Abstract
Background
lack of medical practitioners’ knowledge about oral cancer has contributed to delays in referral and treatment. Oral cancer is amenable to treatment when detected early, which leads to better prognosis and survival rates. In this study, we aimed to assess the knowledge of the Syrian medical students about the risk factors of oral cancer, oral cavity changes associated with oral cancer, and the relation between the relation with Human Papilloma Virus (HPV) and oral cancer.
Methods
This is a cross-sectional study conducted at the Syrian Private University. Data were collected through self-administered questionnaires, which targeted social demographic information, general knowledge, risk factors, oral changes and HPV knowledge associated with oral cancer. Data was categorized and analyzed to assess and compare the levels of knowledge between clinical and preclinical students.
Results
301 out of 401 medical students responded to the questionnaires bringing the response rate to 75.25%. The study revealed adequate knowledge about oral cancer, general information, clinical features, risk factors and relation to HPV. Clinical students showed higher levels of awareness compared to pre-clinical students. No significance in knowledge was found between the genders.
Conclusion
The findings of the present study suggest that there is a need to reinforce the medical curriculum concerning oral cancer education, particularly in prevention and early detection to improve practices.
Keywords: Oral cancer, Awareness, Knowledge, HPV, Syria, Medical students
Highlights
-
•
In Syria, the incidence and mortality rates of OC and OPC were 2 and 0.8 per 100,000 annum, respectively.
-
•
Awareness about OC was positively correlated with the year of study
-
•
Low level of awareness about OC was found among medical students.
Abbreviations
- OC
Oral cancer
- SCC
Squamous cell carcinoma
- HPV
human papillomavirus
- MENA
Middle East and North Africa region
- OPC
Oropharyngeal Cancer
- HNC
Head and Neck Cancer
- SCC
Squamous Cell Carcinoma
- SPU
Syrian Private University
- SD
standard deviation
- SPSS
Statistical Package for Social Sciences
- IRB
Institutional Review Board
- GPA
Grade Point Average
- CME
Continuing Medical Education
1. Introduction
Oral cancer (OC) and oropharyngeal cancer (OPC) are principally divided into two subtypes: Human Papillomavirus (HPV)-positive OC and OPC), which result from an oral HPV sexually-transmitted infection (STI), and HPV-negative OC and OPC, which are mainly linked to the use of alcohol and tobacco. OC and OPC, which include malignant neoplasms of the lips, oral cavity, and pharynx, pose a significant and growing concern to health systems worldwide [1,2]. OC and OPC rank in the top 10 cancers worldwide [3]. In 2018, the worldwide incidence and mortality for OC were reported to be 656,000 and 336,000 respectively, accounting for 3.6% of both new cancer cases as well as cancer deaths [4]. These rates are likely to increase, as indicated by one report that expected the incidence rate of HPV-positive head and neck cancer (HNC) to surpass that of cervical cancer in the United States by the year 2020 [5]. The significance of this report predict the increasable risk of diffusion the cancer in the next years if there is no reliance the suitable investigations for early diagnosis and accurate therapy. GLOBOCAN estimated the incidence and mortality of OC and OPC in the Middle East and North Africa region (MENA) as 2.2 and 1 per 100,000 per annum. In Syria, the incidence and mortality rates of OC and OPC were 2 and 0.8 per 100,000 annum, respectively, which were higher than what was observed in Iran (1.8 and 0.7 per 100,000 annum) and Jordan (1.7 and 0.6 per 100,000 annum) but lower than those reported in Iraq (2.3 and 1.1 per 100,000 annum), and Egypt (2.4 and 1 per 100,000 annum) [6].
OC has various etiological agents such as tobacco, alcohol, areca nut chewing, advanced age, and HPV infection [7]. HPV is among the most common STI8, and studies from developed countries reported that 56% of OPCs are HPV-related [8]. However, developing countries provided limited studies on this topic [9]. In Syria, the absence of a widely available HPV suggests the OC is becoming a serious problem on the national level.
The majority of OCs can be detected in their early stages during screening programs, thereby reducing rates of morbidity and mortality, lowering treatment costs, and improving quality of life [10]. Therefore, physician and patient awareness must be the first line of defense in preventing the proliferation of this disease and subsequent malignancies. Increasing the number of medical professionals who perform accurate oral examinations is one way to meet this goal and improve prognosis. This invaluable training must start at medical school to alter future career habits. Studies suggest that most pediatricians do not routinely discuss HPV-positive HNC owing to a self-reported lack of knowledge [11]. Hence, it becomes imperative to examine how we are training our next generation of physicians regarding this epidemic.
The awareness and knowledge of OC is essential for the diagnosis, treatment, and prevention of this disease, especially among medical students who are going to tackle this health problem in different specialization. Therefore, the aim of this study is to measure the level of awareness and general knowledge of OC among medical students at the Syrian Private University (SPU), note the influence of clinical years on the students' knowledge, identify the gabs in the medical students’ awareness, and suggest solutions for these problems.
2. Methods
2.1. Study design, setting, and participants
A cross sectional study was conducted at the medical school of the Syrian Private University (SPU) in Damascus, Syria. The data were collected in July 2021. The sample included medical students in all years of study. Participation was voluntary, and anonymity was assured. Students were permitted to withdraw from the study at any in time. The sample size was calculated using an online sample size calculator (https://epitools.ausvet.com.au/oneproportion). Setting the confidence level at 95% and the desired accuracy at 5%, the target sample size was 297 students out of 1300. The questionnaire was distributed to 401 random students to ensure that the required number was reached even after excluding the incomplete questionnaires. In total, 343 students responded to the questionnaires. Of these, 301 students returned complete questionnaires, and these were included in the data analysis. Our article is fully compliant with the STROCSS 2021 criteria [38].
2.2. Tools of study
We used a structured self-administered questionnaire in English. The questionnaire was formulated using questions from previously published studies [12,13], and it was reviewed by a specialist. The first section of the questionnaire included socio-demographic questions including, age, marital status, gender, current residence, educational year, GPA, smoking and alcohol consuming. The second section of the survey contained 28 knowledge-assessing questions organized in four sections, and these were “basic knowledge and practices” which contained 6 questions, “risk factors”, which contained 7 questions, “oral cavity changes in oral cancer” which contained 10 questions, and “knowledge of the relation between HPV and OC” which contained 5 questions. For each question, the participants were offered multiple options to choose from with only one option being the correct answer. One point was given to each correct answer, while incorrect answers or “Do not know” answers were given zero points. Individual knowledge scores were calculated as the percentage of points obtained by each student, with 100% considered equivalent to the maximum number of points that a student can obtain. Mean knowledge scores were calculated as the average of the individual scores. The questionnaire is available in Appendix.
Ethical approval of the study was obtained from the Institutional Review Board (IRB) at the Faculty of Medicine in SPU.
2.3. Statistical analysis
Data was analyzed using the Statistical Package for Social Sciences version 25.0 (SPSS Inc., Chicago, IL, United States). Data was reported as frequencies and percentages (for categorical variables) or means, medians and standard deviations (SD) (for continuous variables). The relationship between independent variables and the mean knowledge scores was assessed using Independent Samples t-Test and Pearson chi-square test. P-values < 0.05 was considered statistically significant.
2.4. Ethical consideration
Informed consent was obtained from all participants before filling out the questionnaires.
3. Results
3.1. Demographic characteristics
Of the 401 medical students who participated in this study, 301 fully answered the administered questionnaire, thereby placing the respondent rate at 72.25%. The age of participants ranged from 18 to 30 years (21.6years ± 3.6). Moreover, the majority were males [148 (61.15%)], single [266(88.3%)], and live in Damascus [172 (57.1%)]. Finally, our sample was composed of clinical [197 (65.5%)] and preclinical students [104 (34.5%)] (Table 1).
Table 1.
Socio-demographic characteristics: (n = 301).
| Age | Under 20 | 52 (17.2%) | GPA | <2.0 | 34 (11.2%) |
| 20–25 | 235 (78%) | 2.0–2.5 | 176 (58.5%) | ||
| Above 25 | 14 (4.6%) | 2.5–3.0 | 71 (23.5%) | ||
| Gender | Male | 184 (61.1%) | >3.0 | 20 (6.6%) | |
| Female | 117 (38.8%) | Current residence | City | 172 (57.1%) | |
| Social Status | Single | 266 (88.3%) | Rural | 129 (42.8%) | |
| In a relationship | 28 (9.3%) | College Year | 1st | 43 (14.2%) | |
| Married | 7 (2.3%) | 2nd | 13 (4.3%) | ||
| Alcohol Use | yes | 30 (10%) | 3rd | 48 (15.9%) | |
| no | 271 (90%) | 4th | 51 (16.9%) | ||
| Smoking | yes | 103(34.2%) | 5th | 85 (28.2%) | |
| no | 198(65.7%) | 6th | 61 (20.2% | ||
3.2. Knowledge assessment
-
1.
Oral cancer Basic knowledge and Practice:
Overall, 165 students (54.8%) knew that squamous cell carcinoma (SCC) is the most common type of OC. Of these, 145 students (73.6% were in their clinical years, while only 20 students (19.2%) were in their the preclinical years, and the difference was significant (Chi-square = 81.248, P-value <0.001) .
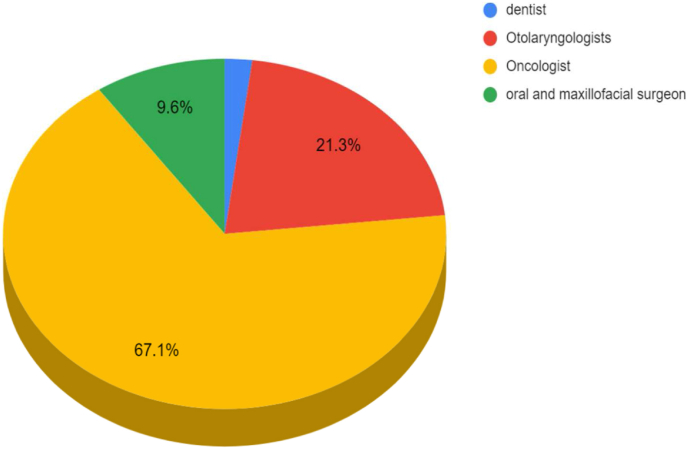
Moreover, 226 students (86.8%) stated that early detection of OC leads to curation. On the other hand, only 83 participants (27.5%) declared that tongue and floor of the mouth are the most common sites of OC, and 260 responders(86.4%) incorrectly believed that the median border of the tongue is most likely to develop OC. Finally, 217 students (72%) stated that they screen the oral mucosa of high-risk patients. Of these, 157 were clinical students (79.7%) and 60 werepre-clinical students (57.7%), and the difference was significant (Chi-square = 16.379, P-value <0.001)(Table 2). As for referral preferences, 202 responders (67.1%) indicated that they would refer patients with suspicion of OC to an oncologist (Fig. 1).
Table 2.
Oral cancer basic knowledge and practice questions. (n = 301).
| Oral cancer basic knowledge and practice | Assessment results (the correct answer), N (%) |
|||||
|---|---|---|---|---|---|---|
| Pre-clinical (n = 104) | Clinical (n = 197) | Total (n = 301) | Chi-Square | p-value | ||
| 1- Squamous cell carcinoma is the most common form of oral cancer. | 20 | 145 | 165 | 81.248 | 0.000* | |
| 19.2% | 73.6% | (54.8%) | ||||
| 2- Tongue and floor of the mouth are the most common sites of oral cancer. | 25 | 58 | 83 | 0.995 | 0.345 | |
| 24% | 29.4% | (27.5%) | ||||
| 3- Median border of the tongue is most likely to develop oral cancer. | 14 | 27 | 41 | 0.003 | 1 | |
| 13.5% | 13.7% | (13.6%) | ||||
| 4- Oral cancer can be cured if detected early. | 73 | 153 | 226 | 2.032 | 0.163 | |
| 70.2% | 77.7% | (75%) | ||||
| practice question | ||||||
| 5- Do you screen the oral mucosa if the patients are in a high-risk category | 60 | 157 | 217 | 16.379 | 0.000* | |
| 57.7% | 79.7% | (72%) | ||||
Fig. 1.
Where would you refer a patient if you suspect a malignant tumor in the mouth?.
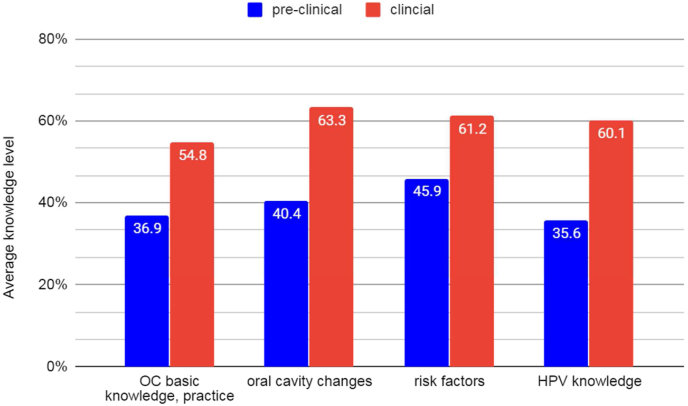
In total, the mean knowledge score in this section was 48.6% ± 23.1 with pre-clinical students having a significantly lower mean knowledge score (36.9%) compared with clinical students (54.8%) (t = -6.851, P value <0.001) (Fig. 3).
-
2.
Oral cancer risk factors
Fig. 3.
Comparison between Pre-medical and medical students knowledge in each axis.
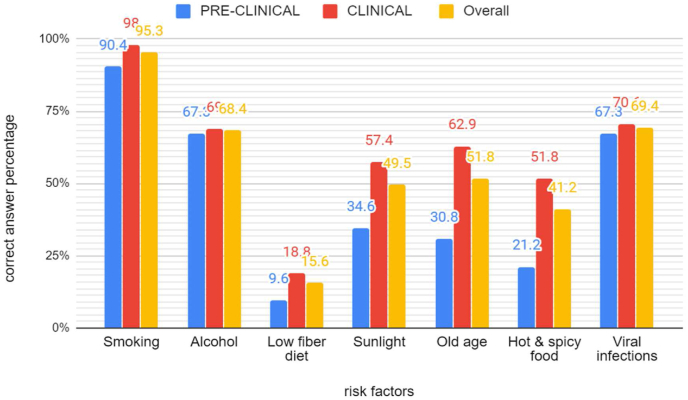
The majority of students knew that smoking [287 (95.3%)], viral infection [209 (69.4%)], and alcohol [206 (68.4%)] were risk factors of OC. Other risk factors of OC that were less recognized by the participants included old age [156 (51.8%)], sunlight [149 (49.5%)], hot and spicy food [124 (41.2%)], and low fiber diet [47 (15.6%)] (Fig. 2).
Fig. 2.
Clinical and pre-clinical students knowledge of oral cancer Risk factors.
Overall, the mean knowledge score in this section was 55.9% ± 21.7 with pre-clinical students having a significantly lower mean knowledge score (45.9%) compared with clinical students (61.2%) (t-test = -6.169, P-value <0.001) (Fig. 3).
-
3.
Oral cavity changes in OC
Most students named oral cavity mass [242 (80.4%)], non-healing ulcers [229 (76.1%)], necrosis [220 (73.1%)], and bleeding [198 (65.8%)] as oral cavity changes in OC. However, only 121 students (40.1%) and 137 students (45.5%) could identify Erythroplakia and leukoplakia, respectively, as oral cavity changes in OC (Table 3). Overall, the mean knowledge score in this section was 55.4% ± 23.2 with pre-clinical students having a significantly lower mean knowledge score (40.4%) compared with clinical students (63.3%) (t-test = -9.193, P-value <0.001) (Fig. 3).
-
4.
Knowledge about the relation between HPV and OC
Table 3.
Knowledge about oral cavity changes. (n = 301).
| Oral changes | Assessment results (yes), n (%) |
||||
|---|---|---|---|---|---|
| Pre-clinical (n = 104) | Clinical (n = 197) | Overall | Chi-Square | p-value | |
| Oral leukoplakia | 30 | 107 | 137 | 17.804 | 0.000* |
| 28.8% | 54.3% | (45.5%) | |||
| oral erythroplakia | 21 | 100 | 121 | 26.203 | 0.000* |
| 20.2% | 50.8% | (40.1%) | |||
| chronic hyperplastic candidiasis | 28 | 62 | 90 | 0.672 | 0.130 |
| (Candida albicans) | 26.9% | 31.5% | 29.9% | ||
| non-healing ulcers | 61 | 168 | 229 | 26.515 | 0.000* |
| 58.7% | 85.3% | 76.1% | |||
| Bleeding | 51 | 147 | 198 | 19.788 | 0.000* |
| 49% | 74.6% | 65.8% | |||
| Necrosis | 44 | 176 | 220 | 76.551 | 0.000* |
| 42.3% | 89.3% | 73.1% | |||
| Difficulty in chewing and swallowing | 59 | 160 | 219 | 20.592 | 0.000* |
| 56.7% | 81.2% | 72.8% | |||
| Restrict mouth movement | 48 | 139 | 187 | 17.229 | 0.000* |
| 46.2% | 70.6% | 62.1% | |||
| Lymphadenopathy | 63 | 164 | 227 | 18.870 | 0.000* |
| 60.6% | 83.2% | 75.4% | |||
| mass in the oral cavity | 78 | 164 | 242 | 2.939 | 0.095 |
| 75% | 83.2% | 80.4% | |||
The awareness level in this section was (51.6% of 29). About half of the participants [148 (49.1%)] knew that HPV infection is one of the main causes of OC development. Moreover, 77 female students (65.8%) and 118 male students (64.1%) stated that HPV could be transmitted through dental procedures. Finally, 146 of the responders (48.5%) were aware of the HPV vaccine, and 123 students (40.8%) knew that it is unavailable in the Syrian national vaccination program (Table 4).
Table 4.
HPV knowledge.
| Female (n = 117) | Male (n = 184) | Overall (n = 301) | Chi-Square | P-value | |
|---|---|---|---|---|---|
| HPV infection is one of the most important causes of OC development | 59 | 89 | 148 | 0.243 | 0.638 |
| 50.4% | 48.3% | 49.1% | |||
| HPV can be transmitted through oral sex | 69 | 96 | 165 | 1.335 | 0.285 |
| 58.9% | 52.1% | 54.8% | |||
| HPV can be transmitted through dental treatment tools | 77 | 118 | 195 | 0.089 | 0.805 |
| 65.8% | 64.1% | 64.7% | |||
| There is a vaccine for HPV | 60 | 86 | 146 | 0.591 | 0.479 |
| 51.2% | 46.7% | 48.5% | |||
| The HPV vaccine is included in the Syrian National Vaccine Program | 48 | 75 | 123 | 0.002 | 1 |
| 41% | 40.7% | 40.8% |
Overall, the mean knowledge score in this section was 51.6% ± 29 with pre-clinical students having a significantly lower mean knowledge score (35.6%) compared with clinical students (60.
1%) (t-test = -7.453, P-value <0.001) (Fig. 3).
4. Discussion
The mean knowledge score in the field of OC was significantly higher among clinical students (65.8% ± 16.7) compared with pre-clinical students (47.9% ± 16.7) (t-test = -10.30, P-value <0.001). This is expected because, unlike preclinical students, clinical students have already attended lectures and completed clinical rotations in otorhinolaryngology which may have contributed to their high level of knowledge about OC. Our findings are consistent with similar studies that were conducted in South Carolina, Nepal, and Sri Lanka [[14], [15], [16]]. In our study, 34.2% of the students reported being smokers. This number is higher than what was observed in a previous study that found that 24.7% of university students in Syria smoke cigarettes [CIC] [7,17]. Similarly, our result is higher than what was reported in studies conducted in Dublin (28.8%), France (21%), Brazil (16.3%), and Nepal 10(3.5%) [14,[18], [19], [20]]. This high prevalence of smokers among our medical students does not only increase the risk of OC, but it also attracts 19 other types of cancers.
Regarding OC basic knowledge. SCC was considered the most common form of OC by 54.8% of the responders, with the significant majority being clinical students (73.6%) (Chi-Square = 81.248, P-value <0.001). Our results are in agreement with several other similar studies. In South Carolina, 49.8% of medical students regarded SCC as the most common type of OC with the majority of the responders being clinical students(72.7%). In Midwestern University, SCC is considered the main type of OC by 83% of medical students, among which 80% are in their clinical years. A study in Chicago reported that 87.5% of clinical students knew that SCC is the most common type of OC compared with only 27.5% of preclinical students [15,21,22]. On another hand, our study revealed a gap in knowledge among our students about the anatomical sites of OC, as only 27.5% of the participants knew that the tongue and the floor of the mouth are the most common sites of OC. In a similar fashion, only 18%, 21% and 31.6% of medical students were aware of the anatomical sites of OC in South Carolina, Chicago and Midwestern University, respectively [15,21,22].
Even though there is a huge development in cancer diagnosis and treatment, OC still has poor survival rates, mainly due to delays in presentation. This is reflected in the 5-year survival rates for late-stage OC, as these rates do not exceed 50% except in the best treatment centers. However, studies show that these results can be improved with early detection and treatment [12,23]. The public health initiative “Healthy People 2010: Understanding and Improving Health and Objectives for Improving Health” predicted that early detection of OC should increase the survival rate from 33% to 51%. In our study, 75% of the students were aware of this information. In comparison, only 38% of Malaysian medical students (38%) said that oral cancer could be cured if detected early [24].
Health care workers do not routinely examine the oral cavity, partially due to inappropriate training on how to conduct a full oral examination [25]. Our study showed that 72% of the students will screen high risk patients for oral cancer, which is higher than what was observed in studies conducted in the UK (28%) and Malaysia (60.6%) [13,26].
The majority of patients with head and neck cancers are diagnosed in advanced stages. This is all dependent on the number of healthcare visits in early stages (median=21 visits) and late stages (median=6 visits), and type of healthcare received before diagnosis and location of the facility providing this service [27]. In our study, Oncologists were the most preferred specialists by students to refer patients with suspicion of OC (67.1%). On the other hand, otolaryngologists and maxillofacial surgeons were preferred in Midwestern University and Malaysia, respectively [21,26]. As there are no primary health care systems in Syria, dentists can act as a safety net, since they frequently examine the oral cavity. Therefore, investing in workshops and awareness campaigns among dental students to identify lesions and request referrals on that basis will act as an efficient screening program in the community.
Smoking, viral infection and alcohol consumption were correctly named as risk factors OC by (95.3%), (69.4%), and (68.4%) of our students, respectively. This is in line with the results of similar studies conducted in Saudi Arabia and Malaysia [12,28]. In contrast, our participants were less aware about other risk factors such as old age (51.8%), sunlight (49.5%), hot and spicy food (41.2%), and low fiber diet (15.6%). Similar misconceptions were noticed in other studies [24,28]. The high level of awareness of the dangers cigarette and tobacco smoking, alcohol abuse, and other health risks among medical students is an essential prerequisite for any tobacco and alcohol cessation campaigns targeted at the community.
Regarding the oral cavity changes in OC, only 40.1% and 45.5% of the participants recognized erythroplakia and leukoplakia, respectively, as oral cavity changes in OC. Studies in America, Malaysia, and Midwestern University reported that 19.6%, 24.5%, and 27.5% of the medical students, respectively, were aware that erythroplakia was a sign of OC. Moreover, 35.4%, 33.8%, and 28.5% of the participants, respectively, knew that leukoplakia is associated with OC [15,21,26]. Chronic hyperplastic candidiasis caused by candida albicans was recognized by 29.9% of students, which is lower than what was observed in a Nepali study (38.1%) [14]. In contrast, the majority of our responders were aware that an oral cavity mass (80.4%), an unhealed ulcer (76.1%), necrosis (73.1%), and bleeding (65.8%) were oral cavity changes in OC, and this result was similar to other studies [24]. Finally, 68.1% and 62.1% of our students knew that chewing and swallowing difficulties, and restricted mouth movements, respectively, were oral changes associated with OC. This observation was in line with what was reported in other studies [29].
HPV is the most sexually transmitted infection worldwide, and oropharyngeal cancer (OPC) is an ominous outcome of HPV infection8. In light of the forgoing, we assessed the knowledge of male and female students about the relation between HPV infection and OC, and we found no significant difference in the awareness levels between the two groups. Our study showed that 49.1% of the responders were aware of the association of HPV infections with OC development. However, a higher level of awareness was found in Nepal (83.5%) and Malaysia (53.7%) [14,28]. Data from the Health Information National Trends Survey revealed poor awareness about the relation between HPV and OC, with only 30% of the participants acknowledging this association [30].
Sexual contact, including deep kissing and oral sex, are pathways of HPV transmission. The likelihood of contracting oral HPV is directly associated with the number of sexual partners, and with the early onset of sexual activity. In our study, 54.8% of the students chose oral sex as a source of HPV infection, which is higher than a Polish study (45.1%) [30]., Educational intervention on safe-sex behaviors and evaluations to determine high-risk groups are paramount for primary prevention strategies, especially in this war crisis.
Our study showed that 48.5% of the students knew about the availability of HPV vaccine, which is similar to a Polish study (50%) but higher than a Chinese study (17.5%) [29,31]. A marked decline in HPV infections were noted in countries with implemented HPV vaccination programs as a primary preventive intervention [32,33]. Syria has not integrated the HPV vaccination into the national immunization program [34], and only 123(40.8%) students were aware of this. The key reason for this delay is the inability of the currently suffering economy to manage the added costs of this integration. According to the World Health Organization, phased introductions of HPV vaccination can serve as an alternative in countries where financial or operational constraints prevent implementation of a national immunization programme. In this case, priority should be given to populations that have high risk groups and less access to screening programs [35]. We need to pay more attention to spreading educational understanding about cancer timely identification and how to avoid false and delayed cancer examination outcomes. Continuing medical education reduced the risk of developing cancer of speedily patients – as assessed by medical doctors and had a confined effect on general practitioners' awareness of serious illness and perception toward their own responsibility in the early diagnosis; even so, continuing medical education (CME) had no influence on Physicians' attitudes on procedures associated of emergency consultation and self-assessed competence to examine. A structured CME practice might be successful in improving Physician attitude and perception, particularly risk assessment, that can lead to improve clinical outcomes [36,37]. Finally,We faced limitations in the student response rate, as some final year medical students opted out of the study, which may have affected the results. Some survey questions may have been limiting. For example, question 5 did not specify the type of examination as in inspection, palpation, or both. Moreover, the participants in this study were from a single university, yielding a relatively small.
5. Conclusion
This study showed a higher level of awareness about OC among clinical students compared with pre-clinical students. The low level of awareness about OC found among medical students requires an enhancement in the curricula and teaching methods to optimize oral cancer practices. The increase in the global prevalence of oral cancers requires early prevention and detection from medical practitioners to improve the overall prognosis.
Funding
Syrian Private University obtained all materials needed for this study. No contribution to data design, collection, analysis or interpretation was made by any funding resource. No other funding sources.
Availability of data and materials
All data related to this paper's conclusion are available and stored by the authors. All data can be made available by the corresponding author upon a reasonable request.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) at the Syrian Private University (SPU), and it was rated as a study with humans not on humans. A written consent was obtained from all participants. Participation in the study was voluntary and participants were assured that there would be no negative consequences on anyone who did not want to participate or who decided to withdraw after giving consent.
Authors’ contributions
MAA and HA contributed equally in all stages of the study. HA, MS, MAA, DAA, SS, HG, KM conceptualized the study, participated in the design, wrote the study protocol, performed statistical analysis and drafted the manuscript. HI, MAA, BS, FM participated in the design, did literature search and revision of draft. All authors read and approved the final draft.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None of the authors have any competing interests. The authors alone are responsible for the content and the writing of the article. No conflict of interest is declared.
Acknowledgments
We are thankful for the Syrian Private University administration for the support. We are thankful for all students who participated in this study and for Mrs. Marah Muarrawi for help with the statistical analysis.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2022.103504.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. Apr-May 2009;45(4–5):309–316. doi: 10.1016/j.oraloncology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Kazmi F., Chaudhary M.A., Mumtaz M., Bhatti M.U.D., Khawaja N.J.P.O., Journal D. Oral cancer knowledge and awareness amongst undergraduate dental students of Lahore-Pakistan. Pakistan Oral and Dent. J. 2011;31(1) [Google Scholar]
- 3.Applebaum E., Ruhlen T.N., Kronenberg F.R., Hayes C., Peters E.S. Oral cancer knowledge, attitudes and practices: a survey of dentists and primary care physicians in Massachusetts. JADA (J. Am. Dent. Assoc.) Apr 2009;140(4):461–467. doi: 10.14219/jada.archive.2009.0196. 1939. [DOI] [PubMed] [Google Scholar]
- 4.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca - Cancer J. Clin. Nov 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 5.Laitman B.M., Ronner L., Genden E. The role of otolaryngologists in eradicating human papillomavirus. JAMA otolaryngol. head neck surg. Dec 1 2018;144(12):1186. doi: 10.1001/jamaoto.2018.2444. [DOI] [PubMed] [Google Scholar]
- 6.Pollaers K., Kujan O., Johnson N.W., Farah C.S. Oral and oropharyngeal cancer in Oceania: incidence, mortality, trends and gaps in public databases as presented to the Global Oral Cancer Forum. Translat. Res. Oral Oncol. 2017 doi: 10.1177/2057178X17726455. [DOI] [Google Scholar]
- 7.Idris A., Al Saadi T., Turk T., et al. Eastern Mediterranean health journal = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. Vol. 24. May 3 2018. Smoking behaviour and patterns among university students during the Syrian crisis; pp. 154–160. 2. [PubMed] [Google Scholar]
- 8.WHO Human Papillomavirus (HPV) and Cervical Cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer World Health Organisation. Updated 24 January 2019, Accessed January, 2020.
- 9.de Martel C., Ferlay J., Franceschi S., et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. Jun 2012;13(6):607–615. doi: 10.1016/s1470-2045(12)70137-7. [DOI] [PubMed] [Google Scholar]
- 10.Brill JV, 2020. Screening for cancer: the economic, medical and psychosocial issues, Am J Manag Care. 26 (14 Suppl); S300-S306. doi:10.37765/ajmc.2020.88534. [DOI] [PubMed]
- 11.Laitman B.M., Oliver K., Genden E. Medical student knowledge of human papillomavirus-positive head and neck cancer. JAMA otolaryngol. head neck surg. Apr 1 2018;144(4):380–382. doi: 10.1001/jamaoto.2017.3089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kujan O., Abuderman A., Azzegahiby S., Alenzi F.Q., Idrees M. Assessing oral cancer knowledge among Saudi medical undergraduates. J. Cancer Educ. : the off. j. Am. Associat. Cancer Ed. Dec 2013;28(4):717–721. doi: 10.1007/s13187-013-0527-4. [DOI] [PubMed] [Google Scholar]
- 13.Carter L.M., Ogden G.R. Oral cancer awareness of undergraduate medical and dental students. BMC Med. Educ. Nov 15 2007;7:44. doi: 10.1186/1472-6920-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pokharel M., Shrestha I., Dhakal A., Amatya R.C. Awareness and knowledge of oral cancer among medical students in kathmandu university school of medical Sciences. Kathmandu Univ. Med. J. Jan.-Mar. 2017;15(57):75–77. [PubMed] [Google Scholar]
- 15.Reed S.G., Duffy N.G., Walters K.C., Day T.A. Journal of Cancer Education : the Official Journal of the American Association for Cancer Education. Fall. Vol. 20. 2005. Oral cancer knowledge and experience: a survey of South Carolina medical students in 2002; pp. 136–142. 3. [DOI] [PubMed] [Google Scholar]
- 16.Jayasinghe R.D., Sherminie L.P., Amarasinghe H., Sitheeque M.A. Level of awareness of oral cancer and oral potentially malignant disorders among medical and dental undergraduates. Ceylon Med. J. Jun 2016;61(2):77–79. doi: 10.4038/cmj.v61i2.8289. [DOI] [PubMed] [Google Scholar]
- 17.Abdulrahim S., Jawad M. Socioeconomic differences in smoking in Jordan, Lebanon, Syria, and Palestine: a cross-sectional analysis of national surveys. PLoS One. 2018;13(1) doi: 10.1371/journal.pone.0189829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herity B.A., Horgan J.M., Bourke G.J., Wilson-Davis K. Tobacco, alcohol and other drug use among medical students. Ir. Med. J. Nov 30 1977;70(18):532–539. [PubMed] [Google Scholar]
- 19.Gignon M., Havet E., Ammirati C., et al. Alcohol, cigarette, and illegal substance consumption among medical students: a cross-sectional survey. Workplace Health & Saf. Feb 2015;63(2):54–63. doi: 10.1177/2165079915570917. [DOI] [PubMed] [Google Scholar]
- 20.Petroianu A., Reis D.C., Cunha B.D., Souza D.M. Prevalence of alcohol, tobacco and psychotropic drug use among medical students at the Universidade Federal de Minas Gerais. Rev. Assoc. Méd. Bras. Sep-Oct 2010;56(5):568–571. doi: 10.1590/s0104-42302010000500019. 1992. [DOI] [PubMed] [Google Scholar]
- 21.McCready Z.R., Kanjirath P., Jham B.C. Oral cancer knowledge, behavior, and attitude among osteopathic medical students. J. Cancer Educ. : the off. j. Am. Associat. Cancer Ed. Jun 2015;30(2):231–236. doi: 10.1007/s13187-014-0675-1. [DOI] [PubMed] [Google Scholar]
- 22.Mohyuddin N., Langerman A., LeHew C., Kaste L., Pytynia K. Knowledge of head and neck cancer among medical students at 2 Chicago universities. Arch. Otolaryngol. Head Neck Surg. Dec 2008;134(12):1294–1298. doi: 10.1001/archotol.134.12.1294. [DOI] [PubMed] [Google Scholar]
- 23.Eldsoky I., Ismaiel W.F., Hasan A., Abdelazim M.H., Ibrahim A.A., Alsobky M.E., Mohammed A.R. The predictive value of nasolacrimal sac biopsy in endoscopic dacryocystorhinostomy. Ann. Med. Surg. 2021 May 1;65 doi: 10.1016/j.amsu.2021.102317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Dubai S.A., Ganasegeran K., Alabsi A.M., Alshagga M.A., Ali R.S. Awareness and knowledge of oral cancer among university students in Malaysia. Asian Pac. J. Cancer Prev. APJCP : Asian Pac. J. Cancer Prev. APJCP. 2012;13(1):165–168. doi: 10.7314/apjcp.2012.13.1.165. [DOI] [PubMed] [Google Scholar]
- 25.Canto M.T., Horowitz A.M., Drury T.F., Goodman H.S. Maryland family physicians' knowledge, opinions and practices about oral cancer. Oral Oncol. Jul 2002;38(5):416–424. doi: 10.1016/s1368-8375(01)00080-x. [DOI] [PubMed] [Google Scholar]
- 26.Awan K.H., Khang T.W., Yee T.K., Zain R.B. Assessing oral cancer knowledge and awareness among Malaysian dental and medical students. J. Cancer Res. Therapeut. Oct-Dec 2014;10(4):903–907. doi: 10.4103/0973-1482.138011. [DOI] [PubMed] [Google Scholar]
- 27.Prout M.N., Heeren T.C., Barber C.E., et al. Use of health services before diagnosis of head and neck cancer among Boston residents. Am. J. Prev. Med. Mar-Apr 1990;6(2):77–83. [PubMed] [Google Scholar]
- 28.Gunjal S., Pateel D.G.S., Lim R.Z.S., Yong L.L., Wong H.Z. Assessing oral cancer awareness among dental and medical students of a Malaysian private university. Int. Dent. J. Feb 2020;70(1):62–69. doi: 10.1111/idj.12524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewandowski B., Czenczek-Lewandowska E., Pakla P., et al. Awareness of Polish undergraduate and graduate students regarding the impact of viral infections and high-risk sexual behaviors on the occurrence of oral cancer. Medicine. Oct 2018;97(41) doi: 10.1097/md.0000000000012846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adjei Boakye E., Tobo B.B., Rojek R.P., Mohammed K.A., Geneus C.J., Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum. Vaccines Immunother. Nov 2 2017;13(11):2713–2722. doi: 10.1080/21645515.2017.1363133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu C.R., Liang H., Zhang X., et al. Effect of an educational intervention on HPV knowledge and attitudes towards HPV and its vaccines among junior middle school students in Chengdu, China. BMC Publ. Health. May 2 2019;19(1):488. doi: 10.1186/s12889-019-6823-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seme K., Maver P.J., Korać T., et al. Current status of human papillomavirus vaccination implementation in central and eastern Europe. Acta Dermatovenerol. Alpina Pannonica Adriatica. 2013;22(1):21–25. [PubMed] [Google Scholar]
- 33.Mesher D., Panwar K., Thomas S.L., et al. The impact of the national HPV vaccination program in england using the bivalent HPV vaccine: surveillance of type-specific HPV in young females, 2010-2016. J. Infect. Dis. Aug 14 2018;218(6):911–921. doi: 10.1093/infdis/jiy249. [DOI] [PubMed] [Google Scholar]
- 34.National vaccine program. Minist. Health, Syria. 2020 http://www.moh.gov.sy/Default.aspx?tabid=414&language=ar-YE Accessed January. [Google Scholar]
- 35.World Health Organization = Organisation mondiale. de la S. Weekly Epidemiological Record, 2017, vol. 92, 19 [full issue] Weekly Epidemiol. Record = Relevé épidémiol. hebdomad. 2017-05-12 2017;92(19):241–268. [Google Scholar]
- 36.oftegaard B.S., Bro F., Falborg A.Z., et al. Impact of continuing medical education in cancer diagnosis on GP knowledge, attitude and readiness to investigate - a before-after study. BMC Fam. Pract. 2016;17:95. doi: 10.1186/s12875-016-0496-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasan A., Nafie K., Abbadi O. Histopathology laboratory paperwork as a potential risk of COVID-19 transmission among laboratory personnel. Infect. Prevent. Pract. 2020 Dec 1;2(4) doi: 10.1016/j.infpip.2020.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mathew G., Agha R., for the STROCSS Group Strocss 2021: strengthening the Reporting of cohort, cross-sectional and case-control studies in Surgery. Int. J. Surg. 2021;96 doi: 10.1016/j.ijsu.2021.106165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data related to this paper's conclusion are available and stored by the authors. All data can be made available by the corresponding author upon a reasonable request.