Abstract
Porcine epidemic diarrhea (PED), characterized by diarrhea, vomiting, and dehydration, is an acute enteric infectious disease of pigs. The disease is caused by porcine epidemic diarrhea virus (PEDV), which infects the intestinal mucosal surface. Therefore, mucosal immunization through the oral route is an effective method of immunization. Lactic acid bacteria, which are acid resistant and bile-salt resistant and improve mucosal immunity, are ideal carriers for oral vaccines. The S1 glycoprotein of PEDV mediates binding of the virus with cell receptors and induces neutralizing antibodies against the virus. Therefore, we reversely screened the recombinant strain pPG-SD-S1/Δupp ATCC 393 expressing PEDV S1 glycoprotein by Lactobacillus casei deficient in upp genotype (Δupp ATCC 393). Mice were orally immunized three times with the recombinant bacteria that had been identified for expression, and the changes of anti-PEDV IgG and secreted immunoglobulin A levels were observed over 70 days. The results indicated that the antibody levels notably increased after oral administration of recombinant bacteria. The detection of extracellular cytokines on the 42nd day after immunization indicated high levels of humoral and cellular immune responses in mice. The above results demonstrate that pPG-SD-S1/Δupp ATCC 393 has great potential as an oral vaccine against PEDV.
Keywords: PEDV S1 glycoprotein, recombinant Lactobacillus, mucosal immunity, oral vaccine
1. Introduction
Porcine epidemic diarrhea (PED) is an acute viral disease of pigs that causes huge economic losses to the global agriculture industry [1,2]. Presently, the RNA vaccine and inactivated whole virus vaccine developed by HarrisvaccinesTM and Zoetis, respectively, are widely used and effective against PEDV [3]. Porcine epidemic diarrhea virus (PEDV), which mainly causes intestinal epithelial cell damage in neonatal pigs, is the etiological agent of PED; therefore, oral vaccines that effectively stimulate the intestinal mucosal immune response have proven valuable for practical application [4]. To achieve an adequate level of mucosal immune response at the relevant site, oral vaccines must be protected against a harsh digestive environment [5]. Therefore, effective antigen delivery vehicles are crucial for oral vaccines.
Lactic acid bacteria (LAB) have been reported to effectively induce mucosal immune response as an oral vaccine vector for enteroviruses [6,7]. Lactobacillus casei, a type of LAB, has many beneficial properties that make it an ideal carrier for antigen presentation. L. casei can survive, colonize, and exert intrinsic adjuvant activity in the upper gastrointestinal tract [8]. Furthermore, L. casei can effectively induce the production of secreted immunoglobulin A (SIgA) and enhance both humoral and cellular immunity [9,10,11]. The upp gene, encoding uracil phosphoribosyltransferase (UPRTase), which is involved in the purine and pyrimidine salvage pathways, is a widely used counter-selection marker in bacteria. UPRTase can convert 5-fluorouracil (5-FU) to 5-fluoro-UMP, inhibiting thymidylate synthase and causing cell death [12]. Compared with Δupp mutant strains, upp-expressing bacteria are sensitive to 5-FU [13]. Furthermore, upp was not found to be essential in the genome analysis of L. casei [14]. Therefore, we constructed upp gene-deleted L. casei ATCC 393 (Δupp ATCC 393), providing a new screening method for obtaining recombinant bacterial strains.
The genome of PEDV is 28.5 kb in size and contains at least seven open reading frames (ORF), which code for the spike (S), envelope (E), membrane (M), nucleocapsid (N), ORF1a, ORF1b, and ORF3 proteins [15,16]. The S protein, which is the principal antigenic determinant, is closely associated with virus–host recognition and neutralizing antibodies produced and can be divided into S1 and S2 proteins by cleavage at a specific site [2,17]. The S1 protein, an important determinant of virulence, contributes to receptor recognition of neutralizing epitopes [18,19,20]. Therefore, it is the main target gene for vaccine development.
The predominant antibody isotype on mucosal surfaces, sIgA, can prevent bacterial and viral infections by establishing the defense of the intestinal mucosa [21,22]. The SIgA antibody found in colostrum is an excellent source for piglets to obtain passive immune protection, illustrating its importance in controlling PEDV infection [4]. Therefore, we constructed a recombinant LAB expressing Lactobacillus Ribosome Binding Site (SD) and the PEDV S1 glycoprotein for oral immunization to increase the level of sIgA in the intestinal mucosa.
In this study, a recombinant Δupp L. casei strain expressing the PEDV S1 protein was developed and evaluated for its potency as an oral vaccine. Changes in SIgA and IgG were monitored during the 70-day period after immunization, which provided the basis for the preparation of an effective oral PEDV vaccine.
2. Materials and Methods
2.1. Virus, Plasmid and Bacterial Strain
Δupp L. casei ATCC 393 (Δupp ATCC 393) was grown in de Man, Rogosa, and Sharpe (MRS) broth at 37 °C in a stationary state. The PEDV LJB/15 strain, isolated and identified in our laboratory, was propagated in Vero-L cells at 37 °C and 5% CO2. PEDV LJB2019, the parental sequence of the S1 glycoprotein gene in this experiment, was a PEDV epidemic strain amplified from clinical samples collected in a diseased pig farm in Heilongjiang Province, China in 2019. The Escherichia coli–LAB shuttle vector pPG-T7g10-PPT was constructed in our laboratory.
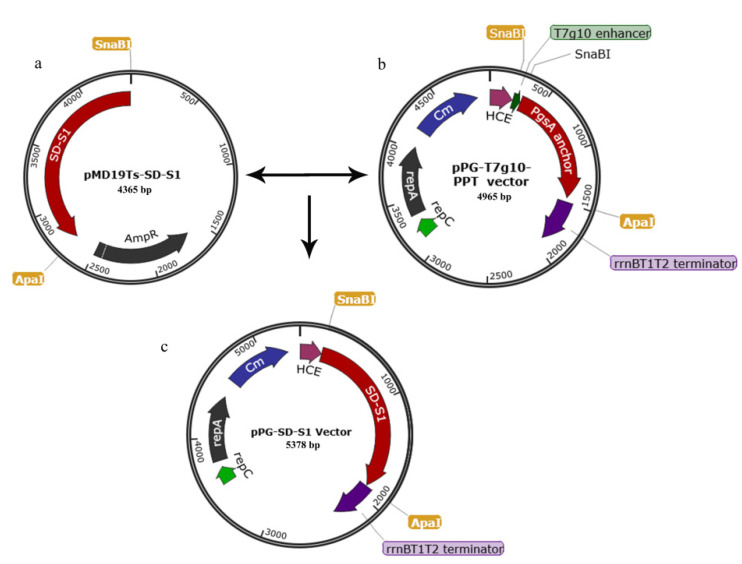
2.2. Construction of pPG-SD-S1/Δupp ATCC 393
The construction method for the recombinant plasmid is outlined in Figure 1. After the extraction of PEDV genomic RNA from PEDV LJB2019, the PEDV S1 gene was subjected to a reverse transcription (RT)-polymerase chain reaction (PCR). The Lactobacillus Ribosome Binding Site sequence (SD) was connected to the 5′ end of the S1 gene (The S1 gene sequence is shown in Figure S1.) by fusion PCR (Fusion PCR primer sequences are shown in Table 1). The SD-S1 (Figure 1a) fragment was linked to the plasmid pPG-T7g10-PPT (Figure 1b) by restriction enzyme digestion, generating the plasmid pPG-SD-S1. The recombinant plasmid pPG-SD-S1 (Figure 1c) was transformed into Δupp ATCC 393 competent cells by electroporation [23], generating the recombinant strain pPG-SD-S1/Δupp ATCC 393.
Figure 1.
Schematic diagram of recombinant plasmid construction. Constitutive cell surface expression plasmid pPG-T7g10-PPT (a), cloning vector pMD19Ts-SD-S1 (b) and recombinant plasmid pPG-SD-S1 (c). Fusion DNA fragment SD-S1 (Lactobacillus Ribosome Binding Site sequence (SD) and PEDV S1 glycoprotein gene) obtained from pMD19Ts-SD-S1 by SnaB I and Apa I digestion was inserted into the corresponding sites of plasmid pPG-T7g10-PPT, generating recombinant plasmid pPG-SD-S1.
Table 1.
Details of primers used in this study.
| Target | ID | Primer Sequence (5′-3′) | PCR Size |
|---|---|---|---|
| SD+ Flag |
SDF | TACGTAGCGAGGAGTGACGATAAAGATGAAATTAAAGCAA | 161 bp |
| SDR | CTTATCGTCGTCATCCTTGTAATCAAGTCGACCATCAGCTTTAACTGTTG | ||
| S1 | S1F | GTCGACTTGATTACAAGGATGACGACGATAAGTGCATTGGTTAT | 1518 bp |
| S1R | GGGCCCCTAGTAAAAGAAACCAGGCAACTC |
Bold type indicates restriction enzyme recognition sites used for cloning.
2.3. Protein Expression
The strain pPG-SD-S1/Δupp ATCC 393 was inoculated into MRS broth (1:100) and incubated for 12 h at 37 °C. Next, the culture was centrifuged at 4 °C, and the pellet and supernatant obtained were sonicated. Further, proteins in the sonicated supernatant and pellet were separated using 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and were electrotransferred onto polyvinylidene fluoride membranes (Millipore, Milford, MA, USA). The membranes were incubated with mouse S1 monoclonal antibody (stored in our laboratory) as the primary antibody for 1 h at 37 °C and horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG antibody (1:5000) (Thermo Scientific, Durham, NC, USA) as the secondary antibody for 1 h at 37 °C. The results were observed using a chemiluminescent substrate reagent (Solarbio, Beijing, China) according to the manufacturer’s instructions.
2.4. Immunization and Sample Collection
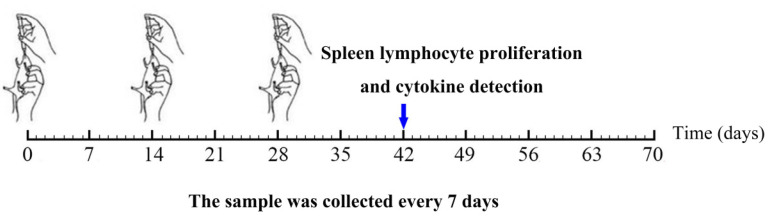
To evaluate the immunogenicity of pPG-SD-S1/Δupp L. casei 393 as an oral vaccine, 35-day-old female specific pathogen-free (SPF) BALB/c mice (n = 90) were housed in an SPF environment and provided with adequate water and food for the standard. The recombinant strains were inoculated in MRS broth (1:100) and cultured for 14 h at 37 °C. Further, the cultures were washed and diluted to a final concentration of 1010 colonu-forming units (CFU)/mL with phosphate-buffered saline (PBS). Three groups of mice were administered 200 µL PBS, Δupp ATCC 393, or pPG-SD-S1/Δupp ATCC 393 (30 mice per group). As shown in Figure 2, each mouse was immunized three times with an immunization cycle of 3 days, and each immunization was 14 days apart. To detect IgG and SIgA, the sera, tears, nasal fluid, genital mucus, intestinal mucus, and feces of the immunized mice were collected at 0, 7, 14, 21, 28, 35, 42, 49, 56, 63, and 70 days after the first immunization and stored at −40 °C until use. Of these, the intestinal mucus and feces required pretreatment. Intestinal mucus was flushed from the intestine using HEPES buffer. After incubation and centrifugation, the supernatant was stored at −40 °C until further use. In addition, 400 µL of 1% bovine serum albumin (BSA) and 1 mmol/L phenylmethylsulfonyl fluoride (Sigma, Ronkonkoma, NY, USA) were added to 0.1 g of feces, processed, and saved as previously described [24].
Figure 2.
The timeline of mice immunization procedure and sample collection. Mice (n = 90) were equally divided into three groups. The black font represents the days of immunization; a sample was collected every seven days. Spleen lymphocyte proliferation assay and cytokine detection were performed on day 42.
2.5. Enzyme-Linked Immunosorbent Assay (ELISA)
Changes in anti-PEDV IgG in serum were detected by indirect ELISA. The same method was used to monitor the levels of the SIgA antibody. Briefly, after overnight storage at 4 °C, PEDV was coated with polystyrene microtiter plates. The plates were washed with 100 µL PBS-0.1% Tween 20, 5% skim milk was added to each well, and the plate was incubated for 2 h at 37 °C. After the 100 µL samples were added (each sample was added in triplicates), the plate was incubated for 2 h at 37 °C. Further, 100 µL HRP-conjugated goat anti-mouse IgG/IgA antibody (1:5000) (Thermo Scientific, Durham, NC, USA) was added to the plate for 1 h at 37 °C. Finally, o-phenylenediamine dihydrochloride (Sigma, Ronkonkoma, NY, USA) was added as substrate, and absorbance was recorded at 490 nm.
2.6. Detection of PEDV Neutralizing Antibody Activity in Serum
To determine the neutralizing activity of anti-PEDV IgG in serum, 50 µL of serum from each immunized mouse was collected on the 42nd day after immunization and serially diluted (two-fold). The mixture of diluted serum and 50 µL of 50% tissue culture infected (TCID50) PEDV was plated at 37 °C, incubated for 1 h, and placed on a Vero-L cell monolayer in a 96-well plate at 37 °C for 1 h. The culture medium was replenished after discarding the solution. The presence of a PEDV-specific cytopathic effect was observed after two days incubation at 37 °C and 5% CO2. In this study, eight biological replicates and three technical replicates were set for each sample. In addition, a negative serum, positive serum, blank, and virus control were included in each experiment.
2.7. Lymphocyte Proliferation and Cytokine Detection
Three mice from each group were sacrificed on the 42nd day, and spleen cells were obtained under sterile conditions for the detection of spleen lymphocyte proliferation. Briefly, splenocytes at a concentration of 5 × 106 cells/mL (three replicates) were cultured in 96-well plates with RPMI1640 + 20% fetal bovine serum at 37 °C and 5% CO2. Splenocytes were stimulated with purified PEDV S1 protein at 1, 5, or 25 µg/mL for 60 h at 37 °C with 5% CO2. Simultaneously, 5 µg/mL concanavalin A (Con A) was set as a positive control, and RPMI1640 medium was set as a negative control. Spleen lymphocytes proliferation, detected by the CellTiter 96® AQueous Non-Radioactive Cell Proliferation Assay (Promega, Madison, WI, USA), was evaluated at 570 nm absorbance, according to the manufacturer’s instructions. Bars represented mean ± standard error of each group. According to the manufacturer’s instructions (Biosource International Inc., Camarillo, CA, USA), serum interleukin-2 (IL-2), interferon-γ (IFN-γ), IL-4, IL-12, IL-10, and IL-17 levels were detected using antigen capture ELISA. All of the above experiments were repeated three times, and the cytokine concentration was calculated based on the standard curve.
2.8. Statistical Analysis
The data are the mean of three replicates for a single sample ± standard error. GraphPad Prism v 5.0 (San Diego, CA, USA) was used for the statistical analysis of the data. Tukey’s multiple comparison test and two-way analysis of variance (ANOVA) were used to analyze the significance of differences between the means. Differences with p values less than 0.05 (p < 0.05) and less than 0.01 (p < 0.01) were considered significant and highly significant, respectively.
3. Results
3.1. Protein Expression
pPG-SD-S1/Δupp ATCC 393 and Δupp ATCC 393 were cultured overnight, centrifuged, and lysed for Western blotting. The bands of predictable size appeared in the supernatant and pellet of the pPG-SD-S1/Δupp ATCC 393 lysate but not in the supernatant and pellet of the Δupp ATCC 393 lysate, indicating that the target protein was effectively expressed (Figure 3a). To confirm that the recombinant bacteria stably expressed the target protein, overnight cultures from the 10th, 20th, 30th, 40th, and 50th generations of pPG-SD-S1/Δupp ATCC 393 were collected, centrifuged, and lysed for Western blotting. Predictable bands appeared in the 10th to 50th generation of pPG-SD-S1/Δupp ATCC 393 lysates (Figure 3b), whereas bands were not visible in the Δupp ATCC 393 lysates. The above results indicate that the recombinant bacteria stably expressed the target protein.
Figure 3.
The expression and stability of the target protein was identified in Western blots using a mouse anti-S1 monoclonal antibody (a,b). pPG-SD-S1/Δupp ATCC 393 lysate supernatant [pPG-SD-S1/Δupp ATCC393 (S)] and pellet [pPG-SD-S1/Δupp ATCC393 (P)] show relevant immunoreactive bands, but the supernatant (Δupp ATCC393 (S)) and pellet (Δupp ATCC393 (P)) of Δupp ATCC 393 lysate do not. The relevant immunoreactive bands are evident in the pPG-SD-S1/Δupp ATCC 393 lysate from the 10th to 50th generations, but not in Δupp ATCC 393. M: protein molecular weight marker.
3.2. Changes in IgG Levels Induced by Oral Immunization
Changes in anti-PEDV IgG antibody levels induced by pPG-SD-S1/Δupp ATCC 393 were detected by ELISA. As shown in Figure 4a, anti-PEDV IgG levels started to increase on day 7 and peaked on day 42 of the oral immunization with recombinant bacteria. In contrast, anti-PEDV IgG levels in the PBS and Δupp ATCC 393 groups did not change significantly (p < 0.05). In addition, the sera from immunized mice exhibited anti-PEDV neutralizing activity. The anti-PEDV neutralizing antibodies (IgG) in the serum obtained from mice orally immunized with pPG-SD-S1/Δupp ATCC 393 (1:28) were significantly higher than that with oral PBS (1:2) and Δupp ATCC 393 (1:2) (Figure 4b). The above results show that oral immunization with recombinant bacteria can effectively induce high levels of anti-PEDV immune response in mice.
Figure 4.
Determination of anti-porcine epidemic diarrhea virus (PEDV) specific IgG antibody (a) and anti-PEDV neutralizing activity in mice post-immunization (b). The levels of anti-PEDV IgG antibody were measured in the sera of immunized mice using indirect ELISA. The polyline represents changes in the anti-PEDV IgG level in orally immunized mice. Anti-PEDV neutralizing antibodies were detected by plaque reduction assay performed with dilutions of serum samples taken at the 42nd day post-immunization. Bars represent the mean ± standard error in each group (** p < 0.01 compared to the control groups: PBS and Δupp ATCC 393).
3.3. Changes in SIgA Levels Induced by Oral Immunization
To evaluate the mucosal immune response induced by oral recombinant bacteria in mice, ELISA was used to detect anti-PEDV SIgA levels in the tears, nasal fluid, genital mucus, intestinal mucus, and fecal samples. The levels of SIgA in the nasal fluid (Figure 5a), tears (Figure 5b), genital mucus (Figure 5c), intestinal mucus (Figure 5d), and feces (Figure 5e) in the oral pPG-SD-S1/Δupp ATCC 393 immunized group were significantly higher than those in the oral PBS and Δupp ATCC 393 groups and increased significantly on day 7 and peaked at 42 days. In contrast, anti-PEDV SIgA in the oral PBS and Δupp ATCC 393 groups did not show a significant change. The above results indicate that pPG-SD-S1/Δupp ATCC 393 could effectively induce a mucosal immune response in mice.
Figure 5.
The changes in anti-PEDV-specific SIgA antibody levels in the nasal fluid (a); tears (b); reproductive tract mucus (c); intestinal mucus (d); and feces (e) of immunized mice. The intestinal mucus was gently scraped from the excised intestinal tissue with HEPES buffer, and 0.1 g of feces was added to 400 µL of 1 mmol/L phenylmethylsulfonyl fluoride and 1% BSA. After incubation and centrifugation, the supernatant was stored at −40 °C until use. The anti-PEDV SIgA levels were measured using indirect ELISA. (** p < 0.01 compared to the control groups: PBS and Δupp ATCC 393).
3.4. Detection of Cytokines in Serum
To determine the type of immune response induced by oral recombinant bacteria, changes in cytokine levels were detected on the 42nd day. Compared to the oral PBS and Δupp ATCC 393 groups, the levels of cytokines IL-2, IFN-γ, IL-4, IL-12, IL-10, and IL-17 in the sera of the oral pPG-SD-S1/Δupp ATCC 393 group were significantly increased (Figure 6). These results show that oral administration of pPG-SD-S1/Δupp ATCC 393 could significantly stimulate the generation of Th1, Th2, and Th17 cellular immunity in mice.
Figure 6.
Determination of cytokine levels in immunized mice. Cytokine levels, including IFN-γ, IL-2, IL-4, IL-10, IL-12 and IL-17, were detected in the sera of mice on the 42nd day after the primary immunization. The concentrations of cytokines were calculated according to the standard curve. Bars represent mean ± standard error in each group (** p < 0.01 compared to the control groups: PBS and Δupp ATCC 393).
3.5. Lymphocyte Proliferation
Using Con A as a positive control and RPMI1640 as a negative control, isolated splenocytes were restimulated in vitro with PEDV S1 pure protein, followed by 3-(4,5-dimethylthiazol-2-yl)-2,5- diphenyltetrazolium bromide (MTT) assay. Compared with the oral PBS and Δupp ATCC 393 groups, the stimulation index of the oral pPG-SD-S1/Δupp ATCC 393 immunization group was significantly increased and showed a dose-dependent phenomenon (Figure 7).
Figure 7.
Lymphocyte proliferation in immunized mice was determined by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. With purified PEDV S1 protein as the stimulation source, the stimulation index of spleen lymphocytes isolated from immunized mice was detected by the MTT assay. Bars represent mean ± standard error in each group (** p < 0.01, compared to controls: PBS and Δupp ATCC 393).
4. Discussion
Currently, PED has become one of the major infectious diseases in pig farms, leading to heavy economic losses to the farming industry. The main surface antigen of PEDV is the spike protein (S), which is present on the capsular membrane [25]. The S protein interacts with specific host cell receptors, mediating the fusion of the virus with the cell membrane and permitting the virus to enter susceptible cells [26]; therefore, the protein is crucial for viral infection. Experimental results prove that neutralizing antibodies, which are closely associated with immune protection against viruses, could be induced by the S protein [27]. Based on the classic PEDV CV777 strain, the S protein is divided into the S1 (AA 1–726) and S2 (AA 727–1386) functional regions [28]. The plants such as tobacco or rice callus have been used for expressing PEDV S1 protein, and significant humoral and mucosal immune responses were induced in animals after feeding on them [29,30]. Therefore, in this study, the S1 glycoprotein gene amplified from the PEDV epidemic strain, with over 97% similarity with PEDV strains prevalent in recent years, was selected as the target gene. The strain contains the neutralizing antibody epitope and is a good candidate antigen for vaccines [31].
Presently, most vaccines against PEDV are intramuscular inactivated vaccines [32]. As PEDV infections mainly occur on the intestinal mucosal epithelial surface, mucosal immunity plays a crucial role in preventing PEDV infections [33]. Oral immunization effectively stimulates the digestive tract to produce local mucosal immunity, causing a systemic immune response [34]. LAB, having advantages such as acid resistance, bile salt resistance, avoidance of immune tolerance, and mucosal immunity improvement, are extensively used as oral vaccine carriers [35]. Research has shown that L. casei ATCC 393, expressing a fusion protein of the PCV2 capsid protein and E. coli thermolabile toxin B subunit, stimulates a strong mucosal immune response against PCV2 in mice after oral immunization [36]. In addition, L. plantarum, which expresses severe acute respiratory syndrome coronavirus 2, can generate an immune response in the respiratory tract. These results suggest that LAB have the potential to become mucosal vaccines against COVID-19 [37]. Therefore, LAB is an ideal carrier for oral vaccines.
In this study, the SD sequence, the RBS and signal peptide sequence of Lactobacillus casei to improve protein expression, and the PEDV S1 glycoprotein were expressed by the shuttle vector E. coli–LAB in Δupp ATCC 393. The recombinant strain was used for oral immunization to evaluate its immune efficacy in mice. In view of the highly mutant form of the PEDV S protein, the S1 gene selected in this experiment was amplified from the PEDV epidemic strains. Therefore, recombinant bacteria have practical applications, and the results of oral immunization in mice corroborate this fact. The experimental results showed that the oral administration of pPG-SD-S1/Δupp ATCC 393 could stimulate an increase in anti-PEDV IgG and SIgA levels in mice, indicating that pPG-SD-S1/Δupp ATCC 393 has the potential to act as a PEDV oral vaccine.
The gut is the primary site of PEDV infection and transmission; therefore, high levels of IgG and SIgA are required for an effective mucosal immune response against PEDV [38]. In addition, SIgA is also one of the evaluation criteria for the degree of virus infection and protective efficacy of vaccines [39,40]. The experimental results showed that anti-PEDV IgG antibodies increased after the oral administration of pPG-SD-S1/Δupp ATCC 393, and this increase was more notable after booster immunization. Furthermore, antibody neutralization experiments demonstrated that IgG on day 42 after immunization (anti-PEDV-specific IgG antibody levels peak on this day) could complement immune defense by reducing the aggressiveness of PEDV. IgA has been shown to peak at six weeks in piglets and decrease at eight weeks [4]. Neonatal pigs could only be protected after 35 days of durable immunity. Therefore, changes in SIgA levels were monitored at 70 days after the primary immunization. The oral administration of pPG-SD-S1/Δupp ATCC 393 effectively induced the production of high levels of SIgA in the nasal fluid, tears, genital mucus, intestinal mucus, and feces of mice. Meanwhile, the levels of SIgA peaked at 42 days after the primary immunization, indicating that oral administration of pPG-SD-S1/Δupp ATCC 393 could effectively elicit the mucosal immune response.
Additionally, the secretion levels of cytokines IL-2, IFN-γ, IL-10, IL-4, IL-12, and IL-17 were significantly increased after oral immunization with pPG-SD-S1/Δupp ATCC 393, indicating that the recombinant bacteria significantly stimulated the production of Th1, Th2, and Th17 cellular immunity in mice. Th1 responses are connected to cell-mediated immunity, whereas Th2 responses are related to humoral immunity [41]. IFN-γ and IL-2, which are Th1-type cytokines, assist antibody production, participate in cellular immune response, T cell proliferation, and induce cytotoxic effects [42,43]. IL-12 stimulates differentiation of T cells into Th1 or committed Th1 cells [44]. IL-4 stimulates the growth and differentiation of B lymphocytes, as well as antibody production. Moreover, IL-4 can also stimulate dendritic cells to produce IFN-γ, displaying a synergistic effect with IL-12 [44]. Both Th1 and Th2 cells can induce the production of IL-10 [43]. IL-17, which is produced by Th17 cells, is involved in neutrophil excitation, further stimulating the production of pro-inflammatory responses [45]. In this study, the cytokines level in serum was significantly increased on the 14th day after the third round of immunization, but oral administration of Δupp ATCC 393 could not produce a significant difference with the oral PBS group, indicating that oral administration of pPG-SD-S1/Δupp ATCC 393 can induce strong humoral and cellular immunity in mice simultaneously. Similar results were observed in spleen lymphocyte proliferation experiments.
In conclusion, oral immunization of pPG-SD-S1/Δupp ATCC 393 could stimulate mice to produce specific immune responses against PEDV. This study can be used as a reference to develop PEDV vaccines for piglets. In the future, we will insert the SD-S1 sequence into the genome of Lactobacillus casei, using the upp gene deficiency as a counter-selection marker, by homologous recombination. Future experiments will focus on the immune protection effect of the recombinant strains in a porcine model.
5. Conclusions
In conclusion, we developed an anti-PEDV vaccine for oral administration using recombinant L. casei to deliver the S1 antigen and demonstrated that the recombinant bacteria pPG-SD-S1/Δupp ATCC 393, reverse screened by Δupp ATCC 393, effectively induces an immune response against PEDV; therefore, this recombinant strain can be a potential oral PEDV vaccine.
Acknowledgments
This experiment was supported by the National Natural Science Foundation of China (NSFC; Grant 31972718 and Grant 32102707), and supported by the State Key Laboratory of Veterinary Etiological Biology, Lanzhou Veterinary Research Institute, Chinese Academy of Agricultural Sciences.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v14050890/s1, Figure S1: The S1 gene sequence used in this study.
Author Contributions
Conceptualization: Y.L. (Yijing Li) and L.T.; methodology: X.W.; software: H.Z. (Haiyuan Zhao); validation: Y.L. (Yue Li), F.L. and Y.S.; formal analysis: L.Z.; investigation: G.D.; resources: J.L.; data curation: W.C.; writing—original draft preparation: Y.X.; writing—review and editing: Z.S.; visualization: Y.J.; supervision: H.Z. (Han Zhou). and X.Q.; project administration: L.W.; funding acquisition: Y.L. (Yijing Li). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All the experimental procedures and animal management procedures were approved by the Institutional Committee of the Northeast Agricultural University for the Animal Experiments (2016NEFU-315, 13 April 2017), Harbin, China.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found in Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhang Q., Yoo D. Immune evasion of porcine enteric coronaviruses and viral modulation of antiviral innate signaling. Virus Res. 2016;226:128–141. doi: 10.1016/j.virusres.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song D., Park B. Porcine epidemic diarrhoea virus: A comprehensive review of molecular epidemiology, diagnosis, and vaccines. Virus Genes. 2012;44:167–175. doi: 10.1007/s11262-012-0713-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crawford K., Lager K.M., Kulshreshtha V., Miller L.C., Faaberg K.S. Status of vaccines for porcine epidemic diarrhea virus in the United States and Canada. Virus Res. 2016;226:108–116. doi: 10.1016/j.virusres.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Yu M., Wang L., Ma S. Immunogenicity of eGFP-Marked Recombinant Lactobacillus casei against Transmissible Gastroenteritis Virus and Porcine Epidemic Diarrhea Virus. Viruses. 2017;9:274. doi: 10.3390/v9100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shima H., Watanabe T., Fukuda S., Fukuoka S., Ohara O., Ohno H. A novel mucosal vaccine targeting Peyer’s patch M cells induces protective antigen-specific IgA responses. Int. Immunol. 2014;26:619–625. doi: 10.1093/intimm/dxu061. [DOI] [PubMed] [Google Scholar]
- 6.Shonyela S.M., Shi C., Yang W., Cao X., Yang G., Wang C. Recombinant Lactobacillus plantarum NC8 strain expressing porcine rotavirus VP7 induces specific antibodies in BALB/c mice. Acta Biochem. Biophys. 2021;53:12. doi: 10.1093/abbs/gmab050. [DOI] [PubMed] [Google Scholar]
- 7.Zhao Y.L., Bo Y.D., Chen Z.Q. Expression of S1 gene of porcine transmissible gastroenteritis virus in food graded lactococcus lactis. Chin. J. Vet. Sci. 2015;35:868–872. [Google Scholar]
- 8.Peran L., Camuesco D., Comalada M. A comparative study of the preventative effects exerted by three probiotics, Bifidobacterium lactis, Lactobacillus casei and Lactobacillus acidophilus, in the TNBS model of rat colitis. J. Appl. Microbiol. 2010;103:836–844. doi: 10.1111/j.1365-2672.2007.03302.x. [DOI] [PubMed] [Google Scholar]
- 9.Wang G.H., Hou X.L., Yu L.Y., Liu J.K., Wei C.H. Studies on Mucosal Immunity Induced by Transmissible Gastroenteritis Virus Nucleocapsid Protein Recombinant Lactobacillus casei in Mice and Sow. Chin. Agric. Sci. 2009;8:231–237. doi: 10.1016/S1671-2927(09)60031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y., Yan X., Han D. Lactobacillus casei DBN023 protects against jejunal mucosal injury in chicks infected with Salmonella pullorum CMCC-533. Res. Vet. Sci. 2019;127:33–41. doi: 10.1016/j.rvsc.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Zhao L., Guo Z., Liu J. Recombinant Lactobacillus casei expressing Clostridium perfringens toxoids α, β2, ε and β1 gives protection against Clostridium perfringens in rabbits. Vaccine. 2017;35:4010–4021. doi: 10.1016/j.vaccine.2017.05.076. [DOI] [PubMed] [Google Scholar]
- 12.Song L., Cui H., Tang L. Construction of upp deletion mutant strains of Lactobacillus casei and Lactococcus lactis based on counterselective system using temperature-sensitive plasmid. J. Microbiol. Methods. 2014;102:37–44. doi: 10.1016/j.mimet.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Peck R.F., Dassarma S., Krebs M.P. Homologous gene knockout in the archaeon Halobacterium salinarum with ura3 as a counterselectable marker. Mol. Microbiol. 2000;35:667–676. doi: 10.1046/j.1365-2958.2000.01739.x. [DOI] [PubMed] [Google Scholar]
- 14.Barrangou R., Azcarate-Peril M.A., Duong T., Conners S.B., Kelly R.M., Klaenhammer T.R. Global analysis of carbohydrate utilization by Lactobacillus acidophilus using cDNA microarrays. Proc. Natl. Acad. Sci. USA. 2006;103:3816–3821. doi: 10.1073/pnas.0511287103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang C.Y., Hsu W.T., Chao Y.C., Chang H.W. Display of Porcine Epidemic Diarrhea Virus Spike Protein on Baculovirus to Improve Immunogenicity and Protective Efficacy. Viruses. 2018;10:346. doi: 10.3390/v10070346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makadiya N., Brownlie R., van den Hurk J. S1 domain of the porcine epidemic diarrhea virus spike protein as a vaccine antigen. Virol. J. 2016;13:57. doi: 10.1186/s12985-016-0512-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wicht O., Li W., Willems L. Proteolytic activation of the porcine epidemic diarrhea coronavirus spike fusion protein by trypsin in cell culture. J. Virol. 2014;88:7952–7961. doi: 10.1128/JVI.00297-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li C., Li W., Lucio de Esesarte E. Cell Attachment Domains of the Porcine Epidemic Diarrhea Virus Spike Protein Are Key Targets of Neutralizing Antibodies. J. Virol. 2017;91:e00273-17. doi: 10.1128/JVI.00273-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang S.H., Bae J.L., Kang T.J. Identification of the epitope region capable of inducing neutralizing antibodies against the porcine epidemic diarrhea virus. Mol. Cells. 2002;14:295–299. [PubMed] [Google Scholar]
- 20.Suzuki T., Terada Y., Enjuanes L., Ohashi S., Kamitani W. S1 Subunit of Spike Protein from a Current Highly Virulent Porcine Epidemic Diarrhea Virus is an Important Determinant of Virulence in Piglets. Viruses. 2018;10:467. doi: 10.3390/v10090467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phalipon A., Cardona A., Kraehenbuhl J.P., Edelman L., Sansonetti P.J., Corthésy B. Secretory component: A new role in secretory IgA-mediated immune exclusion in vivo. Immunity. 2002;17:107–115. doi: 10.1016/S1074-7613(02)00341-2. [DOI] [PubMed] [Google Scholar]
- 22.Hodgkinson A.J., Cakebread J., Callaghan M. Comparative innate immune interactions of human and bovine secretory IgA with pathogenic and non-pathogenic bacteria. Dev. Comp. Immunol. 2017;68:21–25. doi: 10.1016/j.dci.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Jiang X., Yu M., Qiao X. Up-regulation of MDP and tuftsin gene expression in Th1 and Th17 cells as an adjuvant for an oral Lactobacillus casei vaccine against anti-transmissible gastroenteritis virus. Appl. Microbiol. Biotechnol. 2014;98:8301–8312. doi: 10.1007/s00253-014-5893-2. [DOI] [PubMed] [Google Scholar]
- 24.Wang X., Wang L., Huang X. Oral Delivery of Probiotics Expressing Dendritic Cell-Targeting Peptide Fused with Porcine Epidemic Diarrhea Virus COE Antigen: A Promising Vaccine Strategy against PEDV. Viruses. 2017;9:312. doi: 10.3390/v9110312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou Y., Chen C., Chen Y. Effect of route of inoculation on innate and adaptive immune responses to porcine epidemic diarrhea virus infection in suckling pigs. Vet. Microbiol. 2019;228:83–92. doi: 10.1016/j.vetmic.2018.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma S., Wang L., Huang X. Oral recombinant Lactobacillus vaccine targeting the intestinal microfold cells and dendritic cells for delivering the core neutralizing epitope of porcine epidemic diarrhea virus. Microb. Cell Factories. 2018;17:20. doi: 10.1186/s12934-018-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X.N., Wang L., Zheng D.Z. Oral immunization with a Lactobacillus casei-based anti-porcine epidemic diarrhoea virus (PEDV) vaccine expressing microfold cell-targeting peptide Co1 fused with the COE antigen of PEDV. J. Appl. Microbiol. 2018;124:368–378. doi: 10.1111/jam.13652. [DOI] [PubMed] [Google Scholar]
- 28.Zhao P., Wang B., Ji C.M., Cong X., Wang M., Huang Y.W. Identification of a peptide derived from the heptad repeat 2 region of the porcine epidemic diarrhea virus (PEDV) spike glycoprotein that is capable of suppressing PEDV entry and inducing neutralizing antibodies. Antivir. Res. 2018;150:1–8. doi: 10.1016/j.antiviral.2017.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huy N.-X., Yang M.-S., Kim T.-G. Expression of a Cholera Toxin B Subunit-Neutralizing Epitope of the Porcine Epidemic Diarrhea Virus Fusion Gene in Transgenic Lettuce (Lactuca sativa L.) Mol. Biotechnol. 2011;48:201–209. doi: 10.1007/s12033-010-9359-1. [DOI] [PubMed] [Google Scholar]
- 30.Kang T.J., Seo J.E., Kim D.H., Kim T.G., Jang Y.S., Yang M.S. Cloning and sequence analysis of the Korean strain of spike gene of porcine epidemic diarrhea virus and expression of its neutralizing epitope in plants. Protein Expr. Purif. 2005;41:378–383. doi: 10.1016/j.pep.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Hou X., Jiang X., Jiang Y. Oral Immunization against PEDV with Recombinant Lactobacillus casei Expressing Dendritic Cell-Targeting Peptide Fusing COE Protein of PEDV in Piglets. Viruses. 2018;10:106. doi: 10.3390/v10030106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gerdts V., Zakhartchouk A. Vaccines for porcine epidemic diarrhea virus and other swine coronaviruses. Vet. Microbiol. 2017;206:45–51. doi: 10.1016/j.vetmic.2016.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang S., Wu J., Wang F. Expression Pattern Analysis of Antiviral Genes and Inflammatory Cytokines in PEDV-Infected Porcine Intestinal Epithelial Cells. Front. Vet. Sci. 2020;7:75. doi: 10.3389/fvets.2020.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo M., Yi S., Guo Y. Construction of a Recombinant Lactococcus lactis Strain Expressing a Variant Porcine Epidemic Diarrhea Virus S1 Gene and Its Immunogenicity Analysis in Mice. Viral Immunol. 2019;32:144–150. doi: 10.1089/vim.2018.0108. [DOI] [PubMed] [Google Scholar]
- 35.Vilander A.C., Dean G.A. Adjuvant Strategies for Lactic Acid Bacterial Mucosal Vaccines. Vaccines. 2019;7:150. doi: 10.3390/vaccines7040150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li F., Wang X., Ma R. Oral Immunization with Lactobacillus casei Expressing the Porcine Circovirus Type 2 Cap and LTB Induces Mucosal and Systemic Antibody Responses in Mice. Viruses. 2021;13:1302. doi: 10.3390/v13071302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Villena J., Li C., Vizoso-Pinto M.G., Sacur J., Ren L., Kitazawa H. Lactiplantibacillus plantarum as a Potential Adjuvant and Delivery System for the Development of SARS-CoV-2 Oral Vaccines. Microorganisms. 2021;9:683. doi: 10.3390/microorganisms9040683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qian S., Zhang W., Jia X. Isolation and Identification of Porcine Epidemic Diarrhea Virus and Its Effect on Host Natural Immune Response. Front. Microbiol. 2019;10:2272. doi: 10.3389/fmicb.2019.02272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chairatana P., Nolan E.M. Defensins, lectins, mucins, and secretory immunoglobulin A: Microbe-binding biomolecules that contribute to mucosal immunity in the human gut. Crit. Rev. Biochem. Mol. Biol. 2017;52:45–56. doi: 10.1080/10409238.2016.1243654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y., Zhang E., Huang L. Detection and correlation analysis of digestive tract specific SIgA by oral inactivated porcine epidemic diarrhea virus. J. Nanjing Agric. Univ. 2019;42:499–504. [Google Scholar]
- 41.Asseman C., Read S., Powrie F. Colitogenic Th1 cells are present in the antigen-experienced T cell pool in normal mice: Control by CD4+ regulatory T cells and IL-10. J. Immunol. 2003;171:971–978. doi: 10.4049/jimmunol.171.2.971. [DOI] [PubMed] [Google Scholar]
- 42.Szabo S.J. Distinct Effects of T-bet in TH1 Lineage Commitment and IFN-γ Production in CD4 and CD8 T Cells. Science. 2002;295:338–342. doi: 10.1126/science.1065543. [DOI] [PubMed] [Google Scholar]
- 43.O’Garra A., Barrat F.J. In vitro generation of IL-10-producing regulatory CD4+ T cells is induced by immunosuppressive drugs and inhibited by Th1- and Th2-inducing cytokines. Immunol. Lett. 2003;85:135–139. doi: 10.1016/S0165-2478(02)00239-0. [DOI] [PubMed] [Google Scholar]
- 44.Fukao T., Matsuda S., Koyasu S. Synergistic effects of IL-4 and IL-18 on IL-12-dependent IFN-gamma production by dendritic cells. J. Immunol. 2000;164:64–71. doi: 10.4049/jimmunol.164.1.64. [DOI] [PubMed] [Google Scholar]
- 45.Bai H., Cheng J., Gao X. IL-17/Th17 promotes type 1 T cell immunity against pulmonary intracellular bacterial infection through modulating dendritic cell function. J. Immunol. 2009;183:5886–5895. doi: 10.4049/jimmunol.0901584. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found in Supplementary Materials.