Abstract
Introduction
Recent studies have demonstrated a correlation between pemphigus and hidradenitis suppurativa (HS).
Case Presentation
Here, we report the case of a 58-year-old man affected by HS for about 30 years who was found to have lesions attributable to pemphigus during a checkup.
Discussion/Conclusion
There are few data in the literature on the use of systemic corticosteroids for the two diseases, and our article wants to be a food for thought on the management and treatment of these diseases.
Keywords: Hidradenitis suppurativa, Pemphigus, Systemic steroids
Established Facts
A recent analysis of comorbidities in hospitalized pemphigus patients in the USA demonstrated a significant association of hidradenitis suppurativa and pemphigus, showing an odds ratio = 5.34.
Novel Insights
Several authors have recently described how hidradenitis suppurativa patients are likely to benefit from addition of systemic steroids to other medical therapies for both disease control and preoperative care.
Introduction/Literature Review
Hidradenitis suppurativa (HS) is a chronic, inflammatory, recurrent, debilitating skin disease, involving usually the axillae, inguinal, and anogenital regions [1]. Pemphigus diseases are uncommon chronic, autoimmune blistering diseases that involve skin and mucous membranes. Several inflammatory conditions including rheumatoid arthritis, diabetes, and psoriasis are described to be more frequent with Pemphigus [2, 3]. A recent analysis of comorbidities in hospitalized pemphigus patients in the USA demonstrated a significant association of HS and pemphigus, showing an odds ratio = 5.34 [4].
Case Report
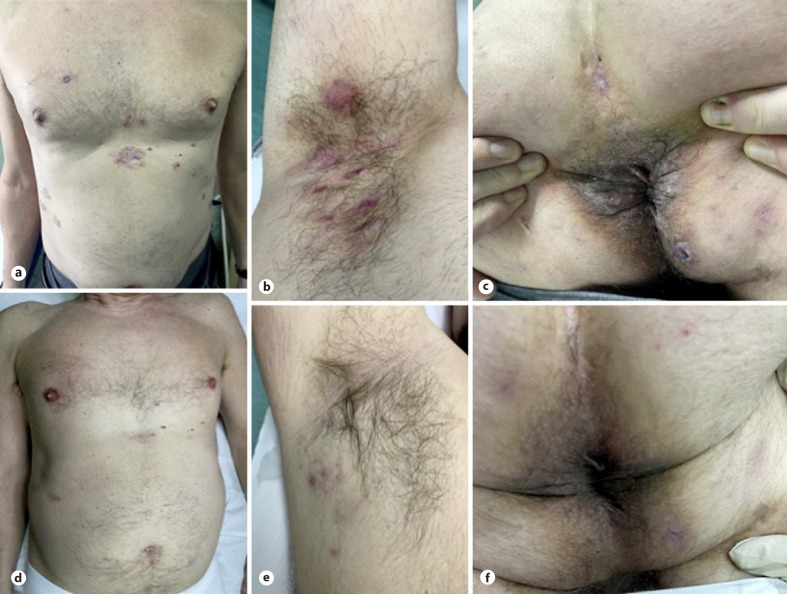
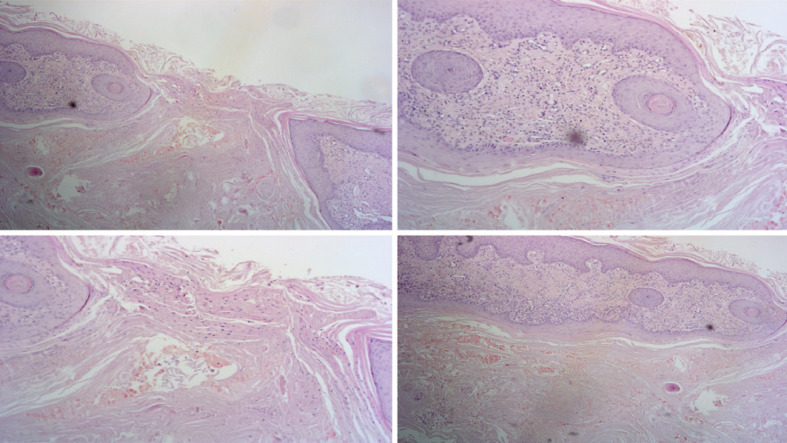
Herein we report the case of a 58-year-old male patient affected by HS since 30 years, who unsuccessfully underwent multiple antibiotic therapies during his life, such as rifampicin and clindamycin, tetracyclines, macrolides, and penicillins. In 2018, the patient was staged as IHS4 12, DLQ1 19, and a VAS pain 8: indeed, the patient was treated with subcutaneous injections of adalimumab at a dose of 160 mg at baseline, 80 mg at week 2, 40 mg at week 4, and 40 mg weekly thereafter. After 6 months, a reduction of pain was achieved (VAS from 8 to 4); nevertheless, after a further 6 months, there was a loss of efficacy of the treatment and the patient referred a worsening of the manifestations (IHS4 = 13). Therefore, treatment was interrupted; from 2018, the patient used only antibiotic therapy as needed with a great worsening of disease's severity (IHS4 = 16) and quality of life (DLQI = 22). During a follow up visit, patient presented multiple erosion and crust lesions located on the chest (Fig. 1a-c). A biopsy and direct immunofluorescence evaluations were performed, showing intraepidermal bullous lesion with acantholytic aspects, consisting mainly of eosinophils and neutrophils about skin biopsy (Fig. 2), while the presence of circulating autoantibodies about indirect immunofluorescence confirming the diagnosis of pemphigus vulgaris. Immunosuppressive therapies were not suitable since patient's comorbidities (chronic liver disease and arterial hypertension treated with ace inhibitors). Systemic steroids (SS) therapy was performed with the following schedule: metilprednisolone 16 mg, twice a day for 10 days, followed by 16 mg daily for further 10 days and finally 8 mg daily for 20 days. The patient came for a follow-up visit after 2 months showing a total regression of the pemphigus and a great improvement of HS lesions as well (IHS4 = 8; DLQI = 7) (Fig. 1d-f). A follow-up visit after 6 months was performed showing the persistence of the regression for both pemphigus and HS.
Fig. 1.
a Pemphigus lesions located in the trunk before the treatment. b HS lesions located in the axillae region before the treatment. c HS lesions located in the anal region before the treatment. d Pemphigus lesions located in the trunk after the treatment. e HS lesions located in the axillae region after the treatment. f HS lesions located in the anal region after the treatment.
Fig. 2.
Suprabasal intraepidermal bullous lesion with acantholytic aspects, the content of the blister consists predominantly of eosinophils and neutrophils.
Discussion
Several data showed that SS were beneficial for pemphigus but at the same time it could be useful for the treatment of HS. Despite this shift toward anti-inflammatory therapies in HS, evidence is scarce regarding the use of SS, with only a limited number of case reports and series available. In the management for HS, we may describe two different use of SS: the use of intralesional triamcinolone acetonide for localized lesions and SS as rescue therapies for the treatment of pain. The majority of patients reported improvements in disease state, quality of life, and overall satisfaction after administration of high-dose intralesional triamcinolone acetonide (20–40 mg/mL) [5]. In any case, this therapeutic approach has limitations regarding the severity and multiple anatomical locations of HS. Finally, the numerous relapses following the treatment should also be reported [6, 7]. Several authors have recently described how HS patients are likely to benefit from addition of SS to other medical therapies for both disease control and preoperative care [8]. In addition, high-dose SS may be recommended for acute flares [9]. Our case of pemphigus and HS, treated successfully with metilprednisolone for both diseases, opens up new therapeutic ideas and reflections on the use of the steroid in the management of patients with HS. Certainly SS demonstrate significant efficacy but a high relapse rate on discontinuation. Nonetheless, our patient maintains a state of well-being after 6 months from the suspension of treatment. However, further studies are needed to better clarify the possible role of SS in the management of HS.
Statement of Ethics
Written consent on photos and clinical data publication was given by the patient. Ethical approval was not required for this study in accordance with national guidelines.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Funding Sources
The authors have received no funding.
Author Contributions
Dr. Fabrizio Martora has given his contribution to manuscript conception and writing. Dr Lorenzo Martora has given his contribution to manuscript conception and writing. Prof. Gabriella Fabbrocini has given her contribution reviewing the paper for important intellectual content. Dr. Claudio Marasca has given his contribution to manuscript conception and reviewed the paper for important intellectual content.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- 1.Marasca C, Tranchini P, Marino V, Annunziata MC, Napolitano M, Fattore D, et al. The pharmacology of antibiotic therapy in hidradenitis suppurativa. Expert Rev Clin Pharmacol. 2020 May;13((5)):521–30. doi: 10.1080/17512433.2020.1762571. [DOI] [PubMed] [Google Scholar]
- 2.Gutierrez Y, Pourali SP, Singh I, Armstrong AW. Pemphigus and bullouspemphigoid in the UnitedStates: a 21-year analysis of patientcharacteristics, treatment patterns, and comorbidities. J Dermatolog Treat. 2021 Apr 7;:1–3. [Google Scholar]
- 3.Clawson RC, Tabata MM, Chen ST. Pemphigus vulgaris flare in a patient treated with nivolumab. Dermatol Ther. 2021 Mar;34((2)):e14871. doi: 10.1111/dth.14871. [DOI] [PubMed] [Google Scholar]
- 4.Kridin K, Jones VA, Patel PM, Gibson FT, Amber KT, Cohen AD. Hidradenitis suppurativa and pemphigus: a cross-sectional study. Arch Dermatol Res. 2020 Sep;312((7)):501–5. doi: 10.1007/s00403-020-02040-x. [DOI] [PubMed] [Google Scholar]
- 5.Garelik J, Babbush K, Ghias M, Cohen SR. Efficacy of high-dose intralesional triamcinolone for hidradenitis suppurativa. Int J Dermatol. 2021 Feb;60((2)):217–21. doi: 10.1111/ijd.15124. [DOI] [PubMed] [Google Scholar]
- 6.Saunte DML, Jemec GBE. Intralesional triamcinolone for hidradenitis suppurativa-how much is needed? Dermatol Surg. 2021 Feb 22;47((7)):1013–4. doi: 10.1097/DSS.0000000000002753. [DOI] [PubMed] [Google Scholar]
- 7.Fajgenbaum K, Crouse L, Dong L, Zeng D, Sayed C. Intralesional triamcinolonemaynot be beneficial for treating acute hidradenitis suppurativa lesions: a double-blind, randomized, placebo-controlled trial. Dermatol Surg. 2020 May;46((5)):685–9. doi: 10.1097/DSS.0000000000002112. [DOI] [PubMed] [Google Scholar]
- 8.Duarte B, Cunha N, Lencastre A, Cabete J. Systemic steroids in the management of moderate-to-severe hidradenitis suppurativa. Actas Dermosifiliogr. 2020 Dec;111((10)):879–83. doi: 10.1016/j.ad.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 9.Wong D, Walsh S, Alhusayen R. Low-dose systemic corticosteroid treatment for recalcitrant hidradenitis suppurativa. J Am Acad Dermatol. 2016 Nov;75((5)):1059–62. doi: 10.1016/j.jaad.2016.06.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.