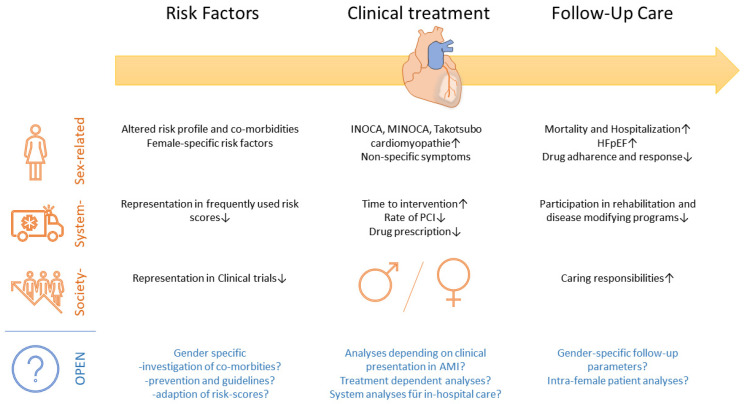
In the recently published review titled “Update on Management of Cardiovascular Diseases in Women”, Lucà et al. highlight sex-related differences in cardiovascular disease [1]. We read this review with great interest and aim to lead the attention of the reader to the following summarized aspects with felt open gaps for possible future analyses (Figure 1):
-
(1)
What are the differences in risk factors and primary prevention for cardiovascular disease?
-
(2)
What are the differences in treatment in case of acute myocardial infarction (AMI) and percutaneous coronary intervention (PCI)?
-
(3)
What are the differences in follow-up care?
Figure 1.
Adapted summarized aspects for gender-specific differences in cardiovascular disease [1], depending on risk factors, clinical treatment, and follow-up care complemented by relevant open questions and aspects.
There is a lack of transfer for a one-fits-all concept for male and female patients. First, women were shown to have an altered risk profile for cardiovascular disease (CVD) with reduced incidence in the pre-menopausal state but increased rates afterward [2,3]. In this context, the importance of the menopause, hormone replacement therapy, and polycystic ovary syndrome is already highlighted in this review [1]. However, the relevance of endometriosis might also be reflected, as this was revealed as a relevant co-associated factor for CVD [4]. Moreover, the current literature lacks information about number of pregnancies or potential aborts. This can help us identify relevant mechanisms behind altered risk profile due to hormone status.
Next to sex-specific risk factors, women show increased rates of relevant CVD co-morbidities, such as anemia, chronic kidney disease, metabolic syndrome, or manifest diabetes and atrial fibrillation [5,6]. The importance of gender is reflected in the “2021 ESC Guidelines on cardiovascular disease prevention in clinical practice” guidelines with the presented SCORE2 risk estimator, which include female gender and age as relevant aspects [7]. However, co-morbidities also affect outcomes after AMI or PCI. Several studies indicated that women show worse follow-up after AMI or PCI. However, gender is only poorly represented infrequently used risk scores to predict outcomes after PCI or AMI. Moreover, reached endpoints are interestingly mainly driven by mortality, bleeding, and re-hospitalization, and not by ischemic events such as re-infarction [5,6]. In this context, balancing major adverse cerebral- and cardiovascular events (MACCE) versus bleeding is crucial. As women show increased bleeding rates, sex-specific adaption of dual antiplatelet therapy duration after stent replacement therapy shall be discussed. Nevertheless, gender is currently not included in the recommended PRECISE-DAPT or high-risk bleeding score by the Academic Research Consortium [8,9,10]. Additionally, cardiac function is a relevant follow-up parameter. In this context, women were, however, shown to have a higher systolic cardiac function than men despite the worsened outcome. This leads to the question if follow-up parameters shall be expanded with inclusion of diastolic dysfunction measurement and strain analysis as more sensitive routine parameters for women.
The current knowledge about women in CVD offers a conflict of a reduced risk profile but worsened outcome in female patients. Women, especially in the pre-menopause state, have strong cards on their hands, but lose the potential at higher ages and during follow-up after an acute event. Thus, what are the main drivers behind this interaction in the multiplicity of hitherto revealed aspects? Along with factors associated with patients and health care systems, society-associated reasons might also play a role. Women have more caring responsibilities which hinders assess to rehabilitation and disease management programs. Is there a need for gender-specific prevention campaigns and risk stratification or follow-up programs? With the goal of an optimized individualized medicine, there is still a lot of space for gender equality in CV medicine.
Abbreviations
AMI = acute myocardial infarction; CVD = cardiovascular disease, MACCE = major adverse cerebral- and cardiovascular events; PCI = percutaneous coronary intervention.
Author Contributions
Conceptualization, L.D., J.W. and J.K.; writing—original draft preparation, J.W., J.K., S.S., L.B., K.S. and S.G.; writing—review and editing, L.D., A.P., T.Z. and M.K.; supervision, L.D., T.Z. and M.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Forschungskommission of the Medical Faculty of the Heinrich Heine University (No. 29-2019, to L.D., No. 18-2019 to A.P.) and by the German Research Foundation (PO 2247/2-1 to A.P. and SFB1116 to A.P.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lucà F., Abrignani M.G., Parrini I., Di Fusco S.A., Giubilato S., Rao C.M., Piccioni L., Cipolletta L., Passaretti B., Giallauria F., et al. Update on Management of Cardiovascular Diseases in Women. J. Clin. Med. 2022;11:1176. doi: 10.3390/jcm11051176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Green D.J., Hopkins N.D., Jones H., Thijssen D.H.J., Eijsvogels T., Yeap B.B. Sex differences in vascular endothelial function and health in humans: Impacts of exercise. Exp. Physiol. 2016;101:230–242. doi: 10.1113/EP085367. [DOI] [PubMed] [Google Scholar]
- 3.Mathur P., Ostadal B., Romeo F., Mehta J.L. Gender-Related Differences in Atherosclerosis. Cardiovasc. Drugs Ther. 2015;29:319–327. doi: 10.1007/s10557-015-6596-3. [DOI] [PubMed] [Google Scholar]
- 4.Tan J., Taskin O., Iews M., Lee A.J., Kan A., Rowe T., Bedaiwy M.A. Atherosclerotic cardiovascular disease in women with endometriosis: A systematic review of risk factors and prospects for early surveillance. Reprod. Biomed. Online. 2019;39:1007–1016. doi: 10.1016/j.rbmo.2019.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Potts J., Sirker A., Martinez S.C., Gulati M., Alasnag M., Rashid M., Kwok C.S., Ensor J., Burke D.L., Riley R.D., et al. Persistent sex disparities in clinical outcomes with percutaneous coronary intervention: Insights from 6.6 million PCI procedures in the United States. PLoS ONE. 2018;13:e0203325. doi: 10.1371/journal.pone.0203325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kosmidou I., Leon M.B., Zhang Y., Serruys P.W., von Birgelen C., Smits P.C., Ben-Yehuda O., Redfors B., Madhavan M.V., Maehara A., et al. Long-Term Outcomes in Women and Men following Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2020;75:1631–1640. doi: 10.1016/j.jacc.2020.01.056. [DOI] [PubMed] [Google Scholar]
- 7.Visseren F.L., Mach F., Smulders Y.M., Carballo D., Koskinas K.C., Bäck M., Benetos A., Biffi A., Boavida J.M., Capodanno D., et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021;42:3227–3337. doi: 10.1093/eurheartj/ehab484. [DOI] [PubMed] [Google Scholar]
- 8.Knuuti J., Wijns W., Saraste A., Capodanno D., Barbato E., Funck-Brentano C., Prescott E., Storey R.F., Deaton C., Cuisset T., et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 9.Collet J.P., Thiele H., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2020;42:1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 10.Dannenberg L., Afzal S., Czychy N., M’Pembele R., Zako S., Helten C., Mourikis P., Zikeli D., Ahlbrecht S., Trojovsky K., et al. Risk prediction of bleeding and MACCE by PRECISE-DAPT score post-PCI. IJC Heart Vasc. 2021;33:100750. doi: 10.1016/j.ijcha.2021.100750. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.