Abstract
Background
Although the Hybrid Emergency Room System (HERS) is a relatively novel method for treating severe trauma patients, there have been few reported cases of gunshot wound patients treated in HERS. Here we report our treatment of a unique gunshot wound case, with shock, in a HERS setting.
Case presentation
A 72-year-old male was transferred to our hospital due to a gunshot wound (GSW). He presented with left chest injuries and vital signs consistent with shock. While resuscitating the patient, including massive blood transfusion and surgery to control the damage, a subsequent computed tomography in HERS revealed the internal distribution of the birdshot and damage to the abdominal organs. Lower lobectomy of the left lung and laparotomy for gastrointestinal repair were performed. After a planned repeat operation and reconstruction of the left chest wall, he was discharged uneventfully.
Conclusions
HERS during resuscitation was useful for helping clinicians not only to find the bullets' distribution and judge the severity of injury caused by the gunshot, but also to develop subsequent therapeutic strategies for rescuing the gunshot wound patient from a life-threatening situation.
Keywords: Gunshot, GSW, Trauma, IVR-CT, Hybrid-ER
Background
The Hybrid Emergency Room System (HERS), which allows clinicians to perform all life-saving procedures (including whole-body computed tomography (CT) examination, damage control surgery, and transcatheter arterial embolization by interventional radiology) on the same table without transferring patients, is a useful system for rescuing patients with severe life-threatening injuries [1]. Use of this system is expanding in emergency medicine departments throughout Japan, and, to date, is included in more than twenty hospitals. The efficacy of HERS has been demonstrated not only in severe blunt trauma cases, but also in cases where interventional radiography or extracorporeal membrane oxygenation has been indicated [2], [3], [4]. Most severe trauma cases reported in Japan are caused by a blunt mechanism, such as a motor vehicle accident or a fall from height. Penetrating trauma injuries in Japan are typically knife stab wounds. Gunshot wounds are extremely rare in Japan, since gun control is strictly regulated by the government. Therefore, little is known about the efficacy of HERS when treating gunshot wounds.
HERS has been installed in our center since 2018. The current case report is our experience using HERS to treat a birdshot patient with shock. HERS was useful in informing the attending clinicians and trauma surgeons of the projectiles' distribution in the abdominal cavity, allowing for immediate minimum laparotomy and thoracotomy for multiple visceral injuries. We think our experience with this unique case will help physicians who use HERS when encountering gunshot wound patients in the future.
Case presentation
A 72-year-old male was transported to our hospital in severe condition with a gunshot wound after a suicide attempt. He shot himself in the left chest wall with birdshot. An emergency physician onboard the helicopter emergency medical service performed endotracheal intubation and chest drainage tube insertion. On hospital arrival, the patient's vital signs were as follows; heart rate 140 bpm, blood pressure 48/15 mmHg, Glasgow coma scale E1VTM4 under sedative drugs.
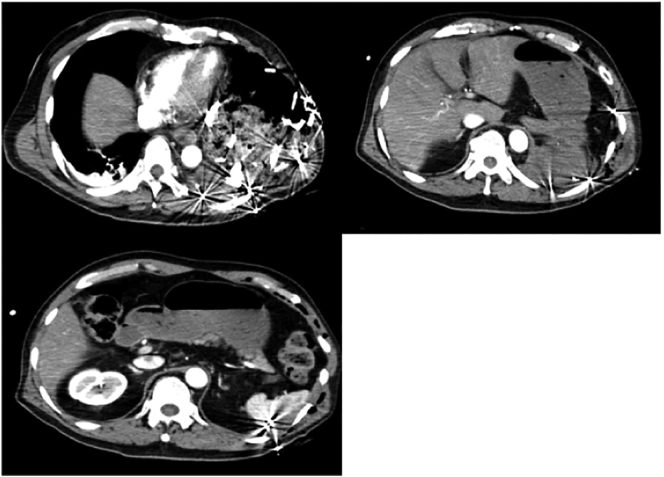
The patient's left thoracic wall was damaged severely, to the point of being destroyed (Fig. 1). Immediate thoracic exploration revealed massive hemothorax, severe left lung injuries, multiple rib fractures, diaphragm injury, and diaphragmatic herniation into the thoracic cavity. Neither cardiac nor pericardiac injury was found. The thoracic cavity and left lung were the main bleeding sites. Therefore, to control massive hemorrhaging, partial resection of the left lung was performed using a linear stapler, as well as gauze packing and administration of blood products, all in the hybrid emergency room. After his hemorrhaging was controlled and his vital signs stabilized, a subsequent CT was performed while the patient was still in the emergency department, within 22 min of his arrival at the hospital. The CT showed us the pellets' distribution in the abdominal cavity. Presumably, some pellets changed direction after deflecting off the rib bones, resulting in damage to abdominal organs, including the spleen and gastrointestinal tract (Fig. 2). To repair active intra-abdominal bleeding seen on the patient's CT scan, the patient was transported to the operating room, with placement of a double lumen endotracheal tube, for definitive surgery to repair his ruptured gastrointestinal tract and resect his severely damaged lung via thoracotomy/laparotomy. Subsequently, the patient underwent a thoracotomy for anatomical lower lobectomy of the left lung and an upper median laparotomy for repairs of the gastrointestinal tract, spleen, and diaphragm, accompanied by transfusion of twenty units of red blood cells and fresh frozen plasma. The next day, the patient's left chest wall was reconstructed by plastic surgeons. He was discharged uneventfully, and transferred to a hospital for psychiatric illness on the 22nd day of hospitalization (Fig. 3).
Fig. 1.
(Left) Left thoracic wall defect and multiple rib fractures caused by gunshot wound.
(Right) Chest X-ray after the operation.
Fig. 2.
Computed tomography revealed lung injury and abdominal visceral injuries.
Fig. 3.

Timeline of this gunshot wound patients.
Discussion
Gunshot wound patients present with a wide range of trauma severity. Similar to any type of injury, emergent surgical intervention is required if the patients show life-threatening pathologies or are hemodynamically unstable. Delaying transport of hypotensive gunshot patients with torso injuries to the operating room leads to increased mortality [5], [6]. Diagnostic laparotomy should be considered for patients without any identified or strongly suspected operative injuries, and non-operative management of appropriately selected patients with selective use of CT may also be feasible [7]. However, mortality increases with time if the patients need surgical control and repair [8]. Algorithms for management and evaluation of gunshot wounds recommend a rapid bedside survey of patients, including X-ray (abdominal, pelvis, chest) and eFAST (extended Focused Assessment of Ultrasonography for Trauma), unless patients present with hemodynamic instability, peritonitis, evisceration, hematemesis, gross blood per rectum, and austere setting [9]. While these examinations are safe and useful methods for detecting massive hemorrhaging, they are not as reliable for identifying the location and severity of ongoing organ damage [10]. In the case reported here, the rupture of the patient's diaphragm caused a pneumoperitoneum, inhibiting a thorough examination of his organ injuries by ultrasonography; physicians therefore were not able to evaluate the location of damaged organs, the severity of the damage, or the amount of bleeding without a CT exam.
As an advanced evaluation, CT has a high sensitivity and specificity to detect the location of projectiles and their trajectories [11], [12]. Among hemodynamically stable gunshot wound patients, screening by CT scan is a beneficial method for evaluating organ damage [13]. Since our CT findings revealed which specific organs were damaged in the abdominal cavity (the spleen and gastrointestinal tract), the trauma surgeon performed a minimal upper median incision, avoiding the extra trauma of an exploratory laparotomy through a midline incision from xiphoid to pubis. Before HERS was introduced in our hospital, we developed a trauma resuscitation protocol called “direct-in to operating room,” triggered by thoracic/abdominal visceral injuries with shock that need a big incision, (a trauma incision) to explore the damaged organ. In most stab wound cases, the trajectory of the knife is simple and predictable, precluding the need for CT evaluation in favor of local wound exploration via laparotomy [14]. However, gunshot wounds, especially by shotgun, cause complicated injuries. Detecting each pellets' location is difficult and time consuming. In our case, use of CT in the HERS identified the specific injuries to the patient's viscera, making it possible to perform definitive surgery soon after his arrival to the hospital.
One of the most valuable aspects of HERS is to allow clinicians to perform CT evaluation even in the middle of resuscitation. Traditionally, Advanced Trauma Life Support protocols recommend CT evaluation after a primary survey for hemodynamically stable patients [15]. However, HERS can be applied as a part of the primary survey in an advanced strategy against trauma cases [1]. In this case, HERS helped us rescue a patient with multiple risk factors from a nearly-lethal gunshot wound by rapidly diagnosing his thoracic/abdominal visceral injuries via a whole body CT, followed by immediate repair of his injuries by thoracotomy and minimum laparotomy procedures [16]. Use of the HERS protocol for trauma patients in our medical center is limited to resuscitative damage control surgery in the hybrid emergency room due to limited space and equipment, while patients who need definitive surgery, including gastrointestinal repair and anatomical lobectomy, are transported to the operating room. The CT evaluation of our gunshot wound patient showed active bleeding in both the thoracic or peritoneal cavities, which, after a brief discussion of strategy, led to him being safely transported to the operating room for gastrointestinal repair and lung lobectomy.
HERS has been developed in Japan, where gun possession is prohibited by law. Due to Japan's prolonged period of peace, Japanese emergency physicians, including trauma surgeons, have not been exposed to a sufficient number of gunshot cases [17]. Therefore, this is the first reported case of a gunshot wound patient being treated in HERS. As HERS is introduced to more hospitals and more widely used, a definitive workflow for treating gunshot wound patients in HERS will need to be established and refined, which will further improve our ability to effectively treat a wider variety of patient scenarios. We are convinced that the current report will help physicians treat gunshot wound patients more efficiently and effectively in countries where this type of trauma occurs more frequently.
Conclusions
In our current case report, CT evaluation of a gunshot wound patient during a primary survey using HERS provided surgeons with precise positions of the pellets, helping them quickly decide on a therapeutic strategy, such as resuscitative thoracotomy or laparotomy. Our use of HERS was valuable in rescuing a patient with life-threatening injuries.
Consent
Consent of publication was obtained from the patient.
Grant support
None.
Declaration of competing interest
None declared.
Acknowledgements
The authors thank Geoffrey Hummelke for editing the manuscript. The authors have no funds or grant.
References
- 1.Founding members of the Japanese Association for Hybrid Emergency Room System The hybrid emergency room system: a novel trauma evaluation and care system created in Japan. Acute Med. Surg. 2019;6(3):247–251. doi: 10.1002/ams2.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kinoshita T., Hayashi M., Yamakawa K., Watanabe A., Yoshimura J., Hamasaki T., et al. Effect of the hybrid emergency room system on functional outcome in patients with severe traumatic brain injury. World Neurosurg. 2018;118:e792–e799. doi: 10.1016/j.wneu.2018.07.053. [DOI] [PubMed] [Google Scholar]
- 3.Ito K., Nagao T., Tsunoyama T., Kono K., Tomonaga A., Nakazawa K., et al. Hybrid emergency room system improves timeliness of angioembolization for pelvic fracture. J. Trauma Acute Care Surg. 2020;88(2):314–319. doi: 10.1097/TA.0000000000002544. [DOI] [PubMed] [Google Scholar]
- 4.Miyazaki K., Hikone M., Kuwahara Y., Ishida T., Sugiyama K., Hamabe Y. Extracorporeal CPR for massive pulmonary embolism in a "hybrid 2136 emergency department". Am. J. Emerg. Med. 2019;37(12):2132–2135. doi: 10.1016/j.ajem.2019.01.039. [DOI] [PubMed] [Google Scholar]
- 5.Alarhayem A.Q., Myers J.G., Dent D., Liao L., Muir M., Mueller D., et al. Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the "golden hour". Am. J. Surg. 2016;212(6):1101–1105. doi: 10.1016/j.amjsurg.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Harvin J.A., Maxim T., Inaba K., Martinez-Aguilar M.A., King D.R., Choudhry A.J., et al. Mortality after emergent trauma laparotomy: a multicenter, retrospective study. J. Trauma Acute Care Surg. 2017;83(3):464–468. doi: 10.1097/TA.0000000000001619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meizoso J.P., Ray J.J., Karcutskie CAt, Allen C.J., Zakrison T.L., Pust G.D. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: the golden 10 minutes. J. Trauma Acute Care Surg. 2016;81(4):685–691. doi: 10.1097/TA.0000000000001198. [DOI] [PubMed] [Google Scholar]
- 8.Navsaria P.H., Nicol A.J., Edu S., Gandhi R., Ball C.G. Selective nonoperative management in 1106 patients with abdominal gunshot wounds: conclusions on safety, efficacy, and the role of selective CT imaging in a prospective single-center study. Ann. Surg. 2015;261(4):760–764. doi: 10.1097/SLA.0000000000000879. [DOI] [PubMed] [Google Scholar]
- 9.Martin M.J., Brown C.V.R., Shatz D.V., Alam H., Brasel K., Hauser C.J., et al. Evaluation and management of abdominal gunshot wounds: a Western trauma association critical decisions algorithm. J. Trauma Acute Care Surg. 2019;87(5):1220–1227. doi: 10.1097/TA.0000000000002410. [DOI] [PubMed] [Google Scholar]
- 10.Boulanger B.R., Kearney P.A., Tsuei B., Ochoa J.B. The routine use of sonography in penetrating torso injury is beneficial. J. Trauma. 2001;51(2):320–325. doi: 10.1097/00005373-200108000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Chiu W.C., Shanmuganathan K., Mirvis S.E., Scalea T.M. Determining the need for laparotomy in penetrating torso trauma: a prospective study using triple-contrast enhanced abdominopelvic computed tomography. J. Trauma. 2001;51(5):860–868. doi: 10.1097/00005373-200111000-00007. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 12.Velmahos G.C., Constantinou C., Tillou A., Brown C.V., Salim A., Demetriades D. Abdominal computed tomographic scan for patients with gunshot wounds to the abdomen selected for nonoperative management. J. Trauma. 2005;59(5):1155–1160. doi: 10.1097/01.ta.0000196435.18073.6d. discussion 60–1. [DOI] [PubMed] [Google Scholar]
- 13.Pryor J.P., Reilly P.M., Dabrowski G.P., Grossman M.D., Schwab C.W. Nonoperative management of abdominal gunshot wounds. Ann. Emerg. Med. 2004;43(3):344–353. doi: 10.1016/s0196-0644(03)00815-1. [DOI] [PubMed] [Google Scholar]
- 14.Johnson A., Rott M., Kuchler A., Williams E., Cole F., Ramzy A., et al. Direct to operating room trauma resuscitation: optimizing patient selection and time-critical outcomes when minutes count. J. Trauma Acute Care Surg. 2020;89(1):160–166. doi: 10.1097/TA.0000000000002703. [DOI] [PubMed] [Google Scholar]
- 15.Subcommittee A, American College of Surgeons' Committee on T. International Awg Advanced trauma life support (ATLS(R)): the ninth edition. J. Trauma Acute Care Surg. 2013;74(5):1363–1366. doi: 10.1097/TA.0b013e31828b82f5. [DOI] [PubMed] [Google Scholar]
- 16.Feliciano D.V., Burch J.M., Spjut-Patrinely V., Mattox K.L., Jordan G.L., Jr. Abdominal gunshot wounds. An urban trauma center's experience with 300 consecutive patients. Ann. Surg. 1988;208(3):362–370. doi: 10.1097/00000658-198809000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uchino H., Kong V.Y., Bruce J.L., Oosthuizen G.V., Bekker W., Laing G.L., et al. Preparing japanese surgeons for potential mass casualty situations will require innovative and systematic programs. Eur. J. Trauma Emerg. Surg. 2019;45(1):139–144. doi: 10.1007/s00068-017-0871-x. [DOI] [PubMed] [Google Scholar]