Abstract
Objective
To investigate the aetiology, subsequent preventive strategies and outcomes of stroke despite anticoagulation in patients with atrial fibrillation (AF).
Methods
We analysed consecutive patients with AF with an index imaging-proven ischaemic stroke despite vitamin K-antagonist (VKA) or direct oral anticoagulant (DOAC) treatment across 11 stroke centres. We classified stroke aetiology as: (i) competing stroke mechanism other than AF-related cardioembolism; (ii) insufficient anticoagulation (non-adherence or low anticoagulant activity measured with drug-specific assays); or, (iii) AF-related cardioembolism despite sufficient anticoagulation. We investigated subsequent preventive strategies with regard to the primary (composite of recurrent ischaemic stroke, intracranial haemorrhage, death) and secondary endpoint (recurrent ischaemic stroke) within 3 months after index stroke.
Results
Among 2946 patients (median age 81 years; 48% women; 43% VKA, 57% DOAC), stroke aetiology was competing mechanism in 713 patients (24%), insufficient anticoagulation in 934 (32%) and cardioembolism despite sufficient anticoagulation in 1299 (44%). We found high rates of the primary (27% of patients; completeness 91.6%) and secondary endpoint (4.6%; completeness 88.5%). Only DOAC (vs VKA) treatment after index stroke showed lower odds for both endpoints (primary: adjusted OR (aOR) (95% CI) 0.49 (0.32 to 0.73); secondary: 0.44 (0.24 to 0.80)), but not switching between different DOAC types. Adding antiplatelets showed higher odds for both endpoints (primary: aOR (95% CI) 1.99 (1.25 to 3.15); secondary: 2.66 (1.40 to 5.04)). Only few patients (1%) received left atrial appendage occlusion as additional preventive strategy.
Conclusions
Stroke despite anticoagulation comprises heterogeneous aetiologies and cardioembolism despite sufficient anticoagulation is most common. While DOAC were associated with better outcomes than VKA, adding antiplatelets was linked to worse outcomes in these high-risk patients. Our findings indicate that individualised and novel preventive strategies beyond the currently available anticoagulants are needed.
Trial registration number
ISRCTN48292829.
Keywords: atrial fibrillation, stroke despite anticoagulation, etiology, prevention strategies, outcome
Introduction
Oral anticoagulation with either direct oral anticoagulants (DOAC) or vitamin K-antagonists (VKA) reduces the risk of ischaemic stroke in patients with non-valvular atrial fibrillation (AF). However, there is a substantial residual stroke risk in patients with AF despite anticoagulation ranging from 0.7% to 2.3% annually in primary and secondary prevention, respectively.1–4 Since the introduction of DOAC, the overall use of oral anticoagulants for stroke prevention in patients with AF has increased steadily, particularly in patients with AF at the highest stroke risk.5 Due to this development, the number of patients with AF suffering a stroke despite anticoagulation is expected to increase, too.6 7 Accumulating evidence suggests that patients with AF and stroke despite anticoagulation are at a higher risk for future recurrence than patients who were naive to anticoagulation treatment before stroke.8–10
For stroke physicians, ischaemic stroke despite anticoagulation in patients with AF represents a challenge in everyday clinical practice, as its aetiology is not well-understood.11 Competing stroke mechanisms such as large artery and small vessel disease, as well as non-adherence or inappropriately dosed anticoagulation have been discussed as potential causes of stroke despite anticoagulation,8–11 but few data on their relative frequency exist.6 A better understanding of the aetiology of stroke despite anticoagulation is needed to inform strategies to prevent recurrence after a stroke despite anticoagulation.11 So far, limited data suggested no benefit from switching the anticoagulant type.8 9 Indeed, the optimal management of patients with stroke despite anticoagulation remains unclear, and the latest guidelines offer no recommendations on this.12
We therefore sought to (i) describe the aetiology of stroke despite oral anticoagulation and (ii) investigate subsequent preventive strategies and outcomes in a large collaborative study of patients with AF and stroke despite anticoagulation from 11 experienced stroke centres.
Methods
Study design, patient population and data collection
We pooled individual data of patients with consecutive stroke in a collaborative effort across 11 experienced stroke centres from Switzerland, Germany and the USA with a special research interest in stroke despite anticoagulation. Patients who had a stroke were identified using local prospective registries complemented by hospital admission records, as in prior research.6 7 Local investigators collected data that were not available in the prospective databases by retrospectively reviewing patient charts. All data were collected using predefined variables in a standardised manner. De-identified patient data were pooled and analysed at the University Hospitals Basel and Bern.
We included patients with previously known AF and an imaging-proven acute ischaemic stroke (hereafter referred to as index stroke) occurring while on oral anticoagulant therapy (ie, prescribed anticoagulation for long-term stroke prevention, excluding non-persistent patients and those with physician-initiated pauses for medical reasons at the time of the stroke). We excluded patients with missing data on anticoagulant treatment, and those with mechanical heart valves. The reporting period was limited to patients presenting no earlier than January 2012 and no later than December 2020.
A detailed description of collected baseline clinical, neuroimaging and laboratory variables, as well as preventive treatments following the index stroke, is presented in the online supplemental file 1.
jnnp-2021-328391supp001.pdf (302.4KB, pdf)
Aetiology of stroke despite anticoagulation
The presumed most likely aetiology of stroke was determined by local investigators according to the following predefined categories:
Competing stroke mechanism other than AF-related cardioembolism (such as small vessel disease, large artery atherosclerosis or other established pathologies as the most likely stroke mechanism in line with the TOAST classification criteria, that is, ‘two or more mechanisms’13);
Insufficient anticoagulation defined (adapting prior research6) as (i) self-reported non-adherence (ie, history of missing intake of anticoagulants within the last 3 days before index stroke); (ii) low anticoagulant activity on admission (ie, international normalised ratio (INR) <2.0 in VKA-treated patients; plasma level <30 ng/mL in DOAC-treated patients14; or, (iii) inappropriately low DOAC dose or dosing frequency (according to current product labelling by the Swiss Agency for Therapeutic Products, European Medicines Agency and the United States Food and Drug Administration, as applicable). Patients with evidence for both (1) and (2) were classified solely as (1), that is, competing stroke mechanism;
AF-related cardioembolism despite sufficient anticoagulation, defined as stroke without evidence for either (1) or (2).
To investigate the reproducibility of the classification, a random sample from the two largest data sets (Basel and Bern, 25 patients each) was reclassified by a different local investigator, showing high inter-rater agreement (82%, kappa 0.73). Additionally, a random sample of 25 patients from the entire data set was reclassified based on available baseline variables by blinded raters from three of the largest centres (Basel, Bern and Heidelberg), showing high inter-centre agreement (87%, kappa 0.80).
3-month outcomes
Out of 11 centres, 8 routinely collected standardised information on the following 3-month outcomes: (i) recurrent ischaemic stroke, (ii) intracranial haemorrhage (ICH), (iii) all-cause death and (iv) functional outcome on the modified Rankin Scale (mRS). The primary endpoint was the composite of recurrent ischaemic stroke, ICH and all-cause death within 3 months, defined as in previous research.8 15 Secondary endpoint was recurrent ischaemic stroke within 3 months. An additional combined endpoint of recurrent ischaemic stroke and ICH within 3 months was defined post hoc.
Statistical analyses
Main analysis
We presented data on the aetiology of stroke despite anticoagulation using descriptive statistics. We stratified patient characteristics according to stroke aetiology and type of anticoagulant (DOAC vs VKA) at the time of the index stroke. Categorical data are presented using frequencies and percentages and continuous data using the median and IQR. We compared categorical variables using the χ2 test or Fisher’s exact test, as appropriate, and continuous variables using the Mann-Whitney U test.
Secondary analyses
To investigate the prognostic significance of the aetiology of stroke despite anticoagulation with regard to the primary and secondary endpoints, we used univariable and multivariable logistic models adjusted for preselected common risk factors (ie, age, sex, hypertension, diabetes, ischaemic heart disease, dyslipidaemia, renal impairment, prior ischaemic stroke or ICH, current smoking and active malignancy).
To explore the association of preventive strategies with the primary and secondary endpoints, we fitted univariable and multivariable logistic models adjusted for preselected common outcome predictors, as described in detail in the online supplemental file 1. As a post-hoc analysis we additionally examined the association of all preventive strategies with the combined endpoint of recurrent ischaemic stroke and ICH.
For all models, we report the (adjusted) OR ((a)OR) along with 95% CIs and two-sided p values. Additionally, the number of missing values are indicated for all data. We fitted all models using only complete cases without data imputation and report the number of patients (and number of events) included in each model.
Statistical analyses were performed using Stata V.17.0 (StataCorp). We conducted this study in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology Statement for observational studies.16 This study is registered with the International Standard Registered Clinical/Social Study Number Registry.
This study complies with the Declaration of Helsinki.
Results
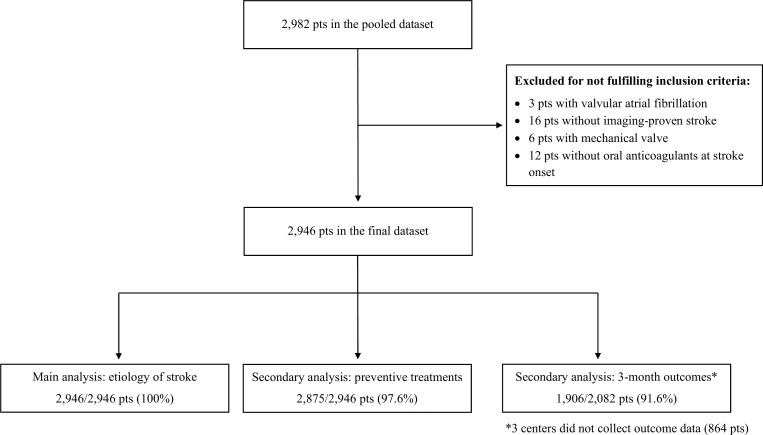
In total, 2946 patients were eligible for analysis. Figure 1 shows the study flowchart and online supplemental Table 1 the centre contributions. The median (IQR) age was 81 (76–86) years, 1404 patients were women (47.7%) and stroke was moderate to severe (National Institutes of Health Stroke Scale 6 (2–14)). At the time of the index stroke, 1674 patients (56.8%) were taking DOAC and 1272 (43.2%) were taking VKA; their detailed characteristics are shown in online supplemental table 2. Plasma level on admission was available for 913 patients on DOAC (54.5%), and INR on admission was available in 1267 patients on VKA (99.6%).
Figure 1.
Study flowchart.
Aetiology of stroke despite anticoagulation
Information on the presumed most likely aetiology of stroke was available for all patients and was classified as competing stroke mechanism in 713 (24.2%), insufficient anticoagulation in 934 (31.7%) and cardioembolism despite sufficient anticoagulation in 1299 (44.1%) patients. The distribution of stroke aetiologies in patients with stroke from January 2012 to June 2016 versus July 2016 to December 2020 did not differ substantially (online supplemental figure 1). The detailed characteristics of all patients stratified to stroke aetiology are presented in table 1.
Table 1.
Patient characteristics stratified to stroke aetiology
| Characteristic | All (N=2946) | N missing | Aetiology of stroke despite anticoagulation | |||
| Competing mechanism (N=713) | Insufficient anticoagulation (N=934) | Cardioembolism despite sufficient anticoagulation (N=1299) | P value | |||
| Demographics | ||||||
| Age, median (IQR), years | 81 (76–86) | 0 | 80 (74–85.1) | 82.45 (77–86.9) | 81 (75–86) | <0.001 |
| Female sex, N (%) | 1404 (47.7) | 0 | 254 (35.6) | 533 (57.1) | 617 (47.5) | <0.001 |
| Risk factors | ||||||
| Hypertension, N (%) | 2649 (89.9) | 0 | 632 (88.6) | 844 (90.4) | 1173 (90.3) | 0.430 |
| Diabetes, N (%) | 871 (29.6) | 0 | 239 (33.5) | 264 (28.3) | 368 (28.3) | 0.029 |
| Dyslipidaemia, N (%) | 1768 (60.3) | 13 | 458 (64.6) | 569 (61.1) | 741 (57.3) | 0.005 |
| Renal impairment, N (%) | 959 (33.2) | 58 | 229 (32.8) | 318 (34.7) | 412 (32.4) | 0.510 |
| Prior ischaemic stroke, N (%) | 984 (33.4) | 0 | 262 (36.7) | 290 (31.0) | 432 (33.3) | 0.052 |
| History of ICH, N (%) | 60 (2.0) | 0 | 13 (1.8) | 14 (1.5) | 33 (2.5) | 0.210 |
| Ischaemic heart disease, N (%) | 905 (30.7) | 0 | 232 (32.5) | 275 (29.4) | 398 (30.6) | 0.400 |
| Bioprosthetic heart valve, N (%) | 151 (5.1) | 0 | 54 (7.6) | 34 (3.6) | 63 (4.8) | 0.001 |
| Current smoking, N (%) | 249 (8.8) | 103 | 79 (11.8) | 69 (7.6) | 101 (8.0) | 0.006 |
| Active malignancy, N (%) | 236 (8.1) | 15 | 79 (11.1) | 63 (6.8) | 94 (7.3) | 0.002 |
| Prestroke mRS ≥3, N (%) | 567 (22.1) | 381* | 118 (18.5) | 198 (24.6) | 251 (22.3) | 0.021 |
| Ipsilateral stenosis ≥50%, N (%) | 452 (15.6) | 54 | 307 (43.4) | 65 (7.2) | 80 (6.3) | <0.001 |
| Ipsilateral stenosis <50%, N (%) | 496 (17.1) | 50 | 100 (14.1) | 200 (21.9) | 196 (15.3) | <0.001 |
| Medication at the time of stroke onset | ||||||
| Oral anticoagulant | 0 | |||||
| VKA, N (%) | 1272 (43.2) | 249 (34.9) | 548 (58.7) | 475 (36.6) | <0.001 | |
| DOAC, N (%) | 1674 (56.8) | 464 (65.1) | 386 (41.3) | 824 (63.4) | ||
| DOAC dose | 32 | |||||
| Full, N (%) | 925 (56.3) | 292 (63.8) | 121 (32.0) | 512 (63.5) | <0.001 | |
| Reduced, N (%) | 717 (43.7) | 166 (36.2) | 257 (68.0) | 294 (36.5) | ||
| DOAC dosing frequency | 215† | |||||
| One time per day, N (%) | 848 (58.1) | 247 (57.7) | 221 (66.4) | 380 (54.4) | <0.001 | |
| Two times per day, N (%) | 611 (41.9) | 181 (42.3) | 112 (33.6) | 318 (45.6) | ||
| DOAC mechanism of action | 0 | |||||
| Thrombin inhibitor, N (%) | 152 (9.1) | 39 (8.4) | 29 (7.5) | 84 (10.2) | 0.270 | |
| Factor Xa inhibitor, N (%) | 1522 (90.9) | 425 (91.6) | 357 (92.5) | 740 (89.8) | ||
| Additional antiplatelet, N (%) | 363 (12.3) | 4 | 119 (16.7) | 112 (12.0) | 132 (10.2) | <0.001 |
| Statin, N (%) | 1354 (46.4) | 30 | 371 (52.3) | 387 (41.7) | 596 (46.6) | <0.001 |
| Antihypertensive(s), N (%) | 2683 (91.9) | 27 | 652 (91.8) | 842 (90.7) | 1189 (92.8) | 0.210 |
| Stroke details | ||||||
| NIHSS on admission, median (IQR) | 6 (2–14) | 33 | 4 (2–10) | 8 (3–16) | 6 (2–14) | <0.001 |
| Intravenous thrombolysis, N (%) | 351 (11.9) | 2 | 46 (6.5) | 211 (22.6) | 94 (7.2) | <0.001 |
| Endovascular treatment, N (%) | 787 (26.8) | 6 | 110 (15.4) | 293 (31.4) | 384 (29.7) | <0.001 |
| Embolic infarct pattern, N (%) | 2317 (81.7) | 111 | 468 (67.3) | 805 (89.6) | 1044 (84.1) | <0.001 |
| Large vessel occlusion, N (%) | 1345 (46.2) | 32 | 241 (34.2) | 513 (55.6) | 591 (46.0) | <0.001 |
| Laboratory parameters on admission | ||||||
| INR, median (IQR) | 1.4 (1.1–1.9) | 100 | 1.4 (1.1–2.0) | 1.3 (1.1–1.6) | 1.4 (1.2–2.2) | <0.001 |
| Low anticoagulant activity, N (%)‡ | 957 (43.9) | 766§ | 128 (26.9) | 633 (82.1) | 196 (21.0) | <0.001 |
| Low VKA activity, N (%) | 737 (58.2) | 96 (39.3) | 528 (96.4) | 113 (23.8) | <0.001 | |
| Low DOAC activity, N (%) | 220 (24.1) | 32 (13.8) | 105 (47.1) | 83 (18.1) | <0.001 | |
| DOAC plasma level, ng/mL, median (IQR) | 83.9 (30–164) | 761§ | 110.1 (54.9–193.6) | 34.6 (1.0–93.5) | 100.9 (44.3–192.6) | <0.001 |
| Outcome at discharge | ||||||
| mRS ≥3, N (%) | 1543 (63.3) | 508¶ | 393 (62.8) | 516 (67.9) | 634 (60.3) | 0.004 |
| In-hospital death, N (%) | 204 (8.4) | 35 (5.6) | 78 (10.3) | 91 (8.7) | 0.007 | |
*Not collected in the centre Berlin (reporting period 2013–2015).
†Not collected in the centre Erlangen.
‡Defined in VKA-treated patients as INR <2.0 and in DOAC-treated patients as plasma level <30 ng/mL.
§DOAC plasma level on admission not collected in the centres Berlin, Mainz and George Washington University.
¶Not collected in the centre Mainz.
DOAC, direct oral anticoagulant; ICH, intracranial haemorrhage; INR, international normalised ratio; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale; VKA, vitamin K-antagonist.
Among patients with competing mechanisms other than AF-related cardioembolism as stroke aetiology, information on the exact competing mechanism was available for 685 of 713 patients (96.1%). Of those, 658 patients (96.1%) had one and 27 (3.9%) had more than one competing stroke mechanism as the most likely stroke aetiology. The most common competing mechanism was large artery atherosclerosis, which was present in 415 (60.6%) patients, followed by small vessel disease (present in 180 (26.3%) patients). Less common aetiologies included coagulopathies (ie, cancer-related coagulopathy, antiphospholipid syndrome and others; 5.3%), peri-interventional stroke (3.4%), endocarditis (3.2%) and other cardio-aortic pathologies (3.8%). There were no substantial differences in the distribution of competing mechanisms among patients with DOAC versus VKA therapy at the time of the index stroke. Details are given in table 2.
Table 2.
Details of competing mechanisms
| Competing mechanism | All (N=685)* | DOAC (N=441) | VKA (N=244) |
| Large artery atherosclerosis, N (%) | 415 (60.6) | 255 (57.8) | 160 (65.6) |
| Small vessel disease, N (%) | 180 (26.3) | 120 (27.2) | 60 (24.6) |
| Coagulopathy†, N (%) | 36 (5.3) | 28 (6.3) | 8 (3.3) |
| Peri-interventional stroke‡, N (%) | 23 (3.4) | 18 (4.1) | 5 (2.0) |
| Endocarditis, N (%) | 22 (3.2) | 14 (3.2) | 8 (3.3) |
| Other cardio-aortic causes§, N (%) | 26 (3.8) | 13 (2.9) | 13 (5.3) |
| Cervical artery dissection, N (%) | 9 (1.3) | 6 (1.4) | 3 (1.2) |
| Vasculitis, N (%) | 4 (0.6) | 2 (0.5) | 2 (0.8) |
*Details were available for 685/713 patients (96.1%) who had competing mechanism as stroke aetiology.
†Including suspected cancer-related coagulopathy, hereditary thrombophilia, myeloproliferative disorders and antiphospholipid syndrome.
‡Including percutaneous transluminal coronary angioplasty, transcatheter aortic valve implantation, pulmonary vein isolation, cardioversion and other cardiovascular procedures.
§Including intracardiac thrombus, aortic dissection, patent foramen ovale/atrial septal defect, heart valve fibroelastoma and other structural heart abnormalities.
DOAC, direct oral anticoagulant; VKA, vitamin K-antagonist.
Preventive treatments
Information on antithrombotic treatment after the index stroke was available for 2875 of 2946 patients (completeness 97.6%). At hospital discharge, 2437 patients (84.8%) were treated with oral anticoagulants, 120 (4.2%) received antiplatelets alone, 286 (9.9%) received no antithrombotic treatment and 32 (1.1%) received parenteral anticoagulation.
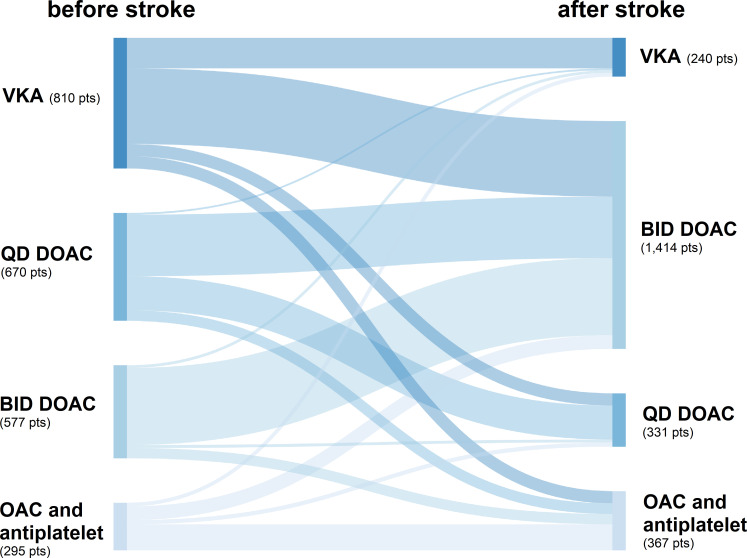
Of patients who received oral anticoagulants, 13.4% were prescribed VKA and 86.8% DOAC, whereby 80.5% received a two times per day DOAC and 66.6% received DOAC at full dose. Antiplatelets as add-on therapy to anticoagulation were prescribed in 367 patients (12.8% of all patients; 15.1% of all patients with anticoagulation), which was more common among those with competing mechanism as stroke aetiology. Most patients were prescribed statins and antihypertensives after the index stroke, and both drug types were more commonly prescribed after stroke due to competing mechanisms than due to other aetiologies. The detailed preventive treatments stratified to stroke aetiology are given in online supplemental table 3. An overview of the changes in oral anticoagulant therapy before versus after stroke is presented in figure 2.
Figure 2.
Changes in oral anticoagulant therapy at the time of the index stroke (before) versus at hospital discharge (after stroke). Patients not receiving oral anticoagulants after stroke and patients with missing type and dosing frequency of anticoagulants before or after stroke are not depicted. BID, two times per day; DOAC, direct oral anticoagulant; OAC, oral anticoagulant; QD, one time per day; VKA, vitamin K-antagonist.
Information on non-pharmacological preventive treatments was available for revascularisation treatments in 2774 of 2946 patients (94.2%) and for left atrial appendage occlusion in 1762 of 2496 patients (59.8%). Revascularisation treatments including carotid endarterectomy or stenting were administered to 94 patients (3.4%) and left atrial appendage occlusion was performed in 17 patients (1.0%), both more commonly among patients with competing mechanisms as stroke aetiology (online supplemental table 3).
3-month outcomes and their association with stroke aetiology
Information on 3-month outcomes was available in all but three centres for 2082 patients in total. Here, information on the primary and secondary endpoint was complete in 1906 (91.6%) and 1842 (88.5%) patients, respectively. The primary endpoint (ie, the composite of recurrent ischaemic stroke, ICH or all-cause death) occurred in 516 patients (27.1%) and the secondary endpoint (ie, recurrent ischaemic stroke) in 84 patients (4.6%) within 3 months. Detailed information on 3-month outcomes is given in table 3.
Table 3.
3-month outcomes according to stroke aetiology
| A. all 3-month outcomes stratified to stroke etiology | |||||
| 3-month outcome | All (N=2082)* | N missing | Stroke etiology | ||
| Competing mechanism (N=533) | Insufficient anticoagulation (N=729) | Cardioembolism despite sufficient anticoagulation (N=820) | |||
| composite outcome, N (%) | 516 (27.1%) | 176 | 125 (25.4%) | 186 (27.8%) | 205 (27.5%) |
| recurrent ischemic stroke, N (%) | 84 (4.6%) | 240 | 33 (6.8%) | 23 (3.6%) | 28 (3.9%) |
| intracranial hemorrhage, N (%) | 15 (0.8%) | 238 | 3 (0.6%) | 6 (0.9%) | 6 (0.8%) |
| all-cause death, N (%) | 434 (22.8%) | 177 | 93 (18.9%) | 164 (24.5%) | 177 (23.8%) |
| mRS ≥3, N (%) | 1,081 (56.7%) | 177 | 258 (52.5%) | 421 (62.9%) | 402 (54.0%) |
| B. Association of stroke etiology with the primary and secondary endpoint | ||||||||||||
| Stroke etiology | Composite outcome | Recurrent ischemic stroke | ||||||||||
| unadjusted | adjusted† | unadjusted | adjusted† | |||||||||
| OR [95%CI] | p value | N events/ total N in model | aOR [95%-CI] | p value | N events/ total N in model | OR [95%-CI] | p value | N events/ total N in model | aOR [95%-CI] | p value | N events/ total N in model | |
| competing stroke mechanism | 0.90 (0.69 to 1.16) | 0.4 | 516/1906 | 1.18 (0.83 to 1.66) | 0.363 | 473/1773 | 1.80 (1.07 to 3.02) | 0.026 | 84/1842 | 1.83 (1.05 to 3.20) | 0.034 | 77/1697 |
| insufficient anticoagulation | 1.02 (0.81 to 1.28) | 0.891 | 0.93 (0.68 to 1.27) | 0.648 | 0.91 (0.52 to 1.60) | 0.751 | 0.99 (0.55 to 1.79) | 0.968 | ||||
| cardioembolism despite sufficient anticoagulation | (reference) | (reference) | (reference) | (reference) | ||||||||
*Adjusted for age, sex, hypertension, diabetes, ischaemic heart disease, dyslipidaemia, renal impairment, prior ischaemic stroke, intracranial haemorrhage, current smoking and active malignancy.
†3-month outcomes not collected in the centres Berlin, Heidelberg and Mainz.
aOR, adjusted OR; mRS, modified Rankin Scale.
Compared with patients with cardioembolism despite sufficient anticoagulation, those with competing mechanisms had higher odds for recurrent ischaemic stroke in unadjusted and adjusted analyses, but not for the composite outcome. The outcomes of patients with stroke due to insufficient anticoagulation did not differ from those with cardioembolism despite sufficient anticoagulation with regard to the primary and secondary endpoints (table 3).
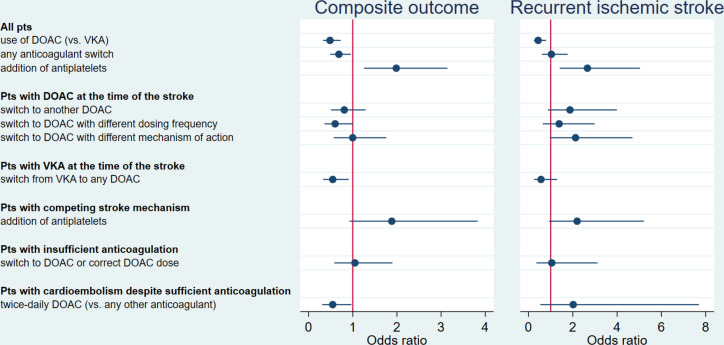
Association of preventive strategies with the primary and secondary endpoint
Figure 3 shows the adjusted estimates for the association of preventive strategies after the index stroke with the primary and secondary endpoints; the detailed unadjusted and adjusted models are given in table 4. Among patients who received oral anticoagulant treatment at hospital discharge and for whom outcome data were available, 1279 (85.4%) patients received DOAC and 219 (14.6%) patients received VKA. Treatment with DOAC versus VKA was associated with lower odds for the primary and secondary endpoints, both in unadjusted and adjusted analyses (table 4). This remained true independent of the type of anticoagulant (DOAC vs VKA) at the time of the index stroke and whether the drug was switched or not after the index stroke in additional models accounting for the anticoagulant type at the time of the index stroke and its interaction with the type of anticoagulant after stroke (composite outcome: aORDOACvs.VKA (95% CI) 0.50 (0.31 to 0.81), pinteraction (before*after)=0.855; recurrent ischaemic stroke: aORDOACvs.VKA (95% CI) 0.47 (0.21 to 1.03), pinteraction (before*after)=0.429).
Figure 3.
Association of preventive strategies after stroke despite anticoagulation with the primary and secondary endpoints from the adjusted models. DOAC, direct oral anticoagulant; Pts, patients; VKA, vitamin K-antagonist; estimates adjusted for age, sex, hypertension, diabetes, ischaemic heart disease, dyslipidaemia, renal impairment, prior ischaemic stroke, history of intracranial haemorrhage, current smoking, active malignancy, use of statins and use of antihypertensives.
Table 4.
Association of preventive strategies after index stroke with the primary and secondary endpoint
| Patients | Preventive strategy | Composite outcome | Recurrent ischaemic stroke | ||||||||||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | ||||||||||
| OR (95%, CI) | P value | N events/total N in model | aOR (95%, CI) | P value | N events/total N in model | OR (95%, CI) | P value | N events/ total N in model | aOR (95%, CI) | P value | N events/ total N in model | ||
| All patients | Use of DOAC (vs VKA) after stroke | 0.49 (0.34 to 0.71) | <0.001 | 194/1498 | 0.49 (0.32 to 0.73) | <0.001 | 179/1394 | 0.51 (0.29 to 0.90) | 0.020 | 69/1489 | 0.44 (0.24 to 0.80) | 0.007 | 62/1368 |
| Any anticoagulant switch | 0.71(0.52 to 0.96) | 0.024 | 194/1498 | 0.69 (0.49 to 0.96) | 0.026 | 179/1394 | 1.03 (0.62 to 1.69) | 0.916 | 69/1489 | 1.03 (0.60 to 1.77) | 0.909 | 62/1368 | |
| Addition of antiplatelets | 1.34 (0.89 to 2.03) | 0.164 | 251/1564 | 1.99(1.25 to 3.15) | 0.004 | 225/1448 | 2.38 (1.31 to 4.32) | 0.004 | 69/1505 | 2.66 (1.40 to 5.04) | 0.003 | 62/1382 | |
| Patients with DOAC at the time of the stroke | Switch to another DOAC | 0.83 (0.54 to 1.27) | 0.380 | 94/829 | 0.81(0.51 to 1.29) | 0.372 | 86/761 | 1.76 (0.89 to 3.47) | 0.105 | 39/826 | 1.87 (0.88 to 3.99) | 0.105 | 33/757 |
| Switch to DOAC with different dosing frequency | 0.65 (0.41 to 1.03) | 0.069 | 89/798 | 0.60 (0.36 to 1.00) | 0.051 | 81/730 | 1.31 (0.67 to 2.58) | 0.436 | 35/794 | 1.38 (0.64 to 2.98) | 0.410 | 29/725 | |
| Switch to DOAC with different mechanism of action | 0.91 (0.55 to 1.52) | 0.722 | 89/799 | 1.00 (0.57 to 1.76) | 0.994 | 81/731 | 2.17 (1.09 to 4.33) | 0.027 | 35/795 | 2.12 (0.96 to 4.69) | 0.063 | 29/726 | |
| Patients with VKA at the time of the stroke | Switch to any DOAC | 0.51 (0.33 to 0.79) | 0.002 | 100/669 | 0.55 (0.33 to 0.91) | 0.019 | 93/621 | 0.50 (0.24 to 1.06) | 0.070 | 30/663 | 0.56 (0.25 to 1.29) | 0.174 | 29/611 |
| Patients with competing stroke mechanism | Addition of antiplatelets | 1.02 (0.56 to 1.87) | 0.936 | 70/414 | 1.88 (0.93 to 3.83) | 0.080 | 63/361 | 1.83 (0.84 to 3.99) | 0.128 | 30/409 | 2.19 (0.92 to 5.21) | 0.075 | 27/359 |
| Patients with insufficient anticoagulation | Switch to DOAC or correct DOAC dose | 0.84 (0.50 to 1.41) | 0.501 | 69/498 | 1.05 (0.58 to 1.90) | 0.874 | 62/467 | 0.87 (0.33 to 2.32) | 0.778 | 17/480 | 1.05 (0.35 to 3.12) | 0.930 | 16/402 |
| Patients with cardioembolism despite sufficient anticoagulation | Two times per day DOAC (vs any other anticoagulant) | 0.29 (0.18 to 0.45) | <0.001 | 96/617 | 0.55 (0.31 to 0.97) | 0.039 | 86/576 | 2.20 (0.64 to 7.56) | 0.212 | 21/592 | 2.02 (0.53 to 7.69) | 0.305 | 18/555 |
*Adjusted for age, sex, hypertension, diabetes, ischaemic heart disease, dyslipidaemia, renal impairment, prior ischaemic stroke, intracranial haemorrhage, current smoking, active malignancy, use of statins, use of antihypertensives.
aOR, adjusted OR; DOAC, direct oral anticoagulant; VKA, vitamin K-antagonist.
Any anticoagulant switch and switch from VKA to DOAC were associated with lower odds for the composite outcome, but not for recurrent stroke. Among patients with cardioembolism despite sufficient anticoagulation, the use of two times per day DOAC was associated with lower odds for the composite outcome, but not for recurrent stroke. No other strategy was associated with lower odds for any of the endpoints, while the addition of antiplatelets to anticoagulants was even associated with higher odds for the primary and secondary endpoints.
A post-hoc analysis focusing on the combined endpoint of recurrent ischaemic stroke and ICH revealed largely consistent results. Among patients treated with VKA at the time of the index stroke, switching to any DOAC was associated with lower odds for this combined endpoint (online supplemental table 4).
Discussion
This study revealed the following key findings: (1) The aetiology of stroke despite anticoagulation in patients with AF is heterogeneous, with about one out of four cases attributable to competing stroke mechanisms and about one out of three to insufficient anticoagulation, while AF-related cardioembolism despite sufficient anticoagulation was the most common aetiology. (2) Following stroke despite anticoagulation, unfavourable outcomes are common and recurrence rate is high. (3) Anticoagulation with DOAC was linked to better outcomes than VKA after stroke despite anticoagulation, while additional antiplatelet therapy was not associated with better outcomes.
Among patients with a competing mechanism other than AF-related cardioembolism as the most likely stroke aetiology, large artery atherosclerosis and small vessel disease were the most frequent mechanisms. Previous case–control and cohort studies on anticoagulated patients with AF demonstrated that vascular risk factors such as diabetes17 and dyslipidaemia,17 18 but also large artery atherosclerosis17 19 and small vessel disease20 per se were associated with higher stroke risk. In line with this, a previous single-centre study on patients with AF and stroke despite anticoagulation using the ASCOD classification (A: atherosclerosis; S: small-vessel disease; C: cardiac pathology; O: other causes; D: dissection) indicated that the coexistence of competing stroke mechanisms is common.6 These findings stress the importance of a thorough work-up in patients with AF and stroke despite anticoagulation in order to uncover non-cardioembolic pathologies that might be less responsive to anticoagulation and warrant additional preventive therapies. Of note, our data indicated that underlying coagulopathies may—less commonly—also account for stroke despite anticoagulation in patients with AF. In these cases, abnormal blood count findings, elevated lactate dehydrogenase, C-reactive protein and particularly D-dimer levels should raise suspicion and prompt further testing including haematological work-up and cancer screening with imaging of the chest and abdomen to uncover potential relevant comorbidities such as myeloproliferative or other neoplasms.21–23
Our study further highlights the problem of insufficient anticoagulation as an important aetiology of stroke despite anticoagulation in patients with AF. Prior reports either lacked this information8–10 or were of small sample size.18 Our definition of insufficient anticoagulation comprised not only self-reported non-adherence and inappropriately low DOAC dosing, combining findings from previous studies,18 24 25 but also included the anticoagulant activity measured on admission. For this, DOAC level was available in over 50% of DOAC-treated patients and INR in almost all VKA-treated patients in our data set. While low time in therapeutic range among VKA-treated patients has been previously reported as a contributor to stroke risk in patients with AF,26 only few data about DOAC levels existed in this context so far.6 27 Our finding that a relevant proportion of stroke despite anticoagulation is attributable to insufficient anticoagulation is important because these strokes may potentially be preventable. Such prevention strategies would entail interventions to increase physicians’ awareness about the importance of per-label dosing, and also ways of identifying patients at high risk for non-adherence,28 a more nuanced evaluation of drug intake behaviour29 and adherence-enhancing interventions.30
Another main finding of our study is that the largest proportion of stroke despite anticoagulation was attributable solely to AF-related cardioembolism without evidence for insufficient anticoagulation or competing mechanisms. The profile of these patients resembled more the profile of patients with insufficient anticoagulation in terms of traditional cardiovascular risk factors and neuroimaging characteristics than the profile of patients with competing stroke mechanisms. This suggests shared stroke mechanisms in these patients, in whom inadequate anticoagulant activity might be ultimately implicated. Besides non-adherence and inappropriate dosing leading to insufficient anticoagulation, emerging evidence suggests that a high inter-individual variation in DOAC pharmacokinetics and pharmacodynamics exists, which may be attributable to genetic factors.31 More research is needed to evaluate whether tailored pharmacogenomics approaches might mitigate the risk of AF-related cardioembolism despite anticoagulation.
Furthermore, our data show that the burden of unfavourable outcomes within 3 months after stroke despite anticoagulation is high, expanding on findings from previous smaller studies that focused mostly on ischaemic stroke recurrence.8–10 In our study, over one out of five patients died and over one out of two patients had a mRS ≥3 at 3 months. While ICH occurred infrequently at <1%, 4.6% of patients suffered ischaemic stroke recurrence, clearly identifying this patient group as high risk and stressing the need to define optimal treatment strategies.
Overcoming limitations of previous studies, the large sample size of this pooled analysis enabled us to comprehensively investigate a series of preventive strategies. Regardless of the type of anticoagulant at the time of the index stroke, treatment with DOAC after the index stroke was associated with lower odds for both the primary and secondary endpoints as opposed to treatment with VKA, even after adjustment for several outcome-modifying variables. Although residual confounding by indication—potentially left unaccounted for despite adjustment—may have influenced this finding by introducing bias against VKA, our data are reassuring for the use of DOAC and support the current guidelines for recurrent stroke prevention which recommend DOAC in preference over VKA,12 providing new evidence for patients with stroke despite anticoagulation.
In contrast to widespread practice, our data do not suggest that any specific switch between DOAC (including switching to different DOAC, or to DOAC with different dosing frequency or mechanism of action) may lead to better outcomes in patients with stroke while on DOAC therapy. Importantly, we found that adding antiplatelets to anticoagulants was not linked to better outcomes, but was instead associated with higher odds for both the primary and secondary endpoints. This finding expands on previous research showing no better or even worse cardiovascular outcomes in anticoagulated patients with AF and add-on antiplatelets,32 33 indicating that this seems to apply also to patients with stroke despite anticoagulation. It is possible that residual confounding by indication that remained unaccounted for despite extensive adjustment for comorbidities may have influenced this finding, as discussed previously.33
The rates of the primary and secondary endpoints in our study were high, although most patients were treated with DOAC after stroke. This indicates that novel approaches to prevent stroke recurrence are needed in these patients. Besides strategies to optimise the currently available drug treatments discussed above, novel pharmacological approaches, such as factor XIa inhibitors,34 or non-pharmacological interventional treatments, including the percutaneous occlusion of the left atrial appendage,35 might advance stroke prevention in AF. Notably, surgical occlusion of the left atrial appendage was shown to confer additional protection against stroke when added to anticoagulation in a recent trial.36
Strengths and limitations
The strengths of this study include (i) its large sample size; (ii) the detailed patient characterisation with high data completeness, allowing for a large number of analyses with extensive adjustment for confounders and limiting the risk of spurious findings; (iii) the standardised classification of the stroke aetiology incorporating DOAC plasma levels, which were available in the majority of participating centres; and (iv) the homogeneity of the study population, which included only patients with imaging-confirmed stroke and previously known AF as the sole indication for anticoagulation.
We are aware of the following limitations: (i) Data were in part collected retrospectively rather than prospectively ascertained; (ii) Although experienced investigators determined the most likely stroke aetiology, inherent limitations in the determination of competing stroke mechanisms may have led to misclassification of the stroke aetiology, and heterogeneity among the participating centres may have introduced bias in the classification; (iii) Local investigators classified the stroke aetiology as insufficient anticoagulation using a standardised definition, but availability of coagulation measurements (DOAC plasma levels vs INR for VKA) differed. This is a potential source of bias, as it decreases the likelihood of patients on VKA (and increases the likelihood of patients on DOAC) to be classified as ‘AF-related cardioembolism despite sufficient anticoagulation’ and may have caused more patients on VKA (and less patients on DOAC) to be classified as ‘insufficient anticoagulation’; (iv) The observational design of the study allowed only the assessment of association between treatment strategies and outcomes, but not causality thereof. Importantly, despite extensive adjustment for comorbidities, indication bias may still have confounded our findings, potentially contributing to the worse outcomes of patients treated with VKA or add-on antiplatelets after stroke despite anticoagulation. These results should therefore be interpreted cautiously, better serving as hypothesis-generating for potential future randomised trials that are necessary to provide robust evidence; (v) Despite the large sample size, the short follow-up time of 3 months may have limited the number of outcomes, thus disallowing the detection of their association with treatment strategies; (vi) With only 17 patients undergoing left atrial appendage occlusion in our observational data set, no meaningful statistical analyses for this preventive strategy were possible; (vii) The limited number of ICH events disallowed statistical analysis of ICH as a separate outcome. Finally, we did not consider extracranial bleeding in our analyses, as this outcome was not collected during follow-up.
In conclusion, this study on ischaemic stroke despite anticoagulant therapy in patients with AF showed that the aetiology of stroke is heterogeneous and unfavourable outcomes are common. While DOAC treatment after stroke despite anticoagulation was associated with better outcomes than VKA, add-on antiplatelets were linked to worse outcomes; further research into more personalised and novel preventive strategies is warranted.
Acknowledgments
We thank all collaborators, listed in Supplementary Table 1, for their contribution to data collection.
Footnotes
Twitter: @TotoMynell, @TweetNeuroLine
AAP and TRM contributed equally.
JCP and DJS contributed equally.
Presented at: European Stroke Organisation Conference 2021
Collaborators: Stefan T Engelter, Philippe A Lyrer, Leo H Bonati, Christopher Traenka, Alexandros A Polymeris, Annaelle Zietz, Lilian Kriemler, Nils Peters, Gian Marco De Marchis, Sebastian Thilemann, Henrik Gensicke, Lisa Hert, Benjamin Wagner, Fabian Schaub, Louisa Meya, Nikolaos Symeon Avramiotis, Joachim Fladt, Tolga Dittrich, Urs Fisch, Jan F Scheitz, Christian H Nolte, Karl Georg Haeusler, Simon Hellwig, Markus G Klammer, Simon Litmeier, Thomas R Meinel, Urs Fischer, David J Seiffge, Lorenz Grunder, Marcel Arnold, Simon Jung, Jan Gralla, Christoph Stretz, Shadi Yaghi, Xing (Cathy) Dai, Svenja Stoll, Ruihao Wang, Bernd Kallmünzer, Christopher R Leon Guerrero, Iman Moeini-Naghani, Hannah Oehler, Kyra Hoelscher, Peter Ringleb, Jan C Purrucker, Patrik Michel, Davide Strambo, Alexander Salerno, Giovanni Bianco, Carlo W Cereda, Timo Uphaus, Klaus Gröschel, Mira Katan, Susanne Wegener
Contributors: DJS acts as guarantor for this study and takes full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish. AAP, TRM, JCP, DJS: design and study conception; data acquisition and analysis; first manuscript draft. All authors: data acquisition and analysis; critical manuscript revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: JFS: grant from Corona-Stiftung, outside the submitted work. CHN: grants from German Ministry of Research and Education, German Center for Neurodegenerative Diseases, German Center for Cardiovascular Research; speaker and/or consultation fees from Bayer, Boehringer Ingelheim, Bristol Myers Squibb (BMS), Pfizer, Alexion, Daiichi-Sankyo, Abbott, W.L. Gore and Associates. CS: departmental funding from Massachusetts General Hospital for the Neuro-AF study. SY: steering committee member Neuro-AF study, non-funded; research collaboration Medtronic, non-funded. KGH: speaker’s honoraria, consulting fees, lecture honoraria and/or grants from Abbott, Alexion, AMARIN, AstraZeneca, Bayer, Sanofi, Boehringer Ingelheim, Daiichi Sankyo, Pfizer, BMS, Biotronik, Medtronic, Premier Research, Portola, W.L. Gore and Associates, Sun Pharma, Edwards Lifesciences. CC: grants from Swiss Heart Foundation (SHF); other support from iSchemaView and Bayer, outside the submitted work. KG: personal fees and/or non-financial support from Alexion Germany GmbH, Abbott Medical, Bayer Vital GmbH, Boehringer Ingelheim, BMS, Daiichi Sankyo, outside the submitted work. MK: funding from Swiss National Science Foundation (SNSF), SHF; contributions from BRAHMS Thermo Fisher, Roche; advisory fees from Bayer, AstraZeneca, Medtronic. SW: research support from SNSF, Olga Mayenfisch Foundation, University of Zurich CRPP stroke; speaker honoraria from Amgen; travel honoraria from Bayer; research grant from Boehringer Ingelheim. STE: research grants from SNSF, SHF, research support from Daiichi Sankyo; educational grant from Pfizer, compensation from Stago for educational material; travel/speaker honoraria from Bayer, Boehringer Ingelheim, BMS, Daiichi Sankyo; advisory board Bayer, Boehringer Ingelheim, BMS. PAR: speaker’s honoraria and lecture fees from Bayer, Boehringer Ingelheim, Daiichi Sankyo, Pfizer, outside the submitted work. UF: research support from the SNSF (32003B_197009), SHF, Medtronic; consultant for Medtronic, Stryker, CSL Behring; advisory board Portola/Alexion (money paid to institution). BK: consultant fees and travel expenses from Bayer, Daiichi Sankyo, Pfizer, Medtronic, outside the submitted work. JCP: consultation fees and travel expenses from Akcea, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Pfizer, outside the submitted work. DJS: advisory board for Bayer Switzerland AG and Portola/Alexion, research funding from SNSF, SHF, Bangerter-Rhyner Foundation, Swiss Society of Neurology, Bayer Foundation. The remaining authors declare no conflicts of interest.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The use and pooling of de-identified patient data from all Swiss centres participating in the study and the study itself were approved by the responsible ethics committee (Cantonal Ethics Committee Bern (Kantonale Ethikkommission (KEK) Bern) 2019–01010). The requirement for additional local ethical approval differed among non-Swiss participating centres and was acquired by the local principal investigators if necessary.
References
- 1. Diener H-C, Connolly SJ, Ezekowitz MD, et al. Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE-LY trial. Lancet Neurol 2010;9:1157–63. 10.1016/S1474-4422(10)70274-X [DOI] [PubMed] [Google Scholar]
- 2. Hankey GJ, Patel MR, Stevens SR, et al. Rivaroxaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of rocket AF. Lancet Neurol 2012;11:315–22. 10.1016/S1474-4422(12)70042-X [DOI] [PubMed] [Google Scholar]
- 3. Easton JD, Lopes RD, Bahit MC, et al. Apixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: a subgroup analysis of the ARISTOTLE trial. Lancet Neurol 2012;11:503–11. 10.1016/S1474-4422(12)70092-3 [DOI] [PubMed] [Google Scholar]
- 4. Rost NS, Giugliano RP, Ruff CT, et al. Outcomes with edoxaban versus warfarin in patients with previous cerebrovascular events: findings from engage AF-TIMI 48 (effective anticoagulation with factor Xa next generation in atrial Fibrillation-Thrombolysis in myocardial infarction 48). Stroke 2016;47:2075–82. 10.1161/STROKEAHA.116.013540 [DOI] [PubMed] [Google Scholar]
- 5. Gadsbøll K, Staerk L, Fosbøl EL, et al. Increased use of oral anticoagulants in patients with atrial fibrillation: temporal trends from 2005 to 2015 in Denmark. Eur Heart J 2017;38:658–906. 10.1093/eurheartj/ehw658 [DOI] [PubMed] [Google Scholar]
- 6. Purrucker JC, Hölscher K, Kollmer J, et al. Etiology of ischemic strokes of patients with atrial fibrillation and therapy with anticoagulants. J Clin Med 2020;9. 10.3390/jcm9092938. [Epub ahead of print: 11 09 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meinel TR, Branca M, De Marchis GM, et al. Prior anticoagulation in patients with ischemic stroke and atrial fibrillation. Ann Neurol 2021;89:42–53. 10.1002/ana.25917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Seiffge DJ, De Marchis GM, Koga M, et al. Ischemic stroke despite oral anticoagulant therapy in patients with atrial fibrillation. Ann Neurol 2020;87:677–87. 10.1002/ana.25700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yaghi S, Henninger N, Giles JA, et al. Ischaemic stroke on anticoagulation therapy and early recurrence in acute cardioembolic stroke: the IAC study. J Neurol Neurosurg Psychiatry 2021;92:1062–7. 10.1136/jnnp-2021-326166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tanaka K, Koga M, Lee K-J, et al. Atrial fibrillation-associated ischemic stroke patients with prior anticoagulation have higher risk for recurrent stroke. Stroke 2020;51:1150–7. 10.1161/STROKEAHA.119.027275 [DOI] [PubMed] [Google Scholar]
- 11. Stretz C, Wu TY, Wilson D, et al. Ischaemic stroke in anticoagulated patients with atrial fibrillation. J Neurol Neurosurg Psychiatry 2021;92:1164–72. 10.1136/jnnp-2020-323963 [DOI] [PubMed] [Google Scholar]
- 12. Kleindorfer DO, Towfighi A, Chaturvedi S. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American heart Association/American stroke association. Stroke 2021;52:e364–467. 10.1161/STR.0000000000000375 [DOI] [PubMed] [Google Scholar]
- 13. Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. definitions for use in a multicenter clinical trial. TOAST. trial of ORG 10172 in acute stroke treatment. Stroke 1993;24:35–41. 10.1161/01.STR.24.1.35 [DOI] [PubMed] [Google Scholar]
- 14. Drouet L, Bal Dit Sollier C, Steiner T, et al. Measuring non-vitamin K antagonist oral anticoagulant levels: when is it appropriate and which methods should be used? Int J Stroke 2016;11:748–58. 10.1177/1747493016659671 [DOI] [PubMed] [Google Scholar]
- 15. Seiffge DJ, Paciaroni M, Wilson D, et al. Direct oral anticoagulants versus vitamin K antagonists after recent ischemic stroke in patients with atrial fibrillation. Ann Neurol 2019;85:823–34. 10.1002/ana.25489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. von Elm E, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paciaroni M, Agnelli G, Ageno W, et al. Risk factors for cerebral ischemic events in patients with atrial fibrillation on warfarin for stroke prevention. Atherosclerosis 2010;212:564–6. 10.1016/j.atherosclerosis.2010.06.016 [DOI] [PubMed] [Google Scholar]
- 18. Paciaroni M, Agnelli G, Caso V, et al. Causes and risk factors of cerebral ischemic events in patients with atrial fibrillation treated with non-vitamin K antagonist oral anticoagulants for stroke prevention. Stroke 2019;50:2168–74. 10.1161/STROKEAHA.119.025350 [DOI] [PubMed] [Google Scholar]
- 19. Lehtola H, Airaksinen KEJ, Hartikainen P, et al. Stroke recurrence in patients with atrial fibrillation: concomitant carotid artery stenosis doubles the risk. Eur J Neurol 2017;24:719–25. 10.1111/ene.13280 [DOI] [PubMed] [Google Scholar]
- 20. Du H, Wilson D, Ambler G, et al. Small vessel disease and ischemic stroke risk during anticoagulation for atrial fibrillation after cerebral ischemia. Stroke 2021;52:91–9. 10.1161/STROKEAHA.120.029474 [DOI] [PubMed] [Google Scholar]
- 21. Kargiotis O, Psychogios K, Safouris A, et al. The role of transcranial Doppler monitoring in patients with Multi-Territory acute embolic strokes: a review. J Neuroimaging 2019;29:309–22. 10.1111/jon.12602 [DOI] [PubMed] [Google Scholar]
- 22. Stefanou MI, Richter H, Härtig F, et al. Recurrent ischaemic cerebrovascular events as presenting manifestations of myeloproliferative neoplasms. Eur J Neurol 2019;26:903–64. 10.1111/ene.13907 [DOI] [PubMed] [Google Scholar]
- 23. Navi BB, Iadecola C. Ischemic stroke in cancer patients: a review of an underappreciated pathology. Ann Neurol 2018;83:873–83. 10.1002/ana.25227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ozaki AF, Choi AS, Le QT, et al. Real-world adherence and persistence to direct oral anticoagulants in patients with atrial fibrillation: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2020;13:e005969. 10.1161/CIRCOUTCOMES.119.005969 [DOI] [PubMed] [Google Scholar]
- 25. Steinberg BA, Shrader P, Pieper K, et al. Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes Registry for better informed treatment of atrial fibrillation II). J Am Heart Assoc 2018;7. 10.1161/JAHA.117.007633. [Epub ahead of print: 16 02 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lehto M, Niiranen J, Korhonen P, et al. Quality of warfarin therapy and risk of stroke, bleeding, and mortality among patients with atrial fibrillation: results from the nationwide FinWAF registry. Pharmacoepidemiol Drug Saf 2017;26:657–65. 10.1002/pds.4194 [DOI] [PubMed] [Google Scholar]
- 27. Seiffge DJ, Kägi G, Michel P, et al. Rivaroxaban plasma levels in acute ischemic stroke and intracerebral hemorrhage. Ann Neurol 2018;83:451–9. 10.1002/ana.25165 [DOI] [PubMed] [Google Scholar]
- 28. Polymeris AA, Traenka C, Hert L, et al. Frequency and determinants of adherence to oral anticoagulants in stroke patients with atrial fibrillation in clinical practice. Eur Neurol 2016;76:187–93. 10.1159/000450750 [DOI] [PubMed] [Google Scholar]
- 29. Albert V, Polymeris AA, Dietrich F, et al. Insights into direct oral anticoagulant therapy implementation of stroke survivors with atrial fibrillation in an ambulatory setting. J Stroke Cerebrovasc Dis 2021;30:105530. 10.1016/j.jstrokecerebrovasdis.2020.105530 [DOI] [PubMed] [Google Scholar]
- 30. Polymeris AA, Albert V, Hersberger KE, et al. Protocol for MAAESTRO: electronic monitoring and improvement of adherence to direct oral anticoagulant Treatment-A randomized crossover study of an educational and Reminder-Based intervention in ischemic stroke patients under polypharmacy. Front Neurol 2018;9:1134. 10.3389/fneur.2018.01134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Raymond J, Imbert L, Cousin T, et al. Pharmacogenetics of direct oral anticoagulants: a systematic review. J Pers Med 2021;11. doi: 10.3390/jpm11010037. [Epub ahead of print: 11 01 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Flaker GC, Gruber M, Connolly SJ, et al. Risks and benefits of combining aspirin with anticoagulant therapy in patients with atrial fibrillation: an exploratory analysis of stroke prevention using an oral thrombin inhibitor in atrial fibrillation (SPORTIF) trials. Am Heart J 2006;152:967–73. 10.1016/j.ahj.2006.06.024 [DOI] [PubMed] [Google Scholar]
- 33. Fox KAA, Velentgas P, Camm AJ, et al. Outcomes associated with oral anticoagulants plus antiplatelets in patients with newly diagnosed atrial fibrillation. JAMA Netw Open 2020;3:e200107. 10.1001/jamanetworkopen.2020.0107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Katsanos AH, Kamel H, Healey JS, et al. Stroke prevention in atrial fibrillation: looking forward. Circulation 2020;142:2371–88. 10.1161/CIRCULATIONAHA.120.049768 [DOI] [PubMed] [Google Scholar]
- 35. Osmancik P, Herman D, Neuzil P, et al. Left atrial appendage closure versus direct oral anticoagulants in high-risk patients with atrial fibrillation. J Am Coll Cardiol 2020;75:3122–35. 10.1016/j.jacc.2020.04.067 [DOI] [PubMed] [Google Scholar]
- 36. Whitlock RP, Belley-Cote EP, Paparella D, et al. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med 2021;384:2081–91. 10.1056/NEJMoa2101897 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jnnp-2021-328391supp001.pdf (302.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.