Summary
Background
Strategies to improve outcomes for Australian First Nations mothers and babies are urgently needed. Caseload midwifery, where women have midwife-led continuity throughout pregnancy, labour, birth and the early postnatal period, is associated with substantially better perinatal health outcomes, but few First Nations women receive it. We assessed the capacity of four maternity services in Victoria, Australia, to implement, embed, and sustain a culturally responsive caseload midwifery service.
Methods
A prospective, non-randomised research translational study design was used. Site specific culturally responsive caseload models were developed by site working groups in partnership with their First Nations health units and the Victorian Aboriginal Community Controlled Health Organisation. The primary outcome was to increase the proportion of women having a First Nations baby proactively offered and receiving caseload midwifery as measured before and after programme implementation. The study was conducted in Melbourne, Australia. Data collection commenced at the Royal Women's Hospital on 06/03/2017, Joan Kirner Women's and Children's Hospital 01/10/2017 and Mercy Hospital for Women 16/04/2018, with data collection completed at all sites on 31/12/2020.
Findings
The model was successfully implemented in three major metropolitan maternity services between 2017 and 2020. Prior to this, over a similar timeframe, only 5.8% of First Nations women (n = 34) had ever received caseload midwifery at the three sites combined. Of 844 women offered the model, 90% (n = 758) accepted it, of whom 89% (n = 663) received it. Another 40 women received standard caseload. Factors including ongoing staffing crises, prevented the fourth site, in regional Victoria, implementing the model.
Interpretation
Key enablers included co-design of the study and programme implementation with First Nations people, staff cultural competency training, identification of First Nations women (and babies), and regular engagement between caseload midwives and First Nations hospital and community teams. Further work should include a focus on addressing cultural and workforce barriers to implementation of culturally responsive caseload midwifery in regional areas.
Funding
Partnership Grant (# 1110640), Australian National Health and Medical Research Council and La Trobe University.
Keywords: First nations, Implementation science, Midwifery
Research in context.
Evidence before this study
In Australia, numerous government reports and enquiries state that strategies to improve health outcomes for Aboriginal and Torres Strait Islander (hereafter called First Nations) mothers and babies are urgently needed. A Cochrane review found that women who had midwife-led continuity of care (compared with standard maternity care) were less likely to experience preterm birth or fetal loss prior to 24 weeks’ gestation, yet the availability of these models for First Nations women is limited, and little is known about the capacity of large maternity services to implement culturally-specific models for First Nations women. Since project commencement, we have had an ongoing search alert for relevant Medical Subject Headings (MeSH) search terms and actively monitored publications, therefore no additional specific literature search was conducted for this study.
Added value of this study
This research translation study demonstrated the ability of three major metropolitan health services in Melbourne, Australia to successfully implement and sustain a culturally responsive model of maternity care for women having a First Nations baby. The model, developed in partnership with the Victorian Aboriginal Community Controlled Health Organisation, along with participating sites and their First Nations health units, provided women with continuity of care during pregnancy, labour, birth and the early postnatal period from the same known midwife (with one or two back-up midwives) – caseload midwifery – a model associated with substantially better perinatal health outcomes for non-First Nations women. We demonstrated a 21-fold increase in access to the model for First Nations women with high uptake (90%), demonstrating feasibility and acceptability. We did not achieve translation in the regional setting.
Implications of all the available evidence
Our successful research translation study demonstrated the ability of three major, metropolitan maternity services to implement a new, culturally responsive, caseload midwifery model that was embedded and sustained throughout the study period. Further scale-up of this model should be prioritised, with further research focused on understanding key features of implementing and sustaining the model (including in regional settings) and continuing to build the partnership between First Nations and hospital maternity services.
Alt-text: Unlabelled box
Introduction
In Australia, numerous government reports have recommended the urgent need for strategies that improve health outcomes for Aboriginal and Torres Strait Islander (hereafter called First Nations) mothers and babies.1,2 Perinatal mortality for First Nations babies is substantially higher than non-First Nations babies (14.8 vs 9.6 deaths/1000 births) and the maternal mortality ratio is more than three times higher for First Nations women (17.5 vs 5.5 deaths/100,000 births).3 Preterm birth (birth before 37 completed gestational weeks) and being low birthweight (< 2500 g) are both substantially higher for First Nations babies, and associated with significant morbidity and mortality.3 Perinatal factors such as preterm birth are responsible for 85% of deaths occurring in the first 18 months of life.2
Poor quality antenatal care can contribute to poorer pregnancy outcomes for First Nations women.4 The National Aboriginal and Torres Strait Islander Health Plan (2013–2023) highlights the need for improved quality and accessibility of routine antenatal care; evidence-based strategies to reduce maternal stress and smoking, improve nutrition in pregnancy, and increase breastfeeding; and better monitoring of maternal and fetal health.1 More recently, the National Strategic Directions for Australian Maternity Services report5 and Victorian Government strategic plans emphasise the need for services to provide appropriately developed, culturally safe and accessible perinatal care for First Nations women.6,7 The caseload midwifery model may be an important strategy to address these requirements.8, 9, 10, 11, 12, 13
In the caseload midwifery model, women receive continuity in pregnancy, labour, birth and the early postnatal period from the same known midwife (and one or two ‘back-up’ midwives). Our team conducted the world's largest randomised controlled trial (RCT) of caseload midwifery (the COSMOS trial, n = 2314 low-risk women),14 and found that compared with standard maternity care, babies of women allocated to caseload care were less likely to be low birthweight or admitted to neonatal special or intensive care units. Women were more likely to report being satisfied with their care, and to feel safe, informed, supported emotionally, and that their concerns were taken seriously.15 The model was further tested with women of any obstetric risk in another Australian RCT, the M@NGO trial (n = 1748 women), and was found to be safe and cost effective.16
The Cochrane review of midwife-led care (n = 15 RCTs (including COSMOS and M@NGO) and 17,674 women), found that women who had midwife-led continuity of care (compared with other models of maternity care) were less likely to experience preterm birth or fetal loss prior to 24 weeks’, and less likely to have interventions such as instrumental birth and episiotomy.17 Women were more satisfied with care, and there was some evidence of reduced costs. The review concluded that most women should be offered midwife-led care, but that caution be exercised in applying this to women at substantial risk of obstetric or medical complications.
Many hospital-based caseload models have restrictive inclusion criteria related to medical and obstetric risk factors, thus often exclude First Nations women. An Australian national survey found 16 services specifically offered caseload midwifery care to First Nations women, but actual numbers of First Nations women receiving caseload was low.18 However, where First Nations women accessed caseload care, they reported it to be very positive, and valued having a known care provider.10,11,13,19 A recent large prospective, non-randomised intervention study (n = 766 intervention group; n = 656 control) conducted in Queensland, Australia, evaluated a midwifery group practice (caseload) continuity of care model for First Nations women. The study found that women in the intervention group were more likely to access early antenatal care and have five or more antenatal visits, with significantly reduced preterm births, neonatal nursery admissions, planned caesareans, and epidural pain relief, and increased exclusive breastfeeding on discharge from hospital.10 Other studies have found increased antenatal engagement,8 increased pregnancy visits, and more antenatal screening13 and a recent review concluded that there is an urgent need to extend continuity of care for First Nations women in order to improve outcomes.20 However, implementation of culturally appropriate caseload midwifery care models requires local leadership, specific funding and strong partnerships.21, 22, 23
The caseload midwifery model offers a collaborative and coordinated approach, providing First Nations women the opportunity to have a known midwife who has appropriate cultural training to help them navigate their journey through the maternity care system, while maintaining their community and family supports. Given how few First Nations women in Australia currently have access to this model of care, we aimed to assess the capacity of four Victorian maternity services (including a regional hospital), to implement, embed and sustain a culturally responsive caseload midwifery model for First Nations women. This paper reports on the outcomes of the primary aim of the study – to increase the proportion of First Nations women and non-First Nations women having a First Nations baby, (hereafter referred to as women having a First Nations baby) proactively offered and receiving caseload midwifery.
Methods
Study design
This study was co-designed in partnership with the Victorian Aboriginal Community Controlled Health Organisation (VACCHO), the peak body for First Nations health in Victoria, along with participating health services and their First Nations health units. The project was developed with a focus on evidence translation – offering First Nations women access to caseload midwifery care given the known beneficial outcomes, both clinical and psychosocial.17 An RCT was considered, but the group's view was that implementing the model and offering it to all First Nations women at the study sites was the most appropriate design. We therefore developed a prospective non-randomised implementation study, using before and after outcome measures. The study was conducted in Melbourne, Australia with data collection commencing at the Women's on 06/03/2017, Joan Kirner 01/10/2017 and the Mercy 16/04/2018. Data collection was completed at all sites on 31/12/2020.
This paper includes among its authors members of the study's First Nations Advisory Committee (comprising all First Nations project investigators, two Elders, a recent new mother from the First Nations community, and representatives from VACCHO), the research team, and key stakeholders from partner organisations, both First Nations and non-First Nations. The Advisory Committee provided cultural guidance and oversight to the research team regarding methods, community engagement, discussion of findings, and knowledge translation. Participating health services each established a steering committee of key staff responsible for model implementation.
Study aims
The overall study aimed to explore (1) model implementation (2) women's views, experiences and outcomes (clinical and psychosocial, including infant outcomes), and (3) potential for sustainability of the model in the organisations (staff views, workforce capacity building cultural safety, costs etc.). This paper reports on Aim 1 (model implementation). Aims 2 and 3 will be reported elsewhere. Specific aims related to model implementation were:
-
(a)
Develop and implement culturally appropriate caseload midwifery care for First Nations women at the study sites;
-
(b)
Increase the proportion of First Nations women booking for maternity care at the study sites who are i. identified and ii. offered caseload midwifery care; and
-
(c)
Measure the uptake of caseload midwifery care by First Nations women booking for maternity care at the study sites.
Participants
Four health services in Victoria, Australia, were partners in the project, along with VACCHO and La Trobe University. The sites were specifically chosen for having an established functioning caseload midwifery model, and a relatively large number of First Nations babies born at the site. Prior to study commencement there were approximately 250 First Nations women per year birthing across the four sites. Table 1 describes the sites. Many women accessing maternity care at the Women's and the Mercy hospital are referred from the Victorian Aboriginal Health Service (VAHS), a number of whom chose maternity care shared between VAHS and the health service (for women attending Joan Kirner, VAHS was not ‘local’, thus this was not the case).
Table 1.
Site descriptions.
| Site | Location, classification | Births per year (≈) | Caseload places per year (% of total births) |
Women who identified as First Nations who received caseload care prior to project # | Cultural support unit and staff positions | Aboriginal Community Controlled Health Organisation (ACCHO) ‘partner’ |
|---|---|---|---|---|---|---|
| Royal Women's Hospital* | Metropolitan, tertiary | ≈ 7500 | 500 women / year (8% of births) |
2011–2014: 6 women (0.3% of 2093 caseload places) | Badjurr-Bulok Wilam 1.5 Aboriginal Hospital Liaison Officers (AHLO) positions |
Victorian Aboriginal Health Service (VAHS) offers shared care model |
| Joan Kirner Women's and Children's Hospital | Metropolitan, tertiary | ≈ 5500 | 1100 women / year (20% of total births) | 2012–2013: 24 women (0.9% of 2744 caseload places) | Wilim Berrbang 2 AHLOs⁎⁎ 1 Koori Maternity Services worker |
Not located near an ACCHO |
| Mercy Hospital for Women | Metropolitan, tertiary | ≈ 6000 | 650 women / year (9% of total births) | 2014: 4 women (1.0% of 398 caseload places) | Nangnak Baban Murrup 2 AHLOs 2 Nangnak Wan Myeek: postnatal support workers |
VAHS offers shared care model |
| Goulburn Valley Health | Regional | ≈ 1200 | 130 (11% total births) | 2011–2014: 15 women (3.0% of 514 caseload places) | 2 AHLOs | Rumbalara offers shared care, with midwife and obstetric antenatal care available from GVH |
Data are provided for different years due to what was available from the sites.
Model commenced as part of COSMOS trial in 2008.
including a dedicated Aboriginal Hospital Liaison Officer whose role is to work with midwives to support First Nations women and their families throughout pregnancy, birth and up to eight weeks postpartum.
Description of the caseload midwifery model implemented for First Nations women
In the standard caseload model, women receive antenatal, intrapartum and postpartum care from a caseload midwife with one or two antenatal visits conducted by a ‘back-up’ midwife (so they are also ‘known’), with midwives taking a caseload of approximately 40 to 45 women per Equivalent Full-time (EFT) per year (varies by site and by the risk profile of the caseload). The primary midwife is on-call for a woman's labour and birth and for other telephone contact except in designated circumstances such as annual leave, sick leave, having already worked >12 h in a 24 h period, having more than one woman in labour, or being off duty, when care is provided by the back-up midwife, or on occasion, by core staff.14 Collaboration with obstetricians and other health professionals is as needed.
In this study, caseload care was provided in conjunction with existing supports provided through community- and hospital-based First Nations health services and tailored at each site and for individual women. All women having a First Nations baby were eligible to be offered the model, regardless of risk factors. The model was designed to enhance, not replace, existing systems, to further close care gaps. The aim was that no matter where a woman chose to have most of her pregnancy care, she was linked with, and had 24/7 phone access to, a known caseload midwife who was her primary care provider for the hospital components of her care. Care could be solely hospital-based, with all care by the caseload midwife, or shared care between the caseload midwife and other specialised hospital service, e.g. maternal fetal medicine unit, obstetric team etc. Care could also be caseload care shared with a community-based provider e.g. a local Aboriginal Health Service or General Practitioner. It was expected that the caseload for each midwife would be slightly less than standard caseload if/where women had more complex needs.
All caseload midwives, managers, and some obstetric staff working within the model of care participated in-house cultural training as well as cultural safety training in First Nations health conducted by VACCHO, including face-to-face and online. The aim of the training was to assist staff to understand the impact of colonial history on First Nations people and the context of women's lives and to explore how to work effectively with First Nations people and their communities. It included information on working with the Victorian First Nations community health sector, and on closing the health gap between First Nations and non-First Nations people. During the project the caseload midwives liaised regularly with the Aboriginal Hospital Liaison Officers (AHLOs) to facilitate the best outcomes for women.
Operationalising the model at the study sites
Each participating health service had a steering committee to oversee project implementation and provide governance, and a smaller working group to develop and implement the model. Steering committees met four to five times each year on average, and included key hospital staff such as maternity managers, manager of Aboriginal programs, Koori Maternity Service (KMS) staff, and social work representation, along with some of the project investigators, a First Nations research midwife, hospital research midwives and the project co-ordinator. Working groups included staff relevant to implementation, e.g. caseload manager, clinic manager, research midwives.
Sample size considerations
There was no sample size calculation for this aspect of the overall study. This population-based study aimed to see if the sites could implement the model as planned and offer it to all women having a First Nations baby.
Outcome measures
Number and percentage of women having a First Nations baby who:
-
•
Were identified, then offered caseload midwifery care at the hospital booking visit or later in pregnancy;
-
•
Enrolled in the model;
-
•
Received caseload midwife care during pregnancy and remained in the model for labour, birth and postnatal care.
All women having a First Nations baby were eligible. There were no exclusion criteria.
Data collection
Research midwives at each site educated staff about the study and reinforced the importance of identification of First Nations women and babies (with site AHLOs), collected data to meet the study aims, and recruited women to the embedded evaluation of women's views and experiences (study Aim 2, reported elsewhere). Data collection forms were developed to record the number of eligible women identified, then, of those, the number that were (a) offered the caseload model; (b) enrolled in the model; and (c) received it. These data are not routinely collected. Data were collected from clinic booking schedules, routine data sets, the caseload midwives’ records etc.
Statistical analysis
Data were recorded on Excel spreadsheets, then data cleaning and analysis were undertaken in STATA 17. Data cleaning included range, logic and missing data checks. Analysis was first by site, then combined, with site identifiers included. Quantitative data were summarised using frequencies and percentages for categorical data and means and standard deviations calculated for continuous data.
Ethics
Ethics approval was granted by St Vincent's Hospital (16\SVHM\233), La Trobe University (HREC 195/16) and all partner organisations. Multi-institutional agreements were signed by each partner organisation and the study conducted in accordance with National Guidelines for Ethical Conduct in Aboriginal and Torres Strait Islander Research.24
Role of the funding source
The funders of the study had no role in study design, collection, analysis, and interpretation of data nor any role in the writing of this paper. All authors had full access to the data, and contributed to data interpretation. FMc, HMc, DF and TS prepared the data and did the statistical analysis. All authors contributed to manuscript revisions and accept responsibility to submit for publication.
Results
Caseload implementation and uptake
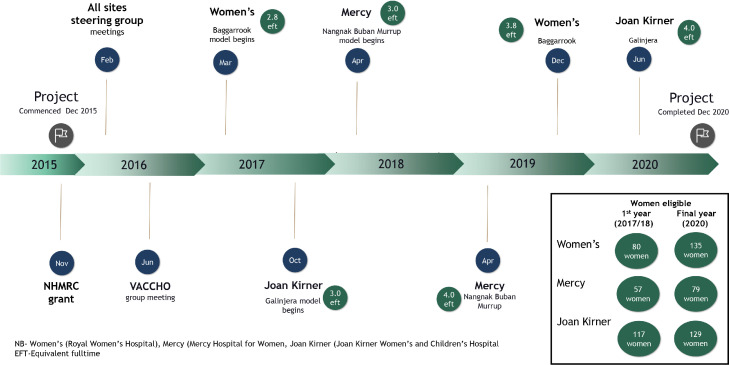
Three of the four partner sites successfully implemented the new, culturally specific caseload models during the study implementation period, which commenced in March 2017 (Figure 1), and all three sites sustained and continued the caseload model to the completion of data collection in December 2020. Table 2 shows model implementation by site, including midwife EFT and staff turnover, along with caseload size, and Figure 1 shows the implementation timeline.
Figure 1.
Baggarrook Yurrongi project timeline.
NB- Women's (Royal Women's Hospital), Mercy (Mercy Hospital for Women, Joan Kirner (Joan Kirner Women's and Children's Hospital. EFT-Equivalent fulltime.
Table 2.
Pregnancy models of care
| Mercy n=242 |
Joan Kirner n=387 |
Women's n=411 |
Total n=1040 |
|||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| First Nations women*offered culturally specific model | 211 | 87.2 | 304 | 78.6 | 329 | 80.0 | 844 | 81.2 |
| Accepted | 198 | 93.8 | 258 | 85.0 | 302 | 91.8 | 758 | 89.8 |
| Accepted & awaiting first appointment (as at end of data collection period) | 2/198 | 1.0 | 10/258 | 3.8 | 0 | 0 | 12/758 | 1.6 |
| Accepted & received (n=196, n=248, n=302, total n=746) | 192/196 | 98.0 | 191/248 | 77.0 | 280/302 | 92.7 | 663/746 | 88.9 |
| Transferred care to other hospital before accepting/declining | 0 | 0 | 2 | 0.65 | 0 | 0 | 2 | 0.2 |
| Declined | 13 | 6.2 | 44 | 14.5 | 27 | 8.2 | 84 | 10.0 |
| First Nations women*NOT offered culturally specific model | 31 | 12.8 | 83 | 21.4 | 82 | 20.0 | 196 | 18.8 |
| Family identified but model not offered by staff | 12 | 5.0 | 53 | 13.7 | 30 | 7.3 | 95 | 9.1 |
| Not documented as First Nations until after birth | 17 | 7.0 | 7 | 1.8 | 28 | 6.8 | 52 | 5.0 |
| Booked or /transferred from other hospital later in pregnancy, unable to access model | 1 | 0.4 | 3 | 0.8 | 17 | 4.1 | 21 | 2.0 |
| Transferred care out, prior to model offered | 1 | 0.4 | 7 | 1.8 | 4 | 1.0 | 12 | 1.2 |
| Other (e.g. pregnancy loss) | 0 | 0 | 13 | 3.4 | 3 | 0.7 | 16 | 1.5 |
| Total First Nations women*receiving culturally specific model | 192 | 79.3 | 191 | 49.4 | 280 | 68.2 | 663 | 63.8 |
| Nangnak/Galinjera/Baggarrook ⁎⁎caseload midwife only care | 127/192 | 66.1 | 89/191 | 46.6 | 111/280 | 39.6 | 327/663 | 49.3 |
| Nangnak/Galinjera/Baggarrook shared care with hospital team⁎⁎⁎ (total) | 35/192 | 18.2 | 102/191 | 53.4 | 141/280 | 50.4 | 278/663 | 41.9 |
| General obstetrics | 15/192 | 7.8 | 65/191 | 34.0 | 12/280 | 4.3 | 92/663 | 13.9 |
| Perinatal medicine | 16/192 | 8.3 | 17/191 | 8.9 | 56/280 | 20.0 | 89/663 | 13.4 |
| Drug and alcohol service | 4/192 | 2.1 | 0 | 0 | 36/280 | 12.9 | 40/663 | 6.0 |
| Endocrinology | 0 | 0 | 20/191 | 10.5 | 14/280 | 5.0 | 34/663 | 5.1 |
| Young Women's clinic | 0 | 0 | NA | NA | 14/280 | 5.0 | 14/663 | 2.1 |
| Women with individual needs | NA | NA | NA | NA | 9/280 | 3.2 | 9/663 | 1.4 |
| Nangnak/Galinjera/Baggarrook shared care in community | 30/192 | 15.6 | 0 | 0 | 28/280 | 10.0 | 58/663 | 8.7 |
| Shared care model with Victorian Aboriginal Health Service (VAHS) | 29/192 | 15.1 | NA | NA | 28/280 | 10.0 | 57/663 | 8.6 |
| Shared care model with General Practitioner | 1/192 | 0.5 | 0 | 0 | 0 | 0 | 1/663 | 0.2 |
| Total First Nations women*receiving other caseload care (i.e., not culturally specific model) | 3 | 1.3 | 32 | 8.4 | 5 | 1.2 | 40 | 3.9 |
| Total First Nations women*receiving any caseload model of care | 195 | 80.6 | 223 | 57.6 | 285 | 69.3 | 703 | 67.6 |
| Model of care received if not in Nangnak/Galinjera/Baggarrook or standard caseload model | 45 | 18.6 | 154 | 39.8 | 126 | 30.7 | 325 | 31.3 |
| General obstetric care | 23 | 9.6 | 86 | 22.2 | 0 | 0 | 109 | 10.5 |
| Perinatal medicine/ Fetal Management Unit | 8 | 3.3 | 25 | 6.5 | 40 | 9.7 | 73 | 7.0 |
| Standard hospital care (mostly midwife care if medically low risk) | 2 | 0.8 | 8 | 4.0 | 60 | 14.6 | 70 | 6.7 |
| Drug and alcohol service | 9 | 3.8 | NA | NA | 15 | 3.6 | 24 | 2.3 |
| Shared care with General Practitioner | 0 | 0 | 2 | 0.5 | 6 | 1.5 | 8 | 0.8 |
| Young Women's clinic | 2 | 0.8 | NA | NA | 4 | 1.0 | 6 | 0.6 |
| Hospital community/satellite clinic | 0 | 0 | 2 | 0.5 | 1 | 0.2 | 3 | 0.3 |
| Incarcerated ⁎⁎⁎⁎ | NA | NA | 20 | 5.2 | NA | NA | 20 | 1.9 |
| Transferred care prior to model allocation | 1 | 0.4 | 11 | 2.8 | 0 | 0 | 12 | 1.2 |
| Other pregnancy booking information | ||||||||
| Direct referral from a local Aboriginal Community Controlled Organisation | 33 | 13.6 | 0 | 0 | 67 | 16.3 | 100 | 9.6 |
| Gestation at booking visit, weeks (mean, sd, (range)) (n=240, n=387, n=409, total n=1036) | 17.5 | 5.7 (6.5, 37) | 18.9 | 6.8 (8.5,39.7) | 20.5 | 6.9 (6.8,39.8) | 19.2 | 6.7 (6.5,39.8) |
| Booking appointment by midwife from Nangnak/Galinjera/Baggarrook | 82 | 34.0 | 25 | 6.5 | 63 | 15.3 | 170 | 16.4 |
Includes women having a First Nations baby.
Site names for culturally specific models Nangnak/Galinjera/Baggarrook,
as main speciality team, care may have involved more than one team,
Care provided by visiting midwife (caseload not available), NA=Not Applicable.
Goulburn Valley Health (GVH) was committed to offering all First Nations women culturally specific caseload care, and met with the investigator team many times over the study period with meetings at the hospital and Rumbalara, the local Aboriginal Community Controlled Health Organisation (ACCHO). A steering group with broad key stakeholder representation was formed early in the study period, which included the Divisional Operational Director of Women's and Children's Services, the Maternity Services Director, the hospital AHLOs, Aboriginal health staff from Rumbalara, two local Chief Investigators and other members of the research team. Despite this, and the comprehensive preparation for model implementation (such as obtaining site specific ethics approval, ongoing site and key personnel meetings with Rumbalara, and appointment of a research midwife), ongoing acute and chronic staffing crises in maternity services at the hospital precluded model implementation. The data below therefore do not include GVH.
At the three implementation sites, all midwives appointed to the roles received cultural competency training, and all sites implemented education for staff more broadly regarding internal referral pathways, identification processes and data integrity i.e., the importance of accurately documenting the First Nations status of mothers and babies. There was regular engagement between the caseload midwives and all the relevant internal and external key stakeholders, e.g., the First Nations teams in the hospitals, and external midwives and other health care professionals. Midwives and managers from the Women's and Mercy regularly met with staff from VAHS to build on the relationship and enhance communication, with the caseload midwives being the hospital point of contact for the VAHS staff. Approximately 10% of women were directly referred into the model from their local ACCHO.
First nations women and babies who received caseload care
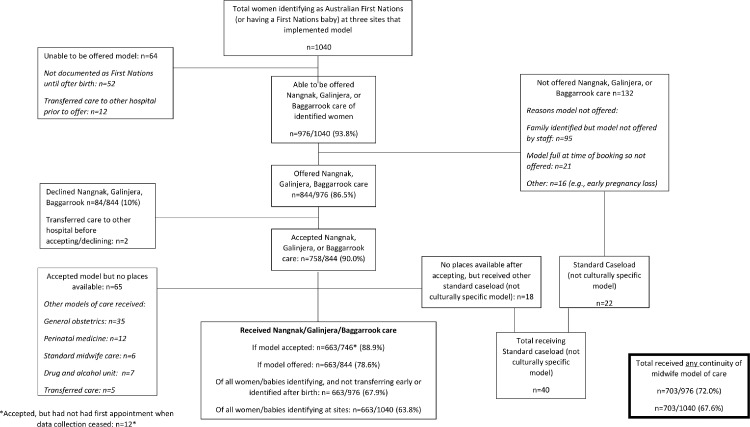
During the program implementation period (March 2017 to December 2020), 1040 women having a First Nations baby) were identified at the three sites (Figure 2, Tables 3 and 4). Approximately 70% of mothers identified as Aboriginal and/or Torres Strait Islander, the majority as Aboriginal (Table 4). Of the two sites which documented the father's First Nation status, 39.1% identified as Aboriginal and/or Torres Strait Islander, with >90% of these being Aboriginal. At the Women's the baby (not the father's) First Nations status was recorded during the antenatal period.
Figure 2.
Pregnancy care pathway for women having a First Nations baby.
*Accepted, but had not had first appointment when data collection ceased: n = 12.*
Table 3.
Model implementation by site.
| Site | Date commenced | Name of model | Midwife EFT 1st year | Mothers eligible for model 1st year | Midwife EFT end final year(2020) | Mothers eligible for model final year (2020) | Caseload of women per year | Staff exiting modeld |
|---|---|---|---|---|---|---|---|---|
| Women's | March 2017 | Baggarrook - ‘Woman’ in Woiwurrung language | 2.8 EFTa (3 mws) |
80 | 3.8 EFT (4 mws) |
135 | 1.0 EFT- 40 0.8 EFT- 35 |
4 (1 retired) |
| Joan Kirner | October 2017 | Galinjera - ‘To come together and connect and love’ in Wemba language | 3.0 EFTb | 117 | 4.0 EFT | 129 | 1.0 EFT - 35 | 5 |
| Mercy | April 2018 | Nangnak Babun Murrup - ‘Nurturing Mother's Spirit’ in Woiwurrung language | 3.0 EFTc | 57 | 4.0 EFT | 79 | 1.0 EFT 40–45 (including leave relief) | 1 (maternity leave) |
2.8 Equivalent fulltime (EFT) = 3 midwives, one of the four pre-existing caseload groups adapted; b: used EFT from an existing caseload group (2 EFT initially, another EFT added within two months due to high demand); c: newly configured group reallocated from of existing caseload EFT; d: Women's – one midwife stayed all through project and another stayed from when she joined the model until the end, Joan Kirner had 100% midwife turnover, Mercy – all three midwives who commenced stayed in model (one had maternity leave – and her replacement did not leave the model).
Table 4.
Identification of First Nations mothers and fathers, as documented in maternal medical record.
| Mercy n = 242 | Joan Kirner n = 387 | Women's n = 411 | Total n = 1040 | |||||
|---|---|---|---|---|---|---|---|---|
| MOTHER | n | % | n | % | n | % | n | % |
| Mother identifies as either Aboriginal and/or Torres Strait Islander | 184 | 76.0 | 249 | 64.3 | 298 | 72.5 | 731 | 70.2 |
| Mother Aboriginal | 169/184 | 91.8 | 227/249 | 91.2 | 274/298 | 91.9 | 670/731 | 91.7 |
| Mother Torres Strait Islander | 5/184 | 2.7 | 9/249 | 3.6 | 10/298 | 3.6 | 24/731 | 2.3 |
| Mother both Aboriginal and Torres Strait Islander | 10/184 | 5.4 | 13/249 | 5.2 | 14/298 | 4.7 | 37/731 | 3.6 |
| Mother identifies as neither Aboriginal nor Torres Strait Islander | 58 | 24.0 | 138 | 35.7 | 113 | 27.5 | 309 | 29.8 |
| FATHER | ||||||||
| Father identifies as either Aboriginal and/or Torres Strait Islander | 87 | 36.0 | 159 | 41.1 | ⁎⁎ | ⁎⁎ | 246 | 39.1 |
| Father Aboriginal | 83/87 | 95.4 | 141/159 | 88.7 | ⁎⁎ | ⁎⁎ | 224 | 91.1 |
| Father Torres Strait Islander | 0 | 0 | 92/159 | 5.7 | ⁎⁎ | ⁎⁎ | 9 | 3.7 |
| Father both Aboriginal and Torres Strait Islander | 4/87 | 4.6 | 9/159 | 5.7 | ⁎⁎ | ⁎⁎ | 13 | 5.3 |
| Father identifies as neither Aboriginal nor Torres Strait Islander | 122 | 50.4 | 128 | 33.1 | ⁎⁎ | ⁎⁎ | 250 | 39.8 |
| Father's status not documented | 33 | 13.6 | 100 | 25.8 | ⁎⁎ | ⁎⁎ | 133 | 21.3 |
At the Women's the baby's and not the baby's father's identification information is routinely collected.
A small number of women transferred to another hospital before being allocated to a model of care (n = 12), and some were not documented as First Nations until after birth (n = 52) (Table 2, Figure 2). Of the 976 remaining women, 86.5% (844/976) were offered care in the model. Some women were not offered the model or referred by hospital staff (9.7%, 95/976) and in a few cases (2.2%, 21/976) there were no places available in the model. Almost all women who were offered the culturally specific model accepted it (758/844; 90%), with the remainder choosing other models of care (Figure 2). Of the 758 women who accepted the model, 87.5% (663/758) received it. The most frequent reason for not receiving the model (after accepting it) was that there were no places available i.e. the midwives’ caseloads were full for the month (n = 83), although 18 of these women were subsequently offered midwifery caseload care in the standard hospital caseload program. For the remaining women (n = 65), most received standard hospital care including specialist obstetric or perinatal care (n = 47), standard midwife care (n = 6), care in the drug and alcohol unit (n = 7), or had their care transferred elsewhere (n = 5).
In total, 663 of 1040 women (63.8%) having a First Nations baby received the culturally specific caseload model and another 40 women received standard caseload, therefore 67.6% of all the identified women received caseload care (703/1040). Excluding those women who transferred to another hospital before the model could be offered, or who were not identified until after birth, 67.9% (663/976) received the culturally specific caseload model and 72.0% received any caseload care (703/976).
For women who received the culturally specific caseload model, care was exclusively within the model, or shared with other hospital and community-based models. Approximately half of the women (49%) had caseload care solely with their primary or back up midwife in the culturally specific models - Nangnak Buban Murrup (Mercy Hospital), Galinjera (Joan Kirner Hospital), or Baggarrook (the Women's) with no scheduled shared care with another provider. A further 41.9% (n = 605 women) had hospital-based collaborative care, i.e., caseload care shared with another specialist team at the respective hospital, including obstetrics, perinatal medicine, drug and alcohol, endocrinology, young women's clinic, and a clinic for women with a disability (Table 2). A small percentage of women (n = 58/663, 8.7%) had community-based shared care, and their caseload midwife was their primary hospital-based care provider, with the number of each varying by individual need and choice). Of these, 57 women had shared care with VAHS (on site, and midwife-led) and one woman with her GP. The VAHS midwife aimed to visit women in hospital, after the birth, to help with the transition back to VAHS care. Where women needed transport to attend pregnancy appointments VAHS was often able to organise and provide transport (for VAHS, Mercy or Women's), and alternatively, when needed, all sites provided support to access transport, e.g., cab vouchers, parking vouchers, public transport cards. At two hospitals there were dedicated social workers linked to the new model. One hospital ran a ‘Yarning Circle’ facilitated by the AHLO and the caseload midwives, where mothers could meet to ‘yarn’ (informally discuss/chat) about pregnancy, birth and parenting while doing craft and artwork.
At the completion of data collection (December 31st 2020) 32/663 (4.8%) women who had pregnancy care in the culturally specific caseload model gave birth elsewhere, 48/663 (7.2%) had not yet given birth, and 2/663 (0.3%) had opted to leave the model. All other women allocated to the model had pregnancy care, gave birth and had postnatal care in the model, with a varying number of pregnancy visits with their caseload midwife depending on gestation at booking and amount of collaborative care required.
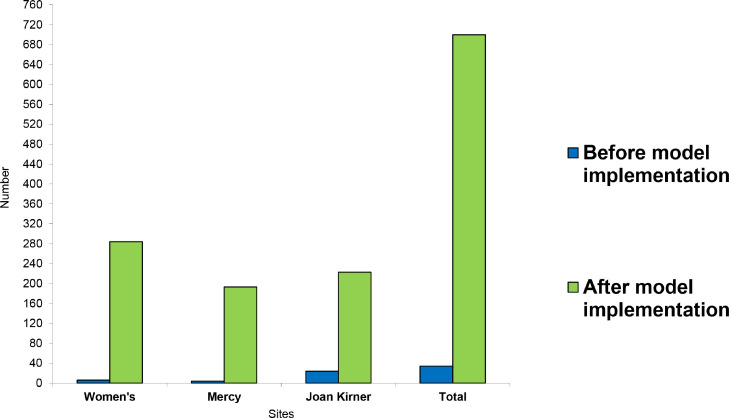
Figure 3 shows the number of First Nations women receiving caseload care before and at the end of the project at the implementation sites.
Figure 3.
Number of women having a First Nations baby who received caseload (before and after program implementation).
Before program implementation – blue; after program implementation – green.
Discussion
This implementation study demonstrated how three metropolitan tertiary maternity services in Melbourne, Australia, successfully translated gold standard evidence into practice on a large scale. Working collaboratively with all study partners, the sites successfully implemented a culturally responsive caseload midwifery model for women having a First Nations baby resulting in a 21-fold increase in access to this model for First Nations women from March 2017 to December 2020. In total, 703 women received caseload midwifery care during project implementation (663 in culturally specific caseload, and 40 in standard caseload) compared to only 34 First Nations women ever receiving caseload midwifery at the three sites previously.
Successful and timely translation of evidence into practice is rare and there is an urgent need to translate knowledge produced. For First Nations communities, this is even more so; uptake of western research evidence is limited due to factors such as lack of involvement of First Nations communities, lack of trust, and limited relevance for First Nations communities.24 This study was able to overcome these challenges in three of the four sites.
Despite many attempts to implement the model in the regional hospital, this was not achieved. Contributing factors in research translation failure include poor communication; lack of stakeholder engagement, funding, and technical expertise; resistance to change; and a lack of planning and effort in relation to evidence scale-up.25,26 In this case, the reasons for non-implementation were likely multifactorial. Arguably there was adequate technical expertise to achieve the outcome (the caseload model was already operational at the health services), there was planning, local leadership and a governance structure set up for the project, including a steering committee that met regularly. Analysis of project meeting minutes demonstrates this ongoing commitment to program implementation, however the hospital had ongoing major staffing issues that are not unusual for regional and rural maternity services.27 It is also possible that the smaller size of the unit made a difference and especially given the often poorer resourcing of rural health services.28 There may also have been other unseen and unspecified barriers that will be further elucidated following analyses of key stakeholder interview data (to be reported elsewhere).
Key contributors to the successful model implementation at the other three sites include being a First Nations’ community-driven and endorsed, collaborative project that included significant input and commitment from each partner organisation, having a research team with significant technical expertise in implementing caseload models, and funding to support the process. Engagement with all key stakeholders was critical. The partnership with VACCHO was a key driver (the project was initiated following an approach from VACCHO to partner on the initiative), and ensured high level input in the development and implementation of the work. There was First Nations community leadership on the investigator team, and an Aboriginal Advisory Committee to provide cultural guidance and oversight, and to promote community engagement. Steering committee members from the participating health services, along with senior project investigators, met regularly throughout the project to monitor program implementation. Engagement with VAHS and KMS was critical as they are key providers of maternity care, and in this instance continued to provide shared care for 8.6% of women in the caseload model. This adaptation of the caseload model to enable shared care with the ACCHO sector enabled effective integration of the hospital- and community-based services without significant duplication of services, and decreased the chance of women ‘falling through the cracks’, as the model enhanced communication and co-ordination between hospital and community services. This type of partnership approach has long been advocated by both government and the First Nations community-controlled sector, and is considered to be a fundamental component of any strategy for improving health outcomes for First Nations people.21,29 Similar to our study, a recent study that explored stakeholder experiences in establishing an Aboriginal-Mainstream partnership in Queensland found that key factors for success were trusting relationships, maintaining flexibility in service provision and planning, clear expectations and distinction of staff roles and responsibilities, a shared vision, committed leadership, and engaging all staff in the process.29
The successful implementation of the culturally responsive program is consistent with the 2019 Australian National Strategic Directions for Australian Maternity Services that recommends the development and implementation of culturally safe, evidence-based models of care in partnership with First Nations people and communities,30 enabled through utilisation of a ‘Birthing on Country Service Model and Evaluation Framework’ which includes engagement and governance as being important in model design, services co-designed with community, including continuity of midwifery care, First Nations workforce inclusion, partnerships with primary and tertiary services, and cultural strengthening programs. Given the challenges of implementation of complex interventions such as ‘Birthing on Country’ services, Kildea and colleagues have developed a framework to guide implementation of models of care like that implemented in this study. It allows for customisation of the model to the local community context through a participatory action process, enabled by strong partnerships and leadership from First Nations people and ACCHOs.22
The three sites that implemented the model, all reallocated resources (EFT) from existing caseload models, and it may be that this ability does make it easier to implement such a model. It follows that this reallocation of resources potentially reduces the caseload places available for non-First Nations women, and moves the benefits of the model to those First Nations families who access it. In this study we do not know if the non-First Nations women who missed out were equally ‘at risk’, such as other socially vulnerable groups, but it is our view that the caseload model needs to be scaled up more broadly, and available to all women. While the proportion of women having a First Nations baby increased over the study period (254 women identified in the first 12 months for combined sites compared to 343 in final 12 months, a 35% increase) we cannot determine if this simply reflects more close attention to identification – all sites had research midwives employed to coordinate the study on site, and education and follow-up regarding identification was a major aspect of the role.
In Australia, there has been a lack of access to, and availability of, culturally responsive maternity services for First Nations women and babies and to caseload midwifery. This study has demonstrated the ability of three large, metropolitan maternity services to implement caseload midwifery for First Nations women, with cultural competency training for all participating midwives, and services sustained and popular over three to four years. Ninety percent model uptake meant an exponential (21-fold) increase in the number of First Nations women receiving caseload midwifery at the three sites during the study period. Early and ongoing consultation, collaboration and engagement with key First Nations community stakeholders was crucial to the success of the programs. The model has enabled First Nations women to have a known midwife in the hospital system, who is there for them for all parts of their maternity care – a model that has built on existing initiatives in a responsive and individualised way. The findings support government policies that have recommended the development and implementation of culturally safe, evidence-based models of care that have been developed in partnership with First Nations communities and underpinned by ‘Birthing on Country’ principles. The expansion of this model should be prioritised, with further research focused on understanding key features of sustaining the model and continuing to bridge the partnership between First Nations and mainstream health services.
Contributors
HMc and DF conceived the project. All authors contributed to study design. HMc, DF, RH and RM undertook the literature review. HMc, DF, SK, CC, MJ, JB, JR, JF, JO, SJ, NB, KF, LG, JW and MN all contributed to writing the initial funding application. FMc, HMc, DF and TS prepared and verified the data and did the statistical analysis. All authors had full access to the data, and contributed to data interpretation. HMc and DF wrote the first draft of the manuscript. All authors contributed to manuscript revisions and accept responsibility to submit for publication.
Funding
Partnership Grant (# 1110640), Australian National Health and Medical Research Council and La Trobe University.
Data sharing
Data collected for the study that contributed to this paper, including de-identified individual data and a data dictionary defining each field in the set, will be made available to others after publication of the paper for use by other researchers for further analysis unspecified in the Baggarrook Yurrongi publication plan, with investigator support, after ethical approval including scientific review of a proposal, and with a signed data access agreement.
Declaration of interests
We declare there are no competing interests.
Acknowledgments
We gratefully acknowledge the First Nations families who participated in the program as well as staff at the Victorian Aboriginal Community Controlled Health Organisation, Goulburn Valley Health, the Mercy Hospital for Women, including the Nangnak Baban Murrup team, Joan Kirner Hospital, including the Wilim Berrbang team, and the Royal Women's Hospital, including the Badjurr-Bulok Wilam team. Thank you also to the Victorian Aboriginal Health Service and Rumbalara Aboriginal Co-operative. We would also like to thank the members of our Aboriginal Advisory Committee (including elders Aunty Di Kerr, Aunty Doseena Fergie), and Shawana Andrews for the project artwork. Thank you also for the generous naming of the programs in traditional language by Aunty Di Kerr (‘Baggarrook Yurrongi’ ‘Woman's Journey’ in Woiwurrung language) and Skye Stewart (‘Galinjera’; Wemba language meaning to come together and connect and love). We would also like to acknowledge members of the steering committees and working groups at the respective health services as well as research midwives Zoe Lock, Ingrid Holmes, Lynnelle Moran, Clare Robinson, and Frances Hearn. We are grateful for the funding from the Australian National Health and Medical Research Council that allowed us to conduct this study.
References
- 1.Australian Government. National Aboriginal Torres Strait Islander Health Plan 2013–2023. Canberra: Commonwealth of Australia; 2013.
- 2.Commonwealth of Australia. Closing the gap Prime Minister's Report. In: Department of the Prime Minister and Cabinet, editor. Canberra; 2020.
- 3.Australian Institute of Health and Welfare. Australia's Mothers and Babies. Canberra; 2021.
- 4.Jongen C., McCalman J., Bainbridge R., Tsey K. Aboriginal and Torres Strait Islander maternal and child health and wellbeing: a systematic search of programs and services in Australian primary health care settings. BMC Pregnancy Childbirth. 2014;14:251. doi: 10.1186/1471-2393-14-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Department of Health. Woman-centred care: strategic directions for Australian maternity services, In: COAG Health Council, editor. 2019.
- 6.Department of Health. Koolin Balit, Victorian government strategic directions for aboriginal health 2012–2022. Melbourne: State of Victoria; 2012.
- 7.Department of Health and Human Services. Korin Korin Balit-Djak Aboriginal Health, wellbeing and safety strategic plan 2017–2027. Melbourne, 2017.
- 8.Barclay L., Kruske S., Bar-Zeev S., et al. Improving Aboriginal maternal and infant health services in the 'Top End' of Australia; synthesis of the findings of a health services research program aimed at engaging stakeholders, developing research capacity and embedding change. BMC Health Serv Res. 2014;14:241. doi: 10.1186/1472-6963-14-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertilone C., McEvoy S. Success in closing the gap: favourable neonatal outcomes in a metropolitan Aboriginal Maternity Group Practice Program. Med J Aust. 2015;203(6):262. doi: 10.5694/mja14.01754. e1-7. [DOI] [PubMed] [Google Scholar]
- 10.Kildea S., Gao Y., Hickey S., et al. Effect of a Birthing on Country service redesign on maternal and neonatal health outcomes for First Nations Australians: a prospective, non-randomised, interventional trial. Lancet Glob Health. 2021;9(5):e651–e6e9. doi: 10.1016/S2214-109X(21)00061-9. [DOI] [PubMed] [Google Scholar]
- 11.Corcoran P.M., Catling C., Homer C.S. Models of midwifery care for Indigenous women and babies: a meta-synthesis. Women Birth. 2017;30(1):77–86. doi: 10.1016/j.wombi.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Hickey S., Roe Y., Gao Y., et al. The Indigenous Birthing in an Urban Setting study: the IBUS study: a prospective birth cohort study comparing different models of care for women having Aboriginal and Torres Strait Islander babies at two major maternity hospitals in urban South East Queensland, Australia. BMC Pregnancy Childbirth. 2018;18(1):431. doi: 10.1186/s12884-018-2067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kildea S., Gao Y., Rolfe M., et al. Remote links: redesigning maternity care for Aboriginal women from remote communities in Northern Australia – a comparative cohort study. Midwifery. 2016;34:47–57. doi: 10.1016/j.midw.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 14.McLachlan H., Forster D., Davey M., et al. Effects of continuity of care by a primary midwife (caseload midwifery) on caesarean section rates in women of low obstetric risk: the COSMOS randomised controlled trial. BJOG. 2012;119(12):1483–1492. doi: 10.1111/j.1471-0528.2012.03446.x. [DOI] [PubMed] [Google Scholar]
- 15.Forster D.A., McLachlan H.L., Davey M.A., et al. Continuity of care by a primary midwife (caseload midwifery) increases women's satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth. 2016;16:28. doi: 10.1186/s12884-016-0798-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tracy S.K., Hartz D.L., Tracy M.B., et al. Caseload midwifery care versus standard maternity care for women of any risk: M@NGO, a randomised controlled trial. Lancet. 2013;382(9906):1723–1732. doi: 10.1016/S0140-6736(13)61406-3. [DOI] [PubMed] [Google Scholar]
- 17.Sandall J., Soltani H., Gates S., Shennan A., Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2016;4 doi: 10.1002/14651858.CD004667.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dawson K., McLachlan H., Newton M., Forster D. Implementing caseload midwifery: exploring the views of maternity managers in Australia - a national cross-sectional survey. Women Birth. 2016;29(3):214–222. doi: 10.1016/j.wombi.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Brown S.J., Weetra D., Glover K., et al. Improving Aboriginal women's experiences of antenatal care: findings from the Aboriginal families study in South Australia. Birth. 2015;42(1):27–37. doi: 10.1111/birt.12143. [DOI] [PubMed] [Google Scholar]
- 20.Sivertsen N., Anikeeva O., Deverix J., Grant J. Aboriginal and Torres Strait Islander family access to continuity of health care services in the first 1000 days of life: a systematic review of the literature. BMC Health Serv Res. 2020;20(1):829. doi: 10.1186/s12913-020-05673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Middleton P., Bubner T., Glover K., et al. Partnerships are crucial': an evaluation of the Aboriginal Family Birthing Program in South Australia. Aust N Z J Public Health. 2017;41(1):21–26. doi: 10.1111/1753-6405.12599. [DOI] [PubMed] [Google Scholar]
- 22.Kildea S., Hickey S., Barclay L., et al. Implementing birthing on country services for aboriginal and Torres Strait Islander families: RISE framework. Women Birth. 2019;32(5):466–475. doi: 10.1016/j.wombi.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Kildea S., Tracy S., Sherwood J., Magick-Dennis F., Barclay L. Improving maternity services for Indigenous women in Australia: moving from policy to practice. Med J Aust. 2016;205(8):374–379. doi: 10.5694/mja16.00854. [DOI] [PubMed] [Google Scholar]
- 24.National Health and Medical Research Council . National Health and Medical Research Council; Canberra: 2018. Ethical Conduct in Research with Aboriginal and Torres Strait Islander Peoples and communities: Guidelines for Researchers and Stakeholders. [Google Scholar]
- 25.Martin K., Mullan Z., Horton R. Overcoming the research to policy gap. Lancet Glob Health. 2019;7(Suppl 1):S1–S2. doi: 10.1016/S2214-109X(19)30082-8. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Nine steps for developing a scaling-up strategy, 2010.
- 27.Barclay L., Kornelsen J. The closure of rural and remote maternity services: where are the midwives? Midwifery. 2016;38:9–11. doi: 10.1016/j.midw.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Longman J., Kornelsen J., Pilcher J., et al. Maternity services for rural and remote Australia: barriers to operationalising national policy. Health Policy. 2017;121(11):1161–1168. doi: 10.1016/j.healthpol.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 29.Hickey S., Couchman K., Stapleton H., Roe Y., Kildea S. Experiences of health service providers establishing an Aboriginal-Mainstream partnership to improve maternity care for Aboriginal and Torres Strait Islander families in an urban setting. Eval Program Plan. 2019;77 doi: 10.1016/j.evalprogplan.2019.101705. [DOI] [PubMed] [Google Scholar]
- 30.Council of Australian Governments Health Council. Woman-Centred Care: Strategic Directions for Australian Maternity Services. Canberra ACT: Department of Health.