Abstract
Background
Intersecting opioid overdose, COVID-19, and systemic racism epidemics have brought unprecedented challenges to the addiction treatment and recovery workforce. From 2017 to 2020, the New England Addiction Technology Transfer Center (ATTC) collected data in real-time on the training and technical assistance (TA) requested and attended by the front-line workforce. This article synthesizes practice-based evidence on the types of TA requests, topics of TA, attendance numbers, and socio-demographics of TA attendees over a 3-year period spanning an unprecedented public health syndemic.
Methods
We assessed TA events hosted by the New England ATTC using SAMHSA’s Performance Accountability and Reporting System post-event survey data from 2017 to 2020. Events were coded by common themes to identify the most frequently requested training types/topics and most frequently attended training events. We also evaluated change in training topics and attendee demographics over the three-year timeline.
Results
A total of 258 ATTC events reaching 10,143 participants were analyzed. The number of TA events and attendance numbers surged in the 2019–2020 fiscal year as TA events shifted to fully virtual during the COVID-19 pandemic. The absolute number of opioid-related events increased, but the relative proportion remained stable over time. The relative proportions of events and attendance rates focused on evidence-based practice and health equity both increased over the 3-year period, with the largest increase after the onset of the pandemic and the murder of George Floyd. As events shifted to virtual, events were attended by providers with a broader range of educational backgrounds.
Conclusions
Results of the current analysis indicate that the demand for TA increased during the pandemic, with a prioritization of TA focused on evidence-based practice and health equity. The practice-based evidence generated from the New England ATTC may help other training and TA centers to anticipate and nimbly respond to the needs of the workforce in the face of the intersecting epidemics.
Keywords: Practice-based evidence, Addiction, Technology transfer Center, Technical assistance
In recent years, the United States addiction treatment and recovery workforce has faced unprecedented and intersecting public health crises: the opioid overdose epidemic, the COVID-19 pandemic, and national reckoning with systemic racism. Opioid overdose deaths rose from 47,600 in 2017 [1] to 49,860 in 2019 [2], resulting in overdose fatalities outpacing deaths due to car accidents and violent crime [3]. The COVID-19 pandemic, declared a national emergency in March 2020, further exacerbated overdose risk and precipitated a spike in overdose deaths in 2020 [4]. Concurrently, the United States faced national reckoning of the pervasive issue of systemic and structural racism, as COVID-19 and barriers to essential harm reduction services disproportionally affected racial/ethnic minority communities [5].
Throughout this syndemic, federally-funded purveyors of training and technical assistance (TA) have been on the front-lines helping agencies and their workforce to adopt and implement evidence-based behavioral health practices. Of existing TA providers, the Addiction Technology Transfer Centers (ATTCs), established in 1993, represent the longest running and most widely studied behavioral health training and technical assistance (TA) initiative [6]. Funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), the ATTC network consists of 10 regional centers, tightly coordinated by a national office, that each serve as a multidisciplinary resource for those working in the addiction treatment and recovery service fields [7].
Each regional ATTC works with expert trainers to provide three different levels of TA that vary in their objectives and duration: basic, targeted, and intensive [8]. TA is defined as a tailored approach to providing implementation support to, and increasing capacity for, continuous quality improvement [9]. Training is considered a discrete activity that can be included as part of any TA effort, guided by extensive evidence that training is insufficient for practice implementation and organizational change [10]. Basic TA focuses on information dissemination to large, heterogenous audiences with the goal to build awareness and/or knowledge. Common examples of basic TA include publications, websites, newsletters, or single-event webinars. Targeted TA provides tailored support for specific populations or settings to foster skill development and readiness to implement specific evidence-based services. Common examples of targeted TA include online courses, communities of practice, or other short-term training series for a specific audience. Intensive TA provides ongoing, customized consultation specific to communities, organizations, or systems aimed to support full incorporation of a new practice in real-world settings. Examples of intensive TA activities include consultation from external intervention experts or ongoing intervention fidelity monitoring.. Each Regional ATTC offers TA based on principles of both “push” and “pull” demand. An ATTC may choose to “push” TA based on feedback from regional advisory boards or an annual needs assessment, or a specific addiction treatment or recovery support organization may “pull” TA by contacting the ATTC with a specific request. When an organization requests TA, decisions about which TA type to provide to a specific community agency are made collaboratively based on circumstances, need, and appropriateness [11].
The ATTC network has not only been at the forefront of providing TA in evidence-based practice, but has also been a leader in generating practice-based evidence by synthesizing data on TA provision and engagement in real-time [12]. Recent work pooling data from the ATTC network with other federally-funded TA purveyors indicated that there was an increase in the number and reach of TA events nationwide in the six-months following COVID-19 social distancing orders relative to the six-months prior [13]. In addition, there was a surge in requests for basic and targeted TA, as agencies sought access to rapid information [14]. These studies focused on general themes across disparate TA networks from 2019 to 2020, which limited detection of longer-term, addiction-specific trends.
The New England ATTC, one of the original ATTCs established in 1993, has been systematically tracking provision of and attendance at TA events since 2017. The New England ATTC serves a region (e.g., Rhode Island, Massachusetts, Connecticut, New Hampshire, Vermont, Maine) that has been at the epicenter of the opioid overdose epidemic [15, 16], and at the forefront of the national response to the COVID-19 pandemic [17]. As a result, the New England ATTC has generated vital practice-based evidence regarding the evolving needs of the addiction treatment and recovery support workforce in the six-state region.
This paper aims to advance knowledge on workforce training needs that emerged during the syndemic by examining the following New England ATTC metrics from 2017 to 2020: a) frequency of TA types delivered (basic, targeted, or intensive); b) most frequently delivered and highly attended TA topics; and c) shifts in TA requests over time. Based on national trends, we anticipated that there would be an increase in TA requests from 2017 to 2020, driven by an increase in requests for basic and targeted TA. We also expected to document a rise in requests for TA on opioid-related topics and on health equity, particularly during 2019–2020 fiscal year following the murder of George Floyd [18] and during the spike in overdose deaths [4]. By generating practice-based evidence, this study may help purveyors of TA to nimbly adapt and better anticipate the types of support that are the most beneficial and timely for the workforce in times of crisis.
Methods
Data extraction
Event attendance and attendee socio-demographic data were extracted from SAMHSA’s Performance Accountability and Reporting System (SPARS) over three fiscal years (October 2017 to September 2020): attendance data were extracted from Event Description Forms and socio-demographic data were extracted from the Government Performance and Results Act (GPRA) post-event forms. GPRA post-event forms were administered to all event attendees, but framed as optional. TA titles and descriptions were drawn from the New England ATTC’s FileMaker® tracking system. Events in the FileMaker® system that were excluded from the final dataset included activities that were not classified as TA (i.e., meetings) or not formally organized by the New England ATTC (i.e., events coordinated by other ATTCs or TA purveyors). Data were collected by the New England ATTC as part of ongoing quality assurance procedures. Attendees provided electronic informed consent for their GPRA data to be used in this manner. All data were fully anonymized and training attendees were identified by a four-digit number; as a result, it was not feasible to determine if participants attended more than one TA event. This retrospective analysis was submitted to the Brown University Institutional Review Board: the board determined that this analysis was not human subjects research that required review. The study was conducted in accordance with relevant national and institutional guidelines.
Event coding
The topics and types of TA events were qualitatively coded using a reflexive, team-based content analysis approach [19] involving three members of the New England ATTC team. The coding team prioritized reflexivity in the analysis process to increase awareness of biases due to their active involvement in ATTC TA delivery. As a first step, the coding team reviewed the list of TA event titles in its entirety. The team then generated a preliminary list of event topics and an initial set of topic definitions in a coding dictionary.
Two rounds of coding were completed to assign topic and type codes to the TA activities. In the first round, a primary coder (MS) independently coded all event topics. A second coder (KS) independently double coded 20% of all events. A third coder (SB) was consulted as needed throughout the coding process to add emergent topics and definitions to the coding dictionary. Once independent coding was completed, the three coders met to identify discrepant codes, to make final consensus coding determinations, and to organize codes into broader TA topics.
The final list of TA topics used for coding included: Evidence-Based Practices (EBPs), Provider Self Care, Leadership Development, Health Equity, Stigma, and Consumer Needs. Topics were mutually exclusive such that each TA event was assigned only one topic code. Table 1 presents definitions of each topic. The coders also indicated whether each event was opioid-, justice-, or COVID-related. TA events could be assigned more than one of these three supplementary codes (i.e. coded as both opioid and justice related). Events that were not coded as opioid-, justice-, or COVID-related only received the broad TA topic codes (e.g. EBPs, Consumer Needs). Following completion of the first round of coding focused on topics, a second round was conducted to classify TA type for each event (i.e. basic, targeted, or intensive TA). Coding continued until the team obtained 100% consensus.
Table 1.
Definitions of Technical Assistance (TA) topics
| Topic | Definition |
|---|---|
| EBPs | TA activities focused on substance use interventions supported by research, including medications for opioid use disorder, motivational interviewing, contingency management, and trauma-informed care |
| Provider Self-Care | TA events focused on compassion fatigue, burnout, and self-care practices for providers caring for clients with substance use disorders |
| Leadership Development | TA events focused on training in both clinical supervision and leadership skills |
| Health Equity and Disparities | TA activities focused on topics including cultural humility and providing culturally and linguistically appropriate treatment services |
| Stigma | TA events focused on providing education about and reducing the stigma associated with substance use disorders |
| Consumer Needs | TA events related to building general knowledge of substance use/substance use treatment such as the etiology and epidemiology of addiction |
Data analysis
Data extracted from SPARS and FileMaker® were integrated into a single dataset and analyzed using SPSS software [20]. Descriptive statistics were run to identify the most frequent TA topic and type codes and the most frequently attended topics across the three-year period. Changes in TA topics and attendance across years were evaluated using Chi-squared analyses with Cramer’s V used to indicate the effect size. Consistent with well-established standards [21, 22], Cramer’s V values were interpreted as: < .10: little or no effect.,10–.19: small effect,.20–.29: moderate effect, and > .30: strong effect.
Results
A total of 10,695 participants attended 345 New England ATTC TA events over the three-year period, of which 258 events (75%) were retained for this analysis. Eighty-seven events with a total of 552 attendees were excluded because they were classified as meetings or as coordinated by other ATTCs. The final analytic sample for total attendance included 10,143 attendees (95% of participants). Demographic information was available from 6642 attendees (66% of the analytical sample) who completed GPRA post event forms.
Participant demographics
Table 2 presents socio-demographic data. Of the TA attendees with available data, respondents predominantly identified as female (69.7%), and White (72.6%) with the next largest identification categories being Black (7.7%), Multi-Race (5.5%), and Hispanic (5.5%). Nearly half of participants held a Bachelor’s Degree or lower (47.3%), with the other half holding a Master’s Degree or higher (52.7%%). Attendees represented over 30 professions, with the majority identifying as behavioral health or substance use treatment providers (50.6%).
Table 2.
Sociodemographic information for participants who completed post-event forms over a 3-year period (N = 6642)
| Demographic Variable | Year 1 10/2017–9/2018 N(%) |
Year 2 10/2018–9/2019 N(%) |
Year 3 10/2019–9/2020 N(%) |
Total 10/2017–9/2020 N(%) |
Change Across Years (X2) | Cramer’s V |
|---|---|---|---|---|---|---|
| Gender | 45.9*** | 0.06 | ||||
| Male | 737 (26.8%) | 459 (25.0%) | 449 (21.8%) | 1645 (24.8%) | ||
| Female | 1850 (67.3%) | 1235 (67.3%) | 1544 (75.1%) | 4629 (69.7%) | ||
| Transgender | 4 (0.1%) | 3 (0.2%) | 9 (0.4%) | 16 (0.2%) | ||
| None of these | 0 (0%) | 1 (0.1%) | 11 (0.5%) | 12 (0.2%) | ||
| Missing | 158 (5.7%) | 138 (7.5%) | 44 (2.1%) | 340 (5.1%) | ||
| Race | 74.7*** | 0.08 | ||||
| American Indian/Alaska Native | 17 (0.6%) | 4 (0.2%) | 15 (0.7%) | 36 (0.5%) | ||
| Asian | 32 (1.2%) | 46 (2.5%) | 46 (2.2%) | 124 (1.9%) | ||
| Black | 191 (6.9%) | 170 (9.3%) | 152 (7.4%) | 513 (7.7%) | ||
| Native Hawaiian/Pacific Islander | 9 (0.3%) | 2 (0.1%) | 8 (0.4%) | 19 (0.3%) | ||
| White | 2027 (73.7%) | 1239 (67.5%) | 1555 (75.6%) | 4821 (72.6%) | ||
| Hispanic | 127 (4.6%) | 98 (5.3%) | 140 (6.8%) | 365 (5.5%) | ||
| Mixed Race | 159 (5.8%) | 137 (7.5%) | 72 (3.5%) | 368 (5.5%) | ||
| Missing | 187 (6.8%) | 140 (7.6%) | 69 (3.4%) | 396 (6.0%) | ||
| Education | 94.0*** | 0.09 | ||||
| Less than high school | 10 (0.4%) | 5 (0.3%) | 3 (0.1%) | 18 (0.3%) | ||
| High school diploma, GED, Some College | 341 (12.4%) | 183 (10.0%) | 322 (15.7%) | 846 (12.7%) | ||
| Associate’s degree | 196 (7.1%) | 109 (5.9%) | 109 (5.3%) | 414 (6.2%) | ||
| Bachelor’s degree | 691 (25.1%) | 420 (22.9%) | 617 (30.0%) | 1728 (26.0%) | ||
| Master’s degree | 1163 (42.3%) | 795 (43.3%) | 823 (40.0%) | 2781 (41.9%) | ||
| Doctoral Degree | 186 (6.8%) | 174 (9.5%) | 91 (4.4%) | 451 (6.8%) | ||
| Other | 39 (1.4%) | 33 (1.8%) | 41 (2.0%) | 113 (1.7%) | ||
| Missing | 123 (4.5%) | 117 (6.4%) | 51 (2.5%) | 291 (4.4%) | ||
| Profession | 658.6*** | 0.23 | ||||
| Behavioral Health/Substance Use Treatment Provider (e.g. Counselor, Addictions Professional) | 1514 (55.1%) | 933 (50.8%) | 916 (44.5%) | 3363 (50.6%) | ||
| Medical Treatment Provider (e.g. Physician, Psychiatrist, Nurse) | 299 (10.9%) | 337 (18.4%) | 168 (8.2%) | 804 (12.1%) | ||
| Peer/Community Support Provider (e.g. Recovery Specialist, Community Health Worker) | 153 (5.6%) | 88 (4.8%) | 187 (9.1%) | 428 (6.4%) | ||
| Education (e.g. Health Educator, Researcher) | 62 (2.3%) | 35 (1.9%) | 82 (4.0%) | 179 (2.7%) | ||
| Student | 0 (0%) | 16 (0.9%) | 245 (11.9%) | 261 (3.9%) | ||
| Law Enforcement Professional (e.g. Parole Officer, Prison Staff) | 97 (3.5%) | 61 (3.3%) | 67 (3.3%) | 225 (3.4%) | ||
| Business Administrator | 35 (1.3%) | 28 (1.5%) | 37 (1.8%) | 100 (1.5%) | ||
| Other | 378 (13.8%) | 184 (10.0%) | 261 (12.7%) | 823 (12.4%) | ||
| Missing | 211 (7.7%) | 154 (8.4%) | 94 (4.6%) | 459 (6.9%) |
*p < 0.05
**p < 0.01
***p < 0.001
Over the three-year period, the socio-demographics of the workforce attending TA events shifted with regard to gender, race/ethnicity, participant training/education background, and participant primary profession. Analyses revealed shifts in the attendee composition in terms of gender, race/ethnicity, and training background that were significant but in the trivial range (Cramer’s V < .10), whereas the shift in primary profession was moderate (Cramer’s V = .23). Attendees’ primary professions diversified across the three-year period, with greater representation among peer community support providers, education professionals, and students.
Training participants/regions
Of the 258 TA events analyzed, 69 % of TA events were face-to-face and the remainder were virtual. Over the first 2 years, the New England ATTC provided TA both in-person (68.5% of events) and virtually (31.5% of events). Midway through the third year (March 2020), all TA was transitioned to fully virtual due to the COVID-19 pandemic.
Table 3 presents TA event counts by state and by type. TA occurred across all six New England states, with the majority of trainings offered to the full New England region (31.4%), followed by New Hampshire (16.7%) and Connecticut (14.3%). Notably, regional coverage was fairly stable, with no significant association between fiscal year and TA by state.
Table 3.
Coverage and type of Technical Assistance (TA) events over 3-year period
| Category | Year 1 10/2017–9/2018 N(%) |
Year 2 10/2018–9/2019 N(%) |
Year 3 10/2019–9/2020 N(%) |
Total 10/2017–9/2020 N(%) |
Change Across Years (X2/% Change) | Cramer’s V |
|---|---|---|---|---|---|---|
| Regional Coverage | 16.2 n.s. | 0.18 | ||||
| Regional | 39 (38.6%) | 14 (20.9%) | 28 (31.1%) | 81 (31.4%) | ||
| New Hampshire | 16 (15.8%) | 10 (14.9%) | 17 (18.9%) | 43 (16.7%) | ||
| Connecticut | 13 (12.9%) | 15 (22.4%) | 9 (10.0%) | 37 (14.3%) | ||
| Rhode Island | 12 (11.9%) | 9 (13.4%) | 15 (16.7%) | 36 (14.0%) | ||
| Massachusetts | 12 (11.9%) | 9 (13.4%) | 8 (8.9%) | 29 (11.2%) | ||
| Maine | 7 (6.9%) | 6 (9.0%) | 11 (12.2%) | 24 (9.3%) | ||
| Vermont | 2 (2.0%) | 4 (6.0%) | 2 (2.2%) | 8 (3.1%) | ||
| Type of TA | 21.0*** | 0.20 | ||||
| Basic TA | 3 (3.0%) | 3 (4.5%) | 7 (7.8%) | 13 (5.0%) | + 4.8% | |
| Targeted TA | 91 (90.1%) | 50 (74.6%) | 56 (62.2%) | 197 (76.4%) | −27.9% | |
| Intensive TA | 7 (6.9%) | 14 (20.9%) | 27 (30.0%) | 48 (18.6%) | + 23.1% |
n.s. not significant
***p < .001
Frequency of TA types offered
Of the 258 events analyzed, most were categorized as targeted TA (76.4%). Intensive (18.6%) and basic TA (5.0%) were offered far less frequently. Over the three-year period, the total number of events decreased by about 10% and the TA types shifted. The proportion of events classified as targeted TA decreased by 28%, whereas the proportion classified as intensive TA increased by 23%. Chi squared analyses revealed significant differences in TA types across the fiscal years, and these changes were moderate in size (Cramer’s V = 0.20; see Table 3).
Most frequently offered and attended training topics
Across all 3 years, the most frequently requested TA topics and the most heavily attended included EBPs (41.5% of events, 30.9% of attendees; see Table 4), Consumer Needs (27.5% of events, 34.8% of attendees), and Health Equity (14.0% of events, 20.6% of attendees). EBPs, Health Equity, and Consumer Needs were most frequently requested as targeted TA (72.0, 77.8, and 81.7% were targeted TA, respectively), though EBP events were also often requested as intensive TA (27.1% intensive). Across TA categories, 21.3% of events were classified as opioid-related, 13.6% were classified as justice related, and 2.3% were classified as COVID-related.
Table 4.
Frequency of and attendance at Technical Assistance (TA) events by topic
| Topic | Year 1 10/2017–9/2018 N(%) |
Year 2 10/2018–9/2019 N(%) |
Year 3 10/2019–9/2020 N(%) |
Total 10/2017–9/2020 N(%) |
Change Across Years (X2/% Change) | Cramer’s V |
|---|---|---|---|---|---|---|
| Frequency of Events | 24.0** | 0.22 | ||||
| EBP | 33 (32.7%) | 29 (43.3%) | 45 (50.0%) | 107 (41.5%) | + 17.3% | |
| Consumer Needs | 33 (32.7%) | 19 (28.4%) | 19 (21.1%) | 71 (27.5%) | −11.6% | |
| Health Equity and Disparities | 10 (9.9%) | 7 (10.4%) | 19 (21.1%) | 36 (14.0%) | + 11.2% | |
| Leadership Development | 9 (8.9%) | 7 (10.4%) | 2 (2.2%) | 18 (7.0%) | −6.7% | |
| Provider Self Care | 6 (5.9%) | 0 (0%) | 1 (1.1%) | 7 (2.7%) | −4.8% | |
| Stigma | 10 (9.9%) | 5 (7.5%) | 4 (4.4%) | 19 (7.4%) | −5.5% | |
| Attendance at Events | # Attendees | # Attendees | # Attendees | |||
| EBP | 841 (27.0%) | 857 (37.2%) | 1440 (30.5%) | 3138 (30.9%) | + 3.5% | |
| Consumer Needs | 1156 (37.1%) | 782 (33.9%) | 1596 (33.8%) | 3534 (34.8%) | −3.3% | |
| Health Equity and Disparities | 383 (12.3%) | 435 (18.9%) | 1268 (26.9%) | 2086 (20.6%) | + 14.6% | |
| Leadership Development | 164 (5.3%) | 145 (6.3%) | 32 (0.7%) | 341 (3.4%) | −4.6% | |
| Provider Self Care | 189 (6.1%) | 0 (0%) | 121 (2.6%) | 310 (3.1%) | −3.5% | |
| Stigma | 386 (12.4%) | 85 (3.7%) | 263 (5.6%) | 734 (7.2%) | −6.8% |
**p < 0.01
Within the three most requested event categories, further patterns emerged. Of the EBP events, the most popular interventions were medication for opioid use disorder (29.9%) and motivational interviewing (29.0%). Within the Consumer Needs events, about two-thirds (69.0%) provided general substance use education, with topics such as diagnosing substance use disorders, recognizing co-occurring mental health disorders, and applying general clinical skills (e.g. group counseling delivery). Finally, more than half (52.8%) of the Health Equity events involved training in effectively working with specific underserved populations (e.g. sexual and gender minorities, Hispanic and Latino populations). Other popular Health Equity topics included cultural humility (33.3%) and use of the Culturally and Linguistically Appropriate Services (CLAS) standards (13.9%).
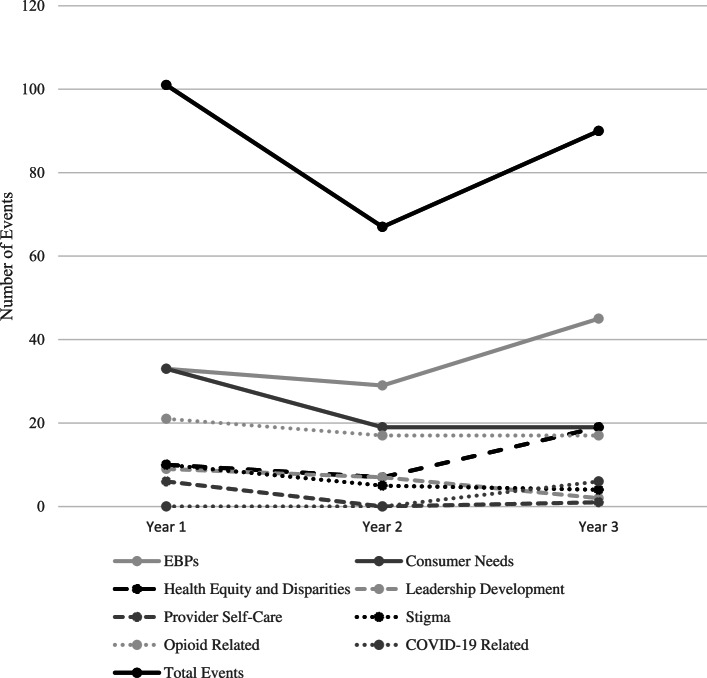
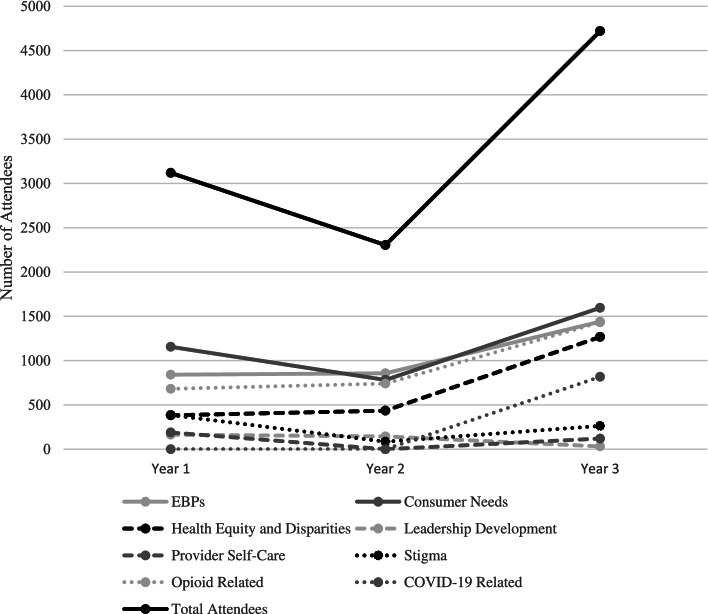
As shown in Figs. 1 and 2, the total number of events declined substantially from Year 1 to Year 2 and then rebounded somewhat in Year 3 (to 90% of the Year 1 level). The number of attendees similarly declined from Year 1 to Year 2, but then jumped up substantially in Year 3 (to 150% of the Year 1 level) as events shifted to virtual delivery during the COVID-19 pandemic.
Fig. 1.
New England ATTC events by topic over a 3-year period
Fig. 2.
Total attendees at New England ATTC training topics across 3 years
Analyses of the relative proportions of events in each year revealed moderate increases in the EBP and Health Equity categories. By contrast, there were decreases in the proportion of events in all other topics (Cramer’s V = 0.22). Similar trends were found in the proportion of attendees; EBP and Health Equity events had increased attendance (3.5 and 14.6% increases, respectively), while all other topics had decreased attendance (see Table 4).
Discussion
The current study provides practice-based evidence from one of the longest operating TA purveyors in the behavioral health field during an unprecedented constellation of public health crises. We detected a significant increase in the number of TA attendees from the first (2017–2018) to final (2019–2020) year, with a marked jump during the pandemic as events were offered fully virtually. We also observed an increase in the number of TA events between the second and final years, though the number of events was highest overall in year one. The increase in the number of attendees corresponded with a broadening of event reach to providers from diverse educational backgrounds, which may also indicate that a wider range of provider types are engaged in substance use and recovery-focused care. The absolute number of events coded as opioid-related also increased, although the proportion of events with this code remained relatively stable over time. The stability of opioid-related requests may have reflected the creation of the Opioid Response Network, a national network of SAMHSA-funded centers specifically focused on opioid-related technical assistance, in February 2018 [23]. Finally, there was an increase (both in terms of absolute numbers and relative proportions) in the number and attendance of events focused on health equity, which corresponded with a period of heightened consciousness around systemic racism. These findings were consistent with analyses of data from multiple TA purveyors in which the overall number and reach of events surged after the announcement of social distancing orders, with health equity events having the highest attendance in the months immediately following the murder of George Floyd [14].
Surprisingly, the increase in TA events was associated with an increase in intensive TA and an accompanying decrease in targeted TA events. This finding directly contradicts the results of the national study [14] of over 40 TA purveyors, which found that provision of basic and targeted TA surged after social distancing orders, and that intensive TA only accounted for 5% of all events. The New England ATTC’s ability to increase intensive TA offerings while other TA purveyors were providing predominantly basic or targeted support is noteworthy, especially given prior research indicating that long-term, ongoing TA is associated with better outcomes than one-shot, time-limited efforts [9]. Furthermore, research on high quality TA provision has suggested that intensive TA should provide frequent, ongoing opportunities for experiential learning [24, 25]. According to the Consolidated Framework for Implementation Research [26], the ability of organizations such as the New England ATTC to provide intensive TA is likely driven by multiple factors including the characteristics of individuals requesting the TA, the characteristics of the interventions for which TA was requested, and the inner setting of the organizations requesting the TA. In the current data, the increase in intensive TA corresponded with an increase in TA generally focused on evidence-based practices, as a means of helping organizations to implement specific interventions into their routine clinical care. More specifically, intensive TA provision was often focused specifically on motivational interviewing, which requires substantial training and supervision to use with fidelity. It is possible that the nature of requests made to the New England ATTC for TA on evidence-based practices in general and on motivational interviewing in particular, contributed to the larger proportion of TA that was intensive in nature.
The New England ATTC is also one of the only federally-funded TA purveyors with a well-established and empirically supported multi-level TA strategy. Since 2008, the New England ATTC has used the Science to Service Laboratory, which combines didactic training, performance feedback, and external facilitation. Didactic training typically consists of single or multi-session workshops focused on intervention knowledge and skill gain, while performance feedback and external facilitation prioritize monitoring of fidelity to the new intervention and provision of ongoing support for sustained use, respectively. The Science to Service Laboratory has been shown to be significantly more effective in promoting the adoption of evidence-based practice than training as usual [27–29]. Having an established TA strategy likely facilitated the steady provision of intensive TA throughout the pandemic, and may be particularly helpful for purveyors seeking to enhance TA quality and effectiveness.
The practice-based evidence generated in this report provides important insights regarding the workforce’s changing needs. Data of this type can be employed to guide TA purveyor decisions about the type of TA to prioritize/make available (e.g. providing more Intensive TA), the most appropriate delivery format to meet TA goals (e.g. online to enhance reach, in-person to promote engagement, or a hybrid approach), the in-demand evidence-based interventions that should be included in the purveyor’s repertoire, optimal trainers to hire based on education and areas of expertise (e.g. motivational interviewing), and the need to tailor TA to fit changing attendee characteristics (e.g. existing expertise, education/degrees). However, the ATTC’s practice-based evidence is limited by the reliance on event-level data, which only reveals whether TA was provided and not whether it was effective. The event level data for the ATTC is also fully de-identified, which means that some training participants may have attended more than one training event. In addition, as is true of all secondary data analysis, the quality of data analyzed is only as strong as the data entered. It is possible that some TA events were not recorded or were tracked inaccurately in the New England ATTC FileMaker system. Finally, the reliance on event titles and descriptions to discern specific TA topics might not have fully captured the focus of events.
Conclusions
Overall, the practice-based evidence generated herein indicates that a regional federally funded TA center experienced a surge in TA attendees during the COVID-pandemic, driven by attendance at events focused on evidence-based practice and health equity as well as TA activities that were intensive in nature. Findings from this analysis can help purveyors of TA to anticipate workforce development needs during the ongoing COVID-19 pandemic and future national crises. Future work should examine factors that predict TA purveyors’ ability to provide effective intensive TA.
Acknowledgements
Not applicable.
Abbreviations
- ATTC
Addiction Technology Transfer Center
- TA
Technical assistance
Authors’ contributions
SB, MS, and KS conceptualized and developed this study, completed all data analysis, and composed and reviewed the full manuscript. DB, RS, and RM reviewed and edited the full manuscript. All authors approved the full manuscript for submission.
Funding
This project was funded by grant UR1TI080209 (PI: Sara Becker) from the Substance Abuse and Mental Health Services Administration, United States Department of Health and Human Services. The effort of Dr. Kelli Scott was supported by grant K23DA050729 funded through the National Institute on Drug Abuse. The views and opinions contained within this document do not necessarily reflect those of the US Department of Health and Human Services or the National Institute on Drug Abuse, and should not be construed as such. Neither of these funding sources had involvement in the study design, data collection, analysis and interpretation, the writing of this report, or the decision to submit this article for publication.
Availability of data and materials
De-identified data regarding training and technical assistance types and topics are available upon request from the manuscript corresponding author.
Declarations
Ethics approval and consent to participate
Data were collected by the New England ATTC as part of ongoing quality assurance procedures. All training attendees were invited to complete the optional GPRA form to share demographic information and feedback on their training satisfaction. Prior to completing the optional form, attendees provided electronic informed consent for their data to be used in this manner. Training attendees were identified by a four-digit number and no potentially identifiable information (name, date of birth, address, etc.) were collected; thus, data were fully anonymized. This retrospective analysis was submitted to the Brown University Institutional Review Board: the board determined that this analysis was not human subjects research that required review. The study was conducted in accordance with relevant national and institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors have no competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;67 Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm675152e1.htm. [DOI] [PMC free article] [PubMed]
- 2.Centers for Disease Control and Prevention . Drug overdose deaths. 2021. [Google Scholar]
- 3.Faust JS, Du C, Mayes KD, Li S-X, Lin Z, Barnett ML, et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides During the pandemic, March-August 2020. JAMA. 2021;326(1):84–86. doi: 10.1001/jama.2021.8012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexander GC, Stoller KB, Haffajee RL, Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann Intern Med. 2020;173(1):M20–1141. [DOI] [PMC free article] [PubMed]
- 5.Centers for Disease Control and Prevention . Health Equity Considerations and Racial and Ethnic Minority Groups. 2020. [Google Scholar]
- 6.McCance-Katz EF. SAMHSA: creating a system of care that meets the Needs of people with mental and substance use disorders. Psychiatr Serv. 2020;71(5):416–418. doi: 10.1176/appi.ps.202000075. [DOI] [PubMed] [Google Scholar]
- 7.Addiction Technology Transfer Center Network . About the ATTC Network. 2021. [Google Scholar]
- 8.Cross-technology Transfer Center (TTC) Workgroup on Virtual Learning Virtual reality for Behavioral health Workforce Development in the era of COVID-19. J Subst Abus Treat. 2021;121:108157. doi: 10.1016/j.jsat.2020.108157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olson JR, Coldiron JS, Parigoris RM, Zabel MD, Matarese M, Bruns EJ. Developing an evidence-based Technical Assistance model: a process evaluation of the National Training and Technical Assistance Center for Child, youth, and family mental health. J Behav Health Serv Res. 2020;47(3):312–330. doi: 10.1007/s11414-020-09686-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edmunds JM, Beidas RS, Kendall PC. Dissemination and implementation of evidence-based practices: training and consultation as implementation strategies. Clin Psychol Publ Div Clin Psychol Am Psychol Assoc. 2013;20(2):152–165. doi: 10.1111/cpsp.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci. 2015;10(1):21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ammerman A, Smith TW, Calancie L. Practice-based evidence in public health: improving reach, relevance, and results. Annu Rev Public Health. 2014;35(1):47–63. doi: 10.1146/annurev-publhealth-032013-182458. [DOI] [PubMed] [Google Scholar]
- 13.Cross TTC Workgroup on Virtual Learning . Virtual training and technical assistance: a Profile of Behavioral Health Workforce Attendance, Geographic Location, and Perceptions Before and During Emergency Restrictions. 2021. pp. 14–16. [Google Scholar]
- 14.Cross-Technology Transfer Center (TTC) Workgroup on Virtual Learning, Molfenter T. Providing Behavioral Workforce Development Technical Assistance During COVID-19: Adjustments and Needs. Transl Behav Med. 2021:ibab097. 10.1093/tbm/ibab097. [DOI] [PMC free article] [PubMed]
- 15.National Institute on Drug Abuse . Opioid Summaries by State. 2020. [Google Scholar]
- 16.Stopka TJ, Jacque E, Kelso P, Guhn-Knight H, Nolte K, Hoskinson R, et al. The opioid epidemic in rural northern New England: an approach to epidemiologic, policy, and legal surveillance. Prev Med. 2019;128:105740. doi: 10.1016/j.ypmed.2019.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention . COVID-19 Vaccinations in the United States. 2020. [PubMed] [Google Scholar]
- 18.Dreyer BP, Trent M, Anderson AT, Askew GL, Boyd R, Coker TR, et al. The death of George Floyd: bending the arc of history toward justice for generations of children. Pediatrics. 2020;146(3):e2020009639. doi: 10.1542/peds.2020-009639. [DOI] [PubMed] [Google Scholar]
- 19.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 20.IBM Corp . IBM SPSS statistics for windows, version 26.0. Armonk: IBM Corp; 2019. [Google Scholar]
- 21.Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med. 2018;18(3):91–93. doi: 10.1016/j.tjem.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Acock AC, Stavig GR. A measure of association for nonparametric statistics. Social Forces. 1979;57(4):1381–1386. doi: 10.2307/2577276. [DOI] [Google Scholar]
- 23.Alonso J. State targeted response Technical Assistance (STR-TA) consortium. Safe States Alliance; 2018. [Google Scholar]
- 24.Wandersman A, Chien VH, Katz J. Toward an evidence-based system for innovation support for implementing innovations with quality: tools, training, Technical Assistance, and quality assurance/quality improvement. Am J Community Psychol. 2012;50(3–4):445–459. doi: 10.1007/s10464-012-9509-7. [DOI] [PubMed] [Google Scholar]
- 25.Fixsen DL, Blase KA, Horner R, Sugai G. Intensive Techncial Assistance. Scaling up brief #2. Chapel Hill: the University of North Carolina at Chapel Hill, FPG Child Development Institute; 2009. [Google Scholar]
- 26.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Squires DD, Gumbley SJ, Storti SA. Training substance abuse treatment organizations to adopt evidence-based practices: the addiction technology transfer Center of new England Science to service laboratory. J Subst Abus Treat. 2008;34(3):293–301. doi: 10.1016/j.jsat.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Becker SJ, Squires DD, Strong DR, Barnett NP, Monti PM, Petry NM. Training opioid addiction treatment providers to adopt contingency management: a prospective pilot trial of a comprehensive implementation science approach. Subst Abus. 2016;37(1):134–140. doi: 10.1080/08897077.2015.1129524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Helseth SA, Janssen T, Scott K, Squires DD, Becker SJ. Training community-based treatment providers to implement contingency management for opioid addiction: time to and frequency of adoption. J Subst Abus Treat. 2018;95:26–34. doi: 10.1016/j.jsat.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data regarding training and technical assistance types and topics are available upon request from the manuscript corresponding author.