Abstract
Objective:
Traumatic events (TE) are a risk factor for alcohol use disorder (AUD). Resilience may be protective of the effects of TE exposure, but few studies have longitudinally tested the buffering hypothesis. Thus, the present study aimed to fill this gap.
Method:
Participants (N=6,015) were from a longitudinal investigation into substance use and health outcomes at a large, urban university. Participants completed self-report measures on pre-college internalizing symptoms and lifetime trauma load. Resilience was calculated as a quantitative variable. At each of the follow-up assessments, participants reported on past month consumption, AUD symptoms, and new onset TEs. Longitudinal path modeling was used to test interactions.
Results:
Higher new onset TE load was associated with greater AUD symptoms, and higher consumption at one timepoint.. Results demonstrate a significant main effect of resilience at Y1S and Y3S, and a significant interaction between resilience and new onset TE at the last time-point, whereby higher levels of new onset TE were associated with higher levels of AUD symptoms at low (β=.19, p <.001), and average (β=.20, p =.001) levels of resilience. This effect was attenuated at high levels of resilience (β=.07, p=.051). No significant main nor interaction effects of resilience on consumption were found.
Conclusions:
Findings suggest resilience as an important protective factor in relation to the development of AUD symptoms after exposure to a TE, though perhaps less so in relation to consumption. Findings are consistent with prior work demonstrating that AUD symptoms are more clinically relevant than consumption in this population.
Introduction
College is a time of increased vulnerability for problematic alcohol use and the development of symptoms of alcohol use disorder (AUD). Alcohol use peaks during the college-aged years and decreases to moderate levels in the mid-twenties (Slutske, 2005), although some individuals maintain risky use, and subsequently develop an AUD. College students engage in drinking behaviors more often than their same-aged peers (Slutske et al., 2004), and experience more alcohol-related consequences, with 18% of U.S. college students suffering from clinically significant alcohol-related problems in the past year, as compared to 15% of their non-college attending peers (Slutske et al., 2005). Deleterious outcomes associated with alcohol use on college campuses include academic impairment (e.g., Meda et al. 2017), personal injuries (e.g., Mundt, Zakletskaia, Brown, & Femming, 2012), and physical health symptoms (e.g., Piasecki, Slutske, Wood, & Hunt-Carter, 2010). Thus, research examining protective factors for alcohol use phenotypes across the college experience is needed.
One pathway of risk may be via trauma exposure (TE) which is associated with increased drinking (e.g., through PTSD symptoms; Possemato et al., 2015) and AUD (Russell et al., 2014). Although TE is associated with both consumption and AUD, there is evidence to suggest that increased levels of consumption are normative for college students (e.g., Arria et al., 2016), and as such, AUD symptoms and related problems may warrant more focus. Indeed, psychopathology (e.g., depression, PTSD, etc.) is more closely tied to AUD symptoms/alcohol related problems than consumption (Bulloch, Lavorato, Williams & Patten, 2012; Angkaw et al., 2015) and students who endorse experiencing an interpersonal trauma (IPT) in the first two years of college report greater increases in AUD symptoms during those same two years (Bountress, et al. 2019).
Given these associations, identification of protective factors is critical. Resilience (i.e., resistance to distress following an adverse life experience [e.g., Bonanno, 2004; Connor & Davidson, 2003; Luthar, Cicchetti, & Becker, 2000]) is hypothesized to protect against adverse outcomes following TE. Not surprisingly, given this broad conceptualization of resilience (e.g., Bonanno, 2004; Connor & Davison, 2003; Luthar et al., 2000) the concept has been opertationalized in different ways in the literature. Across this heterogeneous literature, resilience is most commonly operationalized as a trait (Connor & Davidson, 2003), outcome (e.g., lack of PTSD symptoms; Bonanno, 2004), or process (Masten & Naryan, 2012). In contextualizing the variable used in the present study with regards to the most commonly seen conceptualizations of resilience (i.e., trait, outcome, process), discrepancy-based resilience is most similar to a trait-based conceptualization. Resilience in the present study is theorized to be an interpersonal characteristic that has been shown to be both moderately heritable with the genetic and environmental influences stable over time (Amstadter et al., 2014). However, the genetic influences on discrepancy-based resilience do not account for 100% of the phenotype, and thus, the environment plays a critical role in influencing levels of discrepancy-based resilience. Existing research has evidenced the protective effects of resilience whereby those individuals high in resilience, as measured by a self-report measure, remain “unchanged” in terms of depressive, anxiety, and somatic symptoms in the face of adversity (e.g., Poole, Dobson, & Pusch, 2017; Bonanno, Kennedy, Galatzer-Levy, Lude, & Elfstrom, 2012). The buffering hypothesis of resilience is one of the predominant theories used to explain its protective effects against adverse outcomes, postulating that those with higher levels of resilience should experience less symptoms of psychopathology following exposure to adversity than those with lower levels of resilience (e.g., Sheerin et al., 2018).
The majority of the literature on resilience as a protective factor is cross-sectional in nature, and does not test the buffering hypothesis (i.e., moderation analyses). If resilience does truly buffer against the effects of TE, to examine the construct validly, resilience at one time point would be hypothesized to protect an individual against the development of symptoms following future TE, requiring the use of longitudinal data. However, in a recent systematic review of the literature (Cusack & Amstadter, under review) on resilience and alcohol-related phenotypes, only two of 20 studies identified for inclusion employed a longitudinal research design (Green, Beckham, Youssef, & Elbogen, 2014; Wong et al., 2006). These studies demonstrated that lower resilience at baseline was related to a higher likelihood of alcohol misuse one year later (Green et al. 2014), and that children with greater resilience were less likely to begin using alcohol in adolescence (Wong et al., 2006).
The buffering hypothesis necessitates a test of moderation by design. Yet, in the same systematic review of resilience and alcohol phenotypes (Cusack & Amstadter, under review), only two studies tested a true moderation model (Morgan, Brown, and Bray, 2018; Wingo et al. 2014), but using cross-sectional data. Findings demonstrated that resilience does indeed interact with stressors to predict alcohol related problems (Morgan, Brown, & Bray, 2018), and further, resilience interacts with severity of TE to protect against harmful alcohol use (Wingo et al. 2014). However, to date, this work has not tested the influence of new onset TE nor validly tested the buffering hypothesis via moderation.
Lastly, the extant research on resilience largely ignores important contextual variables associated with risk or resilience (e.g., parental monitoring, peer deviance). The literature examining alcohol phenotypes is extensive and has found a variety of risk (e.g., peer deviance [Cambron, Kosterman, Catalano, Gutmannova, & Hawkins, 2017], internalizing symptoms [McCaul, Hutton, Stephens, Xu, & Wand, 2017]) and protective factors (e.g., social support [Reed, Reno, & green, 2016], high parental monitoring [Hodder et al., 2018]) associated with use. Thus, critical contextual factors will be incorporated into the models conducted for the present paper.
Taken together, there is a dearth of literature examining the buffering capabilities of resilience on alcohol-related phenotypes. Additional research testing the buffering hypothesis of resilience, with longitudinal data, on externalizing phenotypes is highly warranted. As such, the primary aim of the present study was to longitudinally examine the buffering effects of a quantitative measure of resilience against AUD symptoms in the wake of college-onset TE, over and above the role of key contextual factors (e.g., trauma related distress, peer deviance, etc.). The secondary aim of the present study was to test this model on alcohol consumption. It is hypothesized that baseline resilience will buffer against the development of AUD symptoms, as a marker of problem use, in the context of college onset TE, while controlling for contextual factors assessed at baseline.
Methods
Participants and recruitment
The sample for the current analyses comes from a larger, ongoing cohort study of college students at a mid-Atlantic public university. Baseline assessment data is collected from first year students 18 years of age or older during their first semester of college. Four cohorts (N=9,989) which matriculated in Fall 2011 (Cohort 1; N=2,707), 2012 (Cohort 2; N=2,481), 2013 (Cohort 3; N=2,391), and 2014 (Cohort 4; N=2,310), have been enrolled and have completed data collection thus far. Those individuals who completed the baseline survey were invited via email to complete subsequent follow-up assessments at spring freshman year, spring sophomore year, spring junior year, and spring senior year (for detailed review of study methods, see Dick et al., 2014). For the present study, two sub-samples were created from the larger parent study. Sub-sample 1 (n=6,015) includes those endorsing lifetime TE and were included in the models predicting alcohol consumption. Sub-sample 2 (n=5,346) includes those endorsing lifetime TE and lifetime alcohol use, and were included in the model predicting AUD symptoms.
Phenotypic assessment measures
All surveys were completed online using the RedCap (Research Electronic Data Capture; Harris, et al. 2019) system, a secure, web-based application designed to support data capture for research studies.
Trauma exposure.
TE was measured by a five-item abbreviated version of the Life Events Checklist (LEC; Gray et al., 2004) that assesses exposure to a range of potentially traumatic events (i.e., natural disaster, sexual assault, physical assault, other unwanted sexual experience, motor vehicle accident) experienced, with a “yes” or “no” response. At the baseline time-point (i.e., year 1 fall), individuals report on lifetime types of traumas experienced before attending college, and for each subsequent time-point (e.g., year 1 spring, year 2 spring, etc.), they report on traumas experienced since the last assessment (i.e., past ~12 month). The TE data was used in two ways. First, for the creation of the resilience variable, a sum score was used to capture the total load of TE experienced before attending college. Second, given the hypothesis that resilience will have a dose-response effect on alcohol outcomes in the wake of new onset TE, a continuous variable capturing the total number of new traumatic events was constructed for each of the four-follow-up time-points.
Internalizing symptoms (used in calculation of resilience score).
Internalizing symptoms were assessed at the baseline time-point using the Symptom Checklist-90 Short Version (SCL-27; Hardt & Gerbershagen, 2001). The assessment included four items to assess depressive symptoms (α = 0.89) and four items to assess anxiety symptoms (α = 0.85) over the past month. Responses were made on a Likert-type scale of 1 (not at all) to 5 (extremely). A sum score was computed, combining both depressive and anxiety symptoms.
Resilience
The quantitative measure of resilience utilized the assessment of lifetime TE at baseline and internalizing symptoms at baseline. An individual’s total score on the SCL-27 was regressed onto their total LEC “lifetime” sum (i.e., year 1 fall total endorsed events). The residual (multiplied by −1 for ease of interpretation such that positive scores represent degree of ‘resilient’ responding and negative scores represent degree of ‘non-resilient’ responding) was used to quantify resilience as the difference between a participant’s actual and expected functioning, based on the SCL sum score and LEC total, where higher scores represent greater levels of resilience. In other words, the smaller the difference between one’s actual symptom score and their expected score based on their trauma load, the more “resilient” they are. Evidence from prior examinations using this measure of resilience supports the variable as a stable, trait-like construct (e.g., Amstadter, Myers, & Kendler, 2014; Amstadter, Maes, Sheerin, Myers, & Kendler, 2016; Sheerin et al., 2018). As such, resilience was measured at the baseline time-point (year 1 fall) upon entry into college. This allows for the valid testing of the buffering hypothesis, in which baseline resilience buffers against subsequent AUD symptoms and alcohol consumption.
Alcohol use and AUD
DSM-5 AUD symptoms (α = .84) were assessed for those individuals that endorsed having ever used alcohol. Symptoms were assessed using items adapted from the Semi-Structured Assessment for the Genetics of Alcoholism (SSGA; Buckholz et al., 1994). An AUD symptom count variable for symptoms met within the past 12 months was created for the present study. Symptoms were assessed at each time-point starting with the first spring follow-up time-point for cohort 1, and through all spring follow-up time-points for cohorts 2–4.
Alcohol consumption (i.e., grams of ethanol consumed/month) was calculated using an existing method (Salvatore et al., 2016) with the alcohol frequency and quantity variables. The frequency and quantity items (past 30 days) were from the AUDIT (Bohn, Babor, & Kranzler, 1995). Alcohol consumption was measured, as a continuous variable, at spring follow-up time points (i.e., year 1 spring, year 2 spring, year 3 spring, and year 4 spring) in order to allow for adequate testing of the buffering hypothesis (i.e., resilience at year 1 fall, new TE at year 1 spring, alcohol consumption at year 1 spring). Prior to transformation, the alcohol consumption variables were both skewed and kurtotic. Following log transformation, both skewness and kurtosis values were significantly improved to acceptable levels as done in previous work (Salvatore et al., 2016).
a. Covariates
To reduce the number of estimated parameters, covariates at baseline were included in predicting TE and alcohol variables at the first time point.
Demographics
Data on participant demographics was drawn from the baseline (year 1 Fall) survey, where participants self-reported on sex, race/ethnicity, and age. Dummy codes were created for the sex and race variables. The creation of these dummy codes allows for comparisons between the following groups: Male vs. female, White vs. African American/Black, White vs. Asian, and White vs. Other as has been done in other work using this data (e.g., Bountress et al., 2019; Cusack et al., 2019).
Trauma Related Distress
If a participant endorsed at least one traumatic event on the LEC or at least one item on a measure of stressful life events (e.g., broken engagement, housing difficulties, etc., Kendler, Karkowski, & Prescott, 1999) at baseline, they were administered a modified version of the Primary Care PTSD Screen for DSM-IV (PC-PTSD; Prins et al. 2016). A dichotomous variable representing the endorsement of at least one of the following: “nightmares, attempts to avoid thoughts or reminders of the potentially traumatic experience, hypervigilance, or feelings of detachment”, where a score greater than 0 is classified as demonstrating trauma related distress, was used in the present study.
Social support
Social support (α = 0.91) was measured at baseline (year 1 fall) using three items from the RAND Medical Outcomes Study Social Support Survey (Hays, Sherbourne, & Mazel, 1995). Items were combined to create a sum score, with higher scores indicating higher social support.
Peer deviance
Peer deviance (α = 0.89) was measured using items from two instruments (e.g., Johnston, Bachman, & O’Malley, 1982; Tarter & Hegedus, 1991) compiled for use together in Kendler et al. (2008). Baseline surveys (year 1 fall) prompted individuals to report on high school friends engagement in substance use and related consequences. Items were reverse coded and compiled to create a sum score, with higher scores indicating higher levels of peer deviance.
Parenting style
Parental involvement was measured at baseline using the Steinberg Parenting Style Index (Steinberg, Lamborn, Dornbusch, & Darling, 1992). Parental involvement (α = 0.68) was assessed with three items assessing parental presence during development, a sum score was computed, after reverse coding items, with higher scores representing higher levels of parental involvement.
Data Analytic Plan
Prior to performing main analyses, distributional properties of all variables were examined to ensure normality. Variables that were not normally distributed were transformed. Continuous variables with skewness and kurtosis values falling outside of acceptable ranges (+/2, +/−7, respectively; George & Mallery, 2016), were log transformed. Alcohol consumption at all timepoints was log transformed. Descriptive statistics and correlations among study variables were then calculated using SPSS 26 software (see tables 1 & 2; SPSS, 2019).
Table 1.
Demographic and Clinical Characteristics of study sub-samples.
| Sub-sample 1 | Sub-sample 2 | |||
|---|---|---|---|---|
| M (SD) | % (n) | M(SD) | % (n) | |
| Age | 18.5 (0.44) | - | 18.5(0.43) | - |
| Sex (female) | - | 64.5% (3,449) | - | 63.5% (3,821) |
| Race (White) | - | 53.7% (2,870) | - | 53.1% (3,199) |
| PTSD | - | 29.0% (1,550) | - | 27.6% (1,663) |
| Parent | 9.58 (2.08) | - | 9.56(2.10) | - |
| Peer | 9.22 (4.97) | - | 8.75 (4.97) | - |
| Social support | 9.49 (2.24) | - | 9.47 (2.25) | - |
| Y1S TE | 0.89 (1.14) | 39.2% (2,098) | 0.88 (1.05) | 38.8% (2,333) |
| Y2S TE | 0.64 (.89) | 21.3% (1,138) | 0.62 (.93) | 19.4% (1,157) |
| Y3S TE | 0.53 (.73) | 14.3% (765) | 0.51 (.84) | 13.2% (792) |
| Y4S TE | 0.53 (.77) | 12.0% (642) | 0.51(.86) | 8.5% (510) |
| Y1S AUD sx | 0.54 (1.21) | - | - | - |
| Y2S AUD sx | 1.07 (1.59) | - | - | - |
| Y3S AUD sx | 1.02 (1.50) | - | - | - |
| Y4S AUD sx | 1.14 (1.64) | - | - | - |
| Y1S Consumption | 1.33(1.36) | - | 1.14(1.45) | - |
| Y2S Consumption | 1.50(1.25) | - | 1.33(1.36) | - |
| Y3S Consumption | 1.77(1.06) | - | 1.63(1.18) | - |
| Y4S Consumption | 1.96(.88) | - | 1.95(.89) | - |
Note. TE =traumatic event; Both means of new onset trauma load and percentage of those endorsing new onset trauma at each spring time-point are represented. Y1= Year 1 spring, Y2= Year 2 Spring, Y3= Year 3 Spring, Y4= Year 4 Spring; Sx=symptoms.
Table 2.
Correlations among Study Variables (n=6015).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19 | 20 | 21 | 22 | 23 | 24 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | -- | |||||||||||||||||||||||
| Sex | .079* | -- | ||||||||||||||||||||||
| Race: Caucasian-African-American | −.066* | −.093* | -- | |||||||||||||||||||||
| Race: Caucasian-Asian | .024 | .025 | −.186* | -- | ||||||||||||||||||||
| 5.Race: Caucasian-Other | −.007 | −.008 | −.190* | −.161* | -- | |||||||||||||||||||
| 6.Parental involvement | −.014 | −.045* | −.018 | −.153* | −.031 | -- | ||||||||||||||||||
| 7.Social support | −.038 | −.031 | −.049 | −.069* | −.021 | .391* | -- | |||||||||||||||||
| 8.Peer deviance | −.015 | .083* | −.136* | −.161* | .040 | −.026 | .006 | -- | ||||||||||||||||
| 9. Trauma related distress | .011 | −.193* | .012 | −.063* | .018 | −.096* | −.142* | .104* | -- | |||||||||||||||
| 10. Resilience-Baseline | .002 | .166* | .071* | −.013 | −.001 | .144* | .264* | −.135* | −.264* | -- | ||||||||||||||
| 11. Consumption - Year 1 Spring | .003 | .098* | −.094* | −.154* | .011 | .005 | .053* | .417* | .042 | −.008 | -- | |||||||||||||
| 12. Consumption-Year 2 Spring | −.024 | .120* | −.076* | −.149 | .024 | −.006 | .062 | .373** | .058 | −.005 | .641* | -- | ||||||||||||
| 13. Consumption-Year 3 Spring | .059 | .110* | −.142* | −.127* | .042 | .037 | .059 | .318* | .057 | −.018 | .529* | .612* | -- | |||||||||||
| 14. Consumption-Year 4 Spring | −.053 | .116* | −.109* | −.110* | .009 | .037 | .092* | .272* | .037 | −.022 | .488* | .515* | .594* | -- | ||||||||||
| 15.AUD symptoms-Year 1 Spring | .024 | .055 | −.046 | −.035 | .008 | −.067 | −.033 | .281* | .078* | −.103* | .266* | .168* | .165* | .206* | -- | |||||||||
| 16. AUD symptoms-Year 2 Spring | −.008 | .056 | −.056 | −.025 | −.017 | −.081* | −.056 | .285* | .033 | −.096* | .278* | .289* | .190* | .230* | .494* | -- | ||||||||
| 17. AUD symptoms-Year 3 Spring | −.019 | .095* | −.091* | −.013 | .005 | −.109* | −.034 | .307* | .085 | −.134* | .310* | .288* | .321* | .274* | .502* | .574* | -- | |||||||
| 18. AUD symptoms-Year 4 Spring | −.041 | .089* | −.049 | −.501 | −.014 | −.036 | −.034 | .261* | .086 | −.131* | .304* | .310* | .313* | .374* | .401* | .507* | .570* | -- | ||||||
| 19. New onset TE-Year 1 Spring | .002 | −.042 | .016 | −.040 | −.012 | −.052 | −.061 | .044 | .127* | −.044 | .064* | .041 | .041 | .019 | .134* | .111* | .095* | .095* | -- | |||||
| 20. New onset TE-Year 2 Spring | .034 | −.074* | −.021 | −.043 | .001 | −.089* | −.067 | .089* | .146* | −.120* | .061 | .044 | .062 | .013 | .095* | .146* | .111* | .075 | .270* | -- | ||||
| 21. New onset TE-Year 3 Spring | −.013 | −.057 | −.007 | −.023 | −.036 | −.057 | −.088* | .068 | .118* | −.085* | .105* | .093* | .059 | .023 | .069 | .096* | .171* | .121* | .140* | .250* | -- | |||
| 22. New onset TE-Year 4 Spring | −.046 | −.064 | −.006 | −.036 | .039 | −.033 | −.089 | .118* | .119* | −.114* | .100* | .097 | .054 | .065 | .064 | .160* | .189* | .221* | .144* | .201* | .288* | -- | ||
| 23. Lifetime trauma load | −.088 | −.073* | .004 | −.036 | .036 | −.123* | −.119* | .153* | .398* | −.094* | .077* | .062 | .027 | .022 | .139* | .118* | .106* | .090* | .229* | .201* | .183* | .160* | -- | |
| 24. Anxiety and depressive symptoms-Baseline | .703 | −.156* | −.071* | .018 | .007 | −.155* | −.272* | .149* | .288* | −.992* | .015 | .017 | .021 | .024 | .121* | .102* | .145* | .145* | .071* | .138* | .099* | .140* | .205* | -- |
Notes:
p<.001
Sex is coded 0 for females and 1 for males; For all Race Variables, Caucasian=0, African-American, Asian, or Other is coded 1.
All continuous predictors were grand mean-centered prior to conducting analyses in order to reduce nonessential multicollinearity and increase interpretability of findings (Cohen, Cohen, West, & Aiken, 2003). Within the study models, a Full Information Maximum Likelihood approach was implemented to utilize all available data among individuals who meet inclusion criteria in MPlus Version 8 (Muthen & Muthen, 2017). For the primary model predicting AUD symptoms, sub-sample two was included, as theoretically, one cannot develop problems related to drinking if they have never consumed alcohol.
The buffering effects of resilience on both AUD symptoms and alcohol consumption was tested within a longitudinal path model framework with moderation using MPlus Version 8 (Muthen & Muthen. 2017). Models were assessed for fit using the following fit statistics: comparative fit index (CFI), Tucker Lewis Index (TLI), root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), suggested as best practice in the field (e.g., Taasoobshirazi & Wang, 2016). Models were deemed as demonstrating “good” fit based on the following metrics: a CFI value of ≥ .90 (e.g., Awang, 2012), a TLI value close to .95 (e.g., Hu & Bentler, 2009), a RMSEA value at or below 0.08 (e.g., MacCullum, Browne, & Sugawara, 1996), and a SRMR value less than .08 (e.g. Hu & Bentler, 1999).
Main effects of covariates measured at baseline (e.g., age, sex, race/ethnicity, trauma related distress, peer deviance, parental involvement) on alcohol use outcomes at the Year 1 Spring (Y1S) follow-up timepoint were assessed. Main effects of new onset TE (Y1, Y2, Y3, Y4 spring timepoints) and baseline resilience on AUD symptoms and alcohol consumption at each time-point were examined.
Next, models examining the interaction effects between new onset TE at each follow-up time point and baseline resilience on alcohol use outcomes were tested. When interaction terms were non-significant, they were removed from models to allow for more accurate interpretation of main effects. Significant interaction terms were probed using simple slope analyses as suggested by Aiken, West, and Reno (1991). Interactions were further probed using the Johnson-Neyman Regions of Significance Method (Rast, Rush, Piccinin, & Hofer, 2014) in order to determine where the association between resilience and alcohol phenotypes becomes significant/non-significant. Given the large sample size, effects were considered significant at p<.01.
Results
Participant Characteristics
The first sub-sample was created (N=5,346) for the model predicting AUD symptoms, including only those endorsing lifetime TE and lifetime alcohol consumption. Clinical and demographic characteristics for this sub-sample at the Y1 fall and Y1S timepoints are presented in Table 1.
A second sub-sample from the larger S4S sample (N=6,015) includes individuals endorsing lifetime TE at the baseline time-point that were included in the model predicting consumption. Clinical and demographic characteristics for this sub-sample at the Y1 fall and Y1S timepoints are presented in Table 1. Notably, differences in clinical and demographic characteristics between the two sub-samples were no larger than a small effect size.
Zero-Order Correlations
Table 2 provides the zero-order Pearson, tetrachoric, and biserial correlations among primary study variables (n= 6,015; second sub-sample). In terms of associations among TE, resilience, and alcohol use outcomes, associations were generally as would be predicted. Specifically, new onset TE was positively correlated with consumption and AUD symptoms at Y1S, and with AUD symptoms at Y2S, Y3S, and Y4S. Resilience was significantly correlated with AUD symptoms at Y1S and Y3S but was not significantly correlated with alcohol consumption at any timepoint.
AUD Symptoms Model (n=5,346)
The model predicting AUD symptoms with covariates included demonstrated adequate to good fit, χ2 (116) = 3307.36, p < .001; RMSEA = 0.03, SRMR= 0.05; CFI = 0.85, and TLI = 0.79. To improve model fit, modification indices were considered, and paths recommended to improve model fit were included (i.e., peer deviance with AUD symptoms at year 2, resilience with year 2 TE). The inclusion of these paths significantly improved model fit, χ2 (96) = 403.59, p < .001; RMSEA = 0.03, SRMR= 0.03; CFI = 0.90, and TLI = 0.85. Path coefficients for this model are presented in Table 3.
Table 3.
Path analysis predicting DSM-5 AUD symptoms and new onset TE (n=5,346).
| AUD Symptoms | New Onset TE | |||||||
|---|---|---|---|---|---|---|---|---|
| Y1S | Y2S | Y3S | Y4S | Y1S | Y2S | Y3S | Y4S | |
| Predictor | B (SE) | B (SE) | B (SE) | B(SE) | B (SE) | B (SE) | B(SE) | B(SE) |
| Sex (Male) | .06(.02)** | -- | -- | -- | −.03(.02) | -- | -- | -- |
| Age | .02(.02) | -- | -- | -- | .00(.02) | -- | -- | -- |
| Race: White versus Black | .00(.02) | -- | -- | -- | .00(.02) | -- | -- | -- |
| Race: White versus Asian | −.01(.02) | -- | -- | -- | −.04(.02) | -- | -- | -- |
| Race: White versus Other | .00(.02) | -- | -- | -- | −.02(.02) | -- | -- | -- |
| PTSD | .03(.02) | -- | -- | -- | .10(.02)** | -- | -- | -- |
| Parent | −.06(.02)* | -- | -- | -- | −.04(.02) | -- | -- | -- |
| Peer | .27(.02)** | -- | -- | -- | .04(.02) | -- | -- | -- |
| Social support | .03(.02) | -- | -- | -- | −.03(.02) | -- | -- | -- |
| Resilience | −.06(.02)** | −.05(.02) | −.07(.02)* | −.03(.02) | 00(.02) | −.45(.05)** | −.06(.02) | −.09(.03)* |
| Y1 TE | .13(.02)** | -- | -- | -- | -- | .26(.02)** | -- | -- |
| Y2 TE | -- | .10(.02)** | -- | -- | -- | -- | .26(.02)** | -- |
| Y3 TE | -- | -- | .12(.02)** | -- | -- | -- | -- | .30(.03)** |
| Y4 TE | -- | -- | -- | .13(.02)** | -- | -- | -- | -- |
| Y4 INTX | -- | -- | -- | −.07(.02)* | -- | -- | -- | -- |
Notes.
p<.01,
p<.001.
B= Standardized regression coefficient. SE= Standard error; Sex: 1=males, 0=females.; Race: 0=White, 1=Blacks, Asians, or Other for each of the three dummy codes. TE= Traumatic event, Peer=Peer deviance, Parent=Parental involvement, PTSD= Probable PTSD, INTX=Interaction term between new onset TE and resilience.
One significant interaction was found between resilience and new onset trauma exposure at Y4S in predicting Y4S DSM-5 AUD symptoms (see Figure 1), whereby higher levels of new onset TE were associated with higher levels of AUD symptoms at both low (β=.19, p <.001), and mean (β=.20, p =.001) levels of resilience, but this effect was attenuated at high levels of resilience (β=.07, p=.051). The effect of TE on AUD symptoms was significant (p<.01) up until 2/5 of one SD above the mean on resilience (see Figure 1). Given the non-significant interaction terms at Y1S, Y2S, and Y3S, main effects were examined in a model without interaction terms. Notably, there were significant main effects of resilience on Y1S and Y3S AUD symptoms, whereby those endorsing higher levels of resilience reported lower AUD symptoms. There were significant main effects of TE on AUD symptoms at Y1S, Y2S, Y3S, and Y4S as well, whereby those reporting higher categories of new onset TE report higher symptoms, as compared to those with less new onset TE (see Table 3).
Figure 1.
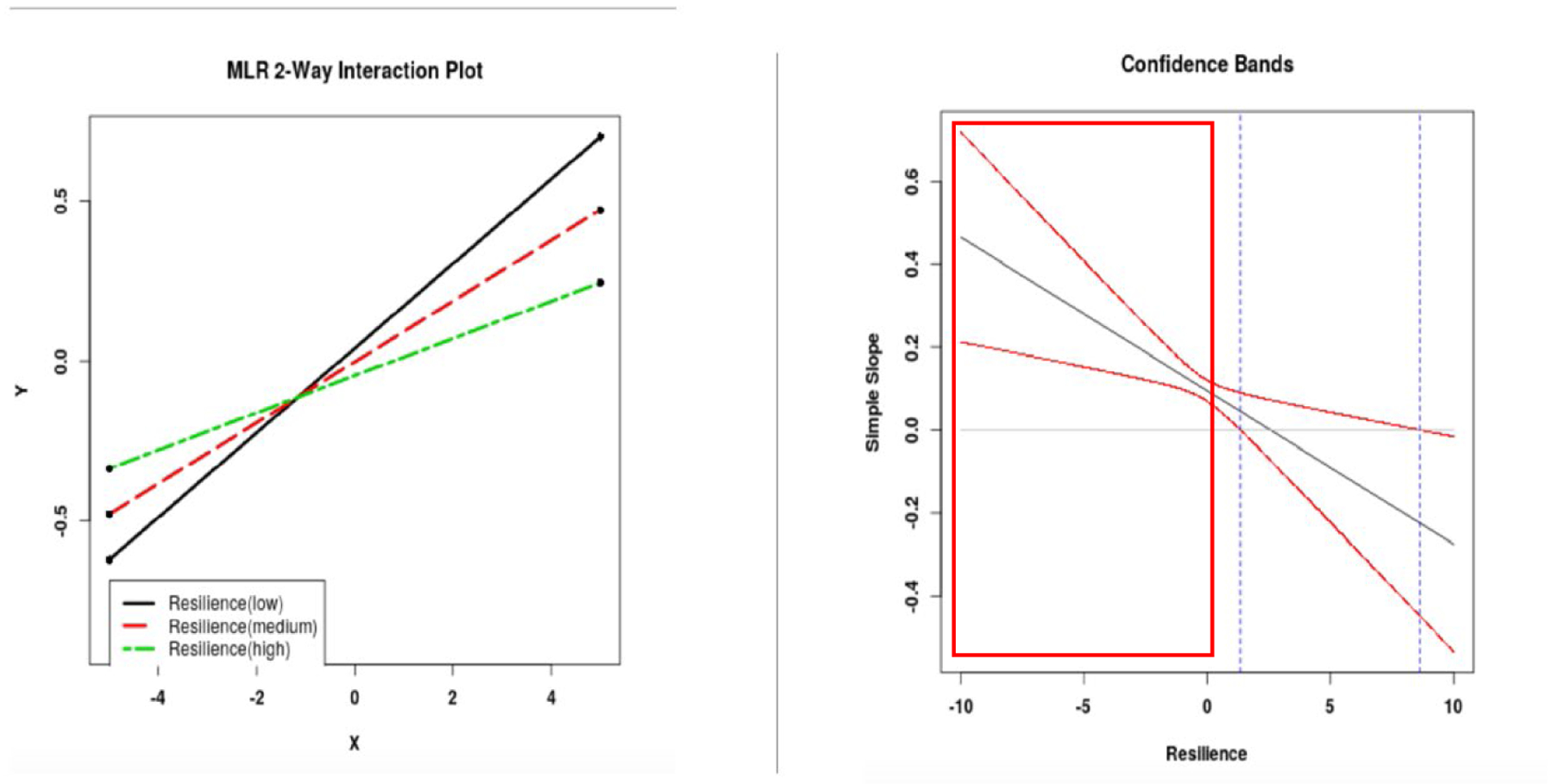
Interaction plot and regions of significance. Note. Regions of significance are presented (p<.01) are presented for the interaction between new onset TE and resilience to predict DSM-5 AUD symptoms. Regression coefficients are nonsignificant at values of the moderator falling within the region (1.4–8.6).
In terms of covariates, sex, peer deviance, and parental involvement all predicted AUD symptoms at Y1S. More specifically, higher levels of peer deviance, lower levels of parental involvement, and male sex were predictive of increased AUD symptoms.
Alcohol Consumption Model (n=6,015)
The path analysis predicting alcohol consumption at each spring follow-up timepoint with covariates included produced a decent to good fitting model, χ2 (98) = 589.9, p < .001, RMSEA = 0.03, SRMR= 0.04; CFI = 0.89, and TLI = 0.85. To improve model fit, modification indices were considered. Paths that were recommended to improve model fit (i.e., peer deviance with year 2 spring consumption, resilience with year 2 spring TE) were incorporated into the model. Including these paths significantly improved model fit, χ2 (99) = 685.9, p < .001, RMSEA = 0.03, SRMR= 0.04; CFI = 0.90, and TLI = 0.86. The path coefficients of this model are presented in Table 4.
Table 4.
Path analysis predicting alcohol consumption and new onset TE (n=6,015).
| Alcohol Consumption | New Onset TE | |||||||
|---|---|---|---|---|---|---|---|---|
| Y1S | Y2S | Y3S | Y4S | Y1S | Y2S | Y3S | Y4S | |
| Predictor | B (SE) | B (SE) | B (SE) | B(SE) | B (SE) | B (SE) | B(SE) | B(SE) |
| Sex (Male) | .04(.01) | -- | -- | -- | −.03(.02) | -- | -- | -- |
| Age | .01(.01) | -- | -- | -- | .01(.01) | -- | -- | -- |
| Race: White versus Black | −.07(.01)** | -- | -- | -- | .00(.02) | -- | -- | -- |
| Race: White versus Asian | −.12(.02)** | -- | -- | -- | −.02(.02) | -- | -- | -- |
| Race: White versus Other | −.03(.10) | -- | -- | -- | −.03(.02) | -- | -- | -- |
| PTSD | .03(.02) | -- | -- | -- | .12(.02)** | -- | -- | -- |
| Parent | −.01(.02) | -- | -- | -- | −.03(.02) | -- | -- | -- |
| Peer | .42(.01)** | -- | -- | -- | .05(.02)* | -- | -- | -- |
| Social support | .05(.02)* | -- | -- | -- | −.03(.00) | -- | -- | -- |
| Resilience | .02(.02) | −.02(.01) | −.01(.02) | −.02(.02) | .02(.02) | −.12(.02)** | −.06(.02)* | −.09(.03)* |
| Y1 TE | .05(.01)* | -- | -- | -- | -- | .28(.02)** | -- | -- |
| Y2 TE | -- | .01(.01) | -- | -- | -- | -- | .26(.02)** | -- |
| Y3 TE | -- | -- | .0(.02) | -- | -- | -- | -- | .30(.03)** |
| Y4 TE | -- | -- | -- | −.02(.02) | -- | -- | -- | -- |
Notes.
p<.01,
p<.001.
B= Standardized regression coefficient. SE= Standard error; Sex: 1=males, 0=females.; Race: 0=White, 1=Blacks, Asians, or Other for each of the three dummy codes. TE= Traumatic event, Peer=Peer deviance, Parent=Parental involvement, PTSD= Probable PTSD, INTX=Y4 Interaction term between new onset TE and resilience.
No significant interaction effects between baseline resilience and new onset TE on alcohol consumption were found for any time-point. Given the non-significant interactions, interaction terms were removed for supplementary analyses aimed at examining main effects of resilience and new onset TE on alcohol consumption. Results demonstrate no main effect of resilience on alcohol consumption levels. Above and beyond key covariates, there was one significant main effect of Y1 new onset TE on Y1 alcohol consumption, whereby those reporting higher levels of TE endorse consuming more alcohol (see Table 4 for full model results).
A number of covariates were significant predictors of alcohol consumption at Y1S. Identifying as white, as compared to Black/African or Asian, was associated with higher levels of alcohol consumption. Both social support and peer deviance as contextual factors also significantly predicted alcohol consumption levels whereby higher levels of peer deviance were associated with increased consumption, and interestingly, higher levels of social support were associated with increased consumption as well.
Discussion
The aim of the present study was to examine the “buffering” effect of resilience on alcohol use phenotypes (AUD symptoms, consumption), in the context of new TE experienced over the course of college. Resilience, in this case conceptualized as a combination of both an interpersonal characteristic and an outcome, can be a powerful explanatory construct when viewed in connection with dynamic processes (Mischel, 2004), such as new onset TE. Rigorous investigations of resilience as a buffer necessitates longitudinal data to determine whether resilience increases the threshold at which individuals react to TE. As such, findings from the present study meaningfully contribute to the extant resilience literature, suggesting that resilience buffers AUD symptoms, but not consumption, against new onset stressors over time.
The main effect of TE over time for both AUD symptoms consistently (Y1S, Y2S, Y3S, Y4S) and alcohol consumption at baseline (Y1S) supports the relevance of TE as a risk factor for alcohol outcomes. Resilience exerted both a main effect (Y1S, Y3S) and interaction effect (Y4S) on AUD symptoms, but not on levels of consumption. The main effect of resilience on AUD symptoms is consistent with the prior literature that demonstrates resilience as being negatively related to alcohol phenotypes, such as number of related problems (Weiland et al., 2012), AUD diagnostic status (Long et al., 2017), and lifetime consumption (Alvarez-Aguirre, Alonso-Castillo, & Zanetti, 2014), though these studies are largely cross-sectional in nature. In line with hypotheses, evidence of a buffering effect was found for AUD symptoms, whereby increased TE led to more AUD symptoms at low and mean levels of resilience, but not at high levels of resilience, highlighting resilience as a key protective factor. This is consistent with prior research that has found that resilience interacts with number of stressors to predict alcohol related outcomes (Morgan, Brown, & Bray, 2018). Our pattern of findings suggests that resilience does not buffer the impact of TE on AUD symptoms until the end of college (Y4S), and at that point, high levels of resilience are required to impact symptoms, suggesting a pervasive effect of TE on AUD symptoms in college students, and that resilience may have an enduring impact. Increased TE led to more AUD symptoms for those less than 1.4 SD above the mean on resilience, suggesting that high levels of resilience is needed to protect against AUD symptoms.
The different patterns of findings with regard to AUD symptoms as compared to alcohol consumption is an important discrepancy to consider with regard to the clinical implications of resilience as it relates to alcohol outcomes. College is a developmentally normative time for alcohol consumption, with epidemiologic studies suggesting that drinking increases during adolescence and reaches a peak during young adulthood, specifically through the early 20s (Jackson, Sher, & Park, 2006). However, while some individuals do not reduce their drinking and subsequently develop related problems, most do not develop symptoms of AUD, and as such, not all consumption in college students is problematic. Consistent with this, our findings suggest resilience as an important protective factor against clinically relevant AUD symptoms, as opposed to consumption levels, which may not be clinically meaningful for every student. Indeed, prior literature has demonstrated that the escalation of drinking across college is a more potent long-term indicator of future problems, as compared to consumption levels alone (Prince, Read, & Colder, 2019), further highlighting the clinical importance of resilience in relation to AUD symptoms as opposed to consumption level.
The nuance between alcohol consumption and related problems has important implications for prevention efforts in adolescents prior to entering college, or during the early years of college. The present paper conceptualizes resilience as a modifiable but inherent characteristic given that prior literature has shown it to be relatively stable over time, but that it is ~50% influenced by environment, suggesting that environmental sources may “dial up” or “dial down” one’s resilience (e.g., Amstadter et al., 2014). As such, findings from the present study highlight the need to implement prevention efforts aimed at reducing risk for TE (a key environmental variable) in earlier years. Existing treatment literature suggests that increased resilience is associated with positive treatment outcomes for comorbid PTSD and substance use disorders (McGuire, Mota, Sippel, Connolly, & Lyons, 2018). School-based interventions aimed at targeting resilience to reduce substance use outcomes have had mixed results, with some studies showing decreased prevalence of alcohol use one year later (Hodder, Daly, Freund, Bowman, Hazell, & Wiggers, 2011), though a meta-analysis of 19 studies found no impact on alcohol use (Hodder et al. 2017). This work, however, is primarily with adolescents in high school settings, and considerations for adapting to first-year college orientation efforts or targeting for those at greater risk upon entry to college, would be useful.
The extant literature examining the impact of resilience on alcohol use outcomes largely ignores contextual factors such as peer and family influences that influence substance use outcomes and tend to interact in important ways. For example, Mahedy et al. (2018) found that young adults whose parents have moderate or high-risk alcohol consumption are more likely to consume alcohol than those with parents with lower consumption, but this relationship was partly accounted for by higher prevalence of association with peer deviance. Alternatively, parental support and distancing moderates the effects of peer influence on adolescent alcohol use (Marshal & Chassin, 2000). Indeed, findings from the present study demonstrate that parental involvement is negatively related to AUD symptoms. Secondly, we found that higher levels of peer deviance and higher levels of social support predicted higher alcohol consumption. Although social support is largely suggested as a protective factor throughout the extant literature (e.g., Gros, et al., 2016; Kahle, Veliz, McCabe, & Boyd, 2019), it may be that students with increased social interaction and contacts are in settings where alcohol consumption is occurring more often. Our findings, taken together with extant research, highlight low affiliation with deviant peers in high school as a potential protective factor against the development of AUD symptoms. Such factors may be more relevant for substance use or initiation, whereas resilience processes may be more relevant for the development of symptoms subsequent to use.
Limitations and Future Directions
Although the present study makes important contributions to the field of resilience research, findings should be considered in the context of a number of limitations. First, the parent study from which data was used (S4S) prioritizes breadth over depth in terms of assessment measures. As such, future research should employ more detailed measures of trauma exposure, internalizing symptoms (for calculation of the resilience variable), alcohol use, and related problems to expand upon findings of the present study. For example, the parent study only includes one question assessing “probable PTSD”, which is not consistent with best practice. Indeed, it is well known that PTSD is an important co-variate that influences alcohol consumption following TE and so a more thorough assessment of the construct as a covariate would allow for a more comprehensive interpretation of findings. Additionally, this study examined resilience as a stable trait, measured at one time point; future work would benefit from examining resilience from a systems, or dynamic perspective as well. Adding a self-report measure of trait or coping-based resilience would allow for comparison to help elucidate different patterns of association between perceived coping and objective measures.
Secondly, the present study uses a college student sample which may limit generalizability. However, the present sample is not a convenience sample, and as such, is less like a “traditional” college population. Virginia Commonwealth University (VCU) students, as compared to more “traditional” college samples that are often seen in psychology research are more diverse, more likely to be a first-generation college student, etc., increasing generalizability. The use of a college student population may also be noted as a limitation as related to the examination of AUD symptoms given that the age of participant precedes the typical age of onset of AUD. However, there was sufficient prevalence and variability in symptoms, likely capturing early risk before full development.
Lastly, all assessments were self-report in nature, introducing sources of potential bias that are commonly seen in self-report measurement tools such as social desirability biases, whereby people respond in a way that they believe will be viewed favorably. Questions regarding alcohol use, particularly in students under the age of 21, are especially vulnerable to this response bias.
Conclusions
The present study sought to extend the extant literature on resilience through examining its association with alcohol use outcomes using a longitudinal framework to rigorously test the buffering hypothesis. Findings further support the relevance of TE on increased alcohol consumption and AUD symptoms. However, findings were mixed with regard to main and interaction effects, demonstrating main and interaction effects for later AUD symptoms, but not alcohol consumption; thus, demonstrating evidence of a buffering effect against new onset TE on problematic alcohol use and symptoms only. Resilience represents an important target for intervention and prevention efforts aimed at protecting against problematic alcohol use outcomes, as well as TE during the college years.
Clinical Impact Statement:
The present study shows that psychiatric resilience is an important protective factor against the development of AUD symptoms after trauma exposure during the college years. Prevention and intervention efforts should thus focus on preventing college onset trauma exposure, and enhancing levels of resilience to protect against alcohol misuse.
Acknowledgments
Spit for Science has been supported by Virginia Commonwealth University, P20 AA017828, R37AA011408, K02AA018755, P50 AA022537, and K01AA024152 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. This research was also supported by the National Institute on Drug Abuse (NIDA) of the National Institutes of Health (NIH) under Award Number U54DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA. Data from this study are available to qualified researchers via dbGaP (phs001754.v2.p1). We would like to thank the Spit for Science participants for making this study a success, as well as the many University faculty, students, and staff who contributed to the design and implementation of the project. Preparation of this manuscript was supported in part by grant NIAAA F31 AA027703-02 (Cusack). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- Aiken LS, West SG, & Reno RR (1991). Multiple regression: Testing and interpreting interactions. sage. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Amstadter AB, Maes HH, Sheerin CM, Myers JM, & Kendler KS (2016). The relationship between genetic and environmental influences on resilience and on common internalizing and externalizing psychiatric disorders. Social psychiatry and psychiatric epidemiology, 51(5), 669–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Myers JM, & Kendler KS (2014). Psychiatric resilience: longitudinal twin study. The British Journal of Psychiatry, 205(4), 275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam E, Kessler R, McLaughlin K, Ruscio A, … Koenen K (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. doi: 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Pérez-Fuentes G, Okuda M, & Wang S (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and alcohol dependence, 132(3), 630–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, & Kranzler HR (1995). The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. Journal of studies on alcohol, 56(4), 423–432. [DOI] [PubMed] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American psychologist, 59(1), 20. [DOI] [PubMed] [Google Scholar]
- Connor KM, & Davidson JR (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and anxiety, 18(2), 76–82. [DOI] [PubMed] [Google Scholar]
- Cusack SE, & Amstadter AB Resilience and alcohol use across the lifespan: a systematic review. Manuscript under review. [Google Scholar]
- Dick D, Nasim A, Edwards AC, Salvatore J, Cho SB, Adkins A, … & Goyal N. (2014). Spit for Science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Frontiers in genetics, 5, 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, & Williams TJ (2014). Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. The American Journal of Drug and Alcohol Abuse, 40(2), 125–130. [DOI] [PubMed] [Google Scholar]
- Green KT, Beckham JC, Youssef N, & Elbogen EB (2014). Alcohol misuse and psychological resilience among US Iraq and Afghanistan era veterans. Addictive behaviors, 39(2), 406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the life events checklist. Assessment, 11(4), 330–341. [DOI] [PubMed] [Google Scholar]
- Hardt J, & Gerbershagen HU (2001). Cross-validation of the SCL-27: A short psychometric screening instrument for chronic pain patients. European Journal of Pain, 5(2), 187–197. [DOI] [PubMed] [Google Scholar]
- Hays RD, Sherbourne CD, & Mazel RM (1995). User’s manual for the Medical Outcomes Study (MOS) core measures of health-related quality of life. Santa Monica: Rand Corporation. [Google Scholar]
- Hawn SE, Bountress KE, Sheerin CM, Dick DM, & Amstadter AB (2020). Trauma-related drinking to cope: A novel approach to the self-medication model. Psychology of addictive behaviors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjemdal O, Friborg O, Stiles TC, Rosenvinge JH, & Martinussen M (2006). Resilience predicting psychiatric symptoms: A prospective study of protective factors and their role in adjustment to stressful life events. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 13(3), 194–201. [Google Scholar]
- Hodder RK, Campbell E, Gilligan C, Lee H, Lecathelinais C, Green S, … & Wiggers J (2018). Association between Australian adolescent alcohol use and alcohol use risk and protective factors in 2011 and 2014. Drug and alcohol review, 37, S22–S33. [DOI] [PubMed] [Google Scholar]
- Hodder RK, Freund M, Bowman J, Wolfenden L, Gillham K, Dray J, & Wiggers J (2016). Association between adolescent tobacco, alcohol and illicit drug use and individual and environmental resilience protective factors. BMJ open, 6(11), e012688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, & Park A (2006). Drinking among College Students: Consumption and Consequences. [DOI] [PubMed]
- Johnston LD, Bachman JG, O’Malley PM, & Schulenberg JE (2009). Monitoring the Future: A Continuing Study of American Youth (12th-Grade Survey), 2008. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 11–23. [Google Scholar]
- Johnston L, Bachman JG, & O’Malley PM (1982). Student drug use, attitudes, and beliefs: national trends, 1975–1982. National Institute on Drug Abuse, US Department of Health and Human Services, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration. [Google Scholar]
- Kendler KS, Karkowski LM, & Prescott CA (1999). Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatric, 156(6), 837–841. [DOI] [PubMed] [Google Scholar]
- Logue MW, Baldwin C, Guffanti G, Melista E, Wolf EJ, Reardon AF, Uddin M, Wildman D, Galea S, Koenen KC, & Miler MW (2013). A genome-wide association study of post-traumatic stress disorder identifies the retinoid-related orphan receptor alpha (RORA) gene as a significant risk locus. Molecular Psychiatry, 18(8), 937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child development, 71(3), 543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological methods, 1(2), 130. [Google Scholar]
- Mahedy L, MacArthur GJ, Hammerton G, Edwards AC, Kendler KS, Macleod J, … & Heron J (2018). The effect of parental drinking on alcohol use in young adults: the mediating role of parental monitoring and peer deviance. Addiction, 113(11), 2041–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, & Chassin L (2000). Peer influence on adolescent alcohol use: The moderating role of parental support and discipline. Applied developmental science, 4(2), 80–88. [Google Scholar]
- McGuire AP, Mota NP, Sippel LM, Connolly KM, & Lyons JA (2018). Increased resilience is associated with positive treatment outcomes for veterans with comorbid PTSD and substance use disorders. Journal of dual diagnosis, 14(3), 181–186. [DOI] [PubMed] [Google Scholar]
- Meda SA, Gueorguieva RV, Pittman B, Rosen RR, Aslanzadeh F, Tennen H, … & Austad CS (2017). Longitudinal influence of alcohol and marijuana use on academic performance in college students. PLoS One, 12(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mischel W (2004). Toward an integrative science of the person. Annu. Rev. Psychol, 55, 1–22. [DOI] [PubMed] [Google Scholar]
- Morgan JK, Brown J, & Bray RM (2018). Resilience as a moderating factor between stress and alcohol-related consequences in the Army National Guard. Addictive behaviors, 80, 22–27. [DOI] [PubMed] [Google Scholar]
- Mundt MP, Zakletskaia LI, Brown DD, & Fleming MF (2012). Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Injury prevention, 18(1), 44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus: Statistical Analysis with Latent Variables: User’s Guide (Version 8). Los Angeles, CA: Authors. [Google Scholar]
- Norman SB, Haller M, Hamblen JL, Southwick SM, & Pietrzak RH (2018). The burden of co-occurring alcohol use disorder and PTSD in U.S. military veterans: comorbidities, functioning, and suicidality. Psychology of Addictive Behaviors, 32(2), 224–229. [DOI] [PubMed] [Google Scholar]
- Ong AD, Bergeman CS, Bisconti TL, & Wallace KA (2006). Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of personality and social psychology, 91(4), 730. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Evans-Polce RJ, & Schulenberg JE (2020). Negative alcohol-related consequences experienced by young adults in the past 12 months: Differences by college attendance, living situation, binge drinking, and sex. Addictive behaviors, 105, 106320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Slutske WS, Wood PK, & Hunt-Carter EE (2010). Frequency and correlates of diary-measured hangoverlike experiences in a college sample. Psychology of addictive behaviors, 24(1), 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, … & Tiet QQ (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, & Farrow S (2011). Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy, 3(2), 148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed D, Reno J, & Green D (2016). Sexual violence among youth in New Mexico. Family & community health, 39(2), 92–102. [DOI] [PubMed] [Google Scholar]
- Rojas SM, Bujarski S, Babson KA, Dutton CE, & Feldner MT (2014). Understanding PTSD comorbidity and suicidal behavior: associations among histories of alcohol dependence, major depressive disorder, and suicidal ideation and attempts. Journal of anxiety disorders, 28(3), 318–325. [DOI] [PubMed] [Google Scholar]
- Salvatore JE, Aliev F, Edwards AC, Evans DM, Macleod J, Hickman M, … & Latvala A (2014). Polygenic scores predict alcohol problems in an independent sample and show moderation by the environment. Genes, 5(2), 330–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, & Amstadter AB (2018). The impact of resilience and subsequent stressful life events on MDD and GAD. Depression and anxiety, 35(2), 140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Batien BD, & Wray TB (2010). Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive behaviors, 35(12), 1045–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS (2005). Alcohol use disorders among US college students and their non–college-attending peers. Archives of general psychiatry, 62(3), 321–327. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Hunt-Carter EE, Nabors-Oberg RE, Sher KJ, Bucholz KK, Madden PA, … & Heath AC (2004). Do college students drink more than their non-college-attending peers? Evidence from a population-based longitudinal female twin study. Journal of abnormal psychology, 113(4), 530. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Lamborn SD, Dornbusch SM, & Darling N (1992). Impact of parenting practices on adolescent achievement: Authoritative parenting, school involvement, and encouragement to succeed. Child development, 63(5), 1266–1281. [DOI] [PubMed] [Google Scholar]
- Tarter RE, & Hegedus AM (1991). The drug use screening inventory. Alcohol Research, 15(1), 65. [Google Scholar]
- Taasoobshirazi G, & Wang S (2016). The performance of the SRMR, RMSEA, CFI, and TLI: An examination of sample size, path size, and degrees of freedom. Journal of Applied Quantitative Methods, 11(3), 31–39. [Google Scholar]
- Temmen CD, & Crockett LJ (2019). Relations of Stress and Drinking Motives to Young Adult Alcohol Misuse: Variations by Gender. Journal of Youth and Adolescence, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo AP, Ressler KJ, & Bradley B (2014). Resilience characteristics mitigate tendency for harmful alcohol and illicit drug use in adults with a history of childhood abuse: A cross-sectional study of 2024 inner-city men and women. Journal of psychiatric research, 51, 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Nigg JT, Zucker RA, Puttler LI, Fitzgerald HE, Jester JM, … Adams K (2006). Behavioral control and resiliency in the onset of alcohol and illicit drug use: a prospective study from preschool to adolescence. Child Dev, 77(4), 1016–1033. doi: 10.1111/j.1467-8624.2006.00916.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veal ML, & Thomson RL (2006). Gender, alcohol consumption, and parental monitoring. The Journal of Psychology: Interdisciplinary and Applied, 140(1), 41–52. [DOI] [PubMed] [Google Scholar]


