Abstract
Background: Chronic kidney disease (CKD) is a common condition, characterized by high burden of comorbidities, mortality and costs. There is a need for developing and validating algorithm for the diagnosis of CKD based on administrative data. Methods: We validated our previously developed algorithm that used administrative data of the Lazio Region (central Italy) to define the presence of CKD on the basis of serum creatinine measurements performed between 2012 and 2015 at the Policlinico Gemelli Hospital. CKD and advanced CKD were defined according to eGFR (<60 and <30 mL/min/1.73 m2, respectively). Sensitivity, specificity, positive and negative predictive values (PPV/NPV) were computed. Results: During the time span of the study, 30,493 adult participants residing in the Lazio Region had undergone at least 2 serum creatinine measurements separated by at least 3 months. CKD and advanced CKD were present in 11.1% and 2.0% of the study population, respectively. The performance of the algorithm in the identification of CKD was high, with a sensitivity of 51.0%, specificity of 96.5%, PPV of 64.5% and NPV of 94.0%. Using advanced CKD, sensitivity was 62.9% (95% CI 59.0, 66.8), specificity 98.1%, PPV 40.4% and NPV 99.3%. Conclusion: The algorithm based on administrative data has high specificity and adequate performance for more advanced CKD; it can be used to obtain estimates of prevalence of CKD and to perform epidemiological research.
Keywords: chronic kidney disease, administrative data, serum creatinine measurements, validation, algorithm, eGFR
1. Introduction
Chronic kidney disease (CKD) is a common condition [1,2] characterized by the progressive decline of the physiological functions of the kidney and a number of abnormalities including hormonal derangements, accumulation of waste products and water and electrolyte disturbances [3]. It is a known risk factor for the development of serious adverse clinical outcomes, including cardiovascular morbidity and mortality and need for kidney replacement therapy. Hence, it is not surprising that CKD is also characterized by high costs for the health systems [4].
For the correct allocation of resources and implementation of prevention and management strategies, national and regional government bodies need to rely on estimates of disease burden. For CKD, precise estimation of prevalence is made difficult by the silent course characterizing the initial stages of the disease, before the development of complications such as cardiovascular events, anemia, fractures, metabolic acidosis, electrolyte disorders, symptoms of intoxication that finally force the patient to seek medical attention. The current definition of CKD relies on biochemical or imaging evidence of impaired kidney structure or function lasting for at least 3 months [5]. In the absence of other abnormalities, a persistently reduced estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 allows the diagnosis of CKD. It is also possible to stage disease severity according to values of eGFR and albumin-to-creatinine ratio (Supplementary Table S1). To obtain estimates of prevalence based on administrative data, thus overcoming the limitations of having to rely on repeated determinations of eGFR (whose estimation is in turn based on serum creatinine), we previously developed and published an algorithm based on health information systems of the Lazio Region, Italy [6]. Such approach has several advantages, including the possibility to export the algorithm to health systems with similar information systems and the immediate availability of data. The purpose of this study was to determine the validity of our algorithm based on administrative data for identifying patients with CKD compared to the reference standard of eGFR.
2. Materials and Methods
2.1. Data Sources
2.1.1. Laboratory Data
Information on serum creatinine was obtained from the central laboratory of the Gemelli Hospital, an academic medical centre in Rome, Lazio, as part of a study on clinical outcomes of patients affected with CKD (local Ethics Committe protocol number 47284/17). The Hospital is a tertiary care centre and serves patients from southern and central Italy. The data contain all laboratory measurements prescribed during hospitalization or emergency room access or ambulatory care. Those data were used to identify participants with CKD.
2.1.2. Health Administrative Data
The procedure followed to generate the algorithm has been already described [6]. Briefly, Lazio Regional Health Information Systems (HIS) used to perform the CKD algorithms were the following: hospital discharge registry, ticket exemption registry (a registry of all residents who are entitled to co-pay fee exemption for particular conditions, e.g., disability, chronic diseases, low income or old age), outpatient specialist service information system and drug dispensing registry. Regional health assistance file was used to assess the residence of individuals and regional mortality registry was used to assess vital status.
2.2. Study Population
All individuals who had undergone at least 2 serum creatinine measurements separated by at least 3 months in the period 1 January 2012–31 January 2015 were potential subjects to be included. For each participant, the last creatinine measurement was selected, and the date of the measurement was defined as index date. Participants younger than 19 years and those who were not resident in the Lazio Region during the 5 years before and 1 year after the index date were excluded.
2.3. Measure of Kidney Function and Definition of CKD
eGFR was estimated using the recently developed race-free CKD-EPI equation [7]. CKD and advanced CKD were defined as the presence of the most recent eGFR values < 60 and < 30 mL/min/1.73 m2, respectively, separated by at least 3 months from another eGFR value < 60 mL/min/1.73 m2. They were used as the working standard indicating presence of CKD or presence of advanced CKD. Serum creatinine was measured with the enzymatic method; measurements from both inpatient and outpatient events were used.
2.4. Health Administrative Data Definitions of CKD
Participants were linked by the regional anonymous personal code with the HIS necessary to implemented our previously developed algorithm for the diagnosis of CKD in a period of 6 years around the index date (5 year before and 1 year after). In Table S2 were presented all codes used to perform the algorithm, for each HIS [6].
Furthermore, among patients with CKD, those with advanced stages of CKD were identified. Higher severity patients were subjects who during the selection period had undergone chronic dialysis or at least one kidney transplant or one hospitalization with diagnosis code of CKD stage G4 or greater, or who had been prescribed at least one of the drugs selected in the algorithm (erythropoietin, darbepoetin alfa, methoxy polyethylene glycol-epoetin beta, polystyrene sulfonate, sevelamer, lanthanum carbonate, sucroferric oxyhydroxide) [6].
2.5. Statistical Analysis
Descriptive analysis was used to describe demographic characteristics of the study population, stratified by CKD stages assessed at the last serum creatinine measurement. Furthermore, the study population was described according to the presence or absence of CKD-working standard and CKD-algorithm, both for CKD cases and advanced cases. Estimates of sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) with 95% confidence intervals (CIs) were generated using 2 × 2 tables. All validity measurements were calculated by sex and age groups (19–44, 45–64, 65–74, 75–84, 85+ years).
A sensitivity analysis was performed restricting the study population to those with serum creatinine measurements in the outpatient setting.
Statistical analyses were done using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
3. Results
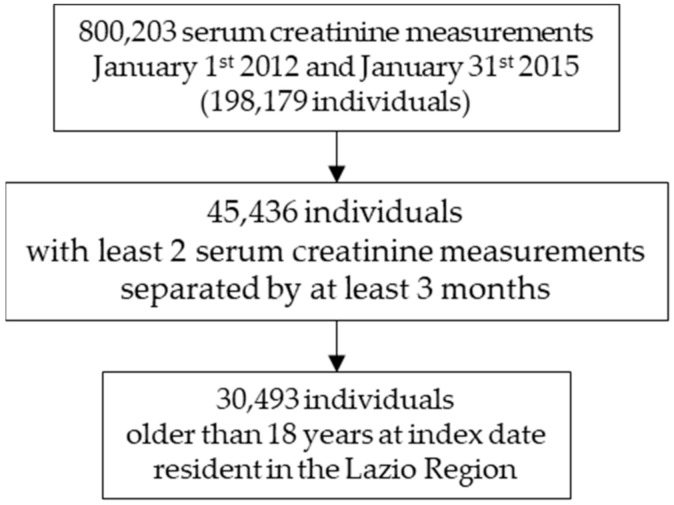
During the time span between 1 January 2012 and 31 January 2015, data from 800,203 serum creatinine measurements from 198,179 individuals were performed. Of those, 45,436 participants had undergone at least 2 serum creatinine measurements separated by at least 3 months. At index date, 30,493 individuals were older than 18 years and resident in the Lazio Region during the period 5 years before and 1 year after the index date (Figure 1). Men were 40.8% and mean age was 57.3 years (SD 17.9), with men being on average older than women (60.2 vs. 55.4 years, p-value t test < 0.0001). Their baseline characteristics are presented in Table 1.
Figure 1.
Flow-chart of study population selection.
Table 1.
Distribution of Chronic Kidney Disease CKD stages based on the CKD-EPI equation *, by sex.
| Total | Male | Female | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| 30,493 | 12,427 | 40.8 | 18,066 | 59.2 | ||
| Age, years (mean (SD)) | 57.3 | (17.9) | 60.2 | (16.9) | 55.4 | (8.3) |
| Age class (years) | ||||||
| 19–44 | 8354 | 27.4 | 2400 | 19.3 | 5954 | 33.0 |
| 45–64 | 9826 | 32.2 | 4242 | 34.1 | 5584 | 30.9 |
| 65–74 | 6179 | 20.3 | 2977 | 24.0 | 3202 | 17.7 |
| 75–84 | 4827 | 15.8 | 2275 | 18.3 | 2552 | 14.1 |
| 85+ | 1307 | 4.3 | 533 | 4.3 | 774 | 4.3 |
| CKD stage | ||||||
| eGFR ≥ 60 mL/min/1.73 m2 | 27,109 | 88.9 | 10,737 | 86.4 | 16,372 | 90.6 |
| eGFR 45–59 mL/min/1.73 m2 | 1749 | 5.7 | 859 | 6.9 | 890 | 4.9 |
| eGFR 30–44 mL/min/1.73 m2 | 1034 | 3.4 | 524 | 4.2 | 510 | 2.8 |
| eGFR 29–15 mL/min/1.73 m2 | 406 | 1.3 | 190 | 1.5 | 216 | 1.2 |
| eGFR < 15 mL/min/1.73 m2 | 195 | 0.6 | 117 | 0.9 | 78 | 0.4 |
* CKD-EPI equation is the recently developed race-free equation to estimate the glomerular filtration rate (eGFR) [7].
Based on the definition of CKD as eGFR consistently < 60 mL/min/1.73 m2, CKD was present in 11.1% (95% CI 10.8, 11.5) of the study population. The prevalence was higher among men compared with women (13.6% vs. 9.4%, p-value χ2 < 0.0001) and increased with age, ranging from 1.1% (95% CI 0.9, 1.3) among those aged between 19 and 44 years up to 47.6% (95% CI 44.9, 50.3) among those aged 85+ years. Advanced CKD (eGFR < 30 mL/min/1.73 m2) was present in 2.0% (95% CI 1.8, 2.1) of the study population, with trends similar to CKD across sex and age (Table 2). The prevalence of CKD and severe CKD based on the diagnostic algorithm was 8.8% (95% CI 8.5, 9.1) and 3.1% (CI 95% 2.9, 3.3), respectively, with trends similar to CKD patients across sex and age class (Table 2).
Table 2.
Characteristics of patients with or without Chronic Kidney Disease CKD-working standard (WS) and CKD-algorithm (AL) and prevalence of CKD in both definitions, by sex and age class.
| No CKD (WS) | CKD (WS) | No CKD (WS) | CKD (WS) | CKD (WS) | CKD (AL) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No CKD (AL) | No CKD (AL) | CKD (AL) | CKD (AL) | Prevalence % | 95% CIs | Prevalence % | 95% CIs | |||||||
| N | % | N | % | N | % | N | % | Inf | Sup | Inf | Sup | |||
| eGFR * < 60 mL/min/1.73 m2/algorithm for identification of CKD | ||||||||||||||
| Total | 26,160 | 1660 | 949 | 1724 | 11.1 | 10.8 | 11.5 | 8.8 | 8.5 | 9.1 | ||||
| Sex | ||||||||||||||
| Male | 10,159 | 38.8 | 676 | 40.7 | 578 | 60.9 | 1014 | 58.8 | 13.6 | 13.0 | 14.2 | 12.8 | 12.2 | 13.4 |
| Female | 16,001 | 61.2 | 984 | 59.3 | 371 | 39.1 | 710 | 41.2 | 9.4 | 9.0 | 9.8 | 6.0 | 5.6 | 6.3 |
| Age class (years) | ||||||||||||||
| 19–44 | 8102 | 31.0 | 13 | 0.8 | 159 | 16.8 | 80 | 4.6 | 1.1 | 0.9 | 1.3 | 2.9 | 2.5 | 3.2 |
| 45–64 | 9060 | 34.6 | 129 | 7.8 | 309 | 32.6 | 328 | 19.0 | 4.7 | 4.2 | 5.1 | 6.5 | 6.0 | 7.0 |
| 65–74 | 5085 | 19.4 | 464 | 28.0 | 221 | 23.3 | 409 | 23.7 | 14.1 | 13.3 | 15.0 | 10.2 | 9.5 | 11.0 |
| 75–84 | 3272 | 12.5 | 720 | 43.4 | 216 | 22.8 | 619 | 35.9 | 27.7 | 26.5 | 29.0 | 17.3 | 16.2 | 18.4 |
| 85+ | 641 | 2.5 | 334 | 20.1 | 44 | 4.6 | 288 | 16.7 | 47.6 | 44.9 | 50.3 | 25.4 | 23.1 | 27.8 |
| eGFR * < 30 mL/min/1.73 m2/algorithm for identification of advanced CKD | ||||||||||||||
| Total | 29,334 | 223 | 558 | 378 | 2.0 | 1.8 | 2.1 | 3.1 | 2.9 | 3.3 | ||||
| Sex | ||||||||||||||
| Male | 11,777 | 40.1 | 92 | 41.3 | 343 | 61.5 | 215 | 56.9 | 2.5 | 2.2 | 2.7 | 4.5 | 4.1 | 4.9 |
| Female | 17,557 | 59.9 | 131 | 58.7 | 215 | 38.5 | 163 | 43.1 | 1.6 | 1.4 | 1.8 | 2.1 | 1.9 | 2.3 |
| Age class (years) | ||||||||||||||
| 19–44 | 8232 | 28.1 | 4 | 1.8 | 90 | 16.1 | 28 | 7.4 | 0.4 | 0.3 | 0.5 | 1.4 | 1.2 | 1.7 |
| 45–64 | 9480 | 32.3 | 29 | 13.0 | 215 | 38.5 | 102 | 27.0 | 1.3 | 1.1 | 1.6 | 3.2 | 2.9 | 3.6 |
| 65–74 | 5937 | 20.2 | 46 | 20.6 | 104 | 18.6 | 92 | 24.3 | 2.2 | 1.9 | 2.6 | 3.2 | 2.7 | 3.6 |
| 75–84 | 4527 | 15.4 | 86 | 38.6 | 104 | 18.6 | 110 | 29.1 | 4.1 | 3.5 | 4.6 | 4.4 | 3.9 | 5.0 |
| 85+ | 1158 | 3.9 | 58 | 26.0 | 45 | 8.1 | 46 | 12.2 | 8.0 | 6.5 | 9.4 | 7.0 | 5.6 | 8.3 |
* eGFR: estimate Glomerular Filtration Rate [7].
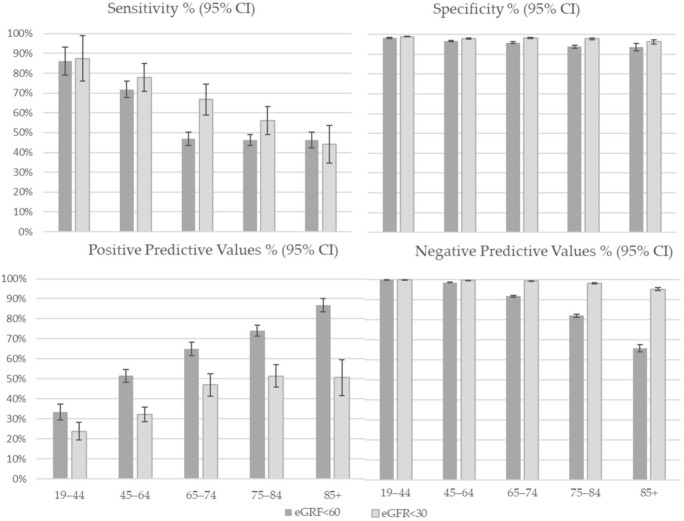
The performance of the algorithm in the identification of CKD was high, with a sensitivity of 51.0% (95% CI 49.3, 52.6), specificity of 96.5% (95% CI 96.3, 96.7), PPV of 64.5% (95% CI 62.9, 66.1) and NPV of 94.0% (95% CI 93.8, 94.2). Sensitivity was higher among men than women (60.0% vs. 41.9%) while specificity was slightly higher among women (97.9 vs. 94.6) (Table 3); both validity measures decreased with increase of age classes: sensitivity was 86.0% in age group 19–44 years and 46.3% in age group 85+ years and specificity was 98.1 and 93.6 in the same age classes (Figure 2). Using advanced CKD, all validity parameters improved except for a slight reduction in PPV. Sensitivity was 62.9% (95% CI 59.0, 66.8), specificity 98.1% (95% CI 98.0, 98.3), PPV 40.4% (95% CI 37.9, 42.9) and NPV 99.3% (95% CI 99.2, 99.3) (Table 3). The differences between sex and age groups were maintained (Figure 2).
Table 3.
Validity of Chronic Kidney Disease (CKD) definitions on administrative data compared with the estimate Glomerular Filtration Rate (eGFR) reference standard, by sex.
| Sensitivity | 95% CIs | Specificity | 95% CIs | PPV * | 95% CIs | NPV ^ | 95% CIs | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| eGFR < 60 mL/min/1.73 m2/algorithm for identification of CKD | ||||||||||||
| Total | 51.0 | 49.3 | 52.6 | 96.5 | 96.3 | 96.7 | 64.5 | 62.9 | 66.1 | 94.0 | 93.8 | 94.2 |
| Sex | ||||||||||||
| Male | 60.0 | 57.7 | 62.3 | 94.6 | 94.2 | 95.0 | 63.7 | 61.7 | 65.7 | 93.8 | 93.4 | 94.1 |
| Female | 41.9 | 39.6 | 44.3 | 97.7 | 97.5 | 98.0 | 65.7 | 63.1 | 68.3 | 94.2 | 94.0 | 94.4 |
| eGFR < 30 mL/min/1.73 m2/algorithm for identification of advanced CKD | ||||||||||||
| Total | 62.9 | 59.0 | 66.8 | 98.1 | 98.0 | 98.3 | 40.4 | 37.9 | 42.9 | 99.3 | 99.2 | 99.3 |
| Sex | ||||||||||||
| Male | 70.0 | 64.9 | 75.2 | 97.2 | 96.9 | 97.5 | 38.5 | 35.5 | 41.6 | 99.2 | 99.1 | 99.4 |
| Female | 55.4 | 49.8 | 61.1 | 98.8 | 98.6 | 99.0 | 43.1 | 39.0 | 47.2 | 99.3 | 99.2 | 99.4 |
* PPV: positive predictive values. ^ NPV: negative predictive values.
Figure 2.
Validity of CKD definitions on administrative data compared with the eGFR reference standard, by age class.
Results were substantially unmodified after restricting the analysis to serum creatinine determinations performed in the outpatient setting (Supplementary Tables S3 and S4).
4. Discussion
In our study, we sought to validate our previously developed algorithm based on administrative data. After linkage with a large database of inpatient and outpatient serum creatinine measurements, we defined the presence of CKD according to repeated eGFR determinations and computed the proportion of participants who were correctly classified by the algorithm as affected or not affected by CKD during a time span covering of 5 years before and 1 year after the date of CKD status definition.
Overall, we found a prevalence of CKD of about 11%. This figure is at odds with previous reports of CKD prevalence in the Italian population. For instance, the prevalence of CKD in the Northeastern Italy INCIPE study was about 13% overall, but only 6.7% when considering stages G3 or worse, which is the definition of CKD used in our study [1]. This discrepancy might in part be due to differences in the study populations, with the INCIPE cohort including a random sample of the general population whereas our sample was selected based on having at least one laboratory measurement performed at the Gemelli Hospital: this approach might have selected a less healthy population in our study. Another potential explanation is that a single determination of serum creatinine might have misclassified some INCIPE participants as non-CKD. Similar considerations apply to the CARHES study, a national survey reporting an even lower prevalence of CKD stage G3 or worse of about 2.9% [8].
We found that 1724 (51.0%) of the 3384 CKD participants and 26,160 (96.5%) of the 27,109 non-CKD participants were correctly classified by the algorithm. When focusing on advanced CKD, 378 (62.9%) of the 601 CKD participants and 29,334 (98.1%) of the 29,892 non-CKD participants were correctly classified. Taken together, these findings suggest that the overall performance of the algorithm is adequate, although it tends to underestimate true CKD, especially the milder forms. This is not unexpected given that the algorithm is based on utilization of healthcare resources, and initial and milder stages of CKD, being generally asymptomatic or paucisymptomatic, might remain undetected. Depending on the setting and on whether a broader or stricter definition of CKD is desired, the algorithm for the prediction of more severe CKD could be used, resulting in an increase in both sensitivity and specificity. However, the algorithm appears to be cost-effective given that no additional resources (both in monetary and person-time terms) are needed to generate its output, the input being constituted of mandatory, administrative data available to all regional health systems in Italy. A further advantage of the algorithm is the possibility to provide estimates of kidney function status for epidemiological research studies, with the possibility to use such estimates as exposure/confounder/outcome variables.
To date, several validation studies have been published, mainly in North America; however, due to heterogeneity of methodology and a variety of data sources, comparing results is difficult. In the systematic review of Vlasschaert et al., the authors conducted a comprehensive global review of 25 studies, quantifying the accuracy of codes for acute kidney injury and CKD. Given the heterogeneity of results, they did not perform a meta-analysis and concluded that the administrative database analyses have utility, but must be conducted and interpreted judiciously to avoid bias arising from poor code validity [9]. In another review, Grams at al. explain that their results show large variability in the accuracy of data items, depending on the variable of interest, study population and the comparison gold standard; so additional research is required to investigate sources of this variation and conclude that existing data sources need careful scrutiny before use in any research effort and that an electronic medical record integrated with laboratory and vital status data would greatly facilitate clinical and epidemiologic research [10]. Moreover, an Italian review (published in 2019) concludes on the need for further effort to improve algorithms for identification of CKD especially for early stages [11]. We found a PPV for eGFR < 60 mL/min/1.73 m2 lower than that reported in a recent large study from the US (64.5% vs. 84.4%), but trends across age classes and gender were similar [12]. In a study conducted in Canada (2020) in a population of just over 400 individuals, different algorithms were validated to identify patients with eGFR < 30 mL/min/1.73 m2, not on kidney replacement treatment (dialysis or kidney transplantation), authors found sensitivity and PPV higher and specificity and VPN lower than in our study [13].
We found that the performance of our algorithm was affected by sex: in particular, sensitivity was higher among men and specificity among women. This phenomenon could be due to differential access to healthcare; for instance, previous work from our group demonstrated that women have significantly lower odds of arteriovenous fistula placement compared with men [14]. Alternatively, women might develop CKD symptoms and signs at lower GFR values compared with men; this is a field in which active research is warranted [15,16].
We also found that age affected the performance of our algorithm, with both sensitivity and specificity reduced among older participants; this could be due, again, to differential access to healthcare across age groups, and/or to potential overestimation of CKD among older participants, giving rise to a higher proportion of CKD cases that would not need specific access to kidney care. However, alternative explanations could be hypothesized; for instance, older individuals might already have ticket exemptions for other conditions, or not receive a discharge diagnosis of CKD due to the number and severity of other comorbidities (thus diminishing the likelihood of being flagged with those criteria). The topic of CKD definition among the elderly is debated, and our results strengthen the idea that age-specific cutoffs for the definition of CKD should be used [17].
Our study has several strengths, including the large sample size accrued over a long time span, the possibility to analyze separately outpatient serum creatinine measurements and CKD defined at different thresholds, the implementation of recently developed eGFR equations and of the working standard definition of CKD, requiring chronic GFR reduction over time; with regard to the latter point, previous studies have shown that using a single serum creatinine measurement might have a significant impact on the definition of CKD [18]. Our study also has limitations, including the non-random sampling (individuals who elect to access the laboratory of a tertiary hospital might not represent the general adult population of the Lazio Region), lack of information on race and socio-economic status, and relatively low sensitivity especially for moderate CKD, causing a non-trivial rate of false negatives. Administrative data are known to have limitations in retrieving details in clinical information however the impact could be limited because our algorithm is used for epidemiological research and not for a diagnostic test.
5. Conclusions
In conclusion, our previously developed algorithm based on administrative data has high specificity and adequate performance for more advanced CKD and can be used to obtain estimates of prevalence of CKD and to perform epidemiological research. Future studies will include the implementation of more detailed laboratory data such as serum cystatin C and urinary albumin excretion as well as the extension of our model to a multi-regional setting to obtain and compare estimates of CKD at the national level.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11102711/s1, Table S1: Staging of CKD according to KDIGO. Table S2: Diagnosis (code = ICD-9-CM), procedures (code = ICD-9-CM), outpatient services (code = Regional codification) and drugs (code = ATC), name and code. Table S3: Characteristics of patients with CKD-working standard and CKD-algorithm and prevalence of CKD in both definitions; by sex and age class. Outpatient setting; Table S4: Validity of CKD definitions on administrative data compared with the eGFR reference standard, by sex and age class. Outpatient setting.
Author Contributions
Conceptualization N.A., A.M.B., M.D., P.M.F., G.G. and C.M.; methodology L.A., S.C. and C.M.; formal analysis C.M.; data curation S.C. and C.M.; writing—original draft preparation P.M.F., G.G. and C.M.; writing—review and editing N.A., L.A., A.M.B., P.M.F. and C.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Ethical Committee of Fondazione Policlinico Gemelli approved the study (Protocol number 47284/17 [1164/18], ID 1784).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
P.M.F. received consultant fees and grant support from Allena Pharmaceuticals, Alnylam, AstraZeneca, BioHealth Italia, Otsuka Pharmaceuticals, Vifor Fresenius, and royalties as an author for UpToDate. The other authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gambaro G., Yabarek T., Graziani M.S., Gemelli A., Abaterusso C., Frigo A.C., Marchionna N., Citron L., Bonfante L., Grigoletto F., et al. Prevalence of CKD in northeastern Italy: Results of the INCIPE study and comparison with NHANES. Clin. J. Am. Soc. Nephrol. 2010;5:1946–1953. doi: 10.2215/CJN.02400310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brück K., Stel V.S., Gambaro G., Hallan S., Völzke H., Ärnlöv J., Kastarinen M., Guessous I., Vinhas J., Stengel B., et al. CKD Prevalence Varies across the European General Population. J. Am. Soc. Nephrol. 2016;27:2135–2147. doi: 10.1681/ASN.2015050542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brück K., Jager K.J., Zoccali C., Bello A.K., Minutolo R., Ioannou K., Verbeke F., Völzke H., Arnlöv J., Leonardis D., et al. Different rates of progression and mortality in patients with chronic kidney disease at outpatient nephrology clinics across Europe. Kidney Int. 2018;93:1432–1441. doi: 10.1016/j.kint.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Manns B., Hemmelgarn B., Tonelli M., Au F., So H., Weaver R., Quinn A.E., Klarenbach S., Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease The Cost of Care for People with Chronic Kidney Disease. Can. J. Kidney Health Dis. 2019;6:2054358119835521. doi: 10.1177/2054358119835521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levin A., Stevens P.E., Bilous R.W., Coresh J., De Francisco A.L., De Jong P.E., Griffith K.E., Hemmelgarn B.R., Iseki K., Lamb E.J., et al. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013;3:4. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 6.Marino C., Ferraro P.M., Bargagli A.M., Cascini S., Agabiti N., Gambaro G., Davoli M. Prevalence of chronic kidney disease in the Lazio region, Italy: A classification algorithm based on health information systems. BMC Nephrol. 2020;21:23. doi: 10.1186/s12882-020-1689-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delgado C., Baweja M., Crews D.C., Eneanya N.D., Gadegbeku C.A., Inker L.A., Mendu M.L., Miller W.G., Moxey-Mims M.M., Roberts G.V., et al. A Unifying Approach for GFR Estimation: Recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease. Am. J. Kidney Dis. 2021;79:268–288.e1. doi: 10.1053/j.ajkd.2021.08.003. [DOI] [PubMed] [Google Scholar]
- 8.De Nicola L., Donfrancesco C., Minutolo R., Noce C.L., Palmieri L., De Curtis A., Iacoviello L., Zoccali C., Gesualdo L., Conte G., et al. Prevalence and cardiovascular risk profile of chronic kidney disease in Italy: Results of the 2008-12 National Health Examination Survey. Nephrol. Dial. Transplant. 2015;30:806–814. doi: 10.1093/ndt/gfu383. [DOI] [PubMed] [Google Scholar]
- 9.Vlasschaert M.E., Bejaimal S.A., Hackam D.G., Quinn R., Cuerden M.S., Oliver M.J., Iansavichus A., Sultan N., Mills A., Garg A.X. Validity of administrative database coding for kidney disease: A systematic review. Am. J. Kidney Dis. 2011;57:29–43. doi: 10.1053/j.ajkd.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Grams M.E., Plantinga L.C., Hedgeman E., Saran R., Myers G.L., Williams D.E., Powe N.R. CDC CKD Surveillance Team Validation of CKD and related conditions in existing data sets: A systematic review. Am. J. Kidney Dis. 2011;57:44–54. doi: 10.1053/j.ajkd.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Domenicantonio R., Cappai G., Agabiti N., Marino C., Simonato L., Canova C., Pitter G. A Systematic Review of Case-Identification Algorithms Based on Italian Healthcare Administrative Databases for Three Relevant Diseases of the Digestive and Genitourinary System: Inflammatory Bowel Diseases, Celiac Disease, and Chronic Kidney Disease. Epidemiol. Prev. 2019;43((Suppl. 2)):88–98. doi: 10.19191/EP19.4.S2.P088.095. [DOI] [PubMed] [Google Scholar]
- 12.Paik J.M., Patorno E., Zhuo M., Bessette L.G., York C., Gautam N., Kim D.H., Kim S.C. Accuracy of identifying diagnosis of moderate to severe chronic kidney disease in administrative claims data. Pharmacoepidemiol. Drug Saf. 2021;31:467–475. doi: 10.1002/pds.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy L., Zappitelli M., White-Guay B., Lafrance J.P., Dorais M., Perreault S. Agreement between Administrative Database and Medical Chart Review for the Prediction of Chronic Kidney Disease G category. Can. J. Kidney Health Dis. 2020;7 doi: 10.1177/2054358120959908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angelici L., Marino C., Umbro I., Bossola M., Calandrini E., Tazza L., Agabiti N., Davoli M., Regional Registry Dialysis. Transplant Lazio Region Gender Disparities in Vascular Access and One-Year Mortality among Incident Hemodialysis Patients: An Epidemiological Study in Lazio Region, Italy. J. Clin. Med. 2021;10:5116. doi: 10.3390/jcm10215116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cobo G., Hecking M., Port F.K., Exner I., Lindholm B., Stenvinkel P., Carrero J.J. Sex and gender differences in chronic kidney disease: Progression to end-stage renal disease and haemodialysis. Clin. Sci. 2016;130:1147–1163. doi: 10.1042/CS20160047. [DOI] [PubMed] [Google Scholar]
- 16.Carrero J.J., Hecking M., Chesnaye N.C., Jager K.J. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat. Rev. Nephrol. 2018;14:151–164. doi: 10.1038/nrneph.2017.181. [DOI] [PubMed] [Google Scholar]
- 17.Delanaye P., Jager K.J., Bökenkamp A., Christensson A., Dubourg L., Eriksen B.O., Gaillard F., Gambaro G., van der Giet M., Glassock R.J., et al. CKD: A Call for an Age-Adapted Definition. J. Am. Soc. Nephrol. 2019;30:1785–1805. doi: 10.1681/ASN.2019030238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gambaro G., Bonfante L., Abaterusso C., Gemelli A., Ferraro P.M., Marchesini S., De Conti G., D’Angelo A., Lupo A. High chronic nephropathy detection yield in CKD subjects identified by the combination of albuminuria and estimated GFR. Nephrol. Dial. Transplant. 2012;27:746–751. doi: 10.1093/ndt/gfr360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.