SUMMARY
A legionellosis outbreak at an industrial site was investigated to identify and control the source. Cases were identified from disease notifications, workplace illness records, and from clinicians. Cases were interviewed for symptoms and risk factors and tested for legionellosis. Implicated environmental sources were sampled and tested for legionella. We identified six cases with Legionnaires’ disease and seven with Pontiac fever; all had been exposed to aerosols from the cooling towers on the site. Nine cases had evidence of infection with either Legionella pneumophila serogroup (sg) 1 or Legionella longbeachae sg1; these organisms were also isolated from the cooling towers. There was 100% DNA sequence homology between cooling tower and clinical isolates of L. pneumophila sg1 using sequence-based typing analysis; no clinical L. longbeachae isolates were available to compare with environmental isolates. Routine monitoring of the towers prior to the outbreak failed to detect any legionella. Data from this outbreak indicate that L. pneumophila sg1 transmission occurred from the cooling towers; in addition, L. longbeachae transmission was suggested but remains unproven. L. longbeachae detection in cooling towers has not been previously reported in association with legionellosis outbreaks. Waterborne transmission should not be discounted in investigations for the source of L. longbeachae infection.
Key words: Legionnaires' disease, legionella, Legionella longbeachae, occupation-related infections, outbreaks, water-borne infections
INTRODUCTION
Legionnaires’ disease (LD) and Pontiac fever (PF) are the most common disease manifestations of legionella infection, collectively termed legionellosis. Internationally, the predominant cause of community-acquired LD is Legionella pneumophila serogroup (sg) 1 [1], however in New Zealand infection with Legionella longbeachae has accounted for more than 50% of reported legionellosis cases annually since 2012 [2], and a review of New Zealand legionellosis epidemiology from 1979 to 2009 found that L. longbeachae occurred at the same frequency as L. pneumophila [3]. Some jurisdictions in Australia also report more L. longbeachae notifications than L. pneumophila, however this is not a consistent trend across Australia as a whole [4]. L. longbeachae infections where the source has been confirmed appear to be exclusively associated with soils, potting mixes and composts [5]; conversely, cases and outbreaks of LD due to other legionella species have often been linked to engineered systems that produce water aerosols [6], and L. pneumophila sg1 transmission from soil has also been described [7].
We describe a mixed species legionellosis outbreak associated with industrial cooling towers that were found to be heavily contaminated with multiple legionella species, including both L. pneumophila and L. longbeachae. An unusual feature of this outbreak was that L. longbeachae was detected both as a contaminant of cooling tower water and as an apparent cause of human infection among cases working at the industrial site; we are not aware that this has been reported previously.
Between 8 October and 4 November 2015, three patients diagnosed with LD due to L. pneumophila sg1 were notified in central North Island, New Zealand. The patients lived in three widely separated towns in two non-adjacent health districts, and recognition of a possible outbreak did not occur until concurrent investigations of the second and third patients identified that all three had worked at the same industrial site.
The industrial site, a dairy processing plant, was situated in a rural area distant from the residential addresses of all three initial cases. The plant had been extensively redeveloped to increase production capacity: this redevelopment had required substantial earthworks. Two new cooling towers had been built to accompany three existing towers on the site. The site workforce comprised approximately 120 workers, the majority employed as tanker drivers who transported milk to the plant for processing. All three initial cases had been ambulatory on the site during their incubation periods. We conducted an investigation to characterize cases, and identify and remedy the outbreak source.
METHODS
This work was undertaken as part of an urgent public health investigation therefore did not require institutional ethical review or approval. In addition to the first three reported cases, case finding was undertaken through review of disease notifications and workplace absenteeism and illness records, and requests to clinicians for notifications of suspected legionellosis. Retrospective case finding extended back to 1 August 2015 because activation of the plant's cooling towers occurred around that date. We defined a case of confirmed LD as radiographically-confirmed pneumonia with laboratory evidence of legionella infection in a person with onset of illness between 1 August and 12 December 2015 and within 14 days of exposure to the site. Laboratory evidence of legionella infection comprised at least one of the following, as per the New Zealand surveillance definitions [8]: legionella isolated from a clinical specimen, L. pneumophila sg1 antigen detected in urine, or seroconversion indicated by a ⩾fourfold rise in immunofluorescent antibody titres against legionella species to ⩾256 between acute- and convalescent-phase sera tested in parallel. Probable LD was defined as above, with laboratory evidence of legionella infection of one or more antibody titres ⩾512 but no fourfold titre rise. Cases with confirmed or probable PF were defined as persons meeting laboratory criteria for confirmed or probable LD, respectively, without radiographic evidence of pneumonia but who had developed an illness with fever and at least one other symptom (of headache, cough, dyspnoea, myalgia, vomiting, diarrhoea) that had commenced within 3 days of exposure to the site in the 1 August–12 December 2015 period.
Data on demographic details, illness onset and symptoms, healthcare utilization, risk factors for legionellosis, and possible exposures to legionella sources in occupational and non-occupational environments were collected from standardized interviews with all persons identified. Medical examination and investigations were sought on all those with history of illness suggestive of legionellosis: for those with acute illness, investigations included sputum culture and isolation, urinary antigen testing, acute-phase serology, and chest radiographs if clinically indicated; convalescent-phase serum specimens were collected if symptoms had occurred 3 or more weeks prior to assessment, or 3 weeks after acute serum collection.
Retrospective detection of antibody levels to legionella species was undertaken using indirect immunofluorescent antibody testing (IFAT) on sera collected from suspected outbreak cases in order to ascertain both evidence of exposure and the identity of the causative Legionella species [9]. The IFAT used fluorescein isothiocyanate conjugated anti-human IgM, A and G antibody and heat-killed whole-cell antigens prepared from 32 type strains of legionella known to cause infection in New Zealand (based primarily on clinical culture isolation). These were grouped into five pools (Supplementary material) and sera reactive against a pool were then retested against the individual pool components to identify the reactive legionella strain. Sera were tested at the Institute of Environmental Science and Research (ESR) Legionella Reference Laboratory (LRL) using a standard process irrespective of the patient's association with the outbreak. Urine specimens were tested for L. pneumophila sg1 antigens using the BinaxNOW kit (Alere Inc., Waltham, Massachusetts, USA). Sputum samples were cultured for legionella at the LRL; isolates were identified to species and serogroup level using direct fluorescent antibody staining (m-Tech, Milton, Georgia, USA) and by mip gene sequencing [10]. Sequence-based typing (SBT) was used to characterize DNA sequences of seven virulence genes in the order flaA, pilE, asd, mip, mompS, proA, and neuA for the L. pneumophila isolates. The nucleotide sequences of these genes can be compared between clinical and environmental isolates, giving results that are considered highly discriminatory and epidemiologically concordant [11]. Each unique combination of the allelic profiles is assigned a unique Sequence Type (ST) using the on-line tool at http://bioinformatics.phe.org.uk/legionella/legionella_sbt/php/sbt_homepage.php [12].
An environmental investigation was conducted to identify possible legionella sources on the industrial site, in particular areas where water aerosols were created or where organic matter was being composted or handled. Possible exposure sources were also sought in case's domestic or non-occupational environments. Water, biofilm and soil samples were collected according to guidance methods [13], and tested at the LRL for legionella bacteria using the appropriate method depending on sample origin (either ISO 11731-2 for potable waters, AS/NZS 3896 for cooling tower waters, or AS/NZS 5024 for soils and composts). Isolates were analysed as described above. Water temperature and free available chlorine (FAC) levels were measured onsite using recently-calibrated instruments.
RESULTS
Including the initial three patients, 13 cases were identified with either LD or PF; six met criteria for LD (four confirmed, two probable), and seven met criteria for PF (all probable). The four cases with confirmed LD had L. pneumophila sg1 identified by culture (2 cases) or urinary antigen testing (1), or L. longbeachae sg1 identified by seroconversion (1). Other legionella species and serogroups were diagnosed by serology in cases with probable LD or PF (Table 1). A further 19 persons identified with respiratory illness following site exposure did not meet case criteria because they did not have clinical illness consistent with LD or PF (3), had negative tests (14) or had no testing done (2).
Table 1.
Basis of case classification and infecting organism
| Case classification and basis for classification | Legionella species | Number of cases | Serological titres (first sample/second sample) |
|---|---|---|---|
| Legionnaires’ Disease – Confirmed | |||
| Sputum culture positive | L. pneumophila sg1 | 2 | Not collected |
| Urinary antigen positive; two elevated convalescent titres | L. pneumophila sg1 | 1 | 512/1024 |
| Fourfold rise in serological titres | L. longbeachae sg1 | 1 | 1024/4096 |
| Legionnaires’ Disease – Probable | |||
| Two elevated serological titres | L. pneumophila sg5 | 1 | 512/512 |
| Single elevated serological titre | L. longbeachae sg1 | 1 | 2048/not collected |
| Pontiac Fever – Probable | |||
| Two elevated serological titres | L. longbeachae sg1 | 3 | 512/512 |
| 512/1024 | |||
| 512/1024 | |||
| L. longbeachae sg2 | 1 | 512/1024 | |
| L. pneumophila sg1 | 1 | 512/512 | |
| L. sainthelensi | 1 | 512/512 | |
| Single elevated serological titre* | L. sainthelensi | 1 | 512 |
| Total cases | 13 |
sg, serogroup; *titre below cut-off value on second sample.
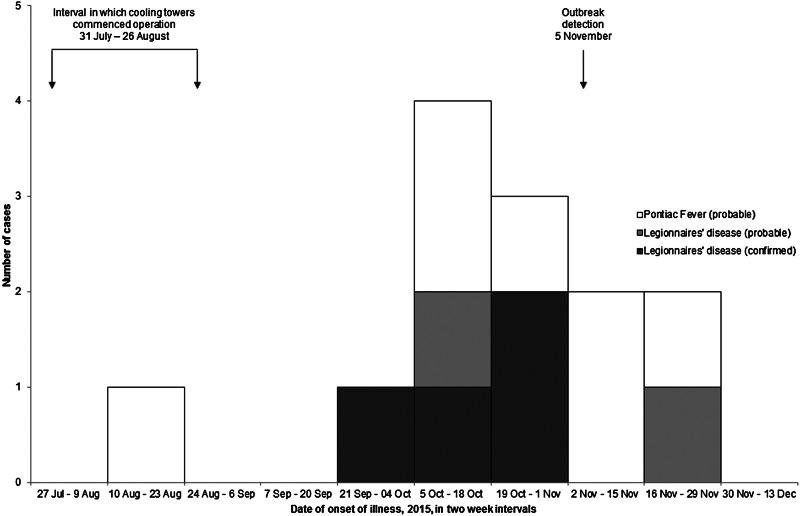
The 13 cases had a median age of 51 years (range 29–72 years), 12 were male. Nine were current or previous smokers; three had a history of asthma, and one was taking anti-rejection immunosuppressant medication following a kidney transplant. The cases’ illnesses began between 15 August and 20 November 2015 (Fig. 1). Six (all with LD) had been hospitalized during their illness, one requiring intensive care.
Fig. 1.
Epidemic curve for 13 patients with legionellosis, August–November 2015, New Zealand.
Of the 13 cases, 12 had been working on the site during their incubation periods: three had worked on the site for the entirety of each working day, and the remaining nine were tanker drivers who visited the site regularly during their working shifts. The remaining case lived on a neighbouring property 500 m from the site and passed close to the site perimeter on each working day. Site investigation identified the five water-based cooling towers as possible sources of legionella exposure; all cases who were site workers had been ambulatory in open air close to the cooling towers. Other possible sources on the site included shower facilities and dust from earthworks. Potential non-site exposures for cases included potting mix (1 case), roof-collected untreated water (3), spa pool (1) and decorative fountain (1).
The cooling towers were situated at ground level, with air intake sites covered by ventilation grills and otherwise open to circulating air. Each of the cooling towers contained sediment and obvious algae growth, with soil residues visible on the ventilation grills on cooling tower A. Although a hypochlorite-based biocide was being used in the cooling towers, FAC levels were undetectable in the two newly-installed cooling towers (A and B), and ranged between 0·07 and 0·14 mg/L in the three pre-existing towers (C, D and E). Legionella bacteria were cultured from samples from all five cooling towers (Table 2). Seven different legionella species were identified from the cooling towers; L. pneumophila sg1 and L. longbeachae sg1 were found in the highest concentrations. The SBT allelic profile for L. pneumophila sg1 isolates from each cooling tower was 12,8, 11, 21, 40, 12, 9; matching the unique profile ST 1694. A 100% DNA sequence homology was established between the L. pneumophila sg1 isolates from cooling towers and from the clinical isolates of the two cases diagnosed on the basis of legionella culture. No legionellae were detected in environmental specimens collected from other locations within the industrial site, including uncovered soil adjacent to cooling towers. L. pneumophila sg1 was isolated from home compost used by one outbreak case, however the SBT allelic profile for the compost isolate was distinct from that of the case and the cooling tower isolates. No legionellae were detected in other non-site implicated sources – these included both domestic hot water systems and compost used by cases during their incubation period.
Table 2.
Legionella testing results on samples collected from cooling towers
| Cooling tower | Sample type | Water temperature | FAC (mg/L) | Legionella species identified* | Enumeration (CFU/mL) |
|---|---|---|---|---|---|
| A | Water | 29 °C | 0 | L. pneumophila sg 1** | 10–100 |
| B | Water | 24 °C | 0 | L. pneumophila sg 1** | 560–640 |
| L. longbeachae sg 1 | 170–180 | ||||
| L pneumophila strain 91–033 | 10 | ||||
| L. taurinensis | 10–130 | ||||
| Biofilm | n/a | n/a | L. pneumophila sg 1** | n/a | |
| L. longbeachae sg 1 | n/a | ||||
| C | Water | 18 °C | 0·07 | L. rubrilucens | 10 |
| D | Water | 18 °C | 0·14 | L. pneumophila sg 1** | 160–220 |
| L quinlivanii sg 1 | 10–40 | ||||
| L rubrilucens | 40–50 | ||||
| Biofilm | n/a | n/a | L. pneumophila sg 1 | n/a | |
| L. quinlivanii sg 1 | n/a | ||||
| E (not in operation) | Water | 0·12 | L. birminghamensis | 10 |
FAC, free available chlorine; CFU, colony-forming units.
Species identification carried out using mip gene sequence analysis [10].
SBT allelic profiling of these L. pneumophila sg 1 isolates indicated 100% homology to ST 1694 strain.
An investigation was undertaken to find factors contributing to the outbreak. It was established that cooling towers A and B had been newly commissioned and had commenced operation on 7 August 2015 and 31 July 2015 respectively; pre-existing towers C and D were re-started on 26 August and 6 August, respectively. Tower E remained offline and non-operational throughout, although the basin contained water. No documentation was available to verify biocide management of the towers before starting operation; following start-up, towers A and B were managed by manual ‘slug’ dosing with biocides once per month, and towers C and D were automatically dosed with two biocide products. Water samples had been collected from all four operational towers on a monthly basis to test for the presence of legionella by a private service provider, and all test results had been negative. However, the samples had been collected using containers that did not include a biocide neutralising agent, were chilled in transport and were often subject to a delay in excess of 48 h between collection and testing.
Following recognition of the outbreak and detection of legionella contamination of the cooling towers, all cooling towers on the site were cleaned and hyperchlorinated to eliminate bacterial growth. Decontamination and clearance testing was undertaken in accordance with AS/NZS3666·3 [14]. The cooling towers were considered under control after two consecutive samples tested at the LRL were legionella culture-negative. Clearance specimens collected from all cooling towers 3 days after hyperchlorination were culture-negative, however repeat samples collected from tower B on 26 November 2015 were found to be positive for L. pneumophila sg1 (enumerated at 60 CFU/mL) and clearance of this tower was not achieved until samples collected on 15 December 2015 were found to be negative. Clearance samples collected from each of the other four towers remained negative.
DISCUSSION
An outbreak of legionellosis with six confirmed and probable LD cases and seven probable PF cases occurred in an industrial site between August and November 2015. Several findings from the investigation indicated that one or more cooling towers on the site were the source of infection: the industrial site was the sole exposure common to all cases, and the cooling towers were the only identified feature containing legionella bacteria; all cases who worked on site were exposed to the cooling tower aerosols, and the one case who did not work on the site regularly passed the site and lived within the radius of possible legionella cooling tower transmission [15]; the epidemic curve for the outbreak reflects evolution of the outbreak over several months, which is similar to other legionellosis outbreaks linked to cooling towers [16, 17]; and finally, clinical L. pneumophila sg1 isolates from two cases matched isolates from each of the site cooling towers using SBT. The ST 1694 strain identified by SBT during this outbreak is the first time this L. pneumophila sg1 strain has been detected in New Zealand, although a detailed understanding of circulating environmental strains is unknown. SBT testing of other L. pneumophila isolates referred to the LRL prior to, during and after this outbreak have not identified other ST 1694, suggesting that the strain is rare and supports identification of the cooling towers as the outbreak source.
L. pneumophila sg1 contamination of cooling towers has been previously linked to legionellosis outbreaks in New Zealand [16]; L. pneumophila in water are released in cooling tower aerosols [18], and many outbreaks have been temporally linked to cooling tower restarts following inactivity [19]. Operation of cooling systems after periods of shutdown has been shown to rapidly increase the legionella concentration in water, considered due to sloughing of biofilm and disturbance of sediments by water flow [20]. The conditions in the cooling towers in this outbreak suggest abundant biofilm was available to act as a legionella reservoir, and biocide levels were inadequate to effect control. The effectiveness of biocide would have been further reduced by sediment present in the cooling tower water basins; this may have resulted from the earthworks undertaken during the site redevelopment.
An unusual feature of this outbreak was detection of L. longbeachae sg1 in the water of one cooling tower, and serological evidence of L. longbeachae sg1 infection in one confirmed LD case and four probable LD and PF cases. L. longbeachae is rarely identified in water [21], and the few reported outbreaks of L. longbeachae legionellosis have typically implicated horticultural growing media [22]. One L. longbeachae outbreak has been linked to a ventilation system, although the ultimate source was unclear; L. longbeachae was not detected in environmental specimens, and the ventilation system did not involve water reservoirs [23].
None of the cases in the current outbreak with serology indicating L. longbeachae sg1 infection had clinical isolates that would enable comparison with environmental L. longbeachae isolates, so it is impossible to confirm the cooling tower as the source of their infections. The L. pneumophila sg1 findings provide circumstantial evidence suggesting transmission of legionellae from these cooling towers was feasible, and no alternative sources for L. longbeachae infection were identified. In a previously reported outbreak, the strain of L. pneumophila bacteria found in soil matched that of isolates from an adjacent spa pool and of clinical isolates from exposed cases [24]; similar links can only be implied in this outbreak because legionella was not detected in soil from the site, although it is feasible that legionella-containing airborne soil may have been the source of the cooling tower contamination. Waterborne transmission should not be discounted in investigations for the source of L. longbeachae infection.
Multiple strain outbreaks of legionellosis have been reported, usually demonstrated as multiple clones of the same species and serogroup [25, 26]. The majority of cases in this outbreak appeared to have been infected with either L. pneumophila sg1 or L. longbeachae sg1, however other cases had serological evidence of probable infection with either L. pneumophila sg5, L. longbeachae sg2 or Legionella sainthelensi, none of which were detected in environmental specimens. Our laboratory investigation of retrospective cases relied on serologic testing methods since many were identified after the sampling period for appropriate acute-phase serum, sputum or urine collection had elapsed. To mitigate the possibility of antibody cross-reactivity in the IFAT we tested paired serum specimens collected at least 2 weeks apart and in parallel for each patient, and titres ⩾512 were required to meet the serological case definition in the absence of seroconversion, however misclassification cannot be excluded. The legionella strains L. longbeachae sg1, L. longbeachae sg2 and L. sainthelensi are all closely related both antigenically and genetically, and have many shared epitopes. This contributes to the observed antibody cross-reaction patterns seen in the IFAT between these strains, and likewise similar cross-reaction patterns are observed between the different L. pneumophila strains. The IFAT relies on visual determination of the fluorescent endpoint and its subjective nature coupled with the antibody cross-reactions contribute to the low specificity of the test, and results require interpretation with caution. The antibodies detected to L. longbeachae sg2 and L. sainthelensi could potentially be the result of a L. longbeachae sg1 infection for these cases, and by the same argument, the antibodies detected to L. pneumophila sg5 may be the result of an infection to L. pneumophila sg1. In general, the sensitivity and specificity parameters of serological testing to diagnose non-L. pneumophila sg1 disease are less well established than for L. pneumophila sg1 infection [27].
There were limitations to this investigation. Full case ascertainment may not have occurred because we neither attempted a systematic investigation of the entire workforce, and nor did we proactively approach residents in the immediate vicinity of the site due to concerns that the presence of concurrent influenza-like illness in the region may have complicated case assessment. We instead raised awareness of the outbreak through media and directly approached medical practitioners to solicit notifications of suspect cases that had sought medical attention or had been hospitalized. We did not undertake a systematic investigation of the entire cohort of workers on the site and therefore were unable to test measures of association between illness and variables such as work roles and risk factors; however, limited comparisons between cases and non-cases included in the investigation did not yield hypotheses that would have warranted a larger epidemiological study.
Primary factors that appeared to have contributed to the cause of legionella growth in the cooling towers implicated in this outbreak were inadequate biocide control and inadequate removal of organic matter that accumulated in the towers during earthworks in the vicinity. Additionally, tests on the cooling tower water prior to the outbreak detection appeared to have given false-negative results and therefore did not provide an alert that problems were developing; cooling tower operators should be cognisant of the impact of all relevant test results, both chemical and microbiological, on water quality in cooling towers. The findings from this outbreak have implications for prevention and control of legionellosis transmission from cooling towers, particularly with regard to routine microbiological monitoring of cooling towers. In New Zealand, the standard for managing the microbiological control of cooling towers is the joint Australia/New Zealand four-part Standard AS/NZS 3666 (Standards New Zealand, Wellington, New Zealand). Cooling tower water samples collected and processed in accordance with the Standard, were not found to contain legionella, however our testing undertaken using ESR guidance [13] as part of the outbreak investigation revealed legionella in abundant quantities. The sampling and processing techniques differed between our testing and that conducted for routine monitoring: we collected samples in containers with biocide neutralizer, kept specimens at ambient temperatures (>10 °C, but <20 °C) while in transit and tested samples within 6 h of collection; in contrast, samples collected for routine monitoring used containers without biocide neutralizer, were chilled while in transit and the delay to testing often exceeded 48 h after collection. False-negative legionella testing results have occurred when water is sampled using containers not containing biocide neutralising agent [28], and it is possible that this may explain the negative results from tests performed before the outbreak was detected.
CONCLUSIONS
Information from this outbreak investigation suggests that legionellosis outbreaks may be heterogeneous, both in the infecting organisms and in the flora of the presumed outbreak source. Testing patients with community-acquired pneumonia using methods that enable identification of legionella species, other than solely relying on urinary antigen tests that only detect L. pneumophila sg1 antigen, and consideration of atypical transmission mechanisms would help improve understanding of legionellosis outbreaks. Contamination of wet cooling towers with legionella may be unavoidable; it is therefore critical to have good maintenance systems in place, and to follow effective monitoring practices that enable prompt detection and mitigation of legionella contamination to avoid outbreaks.
Acknowledgements
We are grateful to the following for support with the investigation: Taranaki DHB public health service staff, in particular Nicky Dymond; MidCentral Health public health services staff, in particular Brett Munro and Reynold Ball; staff of the Legionella Reference Laboratory at ESR, clinical staff involved with assessing and managing affected patients; management at the industrial site, staff of Worksafe New Zealand; the Ministry of Health. Thanks to Professor David Murdoch, University of Otago, for his helpful comments on the paper, and to the anonymous referees whose critique enabled considerable improvements to the manuscript. We give thanks to the affected individuals and their families for their cooperation and support.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
ETHICAL STANDARDS
This work was undertaken as part of an urgent public health investigation therefore did not require institutional ethical review or approval.
DISCLAIMERS
Nil.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268817001170.
click here to view supplementary material
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Yu VL, et al. Distribution of Legionella species and serogroups isolated by culture in patients with sporadic community-acquired legionellosis: an international collaborative survey. Journal of Infectious Diseases 2002; 186: 127–128. [DOI] [PubMed] [Google Scholar]
- 2.The Institute of Environmental Science and Research Ltd. Annual Surveillance Summary (https://surv.esr.cri.nz/surveillance/annual_surveillance.php). Accessed 22 February 2017.
- 3.Graham FF, et al. Changing epidemiological trends of legionellosis in New Zealand, 1979–2009. Epidemiology and Infection 2012; 140: 1481–1496. [DOI] [PubMed] [Google Scholar]
- 4.NNDSS Annual Report Working Group. Australia's notifiable disease status, 2014: annual report of the National Notifiable Diseases Surveillance System. Communicable Diseases Intelligence Quarterly Report 2016; 40: E48–E145. [PubMed] [Google Scholar]
- 5.Whiley H, Bentham R. Legionella longbeachae and legionellosis. Emerging Infectious Diseases 2011; 17: 579–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phin N, et al. Epidemiology and clinical management of Legionnaires’ disease. Lancet Infectious Diseases 2014; 14: 1011–1021. [DOI] [PubMed] [Google Scholar]
- 7.Wallis L, Robinson P. Soil as a source of Legionella pneumophila serogroup 1 (Lp1). Australian and New Zealand Journal of Public Health 2005; 29: 518–520. [DOI] [PubMed] [Google Scholar]
- 8.Ministry of Health. Legionellosis. In: Communicable Disease Control Manual 2012 (http://www.health.govt.nz/system/files/documents/publications/cd-manual-legionellosis-jul16.pdf). Accessed 21 October 2016.
- 9.Edelstein PH. Detection of antibodies to Legionella spp. In: Rose NR, de Macario EC, Folds JD, Lane HC, Nakamura RM, eds. Manual of Clinical Laboratory Immunology, 5th edn. Washington, DC: American Society for Microbiology, 1997, pp. 502–509. [Google Scholar]
- 10.Ratcliff RM, et al. Sequence-based classification scheme for the genus Legionella targeting the mip gene. Journal of Clinical Microbiology 1998; 36: 1560–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ratzow S, et al. Addition of neuA, the gene encoding N-acylneuraminate cytidylyl transferase, increases the discriminatory ability of the consensus sequence-based scheme for typing Legionella pneumophila serogroup 1 strains. Journal of Clinical Microbiology 2007; 45: 1965–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaia V, et al. Consensus sequence-based scheme for epidemiological typing of clinical and environmental isolates of Legionella pneumophila. Journal of Clinical Microbiology 2005; 43: 2047–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Institute of Environmental Science and Research Ltd. Environmental Sampling for Legionella bacteria. Porirua: The Institute of Environmental Science and Research Ltd, 2014. [Google Scholar]
- 14.Joint Standards Australia/Standards New Zealand Committee ME-062. AS/NZS 3666·3:2011 Air-handling and water systems of buildings – microbial control, part 3: performance-based maintenance of cooling water systems. Standards Australia Limited and Standards, New Zealand, 2011.
- 15.Brown CM, et al. A community outbreak of Legionnaires’ disease linked to hospital cooling towers: an epidemiological method to calculate dose of exposure. International Journal of Epidemiology 1999; 28: 353–359. [DOI] [PubMed] [Google Scholar]
- 16.White PS, et al. Epidemiological investigation of a Legionnaires’ disease outbreak in Christchurch, New Zealand: the value of spatial methods for practical public health. Epidemiology and Infection 2013; 141: 789–799. [DOI] [PubMed] [Google Scholar]
- 17.Bennett E, et al. Barrow-in-Furness: a large community legionellosis outbreak in the UK. Epidemiology and Infection 2014; 142(8): 1763–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishimatsu S, et al. Sampling and detection of Legionella pneumophila aerosols generated from an industrial cooling tower. Annals of Occupational Hygiene 2001; 45: 421–427. [PubMed] [Google Scholar]
- 19.Walser SM, et al. Assessing the environmental health relevance of cooling towers-a systematic review of legionellosis outbreaks. International Journal of Hygiene and Environmental Health 2014; 217: 145–154. [DOI] [PubMed] [Google Scholar]
- 20.Bentham RH, Broadbent CR. A model for autumn outbreaks of Legionnaires’ disease associated with cooling towers, linked to system operation and size. Epidemiology and Infection 1993; 111: 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lau R, et al. Prevalence of Legionella strains in cooling towers and legionellosis cases in New Zealand. Journal of Environmental Health 2013; 75: 82–89. [PubMed] [Google Scholar]
- 22.Cramp GJ, et al. An outbreak of Pontiac fever due to Legionella longbeachae serogroup 2 found in potting mix in a horticultural nursery in New Zealand. Epidemiology and Infection 2010; 138: 15–20. [DOI] [PubMed] [Google Scholar]
- 23.Grove DI, et al. An outbreak of Legionella longbeachae infection in an intensive care unit? Journal of Hospital Infection 2002; 52: 250–258. [DOI] [PubMed] [Google Scholar]
- 24.Schalk JA, et al. Soil as a source of Legionella pneumophila sequence type 47. International Journal of Infectious Diseases 2014; 27: 18–19. [DOI] [PubMed] [Google Scholar]
- 25.Visca P, et al. Multiple types of Legionella pneumophila serogroup 6 in a hospital heated-water system associated with sporadic infections. Journal of Clinical Microbiology 1999; 37: 2189–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lück PC, Wenchel HM, Helbig JH. Nosocomial pneumonia caused by three genetically different strains of Legionella pneumophila and detection of these strains in the hospital water supply. Journal of Clinical Microbiology 1998; 36: 1160–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murdoch DR. Diagnosis of Legionella infection. Clinical Infectious Diseases 2003; 36: 64–69. [DOI] [PubMed] [Google Scholar]
- 28.Wiedenmann A, Langhammer W, Botzenhart K. A case report of false negative Legionella test results in a chlorinated public hot water distribution system due to the lack of sodium thiosulfate in sampling bottles. International Journal of Hygiene and Environmental Health 2001; 204: 245–249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268817001170.
click here to view supplementary material