Abstract
Perfluorooctane sulfonate (PFOS) is a persistent, widely present organic pollutant. PFOS can enter the human body through drinking water, ingestion of food, contact with utensils containing PFOS, and occupational exposure to PFOS, and can have adverse effects on human health. Increasing research shows that the liver is the major target of PFOS, and that PFOS can damage liver tissue and disrupt its function; however, the exact mechanisms remain unclear. In this study, we reviewed the adverse effects of PFOS on liver tissue and cells, as well as on liver function, to provide a reference for subsequent studies related to the toxicity of PFOS and liver injury caused by PFOS.
Keywords: perfluorooctane sulfonate, PFOS, liver, PFAS, hepatic function, liver injury
1. Introduction
Per- and polyfluoroalkyl substances (PFAS) are organic anthropogenic compounds applied in many aspects due to their characteristics of oil and water repellence, and stability. The pollution of PFAS in the environment arises from its wide use. PFAS are receiving increasing attention due to their properties of stability, bioaccumulation, and long half-life. Recent research shows that perfluorooctane sulfonate (PFOS), one of the major PFAS, is a persistent organic pollutant that is toxic, bioaccumulative, and resistant to degradation [1]. PFOS can be present in the environment persistently and enter and accumulate in human serum, breast milk, liver, and kidney through ingestion and contact with PFOS-containing products and occupational exposure [2]. Liver is the largest digestive organ of human body and also a large metabolic organ of the body. Most toxic substances are metabolized in the liver, and will be excreted from the body through bile or urine. It is reported that PFOS is able to accumulate in liver [3]. However, it is still unknown whether PFOS can be metabolized in the liver and if damage to the liver is caused by PFOS accumulation. Therefore, it is of great significance to summarize the adverse effects of PFOS on liver and their mechanisms due to the ubiquitous nature of PFOS and the vital role of liver in metabolizing PFOS. We searched the studies on PFOS with cells, animals, and population surveys to summarize the current research on the effects of PFOS on liver.
2. Profile of PFOS
Perfluorooctane sulfonate (PFOS) is a C8 fluorocarbon compound of per- and polyfluoroalkyl substances (PFAS). PFOS is extremely persistent in the environment and there are no indications that the perfluorinated part of PFOS or PFOA could be decomposed in the environment, which makes PFOS or PFOA ubiquitous in organisms or non-organisms, even in remote areas such as the Qinghai-Tibet Plateau and the polar regions [4]. Since 1950, PFOS has been produced in large quantities around the world, posing a huge threat to the environment and human health [5]. Data for 1998–2015 show that emissions of PFOS are estimated at 1228–4930 tons and data for 1970–2012 show that emissions of PFOS precursors are estimated at 45,000 tons [6,7]. It is reported that PFOS and its precursor showed an increasing trend in the environment with time between 2009–2010 and 2018–2019 [8]. Surveys in densely populated areas of the United States and Europe found that PFOS was detected in water systems at high concentrations ranging between 97 and 1371 ng/L [9]. Moreover, the highest PFOS concentrations observed in some areas of the United States were even as high as 8,970,000 ng/L [10]. In addition, PFOS was detected in 47 fatty fish and 45 shellfish samples collected from six coastal provinces in China [11]. Serum data from 1303 participants recruited from the community of Guangzhou, China, from November 2018 to August 2019 showed a median PFOS of 14.85 ng/mL [12]. PFOS was found in the serum of more than 98% of Americans [13]. A cross-sectional study on lipids and PFOS showed that the levels of serum lipids were closely related to the exposure level of PFOS. The mean levels of serum PFOS in 2005–2006 were 22 ng/mL (median, 20 ng/mL) [14]. Plasma data collected from children in the Boston, MA, USA, area from 2007 to 2010 (median age 7.7 years) showed a median PFOS concentration of 6.2 ng/mL [15]. Data from 2015 to 2016 in the United States showed that the geometric mean of PFOS concentration in serum was 4.72 ng/mL, and the 95% CI was 4.40–5.07 ng/mL [16]. This figure is still close to or even exceeds the PFOS HBM-I value of 5 ng PFOS/mL blood plasma established by the German Human Biomonitoring Committee [17]. For human epidemiological studies and experimental animal studies, exposure to PFOS has been shown to have a variety of health effects on the body, such as hepatotoxicity, infertility, altered thyroid function, decreased immunity, neurotoxicity, developmental toxicity, reproductive toxicity, nephrotoxicity, cardiotoxicity, insulin resistance, and carcinogenic effects [18,19,20,21,22,23,24,25]. Data published by the European Food Safety Agency (EFSA) in 2012 showed that the estimated daily dietary intake of PFOS for adults was 5.2–10 ng/kg body weight (bw) [26]. In 2018, EFSA established a tolerable weekly intake (TWI) of 13 ng/kg bw per week for PFOS based on human epidemiological studies [27]. In 2006, PFOS was considered a priority substance under the EU Water Framework Directive (WFD), which restricts the production and use of PFOS throughout the European Union [28]. As a globally present environmental pollutant, PFOS was recognized as a persistent organic pollutant (POP) in 2009 and was listed in the Stockholm Convention to call for global production restrictions [29]. The Stockholm Convention has been ratified by 179 countries and measures have been introduced to restrict the production and use of PFOS [30,31], and PFOS has been phased out or banned in Canada [32], the United States [33], and the European Union [34]. However, PFOS and its related products continue to be produced and used in some developing countries due to the lack of alternative products or technologies with better cost effectiveness in certain application scenarios [35,36].
Currently, PFOS has been restricted from entering the environment and is even banned from manufacture and usage; however, PFOS is almost everywhere and persistent, which means that human beings will be exposed to PFOS for a long time. The arithmetic and geometric mean half-lives of serum elimination were 5.4 years and 4.8 years for PFOS, respectively [37,38]. Although PFOS is detected at low concentrations in the environment and organisms, it cannot be ignored that PFOS will have overt and adverse effects on human health and organisms due to its persistence and bioaccumulation worldwide [39].
3. Relationship between PFOS and the Liver
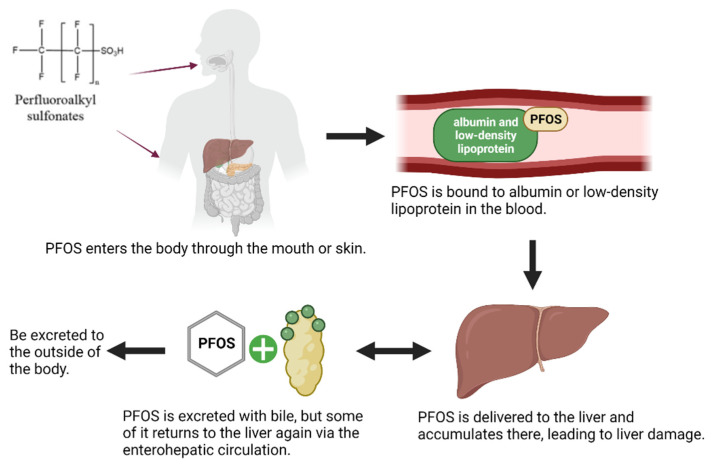
In the past ten years, the adverse effects of PFOS have emerged and the health risk of PFOS is receiving more attention from researchers [40]. The liver is the most common toxic target and is sensitive to the damage caused by foreign substances [41,42,43,44]. PFOS mainly accumulates in the organs which contain high amounts of proteins such as blood and liver, which results in the higher concentration of PFOS in the liver [45]. PFOS from other organs and blood will be transported to the liver through circulation due to its metabolic characteristics, which leads to the increased accumulation of PFOS in liver and increases the toxic risk to liver. In the human body, PFOS is mainly distributed in blood and extracellular fluid after entering the body, binding to albumin and low-density lipoprotein in blood, and circulates to all organs of the body with blood circulation [46,47]. PFOS is preferentially distributed to and accumulates in the liver during circulating distribution in the body, but it is indicated that PFOS does not seem to be metabolized in the liver or in other parts of the body, nor does it undergo any chemical reactions [48,49]. However, PFOS can be excreted through biliary excretion, and this may be the main route of PFOS excretion in humans [50]. Moreover, after being carried by bile into the intestine, some of the PFOS can be sent back to the liver through the enterohepatic circulation due to the reabsorption of bile, which may be one of the reasons for the high concentration of PFOS in the liver (Figure 1) [2,51]. Wang et al. reported that PFOS could accumulate in the liver gradually and participate in the mediation of gene expression related to lipid metabolism and inflammatory response [52]. The human serum levels of enzyme, such as acetyl coenzyme A, peroxisomal acyl-CoA oxidase 1, acyl-CoA dehydrogenase, and the mitochondrial membrane carnitine-dependent enzyme, were increased after exposure to PFOS, indicating that the liver was damaged [53]. PFOS can cause hepatic steatosis in humans and reduce postnatal survival and growth in rodents [54]. Studies in mice have also shown that PFOS accumulates most in the liver, followed by the lungs, kidneys, spleen, heart, and brain, causing the most serious damage to the liver [55]. An analysis of wild freshwater fish collected from rivers in the Pearl River Delta region of China also demonstrated that PFOS was the major PFAS in fish liver [56]. Therefore, it is particularly important to study the adverse effects of PFOS on liver.
Figure 1.
Outline diagram of PFOS entry into the body and excretion from the body.
4. Effects of PFOS on the Liver and Related Mechanisms of Toxicity
4.1. Effect of PFOS on Hepatic Lipid Metabolism
The liver is the main site of fat metabolism in the body and a hub for fat transport. The liver plays a major role in regulating lipid homeostasis through major lipid metabolic pathways, including de novo lipogenesis, fatty acid (FA) synthesis, triglyceride (TG) synthesis, and storage. In addition, there are some complex lipid anabolisms, such as cholesterol, ceramide, phospholipids, lipoprotein synthesis and secretion, and fatty acid oxidation [57]. In the context of human research, in a study that included 290 children (aged 8–10 years) from Taiwan, China, applying lipidomic approaches to examine lipid patterns in the sera of children exposed to different levels of PFAS, the data showed that PFOS was detectable in serum samples from approximately 90% of surveyed children. Upregulation of phosphatidylcholine-containing lipid sphingomyelins (SMs) levels was associated with increased serum PFOS, perfluorotridecanoic acid (PFTrDA), and perfluorodecanoic acid (PFDA) concentration. SMs are thought to be secondary messenger molecules that directly or indirectly influence intercellular or cell–organelle interactions, including insulin resistance, liver dysfunction, and obesity [58]. A recent study on human hepatocytes found that 25 μM PFOS could induce at least 7 transcripts out of 35 related to lipid metabolism, lipid transport, and antioxidant response pathways. Moreover, PFOS induced the expression of genes related to xenobiotic metabolism, such as CYP2B6 and SULT2A1, but no lipid accumulation was observed in hepatocytes [59].
For animal research, toxicological studies have shown that PFOS can induce liver enlargement by directly activating the proliferation of hepatocyte peroxisomes [60]. Moreover, PFOS can induce hepatic steatosis in mice [61]; the mechanism may be that PFOS can cause changes in lipid regulatory genes in the liver, thereby promoting the development of steatosis [62]. A study showed that PFOS administration increases liver weight and expression of genes involved in fatty acid oxidation and transport in rodents [20]. In particular, 10 and/or 5 mg/kg PFOS significantly increases the gene expression levels of fatty acid translocase (FAT/CD36) and lipoprotein lipase (Lpl), and reduces serum levels of very low density lipoproteins, and reduced rates of mitochondrial β-oxidation are also identified [63]. The quantification of gene expression related to lipid metabolism in the mouse liver showed that PFOS caused decreased expression of apolipoprotein genes (ApoA1, ApoA2, ApoB), apolipoprotein packaging gene MTTP, and lipid metabolism gene CES3, but significantly increased PPARγ mRNA levels (PPARγ mRNA is a known nuclear receptor for adipogenesis) in mice [64], which suggested that PFOS could cause the disturbance of hepatic lipid metabolism in mice. Quantification using multilayer glycoproteomics revealed that 241 dysregulated proteins were involved in lipid and xenobiotic metabolism in the liver of PFOS-exposed mice [65]. A study showed that PFOS administration exacerbated the abnormal accumulation of hepatic lipids in mice on a high-fat diet. Moreover, genomic and proteomic analyses showed that PFOS not only induced lipid production and accumulation in mouse liver, but also activated the production of some hepatic transport proteins (for example, OATPs and NTCP, two transporter proteins that have been shown to be closely associated with the transport clearance of PFOS [66]) and stimulated the metabolic pathways to accelerate the clearance of lipids and PFOS in the body [67]. A similar conclusion was drawn in the study by Marisa Pfohl et al. that PFOS increased the expression of target genes and proteins related to lipid metabolism and oxidative stress in the liver [68]. It is hypothesized that PFOS may increase the risk for hepatic metabolic and inflammatory diseases by inducing dysregulation of lipid metabolism and activating oxidative stress [69]. Paradoxically, lipid accumulation was found in rodent-related experiments after PFOS exposure, but not in human-related experiments, which may be attributed to the disparity between species, but these reasons need to be further explored in the future. Another study in zebrafish showed that chronic PFOS exposure induced hepatic steatosis in zebrafish by interfering with lipid biosynthesis, fatty acid β-oxidation, and VLDL/LDL lipoprotein excretion. Further studies showed that PFOS significantly increased the expression of nuclear receptor (NR) and fatty acid oxidation-related genes, and that disruption of NRs regulation contributed to the development and progression of several liver diseases, including fatty liver and liver fibrosis [70]. These results suggest that PFOS can cause damage to the liver by causing abnormalities in lipid metabolism in the liver.
4.2. Direct and Indirect Effects of PFOS on Maternal and Offspring Livers
In the context of human research, it has been shown that PFAS may have genotoxic and cytotoxic potential for human hepatocytes [71]. This conclusion is also supported by a European cohort study in which exposure to PFAS, including PFOS, during fetal development can cause liver injury in children [72]. In a study to detect concentrations of PFAS in fetal and corresponding placental samples and maternal serum samples from elective terminations and intrauterine deaths, it was shown that PFOS was found in all samples and tissues; the sum of all PFASs was highest in livers from mid- and late-pregnancy samples [73], which suggests that PFAS, including PFOS, can cross the placental barrier and deposit into embryonic and fetal tissues, and cause damage to their livers [74]. The results from transcriptome sequencing and bioinformatics analysis show that prenatal PFOS exposure activates fatty acid and lipid synthesis and metabolism, leading to liver damage and interfering with fetal liver development; moreover, several pro-cancer signaling pathways, including Wnt/β-catenin, Rac, and TGF-β, were also activated in fetal liver [75], which suggests that prenatal exposure to PFOS is not only hepatotoxic to the mother, but also leads to long-term liver disease in the offspring. Therefore, it is important to perform PFOS exposure assessments in women during pregnancy.
In terms of animal research, a mice experiment with utero exposure to PFOS has shown that significant hepatomegaly and steatosis occurred in the PFOS group of female rats, and increased triglyceride, total cholesterol, and LDL content and decreased HDL content were found in the liver of postnatal day 1 (PND1) mice; further analysis yielded significant changes in the expression of functional messenger RNAs for PND1 hepatocytochrome P4A14 (CYP4A14), CD36 (hepatic fatty acid uptake), apolipoprotein B100 (APOB), and fibroblast growth factor 21 (FGF21) [76]. In another study on fish chronically exposed to PFOS, it was demonstrated that long-term exposure to PFOS could produce adverse effects on lipid metabolism in both F0 and F1 generations [77]. PFOS damaged the liver structure of juvenile marine medaka by enlarging the nucleus and disrupting the cell structure, and acute exposure to PFOS affected the expression of cirrhosis-related genes at the transcriptional level [44,62]. In addition, studies in Australian finfish pups have shown that PFOS can be transferred from mother to pup through the placenta and during lactation, and can cause damage to the pups’ liver [78]. Moreover, placental transfer is the main source of PFAS in hooded seal pups and is thought to be the main route of excretion of PFAS in adult females [79]. From the above studies, we can see that parental PFOS exposure can be transferred to the liver of the zygotic embryo and fetus, thus causing a disturbance in the lipid homeostasis of the zygotic hepatocytes and leading to the occurrence of liver damage.
4.3. Effect of PFOS on Biomarkers of Liver Function
An analysis of the association between perfluorinated alkyl acid (PFAA) exposure, including PFOS, and biomarkers of liver function in adolescents (12–19 years of age) from the 2013–2016 National Health and Nutrition Examination Survey (NHANES) shows that individual serum perfluoroalkyl acids (PFAA) are closely correlated with markers of liver function, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyl transpeptidase (GGT), which can be used as a basis for analyzing the association between PFOS exposure and liver injury [80]. We determine abnormal liver function by levels of one or more biomarkers of liver function that exceed their upper limit of normal (ULN). PFOS was found to be positively correlated with alanine aminotransferase (ALT, a sensitive marker of acute hepatocellular damage) activity, and every 1 ln unit increase in PFOS exposure was associated with a 4.3% (95% CI: 1.2%, 7.4%) increase in ALT levels and a 33.0% (95% CI: 5.0%, 67.0%) increase in the odds of abnormal ALT [81,82,83,84]. In addition, recent data from China showed a positive correlation between serum concentrations of PFOS and ALT and AST levels [12]. However, this contradicts U.S. data from 2007 to 2010, where serum data showed no significant association between PFOS and AST [13]. Canadian data surprisingly showed no correlation between PFOS and either AST or ALT [85]. We speculate that this may be related to differences in region and ethnicity, and this needs to be explored further. In addition, in animal experiments, PFOS administration increased serum concentrations of ALT and AST in mice [86].
In addition, PFOS was negatively correlated with the levels of tumor necrosis factor alpha (TNFα) and interleukin 8 (IL-8), and further studies revealed that PFOS exposure was strongly associated with increased hepatocyte apoptosis biomarkers (e.g., CK18-M30) and decreased serum TNFα [87]. Previous studies from cohorts and experiments suggest that PFOS may cause liver injury and downregulate certain indicators of immune response.
4.4. Effect of PFOS on Hepatocyte Proliferation
In the area of human cell research, exposure of a human hepatocyte cell line (HL-7702) to 50 μM PFOS identified 52 differentially expressed proteins, 27 of which were associated with cell proliferation, including hepatoma-derived growth factor (Hdgf) and the proliferation biomarkers nuclear protein Ki67(Ki67) and topoisomerase 2 alpha (Top2α). Low doses of PFOS (below 200 μM) enhanced the expression of Hdgf and Ki67 and Top2α [88]. Another study showed that PFOS could promote cell differentiation and cell proliferation by reducing positive targets such as cholesterol 7 alpha-hydroxylase (CYP7A1) in differentiation genes, and increasing negative targets such as Cyclin D1 (CCND1) in mitogenic genes through the study of hepatocyte nuclear factor 4-α (HNF4α) target gene expression [89].
In animal studies, PFOS exposure upregulated the expression of PCNA, c-Jun, c-MYC, and Cyclin D1 in rat Kupffer cells and co-cultured rat primary hepatocytes. The mechanism may be that PFOS induces Kupffer cell activation and leads to hepatocyte proliferation via the NF-κB/TNF-α/IL-6-dependent pathway [86].
4.5. Effect of PFOS on Liver Tumors
Cancer is the second leading cause of death worldwide, with primary liver cancer being the sixth most commonly diagnosed cancer and the third leading cause of cancer death worldwide in 2020 [90]. The liver is the primary target organ for PFOS exposure [91]. Epidemiological surveys reveal that PFOS is associated with the risk of developing cancers [92]. In a study on the relationship between PFAS concentrations in human serum and liver cancer from 2019 to 2021, the highest serum concentrations of PFOS were found in different PFAS with a 100% detection rate, and the concentration of PFOS in human serum was found to be significantly associated with the incidence of liver cancer and the levels of alpha fetoprotein (AFP), indicating that exposure to PFOS can increase the risk of developing liver cancer [93].
Animal studies display that PFOS exposure increases the risk of liver tumorigenesis [94]. A study on transgenic zebrafish showed that PFOS caused liver enlargement in model fish and increased the likelihood of hepatocellular carcinoma (HCC) in zebrafish [95]. The results also showed that PFOS led to reduced synthesis and accelerated degradation of the active form of vitamin D, osteotriol, resulting in a decrease in intracellular osteotriol content. In addition, the population study found that the level of vitamin D in human serum was negatively correlated with the concentration of PFOS [96].
4.6. Effect of PFOS on Hepatic Immune Function
PFOS could suppress the expression levels of almost all immune-related genes (such as interleukins and interleukin receptors, cellular chemokine family and NF-κB family, etc.), suggesting that these genes may be involved in the negative regulation of the body’s immune response following PFOS exposure, which results in a decrease in immunity [97]. Exposure of rodents to PFOS results in marked hepatomegaly, which is associated with significant alterations in liver histophysiology and immune status [98]. Moreover, a study has shown that PFOS exacerbates acute liver injury caused by concanavalin A (Con A), and the injury is associated with reduced levels of the liver pro-inflammatory cytokines tumor necrosis factor alpha (TNF-α) and interferon gamma (IFN-γ). In addition, exposure to PFOS can enhance hepatic DNA fragmentation, particularly after short-term exposure to low doses of PFOS, which suggests that exposure to PFOS may enhance the susceptibility of hepatic parenchymal cells to other injuries caused by activation of the hepatic immune system, thereby exacerbating liver injury during acute inflammation [99]. It was shown that PFOS at 1 μM significantly reduced the immune-related gene il1β in zebrafish liver and correspondingly reduced the protein level of IL-1β, with an increased binding potential to NF-κB [100]. In a study of striped bass, elevated PFOS concentrations were associated with increased lysozyme and AST activity, suggesting that PFOS exposure affects hepatic immune function [101]. In a study on male zebrafish, it was shown that the activities of immune-related enzymes such as acid phosphatase (ACP), alkaline phosphatase (AKP), and myeloperoxidase (MPO) were inhibited and the activity of lysozyme (LSZ) was increased after PFOS exposure. The mRNA levels of immune-related factors IL-1β, IL-6, IL-15, TNF-α, TGF-β, IRF-1, IRF-3, IRF-7, RAG-1, and RAG-2 were significantly increased in a concentration- and time-dependent manner with increasing PFOS exposure, suggesting that PFOS can interfere with normal immune function in zebrafish [102,103,104].
4.7. Effect of PFOS on Cholesterol and Bile Acid Metabolism
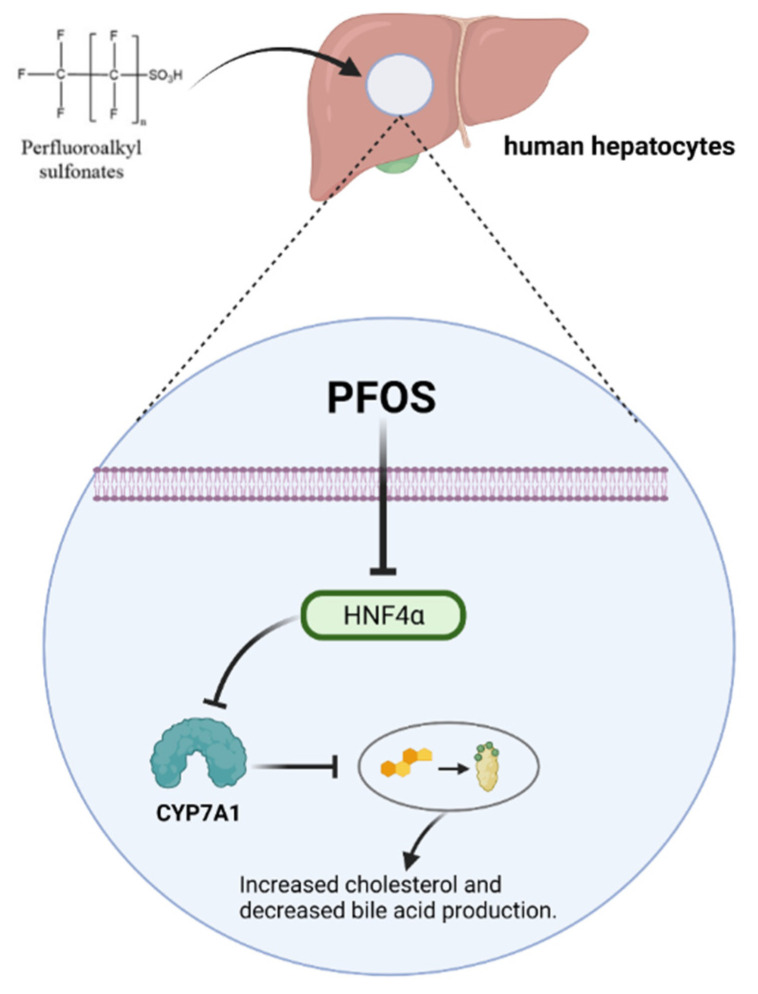
The European Food Safety Authority (EFSA) has identified exposure to PFOS as an important factor contributing to elevated total serum cholesterol levels in humans [27]. In the context of human research, epidemiological studies have also demonstrated that PFOS alters the transcript levels of genes associated with cholesterol mobilization [105]. PFOS has been shown to reduce serum cholesterol levels in rodents [106]. In a study based on hepatic HepaRG cells, it was found that the expression of numerous genes involved in the synthesis, metabolism, and transport of cholesterol and bile acids in cells was significantly affected by PFOS at concentrations above 10 µM, and there was a significant decrease in the synthesis of bile acids. In particular, PFOS leads to significant downregulation of the gene and protein levels of CYP7A1, the key enzyme that catalyzes the first and rate-limiting step in the synthesis of bile acids from cholesterol [107]. PFOS causes a decrease in HNF4α protein expression in human hepatocytes, a transcription factor that regulates CYP7A1, and a decrease in CYP7A1 leads to a decrease in bile acid production and an increase in cholesterol (Figure 2) [89,108].
Figure 2.
PFOS affects the metabolism of cholesterol and bile acid via CYP7A11.
In terms of animal research, another study in estrogen receptor β (ERβ) knockout mice exposed to PFOS revealed that PFOS significantly triggered hepatocyte edema and vacuolization, reduced bile acid and cholesterol levels in liver tissue, and affected the abundance and composition of the intestinal microbiota [60].
5. Signaling Pathways Associated with Hepatotoxic Damage Caused by PFOS
5.1. Role of Inflammation-Associated Signaling Pathways in PFOS-Induced Hepatotoxic Damage
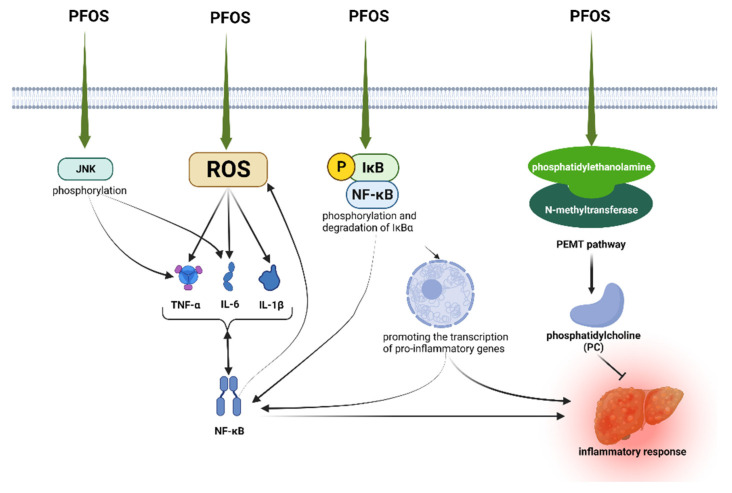
Using liver lipidomic analysis in mice, it was found that phosphatidylcholine (PC) synthesis via the phosphatidylethanolamine N-methyltransferase (PEMT) pathway may be a self-protective mechanism against PFOS-induced inflammation in animals [55]. PC has a variety of beneficial effects, including anti-inflammatory, antioxidant, and anti-fibrotic activities. Increased PC levels can be used to combat inflammation caused by PFOS. PC is upregulated in the PFOS-exposed state, and the upregulated PC may mainly originate from the PEMT pathway. A study showed that PC was increased in chicken embryos exposed to PFOS and was mainly derived from the PEMT synthesis pathway [109].
NF-κB is thought to be an important regulator of pro-inflammatory gene expression and can be activated by various inflammatory stimuli and environmental stressors, including IL-1β, and be transferred from the cytoplasm to the nucleus, thereby promoting the transcription of pro-inflammatory genes [110]. It has been shown that PFOS induces phosphorylation and degradation of IκBα, which will facilitate the translocate NF-κB from the cytoplasm to the nucleus and activate the NF-κB signaling pathway in C6 glioma cell lines. Thus, the NF-κB signaling pathway can be activated after PFOS exposure [104]. Another study found that PFOS exposure increased ROS levels; increased the mRNA expression of IL-1β, IL-6, and TNF-α; and enhanced NF-κB activity in the liver [102]. In addition, PFOS can increase both TNF-α and IL-6 expression by activating the NF-κB signaling pathway, thus affecting the regulation of the immune system [103]. PFOS induces IκB and JNK phosphorylation and activates NF-κB in the liver and induces TNF-α and IL-6 release by regulating JNK and NF-κB signaling pathways in Kupffer cells [86]. Moreover, significant changes in PFOS-induced NF-κB and IκBα protein expression were found to be associated with elevated TNF-α levels [111] (Figure 3).
Figure 3.
Summary diagram of inflammation-related pathways mediated by PFOS.
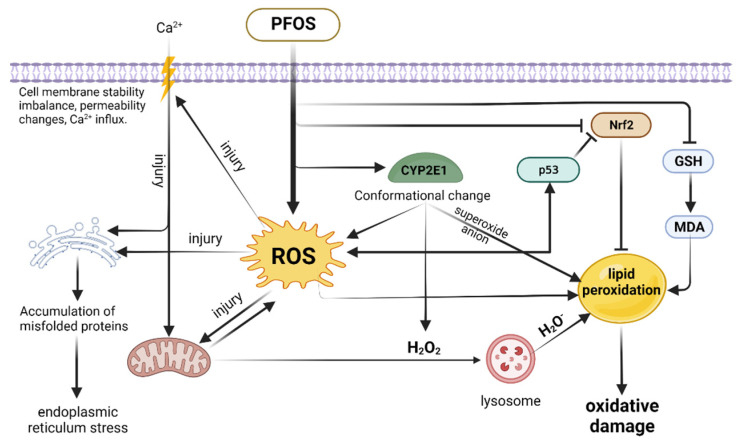
5.2. Role of Oxidative Stress-Related Signaling Pathways in PFOS-Induced Hepatotoxicity
The liver is particularly sensitive to ROS-induced oxidative stress [112]. PFOS exposure is able to increase ROS production in the liver and disrupt intracellular antioxidant defense systems [113]. ROS, an important pathogenic factor in the pathogenesis of many liver diseases, is usually a by-product of hepatocyte metabolism and detoxification. Continuous and excessive ROS production is highly toxic to cells and leads to oxidative damage to biomolecules in hepatocytes [112]. PFOS can directly damage hepatocyte mitochondria by disrupting the electron transport chain and releasing the toxic ROS. Then, hydrogen peroxide (H2O2), resulting from the damaged mitochondria and the conformational change in CYP2E1 caused by PFOS, diffuses into the lysosome and leads to the production of highly reactive hydroxyl radicals (H2O−) [114,115]. CYP2E1 produces superoxide anions during its catalytic cycle, and these ROS can subsequently destroy unsaturated fatty acids, leading to lipid peroxidation and the production of highly reactive aldehydes, such as malondialdehyde [116,117,118]. PFOS exposure promotes the accumulation of H2O2 and increased MDA content, leading to a decrease in SOD and GSH levels. Furthermore, PFOS can cause oxidative damage in the liver by inducing ROS formation and depletion of anti-oxidative defenses [119]. Excess ROS can attack the cell membrane of hepatocytes, leading to imbalance in cell membrane stability and altered permeability. The eventual disintegration will be triggered by lipid peroxidation caused by ROS [120]. ROS can cause an increase in Ca2+ entering the hepatocytes, which in turn leads to an increase in Ca2+ in the organelles, ultimately leading to organelle and overall cellular damage [121]. ROS-induced oxidative stress can induce the occurrence of mitochondrial permeability transition (MPT) in hepatocytes, which also leads to changes in mitochondrial membrane potential [122,123]. Moreover, mitochondrial ROS can escape from the MPT process, which in turn increases the intensity of oxidative stress [124]. In addition, the imbalance of Ca2+ homeostasis caused by ROS interferes with the function of the endoplasmic reticulum, leading to the accumulation of misfolded proteins and the enlargement of the endoplasmic reticulum lumen, and ultimately to endoplasmic reticulum stress [125,126]. Nuclear factor erythroid 2-related factor 2 (Nrf2) is a key transcriptional activator that provides essential protection against cellular oxidative damage by regulating the expression of antioxidant and detoxification enzyme genes, and is considered a key node in the prevention and treatment of liver disease [127]. PFOS can inhibit the activation and expression of target genes of Nrf2 [128]. PFOS can also inhibit Nrf2 expression in rat liver [111]. The tumor suppressor gene p53 is an important transcription factor that regulates the level of cellular ROS. High levels of ROS or prolonged external stimuli upregulate p53 and trigger a pro-oxidative response to further increase ROS expression [129]. Upregulated p53 expression decreases Nrf2 protein levels and subsequently inhibits Nrf2-dependent antioxidation and triggers p53-regulated apoptosis [130]. It was found that PFOS could inhibit the expression of Nrf2 through ROS-induced p53 dysregulation and thus enhance the level of oxidative stress in cells [119]. Exposure of hepatocytes to PFOS induces rapid depletion of glutathione (GSH), an important marker of cellular oxidative stress, and hepatotoxicity of PFOS can be inhibited by antioxidants and ROS scavengers [114] (Figure 4).
Figure 4.
Outline diagram of ROS-related pathways mediated by PFOS.
5.3. Role of PPAR-Related Signaling Pathway in Hepatotoxic Damage Caused by PFOS
Peroxisome proliferator-activated receptors (PPARs) have four main subtypes: PPARα, β, δ, and γ. PPARs are nuclear receptors involved in the regulation of genes related to energy homeostasis, lipid metabolism, and inflammation [131,132]. Studies have shown that PFOS can activate PPAR in the liver, thereby disrupting cholesterol homeostasis and fatty acid ω-oxidation [133]. PPARα-null mice treated with various PFAS exhibit steatosis characterized by the accumulation of lipids in hepatocytes, leading to liver disease [134]. A dose-dependent increase in PPARα-regulated gene expression upon PFOS exposure has been observed in rodents [135]. PFOS increased the expression of PPARα target genes Acox1 and CYP4A10 in mouse liver, thereby activating PPARα and causing pathological changes in the liver tissue [136]. Recently, in a study using a primary human hepatocyte spheroid model, PPARα activity was found to be increased by PFAS exposure in human liver spheroids, particularly by PFOS exposure [137]. Previous studies have shown that PFOS can differentially activate PPARα in mice and humans [138,139]. Prolonged activation of PPARα also increases signaling of hepatocyte proliferation and causes hepatocellular carcinoma in rodents, but PPARα-induced hepatocellular carcinoma appears to occur only in rodents, and there are species differences between rodents and humans in this aspect [140,141,142]. Currently, most researchers agree that liver cancer caused by PPARα does not seem to occur in human cells [143]. It is hypothesized that human PPARα may have lower sensitivity to PPARα agonists compared to rodent [136]. Therefore, more studies are needed to explore the relationship between PFOS, human liver, and PPARα in the future. A study of genes related to lipid metabolism in developing chicken embryos exposed to PFOS revealed that transcription of genes involved in fatty acid oxidation and PPAR-mediated were extensively suppressed, and the effect was more pronounced at lower doses of PFOS exposure [144].
5.4. Role of Autophagy-Related Signaling Pathways in PFOS-Induced Hepatotoxic Damage
Autophagy, as a self-regulated catabolic pathway, plays a key role in energy homeostasis and cytoplasmic quality control. For example, autophagy regulating hepatocyte function and autophagy dysregulation is associated with many liver diseases [145]. Previous studies have shown that PFOS can cause cells to undergo dysregulation of oxidative homeostatic change, leading to abnormal autophagy [146]. PFOS can induce abnormal expression of autophagic markers LC3-II and P62 and increase autophagic flux [147]. For the liver, PFOS induced LC3-II and LC3-II/I expression in L-02 cells in a concentration-dependent manner, stimulated autophagic flux, and decreased p62 expression [148]. It was also found that PFOS altered the post-translational modification of α-tubulin associated with autophagy in L-02 cells, but no changes in α-tubulin were found in the livers of PFOS-treated mice [149]. However, the mechanism is unclear and needs to be further explored. Another study showed that PFOS increased the number of autophagosomes in HepG2 cells and elevated LC3-II expression levels, induced lysosomal membrane permeabilization (LMP), and subsequently blocked autophagic flux, leading to excessive accumulation of autophagosomes and ultimately cellular damage [150]. These studies suggest that PFOS can trigger the disruption of mechanisms associated with autophagy in the liver, ultimately leading to liver damage.
5.5. Role of Apoptosis-Related Signaling Pathways in Hepatotoxic Damage Caused by PFOS
Apoptosis is a physiological form of programmed cell death that plays a critical role in embryogenesis, development, and normal tissue homeostasis [151]. PFOS has been reported to disrupt the homeostasis of the antioxidant system in hepatocellular carcinoma HepG2 cells; to promote the production of ROS, which in turn affects mitochondrial function; and to influence the gene expression of apoptosis regulators, leading to the initiation of the apoptotic program [152]. ROS are mainly derived from mitochondria in cells [153] in response to environmental stimuli. Excess ROS inhibit mitochondrial membrane potential (MMP) and trigger downstream apoptotic effects [154]. PFOS increases ROS levels in hepatocytes in a concentration-dependent manner, enhances Bax and cleaved-caspase-3 expression, inhibits MMP, and reduces Bcl-2 expression and the Bcl-2/Bax ratio to cause apoptosis [148].
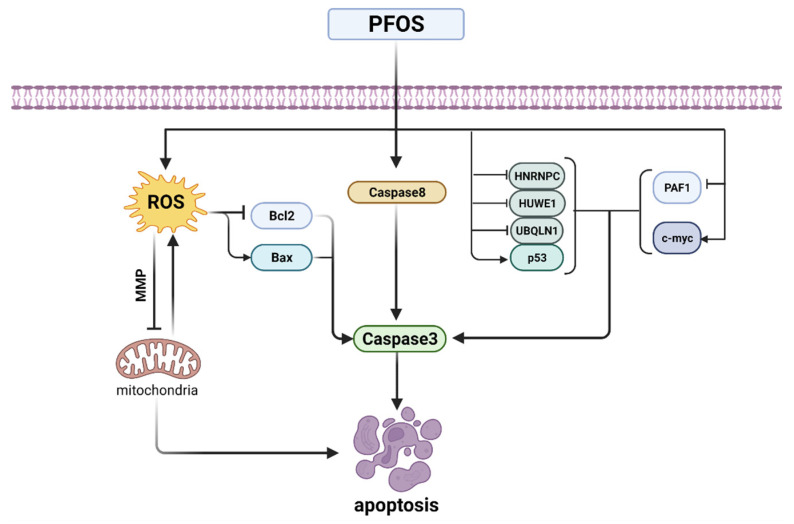
Transcriptional activation of the tumor suppressor gene p53 and the proto-oncogene c-myc have been well documented to be associated with the apoptotic process [155]. PFOS upregulates the gene expression levels of p53 and c-myc in L-02 cells. The suppression of p53-interacting proteins HNRNPC, HUWE1, and UBQLN1 and the overexpression of c-myc-interacting protein PAF1 may contribute to PFOS-induced apoptosis in L-02 cells [156]. The p53 protein plays a key role in cell cycle arrest and apoptosis [157]. PFOS significantly increases p53 mRNA levels and protein expression, which in turn initiates caspase3, the executioner in the caspase family of downstream apoptosis mechanisms, leading to apoptosis [158]. In addition, another study also confirmed that PFOS increased the expression of caspase3 and caspase8 in rat hepatocytes, leading to disrupted gene expression, oxidative damage, and apoptosis in hepatocytes [159] (Figure 5).
Figure 5.
Summary diagram of PFOS-induced apoptotic pathways.
6. Discussion
In recent years, more and more attention has been paid to the widespread presence of PFOS in the environment and its pollution of the environment, and the health risks posed by PFOS have also attracted increasing attention. As previously stated, increasing evidence suggests that the liver is the primary target organ for the toxic effects caused by PFOS [91]. In this paper, we summarized literature that explores the relationship between PFOS exposure and pathological changes and functional effects on the liver. Although we have described many possible mechanisms for the toxic effects of PFOS on liver tissues or cells, the mechanism of PFOS damage to the liver is not fully understood and needs to be further investigated.
PFOS can disrupt the balance of liver lipid metabolism, resulting in a series of morphological and functional pathological changes in the liver, such as liver enlargement and liver steatosis, and leading to liver diseases such as fatty liver and liver fibrosis, and in severe cases, even liver tumors [160]. In addition, PFOS can cross the placental barrier and have direct and indirect effects on the liver of both parents and offspring. The effects on liver function, hepatocyte proliferation, liver tumors, liver immunity, and cholesterol and bile acid metabolism cannot be ignored. There is substantial evidence that impaired structure and function of liver tissues or cells can affect the function of other tissues and organs; for example, emerging changes in renal function in patients with acute or chronic liver disease often lead to acute kidney injury [161] or chronic kidney diseases [162]. Severe abnormalities in liver function can even damage the nervous system and cause central nervous system dysfunction, leading to the development of hepatic encephalopathy [163]. Abnormal liver function can also affect cardiac function, and patients with cirrhosis can develop increased left ventricular weight and left eccentric hypertrophy, leading to the development of cirrhotic cardiomyopathy [164]. Liver damage can also affect the function of some other organs and tissues; therefore, the mechanism of PFOS damage to the liver is relatively complex, and there are limitations in the independent exploration of the mechanism of PFOS damage to the liver. It is also important to note that the mechanisms of cellular transformation and the extent of damage observed in humans and other animals, especially in rodents, are different due to species differences after PFOS exposure, and therefore, we must be careful when applying the results obtained from animal experiments to human studies, especially in terms of genotoxicity, bioaccumulation, and cytotoxicity [165].
The signaling pathways involved in the toxic damage of PFOS to liver are mainly the inflammation-related signaling pathway, oxidative stress signaling pathway, PPAR-related signaling pathway, autophagy-related pathway, and apoptosis-related signaling pathway, among which ROS homeostasis and NF-κB activation are the key nodes. Several signaling pathways play roles in liver function, but the exact mechanisms of toxicity underlying liver damage after PFOS exposure remain unclear. For example, the Wnt/β-catenin pathway regulates liver development, differentiation, and compartmentalization, and regulates basic liver physiological functions, but excessive activation of the Wnt/β-catenin pathway can lead to the development and progression of hepatocellular carcinoma (HCC) [166]. The PI3K/AKT pathway can lead to insulin resistance and abnormal hepatic gluconeogenesis in the liver [167]. These findings provide new directions for further research in the future. Different signaling pathways act individually or in association with other signaling pathways, forming a complex regulatory network of signaling pathways that regulate the expression of every function in our organisms. PFOS can disrupt the blood–testis barrier by downregulating connexins through the p38 MAPK/ATF2/MMP9 signaling pathway [168], and also mediates nitric oxide production in HAPI microglia via the ROS-mediated ERK/JNK MAPK signaling pathway [169]. These results suggest that PFOS does not affect a single signaling pathway and function in body tissues alone, and that these signaling pathways are not independent of each other, but are interconnected. Therefore, the effects of PFOS on the liver through various signaling pathways are complex.
Due to the stable nature of PFOS and the fact that they are not easily decomposed, they are widely present in environmental media and pose a great threat to the life and health of living organisms. Moreover, PFOS may interact with other environmental pollutants and synergistically cause damage to organisms. Differences in species, age, exposure time, and exposure dose pose many difficulties in studies of PFOS toxicity to the liver. Therefore, focusing on the effects of PFOS on the liver function of the organism in different species and at different time points, and the interactions among toxicants, contribute to future exploration of the mechanisms of PFOS toxicity and provide a theoretical reference for related studies on PFOS-induced hepatotoxicity.
Acknowledgments
We would like to thank the Department of Science and Technology of Jilin Province for the financial support (grant no. 20210204024YY).
Author Contributions
Conceptualization, P.W. and S.R.; Funding acquisition, S.R.; Project administration, P.W. and S.R.; Supervision, S.R.; Visualization, P.W. and D.L.; Writing—original draft, P.W. and D.L.; Writing—review and editing, P.W., S.Y., J.C., Y.L. and S.R. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Department of Science and Technology of Jilin Province, grant number 20210204024YY. The APC was funded by the Department of Science and Technology of Jilin Province.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhang Z., Wang F., Zhang Y., Yao J., Bi J., He J., Zhang S., Wei Y., Guo H., Zhang X., et al. Associations of serum PFOA and PFOS levels with incident hypertension risk and change of blood pressure levels. Environ. Res. 2022;212 Pt B:113293. doi: 10.1016/j.envres.2022.113293. [DOI] [PubMed] [Google Scholar]
- 2.Lau C., Anitole K., Hodes C., Lai D., Pfahles-Hutchens A., Seed J. Perfluoroalkyl acids: A review of monitoring and toxicological findings. Toxicol. Sci. 2007;99:366–394. doi: 10.1093/toxsci/kfm128. [DOI] [PubMed] [Google Scholar]
- 3.Pérez F., Nadal M., Navarro-Ortega A., Fàbrega F., Domingo J.L., Barceló D., Farré M. Accumulation of perfluoroalkyl substances in human tissues. Environ. Int. 2013;59:354–362. doi: 10.1016/j.envint.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Lindstrom A.B., Strynar M.J., Libelo E.L. Polyfluorinated compounds: Past, present, and future. Environ. Sci. Technol. 2011;45:7954–7961. doi: 10.1021/es2011622. [DOI] [PubMed] [Google Scholar]
- 5.Leung S.C.E., Shukla P., Chen D., Eftekhari E., An H., Zare F., Ghasemi N., Zhang D., Nguyen N.T., Li Q. Emerging technologies for PFOS/PFOA degradation and removal: A review. Sci. Total Environ. 2022;827:153669. doi: 10.1016/j.scitotenv.2022.153669. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y., Fu J., Ye T., Li X., Gao K., Xue Q., Lv J., Zhang A., Fu J. Occurrence, profiles, and ecotoxicity of poly- and perfluoroalkyl substances and their alternatives in global apex predators: A critical review. J. Environ. Sci. 2021;109:219–236. doi: 10.1016/j.jes.2021.03.036. [DOI] [PubMed] [Google Scholar]
- 7.Paul A.G., Jones K.C., Sweetman A.J. A first global production, emission, and environmental inventory for perfluorooctane sulfonate. Environ. Sci. Technol. 2009;43:386–392. doi: 10.1021/es802216n. [DOI] [PubMed] [Google Scholar]
- 8.Zhang B., He Y., Yang G., Chen B., Yao Y., Sun H., Kannan K., Zhang T. Legacy and Emerging Poly- and Perfluoroalkyl Substances in Finless Porpoises from East China Sea: Temporal Trends and Tissue-Specific Accumulation. Environ. Sci. Technol. 2021 doi: 10.1021/acs.est.1c00062. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X., Lohmann R., Dassuncao C., Hu X.C., Weber A.K., Vecitis C.D., Sunderland E.M. Source attribution of poly- and perfluoroalkyl substances (PFASs) in surface waters from Rhode Island and the New York Metropolitan Area. Environ. Sci. Technol. Lett. 2016;3:316–321. doi: 10.1021/acs.estlett.6b00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jarvis A.L., Justice J.R., Elias M.C., Schnitker B., Gallagher K. Perfluorooctane Sulfonate in US Ambient Surface Waters: A Review of Occurrence in Aquatic Environments and Comparison to Global Concentrations. Environ. Toxicol. Chem. 2021;40:2425–2442. doi: 10.1002/etc.5147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y., Wang Y., Li J., Zhao Y., Guo F., Liu J., Cai Z. Perfluorinated compounds in seafood from coastal areas in China. Environ. Int. 2012;42:67–71. doi: 10.1016/j.envint.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Liu J.J., Cui X.X., Tan Y.W., Dong P.X., Ou Y.Q., Li Q.Q., Chu C., Wu L.Y., Liang L.X., Qin S.J., et al. Per- and perfluoroalkyl substances alternatives, mixtures and liver function in adults: A community-based population study in China. Environ. Int. 2022;163:107179. doi: 10.1016/j.envint.2022.107179. [DOI] [PubMed] [Google Scholar]
- 13.Gleason J.A., Post G.B., Fagliano J.A. Associations of perfluorinated chemical serum concentrations and biomarkers of liver function and uric acid in the US population (NHANES), 2007–2010. Environ. Res. 2015;136:8–14. doi: 10.1016/j.envres.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Steenland K., Tinker S., Frisbee S., Ducatman A., Vaccarino V. Association of perfluorooctanoic acid and perfluorooctane sulfonate with serum lipids among adults living near a chemical plant. Am. J. Epidemiol. 2009;170:1268–1278. doi: 10.1093/aje/kwp279. [DOI] [PubMed] [Google Scholar]
- 15.Mora A.M., Fleisch A.F., Rifas-Shiman S.L., Woo Baidal J.A., Pardo L., Webster T.F., Calafat A.M., Ye X., Oken E., Sagiv S.K. Early life exposure to per- and polyfluoroalkyl substances and mid-childhood lipid and alanine aminotransferase levels. Environ. Int. 2018;111:1–13. doi: 10.1016/j.envint.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torres L., Redko A., Limper C., Imbiakha B., Chang S., August A. Effect of Perfluorooctanesulfonic acid (PFOS) on immune cell development and function in mice. Immunol. Lett. 2021;233:31–41. doi: 10.1016/j.imlet.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Umweltbundesamt Ableitung von HBM-I-Werten für Perfluoroktansäure (PFOA) und Perfluoroktansulfonsäure (PFOS)—Stellungnahme der Kommission “Humanbiomonitoring” des Umweltbundesamts [HBM-I values for Perfluorooctanoic acid (PFOA) and Perfluorooctanesulfonic acid (PFOS) in blood plasma—Statement of the German Human Biomonitoring Commission (HBM Commission)] Bundesgesundheitsblatt Gesundh. Gesundh. 2018;61:474–487. doi: 10.1007/s00103-018-2709-z. [DOI] [PubMed] [Google Scholar]
- 18.Bach C.C., Liew Z., Bech B.H., Nohr E.A., Fei C., Bonefeld-Jorgensen E.C., Henriksen T.B., Olsen J. Perfluoroalkyl acids and time to pregnancy revisited: An update from the Danish National Birth Cohort. Environ. Health. 2015;14:59. doi: 10.1186/s12940-015-0040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ballesteros V., Costa O., Iñiguez C., Fletcher T., Ballester F., Lopez-Espinosa M.J. Exposure to perfluoroalkyl substances and thyroid function in pregnant women and children: A systematic review of epidemiologic studies. Environ. Int. 2017;99:15–28. doi: 10.1016/j.envint.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Salter D.M., Wei W., Nahar P.P., Marques E., Slitt A.L. Perfluorooctanesulfonic Acid (PFOS) Thwarts the Beneficial Effects of Calorie Restriction and Metformin. Toxicol. Sci. 2021;182:82–95. doi: 10.1093/toxsci/kfab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsuda S. Differential toxicity between perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) J. Toxicol. Sci. 2016;41:SP27–SP36. doi: 10.2131/jts.41.SP27. [DOI] [PubMed] [Google Scholar]
- 22.Saikat S., Kreis I., Davies B., Bridgman S., Kamanyire R. The impact of PFOS on health in the general population: A review. Environ. Sci. Process. Impacts. 2013;15:329–335. doi: 10.1039/C2EM30698K. [DOI] [PubMed] [Google Scholar]
- 23.Kim J.H., Barbagallo B., Annunziato K., Farias-Pereira R., Doherty J.J., Lee J., Zina J., Tindal C., McVey C., Aresco R., et al. Maternal preconception PFOS exposure of Drosophila melanogaster alters reproductive capacity, development, morphology and nutrient regulation. Food Chem. Toxicol. 2021;151:112153. doi: 10.1016/j.fct.2021.112153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Z., Zhang Y., Wang F., Wang R., Zhang S., Zhang Z., Li P., Yao J., Bi J., He J., et al. Associations between serum PFOA and PFOS levels and incident chronic kidney disease risk in patients with type 2 diabetes. Ecotoxicol. Environ. Saf. 2022;229:113060. doi: 10.1016/j.ecoenv.2021.113060. [DOI] [PubMed] [Google Scholar]
- 25.Zhou R., Cheng W., Feng Y., Wang W., Liang F., Luo F., Yang S., Wang Y. Combined effects of BPA and PFOS on fetal cardiac development: In vitro and in vivo experiments. Environ. Toxicol. Pharmacol. 2020;80:103434. doi: 10.1016/j.etap.2020.103434. [DOI] [PubMed] [Google Scholar]
- 26.Hölzer J., Lilienthal H., Schümann M. Human Biomonitoring (HBM)-I values for perfluorooctanoic acid (PFOA) and perfluorooctane sulfonic acid (PFOS)—Description, derivation and discussion. Regul. Toxicol. Pharmacol. 2021;121:104862. doi: 10.1016/j.yrtph.2021.104862. [DOI] [PubMed] [Google Scholar]
- 27.EFSA Panel on Contaminants in the Food Chain (CONTAM) Knutsen H.K., Alexander J., Barregård L., Bignami M., Brüschweiler B., Ceccatelli S., Cottrill B., Dinovi M., Edler L., et al. Risk to human health related to the presence of perfluorooctane sulfonic acid and perfluorooctanoic acid in food. EFSA J. 2018;16:e05194. doi: 10.2903/j.efsa.2018.5194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindim C., van Gils J., Cousins I.T. Europe-wide estuarine export and surface water concentrations of PFOS and PFOA. Water Res. 2016;103:124–132. doi: 10.1016/j.watres.2016.07.024. [DOI] [PubMed] [Google Scholar]
- 29.Wang Q., Ruan Y., Jin L., Zhang X., Li J., He Y., Wei S., Lam J., Lam P. Target, Nontarget, and Suspect Screening and Temporal Trends of Per- and Polyfluoroalkyl Substances in Marine Mammals from the South China Sea. Environ. Sci. Technol. 2021;55:1045–1056. doi: 10.1021/acs.est.0c06685. [DOI] [PubMed] [Google Scholar]
- 30.Oliaei F., Kriens D., Weber R., Watson A. PFOS and PFC releases and associated pollution from a PFC production plant in Minnesota (USA) Environ. Sci. Pollut. Res. Int. 2013;20:1977–1992. doi: 10.1007/s11356-012-1275-4. [DOI] [PubMed] [Google Scholar]
- 31.Brambilla G., D’Hollander W., Oliaei F., Stahl T., Weber R. Pathways and factors for food safety and food security at PFOS contaminated sites within a problem based learning approach. Chemosphere. 2015;129:192–202. doi: 10.1016/j.chemosphere.2014.09.050. [DOI] [PubMed] [Google Scholar]
- 32.Kleywegt S., Raby M., McGill S., Helm P. The impact of risk management measures on the concentrations of per- and polyfluoroalkyl substances in source and treated drinking waters in Ontario, Canada. Sci. Total Environ. 2020;748:141195. doi: 10.1016/j.scitotenv.2020.141195. [DOI] [PubMed] [Google Scholar]
- 33.Ochoa-Herrera V., Field J.A., Luna-Velasco A., Sierra-Alvarez R. Microbial toxicity and biodegradability of perfluorooctane sulfonate (PFOS) and shorter chain perfluoroalkyl and polyfluoroalkyl substances (PFASs) Environ. Sci. Process Impacts. 2016;18:1236–1246. doi: 10.1039/C6EM00366D. [DOI] [PubMed] [Google Scholar]
- 34.Liu J., Mejia Avendaño S. Microbial degradation of polyfluoroalkyl chemicals in the environment: A review. Environ. Int. 2013;61:98–114. doi: 10.1016/j.envint.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 35.Zhang L., Liu J., Hu J., Liu C., Guo W., Wang Q., Wang H. The inventory of sources, environmental releases and risk assessment for perfluorooctane sulfonate in China. Environ. Pollut. 2012;165:193–198. doi: 10.1016/j.envpol.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 36.Yue Y., Li S., Qian Z., Pereira R.F., Lee J., Doherty J.J., Zhang Z., Peng Y., Clark J.M., Timme-Laragy A.R., et al. Perfluorooctanesulfonic acid (PFOS) and perfluorobutanesulfonic acid (PFBS) impaired reproduction and altered offspring physiological functions in Caenorhabditis elegans. Food Chem. Toxicol. 2020;145:111695. doi: 10.1016/j.fct.2020.111695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Olsen G.W., Burris J.M., Ehresman D.J., Froehlich J.W., Seacat A.M., Butenhoff J.L., Zobel L.R. Half-life of serum elimination of perfluorooctanesulfonate, perfluorohexanesulfonate, and perfluorooctanoate in retired fluorochemical production workers. Environ. Health Perspect. 2007;115:1298–1305. doi: 10.1289/ehp.10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Y., Beesoon S., Zhu L., Martin J.W. Biomonitoring of perfluoroalkyl acids in human urine and estimates of biological half-life. Environ. Sci. Technol. 2013;47:10619–10627. doi: 10.1021/es401905e. [DOI] [PubMed] [Google Scholar]
- 39.Ahrens L., Bundschuh M. Fate and effects of poly- and perfluoroalkyl substances in the aquatic environment: A review. Environ. Toxicol. Chem. 2014;33:1921–1929. doi: 10.1002/etc.2663. [DOI] [PubMed] [Google Scholar]
- 40.Pachkowski B., Post G.B., Stern A.H. The derivation of a Reference Dose (RfD) for perfluorooctane sulfonate (PFOS) based on immune suppression. Environ. Res. 2019;171:452–469. doi: 10.1016/j.envres.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 41.National Toxicology Program Toxicity studies of perfluoroalkyl carboxylates administered by gavage to Sprague Dawley (Hsd:Sprague Dawley SD) Rats. Toxic Rep. Ser. 2019;97:NTP-TOX-97. doi: 10.22427/NTP-TOX-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gu X., Manautou J.E. Molecular mechanisms underlying chemical liver injury. Expert Rev. Mol. Med. 2012;14:e4. doi: 10.1017/S1462399411002110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang T., Zhang Y., Zhang W., Lin T., Chen L., Yang B., Wu L., Yang J., Zhang D. Attenuation of Perfluorooctane Sulfonate-Induced Steatohepatitis by Grape Seed Proanthocyanidin Extract in Mice. Biomed. Res. Int. 2020;2020:8818160. doi: 10.1155/2020/8818160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fang C., Huang Q., Ye T., Chen Y., Liu L., Kang M., Lin Y., Shen H., Dong S. Embryonic exposure to PFOS induces immunosuppression in the fish larvae of marine medaka. Ecotoxicol. Environ. Saf. 2013;92:104–111. doi: 10.1016/j.ecoenv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Jian J.M., Chen D., Han F.J., Guo Y., Zeng L., Lu X., Wang F. A short review on human exposure to and tissue distribution of per- and polyfluoroalkyl substances (PFASs) Sci. Total Environ. 2018;636:1058–1069. doi: 10.1016/j.scitotenv.2018.04.380. [DOI] [PubMed] [Google Scholar]
- 46.Chang S.C., Noker P.E., Gorman G.S., Gibson S.J., Hart J.A., Ehresman D.J., Butenhoff J.L. Comparative pharmacokinetics of perfluorooctanesulfonate (PFOS) in rats, mice, and monkeys. Reprod. Toxicol. 2012;33:428–440. doi: 10.1016/j.reprotox.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 47.Ehresman D.J., Froehlich J.W., Olsen G.W., Chang S.C., Butenhoff J.L. Comparison of human whole blood, plasma, and serum matrices for the determination of perfluorooctanesulfonate (PFOS), perfluorooctanoate (PFOA), and other fluorochemicals. Environ. Res. 2007;103:176–184. doi: 10.1016/j.envres.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 48.Pizzurro D.M., Seeley M., Kerper L.E., Beck B.D. Interspecies differences in perfluoroalkyl substances (PFAS) toxicokinetics and application to health-based criteria. Regul. Toxicol. Pharmacol. 2019;106:239–250. doi: 10.1016/j.yrtph.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 49.Agency for Toxic Substances Disease Registry (ATSDR) Toxicological profile for Perfluoroalkyls Atlanta GA, U.S. Department of Health and Human Services. Public Health Serv. 2021 doi: 10.15620/cdc:59198. [DOI] [Google Scholar]
- 50.Harada K.H., Hashida S., Kaneko T., Takenaka K., Minata M., Inoue K., Saito N., Koizumi A. Biliary excretion and cerebrospinal fluid partition of perfluorooctanoate and perfluorooctane sulfonate in humans. Environ. Toxicol. Pharmacol. 2007;24:134–139. doi: 10.1016/j.etap.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 51.Ducatman A., Luster M., Fletcher T. Perfluoroalkyl substance excretion: Effects of organic anion-inhibiting and resin-binding drugs in a community setting. Environ. Toxicol. Pharmacol. 2021;85:103650. doi: 10.1016/j.etap.2021.103650. [DOI] [PubMed] [Google Scholar]
- 52.Wang L., Wang Y., Liang Y., Li J., Liu Y., Zhang J., Zhang A., Fu J., Jiang G. PFOS induced lipid metabolism disturbances in BALB/c mice through inhibition of low density lipoproteins excretion. Sci. Rep. 2014;4:4582. doi: 10.1038/srep04582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zeng Z., Song B., Xiao R., Zeng G., Gong J., Chen M., Xu P., Zhang P., Shen M., Yi H. Assessing the human health risks of perfluorooctane sulfonate by in vivo and in vitro studies. Environ. Int. 2019;126:598–610. doi: 10.1016/j.envint.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 54.Marques E.S., Agudelo J., Kaye E.M., Modaresi S., Pfohl M., Bečanová J., Wei W., Polunas M., Goedken M., Slitt A.L. The role of maternal high fat diet on mouse pup metabolic endpoints following perinatal PFAS and PFAS mixture exposure. Toxicology. 2021;462:152921. doi: 10.1016/j.tox.2021.152921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li X., Li T., Wang Z., Wei J., Liu J., Zhang Y., Zhao Z. Distribution of perfluorooctane sulfonate in mice and its effect on liver lipidomic. Talanta. 2021;226:122150. doi: 10.1016/j.talanta.2021.122150. [DOI] [PubMed] [Google Scholar]
- 56.Pan C.G., Zhao J.L., Liu Y.S., Zhang Q.Q., Chen Z.F., Lai H.J., Peng F.J., Liu S.S., Ying G.G. Bioaccumulation and risk assessment of per- and polyfluoroalkyl substances in wild freshwater fish from rivers in the Pearl River Delta region, South China. Ecotoxicol. Environ. Saf. 2014;107:192–199. doi: 10.1016/j.ecoenv.2014.05.031. [DOI] [PubMed] [Google Scholar]
- 57.Wang S., Kaufman R.J. How does protein misfolding in the endoplasmic reticulum affect lipid metabolism in the liver? Curr. Opin. Lipidol. 2014;25:125–132. doi: 10.1097/MOL.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 58.Lee S.H., Tseng W.C., Du Z.Y., Lin W.Y., Chen M.H., Lin C.C., Lien G.W., Liang H.J., Wen H.J., Guo Y.L., et al. Lipid responses to environmental perfluoroalkyl substance exposure in a Taiwanese Child cohort. Environ. Pollut. 2021;283:117007. doi: 10.1016/j.envpol.2021.117007. [DOI] [PubMed] [Google Scholar]
- 59.Marques E., Pfohl M., Wei W., Tarantola G., Ford L., Amaeze O., Alesio J., Ryu S., Jia X., Zhu H., et al. Replacement per- and polyfluoroalkyl substances (PFAS) are potent modulators of lipogenic and drug metabolizing gene expression signatures in primary human hepatocytes. Toxicol. Appl. Pharmacol. 2022;442:115991. doi: 10.1016/j.taap.2022.115991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu C., Jiang Z.Y., Liu Q., Liu H., Gu A. Estrogen receptor beta mediates hepatotoxicity induced by perfluorooctane sulfonate in mouse. Environ. Sci. Pollut. Res. Int. 2017;24:13414–13423. doi: 10.1007/s11356-017-8943-3. [DOI] [PubMed] [Google Scholar]
- 61.Su M., Liang X., Xu X., Wu X., Yang B. Hepatoprotective benefits of vitamin C against perfluorooctane sulfonate-induced liver damage in mice through suppressing inflammatory reaction and ER stress. Environ. Toxicol. Pharmacol. 2019;65:60–65. doi: 10.1016/j.etap.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 62.Fai Tse W.K., Li J.W., Kwan Tse A.C., Chan T.F., Hin Ho J.C., Sun Wu R.S., Chu Wong C.K., Lai K.P. Fatty liver disease induced by perfluorooctane sulfonate: Novel insight from transcriptome analysis. Chemosphere. 2016;159:166–177. doi: 10.1016/j.chemosphere.2016.05.060. [DOI] [PubMed] [Google Scholar]
- 63.Wan H.T., Zhao Y.G., Wei X., Hui K.Y., Giesy J.P., Wong C.K. PFOS-induced hepatic steatosis, the mechanistic actions on β-oxidation and lipid transport. Biochim. Biophys. Acta. 2012;1820:1092–1101. doi: 10.1016/j.bbagen.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 64.Huck I., Beggs K., Apte U. Paradoxical Protective Effect of Perfluorooctanesulfonic Acid Against High-Fat Diet-Induced Hepatic Steatosis in Mice. Int. J. Toxicol. 2018;37:383–392. doi: 10.1177/1091581818790934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li D., Jiang L., Hong Y., Cai Z. Multilayered glycoproteomic analysis reveals the hepatotoxic mechanism in perfluorooctane sulfonate (PFOS) exposure mice. Environ. Pollut. 2021;268 Pt A:115774. doi: 10.1016/j.envpol.2020.115774. [DOI] [PubMed] [Google Scholar]
- 66.Zhao W., Zitzow J.D., Weaver Y., Ehresman D.J., Chang S.C., Butenhoff J.L., Hagenbuch B. Organic Anion Transporting Polypeptides Contribute to the Disposition of Perfluoroalkyl Acids in Humans and Rats. Toxicol. Sci. 2017;156:84–95. doi: 10.1093/toxsci/kfw236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Marques E., Pfohl M., Auclair A., Jamwal R., Barlock B.J., Sammoura F.M., Goedken M., Akhlaghi F., Slitt A.L. Perfluorooctanesulfonic acid (PFOS) administration shifts the hepatic proteome and augments dietary outcomes related to hepatic steatosis in mice. Toxicol. Appl. Pharmacol. 2020;408:115250. doi: 10.1016/j.taap.2020.115250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pfohl M., Ingram L., Marques E., Auclair A., Barlock B., Jamwal R., Anderson D., Cummings B.S., Slitt A.L. Perfluorooctanesulfonic Acid and Perfluorohexanesulfonic Acid Alter the Blood Lipidome and the Hepatic Proteome in a Murine Model of Diet-Induced Obesity. Toxicol. Sci. 2020;178:311–324. doi: 10.1093/toxsci/kfaa148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dale K., Yadetie F., Horvli T., Zhang X., Frøysa H.G., Karlsen O.A., Goksøyr A. Single PFAS and PFAS mixtures affect nuclear receptor- and oxidative stress-related pathways in precision-cut liver slices of Atlantic cod (Gadus morhua) Sci. Total Environ. 2022;814:152732. doi: 10.1016/j.scitotenv.2021.152732. [DOI] [PubMed] [Google Scholar]
- 70.Cheng J., Lv S., Nie S., Liu J., Tong S., Kang N., Xiao Y., Dong Q., Huang C., Yang D. Chronic perfluorooctane sulfonate (PFOS) exposure induces hepatic steatosis in zebrafish. Aquat. Toxicol. 2016;176:45–52. doi: 10.1016/j.aquatox.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 71.Wielsøe M., Long M., Ghisari M., Bonefeld-Jørgensen E.C. Perfluoroalkylated substances (PFAS) affect oxidative stress biomarkers in vitro. Chemosphere. 2015;129:239–245. doi: 10.1016/j.chemosphere.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 72.Stratakis N., Conti D.V., Jin R., Margetaki K., Valvi D., Siskos A.P., Maitre L., Garcia E., Varo N., Zhao Y., et al. Prenatal Exposure to Perfluoroalkyl Substances Associated with Increased Susceptibility to Liver Injury in Children. Hepatology. 2020;72:1758–1770. doi: 10.1002/hep.31483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mamsen L.S., Björvang R.D., Mucs D., Vinnars M.T., Papadogiannakis N., Lindh C.H., Andersen C.Y., Damdimopoulou P. Concentrations of perfluoroalkyl substances (PFASs) in human embryonic and fetal organs from first, second, and third trimester pregnancies. Environ. Int. 2019;124:482–492. doi: 10.1016/j.envint.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 74.Lai K.P., Li J.W., Cheung A., Li R., Billah M.B., Chan T.F., Wong C. Transcriptome sequencing reveals prenatal PFOS exposure on liver disorders. Environ. Pollut. 2017;223:416–425. doi: 10.1016/j.envpol.2017.01.041. [DOI] [PubMed] [Google Scholar]
- 75.Zheng P., Liu Y., An Q., Yang X., Yin S., Ma L.Q., Liu W. Prenatal and postnatal exposure to emerging and legacy per-/polyfluoroalkyl substances: Levels and transfer in maternal serum, cord serum, and breast milk. Sci. Total Environ. 2022;812:152446. doi: 10.1016/j.scitotenv.2021.152446. [DOI] [PubMed] [Google Scholar]
- 76.Liang X., Xie G., Wu X., Su M., Yang B. Effect of prenatal PFOS exposure on liver cell function in neonatal mice. Environ. Sci. Pollut. Res. Int. 2019;26:18240–18246. doi: 10.1007/s11356-019-05245-4. [DOI] [PubMed] [Google Scholar]
- 77.Cui Y., Lv S., Liu J., Nie S., Chen J., Dong Q., Huang C., Yang D. Chronic perfluorooctanesulfonic acid exposure disrupts lipid metabolism in zebrafish. Hum. Exp. Toxicol. 2017;36:207–217. doi: 10.1177/0960327116646615. [DOI] [PubMed] [Google Scholar]
- 78.Taylor S., Terkildsen M., Stevenson G., de Araujo J., Yu C., Yates A., McIntosh R.R., Gray R. Per and polyfluoroalkyl substances (PFAS) at high concentrations in neonatal Australian pinnipeds. Sci. Total Environ. 2021;786:147446. doi: 10.1016/j.scitotenv.2021.147446. [DOI] [PubMed] [Google Scholar]
- 79.Grønnestad R., Villanger G.D., Polder A., Kovacs K.M., Lydersen C., Jenssen B.M., Borgå K. Maternal transfer of perfluoroalkyl substances in hooded seals. Environ. Toxicol. Chem. 2017;36:763–770. doi: 10.1002/etc.3623. [DOI] [PubMed] [Google Scholar]
- 80.Attanasio R. Association between perfluoroalkyl acids and liver function: Data on sex differences in adolescents. Data Brief. 2019;27:104618. doi: 10.1016/j.dib.2019.104618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Salihovic S., Stubleski J., Kärrman A., Larsson A., Fall T., Lind L., Lind P.M. Changes in markers of liver function in relation to changes in perfluoroalkyl substances—A longitudinal study. Environ. Int. 2018;117:196–203. doi: 10.1016/j.envint.2018.04.052. [DOI] [PubMed] [Google Scholar]
- 82.Wang Y., Yao J., Dai J., Ma L., Liu D., Xu H., Cui Q., Ma J., Zhang H. Per- and polyfluoroalkyl substances (PFASs) in blood of captive Siberian tigers in China: Occurrence and associations with biochemical parameters. Environ. Pollut. 2020;265 Pt B:114805. doi: 10.1016/j.envpol.2020.114805. [DOI] [PubMed] [Google Scholar]
- 83.Nian M., Li Q.Q., Bloom M., Qian Z.M., Syberg K.M., Vaughn M.G., Wang S.Q., Wei Q., Zeeshan M., Gurram N., et al. Liver function biomarkers disorder is associated with exposure to perfluoroalkyl acids in adults: Isomers of C8 Health Project in China. Environ. Res. 2019;172:81–88. doi: 10.1016/j.envres.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 84.Gallo V., Leonardi G., Genser B., Lopez-Espinosa M.J., Frisbee S.J., Karlsson L., Ducatman A.M., Fletcher T. Serum perfluorooctanoate (PFOA) and perfluorooctane sulfonate (PFOS) concentrations and liver function biomarkers in a population with elevated PFOA exposure. Environ. Health Perspect. 2012;120:655–660. doi: 10.1289/ehp.1104436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cakmak S., Lukina A., Karthikeyan S., Atlas E., Dales R. The association between blood PFAS concentrations and clinical biochemical measures of organ function and metabolism in participants of the Canadian Health Measures Survey (CHMS) Sci. Total Environ. 2022;827:153900. doi: 10.1016/j.scitotenv.2022.153900. [DOI] [PubMed] [Google Scholar]
- 86.Han R., Zhang F., Wan C., Liu L., Zhong Q., Ding W. Effect of perfluorooctane sulphonate-induced Kupffer cell activation on hepatocyte proliferation through the NF-κB/TNF-α/IL-6-dependent pathway. Chemosphere. 2018;200:283–294. doi: 10.1016/j.chemosphere.2018.02.137. [DOI] [PubMed] [Google Scholar]
- 87.Bassler J., Ducatman A., Elliott M., Wen S., Wahlang B., Barnett J., Cave M.C. Environmental perfluoroalkyl acid exposures are associated with liver disease characterized by apoptosis and altered serum adipocytokines. Environ. Pollut. 2019;247:1055–1063. doi: 10.1016/j.envpol.2019.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cui R., Zhang H., Guo X., Cui Q., Wang J., Dai J. Proteomic analysis of cell proliferation in a human hepatic cell line (HL-7702) induced by perfluorooctane sulfonate using iTRAQ. J. Hazard. Mater. 2015;299:361–370. doi: 10.1016/j.jhazmat.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 89.Beggs K.M., McGreal S.R., McCarthy A., Gunewardena S., Lampe J.N., Lau C., Apte U. The role of hepatocyte nuclear factor 4-alpha in perfluorooctanoic acid- and perfluorooctanesulfonic acid-induced hepatocellular dysfunction. Toxicol. Appl. Pharmacol. 2016;304:18–29. doi: 10.1016/j.taap.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 91.Chang S.C., Ehresman D.J., Bjork J.A., Wallace K.B., Parker G.A., Stump D.G., Butenhoff J.L. Gestational and lactational exposure to potassium perfluorooctanesulfonate (K+PFOS) in rats: Toxicokinetics, thyroid hormone status, and related gene expression. Reprod. Toxicol. 2009;27:387–399. doi: 10.1016/j.reprotox.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 92.Steenland K., Winquist A. PFAS and cancer, a scoping review of the epidemiologic evidence. Environ. Res. 2021;194:110690. doi: 10.1016/j.envres.2020.110690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cao L., Guo Y., Chen Y., Hong J., Wu J., Hangbiao J. Per-/polyfluoroalkyl substance concentrations in human serum and their associations with liver cancer. Chemosphere. 2022;296:134083. doi: 10.1016/j.chemosphere.2022.134083. [DOI] [PubMed] [Google Scholar]
- 94.Butenhoff J.L., Chang S.C., Olsen G.W., Thomford P.J. Chronic dietary toxicity and carcinogenicity study with potassium perfluorooctanesulfonate in Sprague Dawley rats. Toxicology. 2012;293:1–15. doi: 10.1016/j.tox.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 95.Zhu Y., Yang D., Duan X., Zhang Y., Chen D., Gong Z., Liu C. Perfluorooctane sulfonate promotes doxycycline-induced liver tumor progression in male Krasv12 transgenic zebrafish. Environ. Res. 2021;196:110962. doi: 10.1016/j.envres.2021.110962. [DOI] [PubMed] [Google Scholar]
- 96.Etzel T.M., Braun J.M., Buckley J.P. Associations of serum perfluoroalkyl substance and vitamin D biomarker concentrations in NHANES, 2003–2010. Int. J. Hyg. Environ. Health. 2019;222:262–269. doi: 10.1016/j.ijheh.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang L., Sun W., Chen H., Zhang Z., Cai W. Transcriptomic Changes in Liver of Juvenile Cynoglossus semilaevis following Perfluorooctane Sulfonate Exposure. Environ. Toxicol. Chem. 2020;39:556–564. doi: 10.1002/etc.4633. [DOI] [PubMed] [Google Scholar]
- 98.Qazi M.R., Abedi M.R., Nelson B.D., DePierre J.W., Abedi-Valugerdi M. Dietary exposure to perfluorooctanoate or perfluorooctane sulfonate induces hypertrophy in centrilobular hepatocytes and alters the hepatic immune status in mice. Int. Immunopharmacol. 2010;10:1420–1427. doi: 10.1016/j.intimp.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 99.Qazi M.R., Hassan M., Nelson B.D., DePierre J.W., Abedi-Valugerdi M. Both sub-acute, moderate-dose and short-term, low-dose dietary exposure of mice to perfluorooctane sulfonate exacerbates concanavalin A-induced hepatitis. Toxicol. Lett. 2013;217:67–74. doi: 10.1016/j.toxlet.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 100.Huang J., Wang Q., Liu S., Lai H., Tu W. Comparative chronic toxicities of PFOS and its novel alternatives on the immune system associated with intestinal microbiota dysbiosis in adult zebrafish. J. Hazard. Mater. 2022;425:127950. doi: 10.1016/j.jhazmat.2021.127950. [DOI] [PubMed] [Google Scholar]
- 101.Guillette T.C., McCord J., Guillette M., Polera M.E., Rachels K.T., Morgeson C., Kotlarz N., Knappe D., Reading B.J., Strynar M., et al. Elevated levels of per- and polyfluoroalkyl substances in Cape Fear River Striped Bass (Morone saxatilis) are associated with biomarkers of altered immune and liver function. Environ. Int. 2020;136:105358. doi: 10.1016/j.envint.2019.105358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Guo J., Wu P., Cao J., Luo Y., Chen J., Wang G., Guo W., Wang T., He X. The PFOS disturbed immunomodulatory functions via nuclear Factor-κB signaling in liver of zebrafish (Danio rerio) Fish. Shellfish Immunol. 2019;91:87–98. doi: 10.1016/j.fsi.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 103.Zhu J., Qian W., Wang Y., Gao R., Wang J., Xiao H. Involvement of mitogen-activated protein kinase and NF-κB signaling pathways in perfluorooctane sulfonic acid-induced inflammatory reaction in BV2 microglial cells. J. Appl. Toxicol. 2015;35:1539–1549. doi: 10.1002/jat.3119. [DOI] [PubMed] [Google Scholar]
- 104.Chen X., Nie X., Mao J., Zhang Y., Yin K., Sun P., Luo J., Liu Y., Jiang S., Sun L. Perfluorooctane sulfonate mediates secretion of IL-1β through PI3K/AKT NF-kB pathway in astrocytes. Neurotoxicol. Teratol. 2018;67:65–75. doi: 10.1016/j.ntt.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 105.Fletcher T., Galloway T.S., Melzer D., Holcroft P., Cipelli R., Pilling L.C., Mondal D., Luster M., Harries L.W. Associations between PFOA, PFOS and changes in the expression of genes involved in cholesterol metabolism in humans. Environ. Int. 2013;57–58:2–10. doi: 10.1016/j.envint.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 106.Elcombe C.R., Elcombe B.M., Foster J.R., Chang S.C., Ehresman D.J., Butenhoff J.L. Hepatocellular hypertrophy and cell proliferation in Sprague-Dawley rats from dietary exposure to potassium perfluorooctanesulfonate results from increased expression of xenosensor nuclear receptors PPARα and CAR/PXR. Toxicology. 2012;293:16–29. doi: 10.1016/j.tox.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 107.Behr A.C., Kwiatkowski A., Ståhlman M., Schmidt F.F., Luckert C., Braeuning A., Buhrke T. Impairment of bile acid metabolism by perfluorooctanoic acid (PFOA) and perfluorooctanesulfonic acid (PFOS) in human HepaRG hepatoma cells. Arch. Toxicol. 2020;94:1673–1686. doi: 10.1007/s00204-020-02732-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Andersen M.E., Hagenbuch B., Apte U., Corton J.C., Fletcher T., Lau C., Roth W.L., Staels B., Vega G.L., Clewell H.J., et al. Why is elevation of serum cholesterol associated with exposure to perfluoroalkyl substances (PFAS) in humans? A workshop report on potential mechanisms. Toxicology. 2021;459:152845. doi: 10.1016/j.tox.2021.152845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Na J.Y., Song K., Kim S., Kwon J. Hepatoprotective effect of phosphatidylcholine against carbon tetrachloride liver damage in mice. Biochem. Biophys. Res. Commun. 2015;460:308–313. doi: 10.1016/j.bbrc.2015.03.031. [DOI] [PubMed] [Google Scholar]
- 110.Sehnert B., Burkhardt H., Wessels J.T., Schröder A., May M.J., Vestweber D., Zwerina J., Warnatz K., Nimmerjahn F., Schett G., et al. NF-κB inhibitor targeted to activated endothelium demonstrates a critical role of endothelial NF-κB in immune-mediated diseases. Proc. Natl. Acad. Sci. USA. 2013;110:16556–16561. doi: 10.1073/pnas.1218219110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Han R., Hu M., Zhong Q., Wan C., Liu L., Li F., Zhang F., Ding W. Perfluorooctane sulphonate induces oxidative hepatic damage via mitochondria-dependent and NF-κB/TNF-α-mediated pathway. Chemosphere. 2018;191:1056–1064. doi: 10.1016/j.chemosphere.2017.08.070. [DOI] [PubMed] [Google Scholar]
- 112.Cichoż-Lach H., Michalak A. Oxidative stress as a crucial factor in liver diseases. World J. Gastroenterol. 2014;20:8082–8091. doi: 10.3748/wjg.v20.i25.8082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Xing J., Wang G., Zhao J., Wang E., Yin B., Fang D., Zhao J., Zhang H., Chen Y.Q., Chen W. Toxicity assessment of perfluorooctane sulfonate using acute and subchronic male C57BL/6J mouse models. Environ. Pollut. 2016;210:388–396. doi: 10.1016/j.envpol.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 114.Khansari M.R., Yousefsani B.S., Kobarfard F., Faizi M., Pourahmad J. In vitro toxicity of perfluorooctane sulfonate on rat liver hepatocytes: Probability of distructive binding to CYP 2E1 and involvement of cellular proteolysis. Environ. Sci. Pollut. Res. Int. 2017;24:23382–23388. doi: 10.1007/s11356-017-9908-2. [DOI] [PubMed] [Google Scholar]
- 115.Aubert J., Begriche K., Knockaert L., Robin M.A., Fromenty B. Increased expression of cytochrome P450 2E1 in nonalcoholic fatty liver disease: Mechanisms and pathophysiological role. Clin. Res. Hepatol. Gastroenterol. 2011;35:630–637. doi: 10.1016/j.clinre.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 116.Caro A.A., Cederbaum A.I. Oxidative stress, toxicology, and pharmacology of CYP2E1. Annu. Rev. Pharmacol. Toxicol. 2004;44:27–42. doi: 10.1146/annurev.pharmtox.44.101802.121704. [DOI] [PubMed] [Google Scholar]
- 117.Porubsky P.R., Meneely K.M., Scott E.E. Structures of human cytochrome P-450 2E1. Insights into the binding of inhibitors and both small molecular weight and fatty acid substrates. J. Biol. Chem. 2008;283:33698–33707. doi: 10.1074/jbc.M805999200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wu D., Cederbaum A.I. Inhibition of autophagy promotes CYP2E1-dependent toxicity in HepG2 cells via elevated oxidative stress, mitochondria dysfunction and activation of p38 and JNK MAPK. Redox Biol. 2013;1:552–565. doi: 10.1016/j.redox.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lv Z., Wu W., Ge S., Jia R., Lin T., Yuan Y., Kuang H., Yang B., Wu L., Wei J., et al. Naringin protects against perfluorooctane sulfonate-induced liver injury by modulating NRF2 and NF-κB in mice. Int. Immunopharmacol. 2018;65:140–147. doi: 10.1016/j.intimp.2018.09.019. [DOI] [PubMed] [Google Scholar]
- 120.Renu K., Chakraborty R., Myakala H., Koti R., Famurewa A.C., Madhyastha H., Vellingiri B., George A., Valsala Gopalakrishnan A. Molecular mechanism of heavy metals (Lead, Chromium, Arsenic, Mercury, Nickel and Cadmium)-induced hepatotoxicity—A review. Chemosphere. 2021;271:129735. doi: 10.1016/j.chemosphere.2021.129735. [DOI] [PubMed] [Google Scholar]
- 121.Ali E.S., Rychkov G.Y., Barritt G.J. TRPM2 Non-Selective Cation Channels in Liver Injury Mediated by Reactive Oxygen Species. Antioxidants. 2021;10:1243. doi: 10.3390/antiox10081243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Karch J., Kwong J.Q., Burr A.R., Sargent M.A., Elrod J.W., Peixoto P.M., Martinez-Caballero S., Osinska H., Cheng E.H., Robbins J., et al. Bax and Bak function as the outer membrane component of the mitochondrial permeability pore in regulating necrotic cell death in mice. Elife. 2013;2:e00772. doi: 10.7554/eLife.00772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Masubuchi Y., Suda C., Horie T. Involvement of mitochondrial permeability transition in acetaminophen-induced liver injury in mice. J. Hepatol. 2005;42:110–116. doi: 10.1016/j.jhep.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 124.Yan T., Huang J., Nisar M.F., Wan C., Huang W. The Beneficial Roles of SIRT1 in Drug-Induced Liver Injury. Oxid. Med. Cell. Longev. 2019;2019:8506195. doi: 10.1155/2019/8506195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang J., He W., Tsai P.J., Chen P.H., Ye M., Guo J., Su Z. Mutual interaction between endoplasmic reticulum and mitochondria in nonalcoholic fatty liver disease. Lipids Health Dis. 2020;19:72. doi: 10.1186/s12944-020-01210-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bian M., Fan R., Yang Z., Chen Y., Xu Z., Lu Y., Liu W. Pt (II)-NHC Complex Induces ROS-ERS-Related DAMP Balance to Harness Immunogenic Cell Death in Hepatocellular Carcinoma. J. Med. Chem. 2022;65:1848–1866. doi: 10.1021/acs.jmedchem.1c01248. [DOI] [PubMed] [Google Scholar]
- 127.Shin S.M., Yang J.H., Ki S.H. Role of the Nrf2-ARE pathway in liver diseases. Oxid. Med. Cell. Longev. 2013;2013:763257. doi: 10.1155/2013/763257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wan C., Han R., Liu L., Zhang F., Li F., Xiang M., Ding W. Role of miR-155 in fluorooctane sulfonate-induced oxidative hepatic damage via the Nrf2-dependent pathway. Toxicol. Appl. Pharmacol. 2016;295:85–93. doi: 10.1016/j.taap.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 129.Bensaad K., Vousden K.H. Savior and slayer: The two faces of p53. Nat. Med. 2005;11:1278–1279. doi: 10.1038/nm1205-1278. [DOI] [PubMed] [Google Scholar]
- 130.Chen W., Jiang T., Wang H., Tao S., Lau A., Fang D., Zhang D.D. Does Nrf2 contribute to p53-mediated control of cell survival and death? Antioxid. Redox. Signal. 2012;17:1670–1675. doi: 10.1089/ars.2012.4674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liss K.H., Finck B.N. PPARs and nonalcoholic fatty liver disease. Biochimie. 2017;136:65–74. doi: 10.1016/j.biochi.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chinetti G., Fruchart J.C., Staels B. Peroxisome proliferator-activated receptors (PPARs): Nuclear receptors at the crossroads between lipid metabolism and inflammation. Inflamm. Res. 2000;49:497–505. doi: 10.1007/s000110050622. [DOI] [PubMed] [Google Scholar]
- 133.Zhang L., Ren X.M., Wan B., Guo L.H. Structure-dependent binding and activation of perfluorinated compounds on human peroxisome proliferator-activated receptor γ. Toxicol. Appl. Pharmacol. 2014;279:275–283. doi: 10.1016/j.taap.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 134.Das K.P., Wood C.R., Lin M.T., Starkov A.A., Lau C., Wallace K.B., Corton J.C., Abbott B.D. Perfluoroalkyl acids-induced liver steatosis: Effects on genes controlling lipid homeostasis. Toxicology. 2017;378:37–52. doi: 10.1016/j.tox.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ye L., Zhao B., Yuan K., Chu Y., Li C., Zhao C., Lian Q.Q., Ge R.S. Gene expression profiling in fetal rat lung during gestational perfluorooctane sulfonate exposure. Toxicol. Lett. 2012;209:270–276. doi: 10.1016/j.toxlet.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 136.Su S., Billy L.J., Chang S., Gonzalez F.J., Patterson A.D., Peters J.M. The role of mouse and human peroxisome proliferator-activated receptor-α in modulating the hepatic effects of perfluorooctane sulfonate in mice. Toxicology. 2022;465:153056. doi: 10.1016/j.tox.2021.153056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rowan-Carroll A., Reardon A., Leingartner K., Gagné R., Williams A., Meier M.J., Kuo B., Bourdon-Lacombe J., Moffat I., Carrier R., et al. High-Throughput Transcriptomic Analysis of Human Primary Hepatocyte Spheroids Exposed to Per- and Polyfluoroalkyl Substances as a Platform for Relative Potency Characterization. Toxicol. Sci. 2021;181:199–214. doi: 10.1093/toxsci/kfab039. [DOI] [PubMed] [Google Scholar]
- 138.Bjork J.A., Butenhoff J.L., Wallace K.B. Multiplicity of nuclear receptor activation by PFOA and PFOS in primary human and rodent hepatocytes. Toxicology. 2011;288:8–17. doi: 10.1016/j.tox.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 139.Wolf C.J., Takacs M.L., Schmid J.E., Lau C., Abbott B.D. Activation of mouse and human peroxisome proliferator-activated receptor alpha by perfluoroalkyl acids of different functional groups and chain lengths. Toxicol. Sci. 2008;106:162–171. doi: 10.1093/toxsci/kfn166. [DOI] [PubMed] [Google Scholar]
- 140.Corton J.C., Peters J.M., Klaunig J.E. The PPARα-dependent rodent liver tumor response is not relevant to humans: Addressing misconceptions. Arch. Toxicol. 2018;92:83–119. doi: 10.1007/s00204-017-2094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Peters J.M., Cheung C., Gonzalez F.J. Peroxisome proliferator-activated receptor-alpha and liver cancer: Where do we stand? J. Mol. Med. 2005;83:774–785. doi: 10.1007/s00109-005-0678-9. [DOI] [PubMed] [Google Scholar]
- 142.Foreman J.E., Koga T., Kosyk O., Kang B.H., Zhu X., Cohen S.M., Billy L.J., Sharma A.K., Amin S., Gonzalez F.J., et al. Diminished Hepatocarcinogenesis by a Potent, High-Affinity Human PPARα Agonist in PPARA-Humanized Mice. Toxicol. Sci. 2021;183:70–80. doi: 10.1093/toxsci/kfab067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Corton J.C., Cunningham M.L., Hummer B.T., Lau C., Meek B., Peters J.M., Popp J.A., Rhomberg L., Seed J., Klaunig J.E. Mode of action framework analysis for receptor-mediated toxicity: The peroxisome proliferator-activated receptor alpha (PPARα) as a case study. Crit. Rev. Toxicol. 2014;44:1–49. doi: 10.3109/10408444.2013.835784. [DOI] [PubMed] [Google Scholar]
- 144.Jacobsen A.V., Nordén M., Engwall M., Scherbak N. Effects of perfluorooctane sulfonate on genes controlling hepatic fatty acid metabolism in livers of chicken embryos. Environ. Sci. Pollut. Res. Int. 2018;25:23074–23081. doi: 10.1007/s11356-018-2358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ueno T., Komatsu M. Autophagy in the liver: Functions in health and disease. Nat. Rev. Gastroenterol. Hepatol. 2017;14:170–184. doi: 10.1038/nrgastro.2016.185. [DOI] [PubMed] [Google Scholar]
- 146.Qiu T., Chen M., Sun X., Cao J., Feng C., Li D., Wu W., Jiang L., Yao X. Perfluorooctane sulfonate-induced insulin resistance is mediated by protein kinase B pathway. Biochem. Biophys. Res. Commun. 2016;477:781–785. doi: 10.1016/j.bbrc.2016.06.135. [DOI] [PubMed] [Google Scholar]
- 147.Li M., Gao P., Zhang J. Crosstalk between Autophagy and Apoptosis: Potential and Emerging Therapeutic Targets for Cardiac Diseases. Int. J. Mol. Sci. 2016;17:332. doi: 10.3390/ijms17030332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zeng H.C., Zhu B.Q., Wang Y.Q., He Q.Z. ROS-Triggered Autophagy Is Involved in PFOS-Induced Apoptosis of Human Embryo Liver L-02 Cells. Biomed. Res. Int. 2021;2021:6625952. doi: 10.1155/2021/6625952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dong Z., Wang J., Qiu T., Wu J., An Y., Shi X., Sun X., Jiang L., Liu X., Yang G., et al. Perfluorooctane sulfonate induces mitochondrial calcium overload and early hepatic insulin resistance via autophagy/detyrosinated alpha-tubulin-regulated IP3R2-VDAC1-MICU1 interaction. Sci. Total Environ. 2022;825:153933. doi: 10.1016/j.scitotenv.2022.153933. [DOI] [PubMed] [Google Scholar]
- 150.Yao X.F., Cao J., Xu L.M., Sun X.C., Kang J., Yang G., Jiang L.P., Geng C.Y., Gao C.Z., Zhong L.F., et al. Perfluorooctane sulfonate blocked autophagy flux and induced lysosome membrane permeabilization in HepG2 cells. Food Chem. Toxicol. 2014;67:96–104. doi: 10.1016/j.fct.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 151.Fulda S., Debatin K.M. Resveratrol modulation of signal transduction in apoptosis and cell survival: A mini-review. Cancer Detect. Prev. 2006;30:217–223. doi: 10.1016/j.cdp.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 152.Hu X.Z., Hu D.C. Effects of perfluorooctanoate and perfluorooctane sulfonate exposure on hepatoma Hep G2 cells. Arch. Toxicol. 2009;83:851–861. doi: 10.1007/s00204-009-0441-z. [DOI] [PubMed] [Google Scholar]
- 153.Zorov D.B., Juhaszova M., Sollott S.J. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 2014;94:909–950. doi: 10.1152/physrev.00026.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sinha K., Das J., Pal P.B., Sil P.C. Oxidative stress: The mitochondria-dependent and mitochondria-independent pathways of apoptosis. Arch. Toxicol. 2013;87:1157–1180. doi: 10.1007/s00204-013-1034-4. [DOI] [PubMed] [Google Scholar]
- 155.McCarthy N., Mercer J., Bennett M. Apoptotic proteins. p53 and c-myc related pathways. Cardiol. Clin. 2001;19:75–viii. doi: 10.1016/S0733-8651(05)70196-X. [DOI] [PubMed] [Google Scholar]
- 156.Huang Q., Zhang J., Peng S., Du M., Ow S., Pu H., Pan C., Shen H. Proteomic analysis of perfluorooctane sulfonate-induced apoptosis in human hepatic cells using the iTRAQ technique. J. Appl. Toxicol. 2014;34:1342–1351. doi: 10.1002/jat.2963. [DOI] [PubMed] [Google Scholar]
- 157.Vousden K.H. p53: Death star. Cell. 2000;103:691–694. doi: 10.1016/S0092-8674(00)00171-9. [DOI] [PubMed] [Google Scholar]
- 158.Cui Y., Liu W., Xie W., Yu W., Wang C., Chen H. Investigation of the Effects of Perfluorooctanoic Acid (PFOA) and Perfluorooctane Sulfonate (PFOS) on Apoptosis and Cell Cycle in a Zebrafish (Danio rerio) Liver Cell Line. Int. J. Environ. Res. Public Health. 2015;12:15673–15682. doi: 10.3390/ijerph121215012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Eke D., Çelik A., Yilmaz M.B., Aras N., Kocatürk Sel S., Alptekin D. Apoptotic gene expression profiles and DNA damage levels in rat liver treated with perfluorooctane sulfonate and protective role of curcumin. Int. J. Biol Macromol. 2017;104 Pt A:515–520. doi: 10.1016/j.ijbiomac.2017.06.075. [DOI] [PubMed] [Google Scholar]
- 160.Chang E.T., Adami H.O., Boffetta P., Cole P., Starr T.B., Mandel J.S. A critical review of perfluorooctanoate and perfluorooctanesulfonate exposure and cancer risk in humans. Crit. Rev. Toxicol. 2014;44((Suppl. S1)):1–81. doi: 10.3109/10408444.2014.905767. [DOI] [PubMed] [Google Scholar]
- 161.Roedl K., Jarczak D., Fuhrmann V. Organinteraktion Leber und Niere Organinteraction between liver and kidney. Dtsch. Med. Wochenschr. 2017;142:1365–1372. doi: 10.1055/s-0043-104465. [DOI] [PubMed] [Google Scholar]
- 162.Ciardullo S., Ballabeni C., Trevisan R., Perseghin G. Liver Stiffness, Albuminuria and Chronic Kidney Disease in Patients with NAFLD: A Systematic Review and Meta-Analysis. Biomolecules. 2022;12:105. doi: 10.3390/biom12010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ishay Y., Kolben Y., Kessler A., Ilan Y. Role of circadian rhythm and autonomic nervous system in liver function: A hypothetical basis for improving the management of hepatic encephalopathy. Am. J. Physiol. Gastrointest. Liver Physiol. 2021;321:G400–G412. doi: 10.1152/ajpgi.00186.2021. [DOI] [PubMed] [Google Scholar]
- 164.Correale M., Tarantino N., Petrucci R., Tricarico L., Laonigro I., Di Biase M., Brunetti N.D. Liver disease and heart failure: Back and forth. Eur. J. Intern. Med. 2018;48:25–34. doi: 10.1016/j.ejim.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 165.Palazzolo S., Caligiuri I., Sfriso A.A., Mauceri M., Rotondo R., Campagnol D., Canzonieri V., Rizzolio F. Early Warnings by Liver Organoids on Short- and Long-Chain PFAS Toxicity. Toxics. 2022;10:91. doi: 10.3390/toxics10020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Perugorria M.J., Olaizola P., Labiano I., Esparza-Baquer A., Marzioni M., Marin J., Bujanda L., Banales J.M. Wnt-β-catenin signalling in liver development, health and disease. Nat. Rev. Gastroenterol. Hepatol. 2019;16:121–136. doi: 10.1038/s41575-018-0075-9. [DOI] [PubMed] [Google Scholar]
- 167.Chen S.H., Liu X.N., Peng Y. MicroRNA-351 eases insulin resistance and liver gluconeogenesis via the PI3K/AKT pathway by inhibiting FLOT2 in mice of gestational diabetes mellitus. J. Cell. Mol. Med. 2019;23:5895–5906. doi: 10.1111/jcmm.14079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Qiu L., Qian Y., Liu Z., Wang C., Qu J., Wang X., Wang S. Perfluorooctane sulfonate (PFOS) disrupts blood-testis barrier by down-regulating junction proteins via p38 MAPK/ATF2/MMP9 signaling pathway. Toxicology. 2016;373:1–12. doi: 10.1016/j.tox.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 169.Wang C., Nie X., Zhang Y., Li T., Mao J., Liu X., Gu Y., Shi J., Xiao J., Wan C., et al. Reactive oxygen species mediate nitric oxide production through ERK/JNK MAPK signaling in HAPI microglia after PFOS exposure. Toxicol. Appl. Pharmacol. 2015;288:143–151. doi: 10.1016/j.taap.2015.06.012. [DOI] [PubMed] [Google Scholar]