Abstract
Crimean-Congo hemorrhagic fever (CCHF) is a zoonotic arboviral disease that poses a great threat to global health in the Old World, and it is endemic in Europe, Asia, and Africa, including Sudan. In this retrospective study, we reviewed previous epidemiological reports about the major epidemics of CCHF throughout Sudan between 2010 and 2020. During these epidemics, the infection of humans with Crimean-Congo hemorrhagic fever virus (CCHFV), the causative agent of CCHF, was diagnosed using qRT-PCR. We have identified 88 cases of CCHF, including 13 fatalities reported during five epidemics that occurred in 2010, 2011, 2015, 2019, and 2020. The two epidemics in 2010 and 2011 were by far the largest, with 51 and 27 cases reported, respectively. The majority of cases (78%) were reported in the endemic region of Kordofan. Here, we document that the first emergence of CCHFV in the Darfur region, West Sudan, occurred in 2010. We were not able to investigate outbreak dynamics through phylogenetic analysis due to the limited diagnostic capacity and the lack of sequencing services in the country. These findings call for establishing a genomic-based integrated One Health surveillance and response system for the early preparedness, prevention, and control of CCHF in the country.
Keywords: Crimean-Congo hemorrhagic fever (CCHF), zoonotic diseases, arboviral diseases, hemorrhagic fever, epidemic, outbreak, tick-borne diseases, climate change, neurotropic viruses, Sudan
1. Introduction
The public health threat posed by arboviral diseases is rapidly growing worldwide and expanding its geographical distribution [1]. The majority of arboviral diseases are zoonotic, circulating among human and animal populations as they have evolved to continuously expand their host range through several spillover and spillback events [2]. The global risk of arboviral epidemics is increasing. This growth is influenced by several risk factors including globalization, unplanned urbanization, climate change, and socioeconomic inequalities [3,4,5,6]. Other risk factors include armed conflicts, largescale displacements of human populations between endemic and non-endemic areas, and humanitarian crises [7,8,9,10,11]. Arboviruses are emerging in under-resourced, tropical countries, where health systems are not prepared for their early detection and containment, and where limited disease surveillance capacity exists [4,12]. In these settings, arboviral infections are commonly misdiagnosed and treated as malaria [7,8,10]. Additionally, the lack of awareness of local healthcare providers and policymakers about the prevalence of arboviruses in their areas usually leads them to ignore these diseases in their differential diagnoses, surveillance, prevention, and health policy development [13]. The underreporting of arboviral diseases when accidentally detected is also common [4,13]. Moreover, the delay or entire dearth of timely sharing of epidemic data impacts global health, as the population at risk, healthcare providers, and public health policymakers are not alerted in time to take preventive measures [13].
Crimean-Congo hemorrhagic fever (CCHF) is a tick-borne viral infection that is caused by the Crimean-Congo hemorrhagic fever virus (CCHFV), which belongs to the genus Orthonairovirus in the Nairoviridae family [14]. CCHF is a zoonotic disease that infects both humans and animals. It commonly does not cause illness in animals, but it is life-threatening for humans, with high case fatality rates (CFRs) of up to 40% but also very high rates of asymptomatic infections [14,15,16]. According to the World Health Organization (WHO), CCHFV is the most predominant cause of viral hemorrhagic fever outbreaks worldwide [15]. CCHF is endemic in over 45 countries in the Old World, with human cases and epidemics reported in several countries in Africa, Asia, and Europe [15,16,17]. The WHO consider CCHF to be one of the top epidemic-prone diseases globally [15].
In addition to the location of Sudan, as a tropical country in an epidemic-prone region [18], it is endemic with several infectious diseases, including a wide range of vector-borne diseases such as malaria [19], Leishmaniasis [20], onchocerciasis [21], and many arboviral diseases [4]. This co-endemicity and co-transmission imposes a serious diagnostic and overall prevention and control challenge for the limited health system of the country [4]. Therefore, in the absence of a health policy for the prevention and control of arboviral diseases in Sudan, the frequency and intensity of arboviral disease outbreaks are persistently increasing. In addition, the distribution of these arboviruses is steadily expanding throughout the country [4,9,11]. This, in turn, has led to a remarkable shift in diseases’ burden, from malaria to arboviruses in endemic areas [3,22]. This switch in disease burden is mainly attributed to climate change; the prevalence of arboviral diseases is predicted to continue to grow worldwide over the next few decades [22]. More importantly, considering the zoonotic nature of these diseases, the epizootic transmission of arboviral diseases has a devastating socioeconomic impact on the local community and creates a great financial burden for governments in countries that rely on animals and their products [23]. CCHF is endemic in the central region of the country and has recently been reported in the Darfur area in West Sudan, where humans and livestock move freely across the open borders between Sudan, Libya, Chad, Central Africa, and South Sudan [4,8]. CCHFV was isolated from sheep and several species of ticks imported from Sudan to Saudi Arabia [24,25]. This highlights the serious role of the passive dynamics of tick vectors using domestic and wild animals, including birds as mobile vehicles, which eventually expands the geographic distribution of CCHFV-competent tick vectors, mainly members of the genus Hyalomma [26]. Numerous species of ticks, including several members of the genus Hyalomma, are distributed throughout Sudan, increasing the potential risk of CCHF emergence countrywide and expanding the geographical distribution of the disease beyond the endemic region of Kordofan [4,26]. This risk is further intensified by the reliance of the communities in this region on the production and export of animals and their products for human consumption nationally and internationally [27].
Here, we analyze major epidemics of CCHF in Sudan in 2010, 2011, 2019, and 2020, and discuss the implications of this virus’ transmission on the public health, food safety, and security in the region. Furthermore, we highlight the need for a One Health strategy to prevent and control future epidemics of CCHF and other zoonotic diseases.
2. Materials and Methods
This is a retrospective study analyzing data about CCHF epidemics that have occurred in Sudan. The data were extracted from outbreak investigation reports from the Ministry of Health. According to the national protocol for the investigation of viral hemorrhagic fever outbreaks, blood samples were obtained from suspected cases that were clinically identified with hemorrhages. Samples were shipped to the National Public Health Laboratory in Khartoum, where they were molecularly analyzed. The QIAamp viral RNA mini kit (Qiagen Inc., Hilden, Germany) was used for the extraction of total RNA from blood samples following the manufacturer’s instructions. Samples were tested for CCHFV using qRT-PCR Kits (Shanghai ZJ Bio-Tech Co., Ltd., Shanghai, China) following the manufacturer’s guidelines.
3. Results
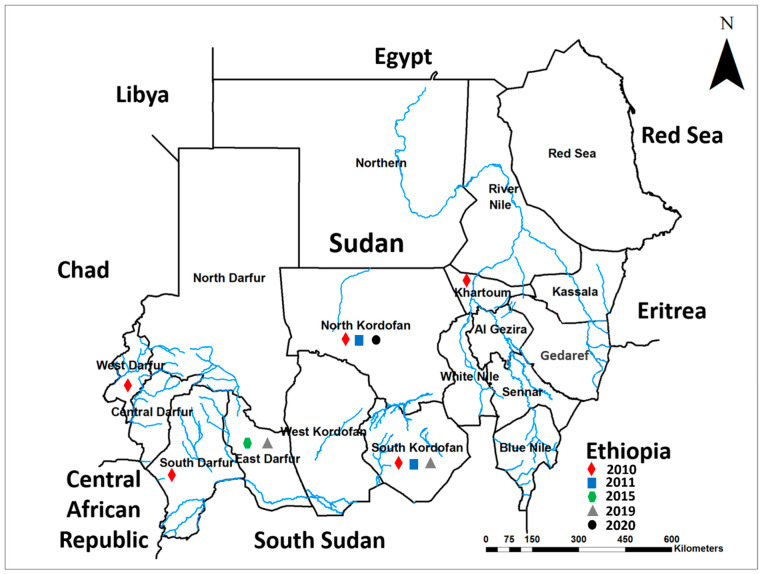
We have identified five epidemics of CCHF that occurred in Sudan during the previous ten years, between 2010 and 2020 (Figure 1). These epidemics occurred in 2010, 2011, 2015, 2019, and 2020 across several states of the country, namely Khartoum, North Kordofan, South Kordofan, East Darfur, North Darfur, South Darfur, and West Darfur states (Figure 1). However, the 2010 epidemic was the largest in magnitude and spread across five states (Figure 1).
Figure 1.
Geographical distribution of Crimean-Congo hemorrhagic fever (CCHF) epidemics in Sudan by years indicated by the colored shapes.
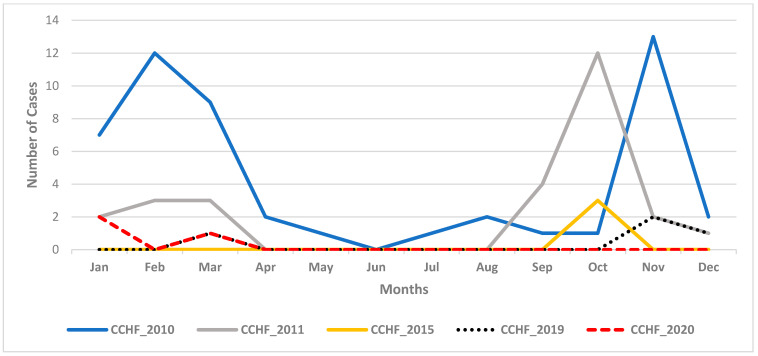
During these epidemics, 88 cases of CCHF in total were identified including 13 fatalities (Figure 2). Although cases were reported throughout the year during these epidemics, most cases clustered between September and January (Figure 2). Another large epidemic was reported in 2011 with 27 cases reported exclusively from the Kordofan region. Two major peaks developed during the two large epidemics in 2010 and 2011 between January and March, and September and November, while infections clustered within one transmission season during the other epidemics in 2015, 2019, and 2020 (Figure 2).
Figure 2.
Epicurve showing Crimean-Congo hemorrhagic fever (CCHF) cases per month during the five epidemics between 2010 and 2020.
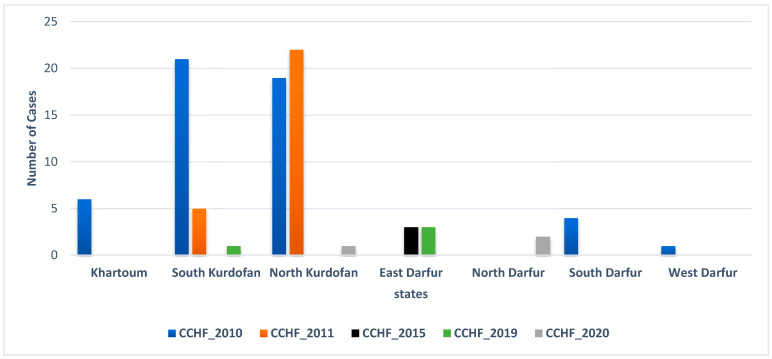
In the 2010 epidemic, 40 cases of CCHF and 11 related deaths were reported in Sudan, of which 78% were from the Kordofan region, namely North and South Kordofan States (Figure 3). Six (12%) and five (10%) cases were reported from Khartoum State and the Darfur region, respectively (Figure 3). Interestingly, in 2010, CCHFV infections were reported for the first time from the Darfur region (Figure 3). Compared to the 2010 outbreak, the 2011 outbreak was less severe in terms of the number and severity of cases and the limited geographical distribution in the Kordofan region (Figure 3), with a total of 27 cases including a single fatality. Of these, 22 cases (81%) were reported from North Kordofan State, and 5 cases (19%) were reported from South Kordofan State (Figure 3). Three cases were reported in 2015 from East Darfur State. In the 2019 and 2020 epidemics, four and three cases were reported, respectively, distributed between the Darfur and Kordofan regions (Figure 3).
Figure 3.
Number of Crimean-Congo hemorrhagic fever (CCHF) cases reported during each epidemic per state.
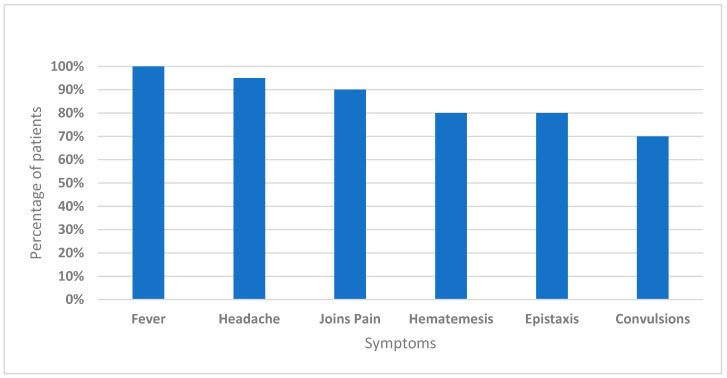
Cases presented with fever (100%), headache (95%), and joint pain (90%), as well as with hematemesis and epistaxis (80%). Around 70% of the patients showed the involvement of neurological syndrome (convulsions) (Figure 4).
Figure 4.
The clinical presentation of Crimean-Congo hemorrhagic fever (CCHF) cases.
Twelve deaths were reported in 2010, representing a 31% case fatality rate (CFR), while a single death was reported in 2011 (CRF 4%). The overall male to female ratio of patients was 2:1, and the average age of patients was 28 years old. Cases presented with fever and hemorrhage, and no other clinical symptoms were recorded.
4. Discussion
In this report, we describe epidemics of CCHF that occurred between 2010 and 2020 throughout Sudan. We update the known distribution of CCHF in the country by reporting recent emergence events of CCHFV in the conflict and humanitarian environment of the Darfur region, West Sudan (Figure 1). The severe clinical presentations that were exhibited by patients included fever, headache, and joint pain, as well as hematemesis, epistaxis, and neurological syndrome (Figure 4). Very high rates of CCHF infections are inapparent, indicating that the original investigations of these epidemics have only identified the severe cases [14,15,16]. The involvement of neurological syndromes among patients with CCHF suggests that the pathogenesis of the disease in humans is beyond just liver manifestation and include the nervous system [28,29].
Here, we show that the geographical distribution of the diseases in Sudan is rapidly expanding out of the original endemic region of Central Sudan [4]. This could be attributed to the increase in the risk factors that influence the transmission of arboviral infections including climate change and humanitarian crises [4,30]. The severe weather events during the recent years in Sudan, including droughts, heavy rainstorms, and flooding, may have contributed to the spread of CCHF by influencing the dynamics of human and animal populations in and out of CCHF-endemic areas, carrying the vector and/pathogen passively [9,30]. In particular, a study implemented among the one-humped camel population in Khartoum state, a non-endemic area for CCHF, revealed a high seroprevalence of CCHF-IgG (over 21%), which is very alarming [31]. This finding suggested the serious role of animal dynamics in spreading zoonotic diseases, including CCHF [31]. Similar scenarios were observed with Chikungunya, dengue, and Rift Valley fevers [3,8,9,11]. CCHF causes severe epidemics of viral hemorrhagic fever with a high fatality rate. A 31% CFR was reported during the 2010 epidemic, yet the disease is severely neglected by the local healthcare providers, researchers, and public health policymakers. This neglect is mainly due to the lack of awareness about the serious health threats imposed by the disease [4,14,15]. This lack of awareness is further underscored by the absence of an early warning surveillance and response system, an adequate health policy for disease prevention and control, and support for research to fill the gaps in our knowledge about the disease [4,14]. Additionally, this underestimation of the public health risk of CCHF in the country is further intensified by the limited reporting and data sharing culture among health authorities and lack of use of animals as mobile sentinel sites for early detection [13,32]. Therefore, the disease in Sudan commonly emerges in nosocomial outbreaks risking the lives of healthcare providers [33,34]. The case fatality rate in 2010 was 31%, typical of the documented rate, while it was relatively low in 2011 at 4% [14,15]. The mortality rate was relatively high in naïve areas such as South Darfur, with a 100% case fatality rate, and 50% in Khartoum, compared to the case mortality rate among cases from endemic areas of the Kordofan region (25%). This apparent reduction in cases per epidemic after 2011 could be attributed to the dysfunction of the health system in the endemic region of Kordofan due to the flair up of armed conflict in the area [35,36]. Moreover, armed conflict in the Darfur region, west Sudan, drastically changed the environment and the socioeconomic structure of the local communities, which, in turn, increased the vulnerability of poor communities with fragile healthcare to the emergence of infectious diseases including arboviral infections [7,8,9,10,30]. Our investigation reveals that CCHF emerged for the first time in the Darfur region in 2010. Apparently, the disease has established endemicity in the area with cases of CCHF reported from the region in 2016 during an epidemic of febrile illness [4,8].
One of the main challenges undermining our understanding of the disease’s transmission, burden, and epidemiology in Sudan is the limited diagnostic capacity and disease surveillance system throughout the country, with the very limited use of molecular and serological diagnostic tools in healthcare facilities [4,12,13]. Additionally, the limited resources in the country and the lack of support for research are challenging investigation attempts to generate evidence to inform and guide the health system [4]. Nonetheless, limited studies showed that at least two strains of CCHFV (Sudan Al-fulah 2018, and Sudan Abyei 2009) are circulating in Sudan and were involved in previous separate epidemics [33,37]. Recent studies about the emergence of the invasive Asian malaria vector Anopheles stephensi in the country have highlighted the importance of using molecular and genomics sequencing tools for the early detection and monitoring of the disease’s vector dynamics [38,39,40].
Exposure to tick bites, animals living in close proximity, and handling sick animals and their infected products are the major risk factors for getting infected with CCHFV [14,15,16]. This leaves poor individual and farming-dependent communities at higher risk of the disease. In particular, the inapparent infection of CCHF among cattle could help spread the disease further, not only through the vectors, but through direct contact with infected animal products, leaving butchers and slaughterhouse workers at higher risk unless strict food safety measures including testing animals for infection and proper infection control measures are implemented [41]. Healthcare providers in endemic areas and/or attending to CCHF patients during epidemics are at a similarly high risk [42]. Particularly in limited diagnostic settings where CCHFV infections are not robustly detected, infections among healthcare providers are fatal [17,25,26,34]. The common delay in the detection of zoonotic diseases has an extremely high accumulative societal cost on the endemic communities [23]. Moreover, other professionals with an occupational hazard of CCHF include agricultural workers, slaughterhouse workers, and veterinarians [15,16]. Therefore, the implementation of an early-preparedness strategy with a One Health approach is crucial for the prevention and control of CCHF epidemics [23,43]. Zoonotic diseases in general have devastating economic impacts. It was reported in 2012 that the annual cost of zoonotic and food-borne diseases is approximately USD 84 billion, 60% of which is due to the cost of human health, 30% is attributed to animal mortality, and 10% to lost productivity [44]. Arboviral diseases pose a severe socioeconomic burden, particularly on poor farm-depending communities, yet those of CCHF are understudied [6,22,37,38]. Therefore, social studies investigating the societal impacts of CCHF and its outbreaks are needed to quantify the cost-effectiveness of prevention and control measures. In particular, safe treatment and vaccines for CCHF are still underdeveloped, and the currently recommended prevention and control measures include avoiding exposure to ticks and the use of personal protective equipment when handling patients and sick animals, specifically in endemic areas [15,16].
The emergence and growing spread of CCHF into novel areas in Sudan seems to be associated with the recently reported changes in biology and expansion of the geographical distribution of tick vectors of CCHFV [45,46]. In addition to their roles as the main vector for transmitting CCHFV, virus circulation in endemic areas is mainly maintained through vertical transmission in tick populations, also known as transovarial transmission from mother ticks to the next generation [26]. Figure 2 clearly indicates the seasonality of CCHF epidemics throughout the years, with a remarkable increase in human cases between mid-September and late March (Figure 2), which corresponds to the rainy season when animals are sent out into the open pastures with their caretakers [11]. A relatively recent study has revealed that cattle pasturing on open grassland were at 27 times the risk of CCHF, compared to cattle in closed farms [47]. The rainy season might also correspond to the increase in the abundance, distribution, and exposure to tick vectors of CCHFV; however, there is a severe gap in data about the seasonality and change in vector populations. Further studies about the distribution, bionomics, dynamics, and vector composition of ticks in the CCHF endemic areas are warranted to generate evidence data that are essential for establishing an effective vector control strategy [48]. This indicates that unless serious action is taken to prevent and control the disease, the threat of CCHF for both public health and the economy will persistently grow, locally and regionally.
Although some antiviral drugs such as ribavirin are promising and vaccines are under development, the current lack of treatments and safe vaccines for preventing CCHF infections urges the need for a vector focused prevention health policy [15,16]. An integrated One Health policy that considers the health of humans, animals, the environment and their co-dependent interactions would reduce the threats of arboviral diseases including CCHF. Such a health policy should aim to increase the awareness of the communities at risk and promote the use of personal protection equipment and clothes to avoid contact with ticks. It must also implement vector control measures for tick populations; invest in improving diagnostic capacity and early warning and response systems; and train healthcare providers for humans and animals on personal safety and infection control during the treatment [23].
5. Conclusions
The global health threat of CCHF is rapidly growing worldwide, including in Sudan, without notice from the healthcare providers and public health policymakers. An early warning system and improvement of diagnostic capacity, particularly in endemic and epidemic-prone areas, is crucial for reducing the frequency and intensity of disease outbreaks and their morbidity and mortality. An effective health policy and integrated One Health strategy for the control and prevention of zoonotic diseases including CCHF needs to be established with multisectoral coordination between the Ministry of Health, the Ministry of Animal Resources, and the Environmental and Metrological authorities and their partners with transparent and timely data sharing. We recommend the establishment of a disease control program for the early detection, prevention, and control of arboviral diseases and hemorrhagic fevers including CCHF. In addition, the Ministry of Health must invest substantial effort and resources in vector surveillance and control throughout the county. Incorporating the use of advanced molecular and genomic sequencing techniques will provide crucial information on the dynamics of pathogens and their vectors, which, in turn, will inform policymakers and guide the national strategy for disease control.
Acknowledgments
We would like to thank all our colleagues at Sudan National Public Health Laboratory, Sudan Federal and States Ministries of Health for their administrative and technical support and help in the data collection.
Author Contributions
Conceptualization, design, formal analysis, and writing—original draft preparation, A.A.; investigation, A.A. and Y.A.; writing—review and editing, A.A., Y.A., B.S., I.D. and J.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and ethical approval was waived for this study because it analyzes secondary data from outbreaks reports without individuals’ identifiers.
Informed Consent Statement
Patient consent was waived because no individuals’ identifier was obtained during the data extraction from the anonymous epidemics’ reports.
Data Availability Statement
All data used in this study are included in the published paper.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
A.A. research is supported by R. Geigy-Stiftung and the Swiss Government Excellence Scholarships for Foreign Scholars and Artists that awarded by the Federal Commission for Scholarships for Foreign Students (FCS) (Personal ESKAS-Nr: 2021.0671). ID research is funded by Biotechnology and Biological Sciences Research Council BBS/E/I/00007033, BBS/E/I/00007036, BB/W01100X/1.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weaver S.C., Reisen W.K. Present and Future Arboviral Threats. Antivir. Res. 2010;85:328–345. doi: 10.1016/j.antiviral.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weaver S.C., Barrett A.D.T. Transmission Cycles, Host Range, Evolution and Emergence of Arboviral Disease. Nat. Rev. Microbiol. 2004;2:789–801. doi: 10.1038/nrmicro1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed A., Ali Y., Mohamed N.S. Arboviral Diseases: The Emergence of a Major yet Ignored Public Health Threat in Africa. Lancet Planet. Health. 2020;4:e555. doi: 10.1016/S2542-5196(20)30269-2. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed A., Dietrich I., LaBeaud A.D., Lindsay S.W., Musa A., Weaver S.C. Risks and Challenges of Arboviral Diseases in Sudan: The Urgent Need for Actions. Viruses. 2020;12:81. doi: 10.3390/v12010081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elduma A.H., LaBeaud A.D., Plante J.A., Plante K.S., Ahmed A. High Seroprevalence of Dengue Virus Infection in Sudan: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2020;5:120. doi: 10.3390/tropicalmed5030120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whiteman A., Loaiza J.R., Yee D.A., Poh K.C., Watkins A.S., Lucas K.J., Rapp T.J., Kline L., Ahmed A., Chen S., et al. Do Socioeconomic Factors Drive Aedes Mosquito Vectors and Their Arboviral Diseases? A Systematic Review of Dengue, Chikungunya, Yellow Fever, and Zika Virus. One Health. 2020;11:100188. doi: 10.1016/j.onehlt.2020.100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed A., Ali Y., Elmagboul B., Mohamed O., Elduma A., Bashab H., Mahamoud A., Khogali H., Elaagip A., Higazi T. Dengue Fever in the Darfur Area, Western Sudan. Emerg. Infect. Dis. 2019;25:2126. doi: 10.3201/eid2511.181766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed A., Elduma A., Magboul B., Higazi T., Ali Y. The First Outbreak of Dengue Fever in Greater Darfur, Western Sudan. Trop. Med. Infect. Dis. 2019;4:43. doi: 10.3390/tropicalmed4010043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed A., Ali Y., Elduma A., Eldigail M.H., Mhmoud R.A., Mohamed N.S., Ksiazek T.G., Dietrich I., Weaver S.C. Unique Outbreak of Rift Valley Fever in Sudan, 2019. Emerg. Infect. Dis. 2020;26:3030–3033. doi: 10.3201/eid2612.201599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed A., Eldigail M., Elduma A., Breima T., Dietrich I., Ali Y., Weaver S.C. First Report of Epidemic Dengue Fever and Malaria Co-Infections among Internally Displaced Persons in Humanitarian Camps of North Darfur, Sudan. Int. J. Infect. Dis. 2021;108:513–516. doi: 10.1016/j.ijid.2021.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahmed A., Mahmoud I., Eldigail M., Elhassan R.M., Weaver S.C. The Emergence of Rift Valley Fever in Gedaref State Urges the Need for a Cross-Border One Health Strategy and Enforcement of the International Health Regulations. Pathogens. 2021;10:885. doi: 10.3390/pathogens10070885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed A. Current Status of Mosquito-Borne Arboviruses in Sudan, and Challenges of Surveillance and Responses; Presented at the Mosquito-Borne Arboviruses: The Rising Global Threat, Malaria Consortium Webinar; online. 10 February 2021; [DOI] [Google Scholar]
- 13.Ahmed A. Urgent Call for a Global Enforcement of the Public Sharing of Health Emergencies Data: Lesson Learned from Serious Arboviral Disease Epidemics in Sudan. Int. Health. 2020;12:238–240. doi: 10.1093/inthealth/ihz122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sánchez-Seco M.P., Sierra M.J., Estrada-Peña A., Valcárcel F., Molina R., de Arellano E.R., Olmeda A.S., Miguel L.G.S., Jiménez M., Romero L.J., et al. Widespread Detection of Multiple Strains of Crimean-Congo Hemorrhagic Fever Virus in Ticks, Spain. Emerg. Infect. Dis. J. 2022;28:394. doi: 10.3201/eid2802.211308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The World Health Organization, (WHO) Crimean-Congo Haemorrhagic Fever. [(accessed on 8 January 2022)]. Available online: https://www.who.int/westernpacific/health-topics/crimean-congo-haemorrhagic-fever.
- 16.CDC Crimean-Congo Hemorrhagic Fever (CCHF) [(accessed on 9 January 2022)]; Available online: https://www.cdc.gov/vhf/crimean-congo/index.html.
- 17.Nasirian H. New Aspects about Crimean-Congo Hemorrhagic Fever (CCHF) Cases and Associated Fatality Trends: A Global Systematic Review and Meta-Analysis. Comp. Immunol. Microbiol. Infect. Dis. 2020;69:101429. doi: 10.1016/j.cimid.2020.101429. [DOI] [PubMed] [Google Scholar]
- 18.Pigott D.M., Deshpande A., Letourneau I., Morozoff C., Reiner R.C., Kraemer M.U.G., Brent S.E., Bogoch I.I., Khan K., Biehl M.H., et al. Local, National, and Regional Viral Haemorrhagic Fever Pandemic Potential in Africa: A Multistage Analysis. Lancet. 2017;390:2662–2672. doi: 10.1016/S0140-6736(17)32092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohamed N.S., Ali Y., Muneer M.S., Siddig E.E., Sibley C.H., Ahmed A. Malaria Epidemic in Humanitarian Crisis Settings the Case of South Kordofan State, Sudan. J. Infect. Dev. Ctries. 2021;15:168–171. doi: 10.3855/jidc.13122. [DOI] [PubMed] [Google Scholar]
- 20.Mohamed N.S., Osman H.A., Muneer M.S., Samy A.M., Ahmed A., Mohammed A.O., Siddig E.E., Abdel Hamid M.M., Ali M.S., Omer R.A., et al. Identifying Asymptomatic Leishmania Infections in Non-Endemic Villages in Gedaref State, Sudan. BMC Res. Notes. 2019;12:566. doi: 10.1186/s13104-019-4608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed A., Elbashir A., Mohamed A.A., Alim A.A., Mubarak A., Abdelrahman D., Mohammed E., Mohamed N.S., Elaagip A.H., Zarroug I.M.A., et al. Socioeconomic Impacts of Elimination of Onchocerciasis in Abu-Hamed Focus, Northern Sudan: Lessons after Elimination. BMC Res. Notes. 2020;13:256. doi: 10.1186/s13104-020-05101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mordecai E.A., Ryan S.J., Caldwell J.M., Shah M.M., LaBeaud A.D. Climate Change Could Shift Disease Burden from Malaria to Arboviruses in Africa. Lancet Planet. Health. 2020;4:e416–e423. doi: 10.1016/S2542-5196(20)30178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zinsstag J., Utzinger J., Probst-Hensch N., Shan L., Zhou X.-N. Towards Integrated Surveillance-Response Systems for the Prevention of Future Pandemics. Infect. Dis. Poverty. 2020;9:87–92. doi: 10.1186/s40249-020-00757-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.El-Azazy O.M.E., Scrimgeour E.M. Crimean-Congo Haemorrhagic Fever Virus Infection in the Western Province of Saudi Arabia. Trans. R. Soc. Trop. Med. Hyg. 1997;91:275–278. doi: 10.1016/S0035-9203(97)90072-9. [DOI] [PubMed] [Google Scholar]
- 25.Hassanein K.M., El-Azazy O.M. Isolation of Crimean-Congo Hemorrhagic Fever Virus from Ticks on Imported Sudanese Sheep in Saudi Arabia. Ann. Saudi Med. 2000;20:153–154. doi: 10.5144/0256-4947.2000.153. [DOI] [PubMed] [Google Scholar]
- 26.Hoogstraal H. The Epidemiology of Tick-Borne Crimean-Congo Hemorrhagic Fever in Asia, Europe, and Africa. J. Med. Entomol. 1979;15:307–417. doi: 10.1093/jmedent/15.4.307. [DOI] [PubMed] [Google Scholar]
- 27.Springer A., Shuaib Y.A., Isaa M.H., Ezz-Eldin M.I.-E., Osman A.Y., Yagoub I.A., Abdalla M.A., Bakiet A.O., Mohmed-Noor S.E.-T., Schaper S., et al. Tick Fauna and Associated Rickettsia, Theileria, and Babesia Spp. in Domestic Animals in Sudan (North Kordofan and Kassala States) Microorganisms. 2020;8:1969. doi: 10.3390/microorganisms8121969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garrison A.R., Smith D.R., Golden J.W. Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses. 2019;11:590. doi: 10.3390/v11070590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdelhakam H.A.A., Taha M.A. Crimean-Congo Hemorrhagic Fever (CCHF) in Southern Kordofan. Sudan. J. Paediatr. 2014;14:81–84. [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmed A., Mohamed N.S., Siddig E.E., Algaily T., Sulaiman S., Ali Y. The Impacts of Climate Change on Displaced Populations: A Call for Actions. J. Clim. Change Health. 2021;3:100057. doi: 10.1016/j.joclim.2021.100057. [DOI] [Google Scholar]
- 31.Suliman H.M., Adam I.A., Saeed S.I., Abdelaziz S.A., Haroun E.M., Aradaib I.E. Crimean Congo Hemorrhagic Fever among the One-Humped Camel (Camelus Dromedaries) in Central Sudan. Virol. J. 2017;14:147. doi: 10.1186/s12985-017-0816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuehnert P.A., Stefan C.P., Badger C.V., Ricks K.M. Crimean-Congo Hemorrhagic Fever Virus (CCHFV): A Silent but Widespread Threat. Curr. Trop. Med. Rep. 2021;8:141–147. doi: 10.1007/s40475-021-00235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aradaib I.E., Erickson B.R., Mustafa M.E., Khristova M.L., Saeed N.S., Elageb R.M., Nichol S.T. Nosocomial Outbreak of Crimean-Congo Hemorrhagic Fever, Sudan. Emerg. Infect. Dis. 2010;16:837–839. doi: 10.3201/eid1605.091815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elata A.T., Karsany M.S., Elageb R.M., Hussain M.A., Eltom K.H., Elbashir M.I., Aradaib I.E. A Nosocomial Transmission of Crimean-Congo Hemorrhagic Fever to an Attending Physician in North Kordufan, Sudan. Virol. J. 2011;8:303. doi: 10.1186/1743-422X-8-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gayer M., Legros D., Formenty P., Connolly M.A. Conflict and Emerging Infectious Diseases. Emerg. Infect. Dis. 2007;13:1625–1631. doi: 10.3201/eid1311.061093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olsson O. After Janjaweed? Socioeconomic Impacts of the Conflict in Darfur. World Bank Econ. Rev. 2010;24:386–411. doi: 10.1093/wber/lhq019. [DOI] [Google Scholar]
- 37.Aradaib I.E., Erickson B.R., Karsany M.S., Khristova M.L., Elageb R.M., Mohamed M.E.H., Nichol S.T. Multiple Crimean-Congo Hemorrhagic Fever Virus Strains Are Associated with Disease Outbreaks in Sudan, 2008–2009. PLOS Negl. Trop. Dis. 2011;5:e1159. doi: 10.1371/journal.pntd.0001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abubakr M., Sami H., Mahdi I., Altahir O., Abdelbagi H., Mohamed N.S., Ahmed A. The Phylodynamic and Spread of the Invasive Asian Malaria Vectors, Anopheles Stephensi, in Sudan. Biology. 2022;11:409. doi: 10.3390/biology11030409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed A., Pignatelli P., Elaagip A., Hamid M.M.A., Alrahman O.F., Weetman D. Invasive Malaria Vector Anopheles Stephensi Mosquitoes in Sudan, 2016–2018. EID. 2021;27:2952–2954. doi: 10.3201/eid2711.210040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmed A., Khogali R., Elnour M.-A.B., Nakao R., Salim B. Emergence of the Invasive Malaria Vector Anopheles Stephensi in Khartoum State, Central Sudan. Parasites Vectors. 2021;14:511. doi: 10.1186/s13071-021-05026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adam I.A., Mahmoud M.A., Aradaib I.E. A Seroepidemiological Survey of Crimean Congo Hemorrhagic Fever among Cattle in North Kordufan State, Sudan. Virol. J. 2013;10:178. doi: 10.1186/1743-422X-10-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ergönül Ö., Keske Ş., Çeldir M.G., Kara İ.A., Pshenichnaya N., Abuova G., Blumberg L., Gönen M. Systematic Review and Meta-Analysis of Postexposure Prophylaxis for Crimean-Congo Hemorrhagic Fever Virus among Healthcare Workers. Emerg. Infect. Dis. 2018;24:1642–1648. doi: 10.3201/eid2409.171709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zinsstag J., Schelling E., Crump L., Whittaker M., Tanner M., Stephen C. One Health: The Theory and Practice of Integrated Health Approaches. CABI; Oxfordshire, UK: 2020. [Google Scholar]
- 44.Grace D., Mutua F., Ochungo P., Kruska R., Jones K., Brierley L., Lapar L., Said M., Herrero M., Phuc P.M., et al. Mapping of Poverty and Likely Zoonoses Hotspots; Zoonoses Project 4, Report to the UK Department for International Development. ILRI; Nairobi, Kenya: 2012. [Google Scholar]
- 45.Mossaad E., Gaithuma A., Mohamed Y.O., Suganuma K., Umemiya-Shirafuji R., Ohari Y., Salim B., Liu M., Xuan X. Molecular Characterization of Ticks and Tick-Borne Pathogens in Cattle from Khartoum State and East Darfur State, Sudan. Pathogens. 2021;10:580. doi: 10.3390/pathogens10050580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shuaib Y.A., Elhag A.M.-A.W., Brima Y.A., Abdalla M.A., Bakiet A.O., Mohmed-Noor S.E.-T., Lemhöfer G., Bestehorn M., Poppert S., Schaper S., et al. Ixodid Tick Species and Two Tick-Borne Pathogens in Three Areas in the Sudan. Parasitol. Res. 2020;119:385–394. doi: 10.1007/s00436-019-06458-9. [DOI] [PubMed] [Google Scholar]
- 47.Ibrahim A.M., Adam I.A., Osman B.T., Aradaib I.E. Epidemiological Survey of Crimean Congo Hemorrhagic Fever Virus in Cattle in East Darfur State, Sudan. Ticks Tick-Borne Dis. 2015;6:439–444. doi: 10.1016/j.ttbdis.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 48.Ahmed A., Abubakr M., Ali Y., Siddig E.E., Mohamed N.S. Vector Control Strategy for Anopheles Stephensi in Africa. Lancet Microbe. 2022 doi: 10.1016/S2666-5247(22)00039-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this study are included in the published paper.