Abstract
Background and Purpose
In 2021, lung cancer in school food workers was first recognized as an occupational cancer. The classification of the carcinogenicity of cooking fumes by International Agency for Research on Cancer (IARC) was based on Chinese epidemiological data. This study aimed to determine the hazard levels of school cooking fumes in Korea.
Materials and Methods
Based on public school cafeterias in one area, 25 locations were selected for the survey according to the number per school type, ventilation states, and environmental pre-assessments of cafeterias. Two inside cooking areas using a heat source and one outside cooking area were selected as control measurement points. Measurements of CO, CO2, polycyclic aromatic hydrocarbons (PAHs), and total volatile organic compounds (TVOCs), including benzene, formaldehyde, and particulate matter (PM10, PM2.5, PM1, respectively), were taken. The concentrations and patterns of each substance in the kitchens were compared with the outdoor air quality.
Result
Known carcinogens, such as the concentrations of PAHs, formaldehyde, TVOC (benzene), and particulate matter in school cooking fumes, were all detected at similar or slightly higher levels than those found outside. Additionally, substances were detected at relatively low concentrations compared to the Chinese cooking fumes reported in the literature. However, the short-term exposure to high concentrations of CO (or composite exposure with CO2) and PM2.5 in this study were shown.
Conclusion
The school cooking fumes in South Korea was a relatively less harmful than Chinese cooking fumes, however short-term, high exposure of toxic substances can cause a critical health effect.
Keywords: CO, CO2, PM2.5, School cooking fumes, Short-term high exposure
1. Introduction
As of 2019, the number of school cooks in Republic of Korea was approximately 71,000 [1]. The Republic of Korea Occupational Safety and Health Agency (KOSHA) operated a surveillance system for acute poisoning in Incheon and the Gyeonggi Province (2017–2018), in which school cooks reported two cases of acute CO poisoning in 2017 and 10 cases in 2018 [2,3]. Since 2017, the possibility of cooks developing respiratory cancer owing to harmful substances generated during cooking in school cafeterias has been continually increasing and covered in the media. In February 2021, lung cancer in school cooks was first recognized as an occupational cancer in Republic of Korea [4]. Most International Agency for Research on Cancer (IARC) epidemiological data regarding carcinogenicity 2A classification in cooking fumes include exposure and health effects found in Chinese cooking environments (e.g., China, Taiwan, Singapore, and Hong Kong) [5]. Recently, attempts have been made to establish the dose-response relationship of cooking fumes and lung cancer by using the frequency of cooking methods as a proxy indicator of cooking fumes [6]. In addition, in most studies reviewed here, few with quantitative study data simultaneously evaluated the amount of CO from the cooking process (e.g., heat source CO) [5].
Cooking fumes contain more than 200 types of gases and other various compounds, such as polycyclic aromatic hydrocarbons (PAHs) and aldehyde-based chemicals [7]. The main carcinogens and harmful gases generated in cooking environments include PAHs, formaldehyde, total volatile organic compounds (TVOC), fine particles (PM2.5, PM10), CO, and CO2. Simultaneous exposure to CO and CO2 exacerbates hypoxia by increasing the body's acidity, slowing the recovery time (compared with exposure to a single gas), and increasing the binding rate of carboxyhemoglobin (compared with exposure to CO alone) [[8], [9], [10]]. For this reason, it should be noted that combined exposure of CO and CO2 increases the hypoxic toxicity of cooking fumes.
In addition, particle size is directly related to the likelihood of health problems. Small particles, < 10 μm in diameter, can penetrate deep into the lungs. Some can even enter the bloodstream, affecting the lungs and heart [11]. Studies involving the short-term exposure effects of PM2.5 have shown substantial evidence that small particles are linked to health problems such as ischemic stroke and mortality [12,13] and that low levels of PM2.5 have harmful health effects [14]. A recently published study also demonstrated that short-term exposure to PM10 and PM2.5 is independently associated with cardiovascular, and respiratory mortality in more than 600 cities worldwide [15]. Recent studies have reported that an annual average concentration <10 has an effect of increasing mortality [15,16]. The harmfulness of cooking fumes is greatly reduced by ventilation [17], likely owing to the reduction of ventilation-effective substances such as fine particles [[18], [19], [20]] and gases (e.g., CO and CO2).
The primary source of particles mainly includes solid fuels (e.g., coal and wood), biomass, and specific recipes such as high-temperature frying [5]. In a study investigating the concentration of PAHs according to cooking method differences used in various countries, frying (fry in Malaysian kitchens or stir-fry in Chinese kitchens) produced higher molecular weight PAHs, such as benzo[b]fluoranthene (BBF), whereas concentrations of low molecular weight PAHs were higher in Indian kitchens where low-temperature cooking (e.g., boiling) was used [21]. Korean cooking methods do not include much high-temperature fried cooking seen in Chinese methods, and most of the fuel sources at group meal venues have been replaced by gas or electricity. Therefore, the detrimental health effects of Korean kitchens have changed, and the current effects cannot be demonstrated in past literature. Furthermore, school cooking fumes differ from fumes in homes and restaurants, as school cooking fumes occur from a large amount of cooking in a short time. This cooking style can increase the deleterious effects of cooking fumes; however, few studies have confirmed this finding. Therefore, the purpose of this study is to provide basic data on health effects through the quantitative evaluation of the characteristics and exposure patterns of cooking gases generated in Korean school cooking environments.
2. Materials and methods
2.1. Selection of survey targets
In 2019, the total number of schools in Republic of Korea was 11,662. The cafeterias operated at 100% capacity. Most cafeterias were directly managed by schools (Ministry of Education, 2019). School cafeterias are mostly structurally similar as they are installed and operated according to the plans and guidelines of the Ministry of Education. The pre-check list was distributed to all public-school field managers (mainly nutritionists) in a metropolitan city located on the southeastern coast of Republic of Korea and was used to select field survey targets. The pre-inspection table includes the number of meals per worker, work classification, cafeteria structure, area, ventilation method, ventilation state, heat source, and work type. Ventilation states were classified into “good,” “moderate,” and “bad.” If the ventilation condition was checked as “bad,” the reason was listed in Table 1. Twenty-five locations were selected based on the preliminary inspection results. Characteristics such as school level, ventilation state, method, and internal structure were considered to select the survey target, and poorly ventilated cafeterias were primarily selected through discussions with researchers and field managers (Table 2). The reasons for poor ventilation included lack of windows, poor location, external pollutants adjacent to the open place of the cafeteria (e.g., evacuation of the parking lot and dust from the playground), and poor exhaust hood performance.
Table 1.
General characteristics of measurement target school cafeterias by school level
| School level(N) | Average number of service meals per worker | location(N) | Ventilation condition(N) |
|---|---|---|---|
| Elementary (9) | 91 | Ground (7) | Good (5) |
| Underground (2) | Moderate (3) | ||
| Other (0) | Bad (1) | ||
| Middle (8) | 77 | Ground (5) | Good (2) |
| Underground (1) | Moderate (3) | ||
| Other (2) | Bad (3) | ||
| High (7) | 81 | Ground (5) | Good (3) |
| Underground (1) | Moderate (2) | ||
| Other (1) | Bad (2) |
Table 2.
Target school cafeterias for measurement
| School level | Total number of school cafeterias in Republic of Korea | The number of public-school cafeterias in one† region for survey. (% by Republic of Korea in a raw) |
The number of survey target (% by region in a raw) |
|---|---|---|---|
| Elementary | 6,087 | 120 (2.0) | 9 (7.5) |
| Middle | 3,218 | 64 (2.0) | 8 (12.5) |
| High | 2,357 | 59 (2.5) | 8 (13.6)‡ |
| Total | 11,662 | 243 (2.1) | 25 (10.3) |
The Office of Education in Republic of Korea (as of 2019).
Metropolitan city located in southeast of Republic of Korea.
One place was excluded from the survey because it was not operated on the day of measurement.
2.2. Selection of measurement region
Typically, Korean school cafeterias have similar structures. Electricity, gas, oil, and steam are used as heating sources in most school cafeterias. Electricity is mainly used as a heat source where the rice is cooked in the school cafeteria. Canopy hoods are installed close together at the top of the rice cooker, where chefs do not linger as they cook. The primary substance generated during cooking is water vapor and not measured. Excluding the rice-cooking area, the school cafeterias' heat originates from the grill and pot point (Fig. 1). At the grill, a crater directly supplying gaseous fuel (e.g., LNG and LPG) is open to workers. The pot point has a closed structure that receives steam or gas as a heat source through a pipe. If a pot with a structure such as a gas stove is used, it may be exposed to toxic gas due to gas leakage accidents or incomplete combustion of heat sources. Measuring personal samples proved difficult owing to the heavy instrument weights and food hygiene concerns. Thus, an area sampling method was used. The instruments were installed 1.2∼1.5 m from the floor at the nearest pot or grill cooking location and outside the building (Fig. 1, Fig. 2).
Fig. 1.
Examples of measurement points in a school cafeteria.
Fig. 2.
Examples of equipment installation and measurement.
2.3. Measurement and analysis method
Measurements were conducted between June and July 2019. General characteristics of the school cafeteria (e.g., number of cooks, kitchen location, ventilation, and work characteristics) were confirmed through manager interviews and observations. The amount of CO, CO2, PAHs, TVOCs (including benzene), formaldehyde, and airborne particles (PM1, PM2.5, and PM 10) were measured (Table 3). CO and CO2 were measured using a nondispersive direct-reading method (TSI 7545, USA). Zero gas calibration for sensors was performed before measurement according to the manufacturer's field calibration menu. The device was warmed up for > 5 min before measurement, and the concentration ranges of CO and CO2 were confirmed by measuring the concentration in the atmosphere. The measurement of CO and CO2 began when cooking commenced (or when the cooking situation changed) and ended when the measurement stabilized. The maximum CO and CO2 values were recorded. A total of 241 measurements were collected, and the beyond-range CO2 values were replaced with the device's upper limit value and used for analysis. The OPC (Grimm Portable laser aerosol spectrometer and dust monitor model 1.108, Germany) installed at the grill automatically measured and recorded fine particles (PM10 and PM2.5) at intervals of 6 s. The result value was calibrated using the C coefficient calculated by the difference in PTFE filter weight (mounted at the air inlet) before and after measurement. Values above the 99th percentile were deleted and analyzed to correct the outliers of the collected data. A total of 30,903 measurements of collected particulate matter data were used for analysis. SOLID SORBENT TUBE (coconut shell charcoal, 100/50 mg, SKC Cat no. 226-01) was used during the cooking process, and air was collected at a rate of 0.2 L/min using measurements taken in the kitchen (two areas—near the pot and grill areas; experimental group) and outside the building (one area; control group) to evaluate TVOC (including benzene). The flow rate was corrected before and after measurements. Sample measurement, transport, and analysis processes were followed by the NIOSH 1501 method.
Table 3.
Measurement and analysis for field survey
| No | Measurement item | Measurement and analysis | Others |
|---|---|---|---|
| 1 | CO, CO2 | Non-dispersive direct-reading method (TSI 7745, USA) | Whenever cooking new food (241 data collected) |
| 2 | Airborne particles (PM1, PM 2.5, PM10) |
Grimm portable laser aerosol spectrometer and dust monitor model 1.108, Germany | Automatically measured and collected data at grill area in cooking room during the cooking time |
| 3 | TVOC (Total Volatile organic compounds including benzene) |
NIOSH MAM 1501 (SKC Cat no. 226-01, flow rate 0.2l/min, GC) | 2 places (pot and grill area, comparing group), 1place (outside building, control group) |
| 4 | Formaldehyde | NIOSH, MAM 2016 (SKC Cat.no 226-119, flow rate 0.5l/min, HPLC) | 2 places (pot and grill area, comparing group), 1place (outside building, control group) |
| 5 | PAHs (Polycyclic aromatic hydrocarbons) |
NIOSH, MAM 5515(FILTER + SORBENT (2-μm, 37-mm PTFE + washed XAD-2, 100 mg/50 mg, flow rate 2l/min, GC) | 2 places (pot and grill area, comparing group), 1place (outside building, control group) |
For formaldehyde measurements, cartridge-retaining silica gel coating with 2,4-dinitrophenylhydrazine (SKC Cat. no 226-119) was used at a rate of 0.5 L/min. The number of measurements and measurement points was the same as those for TVOC. The flow rate was corrected before and after measurements. Sample measurement, transport, and analysis processes were followed by the NIOSH 2016 method. Air was collected at a rate of 2 L/min using FILTER + SORBENT (2 μm, 37 mm PTFE + washed XAD-2, 100/50 mg, SKC, Cat. No. 226-1713/226-30-04) for PAH evaluation, and silver foil was used to protect samples from light exposure during collection and transfer procedures. The number of measurements and measurement points was the same as those for TVOC. PAH measurement and analysis procedures followed the NIOSH 5515 method. All instruments used for measurements were calibrated. Blank samples were introduced and immediately sealed at the site to correct processing errors (e.g., transfer analysis errors). The measurement time was approximately 2 h and 30 min (from 9 a.m. to 11:30 a.m.) and was only performed during cooking.
2.4. Statistical processing of measurement data
To identify differences in cooking methods by location on kitchen or school level, we analyzed data using the χ2 test. Pearson correlation analysis was conducted to confirm the occurrence pattern. The Kolmogorov–Smirnov test was used to determine the distribution characteristics of the group (normality). The t-test was used when the normal distribution of each sample group was statistically determined; otherwise, the Mann–Whitney U test was used to compare two groups, and the Kruskal–Wallis test was used to compare three groups (SPSS version 22).
3. Results
3.1. General characteristics of target school cafeterias
The number of service meals per worker was the highest at 91 in elementary schools. Six (25%) areas were determined to have poor ventilation in the school cafeteria by their cafeteria managers (mainly nutrition). School cafeterias were located underground in four (16%) areas (Table 1).
3.2. Cooking method by location or school level
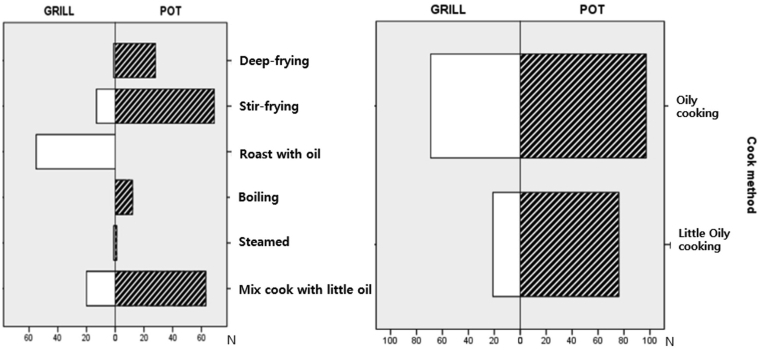
Cooking methods were analyzed by characterizing them as oily-heavy cooking (e.g., deep frying, stir frying, and roasting with oil) and oily-light cooking (e.g., boiling, steaming, mixed cooking without much oil). There were differences in cooking methods by location in the cooking room, and it was found that cooking methods that use little oil were used more in the pot area than in the grill area (Fig. 3). However, the significant difference was borderline in cooking methods at the school level (Fig. 4, p = 0.075).
Fig. 3.
Difference in cook method by location in cooking room (χ2 test, p = 0.001), ※ Cooking method: oily cooking (deep frying, stir-frying, roasted with oil), little oily cooking (boiling, steamed, mixed cook with little oil).
Fig. 4.
Difference of cook method by school gradein cooking room (χ2 test, p = 0.075), ※ Cooking method: oily cooking (deep frying, stir-frying, roasted with oil), little oily cooking (boiling, steamed, mixed cook with little oil).
3.3. Concentration and pattern of substances generated during cooking
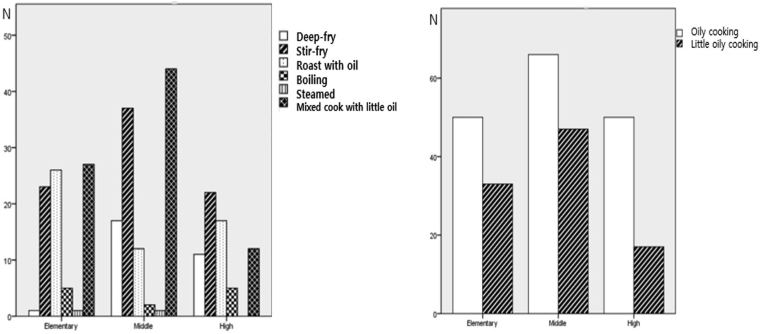
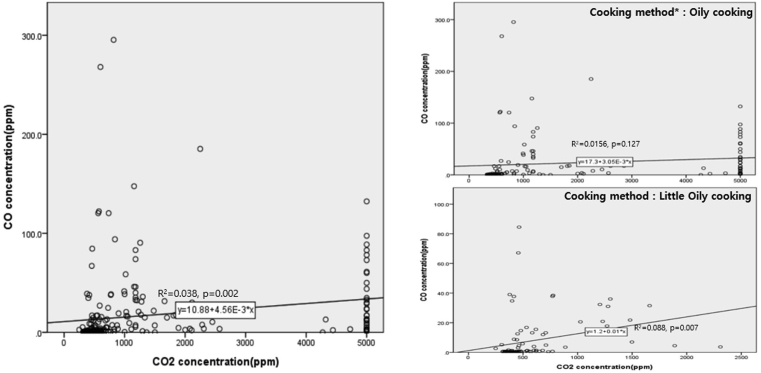
3.3.1. CO and CO2
The correlation between CO and CO2 concentrations in the school kitchen was significant and was particularly noticeable in the minor oil cooking method (Fig. 5). Accordingly, the correlation between CO and CO2 was statistically confirmed in the pot area, where there were relatively many cooking methods that rarely used oil (correlation coefficient = 0.286; p = 0.005). The difference in CO concentrations at the school level was statistically significant, though the concentration was higher in middle or high school kitchens than in elementary schools. This phenomenon was particularly noticeable during oily cooking (Fig. 6). In addition, the CO concentration exceeded the ceiling value of NIOSH (TLV-STEL, in Republic of Korea) of 200 ppm at one middle school (two measurement values; Fig. 6).
Fig. 5.
The correlation between CO and CO2 by cooking method in the school cooking room, ※ Cooking method: oily cooking (deep frying, stir-frying, roasted with oil), little oily cooking (boiling, steamed, mixed cook withlittle oil).
Fig. 6.
Difference in CO by school grade during the Oily cooking, † TLV-Ceiling: Exposure concentration should not be exceeded at any time during a complete cycle of operation or throughout the work shift [8]. ∗ TLV-STEL: 15 min TWA (Time Weighted Average) exposure limit and the concentration to which it is believed that nearly all workers can be exposed continuously for a short period of time without suffering from 1) irritation, 2) chronic or irreversible tissue damage, 3) dose-rate-dependent toxic effects or 4) narcosis of sufficient degree to increase the likelihood of accidental injury, impaired self rescue, or materially reduced work efficiency [10]. ※ Kruskal–Wallis-test, k-independent sample, ordinal, p = 0.000), Elementary<Middle (p = 0.000), Elementary<High (p = 0.000), Middle<High (p = 0.706), ※ Median in the box, 75% above the box boundary, 25% below the box boundary, 95% above the whisker, 5% below the whisker.
3.3.2. PAHs, benzene, VOCs, and formaldehyde
The average concentration of PAHs in cafeterias was 10.6 ng/m3 (1.59)—geometric mean (geometric standard deviation)—with a maximum value of 1,839.52 ng/m3 (Table 5). Naphthalene (NAP) accounted for the majority (70%∼100%) of PAHs. BAP was not detected in most cooking environments. The highest BAP value was 5.85 ng/m3 (Table 4).
Table 5.
Formaldehyde, benzene, PAHs, and TVOC concentration differences by place (ug/m3)
| Materials | Place∗ | N | AM | SD | GM | GSD | Min | Median | Max | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Formaldehyde† | Indoor | 46 | 6.47 | 4.42 | 1.98 | 1.52 | 0.06 | 5.76 | 18.52 | 0.00§ |
| Outdoor | 26 | 2.66 | 1.88 | 1 | 6.09 | 0.00‖ | 2.03 | 6.88 | ||
| Benzene‡ | Indoor | 46 | 11.94 | 8.57 | 2.59 | 1.46 | 0.52 | 10.95 | 50.29 | 0.46 |
| Outdoor | 26 | 10.46 | 7.11 | 2.26 | 1.71 | 0.33 | 11.57 | 19.96 | ||
| PAHs‡(ng/m3) | Indoor | 46 | 371.95 | 446.32 | 10.16 | 1.59 | 40.76 | 163.12 | 1,839.52 | 0.02§ |
| Outdoor | 26 | 168.18 | 151.23 | 7.91 | 1.47 | 27.47 | 137.25 | 617.34 | ||
| TVOC† | Indoor | 46 | 147.03 | 327.05 | 6.5 | 1.64 | 1.09 | 95.94 | 2,237.82 | 0.7 |
| Outdoor | 26 | 92.2 | 71.45 | 6.19 | 1.48 | 4.98 | 64.27 | 301.21 |
※ LOD: Formaldehyde 0.0018ng/ml, Benzene 0.15ng/ml, Treated less than LOD as 1/2 LOD.
Place: Indoor (Grill point and Pot point in cooking room), Outdoor.
T-test for two groups.
Mann–Whitney test for two group.
p < 0.05.
1/2LOD.
Table 4.
PAHs concentration differences by measurement place unit: ng/m3
| Materials∗ | Place‡ | N | AM | SD | GM | GSD | Min | Median | Max | p |
|---|---|---|---|---|---|---|---|---|---|---|
| NAP† (2)¶ | Indoor | 46 | 311.42 | 312.09 | 9.87 | 1.54 | 40.76 | 161.28 | 1,300.65 | 0.02§ |
| Outdoor | 26 | 156.01 | 125.99 | 7.79 | 1.45 | 25.62 | 136.28 | 480.18 | ||
| ANL (3) | Indoor | 46 | 8.08 | 27.17 | 0.00∗∗ | 33.07 | 0.00 | 0.00 | 133.63 | 0.11 |
| Outdoor | 26 | 0.5 | 2.42 | 0.00 | 8.37 | 0.00 | 0.00 | 12.36 | ||
| ANE (3) | Indoor | 46 | 9.1 | 40.49 | 0.01 | 33.73 | 0.00 | 0.00 | 202.04 | 0.23 |
| Outdoor | 26 | 2.77 | 13.53 | 0.00 | 10.04 | 0.00 | 0.00 | 69.05 | ||
| FLU (3) | Indoor | 46 | 8.84 | 17.45 | 0.29 | 31.55 | 0.00 | 2.09 | 83.4 | 0.07 |
| Outdoor | 26 | 2.34 | 5.36 | 0.07 | 43.22 | 0.00 | 1.1 | 27.63 | ||
| PHE (3) | Indoor | 46 | 8.84 | 17.45 | 0.29 | 31.55 | 0.00 | 2.09 | 83.4 | 0.05 |
| Outdoor | 26 | 2.34 | 5.36 | 0.07 | 43.22 | 0.00 | 1.1 | 27.63 | ||
| ANT (3) | Indoor | 46 | 0.22 | 0.85 | 0.00 | 6.96 | 0.00 | 0.00 | 3.57 | 0.07 |
| Outdoor | 26 | 0.09 | 0.46 | 0.00 | 4.45 | 0.00 | 0.00 | 2.34 | ||
| FLT (3) | Indoor | 46 | 0.8 | 5 | 0.00 | 7.29 | 0.00 | 0.00 | 33.89 | 0.08 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0 | ||
| PYR (4) | Indoor | 46 | 2.07 | 9.93 | 0.00 | 17.08 | 0.00 | 0.00 | 66.44 | 0.6 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| BAA (3) | Indoor | 46 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | 1 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| CHR (4) | Indoor | 46 | 0.02 | 0.14 | 0.00 | 2.94 | 0.00 | 0.00 | 0.97 | 0.45 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| BBF (5) | Indoor | 46 | 0.06 | 0.42 | 0.00 | 3.03 | 0.00 | 0.00 | 2.88 | 0.45 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| BKF (5) | Indoor | 46 | 0.04 | 0.18 | 0.00 | 4.39 | 0.00 | 0.00 | 0.91 | 0.28 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| BAP (5) | Indoor | 46 | 0.31 | 1.22 | 0.00 | 7.01 | 0.00 | 0.00 | 5.85 | 0.18 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| ICP (6) | Indoor | 46 | 0.3 | 1.15 | 0.00 | 7.32 | 0.00 | 0.00 | 5.24 | 0.19 |
| Outdoor | 26 | 0.00 | 0.00 | 0.00 | 1 | 0.00 | 0.00 | 0.00 | ||
| DAH (5) | Indoor | 46 | 0.15 | 0.72 | 0.00 | 9.3 | 0.00 | 0.00 | 4.8 | 0.29 |
| Outdoor | 26 | 0.01 | 0.04 | 0.00 | 3.68 | 0.00 | 0.00 | 0.22 | ||
| BGP (6) | Indoor | 46 | 1.35 | 5.36 | 0.00 | 8.8 | 0.00 | 0.00 | 26.17 | 0.65 |
| Outdoor | 26 | 0.04 | 0.19 | 0.00 | 4.26 | 0.00 | 0.00 | 0.96 |
※ LOD(ng/ml): NAP, 0.18; ANL, 0.09; ANE, 0.11; FLU, 0.10; PHE, 0.11; ANT, 0.11; FLT, 0.09; PYR, 0.07; BAA, 0.19; CHR, 0.09; BBF, 0.17; BKF, 0.12; BAP, 0.15; BGP, 0.08; DAH, 0.10; ICP, 0.10).
PAHs: NAP(Naphthalene), ANL(Acenaphthylene), ANE(Acenaphthene), FLU(Fluorene), PHE(Phenanthrene), ANT(Anthracene), FLT(Fluoranthene), PYR(Pyrene), BAA(Benzo[a]anthracene), CHR(Chrysene), BBF(Benzo(b)fluoranthene), BKF(Benzo(k)fluoranthene), BAP(Benzo(a)pyrene), ICP (Indeno(1,2,3-cd) pyrene), DAH (Dibenz(a,h)anthracene), BGP(Benzo(ghi)perylene).
T-test for two groups.
Place: Indoor (Grill point and Pot point in cooking room), Outdoor.
p < 0.05.
Number of benzene rings (source: NIH, National Library of Medicine).
Cut to three decimal places, not real zero. Treated less than LOD (Limt of Detection) as 1/2 LOD.
Among the PAHs in cafeterias, NAP was significantly higher than outdoor PAHs (Table 4). The concentration of formaldehyde was significantly higher in the cafeteria than outside. However, TVOCs (including benzene) inside the cafeteria were not significantly different from those outdoors (Table 5). As a result of comparing the exposure difference by location in the cafeteria, there was no significant difference in exposure for any evaluated substance.
In the PAHs (naphthalene) analysis by school level, the concentration in elementary school cooking rooms was higher than in middle school cafeterias. Additionally, the formaldehyde concentration was relatively lower in middle schools than in elementary and high schools (Table 6).
Table 6.
Formaldehyde, benzene, PAHs, and TVOC concentration differences by school level
| School level | PAHs (ng/m3) |
Naphthalene (ng/m3) |
Formaldehyde (ug/m3) |
Benzene (ug/m3) |
TVOC (ug/m3) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | AM∗ | SD | P | N | AM | SD | P | N | AM | SD | P | N | AM | SD | p | N | AM | SD | P | |
| Elementary | 20 | 574.48 | 558.05 | 0.005∗ | 20 | 456.81 | 358.70 | 0.005∗ | 20 | 7.33 | 4.17 | 0.01∗ | 20 | 11.31 | 8.31 | 0.22 | 20 | 106.19 | 72.15 | 0.50∗ |
| Middle | 13 | 124.29 | 76.15 | 13 | 122.01 | 74.85 | 13 | 3.91 | 3.98 | 13 | 9.25 | 3.84 | 13 | 73.57 | 39.79 | |||||
| High | 13 | 308.04 | 329.98 | 13 | 277.17 | 283.85 | 13 | 7.70 | 4.44 | 13 | 15.61 | 11.32 | 13 | 283.31 | 602.11 | |||||
※ Kruskal–wallis-test, k-independent sample, ordinal, ∗ p < 0.05.
Arithmetric means.
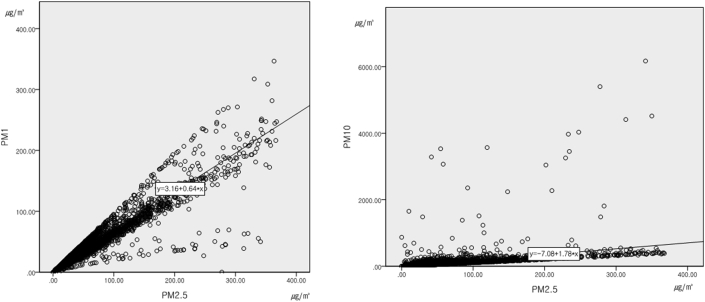
3.3.3. Airborne particles (PM1, PM2.5, and PM10)
The correlation coefficient between concentrations of PM2.5 and PM1 from cooking was 0.90 (p = 0.000; Fig. 7). Concentrations of PM2.5 and PM1 were significantly higher during oil-heavy cooking (Table 7).
Fig. 7.
The correlation between PM2.5 and PM1, PM10 concentration during cooking process in school cooking rooms.
Table 7.
PM1, PM2.5, PM10 concentration differences by cooking method at the grill area unit: ug/m3
| Cooking method† | PM 1∗ |
PM 2.5∗ |
PM 10∗ |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | AM | SD | Median | Max | p | N | AM | SD | Median | Max | p | N | AM | SD | Median | Max | p | |
| Oily cooking | 16,221 | 19.40 | 24.80 | 13.30 | 346.70 | 0.00∗ | 16,221 | 24.78 | 36.87 | 15.30 | 367.90 | 0.00∗ | 16,221 | 36.19 | 129.36 | 17.00 | 6169.00 | 0.00∗ |
| Little oily cooking | 14,682 | 12.91 | 11.38 | 9.80 | 227.90 | 14,682 | 15.85 | 17.17 | 11.20 | 350.00 | 14,682 | 22.00 | 50.35 | 12.90 | 4516.40 | |||
Average PM2.5 concentration in A area (metropolitan city located in southeast of Republic of Korea) of 2019: 20 (2019 Jun 21: 18 , 2019 July:18 , 2019 Aug:17.9 ).
Available from: air KOREA (https://www.airkorea.or.kr).
Mann–Whitney test for two group, ∗ p < 0.05.
Cook Method: oily cooking (deep frying, stir-frying, roasted with oil), little oily cooking (boiling, steamed, mixed cook with little oil).
4. Discussion
There was no difference noted in this study, unlike previous studies, that showed that CO concentration was high in oil-based cooking (e.g., frying) in comparison to water-based cooking (e.g., boiling) [20]. However, there was difference in CO concentrations between school levels. This effect may be due to the number of food ingredients (especially oil) [22], as the same recipe typically uses more ingredients (like oil) for higher school levels than for lower school levels.
Our study showed the association between CO and CO2; however, it would be difficult to predict the CO concentration from the CO2 concentration, as the coefficient was very low. Nevertheless, both CO and CO2 showed higher concentration trends in oil-based cooking than non-oil-based cooking. CO in the kitchen is easily absorbed by water vapor owing to comparable polarity [23], it may be the the reason for the low CO and CO2 concentrations in non-oil-based cooking.
In addition, the highest concentration of CO was 295 ppm, exceeding the ceiling value proposed by NIOSH. This exposure was higher than the transient high-concentration complex exposure (CO: 30 ppm, CO2: 5,000 ppm) found in roasted pork belly in commercial kitchens, as reported by Won-Seok Cha of Republic of Korea. Compared to previous studies [8,23], the CO concentration was relatively high as cafeteria cooking environments use many ingredients at a time. Furthermore, this result is not derived in a strict experimental environment, CO generated from fuel cannot be completely excluded.
Although much of the oil-heavy cooking was performed at school cafeterias in Republic of Korea, carcinogenic substances were detected at a much lower concentration than that in a Chinese cooking environment, where high-temperature cooking using oil was common. In 1999∼2000, 12 types of PAHs in the air were measured in six home kitchens and four commercial kitchens in China. The arithmetic average concentration of total PAHs in commercial kitchens was 7,000 ng/m3, including PAHs consisting of three or four benzene rings. Conversely, in Chinese home kitchens, a total PAH concentration of 7,600 ng/m3 consisting of two and three rings was detected, with NAP as the main component. The BAP level was 6.1∼24 ng/m3 in home kitchens and 150∼440 ng/m3in commercial kitchens [24]. In this study, the concentration of total PAHs was 371.95ng/m3 (446.32 ng/m3)—arithmetic mean (standard deviation)—with a maximum value of 1,839.52 ng/m3, about 4.8% of the average exposure in Chinese home and commercial kitchens. BAP was not detected during cooking. The maximum value of BAP detected was 5.85 ng/m3 and lower than the minimum exposure concentration in Chinese home kitchens.
Cha and Kim (2020) found PAHs with four benzene rings such as BKF and BBF, in the measurement results for two food service workplaces in Republic of Korea. However, these levels were very low. In addition, no BAP were detected. The frying temperature was estimated to be 170∼180 °C, lower than the temperature (280∼300 °C) required for PAHs with five or more benzene rings to become gases [8].
In specific samples of this study, some PAHs with many benzene rings were detected, although their levels were very low. For example, using fried cooking <3 h resulted in a significant difference in the PAH concentrations between cooking rooms and outdoors. However, this effect is owing to the difference in NAP, which accounts for most PAHs. PAHs with numerous rings were found to be more toxic than those with fewer rings [20]. The main PAHs in cooking fumes are 3∼4 ring compounds, regardless of the cooking method, oil amount, and food type [22,24]. However, our results showed that 2∼3 rings were predominantly used in Indian cooking rooms [21] (which contain dishes like stews) or Chinese home kitchens.
TVOCs, including benzene, were generated during cooking. However, there were no significant differences in their concentrations between cooking rooms and outdoors. Formaldehyde concentrations were significantly higher in school kitchens than outdoors, with an average concentration of 4.81 (2.60)—the geometric mean (geometric standard deviation)—and a maximum concentration of 18.52 , which was as low as 20% of the domestic office management standard (100 ) in Republic of Korea. The average concentration of PM2.5 in school cafeterias was 24.78 , including areas using heavy-oil cooking, which was slightly higher than the average concentration of 20.1 in the area at the initiation of the study. In 2008, Pang et al. found that the average exposure concentration of PM2.5 in 23 Taiwanese restaurant kitchens was 58.8 (geometric standard deviation 1.6), with a median value of 56.9 . The median value found in the school cafeteria was 15.30 , and very low [25]. However, its maximum concentration was 367.90 , corresponding to a dangerous air concentration level of AQI (EPA's Air Quality Index) [26]. Thus, the harmful effects of short-term exposure could not be excluded.
5. Conclusion
Known carcinogens of school cooking fumes in Republic of Korea have lower concentrations than those found in the literature on Chinese cooking fumes. However, short-term high-concentration exposure of some substances (e.g., CO, CO2, PM 2.5) in cooking fumes was also confirmed, and adverse health effects such as cardiovascular and respiratory diseases would be expected. In addition, as most epidemiological studies of cooking fumes and lung cancer are based on epidemiological data from China, additional exposure data and health effects reflecting the specificity of domestic cooking environments and epidemiological studies are required for Republic of Korea.
Conflicts of interest
All authors have no conflicts of interest to declare.
Acknowledgements
This work was supported by the Republic of Korea Occupational Safety and Health Institute. We thank the officials of the OO Regional Office of Education for actively supporting the field survey.
References
- 1.KOSIS . 2019. Workforce survey.https://kostat.go.kr/ [cited 2021 Jun 21]. Available from: [in Korean] [Google Scholar]
- 2.Occupational Safety and Health Research Institute of KOREA . 2020. 2019 Pilot operation of occupational acute intoxication surveillance system.https://oshri.kosha.or.kr/oshri/professionalBusiness/occupationalDiseaseReferenceRoom.do.do Report No: 2019-연구원-1442. Available from: [in Korean] [Google Scholar]
- 3.Occupational Safety and Health Research Institute of KOREA . 2019. 2018 Pilot operation of occupational acute intoxication surveillance system.https://oshri.kosha.or.kr/oshri/professionalBusiness/occupationalDiseaseReferenceRoom.do Report No: 2018-연구원-878. Available from: [in Korean] [Google Scholar]
- 4.Kang-jin Lee. Segye newspaper; 2021.04.16. A culinary practitioner who died of lung cancer while working in the school cafeteria… First judgment of “occupational disease” [Newspaper article-internet]https://www.segye.com/newsView/20210406514947?OutUrl=naver.do [cited 2021 Jun 1]. Available from: In press. [in Korean] [Google Scholar]
- 5.IARC . 2010. Monographs on the Evaluation of Carcinogenic Risks to Humans VOLUME 95. Household use of solid fuels and high temperature frying.https://monographs.iarc.who.int/wp-content/uploads/2018/06/mono95.pdf [cited 2021 Jun 1] Available from: [PMC free article] [PubMed] [Google Scholar]
- 6.Yu I.T.S., Chiu Y.-L., Au J.S.K., Wong T.-W., Tang J.-L. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Res. 2006;66:4961–4967. doi: 10.1158/0008-5472.CAN-05-2932. [DOI] [PubMed] [Google Scholar]
- 7.Xue Yingbo, Jiang Ying, Jin Shan, Li Yong. Association between cooking oil fume exposure and lung cancer among Chinese nonsmoking women: a meta-analysis. Onco Targets Ther. 2016;9:2987–2992. doi: 10.2147/OTT.S100949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cha Won-Seok, Kim Eun-Young. A study on exposure of respiratory hazard factors in food service workplace. J Korean Soc Occup Environ Hyg. 2020;30(1):75–86. [Google Scholar]
- 9.Levin B.C., Paabo M., Gurman J.L., Harris S.E., Braun E. Toxicological Interactions Between Carbon Monoxide and Carbon Dioxide. 1987 Dec 1;47(1–2):135. doi: 10.1016/0300-483x(87)90165-x. 64. [DOI] [PubMed] [Google Scholar]
- 10.Levin Barbara C., Paabo Maya, Gurman Joshua L., Harris Steven E. Effects of exposure to single or multiple combinations of the predominant toxic gases and low oxygen atmospheres produced in fires. Fundam Appl Toxicol. 1987 August;9(2):236–250. doi: 10.1016/0272-0590(87)90046-7. [DOI] [PubMed] [Google Scholar]
- 11.Li Tao, Hu Rong, Chen Zi, Li Qiyuan, Huang Shouxiong, Zhu Zhou, Zhou Lin-Fu. Fine particulate matter (PM2.5): the culprit for chronic lung diseases in China. Chronic Dis Transl Med. 2018 Aug 28;4(3):176–186. doi: 10.1016/j.cdtm.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim T.Y., Kim H., Yi S.M., Cheong J.P., Heo J. Short-term effects of ambient PM2.5 and PM2.5-10 on mortality in major cities of Republic of Korea. Aerosol Air Qual Res. 2018;18:1853–1862. [Google Scholar]
- 13.Matsuo Ryu, Michikawa Takehiro, Ueda Kayo, Ago Tetsuro, Nitta Hiroshi, Kitazono Takanari. Short-term exposure to fine particulate matter and risk of ischemic stroke. Stroke. 2016;47:3032–3034. doi: 10.1161/STROKEAHA.116.015303. [DOI] [PubMed] [Google Scholar]
- 14.Shi L., Zanobetti A., Kloog I., Coull B.A., Koutrakis P., Melly S.J., Schwartz J.D. Low-concentration PM2.5 and mortality: estimating acute and chronic effects in a population-based study. Environ Health Perspect. 2016 Jan;124(1):46–52. doi: 10.1289/ehp.1409111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu C., Chen R., Sera F., Vicedo-Cabrera A.M., Guo Y., Tong S., Coelho M.S.Z.S., Saldiva P.H.N., Lavigne E., Matus P., Valdes Ortega N., Osorio Garcia S., Pascal M., Stafoggia M., Scortichini M., Hashizume M., Honda Y., Hurtado-Díaz M., Cruz J., Nunes B., Teixeira J.P., Kim H., Tobias A., Íñiguez C., Forsberg B., Åström C., Ragettli M.S., Guo Y.-L., Chen B.-Y., Bell M.L., Wright C.Y., Scovronick N., Garland R.M., Milojevic A., Kyselý J., Urban A., Orru H., Indermitte E., Jaakkola J.J.K., Ryti N.R.I., Katsouyanni K., Analitis A., Zanobetti A., Schwartz J., Chen J., Wu T., Cohen A., Gasparrini A., Kan H. Ambient particulate air pollution and daily mortality in 652 cities. New Engl J Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) 2013. Review of evidence on health aspects of air pollution—REVIHAAP.https://www.euro.who.int/ [cited 2021 Jun 1]. Available from: [Google Scholar]
- 17.Xue Y., Jiang Y., Jin S., Li Y. Association between cooking oil fume exposure and lung cancer among Chinese nonsmoking women: a meta-analysis. OncoTargets Ther. 2016:2987. doi: 10.2147/OTT.S100949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dong R. Chinese Agricultural University; 2016. Assessment of improvements in the sino-Dutch rural renewable energy project. Chinese agricultural university report to the Chinese association of rural energy industries. [Google Scholar]
- 19.Hu W., Downward G.S., Reiss B., Xu J., Bassig B.A., Hosgood H.D., Zhang L., Seow W.J., Wu G., Chapman R.S., Tian L., Wei F., Vermeulen R., Lan Q. Personal and indoor PM2.5 exposure from burning solid fuels in vented and unvented stoves in a rural region of China with a high incidence of lung cancer. Environ Sci Technol. 2014;48:8456–8464. doi: 10.1021/es502201s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li C.T., Lin Y.C., Lee W.J., Tsai P.J. Emission of polycyclic aromatic hydrocarbons and their carcinogenic potencies from cooking sources to the urban atmosphere. Environ Health Perspect. 2003;111:483–487. doi: 10.1289/ehp.5518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei See S., Karthikeyan S., Balasubramanian R. Health risk assessment of occupational exposure to particulate-phase polycyclic aromatic hydrocarbons associated with Chinese, Malay and Indian cooking. J Environ Monit. 2006 Mar;8(3):369–376. doi: 10.1039/b516173h. [DOI] [PubMed] [Google Scholar]
- 22.Yao Z., Li J., Wu B., Hao X., Yin Y., Jiang X. Characteristics of PAHs from deep-frying and frying cooking fumes. Environ Sci Pollut Res Int. 2015 Oct;22(20):16110–16120. doi: 10.1007/s11356-015-4837-4. [DOI] [PubMed] [Google Scholar]
- 23.Huboyo Haryono S., Tohno Susumu, Cao Renqiu. Indoor PM2.5 characteristics and CO concentration related to water-based and oil-based cooking emissions using a gas stove. Aerosol Air Qual Res. 2011;11:401–411. [Google Scholar]
- 24.Zhu L., Wang J. Sources and patterns of polycyclic aromatic hydrocarbons pollution in kitchen air, China. Chemosphere. 2003 Feb;50(5):611–618. doi: 10.1016/s0045-6535(02)00668-9. [DOI] [PubMed] [Google Scholar]
- 25.Pan Chih-Hong, Chan Chang-Chuan, Wu Kuen-Yuh. Effects on Chinese restaurant workers of exposure to cooking oil fumes: a cautionary note on urinary 8-hydroxy-2 '-Deoxyguanosine. Cancer Epidemiol Biomarkers Prev. 2008 Dec;17(12):3351–3357. doi: 10.1158/1055-9965.EPI-08-0075. [DOI] [PubMed] [Google Scholar]
- 26.EPA . 2003. Particle pollution and your health.https://nepis.epa.gov/Exe/ZyPDF.cgi?Dockey=P1001EX6.txt [cited 2021 Jun 1]. Available from: [Google Scholar]