) is produced by IFN-γ chemokines induced and secreted by monocytes, neutrophils, fibroblasts, DCs, and other cells [70]. CXCL10 expression level is elevated in different diseases such as rheumatoid arthritis and psoriatic arthritis [71,72]. CXCL10 is a receptor-binding ligand of the chemokine receptor CXCR3, and the CXCL10–CXCR3 axis is a pathway for IFN-γ induction. Therefore, CXCL10 and CXCR3 may play essential roles in leukocyte homing to inflammatory tissues and the persistence of inflammation [73]. In the IFN γ-induced vitiligo mouse model, mice with identified depigmentation treated with CXCL10 neutralizing antibody for 8 weeks showed reversal of the disease through pigmentation [74]. Elevated IFN-γ level is one of the disease manifestations of CRS [75], and the increase of CXCL10 in CRS can be predicted, which is also supported by the research results. The researchers’ results indicated that the expression levels of CXCL10 mRNA and protein in nasal fibroblasts of patients with type 2 CRS were significantly enhanced compared to that in normal nasal mucosal cells [76]. Although there are no clinical trials related to anti-CXCL10 biologics in patients with CRS, CXCL10 has the potential to become a target of biological agents for CRS treatment in the future.
The tumor necrosis factor receptor OX40 (CD134) is activated by its cognate ligand OX40L (CD134L, CD252) and co-stimulates T cells [77]. The OX40L-OX40 axis participates in the continuous activation of effector T cells and can accelerate the differentiation of Th1 and Th2 effector cells [78]. Therefore, the inhibition of OX40 may have therapeutic significance in T cell-mediated diseases. A phase 2 clinical study investigated the safety and efficacy of antagonistic antibodies against OX40 in patients with AD. Their study found that after 71 days of injection, the treatment group achieved more than 50% improvement in eczema severity than the placebo group and showed good tolerance, highlighting the potential of OX40 targeted treatment of AD patients [79]. A study using an allergic rhinitis (AR) mouse model also confirmed the potential of OX40 as a therapeutic target for AR. After blocking the OX40/OX40L signal pathway through small interfering RNA (siRNA) interference, researchers found that it can inhibit the allergic reaction in AR mice and effectively alleviate allergic symptoms, such as nose scratching, sneezing, and runny nose [80]. As for CRSwNP, experimental results in the superior nasal cortex of 94 NPs tissues showed that a higher expression level of OX40L was detected in the DCs of NPs nasal mucosa [81], indicating that OX40L may play an important role in the pathogenesis of CRSwNP. If relevant research is conducted in the future, the anti-OX40 biologics may become one of the biologics for the treatment of CRS in the future.
5. Conclusions
Based on an in-depth understanding of the primary drivers of inflammation in CRS, multiple therapeutic targets have been identified to match the appropriate biological agents for CRS treatment. There is considerable clinical evidence supporting the safety and efficacy of biologics in patients with CRS, and the FDA has approved several such drugs for treating CRS. However, the high cost of drugs makes it difficult for people to access such treatment options. In the treatment of patients with uncontrolled CRSwNP, after evaluating the efficacy of surgery and biological agents, clinicians choose sinus surgery, biological methods, or a combination of both, which brings high utility benefits. Using biomarkers to classify and identify different recipients of biologics will also lead to more accurate treatment options. As more studies focus on new therapeutic targets and accurately matched biological agents based on CRS endotypes, the application range of biological agents in various CRS endotypes will be expanded, and the therapeutic effects of biological agents will also be improved. However, it is undeniable that the application of precision medicine and lowering of the associated cost will be essential to ensure that biological agents can become a new treatment option for most patients in the future, in addition to traditional drugs and surgery.
Acknowledgments
Figures are created with BioRender.com (accessed on 10 May 2022).
Abbreviations
| CRS | chronic rhinosinusitis |
| NPs | nasal polyps |
| CRSwNP | CRS with NPs |
| CRSsNP | CRS without NPs |
| Th2 | type 2 T helper |
| Th1 | type 1 T helper |
| Th17 | type 17 T helper |
| IL | interleukin |
| FDA | food and drug administration |
| AD | atopic dermatitis |
| IgE | immunoglobulin E |
| ILC2s | type 2 innate lymphoid cells |
| TSLP | thymic stromal lymphopoietin |
| DCs | dendritic cells |
| IFN | interferon |
| EUFOREA | European Forum for Research and Education in Allergy and Airway Diseases |
| AR | allergic rhinitis |
| siRNA | small interfering RNA |
Author Contributions
Writing—original draft preparation, corrections after review: J.T.; data curation: M.H.; methodology: M.H.; review and editing: T.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the Basic Science Research Program, National Research Foundation of Korea, funded by the Ministry of Science and Technology and the Ministry of Science, ICT & Future Planning (2017R1A2B2003575, NRF-2020R1A2C1006398), the Ministry of Science and ICT (2020R1C1C1012288), Korea, under the ICT Creative Consilience program (IITP-2022-2020-0-01819) supervised by the Institute for Information & Communications Technology Planning & Evaluation (IITP), the Korea Health Technology R&D Project (HI17C0387), Korea Health Industry Development Institute (KHIDI), and the Ministry of Health and Welfare.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fokkens W.J., Lund V.J., Hopkins C., Hellings P.W., Kern R., Reitsma S., Toppila-Salmi S., Bernal-Sprekelsen M., Mullol J., Alobid I., et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020;58:1–464. doi: 10.4193/Rhin20.401. [DOI] [PubMed] [Google Scholar]
- 2.Lee K., Tai J., Lee S.H., Kim T.H. Advances in the Knowledge of the Underlying Airway Remodeling Mechanisms in Chronic Rhinosinusitis Based on the Endotypes: A Review. Int. J. Mol. Sci. 2021;22:910. doi: 10.3390/ijms22020910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim Y.S., Kim N.H., Seong S.Y., Kim K.R., Lee G.B., Kim K.S. Prevalence and risk factors of chronic rhinosinusitis in Korea. Am. J. Rhinol. Allergy. 2011;25:117–121. doi: 10.2500/ajra.2011.25.3630. [DOI] [PubMed] [Google Scholar]
- 4.Shi J.B., Fu Q.L., Zhang H., Cheng L., Wang Y.J., Zhu D.D., Lv W., Liu S.X., Li P.Z., Ou C.Q., et al. Epidemiology of chronic rhinosinusitis: Results from a cross-sectional survey in seven Chinese cities. Allergy. 2015;70:533–539. doi: 10.1111/all.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhattacharyya N., Gilani S. Prevalence of Potential Adult Chronic Rhinosinusitis Symptoms in the United States. Otolaryngol. Head Neck Surg. 2018;159:522–525. doi: 10.1177/0194599818774006. [DOI] [PubMed] [Google Scholar]
- 6.Hastan D., Fokkens W.J., Bachert C., Newson R.B., Bislimovska J., Bockelbrink A., Bousquet P.J., Brozek G., Bruno A., Dahlén S.E., et al. Chronic rhinosinusitis in Europe—An underestimated disease. A GA2LEN study. Allergy. 2011;66:1216–1223. doi: 10.1111/j.1398-9995.2011.02646.x. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharyya N., Villeneuve S., Joish V.N., Amand C., Mannent L., Amin N., Rowe P., Maroni J., Eckert L., Yang T., et al. Cost burden and resource utilization in patients with chronic rhinosinusitis and nasal polyps. Laryngoscope. 2019;129:1969–1975. doi: 10.1002/lary.27852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith K.A., Rudmik L. Medical therapy, refractory chronic rhinosinusitis, and productivity costs. Curr. Opin. Allergy Clin. Immunol. 2017;17:5–11. doi: 10.1097/ACI.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 9.Laidlaw T.M., Buchheit K.M. Biologics in chronic rhinosinusitis with nasal polyposis. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2020;124:326–332. doi: 10.1016/j.anai.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Legrand F., Klion A.D. Biologic therapies targeting eosinophils: Current status and future prospects. J. Allergy Clin. Immunol. Pract. 2015;3:167–174. doi: 10.1016/j.jaip.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel G.B., Peters A.T. The Role of Biologics in Chronic Rhinosinusitis With Nasal Polyps. Ear Nose Throat J. 2021;100:44–47. doi: 10.1177/0145561320964653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bachert C., Gevaert P., Hellings P. Biotherapeutics in Chronic Rhinosinusitis with and without Nasal Polyps. J. Allergy Clin. Immunol.. Pract. 2017;5:1512–1516. doi: 10.1016/j.jaip.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 13.Franzese C.B. The Role of Biologics in the Treatment of Nasal Polyps. Immunol. Allergy Clin. N. Am. 2020;40:295–302. doi: 10.1016/j.iac.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Hoy S.M. Dupilumab: A Review in Chronic Rhinosinusitis with Nasal Polyps. Drugs. 2020;80:711–717. doi: 10.1007/s40265-020-01298-9. [DOI] [PubMed] [Google Scholar]
- 15.Kubo M. T follicular helper and T(H)2 cells in allergic responses. Allergol. Int. Off. J. Jpn. Soc. Allergol. 2017;66:377–381. doi: 10.1016/j.alit.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Siddiqui S., Johansson K., Joo A., Bonser L.R., Koh K.D., Le Tonqueze O., Bolourchi S., Bautista R.A., Zlock L., Roth T.L., et al. Epithelial miR-141 regulates IL-13-induced airway mucus production. JCI Insight. 2021;6 doi: 10.1172/jci.insight.139019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eschenbacher W., Straesser M., Knoeddler A., Li R.-C., Borish L. Biologics for the Treatment of Allergic Rhinitis, Chronic Rhinosinusitis, and Nasal Polyposis. Immunol. Allergy Clin. N. Am. 2020;40:539–547. doi: 10.1016/j.iac.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Corso E., Bellocchi G., De Benedetto M., Lombardo N., Macchi A., Malvezzi L., Motta G., Pagella F., Vicini C., Passali D. Biologics for severe uncontrolled chronic rhinosinusitis with nasal polyps: A change management approach. Consensus of the Joint Committee of Italian Society of Otorhinolaryngology on biologics in rhinology. Acta Otorhinolaryngol. Ital. 2022;42:1–16. doi: 10.14639/0392-100X-N1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bachert C., Han J.K., Desrosiers M., Hellings P.W., Amin N., Lee S.E., Mullol J., Greos L.S., Bosso J.V., Laidlaw T.M., et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet. 2019;394:1638–1650. doi: 10.1016/S0140-6736(19)31881-1. [DOI] [PubMed] [Google Scholar]
- 20.Laidlaw T.M., Bachert C., Amin N., Desrosiers M., Hellings P.W., Mullol J., Maspero J.F., Gevaert P., Zhang M., Mao X., et al. Dupilumab improves upper and lower airway disease control in chronic rhinosinusitis with nasal polyps and asthma. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2021;126:584–592.e1. doi: 10.1016/j.anai.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 21.de Wijs L.E.M., Bosma A.L., Erler N.S., Hollestein L.M., Gerbens L.A.A., Middelkamp-Hup M.A., Kunkeler A.C.M., Nijsten T.E.C., Spuls P.I., Hijnen D.J. Effectiveness of dupilumab treatment in 95 patients with atopic dermatitis: Daily practice data. Br. J. Dermatol. 2020;182:418–426. doi: 10.1111/bjd.18179. [DOI] [PubMed] [Google Scholar]
- 22.Hong C.J., Tsang A.C., Quinn J.G., Bonaparte J.P., Stevens A., Kilty S.J. Anti-IgE monoclonal antibody therapy for the treatment of chronic rhinosinusitis: A systematic review. Syst. Rev. 2015;4:166. doi: 10.1186/s13643-015-0157-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudmik L., Soler Z.M. Medical Therapies for Adult Chronic Sinusitis: A Systematic Review. JAMA. 2015;314:926–939. doi: 10.1001/jama.2015.7544. [DOI] [PubMed] [Google Scholar]
- 24.Wright J.D., Chu H.M., Huang C.H., Ma C., Chang T.W., Lim C. Structural and Physical Basis for Anti-IgE Therapy. Sci. Rep. 2015;5:11581. doi: 10.1038/srep11581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Doroudchi A., Pathria M., Modena B.D. Asthma biologics: Comparing trial designs, patient cohorts and study results. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2020;124:44–56. doi: 10.1016/j.anai.2019.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maurer M., Rosén K., Hsieh H.J., Saini S., Grattan C., Gimenéz-Arnau A., Agarwal S., Doyle R., Canvin J., Kaplan A., et al. Omalizumab for the treatment of chronic idiopathic or spontaneous urticaria. N. Engl. J. Med. 2013;368:924–935. doi: 10.1056/NEJMoa1215372. [DOI] [PubMed] [Google Scholar]
- 27.Tomassen P., Vandeplas G., Van Zele T., Cardell L.O., Arebro J., Olze H., Förster-Ruhrmann U., Kowalski M.L., Olszewska-Ziąber A., Holtappels G., et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016;137:1449–1456.e4. doi: 10.1016/j.jaci.2015.12.1324. [DOI] [PubMed] [Google Scholar]
- 28.Gevaert P., Omachi T.A., Corren J., Mullol J., Han J., Lee S.E., Kaufman D., Ligueros-Saylan M., Howard M., Zhu R., et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 2020;146:595–605. doi: 10.1016/j.jaci.2020.05.032. [DOI] [PubMed] [Google Scholar]
- 29.Bidder T., Sahota J., Rennie C., Lund V.J., Robinson D.S., Kariyawasam H.H. Omalizumab treats chronic rhinosinusitis with nasal polyps and asthma together—A real life study. Rhinology. 2018;56:42–45. doi: 10.4193/Rhin17.139. [DOI] [PubMed] [Google Scholar]
- 30.Armengot-Carceller M., Gómez-Gómez M.J., García-Navalón C., Doménech-Campos E., Muñoz-Fernández N., Miguel A.G., Marco-Algarra J., Palop-Cervera M., Piñero A.G. Effects of Omalizumab Treatment in Patients With Recalcitrant Nasal Polyposis and Mild Asthma: A Multicenter Retrospective Study. Am. J. Rhinol. Allergy. 2021;35:516–524. doi: 10.1177/1945892420972326. [DOI] [PubMed] [Google Scholar]
- 31.Gevaert P., Calus L., Van Zele T., Blomme K., De Ruyck N., Bauters W., Hellings P., Brusselle G., De Bacquer D., van Cauwenberge P., et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 2013;131:110–116.e1. doi: 10.1016/j.jaci.2012.07.047. [DOI] [PubMed] [Google Scholar]
- 32.De Schryver E., Derycke L., Calus L., Holtappels G., Hellings P.W., Van Zele T., Bachert C., Gevaert P. The effect of systemic treatments on periostin expression reflects their interference with the eosinophilic inflammation in chronic rhinosinusitis with nasal polyps. Rhinology. 2017;55:152–160. doi: 10.4193/Rhin16.314. [DOI] [PubMed] [Google Scholar]
- 33.Davydov L. Omalizumab (Xolair) for treatment of asthma. Am. Fam. Physician. 2005;71:341–342. [PubMed] [Google Scholar]
- 34.Bavbek S., Lee M.J. Subcutaneous Injectable Drugs Hypersensitivity and Desensitization: Insulin and Monoclonal Antibodies. Immunol. Allergy Clin. N. Am. 2017;37:761–771. doi: 10.1016/j.iac.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Fanta C.H. Asthma. N. Engl. J. Med. 2009;360:1002–1014. doi: 10.1056/NEJMra0804579. [DOI] [PubMed] [Google Scholar]
- 36.Kato A., Schleimer R.P., Bleier B.S. Mechanisms and pathogenesis of chronic rhinosinusitis. J. Allergy Clin. Immunol. 2022;149:1491–1503. doi: 10.1016/j.jaci.2022.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broughton S.E., Nero T.L., Dhagat U., Kan W.L., Hercus T.R., Tvorogov D., Lopez A.F., Parker M.W. The βc receptor family - Structural insights and their functional implications. Cytokine. 2015;74:247–258. doi: 10.1016/j.cyto.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Ortega H.G., Liu M.C., Pavord I.D., Brusselle G.G., FitzGerald J.M., Chetta A., Humbert M., Katz L.E., Keene O.N., Yancey S.W., et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N. Engl. J. Med. 2014;371:1198–1207. doi: 10.1056/NEJMoa1403290. [DOI] [PubMed] [Google Scholar]
- 39.Gevaert P., Van Bruaene N., Cattaert T., Van Steen K., Van Zele T., Acke F., De Ruyck N., Blomme K., Sousa A.R., Marshall R.P., et al. Mepolizumab, a humanized anti-IL-5 mAb, as a treatment option for severe nasal polyposis. J. Allergy Clin. Immunol. 2011;128:989–995.e1–e8. doi: 10.1016/j.jaci.2011.07.056. [DOI] [PubMed] [Google Scholar]
- 40.Bachert C., Sousa A.R., Lund V.J., Scadding G.K., Gevaert P., Nasser S., Durham S.R., Cornet M.E., Kariyawasam H.H., Gilbert J., et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 2017;140:1024–1031.e14. doi: 10.1016/j.jaci.2017.05.044. [DOI] [PubMed] [Google Scholar]
- 41.Han J.K., Bachert C., Fokkens W., Desrosiers M., Wagenmann M., Lee S.E., Smith S.G., Martin N., Mayer B., Yancey S.W., et al. Mepolizumab for chronic rhinosinusitis with nasal polyps (SYNAPSE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. Respir. Med. 2021;9:1141–1153. doi: 10.1016/S2213-2600(21)00097-7. [DOI] [PubMed] [Google Scholar]
- 42.Jackson K., Bahna S.L. Hypersensitivity and adverse reactions to biologics for asthma and allergic diseases. Expert Rev. Clin. Immunol. 2020;16:311–319. doi: 10.1080/1744666X.2020.1724089. [DOI] [PubMed] [Google Scholar]
- 43.Whittington M.D., McQueen R.B., Ollendorf D.A., Tice J.A., Chapman R.H., Pearson S.D., Campbell J.D. Assessing the value of mepolizumab for severe eosinophilic asthma: A cost-effectiveness analysis. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2017;118:220–225. doi: 10.1016/j.anai.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 44.Matera M.G., Rogliani P., Calzetta L., Cazzola M. Pharmacokinetic/pharmacodynamic profile of reslizumab in asthma. Expert Opin. Drug Metab. Toxicol. 2018;14:239–245. doi: 10.1080/17425255.2018.1421170. [DOI] [PubMed] [Google Scholar]
- 45.Markham A. Reslizumab: First Global Approval. Drugs. 2016;76:907–911. doi: 10.1007/s40265-016-0583-2. [DOI] [PubMed] [Google Scholar]
- 46.Agarwal A., Spath D., Sherris D.A., Kita H., Ponikau J.U. Therapeutic Antibodies for Nasal Polyposis Treatment: Where Are We Headed? Clin. Rev. Allergy Immunol. 2020;59:141–149. doi: 10.1007/s12016-019-08734-z. [DOI] [PubMed] [Google Scholar]
- 47.Ghazi A., Trikha A., Calhoun W.J. Benralizumab—A humanized mAb to IL-5Rα with enhanced antibody-dependent cell-mediated cytotoxicity--a novel approach for the treatment of asthma. Expert Opin. Biol. Ther. 2012;12:113–118. doi: 10.1517/14712598.2012.642359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cushen B., Menzies-Gow A. Benralizumab: An updated treatment of eosinophilic asthma. Expert Rev. Respir. Med. 2020;14:435–444. doi: 10.1080/17476348.2020.1739526. [DOI] [PubMed] [Google Scholar]
- 49.Patel G.B., Kern R.C., Bernstein J.A., Hae-Sim P., Peters A.T. Current and Future Treatments of Rhinitis and Sinusitis. J. Allergy Clin. Immunol. Pract. 2020;8:1522–1531. doi: 10.1016/j.jaip.2020.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hong H., Liao S., Chen F., Yang Q., Wang D.Y. Role of IL-25, IL-33, and TSLP in triggering united airway diseases toward type 2 inflammation. Allergy. 2020;75:2794–2804. doi: 10.1111/all.14526. [DOI] [PubMed] [Google Scholar]
- 51.Shin H.W., Kim D.K., Park M.H., Eun K.M., Lee M., So D., Kong I.G., Mo J.H., Yang M.S., Jin H.R., et al. IL-25 as a novel therapeutic target in nasal polyps of patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 2015;135:1476–1485.e7. doi: 10.1016/j.jaci.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 52.Xu Y., Bi M., Tan K.S., Mi J., Hong H. Biologics in Treatment for Chronic Rhinosinusitis with Comorbid Asthma. Curr. Treat. Options Allergy. 2021;8:133–146. doi: 10.1007/s40521-021-00282-2. [DOI] [Google Scholar]
- 53.Corren J., Parnes J.R., Wang L., Mo M., Roseti S.L., Griffiths J.M., van der Merwe R. Tezepelumab in Adults with Uncontrolled Asthma. N. Engl. J. Med. 2017;377:936–946. doi: 10.1056/NEJMoa1704064. [DOI] [PubMed] [Google Scholar]
- 54.Bachert C., Han J.K., Wagenmann M., Hosemann W., Lee S.E., Backer V., Mullol J., Gevaert P., Klimek L., Prokopakis E., et al. EUFOREA expert board meeting on uncontrolled severe chronic rhinosinusitis with nasal polyps (CRSwNP) and biologics: Definitions and management. J. Allergy Clin. Immunol. 2021;147:29–36. doi: 10.1016/j.jaci.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 55.Fokkens W.J., Lund V., Bachert C., Mullol J., Bjermer L., Bousquet J., Canonica G.W., Deneyer L., Desrosiers M., Diamant Z., et al. EUFOREA consensus on biologics for CRSwNP with or without asthma. Allergy. 2019;74:2312–2319. doi: 10.1111/all.13875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gevaert P., Lang-Loidolt D., Lackner A., Stammberger H., Staudinger H., Van Zele T., Holtappels G., Tavernier J., van Cauwenberge P., Bachert C. Nasal IL-5 levels determine the response to anti–IL-5 treatment in patients with nasal polyps. J. Allergy Clin. Immunol. 2006;118:1133–1141. doi: 10.1016/j.jaci.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 57.Meltzer E.O., Hamilos D.L., Hadley J.A., Lanza D.C., Marple B.F., Nicklas R.A., Bachert C., Baraniuk J., Baroody F.M., Benninger M.S., et al. Rhinosinusitis: Establishing definitions for clinical research and patient care. J. Allergy Clin. Immunol. 2004;114:155–212. doi: 10.1016/j.jaci.2004.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang X., Zhang N., Bo M., Holtappels G., Zheng M., Lou H., Wang H., Zhang L., Bachert C. Diversity of T(H) cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J. Allergy Clin. Immunol. 2016;138:1344–1353. doi: 10.1016/j.jaci.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 59.Stevens W.W., Peters A.T., Tan B.K., Klingler A.I., Poposki J.A., Hulse K.E., Grammer L.C., Welch K.C., Smith S.S., Conley D.B., et al. Associations Between Inflammatory Endotypes and Clinical Presentations in Chronic Rhinosinusitis. J. Allergy Clin. Immunol.. Pract. 2019;7:2812–2820.e3. doi: 10.1016/j.jaip.2019.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guillo L., D’Amico F., Danese S., Peyrin-Biroulet L. Ustekinumab for Extra-intestinal Manifestations of Inflammatory Bowel Disease: A Systematic Literature Review. J. Crohn’s Colitis. 2021;15:1236–1243. doi: 10.1093/ecco-jcc/jjaa260. [DOI] [PubMed] [Google Scholar]
- 61.Wynn D., Kaufman M., Montalban X., Vollmer T., Simon J., Elkins J., O’Neill G., Neyer L., Sheridan J., Wang C., et al. Daclizumab in active relapsing multiple sclerosis (CHOICE study): A phase 2, randomised, double-blind, placebo-controlled, add-on trial with interferon beta. Lancet. Neurol. 2010;9:381–390. doi: 10.1016/S1474-4422(10)70033-8. [DOI] [PubMed] [Google Scholar]
- 62.Reinisch W., de Villiers W., Bene L., Simon L., Rácz I., Katz S., Altorjay I., Feagan B., Riff D., Bernstein C.N., et al. Fontolizumab in moderate to severe Crohn’s disease: A phase 2, randomized, double-blind, placebo-controlled, multiple-dose study. Inflamm. Bowel Dis. 2010;16:233–242. doi: 10.1002/ibd.21038. [DOI] [PubMed] [Google Scholar]
- 63.De Benedetti F., Gattorno M., Anton J., Ben-Chetrit E., Frenkel J., Hoffman H.M., Koné-Paut I., Lachmann H.J., Ozen S., Simon A., et al. Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes. N. Engl. J. Med. 2018;378:1908–1919. doi: 10.1056/NEJMoa1706314. [DOI] [PubMed] [Google Scholar]
- 64.Thorne C., Takeuchi T., Karpouzas G.A., Sheng S., Kurrasch R., Fei K., Hsu B. Investigating sirukumab for rheumatoid arthritis: 2-year results from the phase III SIRROUND-D study. RMD Open. 2018;4:e000731. doi: 10.1136/rmdopen-2018-000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Craig S., Warren R.B. Ixekizumab for the treatment of psoriasis: Up-to-date. Expert Opin. Biol. Ther. 2020;20:549–557. doi: 10.1080/14712598.2020.1729736. [DOI] [PubMed] [Google Scholar]
- 66.Gordon K.B., Blauvelt A., Papp K.A., Langley R.G., Luger T., Ohtsuki M., Reich K., Amato D., Ball S.G., Braun D.K., et al. Phase 3 Trials of Ixekizumab in Moderate-to-Severe Plaque Psoriasis. N. Engl. J. Med. 2016;375:345–356. doi: 10.1056/NEJMoa1512711. [DOI] [PubMed] [Google Scholar]
- 67.Guttman-Yassky E., Brunner P.M., Neumann A.U., Khattri S., Pavel A.B., Malik K., Singer G.K., Baum D., Gilleaudeau P., Sullivan-Whalen M., et al. Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: A randomized, double-blind, phase 2a trial. J. Am. Acad. Dermatol. 2018;78:872–881.e6. doi: 10.1016/j.jaad.2018.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Asano K., Ueki S., Tamari M., Imoto Y., Fujieda S., Taniguchi M. Adult-onset eosinophilic airway diseases. Allergy. 2020;75:3087–3099. doi: 10.1111/all.14620. [DOI] [PubMed] [Google Scholar]
- 69.Cao P.P., Wang Z.C., Schleimer R.P., Liu Z. Pathophysiologic mechanisms of chronic rhinosinusitis and their roles in emerging disease endotypes. Ann. Allergy Asthma Immunol. Off. Publ. Am. Coll. Allergy Asthma Immunol. 2019;122:33–40. doi: 10.1016/j.anai.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jinquan T., Jing C., Jacobi H.H., Reimert C.M., Millner A., Quan S., Hansen J.B., Dissing S., Malling H.J., Skov P.S., et al. CXCR3 expression and activation of eosinophils: Role of IFN-gamma-inducible protein-10 and monokine induced by IFN-gamma. J. Immunol. 2000;165:1548–1556. doi: 10.4049/jimmunol.165.3.1548. [DOI] [PubMed] [Google Scholar]
- 71.Hanaoka R., Kasama T., Muramatsu M., Yajima N., Shiozawa F., Miwa Y., Negishi M., Ide H., Miyaoka H., Uchida H., et al. A novel mechanism for the regulation of IFN-gamma inducible protein-10 expression in rheumatoid arthritis. Arthritis Res. Ther. 2003;5:R74–R81. doi: 10.1186/ar616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Antonelli A., Fallahi P., Delle Sedie A., Ferrari S.M., Maccheroni M., Bombardieri S., Riente L., Ferrannini E. High values of Th1 (CXCL10) and Th2 (CCL2) chemokines in patients with psoriatic arthtritis. Clin. Exp. Rheumatol. 2009;27:22–27. [PubMed] [Google Scholar]
- 73.Lee E.Y., Lee Z.H., Song Y.W. The interaction between CXCL10 and cytokines in chronic inflammatory arthritis. Autoimmun. Rev. 2013;12:554–557. doi: 10.1016/j.autrev.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 74.Rashighi M., Agarwal P., Richmond J.M., Harris T.H., Dresser K., Su M.-W., Zhou Y., Deng A., Hunter C.A., Luster A.D., et al. CXCL10 is critical for the progression and maintenance of depigmentation in a mouse model of vitiligo. Sci. Transl. Med. 2014;6:223ra23. doi: 10.1126/scitranslmed.3007811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee M., Kim D.W., Khalmuratova R., Shin S.H., Kim Y.M., Han D.H., Kim H.J., Kim D.Y., Rhee C.S., Park J.W., et al. The IFN-γ-p38, ERK kinase axis exacerbates neutrophilic chronic rhinosinusitis by inducing the epithelial-to-mesenchymal transition. Mucosal Immunol. 2019;12:601–611. doi: 10.1038/s41385-019-0149-1. [DOI] [PubMed] [Google Scholar]
- 76.Yoshikawa M., Wada K., Yoshimura T., Asaka D., Okada N., Matsumoto K., Moriyama H. Increased CXCL10 expression in nasal fibroblasts from patients with refractory chronic rhinosinusitis and asthma. Allergol. Int. Off. J. Jpn. Soc. Allergol. 2013;62:495–502. doi: 10.2332/allergolint.13-OA-0572. [DOI] [PubMed] [Google Scholar]
- 77.Webb G.J., Hirschfield G.M., Lane P.J. OX40, OX40L and Autoimmunity: A Comprehensive Review. Clin. Rev. Allergy Immunol. 2016;50:312–332. doi: 10.1007/s12016-015-8498-3. [DOI] [PubMed] [Google Scholar]
- 78.Furue M., Furue M. OX40L-OX40 Signaling in Atopic Dermatitis. J. Clin. Med. 2021;10:2578. doi: 10.3390/jcm10122578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guttman-Yassky E., Pavel A.B., Zhou L., Estrada Y.D., Zhang N., Xu H., Peng X., Wen H.C., Govas P., Gudi G., et al. GBR 830, an anti-OX40, improves skin gene signatures and clinical scores in patients with atopic dermatitis. J. Allergy Clin. Immunol. 2019;144:482–493.e7. doi: 10.1016/j.jaci.2018.11.053. [DOI] [PubMed] [Google Scholar]
- 80.Liang Z.P., Xu W., Zhao F.P., Pan H.Z., Feng H.J., Xu S.E., Zhao C., Bao Y.L., Jiang L., Huang Y., et al. Effect of Blocking the OX40/OX40L Signaling Pathway by siRNA Interference on Animal Experimental Study of Allergic Rhinitis. Arch. Med. Res. 2019;50:442–450. doi: 10.1016/j.arcmed.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 81.Liu T., Li T.L., Zhao F., Xie C., Liu A.M., Chen X., Song C., Cheng L., Yang P.C. Role of thymic stromal lymphopoietin in the pathogenesis of nasal polyposis. Am. J. Med. Sci. 2011;341:40–47. doi: 10.1097/MAJ.0b013e3181f20489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.