SUMMARY
The 2012 West Nile virus (WNV) epidemic was the largest since 2003 and the North Texas region was the most heavily impacted. We conducted a serosurvey of blood donors from four counties in the Dallas–Fort Worth area to characterize the epidemic. Blood donor specimens collected in November 2012 were tested for WNV-specific antibodies. Donors positive for WNV-specific IgG, IgM, and neutralizing antibodies were considered to have been infected in 2012. This number was adjusted using a multi-step process that accounted for timing of IgM seroreversion determined from previous longitudinal studies of WNV-infected donors. Of 4971 donations screened, 139 (2·8%) were confirmed WNV IgG positive, and 69 (1·4%) had IgM indicating infection in 2012. After adjusting for timing of sampling and potential seroreversion, we estimated that 1·8% [95% confidence interval (CI) 1·5–2·2] of the adult population in the Dallas–Fort Worth area were infected during 2012. The resulting overall estimate for the ratio of infections to reported WNV neuroinvasive disease (WNND) cases was 238:1 (95% CI 192–290), with significantly increased risk of WNND in older age groups. These findings were very similar to previous estimates of infections per WNND case, indicating no change in virulence as WNV evolved into an endemic infection in the United States.
Key words: Blood transfusion-associated infections, incidence, West Nile virus
INTRODUCTION
West Nile virus (WNV) is the leading cause of arboviral encephalitis in the United States [1]. The virus is now endemic throughout most of the contiguous United States, with the central and northern Great Plains states having the highest incidence [2–5]. A large WNV epidemic occurred in 2012, with 2873 cases of West Nile virus neuroinvasive disease (WNND; encephalitis, meningitis, acute flaccid paralysis) reported nationwide. Nearly one third (844) of these cases occurred in Texas, of which 356 originated from four counties (Collin, Dallas, Denton, Tarrant) in the Dallas–Fort Worth metropolitan area. This figure exceeded the 332 WNND cases recorded in those four counties from 2002 to 2011.
Since fewer than 1% of persons infected with WNV develop WNND [4, 6], the number of WNND cases reported to CDC's ArboNET surveillance system represent a small fraction of the true number of people infected. Based on a seroprevalence survey in New York after the 1999 epidemic, Mostashari et al. [6] estimated that there were 140 infections for each reported case of WNND. Subsequently, Lindsey et al. [3] multiplied the cumulative number of reported WNND cases by this ratio to estimate a 20–34% cumulative attack rate through 2006 in the highest endemic counties of North Dakota and South Dakota. However, a large serosurvey of blood donors in North Dakota indicated that only 8·2% had WNV IgG in late 2008 and estimated that as many as 244 infections may occur for each reported WNND case [4, 7]. Using these data and reported WNND cases, Petersen et al. estimated that over 3 million WNV infections and 780 000 illnesses had occurred in the United States from 1999 to 2010 [5].
We conducted a serosurvey of blood donors in the four-county Dallas–Fort Worth metropolitan area following the 2012 epidemic to estimate WNV infection incidence in the general population and to estimate the ratio of infections to reported neuroinvasive disease cases, both overall and by age and gender subgroups. The survey methodology also permitted an assessment of the proportion of the population previously exposed to related flaviviruses such as dengue and the St Louis encephalitis viruses.
MATERIALS AND METHODS
Study population
Residual plasma specimens from 5000 sequential volunteer blood donors residing in the four-county area (as determined by postal code of residence) that were submitted to Creative Testing Solutions (CTS) for routine screening were retained and frozen. Dates of blood collection ranged from 4 to 16 November 2012. Plasma samples were coded to retain linkage to week of donation, county of residence, age, gender and race-ethnicity. Thirty-nine donors were determined to live outside the four-county area; thus, 4971 specimens comprised the final sample.
Flavivirus testing and interpretation
The samples were initially tested for WNV IgG antibodies using an enzyme-linked immunoassay (ELISA) established at CDC's Arbovirus Reference Laboratory in Fort Collins, CO [8]. Samples with a positive-to-negative (P/N) ratio ⩾2·0 were tested with a WNV IgM antibody capture ELISA (WNV MAC-ELISA) and for neutralizing antibodies to the West Nile, St Louis encephalitis virus (SLEV), and dengue virus type 1 (DENV-1) using a 90% plaque reduction neutralization test (PRNT) with Vero cells [9]. PRNT titres ⩾10 were considered positive. A fourfold or greater PRNT titre to one virus than to the other tested flaviviruses was considered specific for a given flavivirus. Samples positive by WNV IgG ELISA and negative by WNV, SLEV, and DENV-1 PRNT or that yielded equivocal results on PRNT were further tested by PRNT for neutralizing antibodies to yellow fever virus (YFV) and Japanese encephalitis virus (JEV).
Samples negative by WNV IgG ELISA were considered indicative of no previous flavivirus exposure [8, 10, 11]. Samples positive by IgG ELISA and determined to have virus-specific antibodies by PRNT were considered indicative of previous exposure to that virus. All other WNV IgG ELISA-reactive samples were considered to have indeterminate results. Samples with WNV-specific neutralizing antibodies and a positive WNV MAC-ELISA (P/N ratio ⩾2·0) result were considered indicative of acute WNV infection in 2012 [5, 12]. Although WNV IgM antibody persists for more than 1 year in approximately 10% of acutely infected persons, only one reported WNND case was reported in the four counties in the previous 2 years; thus, the presence of WNV IgM antibodies was considered indicative of infection in 2012.
Statistical analyses
Rates of WNV IgG and IgM and other flavivirus IgG seropositivity (confirmed by PRNTs) were computed for demographic subcategories and compared using SAS v. 9.3 for Windows (SAS Institute Inc., USA) and R (www.r-project.org).
The proportion of blood donors infected with WNV during the 2012 epidemic season was estimated from the proportion who were WNV IgM-antibody positive, as explained above. However, this proportion was likely an underestimate of the true proportion infected in 2012 because some persons would have IgM-seroreverted between the time of infection and sample collection. Thus, a five-step process was employed to estimate the expected number and 95% confidence interval (CI) of donors infected during the 2012 outbreak.
First, we used the observed WNND case surveillance data from the four-county area to estimate the trend in WNV infections in the population over time by computing a smoothed estimate of the epidemic curve using kernel density estimation. Second, using data from an independent follow-up study of viraemic blood donors identified during routine blood screening [13, 14], we estimated the profile of IgM response over time by fitting a regression of log (IgM index) over time to the IgM index measurements using a penalized spline accounting for the repeated measurements on individuals [15–17]. The time-dependent probability of IgM positivity (IgM index >1·1) was computed from this penalized spline fit assuming normality with mean given by the estimated mean curve and estimated variance from the fit. Third, we estimated the proportion of infections in the population over time by convoluting the WNV infection trend curve and the IgM positivity curve. The fourth step was to form the ratio of the curve estimating the proportion of infections in the population over time to the proportion of total cases accumulated over time to estimate what proportion of population cases were expected to have seroreverted. This provided a time-dependent inflation factor curve to be applied to the observed number of IgM-positives collected at any point during and after the outbreak. The fifth and final step was to apply these inflation factors to the number of donors in each week of the donor survey to estimate the number of the donors expected to have been infected during the outbreak. Dividing this by the number of donors provided an estimate of the cumulative population WNV infection incidence, assuming the donors in the survey represent the population with respect to WNV infection.
The estimate of the number of infected persons was then derived by multiplying the estimated infection incidence by population estimates for persons aged ⩾16 years in the four-county area. Under the assumption that blood donors represent the general population with respect to WNV exposure, we estimated the infection-to-WNND case ratio by dividing the estimated number of WNV infections by the reported number of WNND cases, overall and by demographic subgroups. CIs for these ratios were computed by scaling the CIs for the prevalences, following Carson et al. [4]. We then compared the infection-to-WNND case ratios derived from this study with ratios derived from the serosurvey by Carson et al., and calculated ratios of these two ratios. CIs for the ratios of the infection-to-WNND case ratios between the results from Texas and those from North Dakota [4] were computed using methods in Gart & Nam [18].
Ninety-five percent CIs for all curves and parameters were computed by bootstrap resampling and using the empirical confidence limits. These latter analyses and graphics were performed in the R statistical software package [19].
Ethical standards
Routine informed consent for blood donation was obtained at the time of donation. This included authorization for testing for WNV and other transfusion-transmitted infectious diseases, as required of all blood donors, and information related to the potential use of samples and demographic information for research purposes. This study evaluated pre-existing samples anonymized to eliminate the possibility of linkage to individual persons. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
RESULTS
Serosurvey results
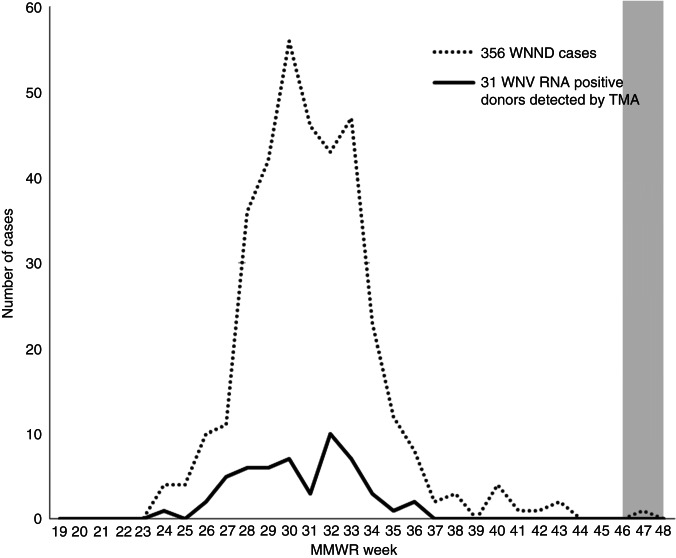
The WNV outbreak in the four-county area, as demonstrated by WNND cases plotted by date of symptom onset and WNV RNA+ blood donors plotted by dates of donation, peaked in the last 2 weeks of July 2012, well before sample collection in November (Fig. 1). Of the 4971 blood donors included in the survey, serological testing indicated that 139 (2·8%) had previous exposure to WNV, 98 (2·0%) to DENV (Table 1). Thirteen (0·3%) had previous exposure to YFV, nine (0·2%) to SLEV, and one to JEV (data not shown). Eleven samples yielded equivocal results. Of the 139 donors previously exposed to WNV, 138 were tested by WNV MAC-ELISA (one sample had insufficient quantity for testing). Of these 138, 69 (50%, 1·4% of total sample) were positive by WNV MAC-ELISA, indicating infection in 2012 (Table 1). In comparison, 52% of the 688 WNNV cases ever reported in the four counties were reported in 2012 [1].
Fig. 1.
Number of reported WNV neuroinvasive disease (WNND) cases by week of symptom onset from 12 May (beginning of week 19) to 7 December (end of week 48), 2012; Collin, Dallas, Denton and Tarrant counties. The grey bar indicates the timing of the serosurvey sample collection period. MMWR, Morbidity and Mortality Weekly Report (http://www.cdc.gov/mmwr/index.html); TMA, transcription-mediated amplification.
Table 1.
Proportion of persons with serological evidence of previous WNV exposure (WNV IgG+) and with evidence of infection in 2012 (WNV IgG+ and IgM+) and dengue exposure (DENV PRNT+), by race/ethnicity, gender, age, and county of residence
| Variable/group | Total (N = 4971) | WNV exposure 2002–2012 (N = 139) (2·8%) | WNV exposure in 2012 (N = 69) (1·4%) | Dengue exposure (N = 98) (2·0%) |
|---|---|---|---|---|
| Age, years | ||||
| 16–24 | 621 | 9 (1·4) | 4 (0·6) | 11 (1·8) |
| 25–44 | 1618 | 40 (2·5) | 21 (1·3) | 64 (4·0) |
| 45–64 | 2237 | 70 (3·1) | 35 (1·6) | 22 (1·0) |
| >65 | 495 | 20 (4·0) | 9 (1·8) | 1 (0·2) |
| Gender | ||||
| Female | 2240 | 55 (2·5) | 30 (1·3) | 28 (1·3) |
| Male | 2731 | 84 (3·1) | 39 (1·4) | 70 (2·6) |
| Race/ethnicity | ||||
| Asian | 174 | 0 | 0 (0·0) | 44 (25·3) |
| Black | 220 | 4 (1·8) | 1 (0·5) | 1 (0·5) |
| Caucasian | 3726 | 109 (2·9) | 56 (1·5) | 7 (0·2) |
| Hispanic | 654 | 19 (2·9) | 11 (1·7) | 31 (4·7) |
| Mixed | 30 | 2 (6·7) | 1 (3·3) | 1 (3·3) |
| Unknown | 107 | 2 (1·9) | 1 (0·9) | 7 (6·5) |
| Other | 60 | 3 (5·0) | 0 | 7 (11·7) |
| County | ||||
| Collin | 900 | 18 (2·0) | 9 (1·0) | 17 (1·9) |
| Dallas | 1601 | 51 (3·2) | 27 (1·7) | 39 (2·4) |
| Denton | 703 | 24 (3·4) | 8 (1·1) | 21 (3·0) |
| Tarrant | 1767 | 46 (2·6) | 25 (1·4) | 21 (1·2) |
Previous exposure to WNV was related to increasing age (P = 0·004, χ2 for linear trend), but did not significantly vary by gender, race/ethnicity, or county of residence (Table 1). Similarly, older persons tended to have higher exposure to WNV in 2012 (P = 0·06, χ2 for linear trend), but recent exposure did not vary significantly by gender, race/ethnicity, or county of residence (Table 1).
Ninety-eight (2%) of the 4971 donors had serological evidence of previous DENV infection; however, 44 (45%) of these were Asians and 31 (32%) were Hispanics (Table 1). In particular, dengue seroprevalence in Asians (25%) was 133 times as high as that in Caucasians (0·2%) and 54 times as high as in blacks (0·5%). These disparate results strongly argue against previous DENV transmission in the four-county area. The 13 persons with evidence of previous YFV exposure were nearly all men (12) and were older (average 62 years) than the entire sample (average 42 years). It is likely that these previous exposures resulted from YFV vaccination, possibly during military service.
WNV incidence in the 2012 epidemic
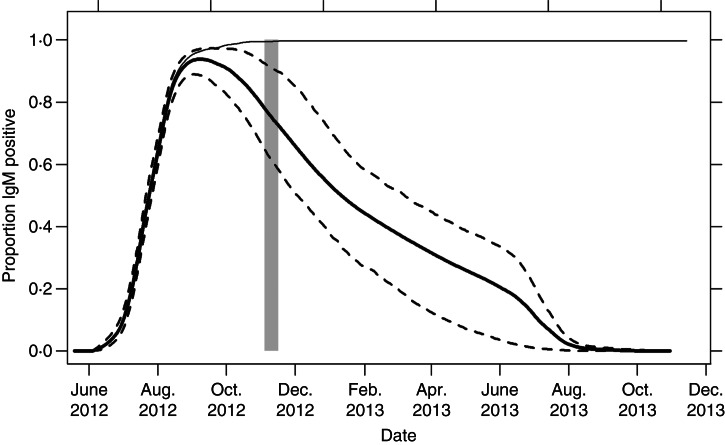
As described in the Methods section, estimation of the expected number of donors who were infected during 2012 accounting for IgM seroreversion began by using the WNND surveillance data shown in Figure 1. Then, estimation of the IgM fall-off curve used 61 donors [13, 14] whose initial IgM index was <1·1, whose results on the date of initial donation were available, and whose IgM profile lacked inconsistent or outlying observations. These data were then combined as described, resulting in the summary estimation curve in Figure 2, which shows the expected proportion of IgM seroreversions over time for this outbreak. From this, we estimated that 1/0·76 = 1·32 (95% CI 1·07–1·61) times as many IgM-positive blood donors would have been observed than were actually observed in our serosurvey had no donors seroreverted between the times of infection and the serosurvey. Sixty-nine donors had WNV IgM antibody and based on the 1·32 inflation factor, the expected number of 2012 infections in the donor survey was 91·1 (95% CI 73·6–110·9), for a resulting cumulative annual incidence estimate of 1·8% (95% CI 1·5–2·2%). This suggests that 82 775 of the 4 521 417 residents of the four-county areas aged at least 16 years were infected during the 2012 epidemic. A total of 349 persons aged at least 16 years were reported with WNND in 2012, giving a ratio of 238 (95% CI 192–290) infections for every reported neuroinvasive adult case.
Fig. 2.
Expected proportion of IgM-positive donations by date (month/year), with the beginning of the months indicated. The heavy solid line (–––) represents the proportion, with dashed lines (- - -) indicating 95% confidence bands of infected donors expected to be IgM-positive over time accounting for IgM seroreversion. The thin solid line (–––) represents the proportion of infected donors who would be IgM positive if IgM positivity did not wane. The grey bar represents the timing of the donor survey.
Age- and gender-specific WNV infection-to-WNND ratios
Table 2 presents WNV infections-to-WNND case ratios stratified by gender and age. The numbers of infections resulting in WNND were similar in males and females [156 (95% CI 109–222) and 221 (95% CI 140–316)]. In contrast, older individuals were significantly more likely to develop WNND with infection-to-case ratios of 47:1 in males and 63:1 in females. Table 2 also juxtaposes the results of our study of infections and WNND cases in North Texas in 2012 with infections-to-WNND ratios reported by Carson et al. [4] based on a serosurvey of blood donors in North Dakota in 2008. After adjusting for IgM fall-off as detailed above, the point estimates for the overall ratios of infections to WNND were very similar in these two studies (238:1 vs. 244:1, respectively), and there were very similar associations with age and gender.
Table 2.
Comparison of WNV-to-WNND ratios, by gender and age, from donors with evidence of infection in 2012 and those described in the Carson et al. [4] serosurvey
| Age group, years | No. donors | WNV 2002–2012 | WNV 2012 | WNV seroprev, % 2012 (95% CI) | Total pop. | WNV-infected population | No. WNND cases | (A) Infections:1 WNND (95% CI) | (B) Infections:1 WNND (95% CI) [4] | A:B (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Male | 2731 | 84 | 39 | 1·4 (1·0–2·0) | 2 204 852 | 31 486 | 202 | 156 (109–222) | 220 (185–263) | 0·72 (0·49–1·06) |
| 16–24 | 299 | 6 | 2 | 0·7 (0·1–3·6) | 412 351 | 2758 | 11 | 251 (45–1359) | 719 (385–1250) | 0·35 (0·06–1·96) |
| 25–44 | 819 | 20 | 9 | 1·1 (0·4–2·6) | 872 522 | 9588 | 41 | 234 (97–559) | 356 (238–556) | 0·71 (0·28–1·83) |
| 45–64 | 1290 | 44 | 23 | 1·8 (1·0–3·1) | 690 617 | 12 313 | 75 | 164 (94–286) | 248 (178–345) | 0·66 (0·36–1·22) |
| ⩾65 | 323 | 14 | 5 | 1·6 (0·5–4·8) | 229 362 | 3550 | 75 | 47 (15–147) | 50 (39–66) | 0·96 (0·27–3·35) |
| Female | 2240 | 55 | 30 | 1·3 (0·9–2·0) | 2 316 862 | 31 029 | 147 | 221 (140–316) | 291 (227–370) | 0·68 (0·44–1·05) |
| 16–24 | 322 | 3 | 2 | 0·6 (0·1–3·4) | 400 255 | 2486 | 5 | 243 (44–1319) | 1231 (11–3333) | 0·40 (0·07–2·29) |
| 25–44 | 798 | 20 | 12 | 1·5 (0·7–3·2) | 891 854 | 13 411 | 36 | 239 (99–571) | 330 (204–556) | 1·13 (0·48–2·68) |
| 45–64 | 947 | 26 | 12 | 1·3 (0·6–2·7) | 721 032 | 9137 | 52 | 171 (98–298) | 387 (238–625) | 0·45 (0·20–1·02) |
| ⩾65 | 173 | 6 | 4 | 2·3 (0·6–7·9) | 303 721 | 7022 | 54 | 63 (20–194) | 61 (41–90) | 2·10 (0·45–9·69) |
| Total | 4971 | 139 | 69 | 1·4 (1·1–1·8) | 4 521 714 | 62 764 | 349 | 180 (142–227) | 244 (213–286) | 0·72 (0·56–0·93) |
| Adjusted total* | 91† | 1·8 (1·5–2·2) | 82 775 | 238 (192–290) | 0·96 (0·76–1·20) |
WNV, West Nile virus; WNND, WNV neuroinvasive disease; CI, confidence interval.
The total number of WNND cases does not include the six reported individuals aged <16 years.
Adjusted total accounts for the estimated IgM fall-off, as described in the Methods section and text.
Estimated number of WNV 2012 infections accounting for IgM fall-off, as described in the Methods section and text.
DISCUSSION
We estimated that approximately 82 800 (1·8%) of the 4·52 million residents aged ⩾16 years in the four-county Dallas–Fort Worth metropolitan area became infected with WNV during the 2012 epidemic. Our serosurvey results also indicate that this total equalled the number infected from 2002 to 2011 combined, with approximately half of WNV IgG reactive donors estimated to have been infected in 2012 based on the adjusted IgM reactivity rate. This latter observation is consistent with the number of WNND reports in 2012 equalling that of all previous years combined. WNV IgG antibody seroprevalence increased by age, a finding consistent with cumulative exposures over a number of years. All other demographic groups appeared equally likely to be exposed to WNV. We also estimated that 238 (95% CI 192–290) infections in adults occurred for every reported neuroinvasive disease adult case.
One other study used two different approaches to estimate WNV infection incidence during the 2012 outbreak in the four-county area [20]. An estimate of 85 156 infections (95% CI 68 302–103 866) or 2·0% (95% CI 1·6–2·4) incidence in adults was derived by multiplying the number of reported WNND cases by age- and gender-adjusted WNND-to-infection ratios based on a previous study in North Dakota [4]. In the other approach, an estimate of 31 013 infections (95% CI 19 133–42 893) or 0·7% (95% CI 0·4–1·0) incidence in adults was based on a modelling approach incorporating rates of detection of WN viraemic blood donors during routine screening during the outbreak and the expected length of detectable viraemia [20]. This latter approach likely results in an underestimate because symptomatic persons are deferred from donating blood.
Our results compare favorably with two previous studies of blood donors in other locations. A serosurvey in North Dakota blood donors indicated a ratio of one reported neuroinvasive disease case for every 244 (95% CI 213–286) infections in adults, with significantly increased rates of WNND in infected persons in older age subgroups [4]. Unlike the Dallas serosurvey, in which this ratio was derived for 1 year using IgM antibody prevalence, the North Dakota serosurvey assessed cumulative infections as measured by IgG seroprevalence with the cumulative number of WNND cases reported from 1999 to 2008, which assumed that IgG persists following infection, a finding corroborated by a 5-year follow-up study of viraemic blood donors (that study also demonstrated loss of IgM in all donors at 5 years of follow-up, which clearly indicated the need for adjustment for IgM seroreversion as done in the current study) [21]. In another approach using nationwide data from WNV nucleic acid screening of blood donors and the duration of time that WNV nucleic acid is detectable in serum, Busch et al. estimated that one reported neuroinvasive disease case occurred for every 256 (95% CI 112–401) infections [7]
The approach and methods for projecting infection incidence rates derived from blood donor serosurveys and combining the incidence projections with ArboNET WNND case reports were essentially identical in the current study of donors who acquired WNV infections in North Texas in 2012 and the North Dakota study of donors who acquired infections prior to 2008. This allowed us to directly compare results from these two studies which demonstrated virtually identical point estimates for the overall ratios of infections to WNND (238:1 vs. 244:1, respectively), as well as very similar associations with age and gender (Table 2). This analysis supports the conclusion that the relative proportion of WNND cases did not measurably change as a result of increased fitness of the virus during the period WNV became endemic in the United States. This finding is reassuring in light of evidence for significant evolution of WNV sequences which has been hypothesized to increase viral fitness and potential pathogenicity [2, 22, 23]. We believe our approach of conducting donor serosurveys at ~5-year intervals and comparing the infections-to-WNND ratios is a feasible and important surveillance strategy to monitor for evolving viral pathogenicity, with the caveat that WNND case-reporting is comparable in different regions and over time.
Two other informative community-wide serosurveys have examined infection incidence in the United States. The first, a household-based serosurvey conducted after the 1999 New York City outbreak in one neighbourhood with a high concentration of WNND cases, showed a 2·6% (95% CI 1·2–4·1) WNV IgM antibody seroprevalence and an estimated ratio of one reported WNND case for every 140 infections [6]. The lower estimated ratio of reported cases of WNND to infections in New York City could have been due to the fact that the area sampled was demographically older than New York City as a whole, and thus more likely to develop WNND after WNV infection [6]. In addition, possible IgM seroreversion was not accounted for. On the other hand, the New York City serosurvey included children, who are much less likely to develop WNND. It should also be noted that the ratio of reported WNND cases and infections was based on only 19 persons with WNV IgM or IgG antibodies and nine WNND cases, suggesting that confidence limits, while not provided, were wide (95% CI 60·7–216·7).
The second study was a large household-based seroprevalence study in Cuyahoga County, Ohio following a large WNV outbreak in 2002 [24]. This survey indicated a countywide WNV IgG seroprevalence of 1·9% (95% CI 0·8–4·6) and a ratio of one reported WNND case for every 160 infections with wide confidence intervals (95% CI 67–386), consistent with the estimates derived from our large blood donor serosuveys.
The cross-reactivity of the IgG WNV antibody test with other flaviviruses permitted several other important observations. The substantially higher DENV seroprevalence in Asians and Hispanics compared to other race/ethnicities strongly argues against significant autochthonous transmission in the Dallas–Fort Worth area despite the presence of vector mosquitoes. In addition, SLEV seroprevalence was quite low, which validates that the paucity of SLEV cases reported in recent years reflects true incidence trends.
Our data have several limitations. Blood donors differ from the general population with respect to age, gender, and race/ethnicity. While these factors did not appear to have a large influence on WNV incidence in this study, blood donors may have behavioural differences compared to the general population that influence exposure to vector mosquitoes. In addition, blood donation is limited to persons aged ⩾16 years; therefore, our analysis was limited to the adult population. The completeness of reporting of WNND cases to national surveillance in the four-county area is unknown. Additionally, we acknowledge that we may have underestimated the true IgG seroprevalence of the other flaviviruses since the cross-reactivity of the assay is not likely 100%.
In conclusion, our serosurvey indicated that over 1.8% of the population, or more than 82 000 people, in the Dallas–Fort Worth area became infected in the 2012 epidemic. At least 25–30% of these 82 000 infected persons would have been expected to develop West Nile fever [25], adding to the public health burden of the more than 350 reported cases of WNND. This outbreak reinforces the need for continued vigilance, particularly in high population centres located in WNV-endemic areas where mosquito control has the potential to prevent thousands of infections. Our analysis is similar to a previous estimate for infections per WNND case from a serosurvey of donors in North Dakota infected during 2002–2008, indicating no change in virulence as WNV has evolved into an endemic infection in the United States.
ACKNOWLEDGEMENTS
The authors acknowledge Amanda Noga and Olga Kosoy for performing the arbovirus serological testing. This work was supported by the Centers for Disease Control and Prevention (contract no. 200-2013-M- 58473).
DECLARATION OF INTEREST
Phillip Williamson is the Vice President of Creative Testing Solutions. The remaining authors have no conflict of interest to declare.
REFERENCES
- 1.CDC. West Nile virus (http://www.cdc.gov/westnile/statsmaps/index.html).
- 2.Pybus OG, et al. Unifying the spatial epidemiology and molecular evolution of emerging epidemics. Proceedings of the National Academy of Sciences USA 2012; 109: 15066–15071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindsey NP, et al. West Nile virus neuroinvasive disease incidence in the United States, 2002–2006. Vector Borne Zoonotic Diseases 2008; 8: 35–39. [DOI] [PubMed] [Google Scholar]
- 4.Carson PJ, et al. Neuroinvasive disease and West Nile virus infection, North Dakota, USA, 1999–2008. Emerging Infectious Diseases 2012; 18: 684–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen LR, et al. Estimated cumulative incidence of West Nile virus infection in US adults, 1999–2010. Epidemiology and Infection 2013; 141: 591–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mostashari F, et al. Epidemic West Nile encephalitis, New York, 1999: results of a household-based seroepidemiological survey. Lancet 2001; 358: 261–264. [DOI] [PubMed] [Google Scholar]
- 7.Busch MP, et al. West Nile virus infections projected from blood donor screening data, United States, 2003. Emerging Infectious Diseases 2006; 12: 395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson AJ, et al. Detection of anti-arboviral immunoglobulin G by using a monoclonal antibody-based capture enzyme-linked immunosorbent assay. Journal of Clinical Microbiology 2000; 38: 1827–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martin DA, et al. Standardization of immunoglobulin M capture enzyme-linked immunosorbent assays for routine diagnosis of arboviral infections. Journal of Clinical Microbiology 2000; 38: 1823–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hogrefe WR, et al. Performance of immunoglobulin G (IgG) and IgM enzyme-linked immunosorbent assays using a West Nile virus recombinant antigen (preM/E) for detection of West Nile virus- and other flavivirus-specific antibodies. Journal of Clinical Microbiology 2004; 42: 4641–4648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tardei G, et al. Evaluation of immunoglobulin M (IgM) and IgG enzyme immunoassays in serologic diagnosis of West Nile Virus infection. Journal of Clinical Microbiology 2000; 38: 2232–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prince HE, et al. Development and persistence of West Nile virus-specific immunoglobulin M (IgM), IgA, and IgG in viremic blood donors. Journal of Clinical Microbiology 2005; 43: 4316–4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Busch MP, et al. Virus and antibody dynamics in acute west nile virus infection. Journal of Infectious Diseases 2008; 198: 984–993. [DOI] [PubMed] [Google Scholar]
- 14.Lanteri MC, et al. West Nile virus nucleic acid persistence in whole blood months after clearance in plasma: implication for transfusion and transplantation safety. Transfusion 2014; 54: 3232–3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heckman N, Lockhart R, Nielsen JD. Penalized regression, mixed effects models and appropriate modeling. Electronic Journal of Statistics 2013; 7: 35. [Google Scholar]
- 16.Durban M, et al. Simple fitting of subject-specific curves for longitudinal data. Statistics in Medicine 2005; 24: 1153–1167. [DOI] [PubMed] [Google Scholar]
- 17.Ruppert D, Wand MP, Carroll RJ. Semiparimetric Regression. New York: Cambridge University Press, 2003. [Google Scholar]
- 18.Gart JJ, Nam J. Approximate interval estimation of the ratio of binomial parameters: a review and corrections for skewness. Biometrics 1988; 44: 323–338. [PubMed] [Google Scholar]
- 19.R: A language and environment for statistical computing. (http://www.R-project.org/).
- 20.Cervantes DT, et al. West Nile virus infection incidence based on donated blood samples and neuroinvasive disease reports, Northern Texas, USA, 2012. Emerging Infectious Diseases 2015; 21: 681–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carson PJ, et al. Long-term clinical and neuropsychological outcomes of West Nile virus infection. Clinical Infectious Diseases 2006; 43: 723–730. [DOI] [PubMed] [Google Scholar]
- 22.Anez G, et al. Evolutionary dynamics of West Nile virus in the United States, 1999–2011: phylogeny, selection pressure and evolutionary time-scale analysis. PLOS Neglected Tropical Diseases 2013; 7: e2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mann BR, et al. Continued evolution of West Nile virus, Houston, Texas, USA, 2002–2012. Emerging Infectious Diseases 2013; 19: 1418–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mandalakas AM, et al. West Nile virus epidemic, northeast Ohio, 2002. Emerging Infectious Diseases 2005; 11: 1774–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zou S, et al. West Nile fever characteristics among viremic persons identified through blood donor screening. Journal of Infectious Diseases 2010; 202: 1354–1361. [DOI] [PubMed] [Google Scholar]