Abstract
Rationale
The blood is a rich source of potential biomarkers for the diagnosis of idiopathic and hereditary pulmonary arterial hypertension (iPAH and hPAH, referred to as “PAH”). While a lot of biomarkers have been identified for PAH, the clinical utility of these biomarkers often remains unclear. Here, we performed an unbiased meta-analysis of published biomarkers to identify biomarkers with the highest performance for detection of PAH.
Methods
A literature search (in PubMed, Embase.com, Clarivate Analytics/Web of Science Core Collection and Wiley/Cochrane Library) was performed up to 28 January 2021. Primary end points were blood biomarker levels in PAH versus asymptomatic controls or patients suspected of pulmonary hypertension (PH) with proven normal haemodynamic profiles.
Results
149 articles were identified by the literature search. Meta-analysis of 26 biomarkers yielded 17 biomarkers that were differentially expressed in PAH and non-PH control subjects. Red cell distribution width, low density lipid-cholesterol, d-dimer, N-terminal prohormone of brain natriuretic protein (NT-proBNP), interleukin-6 (IL-6) and uric acid were biomarkers with the largest observed differences, largest sample sizes and a low risk of publication bias. Receiver operating characteristic curves and sensitivity/specificity analyses demonstrated that NT-proBNP had a high sensitivity, but low specificity for PAH. For the other biomarkers, insufficient data on diagnostic accuracy with receiver operating characteristic curves were available for meta-analysis.
Conclusion
This meta-analysis validates NT-proBNP as a biomarker with high sensitivity for PAH, albeit with low specificity. The majority of biomarkers evaluated in this meta-analysis lacked either external validation or data on diagnostic accuracy. Further validation studies are required as well as studies that test combinations of biomarkers to improve specificity.
Short abstract
Meta-analysis of 26 biomarkers yielded 17 differentially expressed biomarkers in PAH. NT-proBNP had the highest diagnostic accuracy but had a low specificity for PAH. Other markers, including IL-6, RDW, LDL-c, D-dimer and UA, lacked clinical validation. https://bit.ly/3J4YAyC
Introduction
Pulmonary arterial hypertension (PAH) is a cardiovascular condition in which progressive occlusive remodelling leads to increased pulmonary vascular resistance and ultimately right ventricular failure. PAH can be hereditary (hPAH) or idiopathic (iPAH) after exclusion of significant comorbidity [1], referred to as “PAH” throughout this study. The diagnosis of PAH is a complex, specialist process, attributing to a mean time to diagnosis of 17–24 months [2]. Availability of noninvasive biomarkers for faster diagnosis and initiation of treatment prior to the development of right heart failure may improve survival and quality of life [3].
Until now, N-terminal prohormone of brain natriuretic protein (NT-proBNP) remains the most useful clinical marker of myocardial strain and is employed for risk stratification of patients in guidelines and clinical practice [1]. However, improved understanding of the pathways leading to PAH, which include endothelial dysfunction, immunity and altered cellular metabolism, may result in the emergence of novel biomarkers that can detect proliferation and occlusive remodelling of the vascular wall with higher specificity. With the ongoing interest to develop biomarkers that help noninvasive diagnosis of PAH, new biomarkers have been proposed. Yet, many of these biomarkers lack external validation, leaving the performance of these biomarkers – in terms of reproducibility and clinical utility – unclear. We used unbiased meta-analysis to identify biomarkers with robust sensitivity and specificity to detect PAH.
We conducted a systematic review and meta-analysis of the literature on published biomarkers of PAH in blood or urine. Here we show: 1) biomarkers differentially expressed in iPAH and hPAH compared to non-pulmonary hypertension (PH) controls; and 2) available evidence supporting the suitability of these biomarkers for clinical implementation, including calculation of diagnostic accuracy employing receiver operating curve analyses.
Materials and methods
Search strategy
The conduct and reporting of this review adhere to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)-statement (www.prismastatement.org) [4] and is registered in PROSPERO (CRD42020215820).
Four bibliographic databases (PubMed, Embase.com, Clarivate Analytics/Web of Science Core Collection and Wiley/Cochrane Library) were searched for relevant literature from inception to 28 January 2021. Searches were constructed in collaboration with a medical information specialist (K.A.Z.). Search terms including synonyms, closely related words and keywords were used as index terms or free-text words. The searches contained no methodological search filter, date or language restrictions that would limit results to specific study designs, date or language (detailed search; supplementary table S1). Duplicate articles were excluded using Endnote (X9.3.3), Amsterdam Efficient Deduplication-method and Bramer-method [5]).
Two reviewers (A.J.S. and L.B.) independently screened all potentially relevant titles and abstracts for eligibility using Rayyan. If necessary, the full text article was checked for the eligibility criteria. Differences in judgement were resolved through: 1) discussion among reviewers (A.J.S. and L.B.); 2) arbitration of a third reviewer (J.A.); or 3) contacting the author. Studies were included if they met the following criteria: 1) analysis of potential blood and urine biomarkers in any form, including growth factors, inflammatory mediators, circulating cells, protein, (micro)RNA, or microvesicles; and 2) involved group 1 PAH, provided that iPAH or hPAH patients were included. The following studies were excluded: 1) animal studies; 2) studies involving subjects <18 years of age; 3) studies that did not report biomarker levels for group 1 PAH, or lacked inclusion of iPAH or hPAH patients; 3) studies that lacked a control group, or included a control group suspected of PH without measurement of haemodynamics; and 4) certain publication types: editorials, letters, legal cases, interviews, etc. The full text of the selected articles was obtained for further review and data extraction. In a minority of articles data were estimated from figures. Biomarker levels were conversed to a uniform unit of measurement. Two reviewers (A.J.S. and L.B.) independently evaluated the methodological quality of the full text papers using QUADAS-2 [6]. Articles were scored as low, unclear or high on domains “patients inclusion (P)”, “index test (I)”, “reference test (R)” and “flow and timing (T)” [6]. The risk of bias assessment tool was optimised by A.J.S. and L.B. from a pilot of 10 studies and are presented in supplementary table S2.
A similar search strategy was adopted in identical databases to identify “omics” studies performed in patients with iPAH and hPAH, compared to non-PH control subjects. Studies were included if they met the following criteria: 1) adopted an “omics” technology, including transcriptomics, proteomics, metabolomics, glycomics or lipidomics in blood or urine; and 2) involved patients with group 1 PAH, including iPAH or hPAH. Equal exclusion criteria applied as described above.
Data extraction
The following data were extracted from each publication: mean with standard deviation (sd) and the number of patients for each group (PAH versus non-PAH controls), area under the receiving-operating-curve (AUC/ROC), cut-off values, as well as sensitivity and specificity of a given biomarker for the diagnosis of PAH.
Statistics
Primary outcomes were biomarker concentrations in PAH and asymptomatic controls. Meta-analyses were performed when original data (expressed as mean±sd) were available from a minimum of three publications using Review Manager 5.3.5 software (The Nordic Cochrane Center, Copenhagen, Denmark). A randomised model for continuous data was adopted, due to possible risk of bias. Based on population size, mean and standard deviation, the standardised mean difference, mean difference and odds ratio of biomarker levels in patients with PAH and non-PH controls were calculated. Mean and standardised mean differences are represented as mean with 95% confidence intervals (95% CI), or odds ratio with 95% CI. Biomarkers were ranked according to effect size and statistical significance. I2 and Tau2 statistics were performed to assess heterogeneity among studies, and explainable heterogeneity was solved by exclusion of the aberrant publication.
Publication bias was assessed in Comprehensive Meta-Analysis software V3 (Biostat, Englewood, NJ, USA) using funnel plots, Egger's regression test (p<0.10), Duval and Tweedie's trim and fill, and Orwin's Fail-safe number-test. The Fail-safe number estimates the number of unpublished studies required to turn the meta-analysis result into a clinically insignificant value. The clinically insignificant value was arbitrarily set at a standardised mean difference of <−0.25 or 0.25.
Selection of biomarkers for clinical implementation
We made a selection of differentially expressed biomarkers based on statistical significance (p<0.05) of the observed difference, sample size and quality of validation outside the discovery cohort by means of calculation of sensitivity and specificity values using ROC analyses in an independent validation cohort. Additionally, we selected for a negligible risk for publication bias, defined by Egger's regression p>0.10, Duval and Tweedie's trim and fill (p<0.05), and a minimum of five publications predicted to bring the result to a clinically insignificant value (standardised mean difference – 0.25, 0.25).
All biomarkers were grouped in six pathobiological domains: haematological, metabolic, coagulation, inflammatory, cardiac and renal. In each domain, we selected one preferred biomarker on the basis of observed difference, sample size, quality of external validation and risk of publication bias (see supplementary table S1).
Results
Inclusion and selection of publications
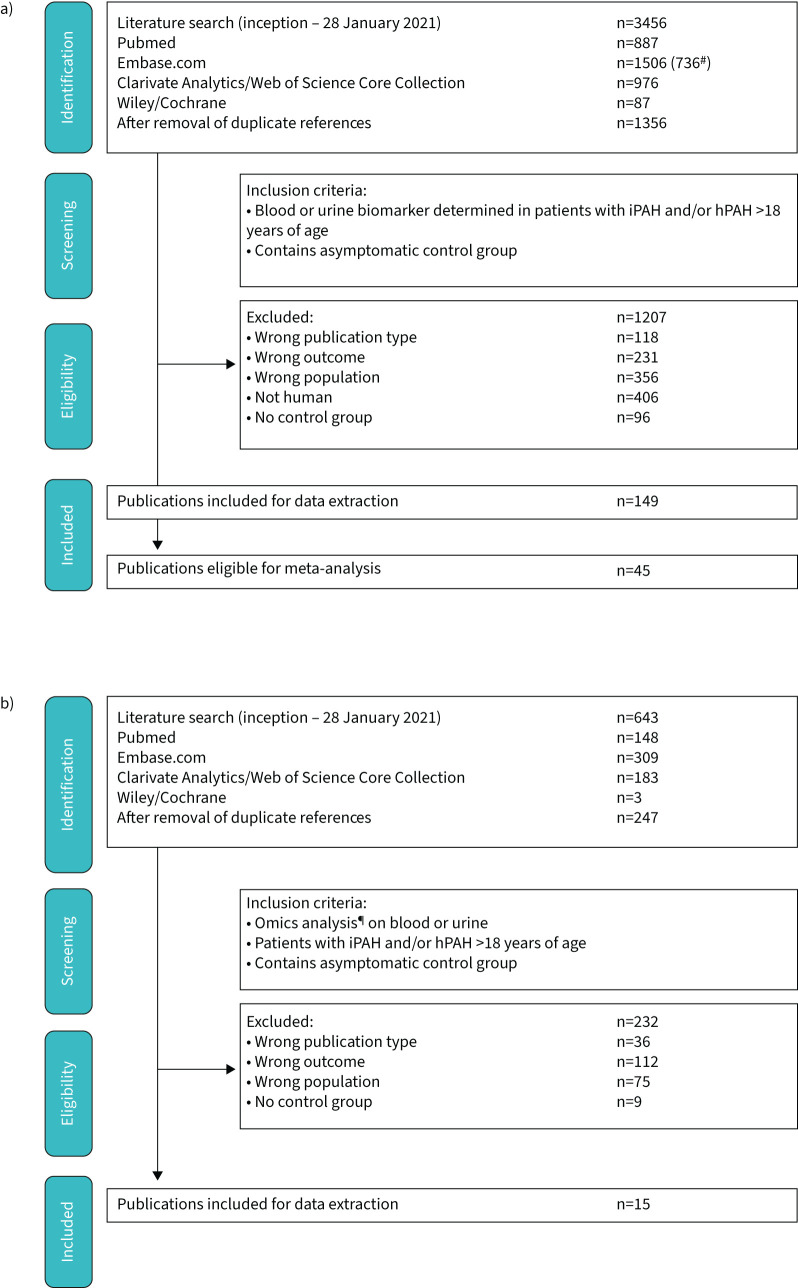
The literature search yielded a total of 3456 references: 887 in PubMed, 1506 in Embase.com, 976 in Clarivate Analytics/Web of Science Core Collection and 87 in Wiley/Cochrane Library. After removal of duplicates 1356 remained. 1207 full text articles were excluded based on inclusion and exclusion criteria (figure 1a). 149 publications remained eligible for data extraction. 45 publications were identified that describe biomarkers meeting criteria for meta-analysis and risk of publication bias assessment. A detailed overview of biomarker origin (whole blood, plasma or serum), location of blood draw (peripheral or central (RHC) blood draw), demographic criteria, treatment and concerns regarding inclusion procedure of these publications is provided in supplementary table S3. Risk of bias, attributable to the procedure of patient selection, index and reference test, as well as timing of the biomarker blood draw (see supplementary table S2), was systematically assessed using QUADAS-2 [6] and is reported in supplementary figure S1.
FIGURE 1.
Flow chart visualising identification of publications, inclusion and exclusion criteria, and selection of publications eligible for meta-analysis. a) Biomarker search; b) omics search. #: excluding conference abstracts; ¶: transcriptomics, proteomics, metabolomics, glycomics and lipidomics. iPAH: idiopathic pulmonary arterial hypertension; hPAH: hereditary pulmonary arterial hypertension.
Exclusion of urine and non-protein blood biomarkers
In several publications, biomarker expression was studied on circulating platelets [7, 8], immune cells [9–12] and progenitor cells [13–16]. Heterogeneity in measurement methods, characterisation and flow cytometry (FACS) gating precluded meta-analysis of these publications.
Three publications reported on different types of extracellular vesicles as biomarker [17, 18] and three on different types of miRNA as biomarker [19–22]. A single publication reported on a urine biomarker [23]. These publications did not meet the criteria for meta-analysis.
Selection of eligible biomarkers
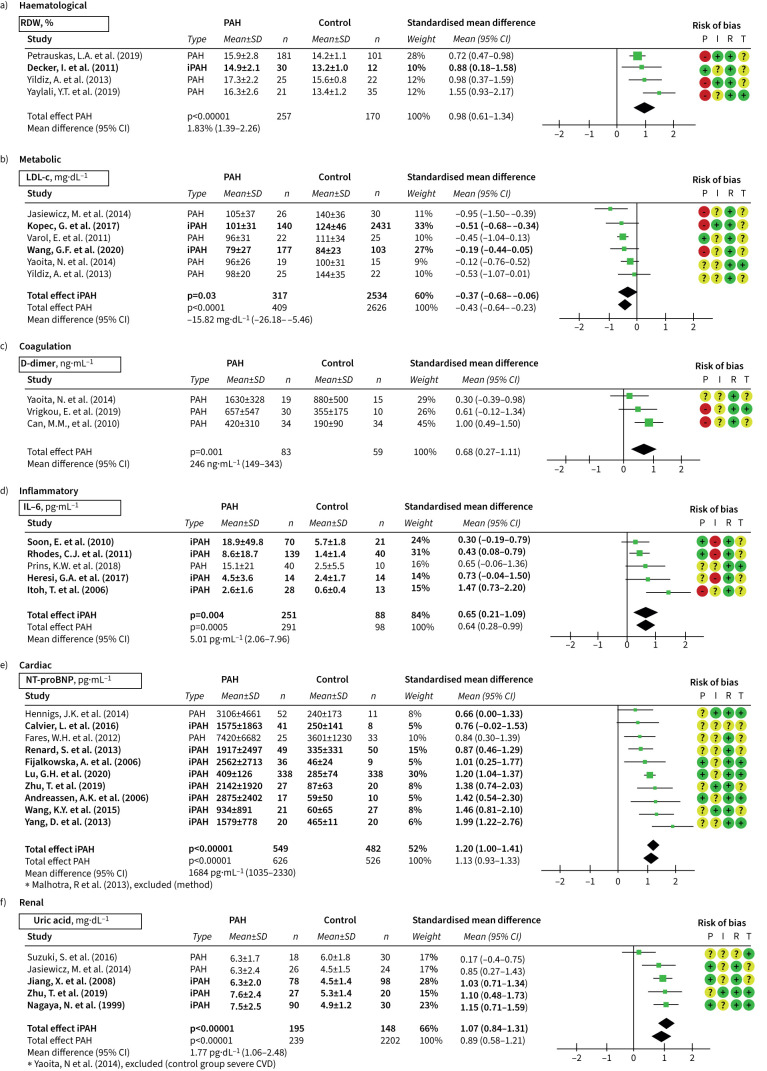
26 biomarkers were eligible for meta-analysis (table 1). A significant difference in expression was detected for 17 biomarkers in six pathobiological domains. In the haematological domain, these were red blood cell distribution width (RDW), platelet distribution width (PDW), mean platelet volume (MPV) and thrombocytes; in the metabolic domain, total cholesterol, low density lipid-cholesterol (LDL-c), triglycerides and fasting glucose. In the coagulation domain, d-dimer was differentially expressed. In the inflammatory domain, interleukin-6 (IL-6), C-reactive protein (CRP), soluble vascular adhesion molecule-1 (sVCAM-1), C-X-C motif chemokine ligand-10 (CXCL-10) and tissue inhibitor metalloproteinase-1 (TIMP1) were differentially expressed. In the cardiac domain, NT-proBNP, and in the renal domain, uric acid (UA) and blood urea nitrogen (BUN) were differentially expressed. Biomarkers described in fewer than three publications or as median with IQR are summarised in supplementary tables S4 and S5. Selected biomarkers are shown in figure 2 (see Materials and methods). These include RDW, LDL-c, d-dimer, IL-6, NT-proBNP and UA. Forest plots for PDW, MPV, thrombocytes, total cholesterol, triglycerides, fasting glucose, CRP, sVCAM-1, CXCL-10, TIMP1 and BUN are provided in the supplementary material (supplementary figures S2–7, supplementary table S6).
TABLE 1.
Summary of 26 meta-analyses
| Marker | Studies n | Participants n | Mean difference | St. mean difference | Overall effect (p-value) | Tau2 | I2 (%) | Heterogeneity (p-value) | Forest plot |
| Haematological markers | |||||||||
| RDW % | 4 | 427 | 1.83 (1.39–2.26) | 0.98 (0.61–2.17) | <0.00001 | 0.07 | 51 | 0.11 | Figure 2a |
| PDW % | 3 | 245 | 1.42 (0.16–2.67) | 0.81 (0.50–1.12) | <0.00001 | 0.02 | 19 | 0.29 | Figure S2a |
| MPV fL | 5 | 361 | 0.95 (0.76–1.13) | 1.0 (0.81–1.25) | <0.00001 | 0.00 | 0 | 0.68 | Figure S2b |
| 6# | 395 | 0.66 (0.24–1.09) | 0.72 (0.24–1.19) | 0.003 | 0.27 | 78 | 0.0003 | ||
| Thrombocytes (×109 L−1) | 7 | 334 | −23.9 (−38.6– −9.2) | −0.38 (−0.62– −0.15) | 0.001 | 0.01 | 5 | 0.39 | Figure S2c |
| Hb g dL−1 | 9 | 400 | −0.59 (−1.23–0.06) | −0.18 (−0.43–0.07) | 0.15 | 0.04 | 29 | 0.19 | Figure S2d |
| Hct % | 5 | 229 | −1.07 (−3.91–1.76) | −0.21 (−0.76–0.34) | 0.46 | 0.29 | 74 | 0.004 | Figure S2e |
| Leukocytes (×109 L−1) | 7 | 294 | −0.23 (−0.70,0.24) | −0.10 (−0.41–0.21) | 0.52 | 0.07 | 39 | 0.13 | Figure S2f |
| Metabolic markers | |||||||||
| LDL-c mg dL−1 | 6 | 3035 | −15.82 (−26.18– −5.46) | −0.44 (−0.65– −0.22) | <0.00001 | 0.03 | 46 | 0.10 | Figure 2b |
| Total cholesterol mg dL−1 | 4 | 408 | −17.70 (−24.15– −11.26) | −0.52 (−0.73– −0.32) | <0.00001 | 0.00 | 67 | 0.67 | Figure S3a |
| TG mg dL−1 | 4 | 198 | −32.56 (−54.17– −10.94) | −0.52 (−0.87– −0.17) | 0.004 | 0.04 | 34 | 0.21 | Figure S3b |
| Glucose (fasted) mg dL−1 | 3 | 103 | 24.06 (0.54–7.58) | 0.48 (0.08–0.87) | 0.02 | 0.00 | 0 | 0.85 | Figure S3c |
| HDL-c mg dL−1 | 6 | 577 | −6.15 (−2.11–14.40) | −0.53 (−1.20–0.15) | 0.13 | 0.63 | 91 | <0.00001 | Figure S3d |
| Coagulation markers | |||||||||
| D-dimer ng mL−1 | 3 | 142 | 245.99 (148.55–343.43) | 0.69 (0.27–1.11) | 0.001 | 0.04 | 27 | 0.26 | Figure 2c |
| Fibrinogen mg dL−1 | 4 | 227 | 73.75 (−2.58–150.08) | 0.84 (−0.14–1.81) | 0.09 | 0.88 | 90 | <0.00001 | Figure S4 |
| Inflammatory markers | |||||||||
| IL-6 pg mL−1 | 5 | 389 | 5.01 (2.06–7.96) | 0.64 (0.28–0.99) | 0.0005 | 0.08 | 47 | 0.11 | Figure 2d |
| CRP mg L−1 | 8 | 387 | 0.74 (0.13–1,6) | 0.25 (0.04–0.47) | 0.02 | 0.02 | 0 | 0.98 | Figure S5a |
| 9# | 493 | 0.13 (0.10–0.17) | 0.77 (−0.08–1.61) | 0.08 | 1.57 | 94 | <0.00001 | ||
| sVCAM-1 ng mL−1 | 3 | 150 | 626.72 (29.38–1224.07) | 1.03 (0.53–1.52) | <0.00001 | 0.08 | 40 | 0.19 | Figure S5b |
| CXCL-10 pg mL−1 | 3 | 171 | 99.77 (54.53–145.01) | 0.82 (0.49–1.16) | <0.00001 | 0.00 | 0 | 0.46 | Figure S5c |
| TIMP-1 ng mL−1 | 3 | 224 | 15.58 (−2.56–33.72) | 0.40 (0.13–0.67) | 0.003 | 0.00 | 0 | 0.54 | Figure S5d |
| 4# | 329 | 40.15 (1.02–79.29) | 0.67 (0.14–1.21) | 0.01 | 0.24 | 82 | 0.0009 | ||
| sP-selectin ng mL−1 | 4 | 180 | 0.52 (−11.10–12.14) | −0.04 (0.35–0.28) | 0.82 | 0.00 | 0 | 0.72 | Figure S5e |
| Cardiac markers | |||||||||
| NT-proBNP pg mL−1 | 10 | 1152 | 1684 (1035–2330) | 1.13 (0.93–1.33) | <0.00001 | 0.03 | 30 | 0.17 | Figure 2e |
| 11# | 1258 | 1004 (787–1221) | 1.37 (0.96–1.79) | <0.00001 | 0.39 | 85 | <0.00001 | ||
| Renal markers | |||||||||
| UA mg dL−1 | 5 | 441 | 1.77 (1.06–2.48) | 0.89 (0.58–1.12) | <0.00001 | 0.06 | 51 | 0.09 | Figure 2f |
| 6# | 531 | 1.52 (0.77–2.27) | 0.81 (0.53–1.09) | <0.00001 | 0.09 | 59 | 0.03 | ||
| BUN mg dL−1 | 5 | 891 | 1.76 (0.51–3.01) | 0.43 (0.29–0.56) | <0.00001 | 0.00 | 0 | 0.48 | Figure S6a |
| Creatinine mg dL−1 | 10 | 475 | 0.03 (−0.04–0.10) | 0.13 (−0.08–0.34) | 0.23 | 0.02 | 20 | 0.26 | Figure S6b |
| eGFR mL min−1/1.73 m2 | 4 | 180 | 1.70 (5.98–9.37) | 0.09 (−0.32–0.49) | 0.67 | 0.08 | 47 | 0.13 | Figure S6c |
| Hepatic markers | |||||||||
| ALT U L−1 | 3 | 115 | 3.57 (−4.18–11.31) | 0.18 (−0.56–0.92) | 0.37 | 0.30 | 71 | 0.03 | Figure S7 |
Per biomarker the number of studies included, total sample size, mean difference, and the standardised difference between iPAH and non-PH control with 95% confidence interval, p-value of the difference, and heterogeneity of the result (I2, Tau2 and p-heterogeneity) are shown. St. mean difference; standardised mean difference; RDW: red cell distribution width; PDW: platelet distribution width; MPV: mean platelet volume; Hb: haemoglobin; Hct: haematocrit; TG: triglycerides; LDL-c: low density lipoprotein; HDL-c: high density lipoprotein; IL-6: interleukin-6; CRP: c-reactive protein; sVCAM-1: circulating vascular cell adhesion molecule-1; CXCL-10: C-X-C motif chemokine ligand-10; TIMP-1: tissue inhibitors of metalloproteinases-1; NT-proBNP: N-terminal prohormone of brain natriuretic peptide; UA: uric acid; BUN: blood urea nitrogen; eGFR: estimated glomerular filtration rate: ALT: alanine transaminase. #: publication excluded due to heterogeneity.
FIGURE 2.
Forest plots of selected biomarkers. a) The haemtological biomarker RDW: red cell distribution width; b) the metabolic biomarker LDL-c: low density lipid-cholesterol; c) the coagulation biomarker d-dimer; d) the inflammatory biomarker IL-6: interleukin-6; e) the cardiac biomarker NT-proBNP: N-terminal prohormone of brain natriuretic peptide; f) the renal biomarker UA: uric acid; CVD: cardiovascular disease. Risk of bias (QUADAS-2) – P: patient inclusion; I: index test (biomarker); R: reference standard (diagnosis); T: flow and timing. Publications in bold type represent biomarker levels of idiopathic pulmonary arterial hypertension (iPAH) and/or hereditary pulmonary arterial hypertension (hPAH) uniquely.
Evaluation of publication bias
Egger's regression analysis revealed a significant association (p<0.10) between effect size and standard error for MPV and thrombocytes. After correction for possible publication bias by Duval and Tweedie's trim and fill, the mean difference between PAH and control groups remained significant. The fail-safe test indicated that a minimum of five publications were required to bring the differences to a clinically trivial value, defined as a standardised mean difference of <−0.25 or 0.25. This suggests that the chance that the observed difference relies on publication bias is small (supplementary table S7). Funnel plots of all meta-analyses are given in supplementary figure S8a–z.
Haematological markers: RDW
All five publications on RDW were eligible for meta-analysis. RDW was determined in treatment-naïve iPAH [24] and PAH [25] patients, and in PAH patients receiving vasodilatory treatment [11, 26]. As a reference, asymptomatic controls [11, 24–26] and patients suspected of PH [26] or common disease controls [24] were included (figure 2a). Meta-analysis confirmed a positive mean difference of 1.67% (95% CI 1.45–1.89, p<0.00001) between PAH and non-PH control (table 1). For RDW no sensitivity, specificity or diagnostic accuracy could be extracted from the original data.
A rise in RDW is predictive for the presence of PH in patients with acute pulmonary embolism [27] or systemic sclerosis [26, 28]. RDW was positively associated with pulmonary artery pressure [11, 24], right atrial pressure [24], pulmonary vascular resistance [24], BNP [26] and NT-proBNP [29], and inversely with 6- min walk distance (6MWD) [24, 26, 29]. Remarkably, in one study RDW performed better than NT-proBNP and IL-6 as prognostic markers in PAH patients [27].
Other markers in the haematological domain are summarised in table 1. PDW was increased with a mean difference of 1.42% (95% CI 0.16–2.67, p<0.00001, supplementary figure S2a), as well as MPV (0.95 fL (95% CI 0.76–1.13, p<0.00001; supplementary figure S2b), while thrombocyte count was decreased by a mean of −23.9×109 cells L−1 (95% CI −38.6– −9.2, p=0.001); supplementary figure S2c). Eligible for meta-analysis but without significant differences were haemoglobin, haematocrit and leukocytes (supplementary figure S2d–f).
Metabolic markers: LDL-c
LDL-c was reported in six publications eligible for meta-analysis and determined in patients with PAH receiving vasodilatory treatment. Asymptomatic controls [11, 30–32] or patients with cardiovascular disease or patients suspected of PH [8] were included as reference (figure 2b). All measurements were performed in blood obtained after >8 h of fasting. LDL-c was lower in patients with PAH, with a mean difference of −15.82 mg dL−1 (95% CI −26.18– −5.46, p<0.00001) (table 1). For LDL-c no sensitivity, specificity or diagnostic accuracy could be extracted from the original data. Decreased insulin sensitivity and altered lipid metabolism in iPAH are a possible consequence of chronic inflammation, malnourishment and alterations in liver function [33, 34]. LDL-c was not related to haemodynamic parameters, NT-proBNP, 6MWD or body mass index. LDL-c was negatively associated with 3-year survival in PAH (hazard ratio 0.18 mmol L−1 (95% CI 0.07–0.47), p<0.01, corrected for statin use) [30]. A similar relationship has been described in chronic heart failure [35, 36].
A lower LDL-c in patients with PAH was accompanied by a lower mean total cholesterol of −17.70 mg dL−1 (95% CI −24.15– −11.26, p<0.00001; supplementary figure S3a) and lower mean triglycerides of −32.56 mg dL−1 (95% CI −54.17– −10.94, p=0.004; supplementary figure S3b). Despite the availability of six publications, no significant difference was found in meta-analyses for high-density lipoprotein (HDL-c) (mean difference −6.15 mg dL−1, 95% CI −2.11–14.40, p=0.13; supplementary figure S3d) or fasting glucose (supplementary figure S3c).
Coagulation markers: D-dimer
From the available markers representing coagulation pathways, meta-analyses could be performed for fibrinogen and d-dimer levels. D-dimer was studied in treatment-naïve iPAH patients [37] and in PAH patients receiving vasodilatory treatment [8, 38], and results were compared to asymptomatic controls (figure 2c). Meta-analysis revealed a significantly higher d-dimer level in patients with PAH compared to asymptomatic controls, with a mean difference of 245.99 ng mL−1 (95% CI 148.55–343.43, p=0.001, table 1), in contrast to fibrinogen (73.75 ng mL−1, 95% CI −2.58–150.08, p=0.09); supplementary figure S4), all consistent with the hypothesis that hypercoagulability and in situ thrombosis may contribute to disease pathobiology in PAH [39].
Inflammatory markers: IL-6
From 10 publications reporting on IL-6, five were eligible for meta-analysis. All studies detected elevated levels of circulating IL-6 in treatment-naïve iPAH [40], or iPAH receiving vasodilatory treatment [27, 41–45] and naïve PAH [46, 47] or PAH patients receiving treatment [48]. Findings were compared to asymptomatic controls (figure 2d). A significant rise in IL-6 levels was observed in PAH compared to non-PH controls (mean difference 5.01 (95% CI 2.06–7.96) pg mL−1, p=0.0005) (table 1).
Il-6 levels were negatively associated with the number of circulating endothelial progenitor cells [41] and were elevated in parallel to several interleukins [44], as well as CXCL-10 [42], monocyte chemoattractive protein-1 (MCP-1) [47, 48], tumour necrosis factor-α (TNF-α) [40, 46–48], placental growth factor (PlGF) [40], soluble vascular endothelial growth factor (VEGF) receptor-1 (sVEGFR-1) [40], VEGF-A [40], VEGF-D [40] and markers related to thrombogenesis [45]. IL-6 was negatively associated with right ventricular function [47] and 6MWD [27, 40], while positively to World Health Organization (WHO) functional class [27], NT-proBNP [27, 40] and mean right atrial pressure [40]. IL-6 levels were predictive for all-cause mortality [27, 44] in PAH. No data on diagnostic accuracy, including ROC and AUC were available for meta-analysis.
Eight publications detected a subtle elevation in CRP levels in PAH [11, 41, 49–57] (supplementary figure S5a), (mean difference 0.74 mg L−1, 95% CI 0.13–1.6, p=0.02) (table 1). However, since only one study was predicted to bring the difference to a clinically insignificant value, the risk of bias is significant. The study of Wang et al. [50] yielded an AUC of 0.51 (p=0.899) with a 85% specificity but low (39%) sensitivity [50], when using a diagnostic cut-off of 2.7 mg L−1 CRP, indicating diagnostic accuracy is low in an external validation cohort consisting of iPAH and asymptomatic controls. CRP is commonly attributed to other cardiovascular or inflammatory disease [58], and these data indicate that an elevated CRP lacks the specificity required for detection of PAH among non-PH controls.
Other inflammatory markers that were eligible for meta-analysis and significantly increased in patients with iPAH compared to non-PH controls included: sVCAM-1 (mean difference of 626.72 ng mL−1, 95% CI 29.38–1224.07, p=0.003; supplementary figure S5b), CXCL-10 (mean difference 99.77 pg mL−1, 95% CI 54.53–145.01, p<0.00001; supplementary figure S5c) and TIMP-1 (mean difference of 15.58 ng mL−1, 95% CI −2.56–33.72, p=0.003; supplementary figure S5d). No significant difference was observed for sP-selectin (supplementary figure S5e). From these markers no sensitivity, specificity or diagnostic accuracy could be extracted from the original data.
Cardiac markers: NT-proBNP
11 publications reporting on NT-proBNP met the inclusion criteria, 10 of which were eligible for meta-analysis. NT-proBNP was measured in treatment-naïve iPAH patients [32, 59–63], as well as in iPAH [50–52, 62–64] and PAH patients receiving vasodilatory treatment [55, 56, 65, 66]. Data were compared to asymptomatic controls [32, 57, 59–63, 66] or subjects suspected of PH [55, 56, 65] (figure 2e). The overall mean difference was 1684 pg mL−1, (95% CI 1035–2330, p<0.00001) (table 1).
Wang et al. [50] determined the diagnostic accuracy of NT-proBNP in patients with iPAH among asymptomatic controls employing a cut-off >89.25 pg mL−1 (AUC 0.87, p<0.0001) with a sensitivity of 89% and specificity of 78%. Similarly, Malhotra et al. [52] detected PAH patients receiving vasodilatory treatment among asymptomatic controls with an AUC of 0.714. However, with a specificity of 78% [50], NT-proBNP is not suitable for identifying PAH amongst patients with left heart disease.
NT-proBNP was positively associated with markers of disease severity, including right ventricular function, including pulmonary vascular resistance [60, 65], right atrial pressure [60], right ventricular dimensions [59, 61, 66] and exercise tolerance (WHO functional class [51, 60, 65]). NT-proBNP was inversely related to 6MWD [51, 65], cardiac index [60, 65] and mixed venous oxygen concentration [60, 65]. In addition, NT-proBNP decreased significantly after initiation of treatment, in line with decreased pulmonary vascular resistance and is predictive of survival [59, 60, 65]. NT-proBNP was not dependent on the location of blood draw or pulmonary capillary wedge procedure [55].
Renal markers: uric acid
Six publications reporting on UA levels were included in this review, five of which were eligible for meta-analysis. UA levels were measured in treatment-naïve iPAH patients [32, 62, 67], iPAH patients receiving treatment [8, 68] and PAH patients on treatment [54, 69], and compared to asymptomatic controls [8, 32, 54, 62, 67–69] (figure 2f). Meta-analyses detected a significantly higher UA level in PAH compared to control with a mean difference of 1.77 mg dL−1 (95% CI 1.06–2.48, p<0.00001) (table 1).
UA levels in PAH patients were positively associated with right ventricular volume [68], pulmonary vascular resistance [67, 68] and WHO functional class [67, 68], and negatively correlated with cardiac output [67, 68] and mixed venous saturation [68]. UA decreased significantly after initiation of vasodilatory treatment, proportional to the decrease in pulmonary vascular resistance [67, 68]. UA is an independent predictor of 3-year mortality in iPAH [67] and heart failure [70].
BUN was the second renal marker that was analysed. We observed a significant increase of 1.76 mg dL−1 (95% CI 0.51–3.01, p<0.0001; supplementary figure S6a). Creatinine and estimated glomerular filtration rate were eligible but not significantly altered (supplementary figure S6b–c).
Hepatic markers
In three individual studies reporting on alanine aminotransferase (ALT) in treatment-naïve iPAH patients [62], iPAH patients receiving vasodilatory treatment [49] and treatment-naïve PAH patients [37], no significant difference was observed in our meta-analysis (supplementary figure S7). No other hepatic marker was eligible for meta-analysis.
Omics studies
The omics search strategy generated a total of 643 articles: 148 in PubMed, 309 in Embase.com, 183 in Clarivate Analytics/Web of Science Core Collection and three in Wiley/Cochrane Library. After removal of duplicates, 247 remained (represented in figure 1b). We identified 15 publications that analysed metabolomic [71–80] and proteomic profiles [81–85] in iPAH and PAH patients in plasma [71–76, 78, 79, 81, 83, 85, 86] and serum [77, 80, 84, 85, 87]. 14 studies compared signatures to asymptomatic controls, while two studies used common disease controls [72, 74]. Liquid and gas chromatography coupled with mass spectrometry or multiplex assays were the most frequently used methods to detect altered metabolites, proteins or antigens. Targeting component analysis was performed employing a variety of statistical tests (supplementary table S1). Metabolomic studies mainly described glycolytic shift and increased fatty-acid metabolism in patients with PAH, implicating an enhanced glycolytic catabolic state [71, 72–74, 76–79], which Rhodes et al. [72], and He et al. [75] validated in independent cohorts. Proteomic studies describe induced growth factors [82], including erythropoietin [85], hepatic growth factor [82], and inflammatory or immune-response pathways, including complement C4a [81] and several interleukins [85]. Outcomes are summarised in supplementary table S8.
Discussion
Biomarkers may contribute to early noninvasive detection and monitoring of disease. To our knowledge, this is the first systematic review with meta-analyses to evaluate the performance of diagnostic blood markers in patients with group 1 PAH. In this meta-analysis, we identified RDW, LDL-c, d-dimer, NT-proBNP, IL-6 and UA as biomarkers with the largest observed difference and sample size. Plasma NT-proBNP levels showed the largest difference between PAH and non-PH controls. Although it has a high sensitivity for PAH, NT-proBNP lacks specificity to distinguish PAH from other heart diseases. For other biomarkers, including IL-6, RDW, LDL-c, d-dimer and UA, insufficient data were available for meta-analysis of diagnostic accuracy. Owing to the lack of clinical validation, none of the newly proposed biomarkers could equal the sensitivity and specificity of NT-proBNP for detection of PAH.
Performance of current biomarkers in PAH diagnosis
Clinical adoption and implementation of new biomarkers is subject to strict performance metrics and involves: 1) an evidence-based relation between a biomarker and disease; 2) statistical quantification of the predictive strength of biomarker level for the presence of disease, by using calculation of clinical sensitivity and specificity or evaluating ROC curves in diagnostic studies; and 3) availability of multiple independent data sources with sufficient sample sizes and power. When considering the first criterion, the current meta-analysis demonstrates that for various biomarkers a consistent and reproducible relation between PAH and biomarker levels can be found. By using a predefined search and selection strategy 26 biomarkers showed differential expression between the PAH and control population, reflecting the various pathophysiological processes (domains) that contribute to PAH. The number of biomarkers identified in this review is limited by the requirement of a minimum of three publications reporting on a given biomarker to perform a meta-analysis. This approach visualises biomarkers that have consistently been shown to relate to PAH (i.e. in at least three studies) but may ignore promising biomarkers that have not been reproduced in other studies. Markers included in less than three studies or expressed as medians were rendered unsuitable for meta-analysis and are depicted in supplementary tables S4 and S5. These markers include serotonin (5-Ht), asymmetric dimethylarginine (ADMA), angiopoietin-1 (Ang-1), BNP, endostatin, endothelin-1 (ET-1), galectin-3 (Gal-3), hepatocyte growth factor (HGF), high mobility group box 1 (HMGB-1), IL-8, MCP-1, matrix metalloproteinase-2 and -8 (MMP-2, -8), sodium (Na), PlGF, stem cell factor (SCF), sF-selectin, superoxide dismutase (SOD), sVCAM, transforming growth factor-β1 (TGF-β1), angiopoietin-1 receptor-2 (Tie-2), TIMP-4, VEGF and TNF-α (supplementary table S4), and caveolin-1 (CAV-1), HbA1c, IL-12, potassium (K), mean corpuscular volume (MCV), nitric oxide (NO), osteopoietin (OPN), provirus integration site for moloney murine leukaemia virus kinase (Pim-1), selenoprotein-P (Se-p), FGF-2, endoglin (Eng), kynurine (KYN), osteoprotegerin (OPG), N-terminal propeptide of type III procollagen (PIIINP), soluble fms-like tyrosine kinase 1 (sFLT), tissue factor pathway inhibitor (TFPI), thrombomodulin, tryptophan (TRP) and VEGFR1 (supplementary table S5). More studies focusing on these markers would clarify the relation between these markers and PAH.
With regard to the second criterion, while out of 26 meta-analyses, 17 biomarkers were consistently related to the presence of disease, data on ROC curves and calculation of clinical sensitivity and specificity for diagnosis of PAH were only available for NT-proBNP and CRP [50]. Independent validation, preferably in studies including a heterogeneous group of patients and including patients suspected or at risk of developing PAH are needed to clarify diagnostic accuracy, with a focus on providing sensitivity and specificity of a biomarker for disease at relevant and reproducible cut-off values. The latter is an essential step in the identification of biomarkers that may replace invasive diagnostics.
With regard to the third criterion, the drawback of most studies included in this review is a low sample size. The combined sample sizes were largest for NT-proBNP and LDL-c (1152 and 3035, respectively); most other analyses are based on a combined sample size below 450 subjects. Including low sample sizes carries the risk of bias and skewing of data to a selected patient population. This is a general limitation that may be addressed by biobanking, or concurrent analysis of biomarkers in clinical trials. A more systematic approach to biomarker studies may aid authors to increase the number of subjects in biomarker studies
Altogether, our systemic review and meta-analysis reveals a considerable number of biomarkers that were consistently found to be altered in PAH. However, these biomarkers lack the scientific underpinning to replace invasive diagnostics in PAH, either because data on them are lacking or because of a lack of specificity.
Future directions for biomarker development in PAH
Considering the fact that research on single biomarkers has failed to identify a single biomarker with sufficient sensitivity and specificity to foster noninvasive PAH diagnosis, various approaches may be considered to improve noninvasive diagnostics in the future. The first involves combining biomarkers with a strong relation to PAH pathophysiology, which have insufficient diagnostic accuracy on an individual basis, for example, implementing a panel of circulating biomarkers from several domains, weighed by importance to improve biomarker specificity. Based on our meta-analyses, a set of readily available biomarkers may be proposed: a panel including NT-proBNP, IL-6, RDW, UA and LDL-c could potentially be used to score the risk of PAH among clinically similar diseases. A second approach involves combining biomarkers with the strength of noninvasive radiological or haemodynamic measurements. This approach has proven successful in the OPTICS study [88] or DETECT study [89] to exclude iPAH, and in the European Respiratory Society (ERS)/European Respiratory Journal (ERJ) risk criteria and the REVEAL risk stratification [90] to predict outcome in PAH. A third approach may involve unbiased collection of large data sets, including proteomics, transcriptomics and metabolomics, which measure multiple diagnostic biomarkers representative for multiple disease domains in PAH [91]. A PAH-like signature can be used to distinguish iPAH from other diseases. An example is provided by Rhodes et al. [92], employing a selection of nine proteins derived from plasma proteomics, which accurately predict disease outcome in iPAH patients. We believe collaborative biobanks and concomitant analysis of biomarkers in clinical trials and registries are an efficient step forward to improve translation to a clinical setting. External validation cohorts should include patients suspected of PH, and a thoroughly characterised control cohort that contains clinically similar and common diseases.
Strengths and limitations
This review has certain strengths. First, the search strategy of the current study was designed to cover all diagnostic biomarkers research in PAH thus far, resulting in a database on PAH biomarkers of unanticipated size. Second, the meta-analysis was designed to identify biomarkers with consistent performance over several studies. Although this approach may neglect novel, promising biomarkers to a certain extent, the design guarantees identification of biomarkers that were identified in at least three studies, thereby providing surrogate external validation of the biomarker. Third, we focused on easily accessible blood biomarkers thereby potentially bridging the technical gap towards implementation of diagnostic biomarkers in clinical care.
In addition, this meta-analysis has a number of limitations. The major limitation is the lack of validation and calculation of diagnostic accuracy of biomarkers outside their discovery cohort. This renders the reviewing process of sensitivity and specificity for detection of PAH impossible. Second, the meta-analyses were hampered by the limited number of publications addressing iPAH uniquely. Handling iPAH and hPAH patients together as one group, and extracting data of group 1 PAH as second best, meant inclusion of patients with PAH associated with connective tissue disease, congenital heart disease, and drug or toxin use, which may have introduced bias. Next, due to the limited number of studies, we chose not to exclude publications based on QUADAS-2 risk of bias scores, which may have led to inclusion of unreliable data and may have attributed to heterogeneity. However, correction of the most evident sources of bias (treatment status, diagnosis) indicated that bias was negligible.
Conclusion
This study summarises a large number of biomarker studies performed in PAH during the last three decades. Most of the described studies investigated the performance of one single blood biomarker. We conclude that none of these biomarkers have sufficient diagnostic accuracy to replace invasive diagnostics, as all single biomarkers lacked specificity. Using a combination of multiple biomarkers may improve specificity, and this can be achieved by combining a number of routinely available blood tests as well as via an unbiased omics approach.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00009-2022.SUPPLEMENT (985.9KB, pdf)
Footnotes
Provenance: Submitted article, peer reviewed.
Conflict of interest: M.R. Wilkins reports consulting fees from Actelion, MorphogenIX and Novartis, outside the submitted work; and patent (Prognostic biomarker panel derived from discovery science); and a leadership or fiduciary role for the Pulmonary Vascular Research Institute (unpaid). H.J. Bogaard reports receiving grants or contracts from Janssen, MSD, and Ferrer, outside the submitted work; and payment or honoraria for lectures, presentations, speakers’ bureaus, manuscript writing or educational events received from Janssen and MSD, outside the submitted work. The remaining authors have nothing to disclose.
Support statement: This study was supported by the Netherlands Cardio Vascular Research Initiative: CVON-2017-10 DOLPHIN-GENESIS and CVON-2018-29 PHAEDRA-IMPACT. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 2016; 37: 67–119. doi: 10.1093/eurheartj/ehv317 [DOI] [PubMed] [Google Scholar]
- 2.Swinnen K, Quarck R, Godinas L, et al. Learning from registries in pulmonary arterial hypertension: pitfalls and recommendations. Eur Respir Rev 2019; 28: 190050. doi: 10.1183/16000617.0050-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van de Veerdonk MC, Kind T, Marcus JT, et al. Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol 2011; 58: 2511–2519. doi: 10.1016/j.jacc.2011.06.068 [DOI] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339: b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016; 104: 240–243. doi: 10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–536. doi: 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 7.Kereveur A, Callebert J, Humbert M, et al. High plasma serotonin levels in primary pulmonary hypertension. Effect of long-term epoprostenol (prostacyclin) therapy. Arterioscler Thromb Vasc Biol 2000; 20: 2233–2239. doi: 10.1161/01.ATV.20.10.2233 [DOI] [PubMed] [Google Scholar]
- 8.Yaoita N, Shirakawa R, Fukumoto Y, et al. Platelets are highly activated in patients of chronic thromboembolic pulmonary hypertension. Arterioscler Thromb Vasc Biol 2014; 34: 2486–2494. doi: 10.1161/ATVBAHA.114.304404 [DOI] [PubMed] [Google Scholar]
- 9.Edwards AL, Gunningham SP, Clare GC, et al. Professional killer cell deficiencies and decreased survival in pulmonary arterial hypertension. Respirology 2013; 18: 1271–1277. doi: 10.1111/resp.12152 [DOI] [PubMed] [Google Scholar]
- 10.Sada Y, Dohi Y, Uga S, et al. Non-suppressive regulatory T cell subset expansion in pulmonary arterial hypertension. Heart Vessels 2016; 31: 1319–1326. doi: 10.1007/s00380-015-0727-4 [DOI] [PubMed] [Google Scholar]
- 11.Yildiz A, Kaya H, Ertas F, et al. Association between neutrophil to lymphocyte ratio and pulmonary arterial hypertension. Turk Kardiyol Dern Ars 2013; 41: 604–609. doi: 10.5543/tkda.2013.13265 [DOI] [PubMed] [Google Scholar]
- 12.Hautefort A, Girerd B, Montani D, et al. T-helper 17 cell polarization in pulmonary arterial hypertension. Chest 2015; 147: 1610–1620. doi: 10.1378/chest.14-1678 [DOI] [PubMed] [Google Scholar]
- 13.Toshner M, Voswinckel R, Southwood M, et al. Evidence of dysfunction of endothelial progenitors in pulmonary arterial hypertension. Am J Respir Crit Care Med 2009; 180: 780–787. doi: 10.1164/rccm.200810-1662OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smadja DM, Mauge L, Sanchez O, et al. Distinct patterns of circulating endothelial cells in pulmonary hypertension. Eur Respir J 2010; 36: 1284–1293. doi: 10.1183/09031936.00130809 [DOI] [PubMed] [Google Scholar]
- 15.Farha S, Asosingh K, Xu W, et al. Hypoxia-inducible factors in human pulmonary arterial hypertension: a link to the intrinsic myeloid abnormalities. Blood 2011; 117: 3485–3493. doi: 10.1182/blood-2010-09-306357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foris V, Kovacs G, Marsh LM, et al. CD133+ cells in pulmonary arterial hypertension. Eur Respir J 2016; 48: 459–469. doi: 10.1183/13993003.01523-2015 [DOI] [PubMed] [Google Scholar]
- 17.Visovatti SH, Hyman MC, Bouis D, et al. Increased CD39 nucleotidase activity on microparticles from patients with idiopathic pulmonary arterial hypertension. PLoS One 2012; 7: e40829. doi: 10.1371/journal.pone.0040829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khandagale A, Aberg M, Wikstrom G, et al. Role of extracellular vesicles in pulmonary arterial hypertension: modulation of pulmonary endothelial function and angiogenesis. Arterioscler Thromb Vasc Biol 2020; 40: 2293–2309. doi: 10.1161/ATVBAHA.120.314152 [DOI] [PubMed] [Google Scholar]
- 19.Estephan LE, Genuardi MV, Kosanovich CM, et al. Distinct plasma gradients of microRNA-204 in the pulmonary circulation of patients suffering from WHO Groups I and II pulmonary hypertension. Pulm Circ 2019; 9: 2045894019840646. doi: 10.1177/2045894019840646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baptista R, Marques C, Catarino S, et al. MicroRNA-424(322) as a new marker of disease progression in pulmonary arterial hypertension and its role in right ventricular hypertrophy by targeting SMURF1. Cardiovasc Res 2018; 114: 53–64. doi: 10.1093/cvr/cvx187 [DOI] [PubMed] [Google Scholar]
- 21.Qian Z, Li Y, Chen J, et al. miR-4632 mediates PDGF-BB-induced proliferation and antiapoptosis of human pulmonary artery smooth muscle cells via targeting cJUN. Am J Physiol Cell Physiol 2017; 313: C380–C391. doi: 10.1152/ajpcell.00061.2017 [DOI] [PubMed] [Google Scholar]
- 22.Han Y, Liu Y, Yang C, et al. LncRNA CASC2 inhibits hypoxia-induced pulmonary artery smooth muscle cell proliferation and migration by regulating the miR-222/ING5 axis. Cell Mol Biol Lett 2020; 25: 21. doi: 10.1186/s11658-020-00215-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bogdan M, Humbert M, Francoual J, et al. Urinary cGMP concentrations in severe primary pulmonary hypertension. Thorax 1998; 53: 1059–1062. doi: 10.1136/thx.53.12.1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Decker I, Ghosh S, Comhair SA, et al. High levels of zinc-protoporphyrin identify iron metabolic abnormalities in pulmonary arterial hypertension. Clin Transl Sci 2011; 4: 253–258. doi: 10.1111/j.1752-8062.2011.00301.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yaylali YT, Kilic-Toprak E, Ozdemir Y, et al. Impaired blood rheology in pulmonary arterial hypertension. Heart Lung Circ 2019; 28: 1067–1073. doi: 10.1016/j.hlc.2018.07.014 [DOI] [PubMed] [Google Scholar]
- 26.Petrauskas LA, Saketkoo LA, Kazecki T, et al. Use of red cell distribution width in a population at high risk for pulmonary hypertension. Respir Med 2019; 150: 131–135. doi: 10.1016/j.rmed.2019.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes CJ, Wharton J, Howard LS, et al. Red cell distribution width outperforms other potential circulating biomarkers in predicting survival in idiopathic pulmonary arterial hypertension. Heart 2011; 97: 1054–1060. doi: 10.1136/hrt.2011.224857 [DOI] [PubMed] [Google Scholar]
- 28.Zhao J, Mo H, Guo X, et al. Red blood cell distribution width as a related factor of pulmonary arterial hypertension in patients with systemic sclerosis. Clin Rheumatol 2018; 37: 979–985. doi: 10.1007/s10067-017-3918-9 [DOI] [PubMed] [Google Scholar]
- 29.Liu J, Yang J, Xu S, et al. Prognostic impact of red blood cell distribution width in pulmonary hypertension patients: a systematic review and meta-analysis. Medicine (Baltimore) 2020; 99: e19089. doi: 10.1097/MD.0000000000019089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kopeć G, Waligóra M, Tyrka A, et al. Low-density lipoprotein cholesterol and survival in pulmonary arterial hypertension. Sci Rep 2017; 7: 41650. doi: 10.1038/srep41650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Varol E, Uysal BA, Ozaydin M. Platelet indices in patients with pulmonary arterial hypertension. Clin Appl Thromb Hemost 2011; 17: E171–E174. doi: 10.1177/1076029610394438 [DOI] [PubMed] [Google Scholar]
- 32.Wang GF, Guan LH, Zhou DX, et al. Serum high-density lipoprotein cholesterol is significantly associated with the presence and severity of pulmonary arterial hypertension: a retrospective cross-sectional study. Adv Ther 2020; 37: 2199–2209. doi: 10.1007/s12325-020-01304-2 [DOI] [PubMed] [Google Scholar]
- 33.Zamanian RT, Hansmann G, Snook S, et al. Insulin resistance in pulmonary arterial hypertension. Eur Respir J 2009; 33: 318–324. doi: 10.1183/09031936.00000508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brunner NW, Skhiri M, Fortenko O, et al. Impact of insulin resistance on ventricular function in pulmonary arterial hypertension. J Heart Lung Transplant 2014; 33: 721–726. doi: 10.1016/j.healun.2014.02.016 [DOI] [PubMed] [Google Scholar]
- 35.Charach G, George J, Roth A, et al. Baseline low-density lipoprotein cholesterol levels and outcome in patients with heart failure. Am J Cardiol 2010; 105: 100–104. doi: 10.1016/j.amjcard.2009.08.660 [DOI] [PubMed] [Google Scholar]
- 36.Gombos T, Forhecz Z, Pozsonyi Z, et al. Long-term survival and apolipoprotein a1 level in chronic heart failure: interaction with tumor necrosis factor alpha -308 G/A polymorphism. J Card Fail 2017; 23: 113–120. doi: 10.1016/j.cardfail.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 37.Vrigkou E, Tsangaris I, Bonovas S, et al. Platelet and coagulation disorders in newly diagnosed patients with pulmonary arterial hypertension. Platelets 2019; 30: 646–651. doi: 10.1080/09537104.2018.1499890 [DOI] [PubMed] [Google Scholar]
- 38.Can MM, Tanboga IH, Demircan HC, et al. Enhanced hemostatic indices in patients with pulmonary arterial hypertension: an observational study. Thromb Res 2010; 126: 280–282. doi: 10.1016/j.thromres.2010.06.020 [DOI] [PubMed] [Google Scholar]
- 39.Herve P, Humbert M, Sitbon O, et al. Pathobiology of pulmonary hypertension. The role of platelets and thrombosis. Clin Chest Med 2001; 22: 451–458. doi: 10.1016/S0272-5231(05)70283-5 [DOI] [PubMed] [Google Scholar]
- 40.Kylhammar D, Hesselstrand R, Nielsen S, et al. Angiogenic and inflammatory biomarkers for screening and follow-up in patients with pulmonary arterial hypertension. Scand J Rheumatol 2018; 47: 319–324. doi: 10.1080/03009742.2017.1378714 [DOI] [PubMed] [Google Scholar]
- 41.Diller GP, van Eijl S, Okonko DO, et al. Circulating endothelial progenitor cells in patients with Eisenmenger syndrome and idiopathic pulmonary arterial hypertension. Circulation 2008; 117: 3020–3030. doi: 10.1161/CIRCULATIONAHA.108.769646 [DOI] [PubMed] [Google Scholar]
- 42.Heresi GA, Malin SK, Barnes JW, et al. Abnormal glucose metabolism and high-energy expenditure in idiopathic pulmonary arterial hypertension. Ann Am Thorac Soc 2017; 14: 190–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Itoh T, Nagaya N, Ishibashi-Ueda H, et al. Increased plasma monocyte chemoattractant protein-1 level in idiopathic pulmonary arterial hypertension. Respirology 2006; 11: 158–163. doi: 10.1111/j.1440-1843.2006.00821.x [DOI] [PubMed] [Google Scholar]
- 44.Soon E, Holmes AM, Treacy CM, et al. Elevated levels of inflammatory cytokines predict survival in idiopathic and familial pulmonary arterial hypertension. Circulation 2010; 122: 920–927. doi: 10.1161/CIRCULATIONAHA.109.933762 [DOI] [PubMed] [Google Scholar]
- 45.Kopec G, Moertl D, Steiner S, et al. Markers of thrombogenesis and fibrinolysis and their relation to inflammation and endothelial activation in patients with idiopathic pulmonary arterial hypertension. PLoS One 2013; 8: e82628. doi: 10.1371/journal.pone.0082628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Säleby J, Bouzina H, Lundgren J, et al. Angiogenic and inflammatory biomarkers in the differentiation of pulmonary hypertension. Scand Cardiovasc J 2017; 51: 261–270. doi: 10.1080/14017431.2017.1359419 [DOI] [PubMed] [Google Scholar]
- 47.Prins KW, Archer SL, Pritzker M, et al. Interleukin-6 is independently associated with right ventricular function in pulmonary arterial hypertension. J Heart Lung Transplant 2018; 37: 376–384. doi: 10.1016/j.healun.2017.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schlosser K, Taha M, Deng Y, et al. Lack of elevation in plasma levels of pro-inflammatory cytokines in common rodent models of pulmonary arterial hypertension: questions of construct validity for human patients. Pulm Circ 2017; 7: 476–485. doi: 10.1177/2045893217705878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gabrielli LA, Castro PF, Godoy I, et al. Systemic oxidative stress and endothelial dysfunction is associated with an attenuated acute vascular response to inhaled prostanoid in pulmonary artery hypertension patients. J Card Fail 2011; 17: 1012–1017. doi: 10.1016/j.cardfail.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 50.Wang KY, Lee MF, Ho HC, et al. Serum Caveolin-1 as a novel biomarker in idiopathic pulmonary artery hypertension. Biomed Res Int 2015; 2015: 173970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Calvier L, Legchenko E, Grimm L, et al. Galectin-3 and aldosterone as potential tandem biomarkers in pulmonary arterial hypertension. Heart 2016; 102: 390–396. doi: 10.1136/heartjnl-2015-308365 [DOI] [PubMed] [Google Scholar]
- 52.Malhotra R, Paskin-Flerlage S, Zamanian RT, et al. Circulating angiogenic modulatory factors predict survival and functional class in pulmonary arterial hypertension. Pulm Circ 2013; 3: 369–380. doi: 10.4103/2045-8932.110445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Santos M, Reis A, Goncalves F, et al. Adiponectin levels are elevated in patients with pulmonary arterial hypertension. Clin Cardiol 2014; 37: 21–25. doi: 10.1002/clc.22210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Suzuki S, Nakazato K, Sugimoto K, et al. Plasma levels of receptor for advanced glycation end-products and high-mobility Group Box 1 in patients with pulmonary hypertension. Int Heart J 2016; 57: 234–240. doi: 10.1536/ihj.15-188 [DOI] [PubMed] [Google Scholar]
- 55.Fares WH, Ford HJ, Ghio AJ, et al. Safety and feasibility of obtaining wedged pulmonary artery samples and differential distribution of biomarkers in pulmonary hypertension. Pulm Circ 2012; 2: 477–482. doi: 10.4103/2045-8932.105036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hennigs JK, Baumann HJ, Lüneburg N, et al. Fibrinogen plasma concentration is an independent marker of haemodynamic impairment in chronic thromboembolic pulmonary hypertension. Sci Rep 2014; 4: 4808. doi: 10.1038/srep04808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Quarck R, Nawrot T, Meyns B, et al. C-reactive protein: a new predictor of adverse outcome in pulmonary arterial hypertension. J Am Coll Cardiol 2009; 53: 1211–1218. doi: 10.1016/j.jacc.2008.12.038 [DOI] [PubMed] [Google Scholar]
- 58.Smith CL. C-reactive protein and asymmetric dimethylarginine: markers or mediators in cardiovascular disorders? Curr Pharm Des 2007; 13: 1619–1629. doi: 10.2174/138161207780831338 [DOI] [PubMed] [Google Scholar]
- 59.Fijalkowska A, Kurzyna M, Torbicki A, et al. Serum N-terminal brain natriuretic peptide as a prognostic parameter in patients with pulmonary hypertension. Chest 2006; 129: 1313–1321. doi: 10.1378/chest.129.5.1313 [DOI] [PubMed] [Google Scholar]
- 60.Andreassen AK, Wergeland R, Simonsen S, et al. N-terminal pro-B-type natriuretic peptide as an indicator of disease severity in a heterogeneous group of patients with chronic precapillary pulmonary hypertension. Am J Cardiol 2006; 98: 525–529. doi: 10.1016/j.amjcard.2006.02.061 [DOI] [PubMed] [Google Scholar]
- 61.Yang D, Liu Z, Yang Z. Ghrelin and its relation with N-terminal brain natriuretic peptide, Endothelin-1 and nitric oxide in patients with idiopathic pulmonary hypertension. Cardiology (Switzerland) 2013; 124: 241–245. [DOI] [PubMed] [Google Scholar]
- 62.Zhu T, Luo J, Wang Y, et al. Elevated plasma Pim-1 and its clinical significance in patients with pulmonary arterial hypertension. Clin Exp Pharmacol Physiol 2019; 46: 752–760. doi: 10.1111/1440-1681.13102 [DOI] [PubMed] [Google Scholar]
- 63.Lu GH, Gong SG, Li C, et al. Prognostic value of gamma-glutamyltransferase in male patients with idiopathic pulmonary arterial hypertension. Front Cardiovasc Med 2020; 7: 580908. doi: 10.3389/fcvm.2020.580908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Renard S, Paulin R, Breuils-Bonnet S, et al. Pim-1: a new biomarker in pulmonary arterial hypertension. Pulm Circ 2013; 3: 74–81. doi: 10.4103/2045-8932.109917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nickel NP, Lichtinghagen R, Golpon H, et al. Circulating levels of copeptin predict outcome in patients with pulmonary arterial hypertension. Respir Res 2013; 14: 130. doi: 10.1186/1465-9921-14-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fenster BE, Lasalvia L, Schroeder JD, et al. Cystatin C: a potential biomarker for pulmonary arterial hypertension. Respirology 2014; 19: 583–589. doi: 10.1111/resp.12259 [DOI] [PubMed] [Google Scholar]
- 67.Nagaya N, Uematsu M, Satoh T, et al. Serum uric acid levels correlate with the severity and the mortality of primary pulmonary hypertension. Am J Respir Crit Care Med 1999; 160: 487–492. doi: 10.1164/ajrccm.160.2.9812078 [DOI] [PubMed] [Google Scholar]
- 68.Jiang X, Han ZY, Wang Y, et al. Hemodynamic variables and clinical features correlated with serum uric acid in patients with pulmonary arterial hypertension. Chin Med J (Engl) 2008; 121: 2497–2503. doi: 10.1097/00029330-200812020-00006 [DOI] [PubMed] [Google Scholar]
- 69.Jasiewicz M, Kowal K, Kowal-Bielecka O, et al. Serum levels of CD163 and TWEAK in patients with pulmonary arterial hypertension. Cytokine 2014; 66: 40–45. doi: 10.1016/j.cyto.2013.12.013 [DOI] [PubMed] [Google Scholar]
- 70.Huang H, Huang B, Li Y, et al. Uric acid and risk of heart failure: a systematic review and meta-analysis. Eur J Heart Fail 2014; 16: 15–24. doi: 10.1093/eurjhf/hft132 [DOI] [PubMed] [Google Scholar]
- 71.Bujak R, Mateo J, Blanco I, et al. New biochemical insights into the mechanisms of pulmonary arterial hypertension in humans. PLoS One 2016; 11: e0160505. doi: 10.1371/journal.pone.0160505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rhodes CJ, Ghataorhe P, Wharton J, et al. Plasma metabolomics implicates modified transfer RNAs and altered bioenergetics in the outcomes of pulmonary arterial hypertension. Circulation 2017; 135: 460–475. doi: 10.1161/CIRCULATIONAHA.116.024602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sanders JL, Han Y, Urbina MF, et al. Metabolomics of exercise pulmonary hypertension are intermediate between controls and patients with pulmonary arterial hypertension. Pulm Circ 2019; 9: 2045894019882623. doi: 10.1177/2045894019882623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rafikov R, Coletta DK, Mandarino LJ, et al. Pulmonary arterial hypertension induces a distinct signature of circulating metabolites. J Clin Med 2020; 9: 217. doi: 10.3390/jcm9010217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.He YY, Yan Y, Jiang X, et al. Spermine promotes pulmonary vascular remodelling and its synthase is a therapeutic target for pulmonary arterial hypertension. Eur Respir J 2020; 56: 2000522. doi: 10.1183/13993003.00522-2020 [DOI] [PubMed] [Google Scholar]
- 76.Hemnes AR, Luther JM, Rhodes CJ, et al. Human PAH is characterized by a pattern of lipid-related insulin resistance. JCI Insight 2019; 4: e123611. doi: 10.1172/jci.insight.123611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen C, Luo F, Wu P, et al. Metabolomics reveals metabolite changes of patients with pulmonary arterial hypertension in China. J Cell Mol Med 2020; 24: 2484–2496. doi: 10.1111/jcmm.14937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Heresi GA, Mey JT, Bartholomew JR, et al. Plasma metabolomic profile in chronic thromboembolic pulmonary hypertension. Pulm Circ 2020; 10: 2045894019890553. doi: 10.1177/2045894019890553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mey JT, Hari A, Axelrod CL, et al. Lipids and ketones dominate metabolism at the expense of glucose control in pulmonary arterial hypertension: a hyperglycaemic clamp and metabolomics study. Eur Respir J 2020; 55: 1901700. doi: 10.1183/13993003.01700-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yu M, Wang XX, Zhang FR, et al. Proteomic analysis of the serum in patients with idiopathic pulmonary arterial hypertension. J Zhejiang Univ Sci B 2007; 8: 221–227. doi: 10.1631/jzus.2007.B0221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Abdul-Salam VB, Paul GA, Ali JO, et al. Identification of plasma protein biomarkers associated with idiopathic pulmonary arterial hypertension. Proteomics 2006; 6: 2286–2294. doi: 10.1002/pmic.200500510 [DOI] [PubMed] [Google Scholar]
- 82.Amsallem M, Sweatt AJ, Arthur Ataam J, et al. Targeted proteomics of right heart adaptation to pulmonary arterial hypertension. Eur Respir J 2021; 57: 2002428. doi: 10.1183/13993003.02428-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Al-Naamani N, Sagliani KD, Dolnikowski GG, et al. Plasma 12- and 15-hydroxyeicosanoids are predictors of survival in pulmonary arterial hypertension. Pulm Circ 2016; 6: 224–233. doi: 10.1086/686311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang J, Zhang Y, Li N, et al. Potential diagnostic biomarkers in serum of idiopathic pulmonary arterial hypertension. Respir Med 2009; 103: 1801–1806. doi: 10.1016/j.rmed.2009.07.017 [DOI] [PubMed] [Google Scholar]
- 85.Karamanian VA, Harhay M, Grant GR, et al. Erythropoietin upregulation in pulmonary arterial hypertension. Pulm Circ 2014; 4: 269–279. doi: 10.1086/675990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bouzina H, Hesselstrand R, Radegran G. Higher plasma fibroblast growth factor 23 levels are associated with a higher risk profile in pulmonary arterial hypertension. Pulm Circ 2019; 9: 2045894019895446. doi: 10.1177/2045894019895446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Terrier B, Tamby MC, Camoin L, et al. Identification of target antigens of antifibroblast antibodies in pulmonary arterial hypertension. Am J Respir Crit Care Med 2008; 177: 1128–1134. doi: 10.1164/rccm.200707-1015OC [DOI] [PubMed] [Google Scholar]
- 88.Jansen SMA, Huis In 't Veld AE, Jacobs W, et al. Noninvasive prediction of elevated wedge pressure in pulmonary hypertension patients without clear signs of left-sided heart disease: external validation of the OPTICS risk score. J Am Heart Assoc 2020; 9: e015992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Coghlan JG, Denton CP, Grunig E, et al. Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: the DETECT study. Ann Rheum Dis 2014; 73: 1340–1349. doi: 10.1136/annrheumdis-2013-203301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Benza RL, Gomberg-Maitland M, Elliott CG, et al. Predicting survival in patients with pulmonary arterial hypertension: the REVEAL Risk Score Calculator 2.0 and comparison with ESC/ERS-based risk assessment strategies. Chest 2019; 156: 323–337. doi: 10.1016/j.chest.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 91.Oldham WM, Hemnes AR, Aldred MA, et al. NHLBI-CMREF Workshop Report on Pulmonary Vascular Disease Classification: JACC State-of-the-Art Review. J Am Coll Cardiol 2021; 77: 2040–2052. doi: 10.1016/j.jacc.2021.02.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rhodes CJ, Wharton J, Ghataorhe P, et al. Plasma proteome analysis in patients with pulmonary arterial hypertension: an observational cohort study. Lancet Respir Med 2017; 5: 717–726. doi: 10.1016/S2213-2600(17)30161-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary material 00009-2022.SUPPLEMENT (985.9KB, pdf)