Abstract
The development of a high-end cannabinoid-based therapy is the result of intense translational research, aiming to convert recent discoveries in the laboratory into better treatments for patients. Novel compounds and new regimes for drug treatment are emerging. Given that previously unreported signaling mechanisms for cannabinoids have been uncovered, clinical studies detailing their high therapeutic potential are mandatory. The advent of novel genomic, optogenetic, and viral tracing and imaging techniques will help to further detail therapeutically relevant functional and structural features. An evolutionarily highly conserved group of neuromodulatory lipids, their receptors, and anabolic and catabolic enzymes are involved in a remarkable variety of physiological and pathological processes and has been termed the endocannabinoid system (ECS). A large body of data has emerged in recent years, pointing to a crucial role of this system in the regulation of the behavioral domains of acquired fear, anxiety, and stress-coping. Besides neurons, also glia cells and components of the immune system can differentially fine-tune patterns of neuronal activity. Dysregulation of ECS signaling can lead to a lowering of stress resilience and increased incidence of psychiatric disorders. Chronic pain may be understood as a disease process evoked by fear-conditioned nociceptive input and appears as the dark side of neuronal plasticity. By taking a toll on every part of your life, this abnormal persistent memory of an aversive state can be more damaging than its initial experience. All strategies for the treatment of chronic pain conditions must consider stress-related comorbid conditions since cognitive factors such as beliefs, expectations, and prior experience (memory of pain) are key modulators of the perception of pain. The anxiolytic and anti-stress effects of medical cannabinoids can substantially modulate the efficacy and tolerability of therapeutic interventions and will help to pave the way to a successful multimodal therapy. Why some individuals are more susceptible to the effects of stress remains to be uncovered. The development of personalized prevention or treatment strategies for anxiety and depression related to chronic pain must also consider gender differences. An emotional basis of chronic pain opens a new horizon of opportunities for developing treatment strategies beyond the repeated sole use of acutely acting analgesics. A phase I trial to determine the pharmacokinetics, psychotropic effects, and safety profile of a novel nanoparticle-based cannabinoid spray for oromucosal delivery highlights a remarkable innovation in galenic technology and urges clinical studies further detailing the huge therapeutic potential of medical cannabis (Lorenzl et al.; this issue).
Keywords: Endocannabinoid system, Chronic pain, Novel galenic
Phytocannabinoids
Cannabis triggers a complex set of experiences in humans including euphoria, heightened sensitivity to external experience, and relaxation [1]. The pharmacological effects of medical cannabis presently used are mainly due to two ingredients of the chemotype- and variety-rich cannabis plant Cannabis sativa [2], the psychoactive phytocannabinoid (−)-∆9-tetrahydrocannabinol (THC) and the primary noneuphorizing and nonaddictive compound cannabidiol (CBD). The different content of THC and CBD and their ratio to each other may offer opportunities for a more individualized treatment (entourage effect, see below). Today, cannabis plant strains are available with more than 20% THC but also variants with content less than 1% THC and up to 20% CBD. Besides THC and CBD, cannabis flowers contain more than 170 different cannabinoids, with dozens of pharmacologically active molecules, such as cannabichromene, cannabigerol, tetrahydrocannabivarin, cannabidivarin, and cannabinol [3, 4]. The proportion of each phytocannabinoid is influenced by various factors such as growing conditions and extraction methods. In addition, the cannabis plant contains more than 200 terpenes and terpenoids with different pharmacological properties and alleged therapeutic potential [5]. Members of this highly heterogeneous group of substances and a plethora of various other noncannabinoids such as flavonoids, steroids, and alkaloids are contained in a formulated full-spectrum cannabis extract and may act in concert [6] (see below). The investigations on the endocannabinoid system (ECS) (see below) enable us to start to understand also the mechanisms of actions of phytocannabinoids. For example, exogenous cannabinoids influence behavior in a biphasic manner, with low and high doses exerting anxiolytic and anxiogenic states, respectively, in both animals and humans [7, 8, 9]. Preclinical data suggest that the anxiolytic effect of cannabinoids at low doses depends on the presence of cannabinoid receptors on cortical glutamatergic neurons, whereas the anxiogenic effect of higher doses is mediated by cannabinoid receptors on forebrain GABAergic neurons. Such a bimodal control via cannabinoid receptors on excitatory glutamatergic and inhibitory GABAergic neurons correlates well with the behavioral alterations observed.
Cannabinoid Receptors
Cannabinoids bind reversibly and stereo-selectively to the canonical cannabinoid receptor type 1 and type 2 receptors (CB1R and CB2R; see refs. in: [10, 11, 12, 13, 14, 15, 16, 17]. There is evidence that also other non-CB1R and non-CB2R (GPR18, GPR119, and GPR55) are involved in the signaling of the ECS [18]. Certain plant natural products, from both cannabis and other plants, target other proteins of the ECS, such as hydrolytic enzymes that control endocannabinoid (eCB) levels [19]. CB1R and CB2R are highly versatile and adaptable containing seven transmembrane spanning domains, which can form homo- and heterodimers with various receptors, thereby altering signaling and trafficking in membranes and in intracellular compartments. Despite their ubiquitous occurrence and cellular plasticity, particularly CB1R acts in a highly specific manner as integrators of synaptic signaling in many neurotransmitter and lipid signaling systems. Their expression levels and location vary greatly depending on the brain region and cell type (see details in [17]. The CB1R appears to be the most highly expressed receptor in the brain. Deleting CB1R specifically in nociceptive neurons localized in the peripheral nervous system of mice reduces the analgesia produced by local and systemic but not intrathecal delivery of cannabinoids, suggesting a substantial contribution of CB1R expressed on the peripheral terminals of nociceptors to cannabinoid-induced analgesia [20].
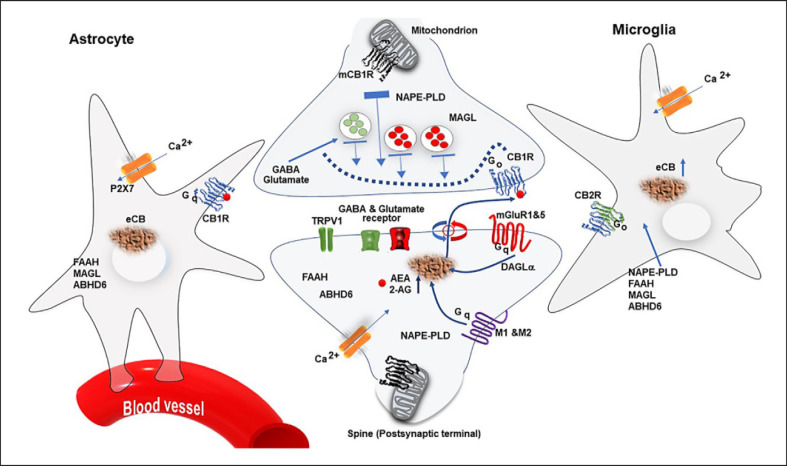
CB1R is also present at very low levels in astrocytes, a major class of glia cells, which tightly interacts with neurons through specific signaling molecules and takes up glucose from the bloodstream to provide energy to the brain (see Fig. 1). There is evidence that astrocytes can directly regulate glucose metabolism and impair behavioral responses in social interaction tests. CB1R is present in the outer mitochondrial membrane (mitochondrial CB1R; mtCB1R). Stimulation of the mtCB1R leads to inhibition of mitochondrial oxidative phosphorylation and ATP production and modulates neurotransmitter release through mechanisms still unknown [21]. The role of mtCB1R in anxiety-, fear-, and stress-related circuits is not known yet, but neuronal redox stress is eventually involved in the fine-tuning of neuronal activity, making bioenergetic processes primary acute regulators of learning, memory formation, and cognitive functions [21, 22]. It was reported that acute cannabinoid intoxication induces amnesia in humans and animals, with causal involvement of CB1R expressed by astrocytes [15].
Fig. 1.
“Tripartite cannabinergic synapse.” The concept of a ‘tripartite cannabinergic synapse” includes neuronal, glial, and vascular elements (for details see text). NAPE-PLD, N-acyl-phosphatidylethanolamine phospholipase D; ABHD6, α-β-hydrolase domain protein 6; DAGL, diacylglycerol lipase.
CB2R is expressed in both neurons and glial cells in the brain under physiological and pathological conditions [23]. CB2R transcripts are less abundant than CB1R mRNA but are strongly upregulated in response to various insults, such as chronic pain and neuroinflammation. CB2R expressed in the immune system is involved in immune-modulating effects on T cells, B cells, monocytes, and microglia cells. CB2R is particularly expressed in activated microglia. CB2R agonists are potential analgesics void of psychotropic effects. Peripheral immune cells, neurons, and glia express CB2R. However, their involvement in neuropathic pain remains unresolved. A recent study identified a simultaneous activity of neuronal and lymphoid CB2R that protects against spontaneous and evoked neuropathic pain [24]. CB2R expressed in the immune system is involved in an overall reduction in pro-inflammatory cytokine expression and an increase in anti-inflammatory cytokines [25]. Functional CB2R are not exclusively expressed in the immune system but also in neurons, suggesting a more widespread expression and functional relevance in the CNS. For instance, action potential-driven eCB release leads to a long-lasting membrane potential hyperpolarization in CA3 and CA2 hippocampal principal cells. Modulating the activity of a sodium-bicarbonate cotransporter alters the input/output function of CA3 hippocampal principal neurons and gamma oscillations in vivo [26]. Noteworthy, eCB diffusion by volume transmission [27] in the extracellular space can alter glial functioning and modulate neurotransmitter release, e.g., at synaptic terminals of neighboring neurons [28, 29].
The ECS
The neuromodulatory lipids, their receptors, and anabolic and catabolic enzymes of eCBs play a crucial role in the regulation of a great variety of physiological and pathological processes including chronic pain [17, 30] (Fig. 1). In the brain, anandamide (AEA) and 2-arachidonoyl glycerol (2-AG) are the main eCBs produced from cell membrane lipid membrane precursors. The synthesis machinery for AEA seems to be mainly located presynaptically, whereas the degrading machinery is at the postsynaptic site. The neuronal CB1R is predominantly expressed at the presynapse; however, functional postsynaptic CB1R and CB2R have also been reported.
On depolarization of the postsynaptic terminal, e.g., by activation of glutamate receptors (N-methyl-D-aspartate [NMDAR] or metabotropic glutamate receptors mGluR1 and mGluR5) or muscarinic receptor type 1 and 2 in response to increased cytoplasmic calcium, 2-AG and possibly AEA are synthesized “on demand” from lipid precursors by the AEA synthesizing enzyme N-acyl-phosphatidylethanolamine phospholipase D, which is predominantly expressed in the presynaptic terminal, although it might also be present postsynaptically and the 2-AG synthesizing enzyme diacylglycerol lipase in dendritic spines of excitatory synapses [17, 31]; see Fig. 1). Transporter systems release 2-AG and possibly AEA, which then travel to the presynaptically located CB1R to inhibit neurotransmitter release, thus acting as an “on demand” negative-feedback mechanism to tune-down synaptic transmission, especially when the postsynaptic terminal is strongly activated. This signaling can typically lead to processes called depolarization-induced suppression of excitation at the glutamatergic synapse and depolarization-induced suppression of inhibition at the GABAergic synapse. Depolarization-induced suppression of excitation and depolarization-induced suppression of inhibition appear to be mediated exclusively by 2-AG. CB1R is typically located presynaptically and coupled to Go proteins. The concept of “on-demand” ECS synthesis represents an attractive construct for understanding the roles of the ECS in neuronal-network modulation and behaviors. ECS signaling appears as a local activity-driven process, which is mostly silent when the neuronal activity is low at this site. However, there are convincing data that AEA is also involved in tonic suppression of neurotransmitter release [32]. This mechanism is very well detailed for glutamatergic and GABAergic synapses. AEA and 2-AG can also activate other receptors, such as TRPV1 and GABAA receptors, respectively [33, 34, 35].
THC treatment evokes long-lasting internalization of presynaptic cannabinoid receptors located within somadendritic endosomes [36]. eCB synthesis in microglia and astrocytes can be stimulated by the activation of P2X purinoreceptor 7 by ATP. ECS signaling is terminated by cellular uptake processes, which likely involve transporter proteins. The cellular uptake is followed by intracellular hydrolysis of 2-AG by presynaptic monoacylglycerol lipase (MAGL), a serine hydrolase. AEA is catabolized by postsynaptic fatty-acid amide hydrolase (FAAH). In the CNS, these components are expressed in neurons, microglia, astrocytes, and oligodendrocytes (see Fig. 1). The synthesis and degradation machinery of AEA and 2-AG have different cellular and subcellular distributions. Noteworthy, AEA binds to ligand-activated transcription factors such as peroxisome proliferator-activated receptor gamma, which regulates genes responsible for fatty-acid and energy metabolism, orphan G-protein-coupled receptors, such as non-CB1R/non-CB2R (GPR18, GPR119, and GPR55), and cytosolic domains of postsynaptically localized TRPV1 channels (transient receptor potential vanilloid type-1; see below), thereby promoting activation. The major 2-AG-degrading enzyme MAGL is located at the presynaptic terminal and in astrocytes, whereas another 2-AG-degrading enzyme α-β-hydrolase domain protein 6 can limit the 2-AG availability at the site of production. Astrocytic MAGL seems to enable astrocyte-neuron transcellular shuttling and metabolism of 2-AG and arachidonic acid. The AEA-degrading enzyme FAAH is present at the postsynaptic terminal. Thus, AEA may act in both an autocrine and a retrograde manner. CB2R and possibly CB1R are also present on microglial cells and are involved in immune reactions. Furthermore, although presynaptic CB1R is coupled to Go, CB1R on astrocytes is Gq-coupled, and agonist stimulation leads to an increase in intracellular Ca2+ concentration, possibly associated with a concomitant release of glutamate, GABA, ATP, and D-serine, the physiological coagonist of NMDA receptors involved in synaptic plasticity [37]. The roles of these molecules released from glial structures in synaptic transmission are still rather scant (for details see [17]). Elevation of D-serine levels fully rescued long-term potentiation (LTP) and memory impairments in mice. These data reveal a novel mechanism of in vivo astroglial control of memory and synaptic plasticity via the D-serine-dependent control of NMDARs [37]. There is substantial evidence from animal studies that the ECS modulates the physiological processes underlying aging. The activity of the ECS declines during aging, as CB1R expression and coupling to G-proteins are reduced in the brain tissues of older mice, and the levels of the major eCB 2-AG are decreasing with age. A chronic low dose of THC restored cognitive function in old mice and reversed the age-related decline. This effect was accompanied by increased hippocampal spine density [38].
Many diseases including neuropathic pain and inflammation involve TRP channel dysfunction. AEA can activate the postsynaptic nonselective cation channel TRPV1, leading to an increase in postsynaptic current. 2-AG can in addition stimulate postsynaptic GABAA receptors. Note, despite that they have AEA as a common ligand, the involvement of CB1R and TRPV1 in anxiety is opposite, comprising an intriguing antagonistic regulatory mode between both signaling systems [39].
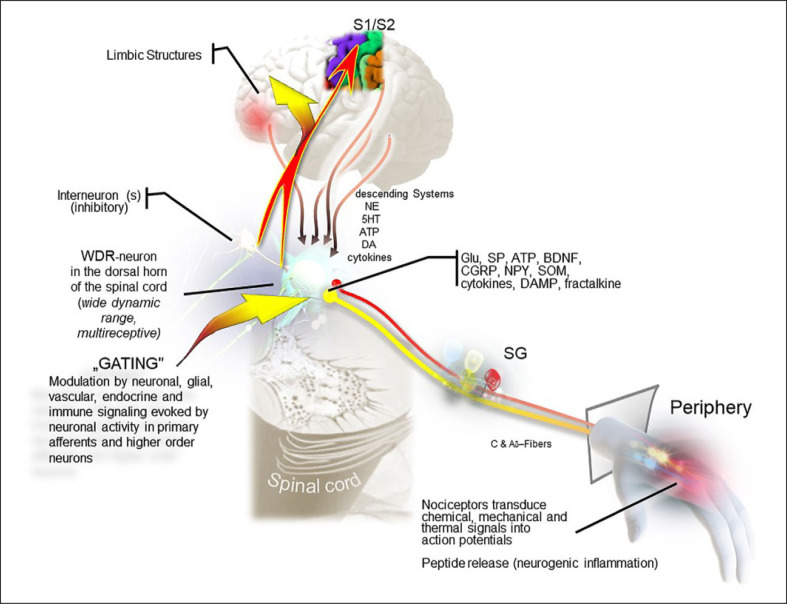
To date, six TRP channels from three subfamilies have been reported to mediate cannabinoid activity (TRPV1–V4, TRPA1, and TRPM8) [40]. THC acts most potently at TRPV2. TRP channels, including several splice variants, can be activated by noxious heat, some endogenous lipid-derived molecules, acidic solutions, and some pungent chemicals and a variety of molecules [41]. Inflammatory mediators in damaged tissues sensitize these ion channels expressed on sensory neurons, triggering an influx of cations to chemical and physical stimuli [42]. This nonselective, outwardly rectifying ion channel functions as a molecular integrator for multiple types of sensory inputs and functions as an important transducer of painful and itch-related stimuli (Fig. 2).
Fig. 2.
Pain pathophysiology (see text). WDR, wide-dynamic range; BDNF, brain-derived neurotrophic factor; CGRP, calcitonin gene-related peptide; NPY, neuropeptide Y; SOM, somatostatin; DAMP, damage-associated-molecular-pattern.
TRPV1 interact physically with the sigma 1 receptor (σ1R). The σ1R is a transmembrane protein, expressed in many different tissue types [43]. The σ1R acts as a chaperone protein at the endoplasmic reticulum that modulates calcium signaling through the inositol 1, 4, 5-trisphosphate receptor. It binds the neurosteroid progesterone and downregulates TRPV1R expression in the plasma membrane of sensory neurons and appears closely associated to the reduction of nociception by elevated progesterone levels [44]. Synthetic compounds, amines, as well as neuroactive steroids, such as dehydroepiandrosterone and pregnenolone [45] activate the receptor and modulate the functionality of different receptors and ion channels (e.g., NMDAR). Other molecules that induce eCB synthesis have also been identified, including corticosteroids and estradiol [46, 47, 48], leading to the hypothesis that ECS signaling is the effector by which these hormones alter synaptic activity.
CBD, a Multi-Target Ligand
CBD, a main ingredient of C. sativa [2], was found to exert beneficial effects in chronic pain, fear, anxiety and stress-coping, epilepsy, cardiovascular disease, inflammation, and autoimmunity to neurodegenerative and kidney diseases. Numerous studies showed that CBD has a therapeutic potential in patients with psychosis [49, 50, 51, 52]. CBD is a multi-target ligand with a poor affinity for CB1R and CB2R and behaves as a modulator of eCB levels [53]. For example, CBD enhances neurogenesis, possibly by increasing AEA levels [54], suggesting mechanisms via an indirect stimulation of the ECS. CBD reduces the negative effects of NMDAR overactivity (see below, entourage effect). Molecular findings support a role for σ1R antagonists in inhibiting augmented excitability, secondary to sustained afferent input [55]. In animal studies, CBD enhanced morphine antinociception, diminished NMDA mediated seizures, and reduced stroke damage via the σ1R [56]. In an in vitro assay, CBD disrupted the regulatory association of σ1R with the NR1 subunit of the NMDAR, an effect shared by σ1R antagonists such as progesterone and prevented by σ1R agonists. σ1R antagonists exert an antinociceptive effect on pain of different etiology, and σ1R knockout mice display reduced pain sensitivity [55].
ECS and Stress
Preclinical data strongly support the hypothesis that ECS signaling is altered by chronic stress. Stress can be defined as a reaction of the body to an internal or external challenge to prepare its response to possible dangers or injuries. Stress has been identified as a major causal factor for several mental disorders [57]. Exposure to nonhabituating chronic stress downregulates CB1R signaling in many brain regions involved in emotional processing. The ECS facilitates the activation of resilience factors during and/or after stress exposure [58, 59]. Chronic stress-induced alterations of the ECS ensue changes in activation and feedback regulation of the hypothalamic-pituitary-adrenal axis [60]. Chronic pain triggers chronic stress responses including dendritic regression and loss of dendritic spines in brain neurons that are accompanied by deficits in synaptic plasticity and memory and may predispose patients to impaired cognition [61, 62]. Dendritic spines are the target structure of most excitatory synapses in the brain and are functionally and structurally highly dynamic. The formation of new synapses and new dendritic processes occurs continuously. Decreased dendritic branches and spine numbers are associated with reduced LTP and short-term spatial memory and increased depression-like behavior. However, our knowledge about the chain of molecular and cellular events translating stress experience into altered behavior is still rather scant, and the presently available evidence from preclinical in vitro, ex vivo, and in vivo studies is consistent but still correlative in nature [36, 63].
The molecular composition of the CB1R complex beyond the classical G-protein signaling components is not known. CB1R assembles with multiple members of the WAVE1 complex and the RhoGTPase Rac1, which orchestrates a variety of events related to actin cytoskeleton rearrangement in postsynaptic spine morphology and density. Abnormal dendritic spine remodeling following disease or injury may be involved in maintaining, e.g., chronic pain states sensitive to cannabinoids [64]. The WAVE regulatory complex is a multi-subunit complex that controls actin cytoskeletal dynamics related to stress. Activation levels of CB1R directly impact on actin polymerization and stability via WAVE1 in growth cones of developing neurons, as well as in synaptic spines of mature neurons. In adult mice, CB1R agonists attenuate activity-dependent remodeling of dendritic spines in spinal cord neurons in vivo and reduce inflammatory pain by regulating the WAVE1 complex. This study reports novel signaling mechanisms for cannabinergic modulation of the nervous system and reveals a previously unreported putative role for the WAVE1 complex in therapeutic applications of cannabinoids [64].
A murine ortholog of the putative tumor suppressor gene DRR1 is a unique stress-induced protein in brain that binds to actin, promotes bundling and stabilization of actin filaments, and impacts on actin-dependent neurite outgrowth [65]. By way of a promotion of F-actin clusters, it participates in the regulation of NMDA receptor signaling and expression and signaling of ionotropic AMPA and metabotropic glutamate receptor-mediated synaptic transmission and plasticity.
Besides the WAVE1 complex, also Shank proteins play a role in synapse formation and dendritic spine maturation. Members of the SHANK gene family code for multidomain scaffold proteins of the postsynaptic density that connect neurotransmitter receptors, ion channels, and other membrane proteins to the actin cytoskeleton and G-protein-coupled signaling pathways. SHANK3 deficiency impairs heat hyperalgesia and TRPV1 signaling in primary sensory neurons [66].
Pain Pathophysiology
The physiology of nociception and pathophysiology of chronic pain include peripheral and central structural and functional neuronal alterations as well as neuro-immune interactions, which become more prominent during inflammatory reactions [67]. Research over the past decades has increasingly detailed the brain's capacity for reorganization of structural and functional neural network architecture to adapt to environmental needs. It is a key goal in the field of pain research to understand mechanisms involved in the transition between nociception (acute pain) and chronic pain (see below). Most importantly, chronic pain is not the same as acute nociception that lasts longer. Chronic pain is a stress-induced disease process associated with anxiety and depression. Human brain imaging studies indicate that cortical and subcortical fear conditioning pathways may be fundamental to chronic pain. There is evidence that brain structures involved in social pain and physical pain are shared [68]. A core set of brain networks is commonly disturbed with chronic pain. No clinically applicable biomarkers are available to predict chronification of pain. The development of chronic pain is a dynamic process that involves continuous interactions among complex ascending and descending systems on all levels of the neuraxis [69]. Descending systems orchestrate spinal cord activity [70], and nociception produces lasting effects in the sensory and the reward circuitry of the brain [71]. Fear conditioning evoked by nociceptive input induces memory traces, which can recover spontaneously or after a reexposure to the aversive stimulus. The physiological and emotional state of the organism at the moment of this perception determines the intensity of the autonomic, hormonal, and behavioral outputs [72]. Note, the brain has no simple “erase” function, and often, decades-old personal experiences can be recalled or come unbidden into everyday consciousness. These recalls may ensue deleterious physical and psychological consequences. Anticipatory anxiety rises when the stress which goes along with these recalls chronically exceeds the normal range and becomes disproportionate to the actual level of threat [73, 74]. Anxiety is an innate behavioral state associated with the anticipation of potential future threats that allows an organism to avoid potentially dangerous or harmful situations. Anxiety behaviors such as avoidance, decreased motion, increased heart rate, and hypervigilance occurring within the normal range of intensity are important for survival [75, 76].
Various neuropeptides such as substance P and calcitonin gene-related peptide were released from nerve endings in the periphery (neurogenic inflammation). They act directly on vascular endothelial and smooth-muscle cells in the skin, muscle, and joints. Release also includes adrenomedullin, neurokinins A and B, vasoactive intestinal peptide, neuropeptide Y, gastrin-releasing peptide as well as glutamate, nitric oxide, and cytokines. Activity-dependent gene expression in the spinal ganglion is evoked by primary afferent signaling via C-fibers and Aδ-fibers. Glu, SP, ATP, brain-derived neurotrophic factor, calcitonin gene-related peptide, neuropeptide Y, somatostatin, cytokines, damage-associated-molecular-pattern, and fractalkine (member of the CX3C chemokine family) are released in the dorsal horn and activate the innate immune system and promote pathological neurogenic neuroinflammatory responses [77].
Persistent nociceptive input increases neuronal excitability (LTP) and induces a program of gene expression in projection neurons and interneurons in the dorsal spinal cord. Glia can be directly activated by afferent stimulation. Peripheral immune cells entering the CNS after injury or in disease may directly affect microglia, astrocyte, and oligodendrocyte function in integrated networks (gating). Projection neurons within Rexed's laminae I and V constitute the major output from the dorsal horn of the spinal cord to the brain. Inflammation enhances the excitability of, e.g., neurons in lamina 1, and reveals their subliminal synaptic input. When these neurons increase their discharge activity, they display response patterns resembling multireceptive wide-dynamic range-type neurons located in lamina 5 of the dorsal horn of the spinal cord. Peripheral nerve injury increases expression of the purinergic receptor P2X4 located on microglia in the spinal cord [78]. Activation of P2X4 receptors results in the release of brain-derived neurotrophic factor, which blocks a chloride transporter (KCC2) in projection neurons in lamina 1 of the spinal dorsal horn. The resulting increase of intracellular chloride reduces or even reverses the inhibitory action of GABAA receptor activation into excitation. GABA released from segmental interneurons might lose its inhibitory control function (disinhibition) or even synergistically excite their target neurons together with, e.g., NMDAR-mediated excitation [79]. The parabrachial nucleus is a major target of ascending neurons from laminae 1 and 5 which bypass the thalamus and innervate targets in limbic structures (Fig. 2). This synaptic input has a potent impact on the strengthening of the nociception-emotion link in persistent pain [80].
Chronic pain is characterized by the abnormal persistent memory (memory of pain) of an aversive state [71, 81]. Recent studies suggest that stable connections of neurons are a support for memories to be generated, whereas flexible connections on the other hand were found to be responsible for learning [82]. There is evidence that these fear memories may be actively protected from erasure by the generation of perineuronal nets (PNNs) in limbic structures which integrate cognitive und emotional signals such as the hippocampus, the anterior cingulate and insular cortex, the amygdala, as well as the nucleus accumbens and the nucleus caudatus [83]. The PNN is a specialized extracellular matrix that envelops mature neurons. PNNs are composed by various link proteins. After the so-called critical period has passed, PNNs are quickly produced, stabilizing the whole neural network, making it difficult for neurons to make new connections.
Repeated noxious stimuli engage central circuits operated by the ECS. These emotion-related limbic circuits play an important role in higher cognitive processes, in the regulation of stress-induced activity, and in the regulation of hypothalamic-pituitary-adrenal activity as well as adult neuroneogenesis (see [31, 84]. In general, assemblies of neurons have a high propensity to engage in oscillatory activity and to form dynamic densely interconnected functional networks [85]. In vitro experiments neural circuits, distributed across several brain areas, can be optically interrogated and controlled with millisecond precision and single-cell resolution. Optogenetically driven oscillations in the hippocampus are impaired by the stress hormone corticotropin-releasing factor [86]. The persistence of excessive fear and anxiety is also a characteristic of disorders such as post-traumatic stress disorder and phobias. The therapeutic benefits of cannabinoids have also raised interest in understanding the molecular mechanisms that underlie the beneficial effects of exposure therapy in phobic disorders [87]. Adding CBD to exposure therapy is expected to strengthen effects of this treatment [88].
Modification of a Dysfunctional Cognition by Cannabinoids
The modification of a dysfunctional cognition by cannabinoids is a novel approach in the therapy of chronic pain states [71, 89]. Long-term memory formation and storage are complex and dynamic processes. Repeated exposure to a feared stimulus in the absence of the previously aversive event leads to a gradual reduction in the fear response (extinction by formation of new memories following a prediction error) (see below). The activation of CB1R specifically located on GABAergic interneurons inhibits long-term depression in the lateral amygdala. These observations indicate that AEA decreases the activity of inhibitory interneurons in the amygdala. This disinhibition increases the activity of common output neurons and could provide a prerequisite for “extinction” by formation of new memories [13, 14].
Therapeutic Targeting
The emotional basis of chronic pain opens up a new horizon of opportunities for developing new treatment strategies since cognitive factors such as beliefs, expectations, and prior experience are key modulators of the perception of pain and can substantially modulate the efficacy and tolerability of therapeutic interventions. All strategies for the treatment of chronic pain conditions must consider stress-related comorbid conditions, such as the altered hedonic state, disordered cognition, and aberrant behaviors with negatively balanced affective states such as fear, anxiety, and depression. A synopsis of clinical findings suggests a negative correlation between ECS activity and anxiety. Enhancement of AEA and 2-AG by FAAH and MAGL blockade, respectively, attenuates anxiety in rodents [90]. Increasing eCB levels locally “on demand” by inhibiting their degrading enzymes could be more selective and avoid unacceptable side effects of CB1R agonists. However, as these indirect agonists have not yet been approved for use in humans, the option of direct CB1R stimulation has yet to be explored. CB1R stimulation with THC enhances fear extinction in humans, which warrants further investigation in post-traumatic stress disorders and chronic pain. Strategies have been proposed to minimize cannabinoid side effects. Blockade of the mammalian target of rapamycin pathway prevents THC-induced cognitive impairment in mice, without modifying its anxiolytic effects [91]. The anxiolytic effect of AEA depends on CB1R and is associated with cognitive impairment, whereas the anxiolytic effect of 2-AG seems to be CB2R-dependent and not associated with cognitive disruption. COX2 inhibition increases eCB levels in the brain, reduces anxiety in rodents, and blocks THC-induced cognitive impairment [92]. Positive allosteric modulators regulating orthosteric ligand activity can open new perspectives for reducing side effects [93]. These novel modulators bind to distinct sites of the CB1 receptor and control their binding to different G-proteins- or β-arrestin-controlled processes. The inhibition of eCB membrane transporters represents another promising pharmacological target.
Human studies and multiple animal pain models support the view that therapeutic interventions with cannabinoids should intercept with chronification processes already at an early stage. The anxiolytic and anti-stress effects of cannabinoids will provide a gateway to a successful multimodal therapy. An experience-based adaptation of expectancies is responsible for the progress of anticipatory anxiety, i.e., a person experiences increased levels of anxiety by thinking about an event or situation in the future [75, 76, 94]. This maladaptive process is best countered by overlaying it with positive new associations to regain the ability to derive pleasure from ordinary activities. Effective recognition and treatment of anxiety and depression [95, 96] may create new links in neuronal circuits and could help to establish context-specific safety signals in chronic pain patients (retraining the brain). Medical cannabis should be used preferentially as an adjunct treatment (add-on), starting out with low doses which are incremented and adjusted individually. Cannabis containing high levels of active ingredients designed for recreational use might expose patients to potential harm. No acute analgesia should be intended.
The Entourage Effect
Studies where THC and CBD were administered under controlled conditions in pure form suggest that cannabis products that are high in THC but low in CBD may be particularly hazardous for mental health [97]. When THC was either smoked or applied together with CBD (ratios of 2:1, 1:1, and 1:2 of CBD to THC), patients highlight the more favorable therapeutic effects and less side effects compared to taking pure THC orally [98]. This so-called entourage effect of cannabinoids, terpenes [99], and other cannabis components [5, 100]) is not only reported in community-based studies but also by patients [101] suggesting that the phytomolecule assemblages found in cannabis chemovars that exhibit entourage activity should be explored further. THC evokes its side effects, such as fear and tachycardia, especially in cannabis-naive patients, limiting its therapeutic potential [98, 102, 103]. Some studies found that CBD reduced intense experiences of anxiety or psychosis-like effects of THC and blunted some of the impairments on emotion and reward processing. Up to now, only few studies have investigated the biological benefits of full-spectrum cannabis plant extract. Employing the full spectrum of cannabis compounds should increase the tolerability of THC and booster the therapeutic benefit of cannabinoids [100, 104]. In a recent randomized placebo-controlled 4-way crossover trial, the acute analgesic effects of inhaled pharmaceutical-grade cannabis varieties were tested. The pharmacokinetics and pharmacodynamics after inhalation of cannabis flowers with a high content of THC (“Bedrocan 6”) were compared with a cannabis chemotype containing THC and CBD in a ratio of 1:1 (“Bediol”). CBD inhalation increased THC plasma concentrations and diminished THC-induced analgesic effects, revealing a synergistic pharmacokinetic but antagonistic pharmacodynamic interaction of THC and CBD. Animal experiments showed that repeated CBD applications reduce the development of tolerance to the acute antinociceptive effects of THC [105]. The mechanism(s) underlying the ameliorating effect of CBD has been recently studied using functional magnetic resonance imaging [106]. Increasing evidence indicates that the positive effect is represented in the intrinsic brain networks. The inhalation of low or non-CBD plant material affected the functional connectivity in the default mode network which consists of discrete, bilateral, and symmetrical cortical areas of the human, nonhuman primate, cat, and rodent brains and is a region that is normally active when the brain is at wakeful rest. A disruption of the salience network, a large-scale network which includes subcortical structures such as the amygdala, the ventral striatum, and the substantia nigra/ventral tegmental area provides a neuronal basis for cognitive decline and may be a candidate neuroimaging biomarker of cognitive impairment. After taking CBD-containing plant material, the connectivity in these regions is slightly influenced, suggesting that CBD might counteract some of the harmful and unpleasant acute effects of THC by influencing brain regions responsible for psychotropic side effects. A dysregulated ECS activity as a consequence of genetic and/or epigenetic alterations may result in several neuropsychiatric disorders. A synopsis of these experimental trials illustrate the complex behavior of inhaled cannabinoids and the shortcomings in an attempt to gain clinically relevant information about long-term treatment of chronic pain states with cannabinoids [107].
The interplay of drug-metabolizing enzymes such as CYP 3A4 and transport systems controls the drug disposition [108]. The bioavailability of most drugs is influenced by hepatic and intestinal biotransformation. The first-pass metabolism increases the concentrations of the metabolites during the first hour after smoking. THC is metabolized to 11-OH-THC (and further 11-nor-carboxy-THC) preferentially by the CYP2C9 pathway in the liver and the intestines after oral administration [109]. The psychoactive effects of this equipotent metabolite of THC are judged of clinical relevance. The evidence that CBD could delay the degradation of THC in the blood by inhibiting the P450-catalyzed degradation to 11-OH-THC is weak since the effect of CBD is rather small in comparison to the variability caused by other factors [110].
Absorption Barriers for Phytocannabinoids
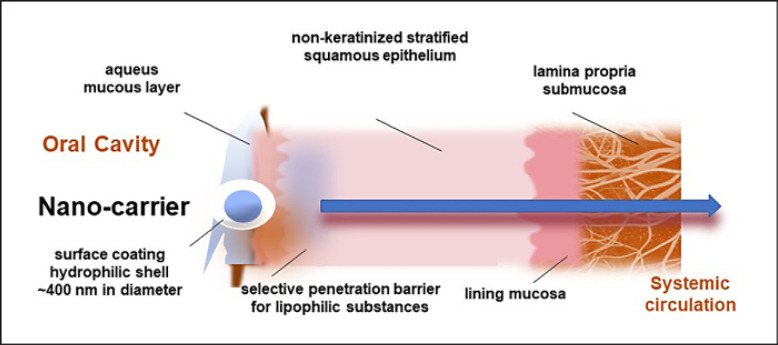
In addition to various other factors such as first-pass metabolism, pre-systemic elimination and the degree of protein binding greatly affect the pharmacokinetics of a drug. Low and imbalanced oral bioavailability jeopardizes the development of a therapeutic algorithm. For effective oral absorption, drugs need to have a balance between hydrophilic and lipophilic properties. Next to the aqueous solubility in body fluids, high lipid solubility is equally required to be able to cross the epithelial membranes [111] (see Fig. 3). Drug substances need to be soluble in the aqueous, buccal, or gastrointestinal fluids in order to permeate across the biological membranes [112].
Fig. 3.
Nano-carrier (see text).
Cannabinoids and terpenes in cannabis flowers are highly lipophilic compounds and considered to be very poorly water-soluble substances and thus exhibit only poor oral bioavailability. The European Pharmacopoeia defines a substance as practically insoluble at a solubility of less than 0.1 mg/mL in a certain solvent. Such substances are scarcely taken up following oral application. By increasing their water solubility, the therapeutic potential for an oral application increases dramatically (see below). At a solubility ranging from 33 to 100 mg/mL, a substance may be considered as water-soluble.
Oral administration followed by intestinal absorption is the most frequently used route of drug delivery [113, 114, 115, 116]. In the oral cavity, the top third region of the epithelium acts as a selective penetration barrier for lipophilic substances [117] taken orally or inhaled [118]. Sublingual and buccal regions of the oral cavity are lined by the nonkeratinized stratified squamous epithelium, which acts as a selective penetration barrier for drugs [117]. The squamous epithelium is covered by a layer of mucins. Mucins are the primary gel-forming components of mucus and provide a critical layer of protection on wet epithelial surfaces in the body including the gastrointestinal tract, female genital tract, and respiratory tract (see [119] for details). Oral mucosal epithelial cells express the membrane-anchored mucins, localized mainly to small vesicles and plasma membranes of oral epithelial cells.
These high-molecular-weight mucopolysaccharides are members of the mucin family encoded by at least 20 different genes. MUC5B is the prevailing mucin in the oral cavity. The lamina propria, situated beneath the squamous epithelium, consists of connective tissue with a network of blood vessels and muscles where drugs are predominantly absorbed via transcellular or paracellular diffusion (see Fig. 3) [113, 116]. It involves three main types of mucosae [120], of which the mucosa, also referred as lining mucosa (cheek area) [118], has the largest surface area.
Smart Lipids (Nano-Carrier)
Water-insoluble ingredients cannot pass through the aqueous mucous layer in the oral cavity without a special surface coating. An intact mucous layer allows only very few water-insoluble particles to pass through [121, 122]. These particles must be smaller than 5 μm in diameter [123], not to be retained. Recently developed nano-carriers (patented for Apurano Life Sciences GmbH, Munich, Germany) are small enough to overcome these limitations. This striking advance in galenic technology uses a hydrophilic shell in order to interact with the hydrophilic nature of the mucous layer. The uptake capacity of nano-carriers can be gauged from enterocytes, the most abundant epithelial cell lineage in both the small and the large intestines. Enterocytes are responsible together with microvilli for nutrient uptake in the small intestine. Importantly, drug particles can only be absorbed when they are significantly smaller than enterocytes [124].
Orally administered lipophilic drugs, such as the phytocannabinoids, are absorbed, after swallowing mainly in the small intestine. The mucous layer of the small intestine allows only very few water-insoluble particles to pass through. The intestinal villi of the small intestine are covered by an aqueous and slightly negatively charged layer (120–480 µm) of MUCs [125, 126] which retains water-insoluble particles and allows only particles with a hydrophilic surface to reach the brush border on the intestinal epithelial cells (microvilli) to be absorbed by the cells of the intestinal wall.
Common Application Routes
The most common application routes for cannabis are oral intake and inhalation. The concentration of THC in the plasma peaks and drops more rapidly after smoking compared to oral administration [127, 128]. During smoking, e.g., a cigarette containing 34 mg THC resulted in a peak plasma concentration of 162 ng/mL, after 9 min, the plasma concentration drops to 10 ng/mL after about 1 h. Since the effect may have vanished after about 2 h, a sufficient treatment will require further attention making smoking cannabis unacceptable in hospitals and care facilities, although THC and CBD would rapidly achieve high plasma concentrations after smoking. Furthermore, the affective consequences of a rapidly achieved peak concentration and the aversive experience of a repeated end-of-dose effect must be avoided. Cigarettes containing cannabis may also more easily pave the way to abuse. Cannabis and tobacco smoke contain similar carcinogenic polyaromatic hydrocarbons [129].
A standardized drug release is a prerequisite for clinically relevant studies. The efficacy is too difficult to gauge when the number and depth of inhalations fluctuate. In general, cannabinoids should not be used to treat acute nociception (vulgo: acute pain). Noteworthily, also cannabis applied primarily for medical purposes can lead to paradoxical and adverse effects, depending on the amount of cannabis used and the individual responsivity of genetically predisposed patients.
Besides smoking, the vaporization of cannabis is another form of inhalative application. Vaporizing cannabis flowers is considered less hazardous than smoking since fewer pyrolytic products are produced, and dosing seems easier. When put side by side, the pharmacokinetic profiles of THC produced either by vaporization or smoking are similar. A higher interindividual variability was observed after smoking compared to vaporization [130]. The absorption and the pharmacokinetic profile of CBD and THC after vaporization are almost identical. In patients, a pharmacokinetic profile was established following the administration of Bedrolite®, a CBD-focused cannabis strain [107]. Vaporization of Bedrolite® with 18.4 mg CBD and less than 1 mg of THC was inhaled. CBD increased within a few min in the plasma and reached a maximum plasma concentration of 160 ng/mL after approximately 5 min.
A standardized cannabis extract with an approximately equal ratio of THC to CBD is Sativex®, approved in Germany and elsewhere [131]. It is used as an oromucosal spray. The two cannabinoids are obviously absorbed mainly via the gastrointestinal tract since there is no delayed second peak in the plasma curve as one would expect from an absorption through the oral mucosa trailed by intestinal uptake. Since the highest plasma concentration for THC was measured 1.5 h following ingestion, it may be concluded that THC is taken up almost exclusively via the gastrointestinal route burdened by a putative increase of 11-OH-THC, the equipotent psychoactive first metabolite of THC. The concentration ratio 11-OH-THC/THC allows distinguishing oral from inhalative cannabis consumption. The pharmacokinetic profile of the plasma concentration of CBD after administration of Sativex® is comparable to THC. After a single administration of three different doses, the highest plasma concentration of THC (4 ng/mL THC) was found approximately 1.5 h after sublingual application of Sativex® (THC 21.6 mg/CBD 20 mg) with no clear linearity with increasing doses [132].
A medication containing only THC (dronabinol) is available in Germany [133]. It can be taken orally using drops or capsules. Drops and capsules with the same THC concentration yield similar plasma concentrations after about 1 h [134]. The pharmacokinetics of dronabinol when applied as liquids or capsules is similar, indicating that dronabinol is not absorbed via the oral mucosa, otherwise it should result in a different outline of the AUC, when applied as drops.
In 2019, the US Food and Drug Administration (FDA) approved the CBD drug Epidiolex® (Epidyolex in Germany) for the treatment of epilepsy (Dravet syndrome and Lennox-Gastaut syndrome) in children [131]. Epidiolex® contains plant-derived CBD. In a human study, the pharmacokinetics of CBD was evaluated after single-dose administrations of Epidiolex® [135]. For all doses, the highest plasma concentration was measured after about 5 h. A plasma concentration of 782 ng/mL was achieved by the highest applied dose of CBD (6,000 mg). CBD appears to have a favorable safety and tolerability profile, but there remains still a paucity of data, particularly in terms of chronic exposure in humans.
Perspectives
Cannabis has been used for centuries for medicinal purposes. The fascinating journey from a legal and frequently prescribed status to illegal and now back to liberalization has been driven by political and social factors rather than by science. Well-designed experimental procedures, as well as landmark studies, have significantly advanced the field, and a synopsis of recent research proposes promising therapeutic potential of cannabinoid-based drugs for a wide range of medical conditions, including neurological and psychiatric disorders.
The ECS describes an evolutionarily highly conserved group of neuromodulatory lipids, their receptors, and anabolic and catabolic enzymes, which is involved in a plethora of physiological and pathological processes. Targeting receptors and metabolic pathways of this wide-spread system and components of biochemically related mediators may provide new therapeutic algorithms. Recent research has suggested that chronic pain can be seen as the inability to extinguish associative memory traces encoded by nociceptive inputs, rendering chronic pain states less somatic and more associative in nature (memory of pain). Adequately modulating stressful chronic pain states critically depends on associative learning processes in the limbic circuitry of the brain, controlling anticipatory anxiety.
The evidence that full-spectrum cannabis preparations have medical benefits with less unwanted central effects stimulated the development of an oromucosal spray containing full-spectrum water-soluble cannabis. This remarkable innovation in galenic technology advocates clinical studies further and enables the realization of the very promising therapeutic potentials. Medicinal cannabis has a favorable safety and tolerability profile, but there remains still a paucity of data, particularly in terms of chronic exposure. A phase I, open-label clinical trial in healthy male subjects was conducted to assess the pharmacokinetic and safety profile of an oromucosal cannabinoid spray (AP701) containing a lipid-based nanoparticular drug formulation standardized to THC (for details see [136]; this issue).
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
There are no funding sources for this study.
Author Contributions
W.Z. wrote the paper. C.T.W. and B.L. contributed to the molecular part. A.B. and T.R.T. contributed to the translational clinical aspects. R.B. contributed to the pharmaceutical aspects. B.B. contributed to the clinically related psychological aspects.
References
- 1.Tart CT. Marijuana intoxication common experiences. Nature. 1970;226:701–4. doi: 10.1038/226701a0. [DOI] [PubMed] [Google Scholar]
- 2.McPartland JM. Cannabis systematics at the levels of family, genus, and species. Cannabis Cannabinoid Res. 2018;3((1)):203–12. doi: 10.1089/can.2018.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanuš LO, Meyer SM, Muñoz E, Taglialatela-Scafati O, Appendino G. Phytocannabinoids: a unified critical inventory. Nat Prod Rep. 2016;33((12)):1357–92. doi: 10.1039/c6np00074f. [DOI] [PubMed] [Google Scholar]
- 4.Sampson PB. Phytocannabinoid pharmacology: medicinal properties of cannabis sativa constituents aside from the “Big Two”. J Nat Prod. 2021;22((841)):142–60. doi: 10.1021/acs.jnatprod.0c00965. [DOI] [PubMed] [Google Scholar]
- 5.Hanuš LO, Hod Y. Terpenes/terpenoids in cannabis: are they important? Med Cannabis Cannabinoids. 2020;3((1)):25–60. doi: 10.1159/000509733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hazekamp A, Fischedick JT. Cannabis - from cultivar to chemovar. Drug Test Anal. 2012;4((7–8)):660–7. doi: 10.1002/dta.407. [DOI] [PubMed] [Google Scholar]
- 7.Moreira FA, Grieb M, Lutz B. Central side-effects of therapies based on CB1 cannabinoid receptor agonists and antagonists: focus on anxiety and depression. Best Pract Res Clin Endocrinol Metab. 2009;23:133–44. doi: 10.1016/j.beem.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Rey AA, Purrio M, Viveros MP, Lutz B. Biphasic effects of cannabinoids in anxiety responses: CB1 and GABAB receptors in the balance of GABAergic and glutamatergic neurotransmission. Neuropsychopharmacol. 2012;37:2624–34. doi: 10.1038/npp.2012.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mechoulam R, Parker LA. The endocannabinoid system and the brain. Annu Rev Psychol. 2013;64:21–47. doi: 10.1146/annurev-psych-113011-143739. [DOI] [PubMed] [Google Scholar]
- 10.Marsicano G, Wotjak CT, Azad SC, Bisogno T, Rammes G, Cascio MG, et al. The endogenous cannabinoid system controls extinction of aversive memories. Nature. 2002;418((6897)):530–4. doi: 10.1038/nature00839. [DOI] [PubMed] [Google Scholar]
- 11.Marsicano G, Goodenough S, Monory K, Hermann H, Eder M, Cannich A, et al. CB1 cannabinoid receptors and on-demand defense against excitotoxicity. Science. 2003;302((5642)):84–8. doi: 10.1126/science.1088208. [DOI] [PubMed] [Google Scholar]
- 12.Monory K, Massa F, Egertová M, Eder M, Blaudzun H, Westenbroek R, et al. The endocannabinoid system controls key epileptogenic circuits in the hippocampus. Neuron. 2006;1751((4)):455–66. doi: 10.1016/j.neuron.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azad SC, Monory K, Marsicano G, Cravatt BF, Lutz B, Zieglgänsberger W, et al. Circuitry for associative plasticity in the amygdala involves endocannabinoid signaling. J Neurosci. 2004 Nov 3;24((44)):9953–61. doi: 10.1523/JNEUROSCI.2134-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azad SC, Kurz J, Marsicano G, Lutz B, Zieglgänsberger W, Rammes G. Activation of CB1 specifically located on GABAergic interneurons inhibits LTD in the lateral amygdala. Learn Mem. 2008 Mar 5;15((3)):143–52. doi: 10.1101/lm.741908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han J, Kesner P, Metna-Laurent M, Duan T, Xu L, Georges F, et al. Acute cannabinoids impair working memory through astroglial CB1 receptor modulation of hippocampal LTD. Cell. 2012;148((5)):1039–50. doi: 10.1016/j.cell.2012.01.037. [DOI] [PubMed] [Google Scholar]
- 16.Cohen K, Weizman A, Weinstein A. Modulatory effects of cannabinoids on brain neurotransmission. Eur J Neurosci. 2019;50((3)):2322–45. doi: 10.1111/ejn.14407. [DOI] [PubMed] [Google Scholar]
- 17.Lutz B. Neurobiology of cannabinoid receptor signaling߭. Dialogues Clin Neurosci. 2020;22((3)):207–22. doi: 10.31887/DCNS.2020.22.3/blutz. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ye L, Cao Z, Wang W, Zhou N. New insights in cannabinoid receptor structure and signaling. Curr Mol Pharmacol. 2019;12((3)):239–48. doi: 10.2174/1874467212666190215112036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gertsch J, Pertwee RG, Di Marzo V. Phytocannabinoids beyond the Cannabis plant: do they exist? Br J Pharmacol. 2010;160((3)):523–9. doi: 10.1111/j.1476-5381.2010.00745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwal N, Pacher P, Tegeder I, Amaya F, Constantin CE, Brenner GJ, et al. Cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors in nociceptors. Nat Neurosci. 2007;10((7)):870–9. doi: 10.1038/nn1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jimenez-Blasco D, Busquets-Garcia A, Hebert-Chatelain E, Serrat R, Vicente-Gutierrez C, Ioannidou C, et al. Glucose metabolism links astroglial mitochondria to cannabinoid effects. Nature. 2020;583((7817)):603–8. doi: 10.1038/s41586-020-2470-y. [DOI] [PubMed] [Google Scholar]
- 22.Hebert-Chatelain E, Desprez T, Serrat R, Bellocchio L, Soria-Gomez E, Busquets-Garcia A, et al. A cannabinoid link between mitochondria and memory. Nature. 2016;539((7630)):555–9. doi: 10.1038/nature20127. [DOI] [PubMed] [Google Scholar]
- 23.Jordan CJ, Xi ZX. Progress in brain cannabinoid CB2 receptor research: from genes to behavior. Neurosci Biobehav Rev. 2019;98:208–20. doi: 10.1016/j.neubiorev.2018.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabañero D, Ramírez-López A, Drews E, Schmöle A, Otte DM, Wawrzczak-Bargiela A, et al. Protective role of neuronal and lymphoid cannabinoid CB2 receptors in neuropathic pain. Elife. 2020;209:e55582. doi: 10.7554/eLife.55582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katz D, Katz I, Porat-Katz BS, Shoenfeld Y. Medical cannabis: another piece in the mosaic of autoimmunity? Clin Pharmacol Ther. 2017;101((2)):230–8. doi: 10.1002/cpt.568. [DOI] [PubMed] [Google Scholar]
- 26.Stempel AV, Stumpf A, Zhang HY, Özdoğan T, Pannasch U, Theis AK, et al. Cannabinoid type 2 receptors mediate a cell type-specific plasticity in the hippocampus. Neuron. 2016;90((4)):795–809. doi: 10.1016/j.neuron.2016.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zieglgänsberger W. Neuropeptides: electrophysiology. In: Squire LR, editor. Encyclopedia of neuroscience. Oxford: Academic Press; 2009. pp. p. 885–90. [Google Scholar]
- 28.Navarrete M, Díez A, Araque A. Astrocytes in endocannabinoid signalling. Philos Trans R Soc Lond B Biol Sci. 2014;369:20130599. doi: 10.1098/rstb.2013.0599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metna-Laurent M, Marsicano G. Rising stars: modulation of brain functions by astroglial type-1 cannabinoid receptors. Glia. 2015;63:353–64. doi: 10.1002/glia.22773. [DOI] [PubMed] [Google Scholar]
- 30.Piomelli D. The molecular logic of endocannabinoid signalling. Nat Rev Neurosci. 2003;4:873–84. doi: 10.1038/nrn1247. [DOI] [PubMed] [Google Scholar]
- 31.Lutz B, Marsicano G, Maldonado R, Hillard CJ. The endocannabinoid system in guarding against fear, anxiety and stress. Nat Rev Neurosci. 2015;16((12)):705–18. doi: 10.1038/nrn4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ohno-Shosaku T, Kano M. Endocannabinoid-mediated retrograde modulation of synaptic transmission. Curr Opin Neurobiol. 2014;29:1–8. doi: 10.1016/j.conb.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 33.Pertwee RG. Endocannabinoids and their pharmacological actions. Handb Exp Pharmacol. 2015;231:1–37. doi: 10.1007/978-3-319-20825-1_1. [DOI] [PubMed] [Google Scholar]
- 34.Lee SH, Ledri M, Tóth B, Marchionni I, Henstridge CM, Dudok B, et al. Multiple forms of endocannabinoid and endovanilloid signaling regulate the tonic control of GABA release. J NeurosciJ Neurosci. 2015;35((27)):10039–57. doi: 10.1523/JNEUROSCI.4112-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ligresti A, De Petrocellis L, Di Marzo V. From phytocannabinoids to cannabinoid receptors and endocannabinoids: pleiotropic physiological and pathological roles through complex pharmacology. Physiol Rev. 2016;96((4)):1593–659. doi: 10.1152/physrev.00002.2016. [DOI] [PubMed] [Google Scholar]
- 36.Katona I, Freund TF. Multiple functions of endocannabinoid signaling in the brain. Annu Rev Neurosci. 2012;35:529–58. doi: 10.1146/annurev-neuro-062111-150420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robin LM, Oliveira da Cruz JF, Langlais VC, Martin-Fernandez M, Metna-Laurent M, Busquets-Garcia A, et al. Astroglial CB1 receptors determine synaptic D-serine availability to enable recognition memory. Neuron. 2018;698((5)):935–e5. doi: 10.1016/j.neuron.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 38.Bilkei-Gorzo A, Albayram O, Draffehn A, Michel K, Piyanova A, Oppenheimer H, et al. A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nat Med Jun. 2017;23((6)):782–7. doi: 10.1038/nm.4311. [DOI] [PubMed] [Google Scholar]
- 39.Moreira FA, Aguiar DC, Terzian AL, Guimarães FS, Wotjak CT. Cannabinoid type 1 receptors and transient receptor potential vanilloid type 1 channels in fear and anxiety-two sides of one coin? Neuroscience. 2012;204:186–92. doi: 10.1016/j.neuroscience.2011.08.046. [DOI] [PubMed] [Google Scholar]
- 40.Muller C, Morales P, Reggio PH. Cannabinoid ligands targeting TRP channels. Front Mol Neurosci. 2019;11:11–487. doi: 10.3389/fnmol.2018.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muller C, Lynch DL, Hurst DP, Reggio PH. A closer look at anandamide interaction with TRPV1. Front Mol Biosci. 2020;7:144. doi: 10.3389/fmolb.2020.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caterina MJ, Julius D. The vanilloid receptor: a molecular gateway to the pain pathway. Annu Rev Neurosci. 2001;24:487–517. doi: 10.1146/annurev.neuro.24.1.487. [DOI] [PubMed] [Google Scholar]
- 43.Hayashi T. The sigma-1 receptor in cellular stress signaling. Front Neurosci. 2019;13((13)):733. doi: 10.3389/fnins.2019.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ortíz-Rentería M, Juárez-Contreras R, González-Ramírez R, Morales-Lázaro SL. TRPV1 channels and the progesterone receptor Sig-1R interact to regulate pain. Proc Natl Acad Sci U S A. 2018;115((7)):E1657–66. doi: 10.1073/pnas.1715972115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tomaselli G, Vallée M. Stress and drug abuse-related disorders: the promising therapeutic value of neurosteroids focus on pregnenolone-progesterone-allopregnanolone pathway. Front Neuroendocrinol. 2019;55:100789. doi: 10.1016/j.yfrne.2019.100789. [DOI] [PubMed] [Google Scholar]
- 46.Di S, Boudaba C, Popescu IR, Weng FJ, Harris C, Marcheselli VL, et al. Activity-dependent release and actions of endocannabinoids in the rat hypothalamic supraoptic nucleus. J Physiol. 2005;569:751–60. doi: 10.1113/jphysiol.2005.097477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hill MN, Karatsoreos IN, Hillard CJ, McEwen BS. Rapid elevations in limbic endocannabinoid content by glucocorticoid hormones in vivo. Psychoneuroendocrinology. 2010;35:1333–8. doi: 10.1016/j.psyneuen.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang GZ, Woolley CS. Estradiol acutely suppresses inhibition in the hippocampus through a sex-specific endocannabinoid and mGluR-dependent mechanism. Neuron. 2012;74:801–8. doi: 10.1016/j.neuron.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leweke FM, Mueller JK, Lange B, et Leweke FM, Mueller JK, Lange B, et al. Role of the endocannabinoid system in the pathophysiology of schizophrenia: implications for pharmacological intervention. CNS Drugs. 2018;32:605–19. doi: 10.1007/s40263-018-0539-z. [DOI] [PubMed] [Google Scholar]
- 50.Davies C, Bhattacharyya S. Cannabidiol as a potential treatment for psychosis. Ther Adv Psychopharmacol. 2019;9:2045125319881916. doi: 10.1177/2045125319881916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woelfl T, Rohleder C, Mueller JK, Lange B, Reuter A, Schmidt AM, et al. Effects of cannabidiol and delta-9-tetrahydrocannabinol on emotion, cognition, and attention: a double-blind, placebo-controlled, randomized experimental trial in healthy volunteers. Front Psychiatry. 2020;11:576877. doi: 10.3389/fpsyt.2020.576877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schoevers J, Leweke JE, Leweke FM. Cannabidiol as a treatment option for schizophrenia: recent evidence and current studies. Curr Opin Psychiatry. 2020;33((3)):185–91. doi: 10.1097/YCO.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 53.Kozela E, Juknat A, Vogel Z. Modulation of astrocyte activity by cannabidiol, a nonpsychoactive cannabinoid. Int J Mol Sci. 2017Jul 31;18((8)):1669. doi: 10.3390/ijms18081669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campos AC, Ortega Z, Palazuelos J, Fogaça MV, Aguiar DC, Díaz-Alonso J, et al. The anxiolytic effect of cannabidiol on chronically stressed mice depends on hippocampal neurogenesis: involvement of the endocannabinoid system. Int J Neuropsychopharmacol. 2013;16((6)):1407–19. doi: 10.1017/S1461145712001502. [DOI] [PubMed] [Google Scholar]
- 55.Merlos M, Romero L, Zamanillo D, Plata-Salamán C, Vela JM. Sigma-1 receptor and pain. Handb Exp Pharmacol. 2017;244:131–61. doi: 10.1007/164_2017_9. [DOI] [PubMed] [Google Scholar]
- 56.Rodríguez-Muñoz M, Onetti Y, Cortés-Montero E, Garzón J, Sánchez-Blázquez P. Cannabidiol enhances morphine antinociception, diminishes NMDA-mediated seizures and reduces stroke damage via the sigma 1 receptor. Mol Brain. 2018;11((1)):51. doi: 10.1186/s13041-018-0395-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zimmermann CA, Arloth J, Santarelli S, Löschner A, Weber P, Schmidt MV, et al. Stress dynamically regulates co-expression networks of glucocorticoid receptor-dependent MDD and SCZ risk genes. Transl Psychiatry. 2019;9((91)):41. doi: 10.1038/s41398-019-0373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Russo SJ, Murrough JW, Han MH, Charney DS, Nestler EJ. Neurobiology of resilience. Nat Neurosci. 2012;15:1475–84. doi: 10.1038/nn.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Franklin TB, Saab BJ, Mansuy IM. Neural mechanisms of stress resilience and vulnerability. Neuron. 2012;75:747–61. doi: 10.1016/j.neuron.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 60.Riebe CJ, Wotjak CT. Endocannabinoids and stress. Stress. 2011;14:384–97. doi: 10.3109/10253890.2011.586753. [DOI] [PubMed] [Google Scholar]
- 61.Chen Y, Dubé CM, Rice CJ, Baram TZ. Rapid loss of dendritic spines after stress involves derangement of spine dynamics by corticotropin-releasing hormone. J Neurosci. 2008;28((11)):2903–11. doi: 10.1523/JNEUROSCI.0225-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Radley JJ, Arias CM, Sawchenko PE. Regional differentiation of the medial prefrontal cortex in regulating adaptive responses to acute emotional stress. J Neurosci. 2006;26((50)):12967–76. doi: 10.1523/JNEUROSCI.4297-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Castillo PE, Younts TJ, Chávez AE, Hashimotodani Y. Endocannabinoid signaling and synaptic function. Neuron. 2012;76:70–81. doi: 10.1016/j.neuron.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Njoo C, Agarwal N, Lutz B, Kuner R. The cannabinoid receptor CB1 interacts with the WAVE1 complex and plays a role in actin dynamics and structural plasticity in neurons. PLoS Biol. 2015;13((10)):e1002286. doi: 10.1371/journal.pbio.1002286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schmidt MV, Schülke JP, Liebl C, Stiess M, Avrabos C, Bock J, et al. Tumor suppressor down-regulated in renal cell carcinoma 1 (DRR1) is a stress-induced actin bundling factor that modulates synaptic efficacy and cognition. Proc Natl Acad Sci U S A. 2011;11108((41)):17213–8. doi: 10.1073/pnas.1103318108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Han Q, Kim YH, Wang X, Liu D, Zhang ZJ, AlexandraBey L, et al. SHANK3 deficiency impairs heat hyperalgesia and TRPV1 signaling in primary sensory neurons. Neuron. 2016;92((6)):1279–93. doi: 10.1016/j.neuron.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ho IHT, Chan MTV, Wu WKK, Liu X. Spinal microglia-neuron interactions in chronic pain. J Leukoc Biol. 2020;108((5)):1575–92. doi: 10.1002/JLB.3MR0520-695R. [DOI] [PubMed] [Google Scholar]
- 68.Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An FMRI study of social exclusion. Science. 2003;302:290–2. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- 69.Melzack R, Katz J. Pain. Wires Interdiscip Cogn Sci. 2013;4((1)):1–15. doi: 10.1002/wcs.1201. [DOI] [PubMed] [Google Scholar]
- 70.Bannister K, Dickenson AH. The plasticity of descending controls in pain: translational probing. J Physiol. 2017;595((13)):4159–66. doi: 10.1113/JP274165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zieglgänsberger W. Substance P and pain chronicity. Cell Tissue Res. 2019;375((1)):227–41. doi: 10.1007/s00441-018-2922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sumislawski JJ, Ramikie TS, Patel S. Reversible gating of endocannabinoid plasticity in the amygdala by chronic stress: a potential role for monoacylglycerol lipase inhibition in the prevention of stress-induced behavioral adaptation. Neuropsychopharmacology. 2011;36:2750–61. doi: 10.1038/npp.2011.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Graham BM, Langton JM, Richardson R. Pharmacological enhancement of fear reduction: preclinical models. Br J Pharmacol. 2011;164:1230–47. doi: 10.1111/j.1476-5381.2010.01175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sylvers P, Lilienfeld SO, LaPrairie JL. Differences between trait fear and trait anxiety: implications for psychopathology. Clin Psychol Rev. 2011;31:122–37. doi: 10.1016/j.cpr.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 75.Bandelow B. Generalized anxiety disorder and pain. Mod Trends Pharmacopsychiatry. 2015;30:153–65. doi: 10.1159/000435939. [DOI] [PubMed] [Google Scholar]
- 76.Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017;19((2)):93–107. doi: 10.31887/DCNS.2017.19.2/bbandelow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xanthos DN, Sandkühler J. Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nat Rev Neurosci. 2014;15((1)):43–53. doi: 10.1038/nrn3617. [DOI] [PubMed] [Google Scholar]
- 78.Mapplebeck JCS, Dalgarno R, Tu Y, Moriarty O, Beggs S, Kwok CHT, et al. Microglial P2X4R-evoked pain hypersensitivity is sexually dimorphic in rats. Pain. 2018;159((9)):1752–63. doi: 10.1097/j.pain.0000000000001265. [DOI] [PubMed] [Google Scholar]
- 79.Salter MW, Beggs S. Sublime microglia: expanding roles for the guardians of the CNS. Cell. 2014;158((1)):15–24. doi: 10.1016/j.cell.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 80.Okutsu Y, Takahashi Y, Nagase M, Shinohara K, Ikeda R, Kato F. Potentiation of NMDA receptor-mediated synaptic transmission at the parabrachial-central amygdala synapses by CGRP in mice. Mol Pain. 2017;13:1744806917709201. doi: 10.1177/1744806917709201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zieglgänsberger W, Berthele A, Tölle TR. Understanding neuropathic pain CNS. Spectr. 2005;10((4)):298–308. doi: 10.1017/s1092852900022628. [DOI] [PubMed] [Google Scholar]
- 82.Castello-Waldow TP, Weston G, Ulivi AF, Chenani A, Loewenstein Y, Chen A, et al. Hippocampal neurons with stable excitatory connectivity become part of neuronal representations. PLoS Biol. 2020;18:e3000928. doi: 10.1371/journal.pbio.3000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gogolla N, Caroni P, Lüthi A, Herry C. Perineuronal nets protect fear memories from erasure. Science. 2009;4325((5945)):1258–61. doi: 10.1126/science.1174146. [DOI] [PubMed] [Google Scholar]
- 84.Patel S, Hill MN, Cheer JF, Wotjak CT, Holmes A. The endocannabinoid system as a target for novel anxiolytic drugs. Neurosci Biobehav Rev. 2017;76((Pt A)):56–66. doi: 10.1016/j.neubiorev.2016.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Singer W. Neuronal oscillations: unavoidable and useful? Eur J Neurosci. 2018;48((7)):2389–98. doi: 10.1111/ejn.13796. [DOI] [PubMed] [Google Scholar]
- 86.Dine J, Genewsky A, Hladky F, Wotjak CT, Deussing JM, Zieglgänsberger W, et al. Local optogenetic induction of fast (20–40 Hz) pyramidal-interneuron network oscillations in the in vitro and in vivo ca1 hippocampus: modulation by crfand enforcement of perirhinal theta activity. Front Cell Neurosci. 2016;26((10)):10816. doi: 10.3389/fncel.2016.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Riebe CJ, Pamplona FA, Pamplona F, Kamprath K, Wotjak CT. Fear relief-toward a new conceptual frame work and what endocannabinoids gotta do with it. Neuroscience. 2012;204:159–85. doi: 10.1016/j.neuroscience.2011.11.057. [DOI] [PubMed] [Google Scholar]
- 88.van der Flier FE, Kwee CMB, Cath DC, Batelaan NM, Groenink L, Duits P, et al. Cannabidiol enhancement of exposure therapy in treatment refractory patients with phobias: study protocol of a randomized controlled trial. BMC Psychiatry. 2019;19:69. doi: 10.1186/s12888-019-2022-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ruehle S, Rey AA, Remmers F, Lutz B. The endocannabinoid system in anxiety, fear memory and habituation. J Psychopharmacol. 2012;26:23–39. doi: 10.1177/0269881111408958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kathuria S, Gaetani S, Fegley D, Valiño F, Duranti A, Tontini A, et al. Modulation of anxiety through blockade of anandamide hydrolysis. Nat Med. 2003;9:76–81. doi: 10.1038/nm803. [DOI] [PubMed] [Google Scholar]
- 91.Puighermanal E, Marsicano G, Busquets-Garcia A, Lutz B, Maldonado R, Ozaita A. Cannabinoid modulation of hippocampal long-term memory is mediated by mTOR signaling. Nat Neurosci. 2009;12((9)):1152–8. doi: 10.1038/nn.2369. [DOI] [PubMed] [Google Scholar]
- 92.Urquhart P, Nicolaou A, Woodward DF. Endocannabinoids and their oxygenation by cyclo-oxygenases, lipoxygenases and other oxygenases. Biochim Biophys Acta. 2015;1851((4)):366–76. doi: 10.1016/j.bbalip.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 93.Slivicki RA, Iyer V, Mali SS, Garai S, Thakur GA, Crystal JD, et al. Positive allosteric modulation of cb1 cannabinoid receptor signaling enhances morphine antinociception and attenuates morphine tolerance without enhancing morphine- induced dependence or reward. Front Mol Neurosci. 2020;13:54. doi: 10.3389/fnmol.2020.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bandelow B. Current and novel psychopharmacological drugs for anxiety disorders. Adv Exp Med Biol. 2020;1191:347–65. doi: 10.1007/978-981-32-9705-0_19. [DOI] [PubMed] [Google Scholar]
- 95.Shen CJ, Zheng D, Li KX, Yang JM, Pan HQ, Yu XD, et al. Cannabinoid CB1 receptors in the amygdalar cholecystokinin glutamatergic afferents to nucleus accumbens modulate depressive-like behavior. Nat Med. 2019;25:337–49. doi: 10.1038/s41591-018-0299-9. [DOI] [PubMed] [Google Scholar]
- 96.Marcus DJ, Bedse G, Gaulden AD, Ryan JD, Kondev V, Winters ND, et al. Endocannabinoid signaling collapse mediates stress-induced amygdalo-cortical strengthening. Neuron. 2020;105:1062–e6. doi: 10.1016/j.neuron.2019.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Englund A, Morrison PD, Nottage J, Hague D, Kane F, Bonaccorso S, et al. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J Psychopharmacol. 2013;27((1)):19–27. doi: 10.1177/0269881112460109. [DOI] [PubMed] [Google Scholar]
- 98.Favrat B, Ménétrey A, Augsburger M, Rothuizen LE, Appenzeller M, Buclin T, et al. Two cases of “cannabis acute psychosis” following the administration of oral cannabis. BMC Psychiatry. 2005;5:17. doi: 10.1186/1471-244X-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ferber SG, Namdar D, Hen-Shoval D, Eger G, Koltai H, Shoval G, et al. The “Entourage Effect”: terpenes coupled with cannabinoids for the treatment of mood disorders and anxiety disorders. Curr Neuropharmacol. 2020;18((2)):87–96. doi: 10.2174/1570159X17666190903103923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ben-Shabat S, Fride E, Sheskin T, Tamiri T, Rhee MH, Vogel Z, et al. An entourage effect: inactive endogenous fatty acid glycerol esters enhance 2-arachidonoyl-glycerol cannabinoid activity. Eur J Pharmacol. 1998;353((1)):23–31. doi: 10.1016/s0014-2999(98)00392-6. [DOI] [PubMed] [Google Scholar]
- 101.Freeman AM, Petrilli K, Lees R, Hindocha C, Mokrysz C, Curran HV, et al. How does cannabidiol (CBD) influence the acute effects of delta-9-tetrahydrocannabinol (THC) in humans? A systematic review. Neurosci Biobehav Rev. 2019;107:696–712. doi: 10.1016/j.neubiorev.2019.09.036. [DOI] [PubMed] [Google Scholar]
- 102.D'Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29((8)):1558–72. doi: 10.1038/sj.npp.1300496. [DOI] [PubMed] [Google Scholar]
- 103.Maayah ZH, Takahara S, Ferdaoussi M, Dyck JRB. The anti-inflammatory and analgesic effects of formulated full-spectrum cannabis extract in the treatment of neuropathic pain associated with multiple sclerosis. Inflamm Res. 2020;69((6)):549–58. doi: 10.1007/s00011-020-01341-1. [DOI] [PubMed] [Google Scholar]
- 104.Russo EB. Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br J Pharmacol. 2011;163((7)):1344–64. doi: 10.1111/j.1476-5381.2011.01238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Greene NZ, Wiley JL, Yu Z, Clowers BH, Craft RM. Cannabidiol modulation of antinociceptive tolerance to Δ9-tetrahydrocannabinol. Psychopharmacology. 2018;235((11)):3289–302. doi: 10.1007/s00213-018-5036-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wall MB, Pope R, Freeman TP, Kowalczyk OS, Demetriou L, Mokrysz C, et al. Dissociable effects of cannabis with and without cannabidiol on the human brain's resting-state functional connectivity. J Psychopharmacol. 2019;33((7)):822–30. doi: 10.1177/0269881119841568. [DOI] [PubMed] [Google Scholar]
- 107.van de Donk T, Niesters M, Kowal MA, Olofsen E, Dahan A, van Velzen M. An experimental randomized study on the analgesic effects of pharmaceutical-grade cannabis in chronic pain patients with fibromyalgia. Pain. 2019;160((4)):860–9. doi: 10.1097/j.pain.0000000000001464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fritz A, Busch D, Lapczuk J, Ostrowski M, Drozdzik M, Oswald S. Expression of clinically relevant drug-metabolizing enzymes along the human intestine and their correlation to drug transporters and nuclear receptors: an intra-subject analysis. Basic Clin Pharmacol Toxicol. 2018;124((3)):245–55. doi: 10.1111/bcpt.13137. [DOI] [PubMed] [Google Scholar]
- 109.Patilea-Vrana GI, Unadkat JD. Quantifying hepatic enzyme kinetics of (-)-∆9-tetrahydrocannabinol (THC) and its psychoactive metabolite, 11-OH-THC, through in vitro modeling. Drug Metab Dispos. 2019;47((7)):743–52. doi: 10.1124/dmd.119.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nadulski T, Pragst F, Weinberg G, Roser P, Schnelle M, Fronk EM, et al. Randomized, double-blind, placebo-controlled study about the effects of cannabidiol (CBD) on the pharmacokinetics of Delta9-tetrahydrocannabinol (THC) after oral application of THC verses standardized cannabis extract. Ther Drug Monit. 2005;27((6)):799–810. doi: 10.1097/01.ftd.0000177223.19294.5c. [DOI] [PubMed] [Google Scholar]
- 111.Hua S. Advances in nanoparticulate drug delivery approaches for sublingual and buccal administration. Front Pharmacol. 2019;10((10)):1328. doi: 10.3389/fphar.2019.01328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Savjani KT, Gajjar AK, Savjani JK. Drug solubility: importance and enhancement techniques. ISRN Pharm. 2012;2012:195727. doi: 10.5402/2012/195727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Harris D, Robinson JR. Drug delivery via the mucous membranes of the oral cavity. J Pharm Sci. 1992;81:1–10. doi: 10.1002/jps.2600810102. [DOI] [PubMed] [Google Scholar]
- 114.Bykov VL. [The tissue and cell defense mechanisms of the oral mucosa] Morfologiia. 1996;110:14–24. [PubMed] [Google Scholar]
- 115.Bykov VL. [The functional morphology of the epithelial barrier of the oral mucosa] Stomatologiia. 1997;76:12–7. [PubMed] [Google Scholar]
- 116.Huh CH, Bhutani MS, Farfán EB, Bolch WE. Individual variations in mucosa and total wall thickness in the stomach and rectum assessed via endoscopic ultrasound. Physiol Meas. 2003;24:N15–22. doi: 10.1088/0967-3334/24/4/401. [DOI] [PubMed] [Google Scholar]
- 117.Gandhi RB, Robinson JR. Bioadhesion in drug delivery. Ind J Pharm Sci. 1988;50((3)):145–52. [Google Scholar]
- 118.Squier CA. The permeability of oral mucosa. Crit Rev Oral Biol Med. 1991;2((1)):13–32. doi: 10.1177/10454411910020010301. [DOI] [PubMed] [Google Scholar]
- 119.Wagner CE, Wheeler KM, Ribbeck K. Mucins and their role in shaping the functions of mucus barriers. Annu Rev Cell Dev Biol. 2018;34:189–215. doi: 10.1146/annurev-cellbio-100617-062818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shojaei AH. Buccal mucosa as a route for systemic drug delivery: a review. J Pharm Pharm Sci. 1998;1((1)):15–30. [PubMed] [Google Scholar]
- 121.Khan J, Iiboshi Y, Cui L, Wasa M, Sando K, Takagi Y, et al. Alanyl-glutamine-supplemented parenteral nutrition increases luminal mucus gel and decreases permeability in the rat small intestine. JPEN J Parenter Enteral Nutr. 1999;23((1)):24–31. doi: 10.1177/014860719902300124. [DOI] [PubMed] [Google Scholar]
- 122.Lai SK, Wang YY, Hanes J. Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv Drug Deliv Rev. 2009;61((2)):158–71. doi: 10.1016/j.addr.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Reineke JJ, Cho DY, Dingle YT, Morello AP, 3rd, Jacob J, Thanos CG, et al. Unique insights into the intestinal absorption, transit, and subsequent biodistribution of polymer-derived microspheres. Proc Natl Acad Sci U S A. 2013;110((34)):13803–8. doi: 10.1073/pnas.1305882110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Molnar A, Fu S. Techniques and technologies for the bioanalysis of Sativex(R), metabolites and related compounds. Bioanalysis. 2016;8((8)):829–45. doi: 10.4155/bio-2015-0021. [DOI] [PubMed] [Google Scholar]
- 125.Gniewek P, Kolinski A. Coarse-grained Monte Carlo simulations of mucus: structure, dynamics, and thermodynamics. Biophys J. 2010;99((11)):3507–16. doi: 10.1016/j.bpj.2010.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ensign LM, Cone R, Hanes J. Oral drug delivery with polymeric nanoparticles: the gastrointestinal mucus barriers. Adv Drug Deliv Rev. 2012;64((6)):557–70. doi: 10.1016/j.addr.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42((4)):327–60. doi: 10.2165/00003088-200342040-00003. [DOI] [PubMed] [Google Scholar]
- 128.Huestis MA. Human cannabinoid pharmacokinetics. Chem Biodivers. 2007;4((8)):1770–804. doi: 10.1002/cbdv.200790152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Aldington S, Harwood M, Cox B, Weatherall M, Beckert L, Hansell A, et al. Cannabis use and risk of lung cancer: a case-control study. Eur Respir J. 2008;31((2)):280–6. doi: 10.1183/09031936.00065707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Eisenberg E, Ogintz M, Almog S. The pharmacokinetics, efficacy, safety, and ease of use of a novel portable metered-dose cannabis inhaler in patients with chronic neuropathic pain: a phase 1a study. J Pain Palliat Care Pharmacother. 2014;28((3)):216–25. doi: 10.3109/15360288.2014.941130. [DOI] [PubMed] [Google Scholar]
- 131.Kocis PT, Vrana KE. Delta-9-tetrahydrocannabinol and cannabidiol drug-drug interactions. Med Cannabis Cannabinoids. 2020;3((1)):61–73. doi: 10.1159/000507998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Stott CG, White L, Wright S, Wilbraham D, Guy GW. A phase I study to assess the single and multiple dose pharmacokinetics of THC/CBD oromucosal spray. Eur J Clin Pharmacol. 2013;69((5)):1135–47. doi: 10.1007/s00228-012-1441-0. [DOI] [PubMed] [Google Scholar]
- 133.Schimrigk S, Marziniak M, Neubauer C, Kugler EM, Werner G, Abramov-Sommariva D. Dronabinol is a safe long-term treatment option for neuropathic pain patients. Eur Neurol. 2017;78((5–6)):320–9. doi: 10.1159/000481089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Parikh N, Kramer WG, Khurana V, Cognata Smith C, Vetticaden S. Bioavailability study of dronabinol oral solution versus dronabinol capsules in healthy volunteers. Clin Pharmacol. 2016;8:155–62. doi: 10.2147/CPAA.S115679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Taylor L, Gidal B, Blakey G, Tayo B, Morrison G. A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs. 2018;32((11)):1053–67. doi: 10.1007/s40263-018-0578-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lorenzl S, Gottwald F, Nistler A, Brehm L, Grötsch R, Haber G, et al. A phase I trial to determine the pharmacokinetics, psychotropic effects and safety profile of a novel nanoparticle-based cannabinoid spray for oromucosal delivery. Med Cannabis Cannabinoids. 2022;5:9–19. doi: 10.1159/000521352. [DOI] [PMC free article] [PubMed] [Google Scholar]