Abstract
Introduction
Gastrointestinal Stromal Tumors (GIST) are rare mesenchymal neoplasm of gastrointestinal tract. Stomach is the most common site affected by GIST compared to other places in gastrointestinal track. The coexistence of GIST with another malignancy represents a rare phenomenon with few literature reported.
Case presentation
We present here 65 years old patient with stomach GIST and synchronous pancreatic adenocarcionoma discovered during surgery for suspected pancreatic mucinious cystadenoma. Distal pancreaticosplenectomy with excision of GIST Tumor & wedge resection of stomach was done. Histopathological examination of resected specimens reported the margins are clear.
Discussion
In this article we discuss on the option of systemic therapy versus upfront surgery and their outcome benefit based on literature review.
Conclusion
The coexistence of GIST with pancreatic adenocarcinoma is a rare condition. High clinical analysis needed during laparotomy for GIST to detect a synchronous tumor. In a case of GIST the surgeon should recognize the possibility of another tumor with different histological origin. Surgical excision is the mainstay of therapy and it has proven to be curative for our patient. . Due to its rare occurrence and limited literature further studies has to be done on GIST with other synchronous tumor to help the surgeon to manage the patient optimally.
Keywords: Gastrointestinal stromal tumor (GIST), Pancreatic adenocarcinoma, Synchronous tumor
Highlights
-
•
A rare presentation of Gastrointestinal Stromal Tumor (GIST) with Pancreatic Adenocarcinoma in a 65 years old gentleman.
-
•
It is a challenging diagnostic dilemma in patients with dual pathology.
-
•
There is a need of Intraoperative assessment in patients with GIST tumor to rule out synchronous tumors.
-
•
It highlight the role of neoadjuvant imatinib versus surgery upfront benefits the prognosis.
1. Introduction
Gastrointestinal Stromal Tumors (GIST) are rare mesenchymal-derived neoplasm arising from gastrointestinal tract and accounts for 1% of all Gastrointestinal malignancy [1]. The incidence is 1.5 per 100,000 per year. GIST is believed to be originating from Interstitial cells of Cajal which is responsible for gut motility [1]. GIST can occur anywhere in the Gastrointestinal Tract and abdominal cavity, yet the most common site of origin is stomach (60%) followed by small intestine (30%) [2]. This tumor have malignant potential and their behaviour is difficult to predict. Synchronous tumor with GIST are rarely reported in literature. Here we present a synchronous Gastrointestinal Stromal Tumor with pancreatic adenocarcinoma in a 65 years old gentleman who presented with abdominal mass. The dual pathology was detected post operatively based in histopathological examination report. This case report has been reported in line with the SCARE 2020 criteria [3].
2. Case presentation
A 65 year old gentleman presented with abdominal discomfort for one year. Patient denies any abdominal pain, fever, altered bowel habits or any constitutional symptoms. He had no positive history of malignancy. On clinical examination, no abdominal mass palpable. Proceeded with abdominal ultrasonography and revealed cystic abdominal mass lesion at the left upper quadrant likely represent serous cystadenoma of pancreatic tail.
Oesophagogastroduodenoscopy (OGDS) showed stomach had indentation at the corpus of the stomach in keeping with external compression. The mucosa overlying the area of indentation appears slightly depressed inflamed with loss of rugae. Proceed with endoscopic ultrasound (EUS), noted there was large irregular cystic mass arising from the body of pancreas measuring more (15 × 12 cm) with thick wall and hyprechoic debris within. We also noted another multiseptatated, multicystic cust visualised at the tail of the pancreas measuring 40 × 30 mm without high risk features. Pancreatic parenchyma was heterogenously hypoechoic within body and the tail with moderate amount of stranding, dilated and tortuous main pancreatic duct with multiple cystic lesions within the pancreatic parenchyma. Pancreatic cyst fluid for cytology showed no malignant cell seen. Computed tomography (CT) scan of the abdomen finding suggesting large cystic pancreatic tail mass lesion compatible with a pre malignant pancreatic mucinous cystadenoma (Fig. 1).
Fig. 1.
Large cystic pancreatic tail mass lesion (white arrow).
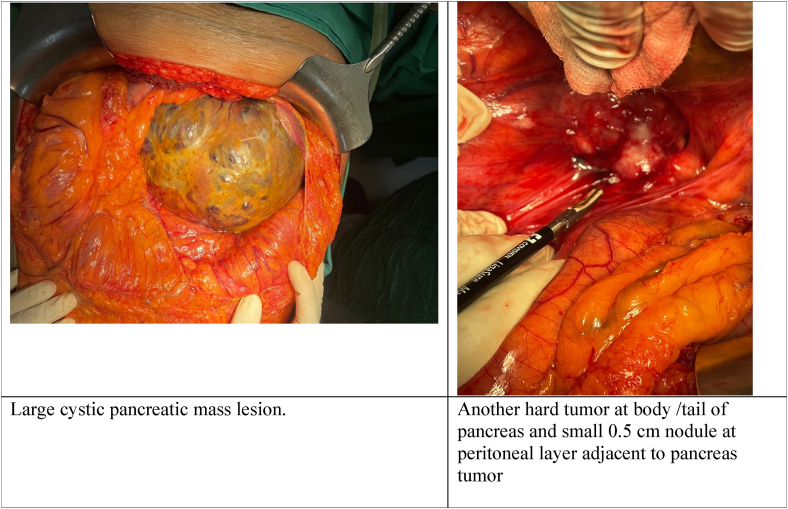
Patient was proceeded with surgery. Operative findings revealed large cystic tumor (15 × 20 cm) with loss of plane with posterior wall of stomach and separate from pancreas (with clear plane) (Fig. 2 and Fig. 3.) and there was no ascites and no peritoneal or liver nodule. On table sonography done,. Another hard tumor at body/tail of pancreas and small 0.5 cm × 0.5cm nodule at peritoneal layer adjacent to pancreas tumor. Distal pancreaticosplenectomy with excision of GIST Tumor and wedge resection of stomach was done. Histopathology revealed ductal adenocarcinoma of pancreas and stomach GIST. Post operative patient was well. On surveillance no recurrence of dual pathology. Patient was subjected to adjuvant therapy subsequently.
Fig. 2.
A: Large cystic pancreatic mass lesion. B: Another hard tumor at body/tail of pancreas and small 0.5 cm nodule at peritoneal layer adjacent to pancreas tumor.
Fig. 3.
A: Cystic tumor with posterior wall of stomach. B: Distal pancreas and spleen.
3. Discussion
GIST and adenocarcinoma represent two distinct oncogenic entities [4]. GIST are mesenchymal origin of the GI tract. Hirota proved that GIST tumor express CD 117 antigen (C-Kit), a mutation responsible for growth of GIST [[4], [5]]. Surgical resection has always been the fundamental in management of GIST. In recent years with discovery of the mutation associated with these tumors, the treatment has changed. Imatinib, a tyrosine kinase inhibitor (TKI) has been introduced as adjuvant or neoadjuvant to improve the management of GIST.
Pancreatic adenocarcinoma develop from epithelial cell.The management depends on the stage of tumor. In term of curative, surgical resection is the only potential cure (Stage 1 & 2). Localised tumor are categorized operable or not (locally advance) based on involvement of local vessels [6]. Despite carefully assessment for surgical candidate, many of these patient has microscopically positive margin in post op histopathology reports. Pancreaticoduodenectomy is surgery of choice for tumors of the head and body of pancrease [6]. Tumors in tail and body are removed via distal pancreatectomy as in our case. Adjuvant and neoadjuvant therapy are also being studied to improve the outcomes associated with surgery alone [6].
4. Conclusion
The coexistence of GIST with pancreatic adenocarcinoma is a rare condition. High clinical analysis needed during laparotomy for GIST to detect a synchronous tumor. Due to its rare occurrence and limited literature further studies has to be done on GIST with another synchronous tumor. In any case of GIST the surgeon should recognize the possibility of another tumor with different histological origin. Surgical excision is the mainstay of therapy and it has proven to be curative for our patient. Further research is needed for explaining this simultaneous tumor development. The postoperative adjuvant chemotherapy should be consider for the adenocarcinoma, depending on the pathology report and disease stage in combination of TKI such as imatinib for the GIST depending on the risk category stratification according to the international guidelines.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. Permission was also obtained from local administrative. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
None.
Ethical approval
Ethical approval obtained from local institution.
Consent
Patient consented for the write up and publication.
Guarantor
Dr Thiru Kumar will be the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish at this given time of submission.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103588.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Theodosopoulos T., Dellaportas D., Psychogiou V., Gennatas K., Kondi-Pafiti A., Gkiokas G., Papaconstantinou I., Polymeneas G. Synchronous gastric adenocarcinoma and gastrointestinal stromal tumor (GIST) of the stomach: a case report. World J. Surg. Oncol. 2011;9(1) [Google Scholar]
- 2.Efstathios P., Athanasios P., Papaconstantinou I., Alexandros P., Frangisca S., Sotirios G., Evangelos F., Athanasios G. Coexistence of gastrointestinal stromal tumor (GIST) and colorectal adenocarcinoma: a case report. World J. Surg. Oncol. 2007;5(1) [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Gonçalves R., Linhares E., Albagli R., Valadão M., Vilhena B., Romano S., Ferreira C. Occurrence of other tumors in patients with GIST. Surg. Oncol. 2010;19(4):e140–e143. doi: 10.1016/j.suronc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 5.C N., L R., T S., A S., Dl D., C C. Gastrointestinal stromal tumor (GIST) associated with synchronous colon adenocarcinoma - a case report. 2021. https://www.ncbi.nlm.nih.gov/pubmed/22457867 [online] PubMed. Available at:
- 6.Ryan D., Hong T., Bardeesy N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014;371(11):1039–1049. doi: 10.1056/NEJMra1404198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.