Abstract
Introduction
Family caregivers of persons living with dementia (PLWDs) have extensive social, physical, emotional, and financial responsibilities. However, less is known about the relationship and interpersonal connection between caregivers and PLWDs. We examined caregiver pronoun use, as an index of the connection between the caregiver and PLWD and its associations with the caregiver's and PLWD's health and well-being.
Methods
Caregivers of PLWDs (N = 320) were asked to describe a recent time they felt connected to the PLWD in their care. Responses were transcribed and coded to quantify pronoun use by category (we-pronouns, I-pronouns, and they-pronouns). Caregivers also reported on their depression, burden, and the PLWD's dementia severity and marital satisfaction. Sixty-eight caregivers repeated the same survey 24 months after the initial survey.
Results
Caregivers used less we-pronouns when the PLWD's dementia was more severe, at both timepoints. Spousal caregivers used more we-pronouns and less I- and they-pronouns than nonspousal caregivers. There was an interaction between spousal relationship and dementia severity, such that spousal caregivers exhibited a stronger negative association between dementia severity and we-pronoun use. There were no associations between pronoun category and caregiver burden or depression.
Discussion
Caregivers may feel increasingly disconnected from the PLWD as their dementia becomes more severe, as reflected by less we-pronoun usage. This study highlights the opportunity to explore relationship connection through text analysis.
Keywords: Connection, Neurodegenerative disease, Alzheimer's disease, Marital satisfaction, Disease severity, Caregiver burden
Introduction
More than 15 million people provide informal care for persons living with dementia (PLWDs) in the USA, which involves immense emotional, physical, and practical support [1, 2, 3, 4]. Growing evidence suggests that dementia can alter the nature of the PLWD-caregiver relationship, which is closely tied to physical health and psychological well-being [5]. Experiences of connection in the caregiving relationship are important for maintaining hope and demonstrating support [6, 7], yet the caregiver-PLWD connection has not been studied extensively.
Text analysis is a powerful tool for studying relational dynamics as language often reflects underlying social and psychological meaning [8]. Studies of personal pronoun usage (“we,” “you,” “I,” and “he/she/they”) in naturalistic conversation have revealed associations of we-pronoun use with marital satisfaction, marital quality, health, and well-being [9, 10, 11, 12]. To our knowledge, no prior studies have investigated pronoun use of individual caregivers in a narrative or interview format, which may offer insights into caregivers' experience outside of the conversational context.
In the present study, caregivers described a recent time they felt connected to the PLWD, and we measured their pronoun use to assess the quality of that connection. As in prior work [9, 13], we conceptualized we-pronoun use as reflecting greater connection between the caregiver and PLWD and greater I- and they-pronoun use as reflecting greater perceived separateness. Given documented associations of relationship factors (e.g., satisfaction, closeness, etc.) with the caregiver's and PLWD's health and well-being [14, 15, 16], we sought to examine whether a language-based measure of connection (i.e., pronoun use) would reveal similar associations with caregiver health and well-being.
We tested two primary hypotheses. We hypothesized that greater use of we-pronouns would be associated with (1) better PLWD health outcomes (e.g., lower dementia severity) and (2) less caregiver depression and burden. We also explored whether caregiving relationship type (i.e., spouse vs. nonspouse) moderated associations between pronoun use and PLWD outcomes and whether associations with we-pronoun use were independent of caregiver-reported PLWD marital satisfaction. Hypotheses were preregistered: https://aspredicted.org/TUD_ACM.
Materials and Methods
Site
The Care Ecosystem is a program in which Care Team Navigators manage caseloads of PLWDs and caregivers by providing emotional support and other resources. The program was administered from two hubs, the University of California, San Francisco (UCSF), and the University of Nebraska Medical Center (UNMC), Omaha, and was studied in a randomized controlled trial. Those in the usual care (control) group completed surveys but did not receive care navigation. The Care Ecosystem intervention improved the quality of life of PLWDs, reduced emergency department visits, and decreased caregiver depression and burden [17].
Participants
Caregivers enrolled in the Care Ecosystem completed a telephone survey 6 months after enrollment that included the question, “Tell me about a time you felt most connected to (PLWD name) in the last few months.” Of the 439 responses to this question, 119 were not recorded verbatim and were excluded, resulting in a sample of 320 caregiver-PLWD dyads. The same survey was given 30 months after enrollment, and the sample was smaller (n = 68) due to study completion, death, and nonverbatim transcription. Demographic characteristics of caregivers and PLWDs are presented in Table 1.
Table 1.
Sociodemographic characteristics and clinical variables (means and standard deviations provided, unless otherwise noted)
| Variable | Full sample (month 6) |
Follow-up sample (month 30) |
||
|---|---|---|---|---|
| caregiver | PLWD | caregiver | PLWD | |
| N | 320 | 320 | 68 | 68 |
| Age at baseline | 74.40 (31.54) | 77.44 (9.19) | 69.25 (17.76) | 76.89 (8.72) |
| Gender = female, N (%) | 234 (73.12) | 163 (59.94) | 59 (86.76) | 29 (42.65) |
| Race, N (%) | ||||
| American Indian or Alaska Native | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Asian | 22 (6.88) | 21 (6.56) | 4 (5.88) | 3 (4.41) |
| Black or African American | 13 (4.06) | 13 (4.06) | 0 (0) | 1 1.47) |
| Native Hawaiian or other Pacific Islander | 2 (0.62) | 1 (0.31) | 0 (0) | 0 (0) |
| White | 249 (77.81) | 248 (77.50) | 56 (82.35) | 57 (83.82) |
| Unknown | 34 (10.62) | 37 (11.56) | 8 (11.76) | 7 10.29) |
| Education | 14.78 (3.44) | 13.34 (4.35) | 14.90 (3.96) | 13.99 (4.82) |
| Relationship to the PLWD = spouse, N (%) | 172 (53.75) | 40 (58.82) | ||
| Caregiver burden (ZBI-12) | 16.19 (9.03) | 22.02 (6.58) | ||
| Caregiver well-being (PHQ-9) | 4.14 (4.42) | 5.62 (4.20) | ||
| Caregiver intervention group = usual care (control), N (%) | 110 (34.38) | 31 (45.59) | ||
| PLWD dementia severity (QDRS) | 14.20 (6.80) | 18.19 (6.65) | ||
| PLWD marital satisfaction (single item from QoL-AD) | 3.05 (0.72) | 2.82 (0.91) | ||
ZBI-12, Zarit Burden Interview; PHQ-9, PLWD Health Questionnaire; QDRS, Quick Dementia Rating Scale; QoL-AD, Quality of Life in Alzheimer's Disease Scale. For clinical variables (i.e., ZBI-12, PHQ-9, QDRS, and QoL-AD), descriptive statistics are reported for each sample from their corresponding timepoint – month 6 or month 30, respectively. All sociodemographic variables are considered constant and are the same at all timepoints (apart from age, which is reported at baseline).
Procedures
Informed consent was obtained from both caregivers and PLWDs upon enrollment. In telephone surveys given 6 and 30 months after enrollment, caregivers responded to questions about PLWD and caregiver demographics, health, and well-being, including an open-ended question about their connection to the PLWD [17]. The UCSF and UNMC institutional review boards approved this study.
Measures
Pronoun Use
Caregivers' responses to the “connection” question were transcribed and processed using software written by one of the authors [18]. Oedipus Text utilizes a dictionary of personal pronouns [9, 13] with four categories: (a) we-pronouns (we, we'd, we'll, we're, we've, our, ours, ourselves, and us), (b) I-pronouns (I, I'd, I'll, I'm, I've, me, mine, my, and myself), (c) they-pronouns (he, his, him, himself, she, her, hers, herself, they, theirs, them, and themself), and (d) you-pronouns (you, you'd, you'll, you're, you've, your, yours, and yourself). Oedipus Text reviewed the transcribed responses and assigned each pronoun used to its dictionary-based category.
Next, a team of five trained coders reviewed each instance of pronoun use to confirm the dictionary-based categorization. Given the interview format, you-pronouns were rare and usually referred to the interviewer; therefore, they were excluded. Pronouns from quotations were retained when the caregiver referred to themselves (e.g., “Isaid, ‘I'mvery happy…'”) but excluded when the caregiver quoted someone else (e.g., “A man came over…and said, ‘You must loveyourwife very much.'”). We- and they-pronouns were excluded when they did not refer to the caregiver-PLWD dyad (e.g., “we” referring to the caregiver and a friend). To establish the reliability, approximately 22% of responses were reviewed by all coders. Interrater reliability was high (ICC = 0.99). See Table 2 for example responses.
Table 2.
Example responses by the pronoun type
| We | I | He/she/they |
|---|---|---|
| “Last night we ate on our patio and he asked if I would turn Alexa on to play music. And as we finished our meal I was walking him back to our sitting area in the bedroom and one of the songs that came on was a romantic song. He used to be an extraordinary, award-winning dancer. So I took his arms and held on to him and we danced for a few minutes. It was pretty special.” | “I feel really close with my mom when she gets up in the morning. Every morning I go and over to her when she is waking up and say ‘Good morning, mom! It's a beautiful day today’ and I start singing to her too. I always try to talk with her even though she can't say any real words but I will tell her about the plans for the day and she'll smile and she looks really happy. It reminds me that my mom is still ‘there’ and seeing her happy and laughing makes everyone else happy.” | “Yeah sure, we feel very connected in general. Just a few nights ago, he woke up in the middle of the night, he was hugging me and saying all these things. He was being very affectionate in his sleep, wrapping his arms around me and putting his legs around me. Other things, he can be very funny and humorous and I feel really connected when he shares these stories.” |
|
| ||
| “Let's see…usually after we eat supper, we usually will watch TV or listen to music. We don't converse but we sit there with each other. She will smile and even laugh when we are together. We will be sitting there and she will smile and laugh with me.” | “I was gone out of town on business for a few days. He doesn't have any sense of time anymore, so he'll forget I was home if I leave the room for a minute. Every night I give him a kiss goodnight, but he takes a medication that makes him really pass out. But every night when I kiss him goodnight he always puckers his lips to kiss me back, which is amazing considering the medication. So when I got back from my business trip I figured he wouldn't remember that I had been gone for the past week. But when I went to kiss him goodnight he not only kissed me but smiled and gave a little laugh. And I could just tell that he had missed me and was happy I was home.” | “Just being with her, spending time with her and knowing that she's well cared for by her family is enough. I wouldn't want to send her to a senior home. I just want to do my job as a daughter and be there for her until the very end. I'm going to be there for her just like she has for me.” |
|
| ||
| “We had gone somewhere but I don't remember where we had gone and we had a good and that evening we had what was the most normal conversation we've had in a long time. I was quite surprised by how clear and focused she was” | “He held me when I was crying. My cousin's son died due to PTSD. I was really sad and he saw me crying. He just held me. He rubbed my back. It was really tender and sweet. He was there for me even in his illness.” | “When we were on our return flight from our travels, there was a little bit of a delay but I had downloaded a bunch of tv shows he liked, provided some drawing pads and he just perked right up. I felt good because I had an answer for him whenever he's stressed. He was really excited to go home and I'm glad he didn't feel overwhelmed from the delay. He even hugged and kissed me on the plane and when the plane took off, he clapped his hands. He was happy to return to the comforts of his home.” |
Caregiver and PLWD Well-Being Survey
PLWD dementia severity was assessed using the Quick Dementia Rating Scale (QDRS), a 10-item questionnaire asking caregivers to rate PLWDs' cognition, function, behavior, and mood. Items are summed, ranging from 0 to 30. Higher scores reflect greater impairment [19].
PLWD marital satisfaction was assessed using a single item from the Quality of Life in Alzheimer's Disease Scale (QoL-AD). Caregivers rated PLWDs' marital satisfaction on a four-point scale ranging from “poor” to “excellent” [20].
Caregiver burden was assessed using the 12-item version of the Zarit Burden Interview (ZBI-12), which measures the perceived impact of providing care on caregivers' health, personal life, and emotional well-being. Ratings are on a five-point scale ranging from “never” to “almost always.” Higher scores reflect greater burden [21].
Caregiver depression was assessed using the Patient Health Questionnaire (PHQ-9), a 9-item questionnaire asking about mood (e.g., feeling down, depressed, or hopeless) on a four-point scale ranging from “not at all” to “nearly every day” [22].
Results
Data Reduction
We calculated a proportion score for each of the three pronoun categories by dividing the number of pronouns in each category by the total number of pronouns in the entire response. To avoid problems with multicollinearity, we analyzed associations with each pronoun category separately.
Data Analysis
All analyses were conducted in R Studio Version 1.2.1335. First, we evaluated bivariate correlations between the pronoun category (we, I, and they) and caregiver's and PLWD's health and well-being (PLWD dementia severity, PLWD marital satisfaction, caregiver burden, and caregiver depression). Second, we probed the robustness of significant associations by controlling for a set of covariates chosen a priori based on their expected associations with these constructs: caregiver age, gender, education (in years), relationship type (spouse vs. nonspouse), and intervention group assignment. To be conservative, we ran analyses with all covariates in the same model. We reevaluated significant associations at the 30-month timepoint.
Next, we explored whether being a spousal caregiver moderates significant associations between we-pronoun use and well-being outcomes and whether significant associations between we-pronoun use and well-being outcomes are independent of caregiver-reported PLWD marital satisfaction (analyses limited to spousal caregivers only). Table 3 presents descriptive statistics of caregivers' responses.
Table 3.
Descriptive statistics of pronouns and words used by caregivers, reported for the 6-month sample and the 30-month sample
| Word category | Mean | SD | Range |
|---|---|---|---|
| We-pronouns | |||
| Raw | 0.97/1.26 | 1.33/1.83 | 0–7/0–10 |
| Proportion | 0.28/0.23 | 0.34/0.30 | 0–1/0–1 |
| 1st person pronouns | |||
| Raw | 1.78/2.54 | 2.19/3.41 | 0–15/0–18 |
| Proportion | 0.32/0.34 | 0.27/0.27 | 0–1/0–1 |
| 3rd person pronouns | |||
| Raw | 2.01/2.78 | 2.44/2.58 | 0–16/0–11 |
| Proportion | 0.40/0.43 | 0.30/0.30 | 0–1/0–1 |
| Total pronouns | 4.76/6.59 | 4.46/5.66 | 0–27/0–31 |
| Total words | 27.71/39.31 | 23.74/32.07 | 1–183/0–172 |
Reporting values for the full, 6-month sample (N = 320) on the left side of the forward slash (/) and for the follow-up, 30-month sample (n = 68) on the right side of the slash, respectively. Raw pronoun categories refer to the total number of pronouns used. The proportion of pronoun categories refers to the total number of pronouns used in that category divided by the total number of pronouns used.
Pronoun Use and Dementia Severity
Six-Month Timepoint
PLWD dementia severity was significantly negatively correlated with we-pronouns and positively correlated with I- and they-pronouns. In other words, less use of we-pronouns and more use of I- and they-pronouns by caregivers were associated with greater dementia severity in PLWDs, supporting our first hypothesis (see Table 4).
Table 4.
Bivariate correlations between the pronoun category (we, I, and they) and PLWD dementia severity at 6-month and 30-month timepoints
| r | df | p value | |
|---|---|---|---|
| Six-month timepoint | |||
| We-pronouns | –0.31 | 274 | <0.001*** |
| I-pronouns | 0.21 | 274 | <0.001*** |
| They-pronouns | 0.17 | 274 | 0.005** |
| Thirty-month timepoint | |||
| We-pronouns | –0.30 | 62 | 0.014* |
| I-pronouns | 0.43 | 62 | <0.001*** |
| They-pronouns | –0.14 | 62 | 0.27 |
PLWD, person living with dementia.
p < 0.05.
p < 0.01.
p < 0.001.
Next, we conducted multiple regression analyses with pronoun use predicting PLWD dementia severity, controlling for caregiver age, gender, education, relationship to PLWD, and intervention group. All three pronoun categories remained significantly associated with dementia severity when accounting for covariates (see Table 5).
Table 5.
Multivariate regressions with the pronoun category (we, I, and they) and covariates predicting PLWD dementia severity
| B | SE | t | p value | |
|---|---|---|---|---|
| We-pronouns model | ||||
| We-pronouns | –0.33 | 0.06 | –5.49 | <0.001*** |
| Caregiver age | 0.00 | 0.05 | –0.08 | 0.94 |
| Caregiver gender = female | 0.05 | 0.07 | 0.69 | 0.49 |
| Caregiver education | –0.12 | 0.06 | –2.03 | 0.04<0.001* |
| Relationship type = spouse | 0.08 | 0.06 | 1.33 | 0.19 |
| Intervention group = usual care | 0.05 | 0.06 | 0.89 | 0.37 |
| I-pronouns model | ||||
| We-pronouns | 0.21 | 0.06 | 3.58 | <0.001<0.001*** |
| Caregiver age | 0.02 | 0.06 | 0.29 | 0.77 |
| Caregiver gender = female | 0.05 | 0.07 | 0.77 | 0.44 |
| Caregiver education | –0.12 | 0.06 | –2.02 | 0.04<0.001* |
| Relationship type = spouse | 0.02 | 0.06 | 0.28 | 0.78 |
| Intervention group = usual care | 0.03 | 0.06 | 0.51 | 0.61 |
| They-pronouns model | ||||
| We-pronouns | 0.17 | 0.06 | 2.84 | 0.005<0.001** |
| Caregiver age | 0.06 | 0.07 | 0.84 | 0.40 |
| Caregiver gender = female | 0.00 | 0.06 | –0.09 | 0.93 |
| Caregiver education | –0.12 | 0.06 | –2.05 | 0.04<0.001* |
| Relationship type = spouse | 0.04 | 0.06 | 0.59 | 0.56 |
| Intervention group = usual care | 0.03 | 0.06 | 0.49 | 0.62 |
PLWD, person living with dementia.
p < 0.05.
p < 0.01.
p < 0.001.
Thirty-Month Timepoint
Bivariate correlations revealed that dementia severity at the 30-month timepoint remained significantly negatively associated with we-pronouns and positively associated with they-pronouns but was no longer associated with I-pronouns (see Table 4). Given the limited sample size, we did not explore the robustness of these associations using covariates.
We-Pronouns, Dementia Severity, and Caregiver-PLWD Relationship
We explored group differences in we-pronoun use, comparing spousal caregivers to nonspousal caregivers. Levene's test revealed heteroskedasticity (p < 0.001); therefore, we used a Welch two-sample t test. Spouses used more we-pronouns (M = 0.37, SD = 0.35) than did non-spouses (M = 0.19, SD = 0.31; t(274.3) = −4.51, p < 0.001).
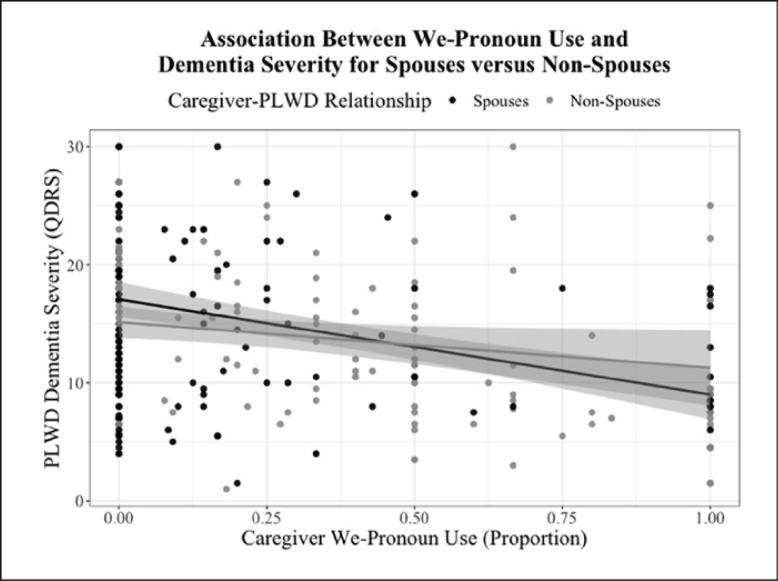
Next, we conducted a regression with spousal relationship (0 = non-spouse, 1 = spouse), PLWD dementia severity, and an interaction term between spousal relationship and dementia severity as independent variables and we-pronouns as the dependent variable. In addition to significant main effects for spousal relationship and dementia severity, we found a significant interaction effect, such that being a spouse amplified the negative association between dementia severity and we-pronoun use (see Table 6; Fig. 1).
Table 6.
Spousal relationship, dementia severity, and their interaction predicting we-pronoun use
| β | SE | t | p value | |
|---|---|---|---|---|
| Relationship type = spouse | 0.26 | 0.06 | 4.63 | <0.001*** |
| PLWD dementia severity | –0.31 | 0.06 | –5.51 | <0.001** |
| Relationship type × dementia severity | –0.27 | 0.11 | –2.44 | 0.016* |
PLWD, person living with dementia.
p < 0.05.
p < 0.01.
p < 0.001.
Fig. 1.
Spousal relationship moderates the association between dementia severity and we-pronoun use. Spousal caregivers (depicted in black) have a stronger, negative association between we-pronoun use and PLWD dementia severity, as compared to non-spousal caregivers (depicted in gray).
Observational versus Caregiver-Reported Relationship Measures and Dementia Severity
We-pronoun use was not correlated with caregiver-reported PLWD marital satisfaction (r = 0.13, p = 0.126) in our sample of spousal caregivers (n = 172). In a regression with we-pronoun use and caregiver-reported PLWD marital satisfaction predicting PLWD dementia severity, we found that greater proportion of we-pronouns and greater marital satisfaction were each independently associated with lower dementia severity (see Table 7).
Table 7.
We-pronoun use and marital satisfaction predicting PLWD dementia severity
| β | SE | t | p value | |
|---|---|---|---|---|
| We-pronouns | –0.39 | 0.08 | –5.23 | <0.001*** |
| Caregiver-reported PLWD marital satisfaction | –0.15 | 0.08 | –2.00 | 0.048<0.001* |
PLWD, person living with dementia.
p < 0.05.
p < 0.001.
Pronoun Use and Caregiver Well-Being
We examined bivariate correlations between pronoun category and caregiver depression and burden, respectively. Contrary to our second hypothesis, neither proportion of we-pronouns and I-pronouns nor they-pronouns were significantly associated with caregiver depression nor burden (p > 0.55).
Discussion
We examined associations between pronoun used by caregivers in response to a question about their connection with the PLWD with caregivers' and PLWDs' health and well-being. Lower use of we-pronouns and greater use of I- and they-pronouns were associated with greater dementia severity. These associations were robust when controlling for covariates and stable across time. Spousal caregivers used more we-pronouns than non-spousal caregivers. There was also an interaction between relationship type and dementia severity such that the negative association between dementia severity and we-pronoun use was stronger for spousal caregivers than for non-spousal caregivers. Finally, we found that lesser use of we-pronouns by spousal caregivers was predictive of dementia severity, independent of caregiver-reported PLWD marital satisfaction. We did not find any associations between caregiver pronoun use and caregiver burden and depression.
The association between caregiver we-language and PLWD dementia severity could reflect a loss of connection as the disease progresses. As the PLWDs dementia becomes more severe, shared activities and conversations may become less frequent and less fulfilling for the caregiver. Additionally, as dementia severity increases, interpersonal problems between the caregiver and PLWD, such as abuse, may also increase [23], impacting their connection.
In contrast, I- and they-pronoun use was positively associated with dementia severity, albeit less robustly (e.g., I-pronouns were not correlated with dementia severity at 30 months). Given prior evidence linking I- and they-pronouns to experiences of separateness [13], these pronouns may reflect caregivers' psychological disconnection from the PLWD. As the disease progresses, caregivers and PLWDs may become disconnected because they no longer have as many shared activities, the PLWD may be more self-focused, or the caregiver takes on a more service-oriented role [24].
Prior text analysis studies have linked greater use of we-pronouns with better caregiver health and well-being [9, 10, 11]; however, we did not find similar associations in the present study. One reason for this may be that prior studies focused on dyadic conversations that can be influenced by many issues in the caregiver-PLWD relationship. These conversations elicit language (and pronoun use) by both members of the dyad as well as moments of felt emotion that may have stronger ties to caregiver health and well-being. Our study only examined caregivers' direct comments about a lived experience of connection, which is less likely to occur during dyadic interactions. We expect that studying pronoun use in both contexts, dyadic interactions and open-ended interview questions, will provide a richer understanding of the ways pronoun usage is related to the different aspects of the caregiving experience, the caregiver-PLWD relationship, and the longer term impact on health and well-being.
We also note that our study did not address the longitudinal changes that occur in caregivers' experience of connection nor the ways these changes are associated with changes in caregiver health and well-being. For example, ample research suggests that distance and disconnection may be helpful for caregivers. In a recent study from our research group, lower levels of emotional empathy in caregivers (i.e., not feeling the emotions of people in distress) were associated with having fewer mental health problems [25]. Disconnecting from the PLWD as dementia progresses may be a natural part of caregivers' grieving and loss [26]. Indeed, longitudinal research has found that decreased caregiver-rated closeness can be a protective factor when dealing with cognitive and functional decline in the PLWD [27].
Finally, we found that we-pronoun use was significantly associated with dementia severity when accounting for caregiver-reported PLWD marital satisfaction. This finding points to the advantage of assessing caregiver pronoun use in addition to more commonly used self-report measures. When assessing current relationship quality, caregivers may face difficulty disentangling feelings from the present and past. Measuring connection in spontaneous speech may capture different aspects of current perceptions and reduce bias. For this reason, clinicians may find it useful to pay closer attention to the words caregivers use to gain a deeper understanding of the impact of the PLWD's disease on the caregiver and the caregiver-PLWD relationship.
Limitations and Future Directions
Several limitations should be considered. First, despite the large sample size at the 6-month timepoint, the sample at the 30-month timepoint was limited. Additionally, all analyses were based on brief natural language samples (the average length was 28 words) that may not adequately capture the full extent of caregiver's experiences of connection as compared to longer language samples and language that occurs in conversation between caregivers and PLWD. Future research should (a) examine relationships between language, dementia progression, and caregiver health and well-being longitudinally; (b) integrate language samples from multiple sources (interview questions, conversations, etc.); and (c) study the possibility that reduced use of we-pronouns may be protective for the caregiver.
Statement of Ethics
The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The study protocol was reviewed and approved by the institutional review boards of the UCSF (IRB #: 14-14537) and the UNMC (IRB #: 483-14-FB). Patients with capacity to provide informed consent were given the opportunity to consent for themselves; otherwise, consent was obtained from a legally authorized representative. Caregivers also provided informed consent. Consent was provided with written or electronic (digital) signature.
Conflict of Interest Statement
Dr. K.L. Possin reported receiving grants from the Centers for Medicare & Medicaid Services (CMS), National Institute on Aging (NIA), National Institute of Neurological Disorders and Stroke (NINDS), Global Brain Health Institute, Quest Diagnostics, and the Rainwater Foundation during the conduct of the study and personal fees from ClearView Healthcare Partners and Vanguard outside the submitted work.
Funding Sources
This Care Ecosystem study was funded by the Department of Health and Human Services, CMS (1C1CMS331346), Global Brain Health Institute, NIA (5R01AG056715), and National Institute on Neurological Disorders and Stroke (UH3NS105557). Preparation of this manuscript was supported by a National Institute of Health Mentored Research Scientist Career Development Award (1K01AG059840-01A1) awarded to Alissa Bernstein Sideman and a National Institute of Health National Research Service Award (1F31AG072891-01) awarded to Jenna L. Wells.
Author Contributions
Concept and design: A. Bernstein Sideman, J.L. Wells, J. Merrilees, S.M. Shdo, C.I. Yee, K.L. Possin, and R.W. Levenson; acquisition, analysis, or interpretation of data: A. Bernstein Sideman, J.L. Wells, J. Merrilees, S.M. Shdo, C.I. Yee, K.L. Possin, and R.W. Levenson; drafting of the manuscript: A. Bernstein Sideman; critical revision of the manuscript for important intellectual content: A. Bernstein Sideman, J.L. Wells, J. Merrilees, S.M. Shdo, C.I. Yee, K.L. Possin, and R.W. Levenson; statistical analysis: J.L. Wells; obtained funding: K.L. Possin; administrative, technical, or material support: A. Bernstein Sideman, J.L. Wells, J. Merrilees, S.M. Shdo, C.I. Yee, K.L. Possin, and R.W. Levenson; and supervision: K.L. Possin and R.W. Levenson.
Data Availability Statement
Public archiving of the anonymized data is not permitted under the study's IRB approval. Specific requests can be submitted through the UCSF MAC Resource Request form: http://memory.ucsf.edu/resources/data. Following a UCSF-regulated procedure, access will be granted to designated individuals in line with ethical guidelines on the reuse of sensitive data. This would require submission of a Material Transfer Agreement, available at: https://icd.ucsf.edu/material-transfer-and-data-agreements. Commercial use will not be approved.
References
- 1.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176((3)):372–9. doi: 10.1001/jamainternmed.2015.7664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11((2)):217–28. doi: 10.31887/DCNS.2009.11.2/hbrodaty. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schulz R, Beach SR, Czaja SJ, Martire LM, Monin JK. Family caregiving for older adults. Annu Rev Psychol. 2020;71:635–59. doi: 10.1146/annurev-psych-010419-050754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.2021 Alzheimer's disease facts and figures. Alzheimers Dement. 2021;17((3)):327–406. doi: 10.1002/alz.12328. [DOI] [PubMed] [Google Scholar]
- 5.Fauth E, Hess K, Piercy K, Norton M, Corcoran C, Rabins P, et al. Caregivers' relationship closeness with the person with dementia predicts both positive and negative outcomes for caregivers' physical health and psychological well-being. Aging Ment Health. 2012;16((6)):699–711. doi: 10.1080/13607863.2012.678482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duggleby W, Williams A, Wright K, Bollinger S. Renewing everyday hope: the hope experience of family caregivers of persons with dementia. Issues Ment Health Nurs. 2009;30((8)):514–21. doi: 10.1080/01612840802641727. [DOI] [PubMed] [Google Scholar]
- 7.Keller HH, Schindel Martin L, Dupuis S, Genoe R, Gayle Edward H, Cassolato C. Mealtimes and being connected in the community-based dementia context. Dementia. 2010;9((2)):191–213. [Google Scholar]
- 8.Pennebaker JW, Mehl MR, Niederhoffer KG. Psychological aspects of natural language use: our words, our selves. Annu Rev Psychol. 2003;54((1)):547–77. doi: 10.1146/annurev.psych.54.101601.145041. [DOI] [PubMed] [Google Scholar]
- 9.Seider BH, Hirschberger G, Nelson KL, Levenson RW. We can work it out: age differences in relational pronouns, physiology, and behavior in marital conflict. Psychol Aging. 2009;24((3)):604–13. doi: 10.1037/a0016950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alea N, Singer JA, Labunko B. “We-ness” in relationship-defining memories and marital satisfaction. In: Skerrett K, Fergus K, editors. Couple resilience. Springer; 2015. pp. p. 163–77. [Google Scholar]
- 11.Williams-Baucom KJ, Atkins DC, Sevier M, Eldridge KA, Christensen A. “You” and “I” need to talk about “us”: linguistic patterns in marital interactions. Pers Relatsh. 2010;17((1)):41–56. [Google Scholar]
- 12.Ascher EA, Sturm VE, Seider BH, Holley SR, Miller BL, Levenson RW. Relationship satisfaction and emotional language in frontotemporal dementia and Alzheimer disease patients and spousal caregivers. Alzheimer Dis Assoc Disord. 2010;24((1)):49–55. doi: 10.1097/WAD.0b013e3181bd66a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connelly DE, Verstaen A, Brown CL, Lwi SJ, Levenson RW. Pronoun use during patient-caregiver interactions: associations with caregiver well-being. Dement Geriatr Cogn Disord. 2020;49:202–9. doi: 10.1159/000508095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haase CM, Saslow LR, Bloch L, Saturn SR, Casey JJ, Seider BH, et al. The 5-HTTLPR polymorphism in the serotonin transporter gene moderates the association between emotional behavior and changes in marital satisfaction over time. Emotion. 2013;13((6)):1068–79. doi: 10.1037/a0033761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monin JK, Levy B, Doyle M, Schulz R, Kershaw T. The impact of both spousal caregivers' and care recipients' health on relationship satisfaction in the Caregiver Health Effects Study. J Health Psychol. 2019;24((12)):1744–55. doi: 10.1177/1359105317699682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fitzpatrick KE, Vacha-Haase T. Marital satisfaction and resilience in caregivers of spouses with dementia. Clin Gerontol. 2010;33((3)):165–80. [Google Scholar]
- 17.Possin KL, Merrilees JJ, Dulaney S, Bonasera SJ, Chiong W, Lee K, et al. Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: the care ecosystem randomized clinical trial. JAMA Intern Med. 2019;179((12)):1658–67. doi: 10.1001/jamainternmed.2019.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levenson RW. Oedipus text. Berkeley, CA: University of California, Berkeley; 1992. [Google Scholar]
- 19.Galvin JE. The quick dementia rating system (QDRS): a rapid dementia staging tool. Alzheimers Dement. 2015;1((2)):249–59. doi: 10.1016/j.dadm.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosom Med. 2002;64((3)):510–9. doi: 10.1097/00006842-200205000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. The zarit burden interview: a new short version and screening version. Gerontologist. 2001;41((5)):652–7. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16((9)):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee M, Kolomer SR. Caregiver burden, dementia, and elder abuse in South Korea. J Elder Abuse Negl. 2005;17((1)):61–74. doi: 10.1300/J084v17n01_04. [DOI] [PubMed] [Google Scholar]
- 24.Bozeat S, Gregory CA, Ralph MA, Hodges JR. Which neuropsychiatric and behavioural features distinguish frontal and temporal variants of frontotemporal dementia from Alzheimer's disease? J Neurol Neurosurg Psychiatry. 2000;69((2)):178–86. doi: 10.1136/jnnp.69.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hua AY, Wells JL, Brown CL, Levenson RW. Emotional and cognitive empathy in caregivers of people with neurodegenerative disease: relationships with caregiver mental health. Clin Psychol Sci. 2021;9((3)):449–66. doi: 10.1177/2167702620974368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alsawy S, Tai S, McEvoy P, Mansell W. “It's nice to think somebody's listening to me instead of saying ‘oh shut up.'” People with dementia reflect on what makes communication good and meaningful. J Psychiatr Ment Health Nurs. 2020;27((2)):151–61. doi: 10.1111/jpm.12559. [DOI] [PubMed] [Google Scholar]
- 27.Norton MC, Piercy KW, Rabins PV, Green RC, Breitner JC, Østbye T, et al. Caregiver-recipient closeness and symptom progression in alzheimer disease. The Cache county dementia progression study. J Gerontol B Psychol Sci Soc Sci. 2009;64((5)):560–8. doi: 10.1093/geronb/gbp052. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Public archiving of the anonymized data is not permitted under the study's IRB approval. Specific requests can be submitted through the UCSF MAC Resource Request form: http://memory.ucsf.edu/resources/data. Following a UCSF-regulated procedure, access will be granted to designated individuals in line with ethical guidelines on the reuse of sensitive data. This would require submission of a Material Transfer Agreement, available at: https://icd.ucsf.edu/material-transfer-and-data-agreements. Commercial use will not be approved.