Abstract
Depression is a significant cause of disability and affects millions worldwide; however, antidepressant therapies often fail or are inadequate. Current medications for treating major depressive disorder can take weeks or months to reach efficacy, have troubling side effects, and are limited in their long-term capabilities. Recent studies have identified a new set of glutamate-based approaches, such as blood glutamate scavengers, which have the potential to provide alternatives to traditional antidepressants. In this review, we hypothesize as to the involvement of the glutamate system in the development of depression. We identify the mechanisms underlying glutamate dysregulation, offering new perspectives on the therapeutic modalities of depression with a focus on its relationship to blood–brain barrier (BBB) permeability. Ultimately, we conclude that in diseases with impaired BBB permeability, such as depression following stroke or traumatic brain injury, or in neurogenerative diseases, the glutamate system should be considered as a pathway to treatment. We propose that drugs such as blood glutamate scavengers should be further studied for treatment of these conditions.
Keywords: blood–brain barrier, blood glutamate scavengers, depression, glutamate
1. Introduction
Major depressive disorder (MDD) is a significant contributor to the development of disability [1]. Projections by the World Health Organization predict that depression will be the highest ranked cause of disease burden in middle- and high-income countries by the year 2030 [1,2]. In the United States, the prevalence of depression has been estimated at 17% [3]. Nearly two dozen distinct antidepressant medications involving monoaminergic systems are in use today [4]. These medications, though, have limited effectiveness, with many failing to provide long-term remission for patients [5]. Often, treatments do not begin to work until weeks or months of administration [6]. Side effects of antidepressants are common and significantly reduce the quality of life of patients [4,7]. New antidepressants that work quickly and effectively are necessary, especially for patients whose depression is not fully mitigated by traditional monoaminergic antidepressants. Conditions that have depression as a co-morbidity include subarachnoid hemorrhage, acute ischemic stroke, intracerebral hemorrhage (ICH) or traumatic brain injury (TBI), as well as chronic neurological conditions, such as Parkinson’s disease, Alzheimer’s disease, epilepsy, multiple sclerosis and schizophrenia.
Recent studies have reported on a promising new group of drugs called glutamate-based antidepressants, which have the potential to act in ways that traditional antidepressants cannot. In this review, we provide evidence for the involvement of the glutamate system in the development of depression. We specifically examine the disruption of the glutamate efflux through the blood–brain barrier (BBB). The purpose of this manuscript is to evaluate the glutamate theory and offer new perspectives on the therapeutic modalities of depression with a focus on BBB permeability.
2. Glutamate
Glutamate, a non-essential amino acid, is responsible for the majority of fast excitatory transmission in the brain, and another amino acid neurotransmitter, γ-aminobutyric acid (GABA), enables the majority of fast inhibitory transmission [8]. Data indicate that glutamate neurons and synapses represent the largest neurotransmitter system in the brain, besides the GABAergic system [8]. Glutamate has numerous biological functions and plays a critical role in cellular metabolism and synaptic plasticity [9,10]. Therefore, the brain is heavily regulated by glutamatergic excitatory functions, including by the GABAergic inhibitory component and neurons that release other types of neurotransmitters such as monoamines [8]. Monoamines, which regulate chemical neurotransmission, have been shown to regulate certain brain functions including sleep/wakefulness, hypothalamic activities, emotional/motivational activities mediated by limbic circuitry and value-based behaviors in the neocortex [11]. Changes in excitatory transmission that are offset by the inhibitory transmissions are the primary factors in these functions, especially in cognition and emotion.
3. Glutamatergic Hypothesis of Depression
A relationship between depression and glutamate has been firmly established for several decades [8,12,13]. The hypothesis about this relationship first emerged in the early 1990s, when antagonists of the N-methyl-D-aspartate (NMDA) ionotropic glutamate receptor were associated with antidepressant-like behaviors in mice [12]. In addition, infusion of low-dose ketamine, an NMDA receptor antagonist, was associated with substantial decreases in depressive symptoms in a human study [13]. Other glutamate receptors, including α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA), have become known as well.
More recent data continues to advance the idea that glutamate dysregulation plays a role in the biological mechanisms underlying depression [14]. Studies in animals and humans clearly show the involvement of the glutamate system in the pathophysiology of depression [8,12,13]. Several studies observed changes in glutamate levels in the blood, cerebrospinal fluid (CSF) and brains of patients with MDD. Higher glutamate levels were observed in the serum [15] of patients with MDD, and antidepressant treatment reduces those levels [16,17]. Increased glutamate levels have also been seen in the plasma of patients with MDD [18]. Depressive patients have higher glutamate levels in CSF [19] and in the frontal cortex, according to postmortem brain samples. A study by Mitani et al. determined that the relationship between plasma levels of glutamate and severity of depression was predicated on plasma levels of glutamate, in addition to levels of alanine and L-serine, as an indication of the severity of the disease [18].
The results of a recent meta-analysis of magnetic resonance spectroscopy (MRS) also support the theory of the important role of glutamatergic neurotransmission in the pathophysiology of depression [20]. Many studies indicated disrupted glutamate receptors (NMDA receptors, AMPA receptors and metabotropic glutamate receptors, or mGluR) in postmortem brain samples from individuals with MDD. In addition, positron emission tomography studies identified a reduction in the density of mGluR subtype 5 in patients with depression, which was also corroborated by a post-mortem study [21].
A reduction in the relative density of one form of a NMDA subunit in bipolar disorder and depressed patients is consistent with significant decreases in NMDA receptor density in the same series of cases, and the report of a decrease in NMDA receptor density in the frontal cortex of suicide victims [22]. An in situ hybridization study of patients with MDD showed significantly lower mRNA levels of subunits of NMDA receptors and AMPA receptors in the perirhinal cortex [23], though mRNA was not reduced in the hippocampus or entorhinal cortex. Western blotting analyses showed decreased levels of these same subunits of NMDA receptors in the anterior prefrontal cortex of patients with MDD [24]. Contradictorily, however, receptor binding assays and autoradiography in patients with MDD showed more binding of [3H]CGP39653 to a glutamate site on NMDA receptors in the hippocampus, though not in the entorhinal or perirhinal cortex [23]. Similarly, two recent reports demonstrated elevated levels of mGluR2/3 protein [25] and reduced levels of mGluR5 protein [26], which are both subtypes of mGluRs, in the prefrontal cortex of patients with MDD. Data from the selective mGluR5 antagonist [11C]ABP-688 and positron emission tomography indicate reductions in mGluR5 binding in multiple areas of the frontal, temporal and parietal cortices of patients with MDD [21]. In another meta-analysis, Luykx et al. [27] also noted region- and state-specific alterations in concentrations of glutamate and glutamine, an essential amino acid that is a result of glutamate conversion, in depression. The importance of glutamatergic neurotransmission in depression is also based on studies that showed altered glutamine concentrations despite normal glutamate levels [28,29].
As a whole, these data suggest that glutamate receptor abnormalities and changes in blood, plasma and brain glutamate levels are involved in the pathophysiology of MDD. Studies of depressive-like behavior in genetic models of deficient glutamate function and advances in the treatment of MDD with glutamate-based antidepressants strongly support this theory [30,31,32].
4. Depression and the BBB
Based on this theory of the involvement of glutamate in the development of depression, an increase in the concentration of brain glutamate is a significant factor in the development of depression. Here, we identify some potential mechanisms that lead to elevated brain glutamate levels. Some evidence shows that depression is a consequence of a destruction of the integrity of the BBB through its disturbance of the glutamate efflux.
Normal equilibrium of BBB glutamate is required to maintain an appropriate concentration gradient [33]. Under normal conditions, glutamate cannot move between the intraparenchymal and blood compartments of the BBB without adverse effects. The BBB consists of a physical barrier that defends the central nervous system (CNS) against influx of toxic substances in the blood. It can present high electrical impedance (≈2000 Ω/cm2), making it impermeable to ions [34]. The BBB is formed by brain microvascular endothelial cells and junctional complexes, an endothelial basement membrane and astrocyte end feet around the endothelial cells.
The BBB has distinct layers, each of which assists in restricting the flow of solutes [35]. Under physiological conditions, a high concentration of blood glutamate needs to penetrate at least five of these layers to enter the brain. Glutamate is transported at a relatively low rate, lower than other amino acids, from the blood into the brain [36]. Therefore, in normal circumstances, only a very minute amount of blood glutamate crosses the BBB into the brain [37].
There is a high range of sensitivity of nervous tissue to high concentrations of glutamate. However, there is evidence that a prolonged increase of even 10% of extracellular brain glutamate, i.e., glutamate neurotoxicity, can initiate non-degenerative processes that eventually lead to the development of depression [38].
Depression is a known co-morbidity of many conditions [39,40]. Given the theory of glutamate involvement in the development of depression and the importance of BBB permeability in these disorders, it is reasonable to consider that there is a link between depression and BBB permeability in these neurological and neurogenerative diseases.
In this review, we hypothesize that a moderate but prolonged increase of glutamate in the extracellular brain due to BBB disruption is the underlying mechanism of the development of depression when it occurs after stroke, after traumatic brain injury and in conditions with compromised BBB integrity associated with age, environment, or chronic disease.
5. The Imbalance of Blood-Glutamate Concentration Gradient Following Brain Injury
Many studies have found that during acute brain injury, such as subarachnoid hemorrhage, acute ischemic stroke, intracerebral hemorrhage (ICH) or traumatic brain injury (TBI), glutamate levels in the brain and blood can rise to very high levels [33]. This elevation has also been observed in patients with chronic neurological conditions, such as Parkinson’s disease, Alzheimer’s disease, epilepsy, multiple sclerosis and schizophrenia. These patients have significantly elevated glutamate levels in the blood and CSF compared to non-affected individuals, and the intraparenchymal-blood glutamate concentration gradient also becomes extremely high. Similarly, a recent study has proposed a connection between the gut–brain axis and glutamate that can contribute to the development of depression during gut–brain dysfunction [28].
A decrease may occur in the transport of intraparenchymal glutamate by the glymphatic system after brain insult. Studies have examined the role of regulators, especially aquaporin-4 (AQP4), and glutamate transporter-1 (GLT-1), which are the two essential water and glutamate astrocyte buffering pathways to the brain. In several different animal models of brain insult, including models of AD [41], aging [42], epilepsy [43] and ICH [44], AQP4 expression is lessened and its polarity becomes disrupted.
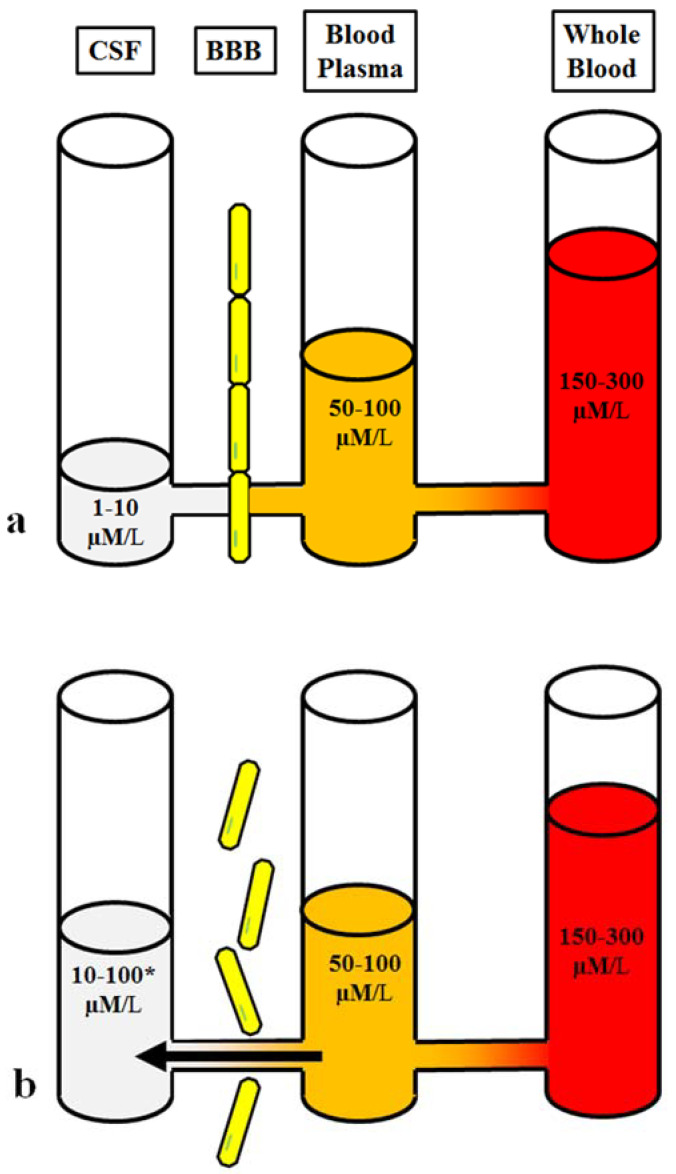
Animal studies using dye injections [45] and magnetic resonance imaging (MRI) in humans [46] have also shown increased permeability of the BBB after a brain injury. These studies indicate that more blood glutamate can also cross into the brain through the functionally impaired BBB and have an effect on the increased intraparenchymal glutamate observed after brain injury (shown in Figure 1).
Figure 1.
Brain-blood glutamate equilibrium: (a). Homeostasis of the normal physiological state. (b). Imbalanced glutamate under pathological conditions and disruption of BBB integrity. 10–100*µM/L The concentration of brain glutamate depends on the degree of disruption of BBB integrity.
Until recently, doubts persisted about whether the BBB exhibits severe physical impairment following brain injury for a significant period of time. Studies have shown that recovery of BBB integrity can take 1–3 months [47] or even up to 10 months [48] in rat models, and in humans, recovery can take years [49]. Immediately after TBI, the concentration of cerebral glutamate increases, then decreases. However, the level does not decrease to normal levels, and the excess can last for many months and even years [50,51].
As noted above, damage to the BBB prevents effective clearance of cerebral glutamate from extracellular fluid into the bloodstream, in which excitatory amino acid transporters (EAAT) on endothelial cells propel the maintenance of the intraparenchymal-blood glutamate concentration gradient [33]. Thus, controlling excess glutamate is a primary goal in preventing the spread of brain damage. Extracellular glutamate is removed by several types of EAATs located on neurons and astrocytes. Loss of astrocytes and neurons as a result of the traumatic impact subsequently reduces the number of available sodium-dependent astroglial glutamate GLT-1 and EAATs, exacerbating the accumulation of extracellular glutamate [52].
6. Blood as the Source of Elevated Brain Glutamate
In healthy adults, the glutamate concentrations in the plasma and whole blood are 50–100 µM/L and 150–300 µM/L, respectively [53]. In several in vitro studies using acute brain slices, extracellular glutamate levels were recorded between 25 and 90 nM [54,55]; however, most in vivo studies using microdialysis found much greater increases in glutamate levels in the brain between 0.2 μM and approximately 20 μM [56,57]. Currently, researchers estimate that glutamate concentrations in the CSF or brain intercellular fluid range from 1 to 10 μM [58,59]. In the healthy brain, the glutamate concentration is much higher in the plasma, which in turn contains higher concentrations that the CSF, with a difference of 50 μM between these different approaches; this results in the intraparenchymal-blood glutamate concentration gradient [58]. Intraparenchymal glutamate homeostasis mainly depends on the integrity of the BBB, and its ability to control the influx of blood glutamate, and on the activity of endothelial glutamate transporters (EAATs), which constantly move intraparenchymal glutamate into the blood [60].
When restoring an imbalance in intraparenchymal-blood glutamate homeostasis, it is necessary to lower the elevated glutamate levels in both the blood and the brain. This process involves impeding the entry of blood glutamate into the brain and improving the transport efficiency of glial and endothelial EAATs and the glymphatic system under pathological conditions.
Glutamate does not solely exist in the brain or blood. One study showed that an increase in the glutamate concentration from 1 to 500 μM in the carotid artery in primary hypertension rats was associated with a higher rate of glutamate penetration into the brain [61]; additionally, systemic injection of glutamate has been indicated to aggravate brain damage [62]. Another study showed that intravenous administration of aspartate aminotransferase [63], pyruvate and oxaloacetate [62,64] could significantly reduce glutamate levels in the blood in addition to accelerating the discharge of glutamate from the brain. These blood glutamate scavengers (BGS) work through decreasing intraparenchymal glutamate levels [59], significantly improving prognoses and outcomes [65], and extending the lifetimes of mice [38,66,67]. From this data, we conclude that the environments of the blood and brain have shared influences, and that blood glutamate is a significant factor in the brain.
7. Neurological Conditions Associated with BBB Permeability and Depression
Dysfunction of the glutamatergic system has been implicated in the pathophysiology of several neurological and neurogenerative disorders. There are several possible pathways through which BBB permeability affects depression. These include increases in CSF or S100B, a neurotrophic factor produced by astrocytes, which are both associated with depression, and increased permeability of the BBB [66,67,68]. In addition, studies have demonstrated that brain endothelial cells and tight junction proteins claudin-5 and occludin were disrupted after chronic stress, indicating weakened BBB integrity after stress. BBB permeability causes increased influx of peripheral material into the brain, leading to neuroinflammation and oxidative stress [69]. These outcomes all point to a correlation between BBB permeability and depression [70,71,72].
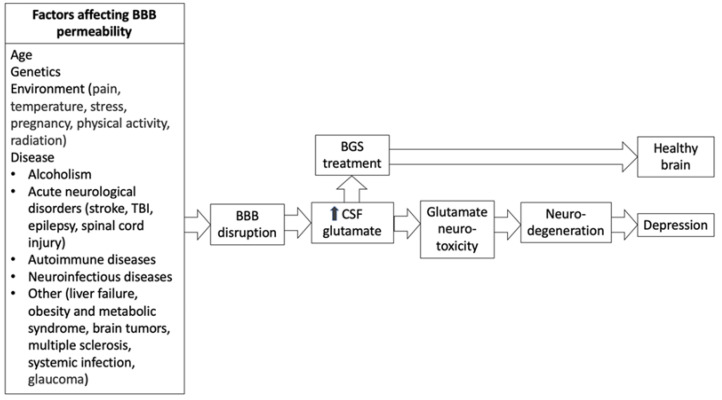
Although the exact mechanisms of BBB permeability have not yet been clearly elucidated, BBB dysregulation has negative effects on a number of conditions, including stroke, TBI, Alzheimer’s disease, Parkinson’s disease, multiple sclerosis and schizophrenia [73,74], known to be a major contributor to the pathology of CNS disorders [75]. Specifically, glutamate excitotoxicity, in which cell death occurs as a result of excessive glutamate release from neurons and glial cells, contributes to the influx of glutamate in the BBB. Glutamate excitotoxicity is an acknowledged factor in neurological conditions [76]. From this evidence, it is likely that treatments that target BBB functionality may be a viable pathway to improving neurological outcomes [77] (Figure 2).
Figure 2.
The relationship between conditions that disrupt the blood–brain-barrier, glutamate and depression.
A full assessment of all neurodegenerative conditions associated with depression and BBB destruction is beyond the scope of our review. Here, we provide a preliminary examination of this relationship through examples of several conditions in which severe BBB destruction leading to an increase in brain extracellular glutamate levels in the short and long term has been well researched and documented.
7.1. Stroke
Stroke is the third most prevalent cause of mortality worldwide and can cause lifetime disability for survivors [78]. Ischemic stroke, the more common type of stroke, occurs after a thrombosis, embolism or systemic hypo-perfusion, which restrict blood flow to the brain. In an ischemic stroke, not enough oxygen and glucose are delivered to maintain cellular homeostasis. This results in cell death from a variety of causes, including from excitotoxicity. During stroke, the increase in BBB permeability is mainly due to changes in junctional protein expression and function [78,79,80]. This disruption begins immediately after vessel occlusion and continues for a significant amount of time after stroke.
The relationship between stroke and depression is also well documented. Post-stroke depression is an acknowledged symptom that affects recovery and mortality after the stroke incident, and early use of antidepressants has been shown to improve outcomes [79,81]. One preliminary study suggests that the use of the BGS pyruvate is a potential treatment for post stroke depression due to the interconnected relationship between glutamate, depression and the BBB [30].
7.2. TBI
The mechanisms of TBI, another major cause of disability and mortality, similarly involve glutamate dysregulation. Disruption of the BBB through inflammation causes cell death and brain edema [82], and TBI has a clear association with a breakdown in BBB permeability [80]. TBI, like stroke, has a known association with depression after its occurrence. Studies report that a quarter to a half of sufferers develop major depression within the first year following TBI [82,83]. A rodent model of TBI used pyruvate as an effective treatment toward mitigating post-TBI depressive-like symptoms, proposing its viability for future studies in the topic of treatments for post-TBI depression in humans [31].
7.3. Other
Other neurological conditions that are caused or exacerbated by BBB disruption and glutamate excitotoxicity and have an association with depression include Parkinson’s disease [84], Huntington’s disease [85], amyotrophic lateral sclerosis [86,87], multiple sclerosis [75,88], Alzheimer’s disease [89,90,91,92], epilepsy [93,94,95], aging [77] and schizophrenia [96,97]. There are likely interpolations to be made to similar conditions for which the association between BBB or depression lacks conclusive data [75], such as in hepatic encephalopathy [98] and brain tumors [99]. The idea of glutamatergic involvement in depression present during these conditions requires additional research.
8. Manipulation of Brain-Blood Glutamate Equilibrium
Excess brain glutamate can be mitigated by manipulating the brain-blood glutamate equilibrium and inducing excess glutamate from the brain’s interstitial fluid to flow into the body’s circulatory system [100]. A method proven in a rat model to reduce the early neuroanatomical and neurological signs caused by TBI includes treatment with BGS. This occurs by administering the enzymes glutamate-oxaloacetate transaminase 1 (GOT) or glutamate pyruvate transaminase (GPT) with their co-substrates oxaloacetic acid (OxAc) or pyruvate, respectively, which reduces excess brain glutamate by altering the balance between blood and brain glutamate [101,102,103]. This method does not directly stimulate or block synaptic NMDA receptors, avoiding some of the negative effects of direct interference. The ability of this method to mitigate emotional and cognitive deficits has begun to be investigated.
Studies indicate that low GOT levels are associated with poor neurological outcomes in humans after stroke, and high GOT levels are associated with a better neurological outcome [65,104]. GOT and GPT include glutamate as a substrate in the general formula: A + glutamate ← (enzyme) → C + D. In this formula, A represents the co-substrate; ← (enzyme) → symbolizes a reversible enzyme; and C and D are metabolites of the enzyme. These enzymes both use pyridoxal phosphate as a cofactor, and reversibly convert glutamate into 2-ketoglutarate, causing blood glutamate levels to reach levels below basal levels. Thus, in a state of impaired BBB permeability, and as a result of the equalization of glutamate levels between the extracellular cerebral fluid and plasma, much less glutamate is able to cross the BBB from the plasma into the extracellular cerebral fluid.
During glutamate transformation via an enzymatic reaction into 2-ketoglutarate, a buildup of 2-ketoglutarate occurs, leading to the possibility of the enzyme converting 2-ketoglutarate into glutamate. It is therefore beneficial to further break down 2-ketoglutarate to ensure the continual metabolism of glutamate. The enzyme 2-ketoglutarate dehydrogenase metabolizes 2-ketoglutarate through the general reaction: 2-ketoglutarate + lipoamide ← (2-ketoglutarate dehydrogenase) → S-succinyldihydrolipoamide + CO2 [105].
In addition to its success in limiting the excess glutamate and the neurological and immunological signs of traumatic injury to the brain and spinal cord, BGS effectively reduces the neurological and behavioral symptoms of subarachnoid hemorrhage [103] and middle cerebral artery occlusion [32]. BGS continues the physiological effects of glutamate in maintaining the metabolic and electrolyte balance and neuronal integrity and improving neuro-repair after brain injury. OxAC and GOT have been proposed as treatments for stroke [65,106]. The safety of OxAc has been demonstrated in elderly patients [107,108], and its potential to alleviate symptoms of anxiety, depression, suicidal ideation and aggression have been suggested in a clinical trial [109]. Thus, despite the destruction of the main mechanisms for maintaining glutamate homeostasis between the blood and the brain in diseases associated with impaired BBB, and a resultant increase in cerebral glutamate and the occurrence of mental disorders, the BGS method looks very promising for the treatment and prevention of depression, and in other conditions associated with high levels of brain glutamate.
Based on the mechanisms described above for the development of depression as a result of BBB disruption and glutamate neurotoxicity, there may be alternatives to BGS. Other therapeutic strategies are possible that would be aimed at restoring the BBB or facilitating the transport of glutamate through the BBB. The efficacy of BGS, however, has been proven in previous studies, which makes it a likely candidate for application in these circumstances as well.
9. Contrary Findings of Impaired BBB Permeability and Brain-Blood Glutamate Equilibrium
Despite the evidence for the involvement of glutamate in the pathophysiology of depression, a few contrary approaches appear to put this evidence in doubt. Studies using proton magnetic resonance spectroscopy (1H-MRS) have observed elevated regional levels of glutamatergic metabolites in patients with depression compared with controls [20]. However, other studies indicate inconsistent results, including increases [110], no differences [111,112] or decreases [113] in glutamatergic neurometabolite levels across different brain regions in patients with depression. This variability may be attributable to differences in the regions examined, MRS methodologies, stages or severities of illness or in medications such as antidepressant treatments [114].
This inconsistency can also be explained by the understanding that MRI usually cannot distinguish between a glutamate and glutamine peak and instead measures the combined glutamate-glutamine peak. Since glutamate breaks down into glutamine, this information does not reflect the state of increasing or decreasing levels of glutamate in the brain. In addition, most importantly, the results obtained using MRS are not very informative, since this technique cannot separate intracellular and extracellular brain glutamate. Therefore, the average result of total brain glutamate is given, including the blood found in that particular region.
This information does not reflect the level of extracellular glutamate that, according to the glutamate theory, is the cause of depression. Therefore, MRS studies of brain glutamate levels can be more confusing than illuminating, unlike glutamate concentration data obtained from CSF collection, microdialysis or brain slice staining for glutamate receptor counts.
Also, blood glutamate levels can be inconsistent, sometimes high and sometimes normal. Some data suggests that glutamate levels in plasma and whole blood are increased in patients with depression versus controls [17,115,116], while others have indicated no disparity between the two groups [16,117]. The reason for the observed elevation in blood glutamate levels have not yet been elucidated [34,38,118].
Blood cells also provide a source of blood glutamate. Cerebral infarction involves the release of platelets, which allows for the entrance of a large amount of glutamate into the blood [119]. Due to the secretion of glutamate in osteoclasts when stimulated with KCl or ATP, bone might be another source [120].
Additionally, blood and plasma glutamate levels can be recorded over a long timeframe and are highly dependent on gender [121,122], body temperature [123], diet [115], stress [116], meal time [124], age [118,119], background diseases [125] and even blood sampling sites [126]. Therefore, the level of blood/plasma glutamate probably plays an important role in the change in the level of brain glutamate, but the degree of destruction of the BBB plays a more important role. This ultimately determines the level of increase in brain glutamate and, as a consequence, the development of depression.
10. Conclusions
The development of antidepressant drugs has made much progress in the last several decades. However, standard treatment still relies exclusively on the monoaminergic system and therefore has many shortcomings. Existing monoaminergic antidepressants require long-term treatment of weeks or months to reach their full therapeutic efficacy and are effective in only a fraction of depressed patients. More nuanced analyses have revealed many factors and mechanisms that contribute to the development of MDD, including monoamine dysfunction, hormones, hypothalamic-pituitary-adrenal axis activation, genetics, neurogenesis, immune dysfunction and gender. In addition, the innovative theory about the involvement of the glutamate system aims to contribute more to our understanding of depression. In this review, we examined specific conditions in which depression is a co-morbidity that which are also associated with the glutamatergic system. In neurological and neurogenerative diseases with impaired BBB permeability and excitotoxicity as a contributing factor to the disease pathogenesis, we suggest that treatment for depression should be directed toward stabilizing the glutamate system through restoring homeostasis. In our opinion, drugs such as blood glutamate scavengers should be considered for the treatment of depression associated with these conditions. We anticipate more research on this topic will elucidate this and other treatment options.
Acknowledgments
The authors would like to thank the late Vivian I. Teichberg, a pioneer in glutamate metabolism and neurotoxicity, whose work at the Weizmann Institute of Science laid the foundation of our current work. We feel privileged for the opportunity to have collaborated and learned from him.
Author Contributions
B.F.G., A.Z., A.F., I.F. and M.B. contributed to the conceptualization, investigation, writing, reviewing and editing of this manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bading H. Nuclear calcium signalling in the regulation of brain function. Nat. Rev. Neurosci. 2013;14:593–608. doi: 10.1038/nrn3531. [DOI] [PubMed] [Google Scholar]
- 2.Musazzi L., Treccani G., Popoli M. Glutamate hypothesis of depression and its consequences for antidepressant treatments. Expert Rev. Neurother. 2012;12:1169–1172. doi: 10.1586/ern.12.96. [DOI] [PubMed] [Google Scholar]
- 3.Gladding C.M., Raymond L.A. Mechanisms underlying NMDA receptor synaptic/extrasynaptic distribution and function. Mol. Cell. Neurosci. 2011;48:308–320. doi: 10.1016/j.mcn.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Abdallah C.G., Sanacora G., Duman R.S., Krystal J.H. Ketamine and rapid-acting antidepressants: A window into a new neurobiology for mood disorder therapeutics. Annu. Rev. Med. 2015;66:509–523. doi: 10.1146/annurev-med-053013-062946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hardingham G.E., Bading H. The Yin and Yang of NMDA receptor signalling. Trends Neurosci. 2003;26:81–89. doi: 10.1016/S0166-2236(02)00040-1. [DOI] [PubMed] [Google Scholar]
- 6.Kavalali E.T., Monteggia L.M. Synaptic mechanisms underlying rapid antidepressant action of ketamine. Am. J. Psychiatry. 2012;169:1150–1156. doi: 10.1176/appi.ajp.2012.12040531. [DOI] [PubMed] [Google Scholar]
- 7.Wang S.-M., Han C., Bahk W.-M., Lee S.-J., Patkar A.A., Masand P.S., Pae C.-U. Addressing the side effects of contemporary antidepressant drugs: A comprehensive review. Chonnam Med. J. 2018;54:101–112. doi: 10.4068/cmj.2018.54.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanacora G., Treccani G., Popoli M. Towards a glutamate hypothesis of depression: An emerging frontier of neuropsychopharmacology for mood disorders. Neuropharmacology. 2012;62:63–77. doi: 10.1016/j.neuropharm.2011.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoo H.C., Yu Y.C., Sung Y., Han J.M. Glutamine reliance in cell metabolism. Exp. Mol. Med. 2020;52:1496–1516. doi: 10.1038/s12276-020-00504-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DuBourdieu D. Nutraceuticals. Elsevier; Amsterdam, The Netherlands: 2021. Glutamine supplementation: Hope, hype, or stay tuned? pp. 1027–1036. [Google Scholar]
- 11.Pralong E., Magistretti P., Stoop R. Cellular perspectives on the glutamate–monoamine interactions in limbic lobe structures and their relevance for some psychiatric disorders. Prog. Neurobiol. 2002;67:173–202. doi: 10.1016/S0301-0082(02)00017-5. [DOI] [PubMed] [Google Scholar]
- 12.Trullas R., Skolnick P. Functional antagonists at the NMDA receptor complex exhibit antidepressant actions. Eur. J. Pharmacol. 1990;185:1–10. doi: 10.1016/0014-2999(90)90204-J. [DOI] [PubMed] [Google Scholar]
- 13.Berman R.M., Cappiello A., Anand A., Oren D.A., Heninger G.R., Charney D.S., Krystal J.H. Antidepressant effects of ketamine in depressed patients. Biol. Psychiatry. 2000;47:351–354. doi: 10.1016/S0006-3223(99)00230-9. [DOI] [PubMed] [Google Scholar]
- 14.Lener M.S., Niciu M.J., Ballard E.D., Park M., Park L.T., Nugent A.C., Zarate C.A., Jr. Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol. Psychiatry. 2017;81:886–897. doi: 10.1016/j.biopsych.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim J., Schmid-Burgk W., Claus D., Kornhuber H. Increased serum glutamate in depressed patients. Arch. Für Psychiatr. Und Nervenkrankh. 1982;232:299–304. doi: 10.1007/BF00345492. [DOI] [PubMed] [Google Scholar]
- 16.Maes M., Verkerk R., Vandoolaeghe E., Lin A., Scharpe S. Serum levels of excitatory amino acids, serine, glycine, histidine, threonine, taurine, alanine and arginine in treatment-resistant depression: Modulation by treatment with antidepressants and prediction of clinical responsivity. Acta Psychiatr. Scand. 1998;97:302–308. doi: 10.1111/j.1600-0447.1998.tb10004.x. [DOI] [PubMed] [Google Scholar]
- 17.Küçükibrahimoğlu E., Saygın M.Z., Çalışkan M., Kaplan O.K., Ünsal C., Gören M.Z. The change in plasma GABA, glutamine and glutamate levels in fluoxetine-or S-citalopram-treated female patients with major depression. Eur. J. Clin. Pharmacol. 2009;65:571–577. doi: 10.1007/s00228-009-0650-7. [DOI] [PubMed] [Google Scholar]
- 18.Mitani H., Shirayama Y., Yamada T., Maeda K., Ashby C.R., Jr., Kawahara R. Correlation between plasma levels of glutamate, alanine and serine with severity of depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2006;30:1155–1158. doi: 10.1016/j.pnpbp.2006.03.036. [DOI] [PubMed] [Google Scholar]
- 19.Levine J., Panchalingam K., Rapoport A., Gershon S., McClure R.J., Pettegrew J.W. Increased cerebrospinal fluid glutamine levels in depressed patients. Biol. Psychiatry. 2000;47:586–593. doi: 10.1016/S0006-3223(99)00284-X. [DOI] [PubMed] [Google Scholar]
- 20.Moriguchi S., Takamiya A., Noda Y., Horita N., Wada M., Tsugawa S., Plitman E., Sano Y., Tarumi R., ElSalhy M. Glutamatergic neurometabolite levels in major depressive disorder: A systematic review and meta-analysis of proton magnetic resonance spectroscopy studies. Mol. Psychiatry. 2019;24:952–964. doi: 10.1038/s41380-018-0252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deschwanden A., Karolewicz B., Feyissa A.M., Treyer V., Ametamey S.M., Johayem A., Burger C., Auberson Y.P., Sovago J., Stockmeier C.A. Reduced metabotropic glutamate receptor 5 density in major depression determined by [11C] ABP688 PET and postmortem study. Am. J. Psychiatry. 2011;168:727–734. doi: 10.1176/appi.ajp.2011.09111607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nudmamud-Thanoi S., Reynolds G.P. The NR1 subunit of the glutamate/NMDA receptor in the superior temporal cortex in schizophrenia and affective disorders. Neurosci. Lett. 2004;372:173–177. doi: 10.1016/j.neulet.2004.09.035. [DOI] [PubMed] [Google Scholar]
- 23.Beneyto M., Kristiansen L.V., Oni-Orisan A., McCullumsmith R.E., Meador-Woodruff J.H. Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology. 2007;32:1888–1902. doi: 10.1038/sj.npp.1301312. [DOI] [PubMed] [Google Scholar]
- 24.Feyissa A.M., Chandran A., Stockmeier C.A., Karolewicz B. Reduced levels of NR2A and NR2B subunits of NMDA receptor and PSD-95 in the prefrontal cortex in major depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2009;33:70–75. doi: 10.1016/j.pnpbp.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feyissa A.M., Woolverton W.L., Miguel-Hidalgo J.J., Wang Z., Kyle P.B., Hasler G., Stockmeier C.A., Iyo A.H., Karolewicz B. Elevated level of metabotropic glutamate receptor 2/3 in the prefrontal cortex in major depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2010;34:279–283. doi: 10.1016/j.pnpbp.2009.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karolewicz B., Feyissa A.M., Chandran A., Legutko B., Ordway G.A., Rajkowska G., Stockmeier C.A. Glutamate receptors expression in postmortem brain from depressed subjects. Biol. Psychiatry. 2009;65:177S. [Google Scholar]
- 27.Luykx J., Laban K., Van Den Heuvel M., Boks M., Mandl R., Kahn R., Bakker S. Region and state specific glutamate downregulation in major depressive disorder: A meta-analysis of 1H-MRS findings. Neurosci. Biobehav. Rev. 2012;36:198–205. doi: 10.1016/j.neubiorev.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Onaolapo A.Y., Onaolapo O.J. Glutamate and depression: Reflecting a deepening knowledge of the gut and brain effects of a ubiquitous molecule. World J. Psychiatry. 2021;11:297. doi: 10.5498/wjp.v11.i7.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godlewska B.R., Masaki C., Sharpley A.L., Cowen P.J., Emir U.E. Brain glutamate in medication-free depressed patients: A proton MRS study at 7 Tesla. Psychol. Med. 2018;48:1731–1737. doi: 10.1017/S0033291717003373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frank D., Kuts R., Tsenter P., Gruenbaum B.F., Grinshpun Y., Zvenigorodsky V., Shelef I., Natanel D., Brotfain E., Zlotnik A. The effect of pyruvate on the development and progression of post-stroke depression: A new therapeutic approach. Neuropharmacology. 2019;155:173–184. doi: 10.1016/j.neuropharm.2019.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frank D., Gruenbaum B.F., Shelef I., Severynovska O., Gal R., Dubilet M., Zlotnik A., Kofman O., Boyko M. Blood glutamate scavenging with pyruvate as a novel preventative and therapeutic approach for depressive-like behavior following traumatic brain injury in a rat model. Front. Neurosci. 2022;21:832478. doi: 10.3389/fnins.2022.832478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gruenbaum B.F., Kutz R., Zlotnik A., Boyko M. Blood glutamate scavenging as a novel glutamate-based therapeutic approach for post-stroke depression. Ther. Adv. Psychopharmacol. 2020;10:2045125320903951. doi: 10.1177/2045125320903951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bai W., Zhou Y.-G. Homeostasis of the intraparenchymal-blood glutamate concentration gradient: Maintenance, imbalance, and regulation. Front. Mol. Neurosci. 2017;10:400. doi: 10.3389/fnmol.2017.00400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sifat A.E., Vaidya B., Abbruscato T.J. Blood-brain barrier protection as a therapeutic strategy for acute ischemic stroke. AAPS J. 2017;19:957–972. doi: 10.1208/s12248-017-0091-7. [DOI] [PubMed] [Google Scholar]
- 35.Tajes M., Ramos-Fernández E., Weng-Jiang X., Bosch-Morato M., Guivernau B., Eraso-Pichot A., Salvador B., Fernandez-Busquets X., Roquer J., Munoz F.J. The blood-brain barrier: Structure, function and therapeutic approaches to cross it. Mol. Membr. Biol. 2014;31:152–167. doi: 10.3109/09687688.2014.937468. [DOI] [PubMed] [Google Scholar]
- 36.Hawkins R.A., Simpson I.A., Mokashi A., Viña J.R. Pyroglutamate stimulates Na+-dependent glutamate transport across the blood–brain barrier. FEBS Lett. 2006;580:4382–4386. doi: 10.1016/j.febslet.2006.06.097. [DOI] [PubMed] [Google Scholar]
- 37.Klin Y., Zlotnik A., Boyko M., Ohayon S., Shapira Y., Teichberg V.I. Distribution of radiolabeled l-glutamate and d-aspartate from blood into peripheral tissues in naive rats: Significance for brain neuroprotection. Biochem. Biophys. Res. Commun. 2010;399:694–698. doi: 10.1016/j.bbrc.2010.07.144. [DOI] [PubMed] [Google Scholar]
- 38.Lewerenz J., Maher P. Chronic glutamate toxicity in neurodegenerative diseases—what is the evidence? Front. Neurosci. 2015;9:469. doi: 10.3389/fnins.2015.00469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rickards H. Depression in neurological disorders: An update. Curr. Opin. Psychiatry. 2006;19:294–298. doi: 10.1097/01.yco.0000218601.17722.5b. [DOI] [PubMed] [Google Scholar]
- 40.Hellmann-Regen J., Piber D., Hinkelmann K., Gold S.M., Heesen C., Spitzer C., Endres M., Otte C. Depressive syndromes in neurological disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2013;263((Suppl. S2)):S123–S136. doi: 10.1007/s00406-013-0448-6. [DOI] [PubMed] [Google Scholar]
- 41.Yang S.-J., Kim E.-A., Chang M.-J., Kim J., Na J.-M., Choi S.Y., Cho S.-W. N-Adamantyl-4-methylthiazol-2-amine attenuates glutamate-induced oxidative stress and inflammation in the brain. Neurotox. Res. 2017;32:107–120. doi: 10.1007/s12640-017-9717-x. [DOI] [PubMed] [Google Scholar]
- 42.Kress B.T., Iliff J.J., Xia M., Wang M., Wei H.S., Zeppenfeld D., Xie L., Kang H., Xu Q., Liew J.A. Impairment of paravascular clearance pathways in the aging brain. Ann. Neurol. 2014;76:845–861. doi: 10.1002/ana.24271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hubbard J.A., Szu J.I., Yonan J.M., Binder D.K. Regulation of astrocyte glutamate transporter-1 (GLT1) and aquaporin-4 (AQP4) expression in a model of epilepsy. Exp. Neurol. 2016;283:85–96. doi: 10.1016/j.expneurol.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qiu G.-P., Xu J., Zhuo F., Sun S.-Q., Liu H., Yang M., Huang J., Lu W.-T., Huang S.-Q. Loss of AQP4 polarized localization with loss of β-dystroglycan immunoreactivity may induce brain edema following intracerebral hemorrhage. Neurosci. Lett. 2015;588:42–48. doi: 10.1016/j.neulet.2014.12.053. [DOI] [PubMed] [Google Scholar]
- 45.Hue C.D., Cao S., “Dale” Bass C.R., Meaney D.F., Morrison B., III Repeated primary blast injury causes delayed recovery, but not additive disruption, in an in vitro blood–brain barrier model. J. Neurotrauma. 2014;31:951–960. doi: 10.1089/neu.2013.3149. [DOI] [PubMed] [Google Scholar]
- 46.Merali Z., Huang K., Mikulis D., Silver F., Kassner A. Evolution of blood-brain-barrier permeability after acute ischemic stroke. PLoS ONE. 2017;12:e0171558. doi: 10.1371/journal.pone.0171558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yu M., Wang M., Yang D., Wei X., Li W. Dynamics of blood brain barrier permeability and tissue microstructure following controlled cortical impact injury in rat: A dynamic contrast-enhanced magnetic resonance imaging and diffusion kurtosis imaging study. Magn. Reson. Imaging. 2019;62:1–9. doi: 10.1016/j.mri.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 48.van Vliet E.A., Ndode-Ekane X.E., Lehto L.J., Gorter J.A., Andrade P., Aronica E., Gröhn O., Pitkänen A. Long-lasting blood-brain barrier dysfunction and neuroinflammation after traumatic brain injury. Neurobiol. Dis. 2020;145:105080. doi: 10.1016/j.nbd.2020.105080. [DOI] [PubMed] [Google Scholar]
- 49.Hay J.R., Johnson V.E., Young A.M., Smith D.H., Stewart W. Blood-brain barrier disruption is an early event that may persist for many years after traumatic brain injury in humans. J. Neuropathol. Exp. Neurol. 2015;74:1147–1157. doi: 10.1097/NEN.0000000000000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vespa P., Prins M., Ronne-Engstrom E., Caron M., Shalmon E., Hovda D.A., Martin N.A., Becker D.P. Increase in extracellular glutamate caused by reduced cerebral perfusion pressure and seizures after human traumatic brain injury: A microdialysis study. J. Neurosurg. 1998;89:971–982. doi: 10.3171/jns.1998.89.6.0971. [DOI] [PubMed] [Google Scholar]
- 51.Wu Y., Wu H., Guo X., Pluimer B., Zhao Z. Blood–brain barrier dysfunction in mild traumatic brain injury: Evidence from preclinical murine models. Front. Physiol. 2020;1030 doi: 10.3389/fphys.2020.01030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Piao C.-S., Holloway A.L., Hong-Routson S., Wainwright M.S. Depression following traumatic brain injury in mice is associated with down-regulation of hippocampal astrocyte glutamate transporters by thrombin. J. Cereb. Blood Flow Metab. 2019;39:58–73. doi: 10.1177/0271678X17742792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leibowitz A., Boyko M., Shapira Y., Zlotnik A. Blood glutamate scavenging: Insight into neuroprotection. Int. J. Mol. Sci. 2012;13:10041–10066. doi: 10.3390/ijms130810041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Herman M.A., Jahr C.E. Extracellular glutamate concentration in hippocampal slice. J. Neurosci. 2007;27:9736–9741. doi: 10.1523/JNEUROSCI.3009-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meur K.L., Galante M., Angulo M.C., Audinat E. Tonic activation of NMDA receptors by ambient glutamate of non-synaptic origin in the rat hippocampus. J. Physiol. 2007;580:373–383. doi: 10.1113/jphysiol.2006.123570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dash M.B., Douglas C.L., Vyazovskiy V.V., Cirelli C., Tononi G. Long-term homeostasis of extracellular glutamate in the rat cerebral cortex across sleep and waking states. J. Neurosci. 2009;29:620–629. doi: 10.1523/JNEUROSCI.5486-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Bundel D., Schallier A., Loyens E., Fernando R., Miyashita H., Van Liefferinge J., Vermoesen K., Bannai S., Sato H., Michotte Y. Loss of system xc− does not induce oxidative stress but decreases extracellular glutamate in hippocampus and influences spatial working memory and limbic seizure susceptibility. J. Neurosci. 2011;31:5792–5803. doi: 10.1523/JNEUROSCI.5465-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hawkins R.A. The blood-brain barrier and glutamate. Am. J. Clin. Nutr. 2009;90:867S–874S. doi: 10.3945/ajcn.2009.27462BB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Teichberg V., Cohen-Kashi-Malina K., Cooper I., Zlotnik A. Homeostasis of glutamate in brain fluids: An accelerated brain-to-blood efflux of excess glutamate is produced by blood glutamate scavenging and offers protection from neuropathologies. Neuroscience. 2009;158:301–308. doi: 10.1016/j.neuroscience.2008.02.075. [DOI] [PubMed] [Google Scholar]
- 60.Cohen-Kashi-Malina K., Cooper I., Teichberg V.I. Mechanisms of Glutamate Efflux at the Blood—Brain Barrier: Involvement of Glial Cells. J. Cereb. Blood Flow Metab. 2012;32:177–189. doi: 10.1038/jcbfm.2011.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Al-Sarraf H., Philip L. Increased brain uptake and CSF clearance of 14C-glutamate in spontaneously hypertensive rats. Brain Res. 2003;994:181–187. doi: 10.1016/j.brainres.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 62.Zlotnik A., Sinelnikov I., Gruenbaum B.F., Gruenbaum S.E., Dubilet M., Dubilet E., Leibowitz A., Ohayon S., Regev A., Boyko M. Effect of glutamate and blood glutamate scavengers oxaloacetate and pyruvate on neurological outcome and pathohistology of the hippocampus after traumatic brain injury in rats. J. Am. Soc. Anesthesiol. 2012;116:73–83. doi: 10.1097/ALN.0b013e31823d7731. [DOI] [PubMed] [Google Scholar]
- 63.Ruban A., Berkutzki T., Cooper I., Mohar B., Teichberg V.I. Blood glutamate scavengers prolong the survival of rats and mice with brain-implanted gliomas. Investig. New Drugs. 2012;30:2226–2235. doi: 10.1007/s10637-012-9794-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zlotnik A., Gruenbaum S.E., Artru A.A., Rozet I., Dubilet M., Tkachov S., Brotfain E., Klin Y., Shapira Y., Teichberg V.I. The neuroprotective effects of oxaloacetate in closed head injury in rats is mediated by its blood glutamate scavenging activity: Evidence from the use of maleate. J. Neurosurg. Anesthesiol. 2009;21:235–241. doi: 10.1097/ANA.0b013e3181a2bf0b. [DOI] [PubMed] [Google Scholar]
- 65.Campos F., Sobrino T., Ramos-Cabrer P., Castellanos M., Blanco M., Rodríguez-Yáñez M., Serena J., Leira R., Castillo J. High blood glutamate oxaloacetate transaminase levels are associated with good functional outcome in acute ischemic stroke. J. Cereb. Blood Flow Metab. 2011;31:1387–1393. doi: 10.1038/jcbfm.2011.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gudmundsson P., Skoog I., Waern M., Blennow K., Zetterberg H., Rosengren L., Gustafson D. Is there a CSF biomarker profile related to depression in elderly women? Psychiatry Res. 2010;176:174–178. doi: 10.1016/j.psychres.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 67.Gulen B., Serinken M., Eken C., Karcıoglu Ö., Kucukdagli O.T., Kilic E., Akpinar G., Nogay S., Kuh M. Serum S100B as a surrogate biomarker in the diagnoses of burnout and depression in emergency medicine residents. Acad. Emerg. Med. 2016;23:786–789. doi: 10.1111/acem.12973. [DOI] [PubMed] [Google Scholar]
- 68.Arora P., Sagar R., Mehta M., Pallavi P., Sharma S., Mukhopadhyay A.K. Serum S100B levels in patients with depression. Indian J. Psychiatry. 2019;61:70. doi: 10.4103/psychiatry.IndianJPsychiatry_391_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kealy J., Greene C., Campbell M. Blood-brain barrier regulation in psychiatric disorders. Neurosci. Lett. 2020;726:133664. doi: 10.1016/j.neulet.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 70.Sántha P., Veszelka S., Hoyk Z., Mészáros M., Walter F.R., Tóth A.E., Kiss L., Kincses A., Oláh Z., Seprényi G. Restraint stress-induced morphological changes at the blood-brain barrier in adult rats. Front. Mol. Neurosci. 2016;8:88. doi: 10.3389/fnmol.2015.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Menard C., Pfau M.L., Hodes G.E., Kana V., Wang V.X., Bouchard S., Takahashi A., Flanigan M.E., Aleyasin H., LeClair K.B. Social stress induces neurovascular pathology promoting depression. Nat. Neurosci. 2017;20:1752–1760. doi: 10.1038/s41593-017-0010-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lee S., Kang B.-M., Kim J.H., Min J., Kim H.S., Ryu H., Park H., Bae S., Oh D., Choi M. Real-time in vivo two-photon imaging study reveals decreased cerebro-vascular volume and increased blood-brain barrier permeability in chronically stressed mice. Sci. Rep. 2018;8:13064. doi: 10.1038/s41598-018-30875-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Profaci C.P., Munji R.N., Pulido R.S., Daneman R. The blood-brain barrier in health and disease: Important unanswered questions. J. Exp. Med. 2020;217:e20190062. doi: 10.1084/jem.20190062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schoknecht K., Shalev H. Blood-brain barrier dysfunction in brain diseases: Clinical experience. Epilepsia. 2012;53((Suppl. S6)):7–13. doi: 10.1111/j.1528-1167.2012.03697.x. [DOI] [PubMed] [Google Scholar]
- 75.Archie S.R., Al Shoyaib A., Cucullo L. Blood-Brain Barrier Dysfunction in CNS Disorders and Putative Therapeutic Targets: An Overview. Pharmaceutics. 2021;13:1779. doi: 10.3390/pharmaceutics13111779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Belov Kirdajova D., Kriska J., Tureckova J., Anderova M. Ischemia-Triggered Glutamate Excitotoxicity From the Perspective of Glial Cells. Front. Cell Neurosci. 2020;14:51. doi: 10.3389/fncel.2020.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Uprety A., Kang Y., Kim S.Y. Blood-brain barrier dysfunction as a potential therapeutic target for neurodegenerative disorders. Arch. Pharm. Res. 2021;44:487–498. doi: 10.1007/s12272-021-01332-8. [DOI] [PubMed] [Google Scholar]
- 78.Doyle K.P., Simon R.P., Stenzel-Poore M.P. Mechanisms of ischemic brain damage. Neuropharmacology. 2008;55:310–318. doi: 10.1016/j.neuropharm.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Robinson R.G., Jorge R.E. Post-Stroke Depression: A Review. Am. J. Psychiatry. 2016;173:221–231. doi: 10.1176/appi.ajp.2015.15030363. [DOI] [PubMed] [Google Scholar]
- 80.Chodobski A., Zink B.J., Szmydynger-Chodobska J. Blood-brain barrier pathophysiology in traumatic brain injury. Transl. Stroke Res. 2011;2:492–516. doi: 10.1007/s12975-011-0125-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen Y., Guo J.J., Zhan S., Patel N.C. Treatment effects of antidepressants in patients with post-stroke depression: A meta-analysis. Ann. Pharm. 2006;40:2115–2122. doi: 10.1345/aph.1H389. [DOI] [PubMed] [Google Scholar]
- 82.Lavoie S., Sechrist S., Quach N., Ehsanian R., Duong T., Gotlib I.H., Isaac L. Depression in Men and Women One Year Following Traumatic Brain Injury (TBI): A TBI Model Systems Study. Front. Psychol. 2017;8:634. doi: 10.3389/fpsyg.2017.00634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Scholten A.C., Haagsma J.A., Cnossen M.C., Olff M., van Beeck E.F., Polinder S. Prevalence of and Risk Factors for Anxiety and Depressive Disorders after Traumatic Brain Injury: A Systematic Review. J. Neurotrauma. 2016;33:1969–1994. doi: 10.1089/neu.2015.4252. [DOI] [PubMed] [Google Scholar]
- 84.Gasca-Salas C., Fernandez-Rodriguez B., Pineda-Pardo J.A., Rodriguez-Rojas R., Obeso I., Hernandez-Fernandez F., Del Alamo M., Mata D., Guida P., Ordas-Bandera C., et al. Blood-brain barrier opening with focused ultrasound in Parkinson’s disease dementia. Nat. Commun. 2021;12:779. doi: 10.1038/s41467-021-21022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Di Pardo A., Amico E., Scalabri F., Pepe G., Castaldo S., Elifani F., Capocci L., De Sanctis C., Comerci L., Pompeo F., et al. Impairment of blood-brain barrier is an early event in R6/2 mouse model of Huntington Disease. Sci. Rep. 2017;7:41316. doi: 10.1038/srep41316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Abrahao A., Meng Y., Llinas M., Huang Y., Hamani C., Mainprize T., Aubert I., Heyn C., Black S.E., Hynynen K., et al. First-in-human trial of blood-brain barrier opening in amyotrophic lateral sclerosis using MR-guided focused ultrasound. Nat. Commun. 2019;10:4373. doi: 10.1038/s41467-019-12426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Heidari M.E., Nadali J., Parouhan A., Azarafraz M., Tabatabai S.M., Irvani S.S.N., Eskandari F., Gharebaghi A. Prevalence of depression among amyotrophic lateral sclerosis (ALS) patients: A systematic review and meta-analysis. J. Affect. Disord. 2021;287:182–190. doi: 10.1016/j.jad.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 88.Ortiz G.G., Pacheco-Moises F.P., Macias-Islas M.A., Flores-Alvarado L.J., Mireles-Ramirez M.A., Gonzalez-Renovato E.D., Hernandez-Navarro V.E., Sanchez-Lopez A.L., Alatorre-Jimenez M.A. Role of the blood-brain barrier in multiple sclerosis. Arch. Med. Res. 2014;45:687–697. doi: 10.1016/j.arcmed.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 89.Zenaro E., Piacentino G., Constantin G. The blood-brain barrier in Alzheimer’s disease. Neurobiol. Dis. 2017;107:41–56. doi: 10.1016/j.nbd.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang R., Reddy P.H. Role of Glutamate and NMDA Receptors in Alzheimer’s Disease. J. Alzheimer’s Dis. 2017;57:1041–1048. doi: 10.3233/JAD-160763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Aguera-Ortiz L., Garcia-Ramos R., Grandas Perez F.J., Lopez-Alvarez J., Montes Rodriguez J.M., Olazaran Rodriguez F.J., Olivera Pueyo J., Pelegrin Valero C., Porta-Etessam J. Depression in Alzheimer’s Disease: A Delphi Consensus on Etiology, Risk Factors, and Clinical Management. Front. Psychiatry. 2021;12:638651. doi: 10.3389/fpsyt.2021.638651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Madeira C., Vargas-Lopes C., Brandao C.O., Reis T., Laks J., Panizzutti R., Ferreira S.T. Elevated Glutamate and Glutamine Levels in the Cerebrospinal Fluid of Patients with Probable Alzheimer’s Disease and Depression. Front. Psychiatry. 2018;9:561. doi: 10.3389/fpsyt.2018.00561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rüber T., David B., Lüchters G., Nass R.D., Friedman A., Surges R., Stöcker T., Weber B., Deichmann R., Schlaug G. Evidence for peri-ictal blood–brain barrier dysfunction in patients with epilepsy. Brain. 2018;141:2952–2965. doi: 10.1093/brain/awy242. [DOI] [PubMed] [Google Scholar]
- 94.Scott A.J., Sharpe L., Hunt C., Gandy M. Anxiety and depressive disorders in people with epilepsy: A meta-analysis. Epilepsia. 2017;58:973–982. doi: 10.1111/epi.13769. [DOI] [PubMed] [Google Scholar]
- 95.Gruenbaum B.F., Sandhu M.R.S., Bertasi R.A.O., Bertasi T.G.O., Schonwald A., Kurup A., Gruenbaum S.E., Freedman I.G., Funaro M.C., Blumenfeld H., et al. Absence seizures and their relationship to depression and anxiety: Evidence for bidirectionality. Epilepsia. 2021;62:1041–1056. doi: 10.1111/epi.16862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Futtrup J., Margolinsky R., Benros M.E., Moos T., Routhe L.J., Rungby J., Krogh J. Blood-brain barrier pathology in patients with severe mental disorders: A systematic review and meta-analysis of biomarkers in case-control studies. Brain Behav. Immun. Health. 2020;6:100102. doi: 10.1016/j.bbih.2020.100102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Etchecopar-Etchart D., Korchia T., Loundou A., Llorca P.M., Auquier P., Lancon C., Boyer L., Fond G. Comorbid Major Depressive Disorder in Schizophrenia: A Systematic Review and Meta-Analysis. Schizophr. Bull. 2021;47:298–308. doi: 10.1093/schbul/sbaa153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Eftekar M. The association between hepatic encephalopathy/minimal hepatic encephalopathy and depressive and anxiety disorders: A systematic review. Australas. Psychiatry. 2020;28:61–65. doi: 10.1177/1039856219875054. [DOI] [PubMed] [Google Scholar]
- 99.Huang J., Zeng C., Xiao J., Zhao D., Tang H., Wu H., Chen J. Association between depression and brain tumor: A systematic review and meta-analysis. Oncotarget. 2017;8:94932–94943. doi: 10.18632/oncotarget.19843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Castillo J., Loza M.I., Mirelman D., Brea J., Blanco M., Sobrino T., Campos F. A novel mechanism of neuroprotection: Blood glutamate grabber. J. Cereb. Blood Flow Metab. 2016;36:292–301. doi: 10.1177/0271678X15606721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zlotnik A., Gurevich B., Cherniavsky E., Tkachov S., Matuzani-Ruban A., Leon A., Shapira Y., Teichberg V.I. The contribution of the blood glutamate scavenging activity of pyruvate to its neuroprotective properties in a rat model of closed head injury. Neurochem. Res. 2008;33:1044–1050. doi: 10.1007/s11064-007-9548-x. [DOI] [PubMed] [Google Scholar]
- 102.Li Y., Hou X., Qi Q., Wang L., Luo L., Yang S., Zhang Y., Miao Z., Zhang Y., Wang F. Scavenging of blood glutamate for enhancing brain-to-blood glutamate efflux. Mol. Med. Rep. 2014;9:305–310. doi: 10.3892/mmr.2013.1793. [DOI] [PubMed] [Google Scholar]
- 103.Boyko M., Melamed I., Gruenbaum B.F., Gruenbaum S.E., Ohayon S., Leibowitz A., Brotfain E., Shapira Y., Zlotnik A. The effect of blood glutamate scavengers oxaloacetate and pyruvate on neurological outcome in a rat model of subarachnoid hemorrhage. Neurotherapeutics. 2012;9:649–657. doi: 10.1007/s13311-012-0129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pérez-Mato M., Ramos-Cabrer P., Sobrino T., Blanco M., Ruban A., Mirelman D., Menendez P., Castillo J., Campos F. Human recombinant glutamate oxaloacetate transaminase 1 (GOT1) supplemented with oxaloacetate induces a protective effect after cerebral ischemia. Cell Death Dis. 2014;5:e992. doi: 10.1038/cddis.2013.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bullock R., Zauner A., Woodward J.J., Myseros J., Choi S.C., Ward J.D., Marmarou A., Young H.F. Factors affecting excitatory amino acid release following severe human head injury. J. Neurosurg. 1998;89:507–518. doi: 10.3171/jns.1998.89.4.0507. [DOI] [PubMed] [Google Scholar]
- 106.Khanna S., Briggs Z., Rink C. Inducible glutamate oxaloacetate transaminase as a therapeutic target against ischemic stroke. Antioxid. Redox Signal. 2015;22:175–186. doi: 10.1089/ars.2014.6106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Swerdlow R., Lyons K., Khosla S., Nashatizadeh M., Pahwa R. A pilot Study of oxaloacetate 100 mg capsules in Parkinson’s disease patients. J. Parkinsons Dis. Alzheimers Dis. 2016;3:4. [Google Scholar]
- 108.Swerdlow R.H., Bothwell R., Hutfles L., Burns J.M., Reed G.A. Tolerability and pharmacokinetics of oxaloacetate 100 mg capsules in Alzheimer’s subjects. BBA Clin. 2016;5:120–123. doi: 10.1016/j.bbacli.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tully L., Humiston J., Cash A. Oxaloacetate reduces emotional symptoms in premenstrual syndrome (PMS): Results of a placebo-controlled, cross-over clinical trial. Obstet. Gynecol. Sci. 2020;63:195–204. doi: 10.5468/ogs.2020.63.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.McGirr A., Berlim M., Bond D., Fleck M., Yatham L., Lam R. A systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials of ketamine in the rapid treatment of major depressive episodes. Psychol. Med. 2015;45:693–704. doi: 10.1017/S0033291714001603. [DOI] [PubMed] [Google Scholar]
- 111.Baeken C., Lefaucheur J.-P., Van Schuerbeek P. The impact of accelerated high frequency rTMS on brain neurochemicals in treatment-resistant depression: Insights from 1H MR spectroscopy. Clin. Neurophysiol. 2017;128:1664–1672. doi: 10.1016/j.clinph.2017.06.243. [DOI] [PubMed] [Google Scholar]
- 112.Gabbay V., Bradley K., Mao X., Ostrover R., Kang G., Shungu D. Anterior cingulate cortex γ-aminobutyric acid deficits in youth with depression. Transl. Psychiatry. 2017;7:e1216. doi: 10.1038/tp.2017.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chen L.P., Dai H.Y., Dai Z.Z., Xu C.T., Wu R.H. Anterior cingulate cortex and cerebellar hemisphere neurometabolite changes in depression treatment: A 1H magnetic resonance spectroscopy study. Psychiatry Clin. Neurosci. 2014;68:357–364. doi: 10.1111/pcn.12138. [DOI] [PubMed] [Google Scholar]
- 114.Musazzi L., Treccani G., Mallei A., Popoli M. The action of antidepressants on the glutamate system: Regulation of glutamate release and glutamate receptors. Biol. Psychiatry. 2013;73:1180–1188. doi: 10.1016/j.biopsych.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 115.Kraal A.Z., Arvanitis N.R., Jaeger A.P., Ellingrod V.L. Could dietary glutamate play a role in psychiatric distress? Neuropsychobiology. 2020;79:13–19. doi: 10.1159/000496294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pal M.M. Glutamate: The Master Neurotransmitter and Its Implications in Chronic Stress and Mood Disorders. Front. Hum. Neurosci. 2021;15:722323. doi: 10.3389/fnhum.2021.722323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Altamura C.A., Mauri M.C., Ferrara A., Moro A.R., D’Andrea G., Zamberlan F. Plasma and platelet excitatory amino acids in psychiatric disorders. Am. J. Psychiatry. 1993;150:1731–1733. doi: 10.1176/ajp.150.11.1731. [DOI] [PubMed] [Google Scholar]
- 118.Zlotnik A., Ohayon S., Gruenbaum B.F., Gruenbaum S.E., Mohar B., Boyko M., Klin Y., Sheiner E., Shaked G., Shapira Y. Determination of factors affecting glutamate concentrations in the whole blood of healthy human volunteers. J. Neurosurg. Anesthesiol. 2011;23:45–49. doi: 10.1097/ANA.0b013e3181f82a8f. [DOI] [PubMed] [Google Scholar]
- 119.Morrell C.N., Sun H., Ikeda M., Beique J.-C., Swaim A.M., Mason E., Martin T.V., Thompson L.E., Gozen O., Ampagoomian D. Glutamate mediates platelet activation through the AMPA receptor. J. Exp. Med. 2008;205:575–584. doi: 10.1084/jem.20071474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Morimoto R., Uehara S., Yatsushiro S., Juge N., Hua Z., Senoh S., Echigo N., Hayashi M., Mizoguchi T., Ninomiya T. Secretion of L-glutamate from osteoclasts through transcytosis. EMBO J. 2006;25:4175–4186. doi: 10.1038/sj.emboj.7601317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zlotnik A., Gruenbaum B.F., Mohar B., Kuts R., Gruenbaum S.E., Ohayon S., Boyko M., Klin Y., Sheiner E., Shaked G. The effects of estrogen and progesterone on blood glutamate levels: Evidence from changes of blood glutamate levels during the menstrual cycle in women. Biol. Reprod. 2011;84:581–586. doi: 10.1095/biolreprod.110.088120. [DOI] [PubMed] [Google Scholar]
- 122.Chang L., Jiang C.S., Ernst T. Effects of age and sex on brain glutamate and other metabolites. Magn. Reson. Imaging. 2009;27:142–145. doi: 10.1016/j.mri.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Boyko M., Kuts R., Gruenbaum B.F., Melamed I., Gruenbaum S.E., Klein M., Shapira Y., Zlotnik A. The role of hypothermia in the regulation of blood glutamate levels in naive rats. J. Neurosurg. Anesthesiol. 2013;25:174–183. doi: 10.1097/ANA.0b013e31827ee0ac. [DOI] [PubMed] [Google Scholar]
- 124.Cottell E., Hutchinson M., Simon J., Harrington M.G. Plasma glutamate levels in normal subjects and in patients with amyotrophic lateral sclerosis. Biochem. Soc. Trans. 1990;18:283. doi: 10.1042/bst0180283. [DOI] [PubMed] [Google Scholar]
- 125.Obrenovitch T.P., Urenjak J. Altered glutamatergic transmission in neurological disorders: From high extracellular glutamate to excessive synaptic efficacy. Prog. Neurobiol. 1997;51:39–87. doi: 10.1016/S0301-0082(96)00049-4. [DOI] [PubMed] [Google Scholar]
- 126.Hanigan M., Calvert C., DePeters E., Reis B., Baldwin R. Whole blood and plasma amino acid uptakes by lactating bovine mammary glands. J. Dairy Sci. 1991;74:2484–2490. doi: 10.3168/jds.S0022-0302(91)78425-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.