Abstract
Background: Vaccine hesitancy, as defined by the WHO, is the reluctance or refusal to vaccinate despite the availability of vaccines and is one of the ten threats to global health in 2019. Vaccine hesitancy remains a complex matter influenced by multiple factors, especially in sub-Saharan Africa. Methods: We conducted a cross-sectional study between November 2021 and January 2022 among the general adult public seeking care at six different healthcare facilities in Kenya. The survey, in English, consisted of questions based on demographics, knowledge, and attitudes, including hesitancy towards the COVID-19 vaccine. Results: Of the 3996 surveys collected, 55.1% were from private, 19.5% from faith-based and 25.3% from government facilities., Approximately 81.0% of all the participants reported it was important to get a vaccine to protect other people from COVID-19, 79.9% reported they would take a vaccine to protect against COVID-19, yet 40.5% reported being hesitant to take the vaccine primarily due to side effects. Most of the variables were associated with receiving a vaccine. Only 52.1% of those seeking care from the government facility and 54.5% of those seeking care from the faith-based facility were vaccinated, compared to 81.5% seeking care from the private facilities (p < 0.001). More participants from private facilities felt that vaccines are safe as compared to those at the faith-based and government facilities (p < 0.001). Conclusion: Vaccine hesitancy in Kenya, even though much lower than reported in other countries, remains a dynamic problem. Mitigating strategies specific to Africa need to be developed to help address vaccine hesitancy in this part of the continent.
Keywords: COVID-19, vaccine hesitancy, Kenya
1. Introduction
As of 2021, more than 8 million confirmed cases of COVID-19 were reported within the African continent, with more than 150,000 deaths, of which more than 320,000 cases and about 5500 deaths were in Kenya [1]. One of the greatest tools in combating COVID-19 morbidity and mortality is the COVID-19 vaccine. As of 2021, 9.17 billion doses of the COVID-19 vaccine had been administered worldwide, with 3.82 billion people fully vaccinated. Vaccination coverage is varied widely by income group, with average coverage of 58.49 doses/100 people, 17.30 doses/100 people, 11.95 doses/100 people, and 1.26 doses/100 people for high, upper middle, lower middle, and low income countries, respectively [2]. In Kenya specifically (as at February 2022), 16.6 million doses had been given and 7.58 million (14.1%) of the total population had been fully vaccinated. According to the United Nations website UN News: Global Perspective Human Stories, 832 million vaccine doses had been administered by April 2021 and 82% had gone to high and upper middle income countries, while only 0.2% had been delivered to low and middle income countries (LMICs) [3]. This inequality of healthcare resources, especially during a pandemic, certainly adds to the mistrust in healthcare systems and could promote vaccine hesitancy among people in LMICs [4]. Vaccine inequity remains a challenging issue around the world, especially in LMICs. Given the limited supply, vaccine hesitancy becomes a critical issue to mitigate to ensure the optimal uptake in low resource settings.
Various factors contribute to inequality in vaccine distribution, chief among which is supply and distribution of vaccines. High income countries (HICs), often the manufacturers and preferred customers of pharmaceutical firms, often hoard vaccines. Further, due to high costs of vaccines, LMICs often cannot afford them. However, with vaccination rates now slowing in high income countries, the cost of vaccines falling, and actions through global mechanisms such as COVAX, LMICs are now starting to see an increase in vaccine supply. To get these vaccines finally into the arms of those who need them, low income countries now have to focus on distribution: supply chains, personnel, and what we will discuss in this paper, patient level decision-making and vaccine hesitancy.
Vaccine hesitancy, as defined by the WHO, is the reluctance or refusal to vaccinate despite the availability of vaccines and is one of the ten threats to global health in 2019. Some of the reasons why people chose not to get vaccinated include a lack of trust in the healthcare system, complacency and inconvenience in getting the vaccine [5]. A framework to better understand the five psychological antecedents of vaccination called the 5C model includes: confidence, complacency, convenience, risk calculations, and collective responsibility. This framework, developed mainly in high income countries, harnesses the potential to better understand and come up with strategies to address vaccine hesitancy, but might miss factors that could be pertinent to LMICs. Large knowledge gaps around vaccine hesitancy still remain, especially in Africa, due to limited tools, especially those that have been validated in local or regional context [6,7].
Information on social media outlets is not scientifically filtered and has the potential to misguide. Early studies have already suggested that disinformation about the vaccine posted on various social media outlets appears to have significantly contributed to vaccine hesitancy and the lack of uptake. Wilson and Wiysonge in their study looking at social medial and vaccine hesitancy found that a rise in the number of negative tweets around vaccines related to foreign disinformation campaigns [8]. A number of conspiracy theories appear to have contributed, including one that claims the use of the vaccine is aimed to disable local populations so the “West” can control resources in Africa. Another conspiracy theory is based on the misinformation that vaccines contain microchips that are implanted to control the worlds’ population [9,10,11]. Lucia et al. (2021) found that 23% of US medical students were vaccine hesitant, due to fear of side effects and mistrust of the public health system [12]. Similarly, Salali and Uysal found that 31% of the participants in Turkey and 14% in the UK were not convinced about getting the COVID-19 vaccine, due to misinformation regarding the origin of COVID-19 [13]. Indeed, a major theme that emerged in the literature was misinformation, often stemming from social media, including misinformation on the origin of the virus, infertility, and efficacy of the vaccine [11].
While a vast majority of studies on COVID-19 vaccine decision-making and hesitancy are from HICs, there are a few studies from LMICs. Solis Arce et al. examined COVID-19 acceptance among 10 LMICs in Asia, Africa, and South America as well as Russia and the United States. They found higher willingness to get the COVID-19 vaccines in the LMICs samples as compared to Russia or the United States, but while the acceptance was primarily explained by the desire for personal protection from COVID-19, side effects of the vaccine remained a major reason for hesitancy [14]. Further, Anjorin et al. (2021) conducted a survey of 34 African countries, estimating that 63% were willing to receive the COVID-19 vaccine, 79% were concerned about side effects, and 39% were worried about COVID-19 infection after receiving the vaccine [15]. Similar results were found in studies in South Africa, Ethiopia, Egypt, Nigeria, and Somalia, with major factors of hesitancy being reported [16,17,18,19,20,21].
Kenya, a low–middle income country in sub-Saharan Africa (SSA), has a population of more than 50 million people, with 75% of this population living in rural areas and about 46% living below the poverty line. Kenya’s health budget for 2016–2017 was approximately KES 60.3 billion (4% of the total budget or 5.2% as a share of GDP, equaling USD $530 million). The majority of the healthcare spending goes towards curative therapy and only about 16% is spent on preventive actions such as vaccination, HIV/TB prevention, etc. [22,23]. There are several components to the Kenyan healthcare system; government, private, and faith-based. About half of the healthcare is provided in the public system in government-run facilities, whereas the other half is made up of private facilities, of which about 20% are faith-based organizations [24]. The Ministry of Health in Kenya is the primary supplier of vaccines. Initial policies related to vaccine distribution were based on the WHO Strategic Advisory Group of Experts (SAGE) Roadmap allowing healthcare workers who were at greater risk of infection and front-line workers to get access to the vaccine first [25]. The AstraZeneca vaccine was the first vaccine made available in Kenya in early 2021 and other approved vaccines reached the country later in 2021. Since that time, the vaccine supply has grown due to COVAX and doses are available to all Kenyans over the age of 15.
However, data on vaccine hesitancy in Africa is aging; at the time of writing, the most recent Kenyan study had taken place in August 2021 [26]. Given the rapidly changing landscape, updates of this information are needed. We conducted this study to better understand the reasons for vaccine hesitancy among the general population being treated at six different healthcare facilities in Kenya by government, private, and faith-based hospitals. We hope that this study will help inform vaccination promotion programs in Kenya and similar countries, as the COVID-19 vaccine supply increases.
2. Methodology
We carried out a cross-sectional study between November 2021 and January 2022. The general adult public (patients and relatives) visiting the inpatient and outpatient clinics were recruited from six different healthcare facilities: Aga Khan University Hospital, Nairobi (AKUHN), Penda Health (Nairobi), Avenue Hospital (Nairobi), Mediheal Hospital (Nairobi), Coast General Teaching and Referral Hospital (CGTRH) (Mombasa), and PCEA Chogoria Mission Hospital (Tharakanithi). Aga Khan University Hospital, Penda Health, Avenue Hospital, and Mediheal Hospital are all private hospitals. CGTRH is a government hospital, while PCEA Hospital is a not-for-profit faith-based organization.
The survey was in English and was strategically broken down into various sections including: demographics, medical history knowledge attitudes, and perspectives towards the COVID-19 pandemic and vaccination (Supplementary Materials). The survey used in this study was developed based on a literature review, questions used in other similar studies, and discussion with the research team of this study [27,28]. The survey was designed to reduce survey fatigue. To reduce potential bias of self-reported data, confidentiality of participants and privacy of their responses was prioritized. Data were collected both through online and paper-based surveys. Each site had an investigator that was responsible for administration of the survey. The site investigator, based on the resources available at the respective sites, decided to choose using either or both paper or online surveys. Each site investigator received preliminary training on administration of the survey. The survey was self-administered with the support of the site investigator. Online survey data were collected through the Research Electronic Data Capture (REDCap) platform (Vanderbilt and National Institute of Health) [29]. Online and written consent was obtained from all the participants. Approval for this study was obtained from the Institutional Ethics and Review Committee at the Aga Khan University, Nairobi, and the hospital leaderships at Penda Health, Avenue Hospital, Mediheal Hospital, Coast General Teaching and Referral Hospital, and PCEA Chogoria Mission Hospital. Participants were allowed to withdraw from the study at any time without any consequences.
Sociodemographic characteristics collected were age, gender, marital status, education, employment status, citizenship, and race. Additionally, participants were asked about their medical history and any comorbidities. COVID-19 related questions included if participants were infected with COVID-19 or knew anyone who was infected, if they had contracted the virus with or without a test and concerns or worries about the COVID-19 pandemic. The section on attitudes and perspectives towards COVID-19 vaccines consisted of questions about hesitancy and concerns, scored using a Likert scale (strongly agree, agree, neutral, disagree, and strongly disagree). The details of the full set of questions are in the Supplementary Materials.
Continuous data were analyzed using medians and interquartile ranges (IQRs) whereas categorical data were analyzed as frequencies and percentages. The non-parametric Kruskal–Wallis test was used to compare the continuous variables and Fisher’s exact test was used to compare the categorical variables between group associations. Logistic regression was also employed to identify associations and odds ratio and 95% CI was presented. Data analysis was performed using SPSS statistical software V. 20.0 (IBM, Armonk, NY, USA). The significance level was set at α = 0.05, and all tests were two-tailed.
3. Results
3.1. Demographics
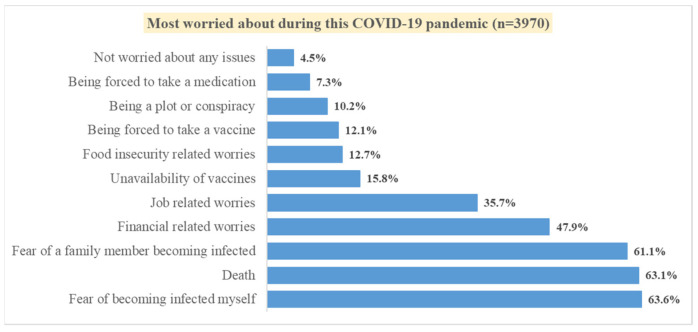
A total of 3996 surveys were completed and included in the analysis. The median age of participants was 33.0 years (IQR: 26.5, 43.0) with 55.8% being females. More than half of the participants (56.9%) were married and about 41.5% had an undergraduate or postgraduate degree. A majority of the participants were Kenyan (97.5%) and about 69.0% were employed or self-employed. About 71.0% reported having no medical conditions whereas 8.7% reported having hypertension, 7.8% having diabetes, and 2.7% having high cholesterol. About 12.2% of the respondents reported that they had tested positive for COVID-19. However, about 43.7% reported that they might have been exposed to or infected with COVID-19 without testing. More than half of our study population reported fear of becoming infected (63.6%), fear of death from the infection (63.1%), and fear of a family member becoming infected (61.1%). From the responses, 3.8% mentioned all three worries (food insecurity/job related worries/financial related worries), whereas 26.9% mentioned any two worries (food insecurity/job related worries/financial related worries. Figure 1 details what our study population most worried about during the COVID-19 pandemic. Detailed demographics are presented in Table 1.
Figure 1.
Proportions of the issues respondents worried about most during the COVID-19 pandemic.
Table 1.
Demographic details of the study participants (n = 3996).
| Variable | n | % | |
|---|---|---|---|
| Study Site | Aga Khan University, Nairobi | 925 | 23.1% |
| Penda Health | 345 | 8.6% | |
| Avenue Hospital | 517 | 12.9% | |
| Mediheal Hospital | 417 | 10.4% | |
| Coast General Hospital | 1012 | 25.3% | |
| PCEA Hospital | 780 | 19.5% | |
| Age (years) (n = 3624) | Median [IQR] | 33.0 [26.5, 43.0] | |
| 18–25 years | 767 | 21.2% | |
| 26–35 years | 1322 | 36.5% | |
| >35 years | 1535 | 42.4% | |
| Gender (n = 3979) | Male | 1759 | 44.2% |
| Female | 2220 | 55.8% | |
| Marital Status (n = 3947) | Single | 1509 | 38.2% |
| Married | 2245 | 56.9% | |
| Other | 193 | 4.9% | |
| Education (n = 3947) | None/School Education | 1051 | 26.6% |
| Diploma | 1258 | 31.9% | |
| Undergraduate/Postgraduate | 1638 | 41.5% | |
| Employment (n = 3953) | Employed/Self Employed | 2726 | 69.0% |
| Unemployed | 1117 | 28.3% | |
| Retired | 110 | 2.8% | |
| Nationality (n = 3975) | Kenyan | 3874 | 97.5% |
| Non-Kenyan | 101 | 2.5% | |
| Race (n = 3959) | African | 3843 | 97.1% |
| Other | 116 | 2.9% | |
| Asian | 79 | 2.0% | |
| Other | 12 | 0.3% | |
| Medical Conditions | Diabetes | 312 | 7.8% |
| Hypertension | 346 | 8.7% | |
| Heart Disease | 81 | 2.0% | |
| High Cholesterol | 107 | 2.7% | |
| Stroke | 20 | 0.5% | |
| HIV | 171 | 4.3% | |
| Cancer | 41 | 1.0% | |
| Other | 267 | 6.7% | |
| None | 2837 | 71.0% | |
| Previously tested positive for COVID-19 (n = 3981) | Myself | 487 | 12.2% |
| Family Member | 905 | 22.7% | |
| Friend | 878 | 22.1% | |
| Colleague | 790 | 19.8% | |
| My Neighbor | 504 | 12.7% | |
| No One | 1427 | 35.8% | |
| Exposed to or infected with COVID-19 (without testing) (n = 3932) | Yes | 1720 | 43.7% |
| No | 2212 | 56.3% | |
3.2. Attitudes and Perspectives toward COVID-19 Vaccines
In this study, 81.0% of the participants strongly agreed/agreed that it was important to get a vaccine to protect other people from COVID-19. Furthermore, about 61.6% of the participants agreed that pharmaceutical companies will be able to develop safe and effective COVID-19 vaccines and only 30.0% believed COVID-19 vaccines made in Europe or America were safer than those made in other countries. A majority of the participants (79.9%) reported they would take a vaccine to protect against COVID-19 yet 40.5% reported being hesitant to take the vaccine due to side effects from the vaccine. Recommending family and friends and getting children vaccinated against COVID-19 vaccine was reported at 77.6% and 65.4%, respectively.
More than half of the participants (65.1%) agreed that the COVID-19 vaccine was rapidly developed and approved and about 25.5% of the participants agreed the vaccines were faulty or fake. More than one-third of the participants (37.6%) agreed the vaccine might cause medical complications in the future and 26.8% stated they felt the vaccine was being promoted for commercial gain. Table 2 depicts the attitudes and perceptions towards the COVID-19 vaccine.
Table 2.
Attitudes and perceptions towards COVID-19 vaccine.
| Strongly Agree/Agree | Neutral | Strongly Disagree/Disagree | |
|---|---|---|---|
| It is important to get a vaccine to protect people from COVID-19. (n = 3966) | 3212 (81.0%) | 513 (12.9%) | 241 (6.1%) |
| Pharmaceutical companies are going to develop safe and effective COVID-19 vaccines? (n = 3891) | 2395 (61.6%) | 1111 (28.6%) | 385 (9.9%) |
| COVID-19 vaccines made in Europe or America are safer than those made in other countries. (n = 3853) | 1155 (30.0%) | 1318 (34.2%) | 1380 (35.8%) |
| I would take a vaccine to protect against COVID-19. (n = 3953) | 3159 (79.9%) | 425 (10.8%) | 369 (9.3%) |
| I am hesitant to take the vaccine due to side effects from the vaccine. (n = 3905) | 1580 (40.5%) | 581 (14.9%) | 1744 (44.7%) |
| I will recommend my family and friends to get vaccinated against the COVID-19 vaccine? (n = 3954) | 3070 (77.6%) | 521 (13.2%) | 363 (9.2%) |
| I will get my children vaccinated against COVID-19? (n = 3704) | 2421 (65.4%) | 658 (17.8%) | 625 (16.9%) |
| COVID-19 vaccine maybe faulty or fake. (n = 3942) | 1005 (25.5%) | 1304 (32.6%) | 1633 (41.4%) |
| COVID-19 vaccine was rapidly developed and approved. (n = 3917) | 2550 (65.1%) | 912 (23.3%) | 455 (11.6%) |
| COVID-19 vaccine might cause some medical complications in the future. (n = 3921) | 1474 (37.6%) | 1551 (39.6%) | 896 (22.9%) |
| COVID-19 vaccine is being promoted for commercial gain. (n = 3906) | 1046 (26.8%) | 1318 (33.7%) | 1542 (39.5%) |
| The government should make the vaccine available for all citizens for free. (n = 3931) | 3408 (86.7%) | 342 (8.7%) | 181 (4.6%) |
3.3. Vaccination Status Differences
Approximately 68.8% of the participants reported being vaccinated with at least one dose. From those that had received the vaccine, 72.0% received two doses, 25.7% received one dose, and 2.3% had received the additional booster dose. More than half (61.9%) reported getting the AstraZeneca vaccine (first vaccine available in Kenya). Variables that were investigated as potential associated variables of receiving COVID-19 vaccines were: age, gender, marital status, education, employment, stating that vaccines are safe, COVID-19 exposure, and questions regarding attitudes and perceptions regarding COVID-19 vaccines. Most of the variables were associated with receiving a vaccine. Older age participants were more likely to receive a vaccine and in addition, unemployed participants and those with no or only school education were less likely to have received the COVID-19 vaccine as compared to employed participants and those with undergraduate or postgraduate education. Furthermore, participants who believed that general vaccines are safe, in the importance of getting a vaccination against COVID-19, and that pharmaceutical companies develop safe and effective vaccines were more likely to have received a vaccine. In contrast, participants who believed COVID-19 vaccines may be faulty or fake, might cause some medical complications in the future, and that vaccines are being promoted for commercial gain were less likely to have received the vaccine. Details of the results from the logistic regression are presented in Table 3.
Table 3.
Association of factors among those vaccinated.
| Factors | Odds Ratio | 95% CI | p Value | |
|---|---|---|---|---|
| Age (years) | 1.029 | 1.023–1.036 | <0.001 | |
| Gender (Ref: Female) | Male | 1.044 | 0.912–1.195 | 0.53 |
| Marital Status (Ref: Single) |
Married | 1.443 | 1.256–1.658 | <0.001 |
| Others | 2.721 | 1.852–3.998 | <0.001 | |
| Education (Ref: Undergraduate/Postgraduate) | None-Primary | 0.422 | 0.358–0.498 | <0.001 |
| Diploma | 0.833 | 0.706–0.983 | 0.030 | |
| Employment (Ref: Employed/Self-employed) |
Unemployed | 0.293 | 0.253–0.340 | <0.001 |
| Retired | 0.779 | 0.509–1.191 | 0.25 | |
| In general, vaccines are safe (Ref: Neutral) |
Agree | 2.994 | 2.507–3.576 | <0.001 |
| Disagree | 0.395 | 0.284–0.549 | <0.001 | |
| Previously tested positive for COVID-19 (Ref: No) |
Self | 2.458 | 1.919–3.148 | <0.001 |
| No One | 0.415 | 0.361–0.476 | <0.001 | |
| Infected with COVID-19 (without testing) (Ref: No) | Yes | 2.223 | 1.927–2.564 | <0.001 |
| Important to get a vaccine to protect people from COVID-19 (Ref: Neutral). | Agree | 8.051 | 6.560–9.789 | <0.001 |
| Disagree | 0.530 | 0.366–0.766 | 0.001 | |
| Pharmaceutical companies are going to develop safe and effective COVID-19 vaccines (Ref: Neutral). | Agree | 2.295 | 1.968–2.676 | <0.001 |
| Disagree | 0.401 | 0.316–0.509 | <0.001 | |
| COVID-19 vaccines made in Europe or America are safer than those made in other countries (Ref: Neutral). | Agree | 1.118 | 0.940–1.329 | 0.21 |
| Disagree | 0.827 | 0.704–0.971 | 0.021 | |
| I am hesitant to take the vaccine due to side effects from the vaccine (Ref: Neutral). | Agree | 0.589 | 0.485–0.716 | <0.001 |
| Disagree | 3.680 | 2.962–4.574 | <0.001 | |
| I will recommend my family and friends to get vaccinated (Ref: Neutral). | Agree | 7.701 | 6.298–9.417 | <0.001 |
| Disagree | 0.449 | 0.327–0.616 | <0.001 | |
| I will get my children vaccinated (Ref: Neutral). |
Agree | 3.223 | 2.681–3.874 | <0.001 |
| Disagree | 0.372 | 0.296–0.467 | <0.001 | |
| COVID-19 vaccines may be faulty or fake (Ref: Neutral), | Agree | 0.417 | 0.352–0.495 | <0.001 |
| Disagree | 2.266 | 1.906–2.694 | <0.001 | |
| COVID-19 vaccine was rapidly developed and approved (Ref: Neutral), | Agree | 1.276 | 1.086–1.499 | 0.003 |
| Disagree | 0.885 | 0.700–1.118 | 0.30 | |
| COVID-19 vaccines might cause some medical complications in the future (Ref: Neutral) | Agree | 0.341 | 0.292–0.399 | <0.001 |
| Disagree | 1.442 | 1.172–1.774 | 0.001 | |
| The COVID-19 vaccine is being promoted for commercial gain (Ref: Neutral), | Agree | 0.490 | 0.414–0.579 | <0.001 |
| Disagree | 2.018 | 1.698–2.397 | <0.001 | |
3.4. Institution Differences
We looked at differences among sociodemographic characteristics, COVID-19 related questions, and attitudes and perspectives towards COVID-19 vaccines. The institutional comparison was divided into “Private” (Aga Khan University Hospital, Avenue Hospital, Mediheal Hospital, and Penda Health), “Faith-Based” (PCEA Chogoria Hospital) and “Government” (Coast General Teaching and Referral Hospital). The distribution of participants from the three groups was 55.1% from private, 19.5% from faith-based, and 25.3% from government facilities. Most of the sociodemographic characteristics were associated with the type of institution. From the private institutions, 59.0% were married, 51.0% had an undergraduate or postgraduate education, and 81.2% reported being employed, which was higher compared to those at the faith-based and government institutions. Only about half of the participants from the government and faith-based facilities, 52.1% and 54.5%, respectively, were vaccinated, whereas 81.5% from the private facilities reported being vaccinated (p < 0.001). More participants from private facilities felt that general vaccines are safe compared to those at the faith-based and government facilities, which was statistically significant (p < 0.001). From the faith-based facility, 42.5% agreed on COVID-19 vaccines being faulty or fake, whereas of those at the government facility and the private institutions, 29.3% and 17.7%, respectively, of respondents agreed that the COVID-19 vaccine was faulty or fake (p < 0.001). About one-third of the participants (35.7%) from the government facility agreed that the COVID-19 vaccine might cause some medical complications in the future whereas about 60.6% from the faith-based facility reported the same. Details of the univariate analysis associations are presented in Table 4.
Table 4.
Differences among institutions.
| Institution | p Value | |||||||
|---|---|---|---|---|---|---|---|---|
| Private (n = 2204) | Faith Based (n = 780) | Govt (n = 1012) | ||||||
| Age (years) (n = 3624) (median [IQR]) | 34.0 [28.0, 45.0] | 30.0 [23.0, 41.0] | 33.0 [26.0, 41.0] | <0.001 | ||||
| Gender (n = 3979) | Male | 991 | 45.2% | 319 | 40.9% | 449 | 44.5% | 0.109 |
| Female | 1200 | 54.8% | 461 | 59.1% | 559 | 55.5% | ||
| Marital Status (n = 3947) | Single | 796 | 36.7% | 368 | 47.4% | 345 | 34.4% | <0.001 |
| Married | 1280 | 59.0% | 388 | 50.0% | 577 | 57.6% | ||
| Others | 93 | 4.3% | 20 | 2.6% | 80 | 8.0% | ||
| Education (n = 3947) | None/School Education | 337 | 15.5% | 187 | 24.0% | 527 | 52.7% | <0.001 |
| Diploma | 726 | 33.5% | 334 | 42.9% | 198 | 19.8% | ||
| Undergraduate/Postgraduate | 1105 | 51.0% | 258 | 33.1% | 275 | 27.5% | ||
| Employment (n = 3953) | Employed/Self Employed | 1763 | 81.2% | 341 | 43.8% | 622 | 61.9% | <0.001 |
| Unemployed | 332 | 15.3% | 431 | 55.4% | 354 | 35.2% | ||
| Retired | 75 | 3.5% | 6 | 0.8% | 29 | 2.9% | ||
| Nationality (n = 3975) | Kenyan | 2098 | 95.9% | 775 | 99.6% | 1001 | 99.2% | <0.001 |
| Non-Kenyan | 90 | 4.1% | 3 | 0.4% | 8 | 0.8% | ||
| Race (n = 3959) | African | 2088 | 95.7% | 778 | 99.9% | 977 | 97.9% | <0.001 |
| Others | 94 | 4.3% | 1 | 0.1% | 21 | 2.1% | ||
| Medical Conditions | None | 1492 | 67.7% | 578 | 74.1% | 767 | 75.8% | <0.001 |
| Medical Conditions | Diabetes | 156 | 7.1% | 79 | 10.1% | 77 | 7.6% | 0.023 |
| Hypertension | 203 | 9.2% | 75 | 9.6% | 68 | 6.7% | 0.038 | |
| Heart Disease | 28 | 1.3% | 26 | 3.3% | 27 | 2.7% | 0.01 | |
| High Cholesterol | 66 | 3.0% | 12 | 1.5% | 29 | 2.9% | 0.088 | |
| Stroke | 15 | 0.7% | 3 | 0.4% | 2 | 0.2% | 0.173 | |
| HIV | 125 | 5.7% | 31 | 4.0% | 15 | 1.5% | <0.001 | |
| Cancer | 11 | 0.5% | 12 | 1.5% | 18 | 1.8% | 0.001 | |
| In general, vaccines are safe (n = 3978). | Agree | 1778 | 81.2% | 641 | 82.5% | 719 | 71.2% | <0.001 |
| Neutral | 348 | 15.9% | 92 | 11.8% | 176 | 17.4% | ||
| Disagree | 65 | 3.0% | 44 | 5.7% | 115 | 11.4% | ||
| Previously tested positive for COVID-19. | Myself | 332 | 15.1% | 82 | 10.5% | 73 | 7.2% | <0.001 |
| No One | 626 | 28.4% | 351 | 45.0% | 450 | 44.5% | <0.001 | |
| Exposed to or infected with COVID-19 (without testing) (n = 3932). | Yes | 1120 | 51.8% | 375 | 48.6% | 225 | 22.6% | <0.001 |
| No | 1044 | 48.2% | 397 | 51.4% | 771 | 77.4% | ||
| Most worried about during the COVID-19 pandemic. | Fear of becoming infected myself | 1349 | 61.2% | 501 | 64.2% | 674 | 66.6% | 0.010 |
| Fear of a family member becoming infected | 1304 | 59.2% | 503 | 64.5% | 619 | 61.2% | 0.031 | |
| Death | 1378 | 62.5% | 572 | 73.3% | 556 | 54.9% | <0.001 | |
| Financial-related worries | 957 | 43.4% | 358 | 45.9% | 588 | 58.1% | <0.001 | |
| Job-related worries | 656 | 29.8% | 187 | 24.0% | 574 | 56.7% | <0.001 | |
| Food insecurity-related worries | 233 | 10.6% | 55 | 7.1% | 218 | 21.5% | <0.001 | |
| Unavailability of vaccines | 387 | 17.6% | 63 | 8.1% | 177 | 17.5% | <0.001 | |
| Being a plot or conspiracy | 203 | 9.2% | 65 | 8.3% | 137 | 13.5% | <0.001 | |
| Being forced to take a medication | 134 | 6.1% | 64 | 8.2% | 90 | 8.9% | 0.008 | |
| Being forced to take a vaccine | 257 | 11.7% | 85 | 10.9% | 137 | 13.5% | 0.182 | |
| Not worried about any issues | 89 | 4.0% | 60 | 7.7% | 30 | 3.0% | <0.001 | |
| Received the COVID-19 vaccine? | Yes | 1796 | 81.5% | 425 | 54.5% | 527 | 52.1% | <0.001 |
| No | 408 | 18.5% | 355 | 45.5% | 485 | 47.9% | ||
| How many doses of the vaccine did you receive? | One | 385 | 21.4% | 138 | 32.5% | 183 | 34.7% | <0.001 |
| Two | 1352 | 75.3% | 287 | 67.5% | 340 | 64.5% | ||
| Three | 59 | 3.3% | 0 | 0.0% | 4 | 0.8% | ||
| Do you think it is important to get a vaccine to protect people from COVID-19? | Agree | 1879 | 85.9% | 617 | 79.1% | 716 | 71.7% | <0.001 |
| Neutral | 231 | 10.6% | 109 | 14.0% | 173 | 17.3% | ||
| Disagree | 77 | 3.5% | 54 | 6.9% | 110 | 11.0% | ||
| Pharmaceutical companies are going to develop safe and effective COVID-19 vaccines? | Agree | 1435 | 67.6% | 407 | 52.4% | 553 | 55.7% | <0.001 |
| Neutral | 572 | 27.0% | 295 | 38.0% | 244 | 24.6% | ||
| Disagree | 115 | 5.4% | 75 | 9.7% | 195 | 19.7% | ||
| COVID-19 vaccines made in Europe or America are safer than those made in other countries? | Agree | 550 | 26.3% | 184 | 24.2% | 421 | 41.9% | <0.001 |
| Neutral | 857 | 41.0% | 274 | 36.1% | 187 | 18.6% | ||
| Disagree | 681 | 32.6% | 302 | 39.7% | 397 | 39.5% | ||
| Which of the following COVID-19 vaccines would you prefer to use in the future? | Some Vaccine | 1855 | 86.6% | 624 | 80.1% | 598 | 59.8% | <0.001 |
| None | 287 | 13.4% | 155 | 19.9% | 402 | 40.2% | ||
| I would take a vaccine to protect against COVID-19. | Agree | 1852 | 85.1% | 595 | 76.3% | 712 | 71.4% | <0.001 |
| Neutral | 205 | 9.4% | 90 | 11.5% | 130 | 13.0% | ||
| Disagree | 119 | 5.5% | 95 | 12.2% | 155 | 15.5% | ||
| I am hesitant to take the vaccine due to side effects from the vaccine. | Agree | 626 | 29.4% | 555 | 71.2% | 399 | 40.1% | <0.001 |
| Neutral | 332 | 15.6% | 81 | 10.4% | 168 | 16.9% | ||
| Disagree | 1172 | 55.0% | 144 | 18.5% | 428 | 43.0% | ||
| I will recommend my family and friends to get vaccinated against the COVID-19 vaccine? | Agree | 1821 | 83.5% | 591 | 76.2% | 658 | 66.1% | <0.001 |
| Neutral | 263 | 12.1% | 124 | 16.0% | 134 | 13.5% | ||
| Disagree | 98 | 4.5% | 61 | 7.9% | 204 | 20.5% | ||
| I will get my children vaccinated against the COVID-19 vaccine? | Agree | 1346 | 69.7% | 486 | 62.4% | 589 | 59.3% | <0.001 |
| Neutral | 373 | 19.3% | 161 | 20.7% | 124 | 12.5% | ||
| Disagree | 212 | 11.0% | 132 | 16.9% | 281 | 28.3% | ||
| COVID-19 vaccine maybe faulty or fake. | Agree | 383 | 17.7% | 330 | 42.4% | 292 | 29.3% | <0.001 |
| Neutral | 696 | 32.1% | 302 | 38.8% | 306 | 30.7% | ||
| Disagree | 1087 | 50.2% | 146 | 18.8% | 400 | 40.1% | ||
| COVID-19 vaccine was rapidly developed and approved. | Agree | 1389 | 64.7% | 636 | 81.5% | 525 | 53.1% | <0.001 |
| Neutral | 533 | 24.8% | 107 | 13.7% | 272 | 27.5% | ||
| Disagree | 226 | 10.5% | 37 | 4.7% | 192 | 19.4% | ||
| COVID-19 vaccine might cause some medical complications in the future. | Agree | 651 | 30.2% | 472 | 60.6% | 351 | 35.7% | <0.001 |
| Neutral | 994 | 46.1% | 223 | 28.6% | 334 | 33.9% | ||
| Disagree | 513 | 23.8% | 84 | 10.8% | 299 | 30.4% | ||
| COVID-19 vaccine is being promoted for commercial gain. | Agree | 450 | 21.0% | 332 | 42.7% | 264 | 26.8% | <0.001 |
| Neutral | 703 | 32.8% | 279 | 35.9% | 336 | 34.1% | ||
| Disagree | 991 | 46.2% | 167 | 21.5% | 384 | 39.0% | ||
| The government should make the vaccine available for all citizens for free? | Agree | 1931 | 89.5% | 727 | 93.2% | 750 | 75.5% | <0.001 |
| Neutral | 173 | 8.0% | 44 | 5.6% | 125 | 12.6% | ||
| Disagree | 54 | 2.5% | 9 | 1.2% | 118 | 11.9% | ||
| Would you be willing to pay for a COVID-19 vaccine privately? | Yes | 375 | 17.4% | 97 | 12.5% | 66 | 6.7% | <0.001 |
| No | 1318 | 61.3% | 594 | 76.4% | 755 | 76.1% | ||
| Not sure | 458 | 21.3% | 86 | 11.1% | 171 | 17.2% | ||
| Who do you trust the most for information about vaccines?) | Media (TV, radio, newspaper, etc.) | 240 | 10.9% | 304 | 39.0% | 244 | 24.1% | <0.001 |
| Internet | 150 | 6.8% | 128 | 16.4% | 77 | 7.6% | <0.001 | |
| Social media (Facebook, Twitter, etc.) | 90 | 4.1% | 100 | 12.8% | 102 | 10.1% | <0.001 | |
| Healthcare providers | 1301 | 59.0% | 349 | 44.7% | 254 | 25.1% | <0.001 | |
| Family members | 94 | 4.3% | 42 | 5.4% | 75 | 7.4% | 0.001 | |
| Government | 379 | 17.2% | 81 | 10.4% | 138 | 13.6% | <0.001 | |
| Pharmaceutical company reports | 237 | 10.8% | 60 | 7.7% | 21 | 2.1% | <0.001 | |
| Scientific articles | 445 | 20.2% | 86 | 11.0% | 73 | 7.2% | <0.001 | |
| I do not trust any source | 208 | 9.4% | 60 | 7.7% | 94 | 9.3% | 0.330 | |
4. Discussion
Vaccine decision-making remains a complex matter defined by social, political, geographical, and cultural factors. It remains a major obstacle in the optimal administration of vaccines to populations in LMICs. Vaccine hesitancy has been inadequately studied in Africa and especially in Kenya, hampering efforts to mitigate these challenges. We chose to further explore the vaccine hesitancy among patients visiting six healthcare facilities in Kenya to add to the scarce data on vaccine hesitancy from sub-Saharan Africa.
Our study showed about 40.5% of the respondents were hesitant to take the vaccine, 81% felt that it was important to be vaccinated against COVID-19, and 77% stated that they would recommend the vaccine to family members and friends. Studies in SSA vary with some studies showing similar numbers while others in Cameroon and the DRC reporting much higher rates of vaccine hesitancy [14,30,31,32]. Media, trust in pharmaceutical companies, lack of information about the vaccines, as well as cost, play a key role in vaccine hesitancy in countries with a higher vaccine hesitancy rate. Approximately 63% of our study population received both dose of primarily the AstraZeneca vaccine. This was the first vaccine made available in Kenya in early 2021 through COVAX—a partnership between CEPI, Gavi, UNICEF, and the WHO [33]. Other approved vaccines reached the country later in 2021.
The depth of vaccine acceptance in our population is reflected in that 65% were agreeable to vaccinate their children against COVID-19. Carcelen and colleagues also found a high acceptability of COVID-19 vaccinations for children brought in by parents for other routine vaccines in Zambia [34]. Concerns about the vaccine ranged from a relative preference for vaccines developed in the West to those based on conspiracy theories; 30% of our study population felt that vaccines developed in the West were of better quality, while 65% felt that the vaccine was rapidly developed and approved for use. In comparison, 28.5% in a study done in Egypt also reported they preferred vaccines from the United States [35]. This appears to reflect mistrust in the local healthcare systems as well as misinformation about research and safety of vaccines used specifically in Africa [36,37,38].
Approximately 25% of the study population felt that the COVID-19 vaccine was either faulty or fake. Similar findings from Zambia and the UK have been reported by other authors raising concerns about vaccine safety and effectiveness [34,39,40]. Conspiracy theories, such as Africans being experimental subjects for Western vaccines, can greatly affect the public’s views on vaccine safety and effectiveness [8,10,30,41]. Almost 47% of the population of Kenya believe that people in Africa are being used as test subjects for vaccine trials, whereas 88% had seen articles stating that the COVID-19 virus had been spread by China, and 71% had forwarded or shared this information with families and friends [42].
The COVID-19 vaccines are being promoted for commercial gain, 27% of our study population felt, similar to findings of other studies. Prior studies have documented a similar mistrust in the intentions of the pharmaceutical industries in Africa, and that they are prioritizing financial gains over public welfare [30]. A majority of our study population also felt that the vaccines should be provided at no cost to the public even though currently the country is providing them for free. It was reported by other studies as well that, specifically in Africa, the cost of the vaccine may be associated with non-acceptance of the vaccine [15,30,43].
It was clear from our study that our respondents’ risk perception was related to their attitude about that vaccine. Similar to other studies, our study showed that higher levels of education and increasing age were associated with getting a COVID-19 vaccine [44,45,46,47]. This is contrary to what the Africa CDC found in its study reporting that people with primary level education and less were more likely to show confidence in the importance and safety of the vaccine, but they also reported that older people were more likely to get the COVID-19 vaccine; 20% of Kenyans aged 18–24 were not willing to take the vaccine versus 7% over the age of 55 [42]. The difference could be partially attributed to the sample size and location of study and certainly deserves further analysis. Participants in our study who believed the COVID-19 vaccine maybe faulty or fake were less likely to have received the vaccine. Our findings were substantiated by the CDC Africa report showing similar findings [42].
Our study, to the best of our knowledge, is the first study to compare vaccine hesitancy among the different types of healthcare institutions in Kenya. Further analysis looked specifically at attitudes and perceptions of the COVID-19 vaccine comparing government facilities to private and faith-based health institutions.
A significant number of participants at the faith-based hospital (42%) felt that the COVID-19 vaccine was fake or faulty. This was in comparison to 29% and 17% at the government and private hospitals, respectively. Similarly, a majority of the participants (82%) at the faith-based hospital felt that the COVID-19 vaccine was rapidly developed and approved compared to 53% and 64% at the government and private hospitals, respectively. It is unclear why the participants at the faith-based hospital felt this way and certainly this question needs further exploration. We also found that healthcare providers followed by scientific articles were the most trusted source of information about COVID-19 vaccines among those in private institutions, whereas in government and faith-based facilities, healthcare providers followed by media sources were most trusted sources for information on the COVID-19 vaccine. This is in contrast to what CDC Africa reported: that social media and newspapers were the most popular source of information about the vaccine in Kenya [42]. Again, this difference could be explained by the varied geographical sample population. Similar to other studies and probably true of our study as well is that misinformation on social media could have accounted for lower rates of trust in the vaccine in the government and faith-based facilities [11,48].
Approximately 53% of the participants in the government hospital had no formal or high school education. This was in comparison to the 51% of the participants in the private institutions who had an undergraduate or postgraduate degree and 43% of the participants in the faith-based hospital who had a diploma. Level of education has been shown to be a positive predictor of vaccine acceptance in the United States and the Middle East, but not necessarily in sub-Saharan Africa [11,14].
Vaccine uptake at the government hospital in Mombasa and the faith-based facilities was around 52% and 55%, respectively, compared to 82% at the private facilities (all located in Nairobi). This geographically aligns with reports from the Government of Kenya, stating that the vaccination rate as of December 2021 in Nairobi remained the highest, approximately 1.3 million, and was much lower in Mombasa at around 160,000 people around the same time [49]. We postulate that difference in education levels among participants at the different sites as well as the primary source of information about the vaccine played a significant role in vaccine hesitancy within the government and faith-based hospitals.
In this study, approximately 48% of the population seeking care at the government hospital and 46% of the population seeking care at faith-based hospital reported not receiving the vaccine compared to only 19% of the population at private hospitals in Kenya. These findings could be explained by the education level of the participants at the different sites as well as the primary source of information about the vaccine. In addition, participants from the government hospital and faith-based hospital in our study were more often than not from low income households, with higher rates of unemployment, compared to participants from the private institutions. Our study also showed that 11% of the participants within the government hospital and 7% within the faith-based hospital did not feel that it was important to get vaccinated to protect others. This is in comparison to 3% within the private hospitals, and could be potentially explained by the level of education among the different participants as well as the key sources of information about the vaccine. Concerns about the side effects of the vaccine were reported by 71% of participants from the faith-based hospital compared to 40% and 29% at the government and private hospitals, respectively. We are not sure if religious backgrounds and affiliations had an impact on vaccine hesitancy in our study. However, some authors in the West have reported no association between religion and vaccine hesitancy and this question needs further exploration in SSA [50].
Our study has several limitations. Firstly, our study population was recruited at outpatient and inpatient healthcare facilities. Patients actively attending a healthcare facility may be more likely to perceive a need to get the vaccine due to medical illness, and may be more likely to access health services of any type. Hence our study population might not be truly reflective of the general population in Kenya, especially the Kenyans living in rural areas. Secondly, we conducted surveys in four private hospitals, one government and one faith-based hospital, hence making generalization of our results difficult, especially concerning government and faith-based facilities. Thirdly, our survey was conducted in English and it was more difficult for non-English speakers to participate. Lastly, even though anonymous, the surveys were conducted in a hospital setting, so some patients might have felt uncomfortable disclosing their true vaccination status for fear of being stereotyped.
In conclusion, vaccine hesitancy in Kenya, even though much lower than reported in other countries, remains a dynamic and challenging problem in LMIC. Lack of trust in the healthcare system, and misinformation about the vaccine and side effects of the vaccine, remain barriers to effectively vaccinating the public. Although theoretically available, access to vaccines especially in rural areas still continues to pose a challenge. Mitigating strategies specific to Africa need to be developed to help address vaccine hesitancy in this part of the world.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10050705/s1. Questionnaire Survey.
Author Contributions
Conceptualization, J.S. and S.K.A.; data curation, J.S., A.A., K.S., S.M., J.N., K.P., M.A.M., M.S. (Mohamed Sood), V.K., P.K., R.T.R., R.P. and S.K.A.; formal analysis, J.S. and S.K.A.; investigation, S.K.A.; methodology, J.S., R.T.R., Z.T. and S.K.A.; project administration, J.S., A.A., K.S., S.M., J.N., R.K., M.S. (Mohamed Said), M.A.M., M.S. (Mohamed Sood), V.K., S.K., R.P., R.S. and S.K.A.; supervision, A.A., K.S., S.M., J.N., R.K., S.K., Z.T. and S.K.A.; validation, J.S., R.T.R., Z.T. and S.K.A.; writing—original draft, J.S. and S.K.A.; writing—review and editing, A.A., K.S., S.M., J.N., R.K., K.P., M.S. (Mohamed Said), M.A.M., M.S. (Mohamed Sood), V.K., P.K., S.K., R.T.R., R.P., R.S. and Z.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Review Committee of the Aga Khan University Nairobi (Ref: 2021/IERC-115 (v3) and date of approval: 19 October 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
According to our institutional information governance regulations, the anonymized data can be requested from the corresponding author.
Conflicts of Interest
The authors have no conflict of interest to declare.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO Coronavirus Disease (COVID-19) Dashboard. [(accessed on 28 January 2022)]. Available online: https://covid19.who.int/
- 2.Duan Y., Shi J., Wang Z., Zhou S., Jin Y., Zheng Z.J. Disparities in COVID-19 Vaccination among Low-, Middle-, and High-Income Countries: The Mediating Role of Vaccination Policy. Vaccines. 2021;9:905. doi: 10.3390/vaccines9080905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations Vaccine Equity the ‘Challenge of Our Time’, WHO Chief Declares, as Governments Call for Solidarity, Sharing. [(accessed on 25 February 2022)]. Available online: https://news.un.org/en/story/2021/04/1089972.
- 4.Machingaidze S., Wiysonge C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021;27:1338–1339. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Ten Threats to Global Health in 2019. [(accessed on 25 February 2022)]. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 6.Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Böhm R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE. 2018;13:e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper S., Betsch C., Sambala E.Z., McHiza N., Wiysonge C.S. Vaccine hesitancy—A potential threat to the achievements of vaccination programmes in Africa. Hum. Vaccines Immunother. 2018;14:2355–2357. doi: 10.1080/21645515.2018.1460987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mphahlele J. Conspiracy Theories on Covid-19 Vaccine Can Be as Deadly as Virus Itself. [(accessed on 25 February 2022)]. Available online: https://www.iol.co.za/news/opinion/conspiracy-theories-on-covid-19-vaccine-can-be-as-deadly-as-virus-itself-8adf871e-2d9e-4d6a-8e43-ae188308ac52.
- 10.Bangalee A., Bangalee V. Fake news and fallacies: Exploring vaccine hesitancy in South Africa. S. Afr. Fam. Pract. 2021;63:e1–e3. doi: 10.4102/safp.v63i1.5345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D., Yaseen A., Ababneh N.A., Bakri F.G., Mahafzah A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines. 2021;9:42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lucia V.C., Kelekar A., Afonso N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health (Oxf.) 2021;43:445–449. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salali G.D., Uysal M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 2020 doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solís Arce J.S., Warren S.S., Meriggi N.F., Scacco A., McMurry N., Voors M., Syunyaev G., Malik A.A., Aboutajdine S., Adeojo O., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anjorin A.A., Odetokun I.A., Abioye A.I., Elnadi H., Umoren M.V., Damaris B.F., Eyedo J., Umar H.I., Nyandwi J.B., Abdalla M.M., et al. Will Africans take COVID-19 vaccination? PLoS ONE. 2021;16:e0260575. doi: 10.1371/journal.pone.0260575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kollamparambil U., Oyenubi A., Nwosu C. COVID19 vaccine intentions in South Africa: Health communication strategy to address vaccine hesitancy. BMC Public Health. 2021;21:2113. doi: 10.1186/s12889-021-12196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adeniyi O.V., Stead D., Singata-Madliki M., Batting J., Wright M., Jelliman E., Abrahams S., Parrish A. Acceptance of COVID-19 Vaccine among the Healthcare Workers in the Eastern Cape, South Africa: A Cross Sectional Study. Vaccines. 2021;9:666. doi: 10.3390/vaccines9060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammed R., Nguse T.M., Habte B.M., Fentie A.M., Gebretekle G.B. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PLoS ONE. 2021;16:e0261125. doi: 10.1371/journal.pone.0261125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Sokkary R.H., El Seifi O.S., Hassan H.M., Mortada E.M., Hashem M.K., Gadelrab M., Tash R.M.E. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: A cross-sectional study. BMC Infect. Dis. 2021;21:762. doi: 10.1186/s12879-021-06392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amuzie C.I., Odini F., Kalu K.U., Izuka M., Nwamoh U., Emma-Ukaegbu U., Onyike G. COVID-19 vaccine hesitancy among healthcare workers and its socio-demographic determinants in Abia State, Southeastern Nigeria: A cross-sectional study. Pan Afr. Med. J. 2021;40:10. doi: 10.11604/pamj.2021.40.10.29816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed M.A.M., Colebunders R., Gele A.A., Farah A.A., Osman S., Guled I.A., Abdullahi A.A.M., Hussein A.M., Ali A.M., Siewe Fodjo J.N. COVID-19 Vaccine Acceptability and Adherence to Preventive Measures in Somalia: Results of an Online Survey. Vaccines. 2021;9:543. doi: 10.3390/vaccines9060543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . Primary Health Care Systems (Primasys): Case Study from Kenya, Abridged Version. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 23.Djesika A. How Much is Spent on Healthcare in Kenya and Where Does the Money Come From? [(accessed on 25 February 2022)]. Available online: https://aphrc.org/blogarticle/how-much-is-spent-on-healthcare-in-kenya-and-where-does-the-money-come-from/
- 24.Mohiddin A., Temmerman M. COVID-19 Exposes Weaknesses in Kenya’s Healthcare System. 2020. And What can be Done. The Conversation Published 2020. [(accessed on 25 February 2022)]. Available online: https://theconversation.com/covid-19-exposes-weaknesses-in-kenyas-healthcare-system-and-what-can-be-done-143356/
- 25.Amref Health Africa COVID-19 Vaccine Deployment in Kenya. [(accessed on 25 February 2022)]. Available online: https://amref.org/coronavirus/vaccine/
- 26.Orangi S., Pinchoff J., Mwanga D., Abuya T., Hamaluba M., Warimwe G., Austrian K., Barasa E. Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya. Vaccines. 2021;9:936. doi: 10.3390/vaccines9080936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumari A., Ranjan P., Chopra S., Kaur D., Upadhyay A.D., Kaur T., Bhattacharyya A., Arora M., Gupta H., Thrinath A., et al. Development and validation of a questionnaire to assess knowledge, attitude, practices, and concerns regarding COVID-19 vaccination among the general population. Diabetes Metab. Syndr. 2021;15:919–925. doi: 10.1016/j.dsx.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.El-Elimat T., AbuAlSamen M.M., Almomani B.A., Al-Sawalha N.A., Alali F.Q. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. PLoS ONE. 2021;16:e0250555. doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L., McLeod L., Delacqua G., Delacqua F., Kirby J., et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dinga J.N., Sinda L.K., Titanji V.P.K. Assessment of Vaccine Hesitancy to a COVID-19 Vaccine in Cameroonian Adults and Its Global Implication. Vaccines. 2021;9:175. doi: 10.3390/vaccines9020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kabamba Nzaji M., Kabamba Ngombe L., Ngoie Mwamba G., Banza Ndala D.B., Mbidi Miema J., Luhata Lungoyo C., Lora Mwimba B., Cikomola Mwana Bene A., Mukamba Musenga E. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmat. Obs. Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Acheampong T., Akorsikumah E.A., Osae-Kwapong J., Khalid M., Appiah A., Amuasi J.H. Examining Vaccine Hesitancy in Sub-Saharan Africa: A Survey of the Knowledge and Attitudes among Adults to Receive COVID-19 Vaccines in Ghana. Vaccines. 2021;9:814. doi: 10.3390/vaccines9080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shen A.K., Lindstrand A., Schreiber B., O'Brien K. Optimizing the supply of vaccines for COVID-19. Bull. World Health Organ. 2021;99:848. doi: 10.2471/BLT.21.287513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carcelen A.C., Prosperi C., Mutembo S., Chongwe G., Mwansa F.D., Ndubani P., Simulundu E., Chilumba I., Musukwa G., Thuma P., et al. COVID-19 vaccine hesitancy in Zambia: A glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub-Saharan Africa. Hum. Vaccines Immunother. 2021;8:1–6. doi: 10.1080/21645515.2021.1948784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Omar D.I., Hani B.M. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J. Infect. Public Health. 2021;14:1481–1488. doi: 10.1016/j.jiph.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: The forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020;35:785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iliyasu Z., Umar A.A., Abdullahi H.M., Kwaku A.A., Amole T.G., Tsiga-Ahmed F.I., Garba R.M., Salihu H.M., Aliyu M.H. “They have produced a vaccine, but we doubt if COVID-19 exists”: Correlates of COVID-19 vaccine acceptability among adults in Kano, Nigeria. Hum. Vaccines Immunother. 2021;17:4057–4064. doi: 10.1080/21645515.2021.1974796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stoop N., Hirvonen K., Maystadt J.F. Institutional mistrust and child vaccination coverage in Africa. BMJ Glob. Health. 2021;6:e004595. doi: 10.1136/bmjgh-2020-004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Razai M.S., Osama T., McKechnie D.G.J., Majeed A. Covid-19 vaccine hesitancy among ethnic minority groups. BMJ. 2021;372:n513. doi: 10.1136/bmj.n513. [DOI] [PubMed] [Google Scholar]
- 41.Mose A., Haile K., Timerga A. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS ONE. 2022;17:e0263081. doi: 10.1371/journal.pone.0263081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Africa C. COVID 19 Vaccine Perceptions: A 15 Country Study. 2021. [(accessed on 25 February 2022)]. Available online: https://africacdc.org/download/covid-19-vaccine-perceptions-a-15-country-study.
- 43.Adebisi Y.A., Alaran A.J., Bolarinwa O.A., Akande-Sholabi W., Lucero-Prisno D.E. When it is available, will we take it? Social media users’ perception of hypothetical COVID-19 vaccine in Nigeria. Pan Afr. Med. J. 2021;38:230. doi: 10.11604/pamj.2021.38.230.27325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dodd R.H., Cvejic E., Bonner C., Pickles K., McCaffery K.J. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021;21:318–319. doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Posel D., Oyenubi A., Kollamparambil U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE. 2021;16:e0249352. doi: 10.1371/journal.pone.0249352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Valenti G.D., Faraci P. Identifying Predictive Factors in Compliance with the COVID-19 Containment Measures: A Mediation Analysis. Psychol. Res. Behav. Manag. 2021;14:1325–1338. doi: 10.2147/PRBM.S323617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oyekale A.S. Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model. Vaccines. 2021;9:1359. doi: 10.3390/vaccines9111359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shakeel C.S., Mujeeb A.A., Mirza M.S., Chaudhry B., Khan S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines. 2022;10:110. doi: 10.3390/vaccines10010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Faria J. Number of COVID-19 First Dose Vaccines Administered in Kenya 2022, by County. [(accessed on 25 February 2022)]. Available online: https://www.statista.com/statistics/1251234/total-number-of-covid-19-vaccination-doses-in-kenya-by-county/
- 50.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., Katikireddi S.V., Benzeval M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
According to our institutional information governance regulations, the anonymized data can be requested from the corresponding author.