Abstract
Purpose of review:
The latest national data reports a 55% prevalence of metabolic syndrome in American Indian adults compared to 34.7% of the general US adult population. Metabolic syndrome is a strong predictor for diabetes, which is the leading cause of heart disease in American Indian and Alaska Native populations. Metabolic syndrome and associated risk factors disproportionately impacts this population. We describe the presentation, etiology, and roles of structural racism and social determinants of health on metabolic syndrome.
Findings:
Much of what is known about metabolic syndrome in American Indian and Alaska Native populations comes from the Strong Heart Study as there is scant literature. American Indian and Alaska Native adults have an increased propensity towards metabolic syndrome as they are 1.1 times more likely to have high blood pressure, approximately three times more likely to have diabetes, and have higher rates of obesity compared with their non-Hispanic White counterparts. Culturally informed lifestyle and behavior interventions are promising approaches to address structural racism and social determinants of health that highly influence factors contributing to these rates.
Summary:
Among American Indian and Alaska Native populations, there is scarce updated literature evaluating the underlying causes of major risk factors for metabolic syndrome, and progression to cardiometabolic disease. As a result, the actual state of metabolic syndrome in this population is not well understood. Systemic and structural changes must occur to address the root causes of these disparities.
Keywords: American Indian, Alaska Native, indigenous populations, metabolic syndrome, metabolic disease, cardiovascular disease, cardiovascular abnormalities, social determinants of health, racism
INTRODUCTION
Metabolic syndrome disproportionately impacts American Indian and Alaska Native populations compared to non-Hispanic White populations [1, 2]. Metabolic syndrome is associated with cardiovascular comorbidities including diabetes and heart disease as well as cardiovascular death [3], but metabolic syndrome has only been independently associated with diabetes in American Indian populations [4–6]. This is of particular importance since diabetes is the leading cause of heart disease in American Indian and Alaska Native populations [7, 8]. However, this does not diminish the role of other components of metabolic syndrome such as hypertension which confers higher risk of cardiovascular morbidity and death [2, 4, 7]. To strategically address metabolic syndrome in American Indian and Alaska Native populations, it is important to understand the presentation, roles of structural racism and social determinants of health, management strategies, and areas for future investigation.
PRESENTATION AND ETIOLOGY OF METABOLIC SYNDROME
Metabolic syndrome is a condition in which the presence of interrelated metabolic risk factors for cardiovascular disease and diabetes concomitantly occur [7, 8]. Components of metabolic syndrome include: 1) Blood pressure with a systolic ≥130 and/or diastolic ≥85 mm Hg, 2) triglyceride levels ≥150 mg/dL (1.7 mmol/L), 3) high-density lipoprotein cholesterol levels <40 mg/dL (1.0 mmol/L) in males and <50 mg/dL (1.3 mmol/L) in females; 4) fasting glucose ≥100 mg/dL and 5) central obesity [7, 8]. From these components, three out of five abnormal findings, or pharmacological treatment for any of the components, are diagnostic criteria for a clinical diagnosis. Individuals with metabolic syndrome are twice as likely to develop cardiovascular disease and have a five-fold increased risk for developing type 2 diabetes compared to those without the syndrome [7]. Although these statistics are not specific to American Indian and Alaska Native populations, these groups experience disproportionate rates of the components of metabolic syndrome [4, 5, 9–11]. There is an increased overall prevalence for reported hypertension in American Indian and Alaska Native men (31.3% vs 26.5%) and women (28.2% vs 22.4%) compared to non-Hispanic White men and women [4]. In 2018, American Indian and Alaska Native adults were at a 1.1 times more likely to have high blood pressure [9], and approximately three times more likely to have diabetes than non-Hispanic White adults [11]. Additionally, data from the 2000–2010 Behavioral Risk Factor Surveillance System (BRFSS) display higher rates of obesity among American Indian and Alaska Native men and women compared with their non-Hispanic White counterparts (33.9% vs 23.3% for men and 35.5% vs 21.0% for women, respectively) [4].
As with other data published, American Indian people have been left out of national estimates of metabolic syndrome. Both historically and in modern times, American Indian and Alaska Native groups have not been included, undersampled, and/or aggregated as “Other” in publications reporting on national surveys, including various iterations of the National Health and Nutrition Examination Survey (NHANES) and the Centers for Disease Control and Prevention (CDC) [12–14]. In addition, few population studies have examined metabolic syndrome among American Indian and Alaska Native adults. Much of what is known about the prevalence of metabolic syndrome in American Indian and Alaska Native communities comes from the Strong Heart Study [1, 6, 14, 15], the Education and Research Toward Health (EARTH) study [2, 14, 16], and the Center for Alaska Native Health Research Study (CANHR) [17], with all being conducted more than a decade ago.
The largest population study to report on metabolic syndrome among American Indian populations is the Strong Heart Study [1, 6, 14, 15]. In this study [1], the overall prevalence for metabolic syndrome was 55% in American Indian adults (aged 45–74 years), approximately 2,502 participants (N=4,549), compared to 34.7% of the general US adult population in the 2011–2016 National Health and Nutrition Examination Survey (NHANES) [12]. The EARTH study reported a 5.2% lower overall participant prevalence (N=4,457) than the Strong Heart Study [14]. Mean ages were not reported in this study but groups were examined by age categories, with prevalence generally increasing with age [14]. Females had an 8.6% (age-adjusted) higher prevalence than males in this study (53.2% versus 44.6%) [14]. The CANHR Study, conducted among Alaska Native populations, reported the lowest prevalence of metabolic syndrome (Table).
Table.
Studies reporting Metabolic Syndrome among American Indian and/or Alaska Native Groups
| Study | Location of study participants and Tribes (if reported) | Age range included | Total participants (N) | Total with MS (%) | Males with MS (%) | Females with MS (%) |
|---|---|---|---|---|---|---|
| Adults | ||||||
| Strong Heart [11, 14, 15] |
Arizona: • Pima Maricopa • Salt River North Dakota: • Devil’s Lake Sioux Oklahoma: • Apache • Caddo • Comanche • Delaware • Ft Sill Apache • Kiowa • Wichita South Dakota: • Cheyenne River Sioux • Oglala Sioux |
45–74 | 4,549 | 55%-All 35% (non-diabetic) |
Not reported | Not reported |
| EARTH [14, 16] |
Alaska Arizona: • Gila River • Navajo New Mexico: • Navajo Northern Plains Utah: • Navajo |
18–88 | 4,457 | 49.8%-All 42.4% (non-diabetic) |
44.6% | 53.2% |
| EARTH [2] | All participants | 20+ | 9,696 | 74.9% | 34.9% | 40.0% |
| Alaska | 3,498 | 57.7% | 26.5% | 31.2% | ||
| Southwest Region | 4,534 | 90.5% | 43.2% | 47.3% | ||
| CANHR [17] |
Southwest Alaska: • Yup’ik Eskimos |
18+ | 710 | 14.7% | 8.6% | 19.8% |
| Youth-Young Adult | ||||||
| Strong Heart [6] | 14–20 | 446 (non-diabetic) | 111 | 11% | 13.9% | |
MS= Metabolic syndrome
Published data on metabolic syndrome among American Indian and Alaska Native youth is even more sparse than for adults. The Strong Heart Study has reported the largest sample of metabolic syndrome among youth ages 14–20 to date. This study began to enroll younger participants in 2001–2003 and found that approximately 24.9% of youth without diabetes had metabolic syndrome [6].
STRUCTURAL RACISM AND SOCIAL DETERMINANTS OF HEALTH
To better understand the larger context of metabolic syndrome in American Indian and Alaska Native populations, the influence of structural racism and certain social determinants of health (e.g., built environment, economic stability, education access and quality, and healthcare access and quality) must be described. Additionally, trauma, racism, and discrimination are linked to poor health outcomes, including components of metabolic syndrome [5, 18, 19]. American Indian and Alaska Native people have long-experienced structural discrimination and oppression that have shaped social circumstances contributing to contemporary cardiometabolic disease disparities and poor health outcomes [19]. Historical and intergenerational trauma describe the collective trauma imposed on a group of people who have a specific group identity and is often used to characterize the multigenerational nature of distress experienced across the lifespan and by American Indian and Alaska Native communities as a whole [18]. Long-lasting effects from European colonization (i.e., loss of ancestral lands through forced relocation, commodity food programs, etc.), and genocidal events and practices (i.e., massacres such as Wounded Knee, introduction of infectious diseases, boarding schools, cultural assimilation, etc.) continue to perpetuate health inequities that significantly contribute to risk factors of metabolic syndrome [5, 18].
Many tribal nations are in rural remote areas that have a higher risk for air pollution and metal exposure, both of which contribute to major risk factors for metabolic syndrome [5, 20, 21]. Several studies have demonstrated that American Indian communities are disproportionally affected by exposure to environmental chemicals and toxic metals including arsenic, cadmium, uranium, and tungsten [5, 20, 21]. Exposure to toxic metals places these communities at increased risk of cardiovascular disease, particularly for those with diabetes [5, 20, 21].
The forced relocation of American Indian and Alaska Native populations into remote regions generated a barrier from continuing agricultural practices due to the loss of traditional lands, creating a dependency on government commodity food programs [18, 19]. The food provided to these communities was often high-calorie and nutrient poor, promoting dietary habits that have likely contributed to existing high rates of diet-related cardiometabolic diseases in American Indian and Alaska Native communities [18]. Still, today, food insecurity affects over 25% of American Indian and Alaska Native members on over 60 tribal reservations [22]. Sustained, traditional agriculture has been challenged by limited water access and low resource availability for farming [19]. Access to healthy food is affected by geographical isolation and the lack of inexpensive, accessible food sources on tribal lands, resulting in food deserts for many American Indian and Alaska Native communities [19]. For example, there are only 13 grocery stores on the Navajo Nation which is over 27,000 square miles stretching across the states of Colorado, Utah, Arizona, and New Mexico and is home to more than 300,000 people [22]. Often residents must drive several hours to buy food at the grocery store. Food available at gas stations and trading posts are more readily accessible but do not offer the nutrient rich benefits fresh produce contains. Food insecurity and the quality of food obtainable by people are closely correlated to socioeconomic status and financial means [18].
Socioeconomic status and level of education are significant social determinants of health that heavily influence the prevalence of metabolic syndrome for American Indian and Alaska Native people and present challenges in access to preventative health and treatment services [5, 18, 19, 21]. American Indian and Alaska Native populations experience the highest level of poverty in comparison to all racial and ethnic groups and have some of the lowest educational attainment rates in the nation [18]. In 2017, the median household income for American Indian and Alaska Native families was $41,882, with nearly one-fourth living below the poverty line, which is 143% higher than non-Hispanic White families [5]. For education, age-adjusted rates show 20.5% of American Indian and Alaska Native adults do not have a high school degree compared to 10% of non-Hispanic White adults [5]. Unemployment rates have also been shown to be as much as three times higher in American Indian and Alaska Native populations [5]. All of these factors are likely to not only contribute to metabolic syndrome, but also overall health disparities for American Indian and Alaska Native populations.
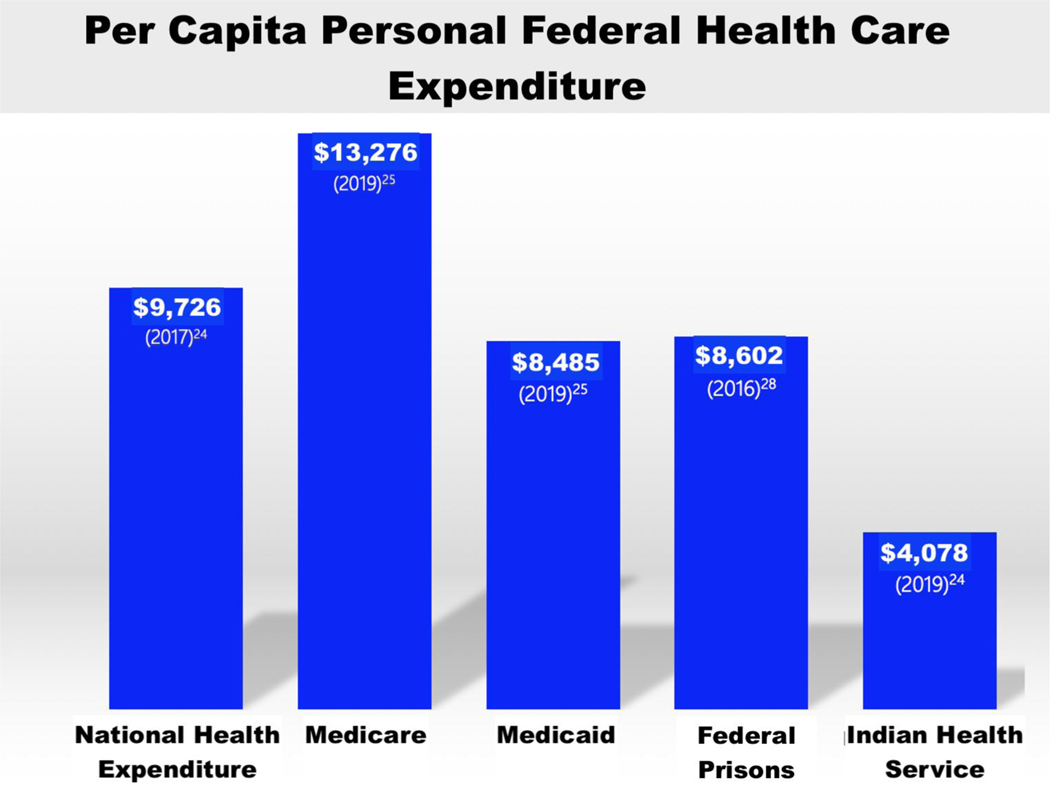
Further contributing to the burden of metabolic syndrome and cardiovascular disease in American Indian and Alaska Native groups is the issue of unfulfilled treaties and an underfunded health system [19, 23]. Through numerous laws and treaties, the Indian Health Service was developed to be the primary system for providing federal health services to American Indian and Alaska Native people [23]. Notwithstanding, the Indian Health Service has been severely and chronically underfunded. For those who receive care through the Indian Health Service, the per capita funding would have to triple to be equivalent to what is provided to individuals receiving Medicare and more than double to match funding provided in the federal prison system [24–26] (Figure 1). The amount of money allocated to each person in the Indian Health Service system is less than half of what is allocated to the general population overall ($4,078 vs $9,726). Long-term underfunding of the principal health system for American Indian and Alaska Native people contributes to cardiovascular disparities, such as metabolic syndrome [23]. To rectify the injustice of providing the least amount of support to populations who experience some of the nation’s worst inequities and honor signed government-to-government treaties, the United States government should uphold established trust and treaty obligations [23].
Figure 1.
Annual federal healthcare spending.
Although prolonged discrimination, colonization, and historical and intergenerational trauma are interconnected with risk factors associated with metabolic syndrome, it is essential to highlight the cultural strength and resilience of American Indian and Alaska Native people as another social determinant of health [5, 18]. Traditional beliefs and practices show promising results in being protective buffers against various health problems [18]. Additional research on the impact of traditional and cultural practices on health outcomes of American Indian and Alaska Native people is needed.
MANAGEMENT OF METABOLIC SYNDROME
To reduce disparities associated with metabolic syndrome, structural changes are indicated at a root level (i.e., poverty, housing, gaps in education and employment as well as access to healthy foods) [27–29]. Improved funding of the Indian Health Service and other culturally appropriate programs will be crucial in taking steps toward a more equitable future. Additionally, there needs to be stronger action in community outreach and engagement efforts to care for individuals who do not have access to facility-based services [27].
Food Security and Traditional Foods:
In the Dietary Intake among American Indians study, economics were related to low adherence to national dietary recommendations for key nutrients and food [30]. Researchers found that 97.5% of participants reported good availability of fruits and vegetables in the grocery stores in study communities, though a significant proportion (30.3%) of participants cited a reason they do not consume at least five servings of fruits or vegetables each day is because it is too costly to do so [30].
In this regard, health promotion strategies must be individualized, culturally responsive, and innovative. It is well documented that American Indian and Alaska Native people do not have sufficient access to healthier, more nutritious food options [31]. Thus, it is important to identify processes to change environmental aspects of food accessibility. In one environmental study, convenient stores and trading posts located on one reservation filled shelves with healthier food options and increased educational campaigns around the store resulting in a reduction of BMI for participants [31]. In addition to healthier food access, there are recommendations to shift meals to healthier American Indian traditional foods [30]. Traditional American Indian foods include corn, beans, squash, wild rice, berries, and lean game meats. Common barriers to programming retention is transportation and childcare. When transportation and childcare options are more readily available, participation retention in culturally tailored health promotion programs remain over 60% at 18-months [32]. Future physical activity and nutrition interventions and programs should aim to address individual barriers.
Health Promotion Activities:
More attention must be given to modification of lifestyles in indigenous communities [7]. Preventative efforts to reduce obesity and increase activity must be prioritized and supported. Not every factor contributing to the rising inequity of metabolic syndrome is instantly modifiable, but changes in health behaviors may have a substantial impact on the prevalence and incidence of metabolic syndrome in American Indian and Alaska Native communities [7, 27, 30, 33].
In pursuing health promotion activities, a little may go a long way. The American Heart Association’s Strategic Planning Task Force & Statistical Committee implemented 2020 Impact Goals for cardiovascular health promotion called Life’s Simple 7, based on modifiable risk factors [34]. These goals are made up of four health behaviors and three health factors: a physically active lifestyle; healthy diet; healthy BMI; avoiding smoking; and lower blood pressure, fasting glucose, and total cholesterol [34]. In a study examining the associations of Life’s Simple 7 goals with the incidence of diabetes among American Indian adults, researchers evaluated 1639 American Indian participants and found that participants who achieved at least two of the Life’s Simple 7 goals had a lower risk of diabetes than participants who met one or none of these criteria [34]. Further, physical activity and nutrition behavior interventions are most successful when they incorporate American Indian and Alaska Native cultural beliefs and practices [32, 35–38]. In a study of culturally tailored physical activity classes, American Indian and Alaska Native participants who attended more classes had greater weight loss and lower incidence of diabetes [37, 38].
Management and Treatment:
Health beliefs, values, and practices are highly influenced with the community and family system [39]. Therefore, the management of metabolic syndrome can be improved with family and community focused approaches, while also addressing individual and environmental barriers. In many American Indian and Alaska Native communities, the role of family and community play a vital role and are considered significant social units [39].
Efforts should also be focused on addressing clinical inertia, potentially biased decision-making, and adherence. An older study demonstrated that 34% of American Indian populations were not treated for hypertension despite a confirmed diagnosis, and women represented most of the untreated population [40]. Another study revealed that approximately 60% of patients eligible for treatment with a statin were not prescribed therapy [41]. Among those treated, approximately 60% were adherent to the prescription therapy [41]. Given known race-based disparities in clinical decision-making [42, 43], management must include consistent treatment according to national diabetes, hypertension, and hypercholesterolemia/prevention guidelines [44–46].
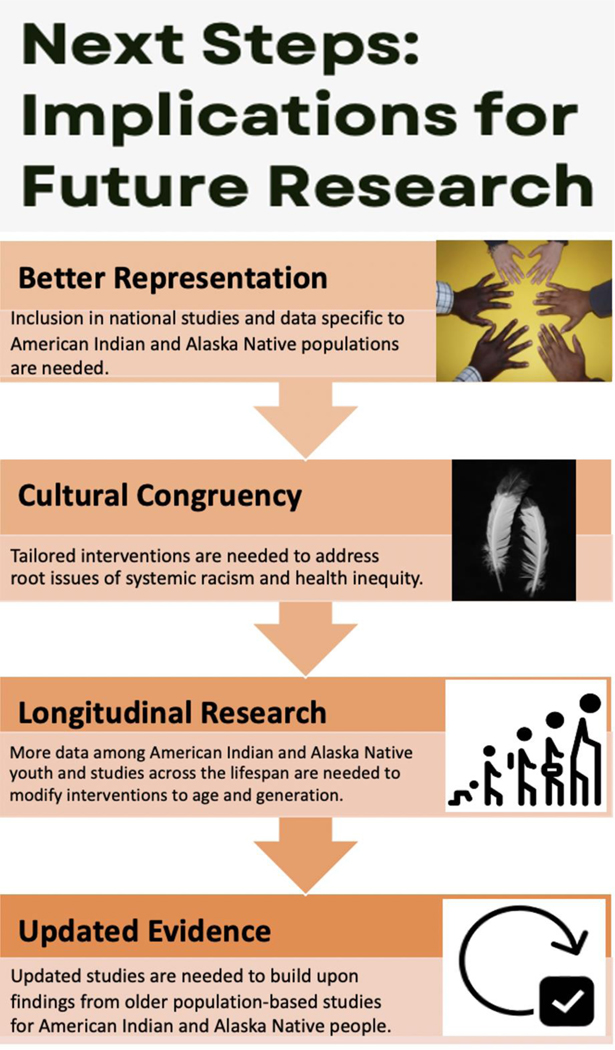
FUTURE INVESTIGATION
Identification and management of metabolic syndrome can be improved among American Indian and Alaska Native groups. Investigations should prioritize inclusivity and innovative techniques that prioritize cultural responsiveness (Figure 2).
Figure 2.
Implications for future research
American Indian and Alaska Native people are often excluded from national studies. Oversampling and disaggregation is needed to understand unique factors impacting these populations. This may require using innovative sampling techniques beyond telephone, given inadequate access on some tribal lands.
Interventions should be culturally tailored and address root issues such as the social determinants of health and structural racism. Studies should address clinical inertia including methods to provide equitable management that is unbiased and addresses barriers to adherence.
Life-course trajectory studies are needed to obtain more detailed information among all age populations. There is a lack of data among American Indian and Alaska Native youth. Interventions to address metabolic syndrome should vary based upon the age and generation of an individual as these factors can affect traditionality and knowledge and beliefs.
Most of the population studies inclusive of American Indian and Alaska Native groups are older. Updates are needed and additional funding to extend population studies focused on these groups would prove to be beneficial.
CONCLUSION
Despite study findings summarized in this review, updated literature is scarce on metabolic syndrome in American Indian and Alaska Native populations. There is a need for increased representative data on national surveys of health behaviors and risk factors for metabolic syndrome specific to American Indian and Alaska Native populations. Without accurate data collection and reporting methods, full comprehension of the magnitude of metabolic syndrome, diabetes, and heart disease cannot be fully understood.
The scientific community should strengthen evidence supporting the prevalence and management of metabolic syndrome in American Indian and Alaska Native communities, and focus on systemic and structural changes that address the root causes of disparities. Efforts should combat structural discrimination contributing to poverty rates, gaps in education, food insecurity, and inadequate funding of the Indian Health Service. Action to overcome these issues must be done in a coordinated, systematic, culturally intelligent approach. Community-based methods in research are needed to uphold cultural rigor in scientific endeavors. Determining the incidence, prevalence, and impact of metabolic syndrome in these communities will lead to culturally relevant interventions, programs, and policies. From this review, it is evident that culturally informed studies specific for American Indian and Alaska Native populations are urgently needed to reduce the disparities of metabolic syndrome and associated risk factors.
Acknowledgments
Funding: Dr. Breathett has research funding from National Heart, Lung, and Blood Institute (NHLBI) R56HL159216, K01HL142848, L30HL148881.
Footnotes
Declarations
Availability of data and material: Not applicable
Code availability: Not applicable
Compliance with Ethics Guidelines
Conflict of Interest
Timian M. Godfrey, Felina M. Cordova-Marks, Desiree Jones, Forest Melton, and Khadijah Breathett declare that they have no conflict of interest
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
REFERENCES
- [1].Resnick HE, Jones K, Ruotolo G, Jain AK, Henderson J, Lu W, & Howard BV. Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease in nondiabetic American Indians: The Strong Heart Study. Diabetes Care. 2003. doi: 10.2337/diacare.26.3.861. [DOI] [PubMed] [Google Scholar]
- [2].Schumacher C, Ferucci ED, Lanier AP, Slattery ML, Schraer CD, Raymer TW, Dillard D, Murtaugh MA, Tom-Orme L. Metabolic syndrome: Prevalence among American Indian and Alaska Native people living in the southwestern United States and in Alaska. Metab Syndr Relat Disord. 2008. doi: 10.1089/met.2008.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Russell M, de Simone G, Resnick HE, Howard BV. The metabolic syndrome in American Indians: The strong heart study. J Cardiometab Syndr. 2007. doi: 10.1111/j.1559-4564.2007.07457.x. PMID: 18059212. [DOI] [PubMed] [Google Scholar]
- [4]. Cobb N, Espey D, King J. Health Behaviors and Risk Factors Among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014. doi: 10.2105/AJPH.2014.301879. * Data related to factors of health from a ten-year period was examined among Non-Hispanic American Indian and Alaska Native participants. This data came from the Behavioral Risk Factor Surveillance System and found that participants had high prevalence of poor health indicators such as high cholesterol, blood pressure and diabetes and risky health behaviors that can lead to these health outcomes.
- [5].Breathett K, Sims M, Gross M, Jackson EA, Jones EJ, Navas-Acien A, Taylor H, Thomas KL, Howard BV, Univ Arizona. Cardiovascular Health in American Indians and Alaska Natives: A Scientific Statement From the American Heart Association. Circulation. 2020. 10.1161/CIR.0000000000000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Chinali M, de Simone G, Roman MJ, Best LG, Lee ET, Russell M, Howard BV, Devereux RB. Cardiac markers of pre-clinical disease in adolescents with the metabolic syndrome: The strong heart study. J Am Coll Cardiol. 2008. doi: 10.1016/j.jacc.2008.04.013. **The Strong Heart Study reported on their adolescent participants (14–20 years of age) in this study that recruited American Indians. Adolescent metabolic syndrome was found in approximately one quarter (n=111) of the participants, with more females (55.9%) than males meeting these criteria.
- [7]. Alberti KGM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WPT, Loria CM, Smith SC. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International atherosclerosis society; And international association for the study of obesity. Circulation. 2009. 10.1161/CIRCULATIONAHA.109.192644. *Risk factors for what constitutes metabolic syndrome varies by organization. Six organizations (1. American Heart Association, 2. International Association for the Study of Obesity, 3. International Atherosclerosis Society, 4. International Diabetes Federation Task Force on Epidemiology and Prevention, 5. National Heart, Lung and Blood Institute, 6. World Heart Federation) previously released their own criteria for metabolic syndrome. A consensus was developed where no specific components were required for diagnosis, rather the presence of three of the five risk factors was representative of metabolic syndrome.
- [8].Han TS, Lean MEJ. Metabolic syndrome. Medicine. 2015. doi: 10.1016/j.mpmed.2014.11.006. [DOI] [Google Scholar]
- [9].Heart Disease and American Indians/Alaska Natives. US Department of Health and Human Services Office of Minority Health. 2021. https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=34. Accessed 30 Sept 2021. [Google Scholar]
- [10].Obesity and American Indians/Alaska Natives. US Department of Health and Human Services Office of Minority Health. 2021. https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=40. Accessed 30 Sept 2021. [Google Scholar]
- [11].Diabetes and American Indians/Alaska Natives. US Department of Health and Human Services Office of Minority Health. 2021. https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=33. Accessed 30 Sept 2021. [Google Scholar]
- [12].Hirode G, Wong RJ. Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. JAMA. 2020. 10.1001/jama.2020.4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Moore JX, Chaudhary N, Akinyemiju T. Metabolic Syndrome Prevalence by Race/Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev Chronic Dis. 2017. 10.5888/pcd14.160287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Sinclair KA, Bogart A, Buchwald D, Henderson JA. The prevalence of metabolic syndrome and associated risk factors in Northern Plains and Southwest American Indians. Diabetes Care. 2011. doi: 10.2337/dc10-0221. *Results from the Education and Research Toward Health (EARTH) study found that approximately half of the American Indian participants had metabolic syndrome. The prevalence increased to 53.1% when looking at older participants and to 86.6% when looking at those with diabetes.
- [15]. Lee ET, Welty TK, Fabsitz R, Cowan LD, Le NA, Oopik AJ, Cucchiara AJ, et al. The Strong Heart Study. Am J Epidemiol. 1990. doi: 10.1093/oxfordjournals.aje.a115757. **The Strong Heart Study (SHS) examined twelve American Indian tribes to determine prevalence and incidence of various cardiovascular risk factors. This publication describes the survey and clinical methods utilized in this study to determine morbidity and mortality as well as their trainings and tribal approvals.
- [16].Slattery ML, Schumacher MC, Lanier AP, Edwards S, Edwards R, Murtaugh MA, Sandidge J, et al. A Prospective Cohort of American Indian and Alaska Native People: Study Design, Methods, and Implementation. Am J Epidemiol. 2007. doi: 10.1093/aje/kwm109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Boyer BB, Mohatt GV, Plaetke R, Herron J, Stanhope KL, Stephensen C, and Havel PJ. Metabolic Syndrome in Yup’ik Eskimos: The Center for Alaska Native Health Research (CANHR) Study. Obesity. 2007. doi: 10.1038/oby.2007.302. *The Center for Alaska Native Health Research Study (CANHR) was conducted from 2003–2006, measuring metabolic syndrome. A total sample of 710 Alaska Native patients were analyzed, with the major finding of metabolic syndrome being less prevalent in this population compared to the general population. Gender also played a role, with more than double the percentage of Alaska Native females having this condition than men.
- [18]. Warne D, Lajimodiere D. American Indian health disparities: psychosocial influences. Soc Personal Psychol Compass. 2015. 10.1111/spc3.12198. *American Indian populations have experienced negative health outcomes since the start of colonialism. In current times, American Indian populations face chronic diseases and other factors related to poor health, leading to a lowered life expectancy. Warne et al. created an intergenerational model considering history, environment and experiences that can lead to stressors and chronic diseases.
- [19].Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska native populations. PloS One. 2014. 10.1371/journal.pone.0080973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Spratlen MJ, Grau-Perez M, Best LG, Yracheta J, Lazo M, Vaidya D, Balakrishnan P, Gamble MV, Francesconi KA, Goessler W, Cole SA, Umans JG, Howard BV, Navas-Acien A. The Association of Arsenic Exposure and Arsenic Metabolism With the Metabolic Syndrome and Its Individual Components: Prospective Evidence From the Strong Heart Family Study. Am J Epidemiol. 2018. 10.1093/aje/kwy048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Deen JF, Adams AK, Fretts A, Jolly S, Navas-Acien A, Devereux RB, Buchwald D, Howard BV. Cardiovascular disease in American Indian and Alaska Native youth: Unique risk factors and areas of scholarly Need. Am J Heart. 2017. 10.1161/JAHA.117.007576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kaufman P, Dicken C, Williams R. Measuring access to healthful, affordable food in American Indian and Alaska Native tribal areas. Economic Research Service. US Department of Agriculture. 2014. https://www.ers.usda.gov/publications/pub-details/?pubid=43908. Accessed 2 Oct 2021. [Google Scholar]
- [23].Warne D, Frizzell LB. American Indian health policy: Historical trends and contemporary issues. Am J Public Health. 2014. doi: 10.2105/AJPH.2013.301682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Indian Health Services. IHS Profile. 2020. https://www.ihs.gov/newsroom/factsheets/ihsprofile/. Accessed 9 Oct 2021.
- [25].Centers for Medicare and Medicaid Services. National Health Expenditure Data. 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical. Accessed 9 Oct 2021.
- [26].Government Accountability Office. Bureau of Prisons. 2017. https://www.gao.gov/products/gao-17-379. Accessed 9 Oct 2021.
- [27]. Colip L, Burge MR, Sandy P, Ghahate D, Bobelu J, Faber T, Shah V. Exercise Intervention Improves the Metabolic Profile and Body Composition of Southwestern American Indian Adolescents. J Diabetes Obes. 2016. doi: 10.15436/2376-0494.16.1180. **Over the course of three years, a lifestyle intervention with 65 Zuni Pueblo youth (ages 12–17) participants was implemented. This intervention included various exercises, as well as education related to healthy diets. The participants showed an improvement in measured metabolic health indicators, BMI, glycemic control, fasting lipids, and uric acid.
- [28].Breathett K, Spatz ES, Kramer DB, Essien UR, Wadhera RK, Peterson PN, Ho PM, Nallamothu BK. The Groundwater of Racial and Ethnic Disparities Research: A Statement From Circulation: Cardiovascular Quality and Outcomes. Circ Cardiovasc Qual Outcomes. 2021. 10.1161/CIRCOUTCOMES.121.007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Love B, Hayes-Greene D. The Groundwater Approach: building a practical understanding of structural racism. The Racial Equity Institute. 2018. https://www.racialequityinstitute.com/groundwaterapproach. [Google Scholar]
- [30]. Ali R, Lee ET, Knehans AW, Zhang Y, Yeh J, Rhoades ER, Jobe JB, Ali T, Johnson MR. Dietary Intake among American Indians with Metabolic Syndrome - Comparison to Dietary Recommendations: the Balance Study. Int J Health Nutr. 2013; 4(1):33–45. *The Balance Study recruited participants (30–75 years of age, N=213) from seven tribes with metabolic syndrome to determine dietary intake as well as the effect of their controlled trial on participant diet. When compared to national recommendations, participants consumed less fiber, vitamins, and minerals and consumed more sodium and fats.
- [31].Gittelsohn J, Kim EM, He S, & Pardilla M. A food store-based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo Nation. Nutr J. 2013. 10.3945/jn.112.165266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Thompson JL, Allen P, Helitzer DL, Qualls C, Whyte AN, Wolfe VK, & Herman CJ. Reducing diabetes risk in American Indian women. Am J Prev Med. 2008. doi: 10.1016/j.amepre.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Current Hypertension Reports. 2018. 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Fretts AM, Howard BV, McKnight B, Duncan GE, Beresford SA, Mete M, Zhang Y, Siscovick DS. Life’s Simple 7 and incidence of diabetes among American Indians: the Strong Heart Family Study. Diabetes Care. 2014. doi: 10.2337/dc13-2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Venkat Narayan KM, Hoskin M, Kozak D, Kriska AM, Hanson RL, Pettitt DJ, Nagi DK, Bennett PH, & Knowler WC. Randomized clinical trial of lifestyle interventions in Pima Indians: a pilot study. Diabetic Medicine. 2004. doi: 10.1002/(SICI)1096-9136(199801)15:1<66::AID-DIA515>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- [36].Lee ET, Jobe JB, Yeh J, Ali T, Rhoades ER, Knehans AW, Willis DJ, Johnson MR, Zhang Y, Poolaw B, Rogers B. A cardiovascular risk reduction program for American Indians with metabolic syndrome: the Balance Study. J Prim Prev. 2012. doi: 10.1007/s10935-012-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Rosas LG, Vasquez JJ, Hedlin HK, Qin FF, Lv N, Xiao L, Kendrick A, Atencio D, Stafford RS. Comparing enhanced versus standard Diabetes Prevention Program among indigenous adults in an urban setting: a randomized controlled trial. BMC Public Health. 2020. doi: 10.1186/s12889-020-8250-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Jiang L, Manson SM, Beals J, Henderson WG, Huang H, Acton KJ, Roubideaux Y, & the Special Diabetes Program for Indian Diabetes Prevention Demonstration Project. Translating the diabetes prevention program into American Indian and Alaska Native Communities. Diabetes Care. 2013. doi: 10.2337/dc12-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Martin D, Yurkovich E. “Close-Knit” Defines a Healthy Native American Indian Family. J Fam Nurs. 2014. 10.1177/1074840713508604. [DOI] [PubMed] [Google Scholar]
- [40].Hayslett JA, Eichner JE, Yeh JL, Wang W, Henderson J, Devereux RB, Welty TK, Fabsitz RR, Howard BV, Lee ET. (2001). Hypertension treatment patterns in American Indians: the Strong Heart Study. Am J Hypertens. 2001. 10.1016/S0895-7061(01)02146-X. [DOI] [PubMed] [Google Scholar]
- [41].Cooke CE, Bresette JL, Khanna R. Statin use in American Indians and Alaska Natives with coronary artery disease. Am J Health Syst Pharm. 2006. doi: 10.2146/ajhp050517. [DOI] [PubMed] [Google Scholar]
- [42].Breathett K, Jones J, Lum HD, Koonkongsatian D, Jones CD, Sanghvi U, Hoffecker L, McEwen M, Daugherty SL, Blair IV, Calhoun E, de Groot E, Sweitzer NK, Peterson PN. Factors Related to Physician Clinical Decision-Making for African-American and Hispanic Patients: a Qualitative Meta-Synthesis. J Racial Ethn Health Disparities. 2018. doi: 10.1007/s40615-018-0468-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Care Health. Smedley BD, Stith AY, Nelson AR, editors. Washington (DC): National Academies Press (US); 2003. PMID: 25032386. [PubMed] [Google Scholar]
- [44].American Diabetes Association. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021. doi: 10.2337/dc21-S001. [DOI] [Google Scholar]
- [45].Whelton Carey, M. R, Aronow WS, Casey Donald E Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith Sidney C Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams Kim A Sr, … Wright Jackson T Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018. 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- [46].Grundy Stone, J. N, A. L. Bailey, C. Beam, K. K. Birtcher, R. S. Blumenthal, L. T. Braun, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, P. A. Heidenreich, Hlatky MA, Jones W, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, … Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019. 10.1016/j.jacc.2018.11.003. [DOI] [Google Scholar]