Abstract
Purpose of review:
This review will discuss the utility of high-resolution anterior segment optical coherence tomography (HR-OCT), in-vivo confocal microscopy (IVCM) and ultrasound biomicroscopy (UBM) in characterizing and diagnosing various ocular surface tumors, namely ocular surface squamous neoplasia (OSSN), conjunctival lymphoma and conjunctival melanoma. The strengths and limitations of each imaging modality will be discussed along with characteristics findings of each lesion on each imaging platform.
Recent findings:
HR-OCT can consistently be utilized in the clinic setting to distinguish between epithelial ocular surface tumors such as OSSN as compared with subepithelial tumors such as conjunctival lymphoma and conjunctival melanoma given their distinctive findings. IVCM can be used as an adjunct to HR-OCT to obtain cellular and surface characteristics while UBM can be used to assess tumor depth and thickness for larger and highly pigmented lesions as well as to detect intraocular invasion.
Summary:
HR-OCT, IVCM and UBM are all helpful imaging modalities to diagnose and characterize various ocular surface tumors and can serve as valuable adjuncts to monitor treatment response and assess for recurrence ocular surface tumors.
Keywords: high-resolution anterior segment optical coherence tomography, in-vivo confocal microscopy, ultrasound biomicroscopy, ocular surface squamous neoplasia, conjunctival lymphoma, conjunctival melanoma, HR-OCT, UBM, IVCM
1. Introduction
Multiple imaging modalities are commercially available and have been studied for the visualization and characterization of ocular surface tumors. These imaging modalities include high-resolution anterior segment optical coherence tomography (HR-OCT), in vivo confocal microscopy (IVCM), and ultrasound biomicroscopy (UBM). These various modalities have been shown to be successful in the diagnosis and characterization of ocular surface tumors such as ocular surface squamous neoplasia (OSSN), conjunctival lymphoma and conjunctival melanoma.
Commercially available HR-OCT machines use spectral-domain technology with shorter wavelengths of light to achieve dynamic and rapid scans of the ocular surface at axial resolutions of less than 5 microns (considered ultra-high resolution) up to greater than 5 microns (considered high resolution). These images provide in-vivo, cross-sectional views of the ocular surface and anterior segment.(1) Images can be taken in a rapid and non-contact fashion, multiple cuts can be taken through the lesion of interest, and outputs can be easily interpreted by novice clinicians.(2) In recent years, evolution of swept-source OCT with OCT-angiography (OCTA) has enabled the acquisition of numerous longitudinal and transverse scans at rapid speeds to create 3-dimensional views of the anatomy and vascularity of anterior segment structures. (3)
IVCM aims to focus light in a single plane and eliminate interference from scattered light to image all layers of the ocular surface. (4) Images obtained can typically have a lateral resolution of 1 to 2 microns and an axial resolution of 5 to 10 microns. These resolutions provide highly magnified images of the area of interest but limited fields of view. (5) Obtaining IVCM images often requires highly skilled operators and cooperative patients, given the proximity with which the confocal microscope is needed to reach the ocular surface. Unlike HR-OCT and UBM images which provide cross-sectional views of the lesion of interest, IVCM is only able to obtain en-face images; in addition, images show microscopic features of the lesion of interest and therefore cannot provide details for thicker lesions or comprehensive scans of the entire ocular surface.(6)
UBM uses high frequency ultrasound, ranging from 20 to 50 MHz, to obtain cross-sectional images of the anterior segment.(7, 8) Unlike HR-OCT images which can be limited by posterior shadowing, UBM images can provide better resolution of thick and dense lesions, allowing clinicians to assess lesion thickness and potential intraocular invasion. Unlike HR-OCT which is non-contact, UBM requires immersing the eye in an eyebath in a reclined position in order to obtain best images. (9)
In this review, the utility of various imaging modalities for ocular surface tumors will be discussed, along with an analysis of each modality’s strengths and weaknesses. Each of these imaging modalities can ultimately assist the clinician in obtaining additional information to help determine if an ocular surface lesion is malignant or benign prior to pursuing additional invasive procedures.
2. Ocular surface squamous neoplasia (OSSN)
2.1. High resolution optical coherence tomography (HR-OCT) for OSSN
HR-OCT has been shown to be a powerful tool for the diagnosis and treatment of OSSN. Previous studies by Karp et al have shown that HR-OCT images of OSSN display 3 distinct features: 1. thickened, 2. hyperreflective epithelium with a 3. rapid transition from normal to abnormal epithelium.(1, 10) (Figure 1). These unique characteristics parallel the changes seen on histopathology and enable clinicians to obtain an “optical biopsy” with HR-OCT and expediently diagnose OSSN in the clinic setting.(10) In addition to providing information in the office setting, HR-OCT can also be utilized intra-operatively to better visualize tumor margins and guide surgical excision of these lesions. (11) In cases of more invasive squamous cell carcinoma (SCC), a subepithelial component can also be appreciated on HR-OCT images (Figure 2).
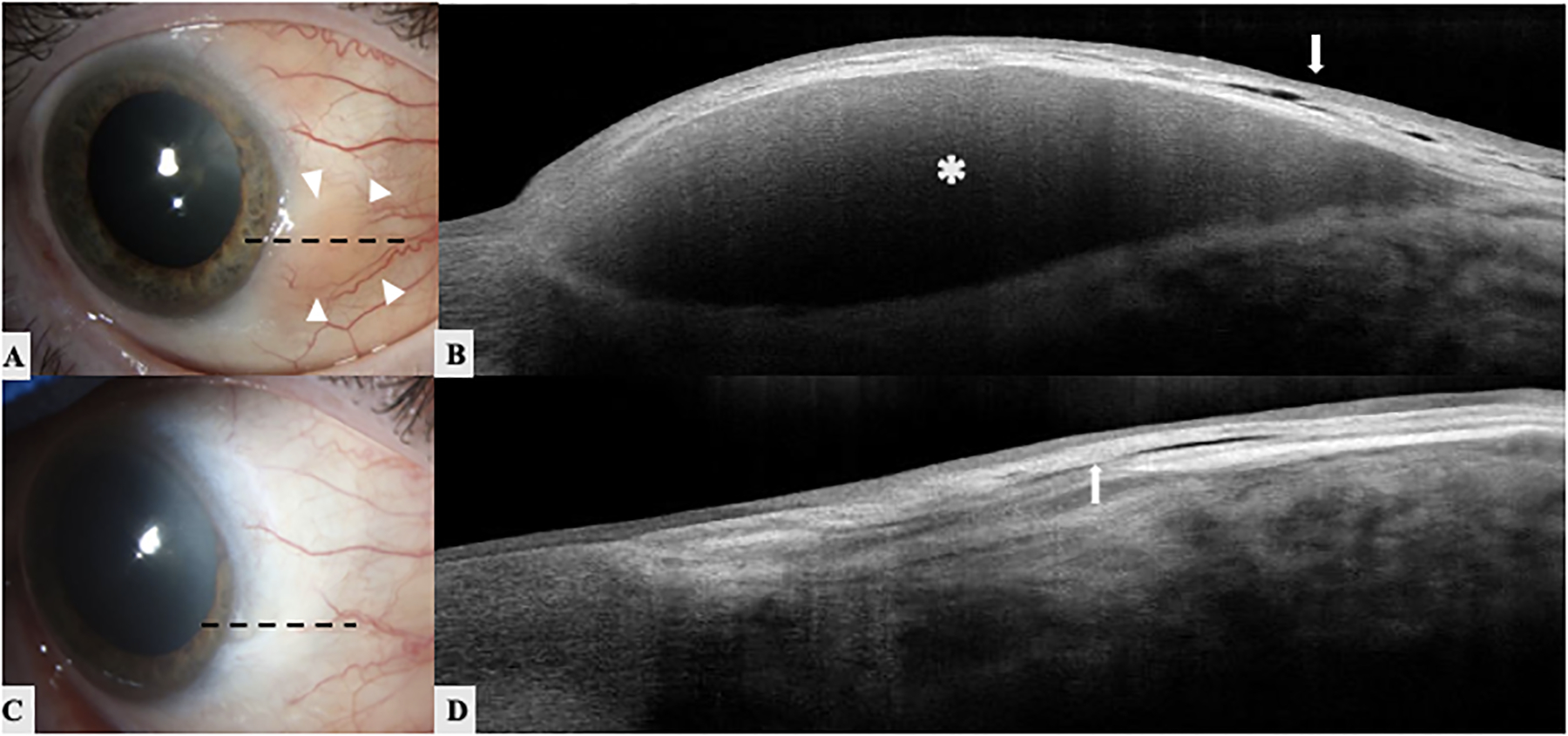
Figure 1. A 70-year-old white male with an ocular surface squamous neoplasia (OSSN) of the left eye.
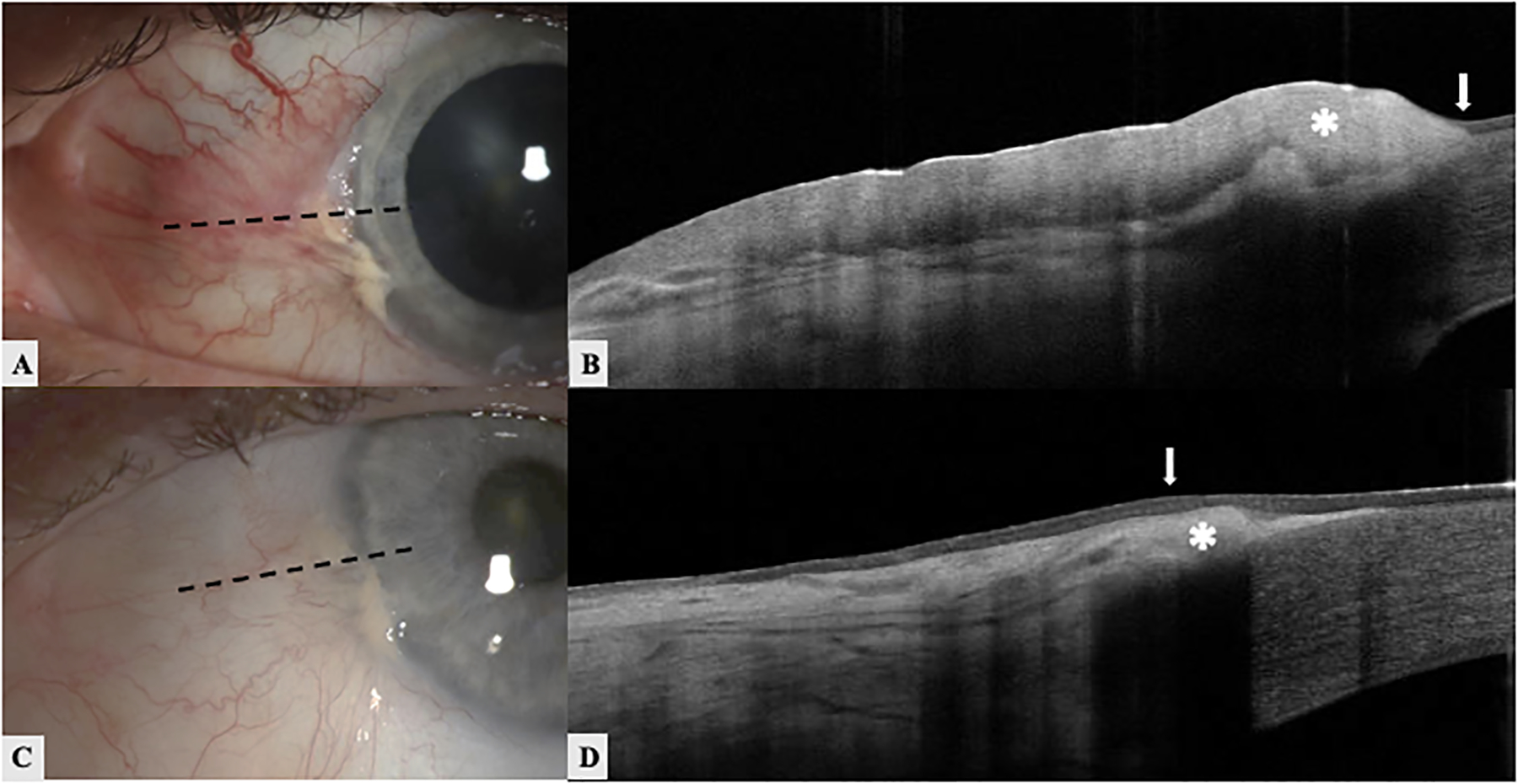
A. Slit lamp image shows a gelatinous OSSN lesion overlying a pterygium on the nasal bulbar conjunctiva. The black dotted line demonstrates the orientation of the HR-OCT raster.
B. High resolution optical coherence tomography (HR-OCT) showing thickened hyperreflective epithelium (asterisk) with an abrupt transition (white arrow) from normal to abnormal epithelium
C. Slit lamp image of the same eye after medical treatment with 5-fluorouracil. The black dotted line demonstrates the orientation of the HR-OCT raster. D. HR-OCT showing normal thickness epithelium (white arrow) following treatment with an underlying hyperreflective subepithelial area consistent with the pterygium (asterisk).
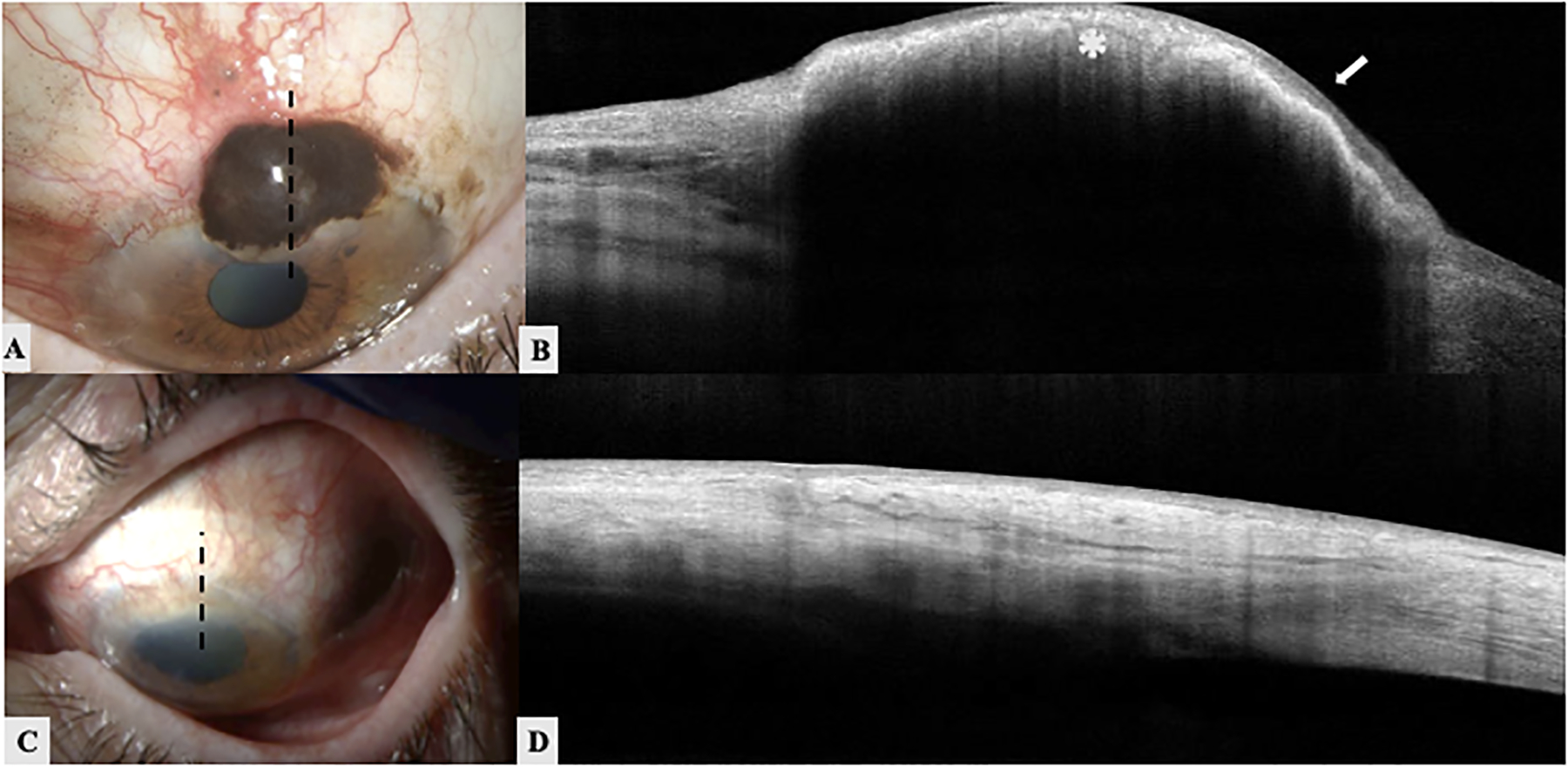
Figure 2. An 82-year-old white male with an invasive squamous cell carcinoma (SCC) of conjunctiva of the right eye.
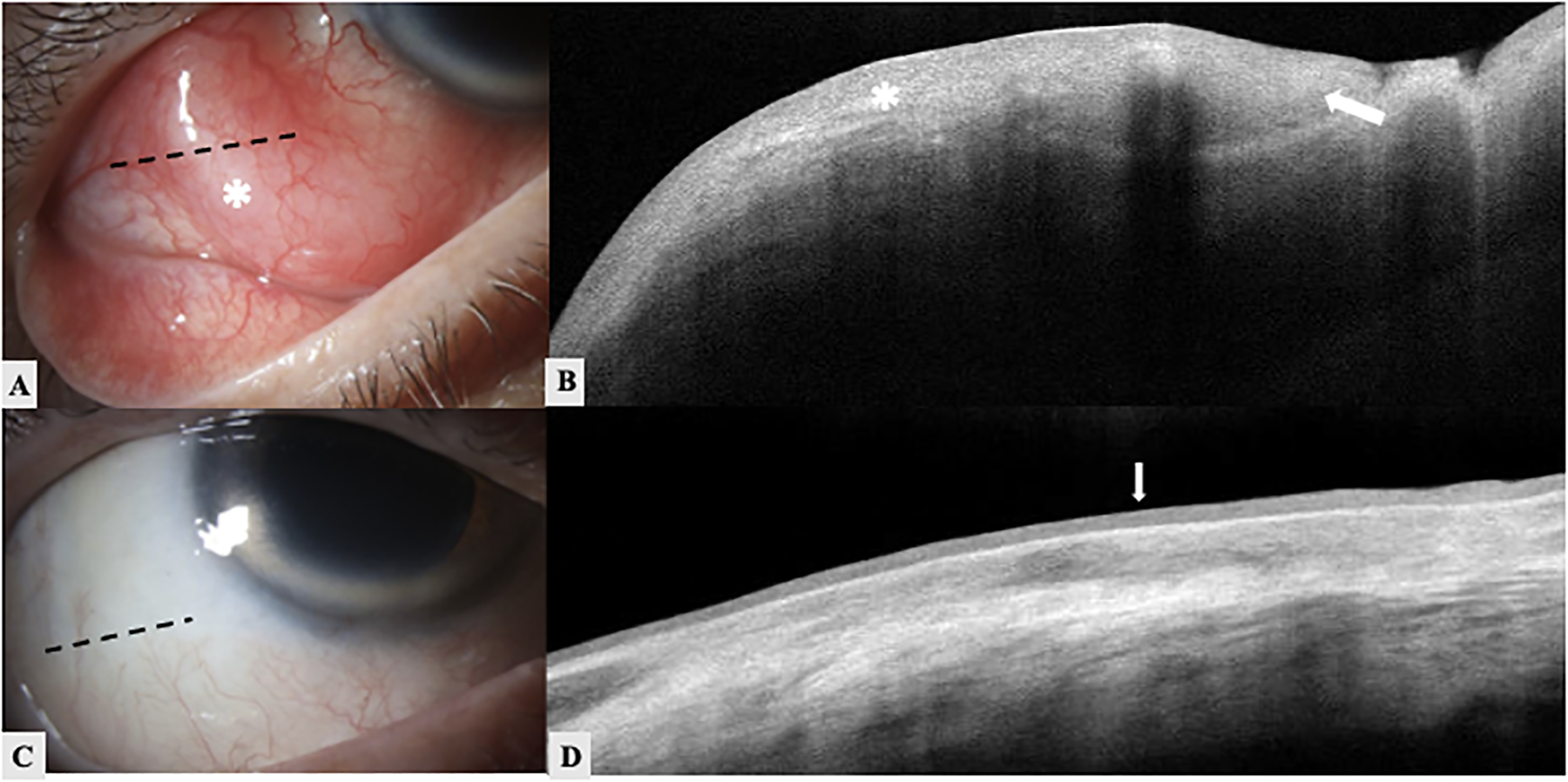
A. Slit lamp image of the right eye shows an immobile elevated nodular conjunctival lesion (white asterisk) with feeder vessels from 7 to 9 o’clock. The black dotted line demonstrates the orientation of the HR-OCT raster. B. HR-OCT showing marked thickened hyperreflective epithelium (asterisk) with significant posterior shadowing effect. Invagination of abnormal epithelium is noted (white arrow). C. Slit lamp image of the same patient after surgical treatment and brachytherapy. The black dotted line demonstrates the orientation of the HR-OCT raster. Excisional biopsy confirmed invasive SCC. D. HR-OCT of the same eye after treatment showing normal thickness epithelium with slight hyperreflectivity (white arrow). The mass is resolved.
Singh et al performed a study that used ultra-high resolution OCT with 3 micron depth OCT images to evaluate the distinguishing characteristics of intraepithelial versus invasive OSSN.(12) All cases of intraepithelial and invasive OSSN showed thickened hyperreflective epithelium with an abrupt transition from normal to abnormal epithelium. However, the majority of cases of intraepithelial disease could be distinguished from invasive SCC by a clear, hyporeflective, plane of separation between the abnormal epithelium and the underlying stromal tissue with a hyperreflective basal membrane overlying the clear plane of separation. On histopathology, this basal membrane correlated to a thick basal layer of dysplastic cells on top of a thickened epithelial basement membrane. Shadowing effects were also observed in leukoplakic lesions as well as in all invasive lesions exceeding 950 microns in depth. Similarly, Nanji et al have found that OSSN lesions with epithelial thicknesses greater than 465 microns exhibited shadowing, precluding clear visualization of the inferior epithelial border. (13)
HR-OCT can also serve as a tool to differentiate malignant ocular surface lesions from benign lesions. Kieval et al initially published a study demonstrating that HR-OCT was 94% sensitive and 100% specific in differentiating OSSN from pterygia with an epithelial thickness cut-off value of 142 microns using a custom built device.(14) More recently, Lozano Garcia et al confirmed that HR-OCT was 100% sensitive and specific in distinguishing OSSN from pterygia with an epithelial thickness cut-off of 141 microns.(15) These results were comparable to the findings by Nanji et al who determined that an epithelial thickness cut-off of 120 microns on a commercial HR-OCT device was 100% sensitive and specific in differentiating OSSN from pterygia.(13) These papers demonstrate that in addition to morphologic changes, epithelial thickness can help guide the clinician in distinguishing malignant OSSN from benign pterygia.
HR-OCT images can also be used to monitor response to topical chemotherapy (Figure 1). Singh et al found decreases in epithelial hyperreflectivity and thickness on serial HR-OCT images and restoration of normal anatomy after topical and subconjunctival chemotherapy. (12) A recent study by Tran et al showed that HR-OCT is an important modality to diagnose subclinical OSSN in cases that have already undergone treatment with topical chemotherapy. In this study, 17% of patients were found to have subclinical disease on HR-OCT imaging that was not appreciated on clinical examination. An additional 1 to 2 months of chemotherapy treatment were needed to achieve complete tumor resolution, with no disease recurrence at two years follow-up. Sub-clinical disease detected by HR-OCT in patients with otherwise apparent clinical resolution of OSSN can help clinicians extend therapy past the point of clinical resolution to prevent disease progression and recurrence. (16)
Lastly, OCTA has recently been used to demonstrate distinctive vessel patters in OSSN lesions. Studies have shown that there are higher blood vessel densities in the body of OSSN tumors as compared with the underlying conjunctiva and adjacent subepithelial tissue (17), which can help further identify malignant lesions on the ocular surface. While at this point not seemingly specific for diagnostic purposes, OCTA may provide insights into the pathophysiology of OSSN and other malignant ocular surface lesions and help determine response to treatment.
2.2. In-vivo confocal microscopy (IVCM) for OSSN
IVCM can be used to image the cornea and conjunctiva to diagnose OSSN. Liang et al showed that OSSN lesions were characterized by dysplastic cells with hyper-reflective cytoplasm and increased nuclear to cytoplasmic ratio on IVCM. Main IVCM parameters suggestive of OSSN as compared to corneal intraepithelial neoplasia (CIN) included presence of dysplastic appearing cells in the superficial stromal layer, nuclear mitotic figures, and nests of vortex cells in the superficial stromal layer.(18) Similarly, another study found that the predominant features of OSSN on IVCM included presence of hyperreflective pleomorphic squamous cells in the anterior and middle layers of the epithelium, a well-defined border between neoplastic and normal epithelium and pleomorphic cells, and loss of sub-basal corneal nerves in the areas involved by OSSN lesions as compared with unaffected epithelium (Figure 3). Additional features of OSSN lesions included findings of enlarged, irregular and hyperchromatic nuclei, bright dots in the basal cells layers (termed a starry sky appearance) of the areas involving OSSN lesions, as well as invasion of malignant cells into Bowman’s layer.(19) However, in a study using IVCM to distinguish between OSSN and benign lesions in an African American population, IVCM was not found to reliably distinguish between OSSN and benign conjunctival lesions given an overlap in findings (ie irregular sized, hyperreflective cells, prominent nucleoli, and presence of mitotic figures) for both the types of lesions.(20)
Figure 3: A 74-year-old white male with corneal intraepithelial neoplasia (CIN) of the right eye.
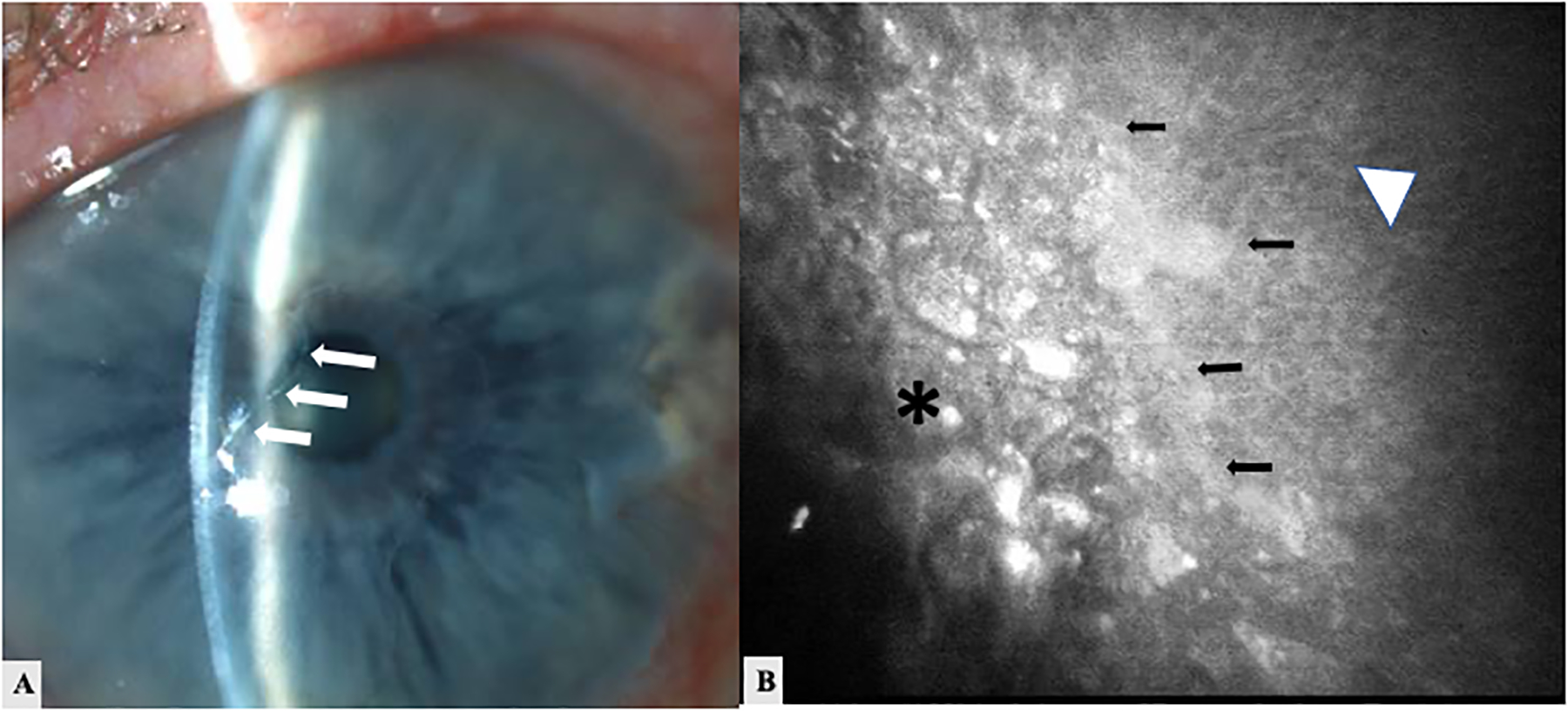
A. Slit lamp image shows a translucent grey epithelial sheet on the inferior limbus extending onto the central cornea (arrows at border). B. In vivo confocal microscopy (IVCM) image showing normal epithelial cells (triangle) adjacent to abnormal neoplastic epithelial cells with hyperreflective nuclei with heteromorphic and hyperreflective borders (asterisk). An abrupt transition zone is seen between normal and abnormal cells (arrows). Courtesy of Dr. Elmer Tu, Chicago, IL.
IVCM, similar to HR-OCT, can also be used to monitor response to chemotherapy when treating OSSN lesions. Sequential IVCM scans obtained at 90–100 micron depth after two months of topical interferon alpha-2b therapy showed decrease in epithelial cell reflectivity, fading of a the previously well-defined demarcation line between normal and neoplastic tissue, and fragmentation of abnormal cell clusters early in treatment. Re-appearance of previously absent sub-basal nerves and distinct cell membranes were observed later in eyes with complete response to topical chemotherapy. In certain cases, regression of subepithelial vessels could also be observed.(19) However, in some patients with complete clinical response to therapy, small degrees of residual epithelial hyperreflectivity persisted. The sensitivity and specificity of IVCM to detect true subclinical disease still remains to be formally studied.
Performing IVCM can oftentimes be challenging for both the operator and patient. Cinotti et al explored the utility of a handheld reflectance confocal microscope to characterize and diagnose various conjunctival tumors in a pilot study. Five OSSN lesions in this series were characterized by large irregular appearing epithelial cells (>20 microns) with an abundance of dendritic cells often in a disarranged pattern.(21) Differing characteristics were seen for other conjunctival tumors (ie conjunctival lymphomas or melanomas, which will be discussed below) and with its mobility and ease of use, the handheld reflectance confocal microscope shows promise in allowing for rapid diagnosis and differentiation of OSSN lesions.
2.3. Ultrasound biomicroscopy (UBM)
The quality of HR-OCT images is often limited by extensive shadowing when tumors are very thick or invasive. In such cases, UBM can offer greater penetration of ocular tissues and permit better visualization of the thickness and depth of OSSN lesions.(22) UBM with 50 MHz wavelengths provides better resolution of lesions (25 micron resolution) while UBM with 20 MHz allows for wider and deeper fields of view.(7) UBM images of OSSN typically reveal high reflectivity of the tumor surface with low reflectivity of the tumor stroma and variable reflectivity of intraocular extensions of the tumor (Figure 4). Invasive tumors can be identified by looking for blunting of the anterior chamber, tissue invasion of the anterior chamber angle or ciliary body or uveal thickening on UBM, and are better viewed with 50 MHz UBM.(22, 23) Meel et al have suggested that occult intraocular invasion of OSSN can be detected with UBM when specifically used in patients with risk factors such as nodular or ulcerative tumor morphology, tumor thickness of >5mm in height, history of immunosuppression or previous history of surgical intervention, as these risk factors are often associated with more aggressive behaving OSSN lesions. (22)
Figure 4:
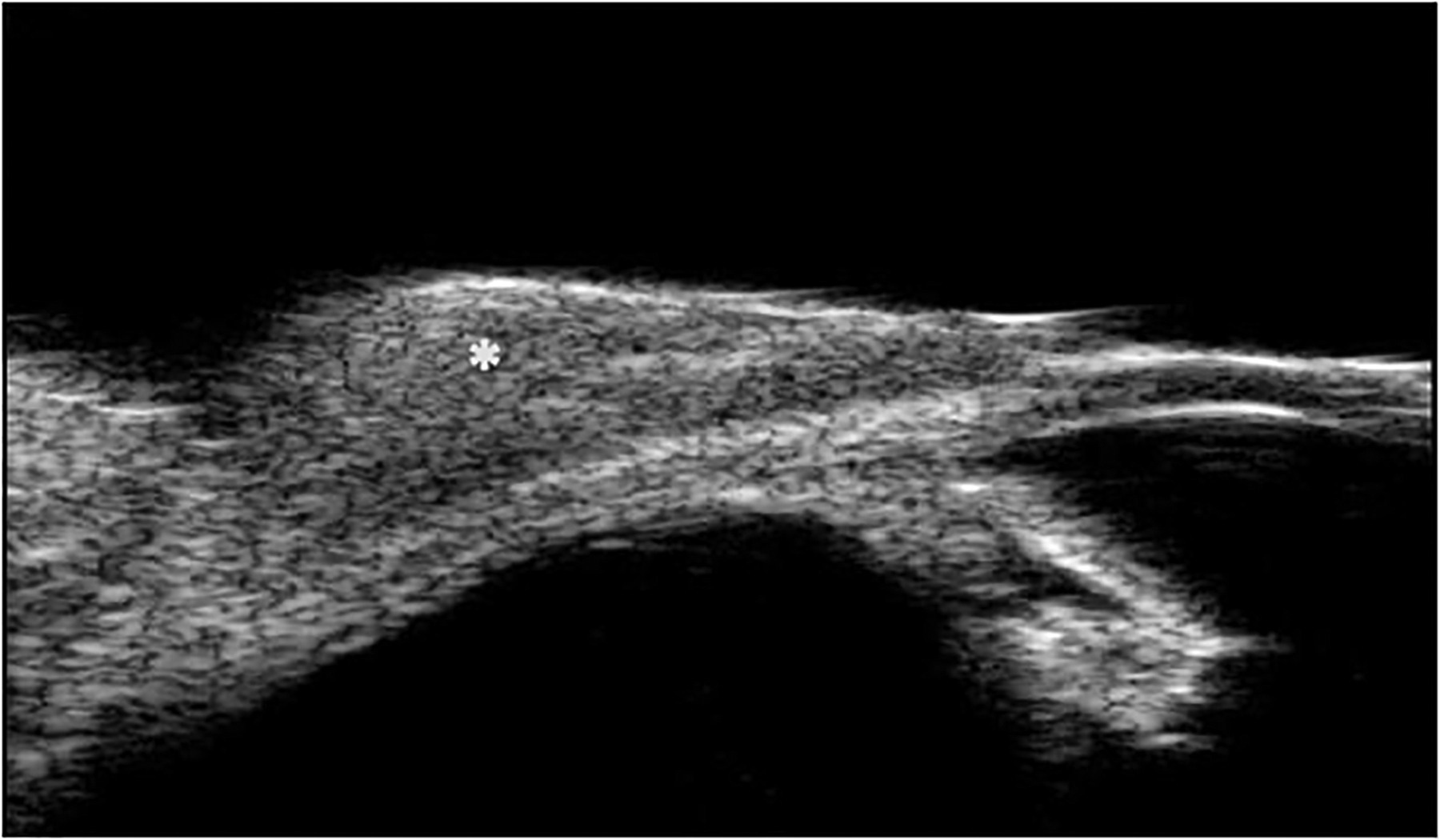
High-resolution ultrasound biomicroscopy (UBM) image shows a dome-shaped, non-vascularized, slightly hypoechoic lesion over the sclera (asterisk). No definite scleral involvement is evident on the UBM. However, the clinical examination and final pathologic report confirmed the scleral invasion of this SCC lesion.
3. Conjunctival Lymphoma
3.1. HR-OCT for conjunctival lymphoma
HR-OCT can be used to diagnose and differentiate conjunctival lymphoma lesions from other conjunctival surface tumors. On HR-OCT, conjunctival lymphoma is characterized by a normal layer of epithelium overlying homogeneous, dark, hyporeflective subepithelial lesions with smooth borders. The lesions often contain monomorphic, stippled, dot-like infiltrates that correspond to the infiltration of monoclonal lymphocytes on histopathology (Figure 5).(1, 24) When compared with lesions such as benign lymphoid reactive hyperplasia (BLRH) or conjunctival amyloidosis that can appear similar clinically to lymphoma lesions, HR-OCT image findings can help the clinician narrow the differential diagnosis. HR-OCT images of BRLH have a normal epithelial layer but instead contain variably reflective subepithelial tissue that is dependent on the cellularity of the monomorphic infiltrate in this tissue. Hyperreflective subepithelial lesions on HR-OCT correspond to a paucicellular infiltrate on histopathology while hyporeflective subepithelial lesions correspond with high levels of cellular infiltrates. (1, 24) In comparison, HR-OCT images of conjunctival amyloidosis shows heterogeneous, dark lesions with irregular borders, often containing hyperreflective linear infiltrates on HR-OCT images. While BRLH and conjunctival lymphoma can sometimes be challenging to differentiate with HR-OCT, lymphoma and amyloidosis are easier to distinguish from one another.
Figure 5: A 56-year-old white female with conjunctival lymphoma of the right eye.
A.Slit lamp image shows elevated round yellowish lesion near the limbus from 3–4 o’clock (arrowheads) with increased vascularity around lesion. The black dotted line demonstrates the orientation of the HR-OCT raster. Biopsy confirmed lymphoma. B. HR-OCT shows normal thickness epithelium (arrow) with a large homogeneous, hyporeflective subepithelial lesion with smooth borders containing monomorphic, stippled, dot-like infiltrates that correspond to the infiltration of monoclonal lymphocytes on histopathology (asterisk). A hyperreflective band of tissue is noted above and below the infiltrate. C. Slit lamp image of the same patient after seventeen sessions of external beam radiation. The black dotted line demonstrates the orientation of the HR-OCT raster. D. HR-OCT after treatment shows normal thickness epithelium with resolution of the subepithelial lesion and mild residual underlying subepithelial scarring (arrow).
Similar to the use of HR-OCT to detect response to clinical treatment of OSSN lesions, HR-OCT can demonstrate normalization of conjunctival architecture after radiation or chemotherapy treatment as well as detect residual tissue thickening and subclinical disease after treatment that is often not detected on clinical examination. (13, 25, 26) However, it is important to note that the ability of HR-OCT to image conjunctival lymphoma lesions can be limited by the substantial thickness of these lesions which can cause posterior shadowing and obscuration of the structural details of the deeper subepithelial tissue.(27) In these circumstances, additional imaging tools, such as UBM may be required to achieve improved visualization of larger lesions.
3.2. IVCM for conjunctival lymphoma
There is limited literature on the use of IVCM for the diagnosis and differentiation of conjunctival lymphoma. The first case of using IVCM to characterize MALT conjunctival lymphoma was in 2008 and found this lymphomatous lesion to contain tightly packed, small, hyperreflective cells arranged in nests or cystic spaces, which closely correlated to its histopathologic appearance.(28) In the study by Cinotti et al, the handheld confocal microscope was able to successfully image 2 conjunctival lymphoma lesions similar to OSSN lesions. Confocal images showed normal epithelium with abundant small hyperrefractive round cells, which once again corresponded to the presence of lymphocytes in the stroma on histopathology.(21) IVCM can likely be used in conjunction with HR-OCT to narrow the differential for a lymphomatous appearing conjunctival lesion, however, histopathology is still required to confirm the diagnosis.
4. Conjunctival Melanoma
4.1. HR-OCT for conjunctival melanoma
HR-OCT of conjunctival melanoma lesions images show a hyperreflective subepithelial lesion with normal to slightly thick layer of epithelium with variable hyperreflectivity of the basal epithelium (Figure 6). Hyperreflectivity of the epithelium is suggestive of involvement of the epithelium with atypical melanocytes. (1) Similar to conjunctival lymphoma lesions, the area of interest is largely in the subepithelial space, allowing clinicians to distinguish melanomas from epithelial tumors such as OSSN on HR-OCT. When comparing conjunctival melanoma to its more benign counterpart primary acquired melanosis (PAM), HR-OCT images of PAM differ by having no subepithelial component and demonstrating normal thickness epithelium with a hyperreflective basal epithelial band, which correlates histopathologically with basal epithelial melanocytic pigmentation. (29)
Figure 6: A 62-year-old white female with a conjunctival melanoma of the left eye.
A.Slit lamp image shows a superior elevated dark brown conjunctival lesion from 11–2 o’clock with prominent feeder vessels. Diffuse conjunctival melanosis almost 360 degrees is seen. The black dotted line demonstrates the orientation of the HR-OCT raster. Biopsy confirmed conjunctival melanoma. B. HR-OCT shows normal thickness epithelium (arrow) overlying a marked hyperreflective subepithelial lesion (asterisk) with posterior shadowing. C. Slit lamp image of the same eye after surgical excision of the conjunctival melanoma and ocular surface reconstruction. The black dotted line demonstrates the orientation of the HR-OCT raster. D. HR-OCT shows normal thickness, mildly hyperreflective epithelium and complete resolution of the subepithelial mass.
OCTA has also been recently implemented to characterize vessel structure and density in ocular surface melanomas as compared with PAM and conjunctival nevi. In a study by Brouwer et al, OCTA showed interlesional tortuous vascular patterns in conjunctival melanomas that differed from the more fine vascular networks seen in PAM as well as normal conjunctiva (30); conjunctival nevi also more commonly contained internal cystic structures as compared with conjunctival melanoma and PAM lesions. (1, 30)
Given that conjunctival melanoma lesions are also often large and thick in nature, quality of HR-OCT images can be limited by posterior shadowing that obscures internal structural details of melanomas. (1) In these circumstances, UBM offers additional details to detect deeper extrascleral or intraocular invasion of these tumors. For all pigmented lesions (conjunctival melanoma, PAM or conjunctival nevi), HR-OCT is not able to confirm or rule-out the presence of atypical or dysplastic cells and histopathology with tissue biopsy is required.
4.2. IVCM for conjunctival melanoma
IVCM has also been shown to be have distinctive characteristics to help diagnose and differentiate conjunctival melanoma lesions. IVCM images of conjunctival melanoma typically show hyperreflective cells with prominent nucleoli, atypical large nuclei, tumor vessels and surrounding inflammation.(31, 32) The IVCM images obtained by Cinotti et al with a handheld confocal microscope confirmed similar image findings of 10 conjunctival melanomas: melanoma lesions contained large >20 micron sized round, hyperreflective cells as well as dendritic and pagetoid cells at the epithelial-stromal junction and/or stroma.(21) In one study that imaged 7 conjunctival melanomas, IVCM was shown to be 89% sensitive and 100% specific in diagnosing conjunctival melanoma.(31)
IVCM images of melanoma have some distinctive differences from conjunctival nevi as well as PAM with and without atypia.(21, 31) In a series of 6 conjunctival nevi imaged with IVCM, conjunctival nevi were found to have multilayered epithelium with collections of uniform, round, medium-size hyporeflective as well as hyperreflective cells arranged diffusely or in nests in the stroma; large pseudocysts partly filled with cellular debris were also visualized in certain cases. (31). PAM with atypia typically has networks of large, >20 micron sized, pagetoid dendritic cells and hyperreflective granules in the epithelium while PAM without atypia has hyperreflective, cells confined to basal epithelium along with small <20 micron sized pagetoid dendritic cells in the epithelium.(21, 31) In one study, IVCM was noted to have 100% sensitivity and 96% specificity to diagnose PAM with atypia; however, this was based on imaging results of only 13 PAM lesions. While IVCM is able to detect changes at the cellular level for conjunctival melanomas, confirmation of cellular atypia is once again best achieved with tissue analysis.
4.3. UBM for conjunctival melanoma
For conjunctival melanomas which are thicker, pigmented lesions, UBM can provide improved resolution of the posterior margins of the tumor and can help better assess posterior tumor surfaces and tumor thickness due to less shadowing effect.(9, 33) UBM can also be helpful to detect intraocular invasion of a conjunctival melanoma from extraocular extension of a uveal melanoma (Figure 7). Ultimately UBM can often be used in conjunction with HR-OCT and IVCM to provide optimal visualization of a melanoma lesion both at the cellular level and deeper stromal levels.
Figure 7: A 90-year-old white female with conjunctival melanoma on the right eye.
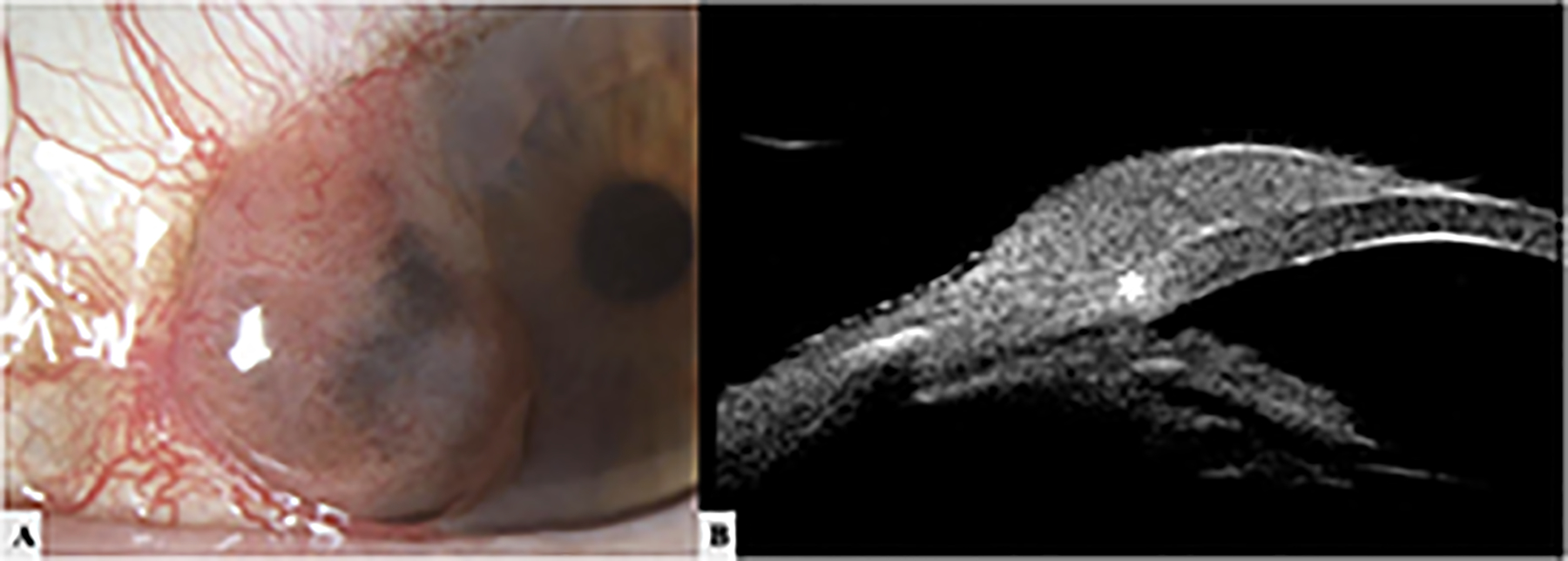
A.Slit lamp image shows a highly elevated mixed melanotic and amelanotic lesion on the bulbar conjunctiva and abutting the cornea from 7–10 o’clock with feeder vessels. B. High resolution UBM image shows a dome-shaped, regular structure with a mild hypoechoic core. Possible invasion into the corneal limbus at the 9 o’clock position (asterisk) is noted.
5. Conclusions
The advent of HR-OCT, IVCM and UBM has provided clinicians with powerful adjuncts to more accurately diagnose, monitor and treat various ocular surface tumors. HR-OCT is an efficient and high-yield diagnostic modality to diagnose and differentiate between various ocular surface tumors and specifically determine if the tumors are epithelial or subepithelial in nature. IVCM can be used as an adjunct to HR-OCT and a UBM image can be obtained if there is concern for deeper scleral or intraocular invasion. While histopathology remains the gold standard, HR-OCT, IVCM and UBMs can provide “optical biopsies” to identify characteristic features that can help differentiate between benign and malignant lesions and can also help narrow the differential diagnosis of a given lesion in the office setting. These imaging adjuncts can also help guide clinicians determine response to therapy and evaluate for recurrent disease.
Key points:
High-resolution anterior segment optical coherence tomography (HR-OCT), in-vivo confocal microscopy (IVCM) and ultrasound biomicroscopy (UBM) are all modalities that can be used to characterize and diagnose various ocular surface tumors, including ocular surface squamous neoplasia, conjunctival lymphoma and conjunctival melanoma.
HR-OCT and IVCM can be used together to assess cellular and surface characteristics of tumors while UBM can be used to assess tumor depth and thickness, especially for larger and highly pigmented lesions.
Images provided by HR-OCT, IVM and UBM can help clinicians obtain “optical biopsies” in the clinic setting and identify characteristics that differentiate benign and malignant lesions.
Financial Support:
NIH Center Core Grant P30EY014801 (institutional), Research to Prevent Blindness Unrestricted Grant (institutional), Dr. Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The Robert Farr Family Grant, The Grant and Diana Stanton-Thornbrough, The Robert Baer Family Grant, The Emilyn Page and Mark Feldberg Grant, The Robert Farr Family Grant, The Jose Ferreira de Melo Grant, The Richard and Kathy Lesser Grant, The Calvin and Flavia Oak Support Fund, The Michele and Ted Kaplan Grant and the Richard Azar Family Grant (institutional grants).
Footnotes
Disclosures: The authors have no financial disclosures to report
References
- *1.Venkateswaran N, Galor A, Wang J, Karp CL. Optical coherence tomography for ocular surface and corneal diseases: a review. Eye Vis (Lond). 2018;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review comprehensively discusses the findings of high-resolution optical coherence tomography for various ocular surface lesions and corneal diseases.
- 2.Yim M, Galor A, Nanji A, Joag M, Palioura S, Feuer W, et al. Ability of novice clinicians to interpret high-resolution optical coherence tomography for ocular surface lesions. Can J Ophthalmol. 2018;53(2):150–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ang M, Baskaran M, Werkmeister RM, Chua J, Schmidl D, Aranha Dos Santos V, et al. Anterior segment optical coherence tomography. Prog Retin Eye Res. 2018;66:132–56. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka S, Kohanim S. The Role of Confocal Microscopy in Diagnosing Ocular Surface Tumors. Int Ophthalmol Clin. 2017;57(1):75–85. [DOI] [PubMed] [Google Scholar]
- 5.Jalbert I, Stapleton F, Papas E, Sweeney DF, Coroneo M. In vivo confocal microscopy of the human cornea. Br J Ophthalmol. 2003;87(2):225–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alomar TS, Nubile M, Lowe J, Dua HS. Corneal intraepithelial neoplasia: in vivo confocal microscopic study with histopathologic correlation. Am J Ophthalmol. 2011;151(2):238–47. [DOI] [PubMed] [Google Scholar]
- 7.Ong SS, Vora GK, Gupta PK. Anterior Segment Imaging in Ocular Surface Squamous Neoplasia. J Ophthalmol. 2016;2016:5435092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gündüz K, Hoşal BM, Zilelioğlu G, Günalp I. The use of ultrasound biomicroscopy in the evaluation of anterior segment tumors and simulating conditions. Ophthalmologica. 2007;221(5):305–12. [DOI] [PubMed] [Google Scholar]
- 9.Bianciotto C, Shields CL, Guzman JM, Romanelli-Gobbi M, Mazzuca D Jr., Green WR, et al. Assessment of anterior segment tumors with ultrasound biomicroscopy versus anterior segment optical coherence tomography in 200 cases. Ophthalmology. 2011;118(7):1297–302. [DOI] [PubMed] [Google Scholar]
- 10.Thomas BJ, Galor A, Nanji AA, El Sayyad F, Wang J, Dubovy SR, et al. Ultra high-resolution anterior segment optical coherence tomography in the diagnosis and management of ocular surface squamous neoplasia. Ocul Surf. 2014;12(1):46–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *11.Karp CL, Mercado C, Venkateswaran N, Ruggeri M, Galor A, Garcia A, et al. Use of High-Resolution Optical Coherence Tomography in the Surgical Management of Ocular Surface Squamous Neoplasia: A Pilot Study. Am J Ophthalmol. 2019;206:17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates the utility of intra-operative high-resolution anterior segment optical coherence tomography to determine tumor margins and guide surfical excision of ocular surface squamous neoplasia lesions.
- *12.Singh S, Mittal R, Ghosh A, Tripathy D, Rath S. High-Resolution Anterior Segment Optical Coherence Tomography in Intraepithelial Versus Invasive Ocular Surface Squamous Neoplasia. Cornea. 2018;37(10):1292–8. [DOI] [PubMed] [Google Scholar]; This study used ultra-high resolution anterior segment optical coherence tomography with 3 micron depth images to evaluate the distinguishing characteristics of intraepithelial versus invasive ocular surface squamous neoplasia.
- 13.Nanji AA, Sayyad FE, Galor A, Dubovy S, Karp CL. High-Resolution Optical Coherence Tomography as an Adjunctive Tool in the Diagnosis of Corneal and Conjunctival Pathology. Ocul Surf. 2015;13(3):226–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kieval JZ, Karp CL, Abou Shousha M, Galor A, Hoffman RA, Dubovy SR, et al. Ultra-high resolution optical coherence tomography for differentiation of ocular surface squamous neoplasia and pterygia. Ophthalmology. 2012;119(3):481–6. [DOI] [PubMed] [Google Scholar]
- *15.Lozano García I, Romero Caballero MD, Sellés Navarro I. High resolution anterior segment optical coherence tomography for differential diagnosis between corneo-conjunctival intraepithelial neoplasia and pterygium. Arch Soc Esp Oftalmol. 2020;95(3):108–13. [DOI] [PubMed] [Google Scholar]; This study found that high resolution optical coherence tomography was 100% sensitive and specific in distinguishing ocular surface squamous neoplasia lesions from pterygia with an epithelial thickness cut-off of 141 microns.
- *16.Tran AQ, Venkateswaran N, Galor A, Karp CL. Utility of high-resolution anterior segment optical coherence tomography in the diagnosis and management of sub-clinical ocular surface squamous neoplasia. Eye Vis (Lond). 2019;6:27. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated how high resolution anterior segment optical coherence tomography is an important modality to diagnose subclinical ocular surface squamous neoplasia in cases that have already undergone treatment with topical chemotherapy. 17% of patients were found to have subclinical disease on OCT imaging that was not appreciated on clinical examination.
- *17.Liu Z, Karp CL, Galor A, Al Bayyat GJ, Jiang H, Wang J. Role of optical coherence tomography angiography in the characterization of vascular network patterns of ocular surface squamous neoplasia. Ocul Surf. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used optical coherence tomography angiography to demonstrate distinctive vessel patters in ocular surface squamous neoplasia lesions and found higher blood vessel densities in the body of surface tumors as compared with the underlying conjunctiva and adjacent subepithelial tissue.
- 18.Liang QF, Huang JJ, Cao K, Su GY, Wang ZQ, Zhang Y, et al. [Histopathology manifestation and imaging characteristics of in vivo confocal microscopy for diagnosis of ocular surface squamous neoplasia]. Zhonghua Yan Ke Za Zhi. 2018;54(9):652–60. [DOI] [PubMed] [Google Scholar]
- 19.Zarei-Ghanavati M, Mousavi E, Nabavi A, Latifi G, Mehrjardi HZ, Mohebbi M, et al. Changes in in vivo confocal microscopic findings of ocular surface squamous neoplasia during treatment with topical interferon alfa-2b. Ocul Surf. 2018;16(2):235–41. [DOI] [PubMed] [Google Scholar]
- 20.Nguena MB, van den Tweel JG, Makupa W, Hu VH, Weiss HA, Gichuhi S, et al. Diagnosing ocular surface squamous neoplasia in East Africa: case-control study of clinical and in vivo confocal microscopy assessment. Ophthalmology. 2014;121(2):484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cinotti E, Perrot JL, Labeille B, Campolmi N, Espinasse M, Grivet D, et al. Handheld reflectance confocal microscopy for the diagnosis of conjunctival tumors. Am J Ophthalmol. 2015;159(2):324–33.e1. [DOI] [PubMed] [Google Scholar]
- 22.Meel R, Dhiman R, Sen S, Kashyap S, Tandon R, Vanathi M. Ocular Surface Squamous Neoplasia with Intraocular Extension: Clinical and Ultrasound Biomicroscopic Findings. Ocul Oncol Pathol. 2019;5(2):122–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *23.Kaliki S, Jajapuram SD, Maniar A, Taneja S, Mishra DK. Ocular surface squamous neoplasia with intraocular tumour extension: a study of 23 patients. Eye (Lond). 2020;34(2):319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates the utility of ultrasound biomicroscopy in imaging intraocular tumor extensions of aggressive ocular surface squamous neoplasia lesions.
- *24.Venkateswaran N, Mercado C, Tran AQ, Garcia A, Diaz PFM, Dubovy SR, et al. The use of high resolution anterior segment optical coherence tomography for the characterization of conjunctival lymphoma, conjunctival amyloidosis and benign reactive lymphoid hyperplasia. Eye Vis (Lond). 2019;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study explores the use of high resolution anterior segment optical coherence tomography to diagnose and differentiate conjunctival lymphoma, amyloidosis and benign reactive lymphoid hyperplasia lesions. Distinctive characteristics were identified for each type of lesion to help clinicians distinguish between these lesions in the office setting using OCT images.
- 25.Nanji AA, Mercado C, Galor A, Dubovy S, Karp CL. Updates in Ocular Surface Tumor Diagnostics. Int Ophthalmol Clin. 2017;57(3):47–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shousha MA, Karp CL, Perez VL, Hoffmann R, Ventura R, Chang V, et al. Diagnosis and management of conjunctival and corneal intraepithelial neoplasia using ultra high-resolution optical coherence tomography. Ophthalmology. 2011;118(8):1531–7. [DOI] [PubMed] [Google Scholar]
- *27.Tanenbaum RE, Galor A, Dubovy SR, Karp CL. Classification, diagnosis, and management of conjunctival lymphoma. Eye Vis (Lond). 2019;6:22. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review summarizes up to date recommendations for the diagnosis and management of conjunctival lymphoma lesions.
- 28.Pichierri P, Martone G, Loffredo A, Traversi C, Polito E. In vivo confocal microscopy in a patient with conjunctival lymphoma. Clin Exp Ophthalmol. 2008;36(1):67–9. [DOI] [PubMed] [Google Scholar]
- 29.Alzahrani YA, Kumar S, Abdul Aziz H, Plesec T, Singh AD. Primary Acquired Melanosis: Clinical, Histopathologic and Optical Coherence Tomographic Correlation. Ocul Oncol Pathol. 2016;2(3):123–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *30.Brouwer NJ, Marinkovic M, Bleeker JC, Luyten GPM, Jager MJ. Anterior Segment OCTA of Melanocytic Lesions of the Conjunctiva and Iris. Am J Ophthalmol. 2020;222:137–47. [DOI] [PubMed] [Google Scholar]; This study demonstrated the ability of optical coherence tomography angiography to non-invasively image the vasculature of melanocytic lesions of the conjunctiva and iris. The study was able to identify different vascular patterns in conjunctival melanoma and conjuncitival nevi as compared with primary acquired melanosis and normal conjunctiva.
- 31.Messmer EM, Mackert MJ, Zapp DM, Kampik A. In vivo confocal microscopy of pigmented conjunctival tumors. Graefes Arch Clin Exp Ophthalmol. 2006;244(11):1437–45. [DOI] [PubMed] [Google Scholar]
- 32.Ronin C, Grivet D, Kaspi M, Dumollard JM, Douchet C, Thuret G, et al. [Contribution of reflectance confocal microscopy in the diagnosis of conjunctival melanoma]. Ann Dermatol Venereol. 2017;144(3):227–9. [DOI] [PubMed] [Google Scholar]
- 33.Vora GK, Demirci H, Marr B, Mruthyunjaya P. Advances in the management of conjunctival melanoma. Surv Ophthalmol. 2017;62(1):26–42. [DOI] [PMC free article] [PubMed] [Google Scholar]


