Abstract
Background:
Health professionals (HPs) coping with the coronavirus pandemic are at risk of working under stressful conditions impacting their professional well-being. The aim of this paper was to explore HP’s professional quality of life and occupational stress during the COVID-19 pandemic in Greece.
Method:
A cross-sectional study was conducted (from October to December 2020) in a COVID-19 reference hospital, one of the biggest in Attica. The method of convenience sampling has been used. Data collection was carried out through an anonymous, self-administered questionnaire including, apart from HPs’ demographic and occupational characteristics, Professional Quality of Life Scale (ProQoL) and Job Stress Measure. A total of 250 questionnaires were distributed to physicians and nurses. One hundred eighty-six questionnaires were fully completed (response rate = 78.8%). The analysis was based on descriptive and inductive statistics, using SPSS v25.
Results:
Participants’ mean age was 41.5 ± 10.4 years; 75.3% were women and 62.4% was nursing staff. ProQoL analysis showed that the majority had moderate compassion satisfaction (74.2%) and burnout (78.5%), while 48.8% had moderate level of secondary post-traumatic stress. The mean value of occupational stress was estimated at 2.76, showing a moderate level of stress. HPs’ demographic and occupational characteristics seemed to affect both work stress and ProQoL (P ⩽ .05). Occupational stress was positively correlated with both burnout (r = 0.461, P = .001) and secondary post-traumatic stress (r = 0.596, P = .001), indicating that an increase in health professionals’ stress at work corresponds to a simultaneous increase in ProQoL.
Conclusions:
HPs’ professional quality of life and occupational stress seemed to be moderate during the COVID-19 pandemic in Greece. In order to achieve an improvement in HPs’ overall professional well-being, priority should be given to the strengthening of the capacity of the healthcare system as well as to supporting HPs in both stress management and psychological resilience.
Keywords: Professional quality of life, occupational stress, health professionals, COVID-19 pandemic, Greece
Introduction
The coronavirus disease 2019 (COVID-19) outbreak has been acknowledged as a global health threat negatively impacting countries’ health care systems and economies.1-4 Numerous cooperative efforts have been initiated by international and European organizations focusing on the implementation of health strategies, funding programs, policy recommendations and socioeconomic recovery plans.5-7
The disruption caused by the COVID-19 pandemic has drastically altered people’s everyday lives and global mental health has become an urgent issue, identified as the tenth leading research topic. 8 Plenty of studies have deduced that COVID-19 has devastating effects on the mental health of the general population, such as depression and anxiety.9-11 A global systematic review regarding mental health symptoms in the general population during the COVID-19 pandemic, showed levels of anxiety ranging from 6.33% to 50.9%, levels of depression from 14.6% to 48.3%, post-traumatic stress disorder from 7% to 53.8%, psychological distress from 34.43% to 38%, and final levels of stress ranging from 8.1% to 81.9%. 12
Additionally, the foregoing results are in accordance with a multinational population-based study conducted in middle-income Asian countries; respondents scored high level of stress, anxiety and depression. 13
As far as the general population is concerned, gender (female), age (⩽40 years), low educational background, chronic diseases, COVID-19 infection, contact with COVID-19 patients and delayed lock-down measures are risk factors associated with adverse mental health.12,14 Another factor that has to do with poor mental health relates to people’s mood, that is, people with mood disorders may be at greater risk for COVID-19 hospitalization and death. 15
As far as the health professionals (HPs) specifically are concerned, sociodemographic and occupational risk factors relating to increased mental disorders include gender (female), age (⩽40 years), limited experience, working in intensive care units (ICU), emergency settings with direct patient contact or working on the frontline. 16
The pandemic brought a wide range of challenges for healthcare professionals, such as witnessing a large number of deaths, facing rational decisions, risk of infection and family members’ exposure, increased workload and working without sufficient equipment.17-19 These stressful conditions also brought symptoms of mental disorders and somatization to healthcare workers.20-22 These short and long term challenges are impacting health professionals’ efficiency, occupational stress and patient care, by influencing their professional quality of life (ProQoL).23,24
ProQoL is a complex concept associated with the degree to which employees are able to fulfill their personal needs through their work environment experiences. 25 It incorporates 2 aspects, the positive (Compassion Satisfaction-CS) and the negative (Compassion Fatigue-CF). Compassion Satisfaction includes people feeling invigorated by their work whereas Compassion Fatigue includes people suffering from burnout (BO) and secondary traumatic stress (STS). BO is characterized by feelings of unhappiness, disconnectedness and insensitivity to the working environment. STS includes inability to sleep and distinguishes between private and professional life. 26 Previous studies suggest that better professional quality of life is associated to less mental disorders27,28 and perceived stress.29,30 Many factors relating to HPs’ professional and social role, such as ambiguity, role conflict and workload can provoke work stress, resulting to the reduction of professional efficiency, especially during the coronavirus pandemic.31-33
Numerous studies focusing on the 2003 SARS epidemic reported that health professionals working in SARS units showed high levels of intensity, anxiety symptoms, hostility, and insomnia.34-36 Furthermore, due to direct exposure to patients with the virus, psychological burden, such as fear, insecurity, and secondary traumatic stress have been recorded. 37 Difficulties have also been reported regarding the ability to manage their personal, family and social life. 38 However, nowadays, there is an even higher prevalence of adverse psychiatric outcomes compared to the pre pandemic period.39,40
Greece, along with many other European countries, was hit by the COVID-19 pandemic in early 2020. The government responded immediately by implementing policies aiming to contain the spread of the virus, such as social distancing, suspension of economic, educational and cultural activities and restrictions on citizens’ mobility (lockdown). These measures resulted in minimizing the number of cases and deaths.41,42 It is worth noting here that the COVID-19 measures that Greece implemented came after a severe economic crisis period lasting more than a decade, with significant restrictions in health and pharmaceutical expenditures, inefficiencies in the healthcare workforce and in hospital equipment and supplies.43-45
There are limited studies assessing health professionals’ stress level (emerging from their work environment) and its impact on their personal and professional lives during the COVID-19 pandemic. Therefore, the objective of this study was to explore healthcare professionals’ ProQoL and occupational stress during the pandemic outbreak in Greece.
Methods
Study design and sample selection
A cross-sectional study was conducted at the «Evangelismos» COVID-19 reference hospital. This is one of the largest general hospitals in the region of Attica, with a resource capacity of 943 beds and approximately 2300 physicians and nurses. The study was performed during the second pandemic wave, that is from October to December 2020.
Convenience sampling was the methodology applied and data collection was carried out through a self-administered questionnaire. A total of 250 questionnaires were distributed to physicians and nurses, out of which 186 were completed (response rate = 78.8%). Participants met the following inclusion criteria: they were professionals who were on duty during the aforementioned period and came in contact with patients. Laboratory, administrative and auxiliary staff were excluded from the sample.
Study instrument
An anonymous questionnaire was distributed to the physicians and nurses aiming to assess the professional quality of life in relation to work stress during the period of the COVID-19 pandemic in Greece. The questionnaire was divided into 3 sections. The first section included questions on the socio-demographic and occupational characteristics of the sample. The other 2 sections consisted of the «Professional Quality of Life Scale—ProQoL» and the «Job Stress Measure», respectively.
ProQoL consists of 30 questions-statements examining the quality of professional life of employees through 3 dimensions: (a) compassion satisfaction (CS), (b) burnout (BO), and (c) secondary traumatic stress (STS). Each dimension is psychometrically unique and is not a binding factor for the rest. The tool is measured at a 5-point Likert scale, where 1 corresponds to “never” and 5 to “very often.” A high score in each dimension refers to high levels of compassion satisfaction, burnout and secondary traumatic stress respectively. The questionnaire has been designed by Stamm 26 and is available in several languages, including Greek. 46
Job Stress Measure explores job stress through 16 questions covering 3 dimensions: (a) the characteristics of work including workload, time pressure, occupational safety and bureaucratic procedures, (b) clarity of objectives focusing on tasks’ distribution and conflicting roles, (c) business travel or meetings indicating high travel frequency and length of meetings. The answers are given at a 5-point Likert scale, where 1 corresponds to “no stress” and 5 to “a great deal of stress.” The tool has been translated and validated in Greek by Sakketou et al. 47
Statistical analysis
The data was analyzed by using SPSS v25 (Statistical Package for Social Sciences). The Cronbach alpha index for ProQol and Job Stress Measure showed adequate internal structure and reliability, a = 0.721 and 0.899, respectively. Descriptive statistics such as frequencies, percentages, mean and standard deviation were performed. The variables were normally distributed and, in order to explore any differences, parametric tests were chosen. Statistically significant differences among ProQoL and Job Stress Measure with dichotomous variables were investigated using Student t-test. Also, one way ANOVA was carried out for the analysis of the differences among variables when examining 3 or more groups. Pearson’s correlation test was applied for the relations between professional quality of life and job stress measure. Finally, linear regression analyses using backward method were carried out in order to investigate which factors predict professional quality of life of the sample. The significance level was set at P < .05.
Results
The socio-demographic and occupational characteristics of the sample are presented in Table 1. The mean age of participants was 41.5 ± 10.4 years; women represent the highest proportion (75.3%), 45.2% had a postgraduate educational level, 47.3% married and 45.2% without children.
Table 1.
Socio-demographic and occupational characteristics.
| Number | Percentage | |
|---|---|---|
| Gender | ||
| Men | 46 | 24.7 |
| Women | 140 | 75.3 |
| Age (years) mean (SD) | 41.5 (10.4) | |
| Educational level | ||
| Secondary | 36 | 19.4 |
| Tertiary | 66 | 35.5 |
| Postgraduate (MSc – PhD) | 84 | 45.2 |
| Marital status | ||
| Unmarried | 70 | 37.6 |
| Married | 88 | 47.3 |
| Divorced | 22 | 11.8 |
| Widow/a | 6 | 3.2 |
| Number of children | ||
| None | 84 | 45.2 |
| One | 22 | 11.8 |
| 2 | 56 | 30.1 |
| 3 or more | 24 | 12.9 |
| Profession | ||
| Physician | 70 | 37.6 |
| Nurse | 116 | 62.4 |
| Working departments | ||
| Pathological | 20 | 10.8 |
| Surgical | 52 | 28.0 |
| Endoscopic/Gastroenterological | 26 | 14.0 |
| Emergency | 18 | 9.7 |
| COVID unit | 32 | 17.2 |
| Other | 38 | 20.4 |
| Contact with COVID patients | ||
| Yes | 170 | 91.4 |
| Years of experience mean (SD) | 15.04 (10.3) | |
The mean years of working experience was 15.04 ± 10.3, 62.4% was nursing staff, 28% worked in surgical departments and 17.2% in the newly established COVID-19 clinics. The majority (91.4%) of health professionals stated that they came in contact with COVID-19 patients.
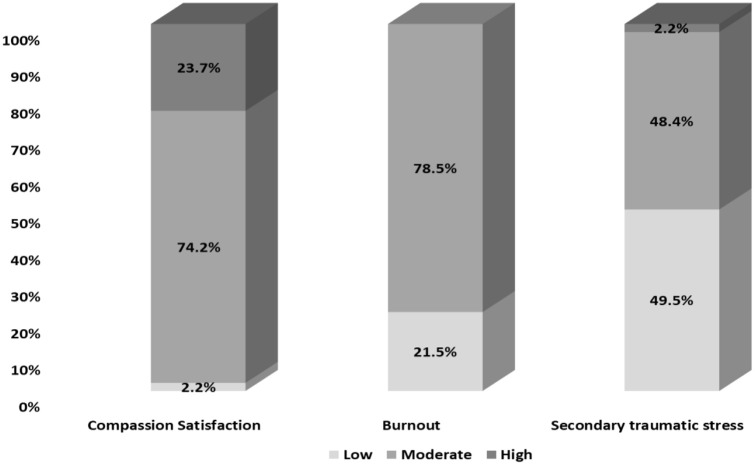
According to the ProQol analysis as presented in Figure 1, the majority of the participants had moderate CS (74.2%) and BO (78.5%). As far as STS levels are concerned, participants were almost evenly split among moderate and low levels of STS. The mean value of CS was 36.24 (±6.11), BO 26.53 (±5.17), and STS 23.45 (±6.34).
Figure 1.
Levels of ProQol dimensions.
As shown in Table 2, the ProQol results are analyzed with respect to the socio-demographic and occupational characteristics of the participants. Women scored significantly higher in CS than men (P = .024). Additionally, unmarried participants scored higher compared to married or divorced/widowed (P = .015) and also, participants with none or one child scored higher in CS compared to those with 2 or more children (P = .001). As far as work experience is concerned, participants with more than 11 years of work experience scored higher than the less experienced ones (P = .010). Those working at emergency departments scored the highest CS while those working at pathological departments scored the lowest CS (P = .001). Regarding BO, significant differences were only found in relation to the working departments (Table 2). Participants working at the pathological, emergency and the COVID-19 units scored a high BO (P = .003). Finally, a high score in STS was found in the following categories of participants; health professionals with secondary education (P = .018), those working in emergencies and COVID-19 units (P = .005) and physicians (P = .020) (Table 2).
Table 2.
Comparisons among health professionals’ ProQol and socio-demographic, occupational characteristics.
| Compassion satisfaction | Burnout | Secondary traumatic stress | P value | |
|---|---|---|---|---|
| Mean (SD) | ||||
| Gender | ||||
| Men | 34.48 (6.84) | .024 | ||
| Women | 36.81 (5.77) | |||
| Educational level | ||||
| Secondary | 25.89 (7.58) | .018 | ||
| Tertiary | 23.55 (7.41) | |||
| Postgraduate (MSc – PhD) | 22.33 (4.31) | |||
| Marital status | ||||
| Unmarried | 38.64 (4.20) | .015 | ||
| Married | 36.59 (6.17) | |||
| Divorced/Widowed | 34.83 (6.39) | |||
| Number of children | ||||
| None | 36.64 (5.34) | .001 | ||
| One | 36.22 (2.86) | |||
| 2 | 35.57 (6.48) | |||
| 3 or more | 34.91 (6.67) | |||
| Profession | ||||
| Physician | 22.26 (3.59) | .020 | ||
| Nurse | 24.17 (7.46) | |||
| Years of experience | ||||
| <10 years | 35.26 (6.45) | .010 | ||
| <11 years | 37.59 (5.37) | |||
| Working departments | ||||
| Pathological | 31.10 (3.51) | 30.10 (3.06) | 23.10 (1.97) | .001/.003/.005 |
| Surgical | 35.69 (6.84) | 25.73 (5.29) | 23.65 (6.44) | |
| Endoscopic/Gastroenterological | 37.54 (5.99) | 24.56 (5.49) | 26.69 (9.37) | |
| Emergency | 39.56 (6.08) | 27.08 (±6.39) | 19.89 (2.35) | |
| COVID unit | 35.13 (5.10) | 27.69 (5.09) | 21.84 (5.17) | |
| Other departments | 38.16 (5.20) | 25.32 (3.79) | 24.63 (6.54) | |
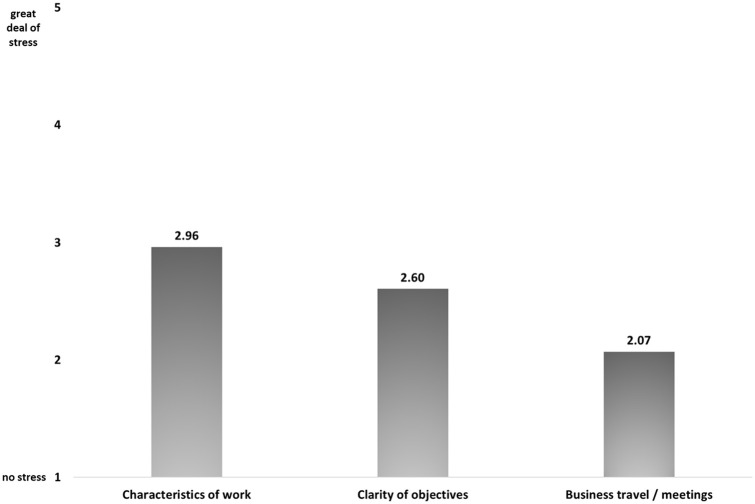
The mean value of job stress measure was 2.76 (±0.67) showing a moderate stress level among health professionals. More specifically, as shown in Figure 2, the characteristics of the working environment (2.96 ± 0.7) and clarity of objectives (2.60 ± 0.8) had a moderate impact on stress compared to business traveling or meetings (2.07 ± 0.7).
Figure 2.
Dimensions of job stress measure.
In Table 3, job stress measure with respect to the occupational characteristics of the participants is presented. Physicians were more likely to be stressed from their job and its characteristics compared to nurses (P = .004 and .002, respectively). Additionally, health professionals who came in contact with COVID-19 patients showed higher stress levels.
Table 3.
Comparisons between health professionals’ job stress measure and occupational characteristics.
| Job stress measure | Characteristics of work | Clarity of objectives | P value | |
|---|---|---|---|---|
| Mean (SD) | ||||
| Profession | ||||
| Physician | 2.93 (0.31) | 3.17 (0.34) | .004 | |
| Nurse | 2.65 (0.79) | 2.84 (0.85) | .002 | |
| Contact with COVID patients | ||||
| Yes | 2.80 (0.59) | 3.01 (0.63) | 2.64 (0.73) | .002/ |
| No | 2.28 (1.10) | 2.45 (1.29) | 2.25 (1.13) | .003/.05 |
Job stress and its dimensions are positively correlated with burnout and secondary traumatic stress (Table 4), showing that an increase in health professionals’ stress at work corresponds to a simultaneous increase in the above-mentioned ProQoL dimensions.
Table 4.
Correlation analysis among ProQoL dimensions and Job stress measure.
| Job stress measure | Characteristics of work | Clarity of objectives | Business travel or meetings | |
|---|---|---|---|---|
| Compassion satisfaction | −0.081 | −0.113 | 0.020 | −.0070 |
| Burnout | 0.461** | 0.497** | 0.290** | 0.258** |
| Secondary Traumatic Stress | 0.569** | 0.535** | 0.525** | 0.354** |
P < .01.
Finally, in order to investigate the factors that predict ProQol, linear regression analyses were conducted (Table 5). Significant models were found for CS (F[6, 179] = 35.818, P < .001, R2adj = 0.530), BO (F[4, 181] = 82.831, P < .001, R2adj = 0.639), STS (F[6, 179] = 28.847, P < .001, R2adj = 0.475).
Table 5.
Linear regression models for ProQol.
| 95% C.I. | ||||
|---|---|---|---|---|
| B | P value | Lower bound | Upper bound | |
| CS | ||||
| (Constant) | 47.052 | .001 | 42.414 | 51.689 |
| Number of children | 0.605 | .023 | 0.084 | 1.126 |
| BO | −0.935 | .001 | −1.076 | −0.793 |
| STS | 0.222 | .001 | 0.103 | 0.342 |
| BO | ||||
| (Constant) | 33.165 | .001 | 29.612 | 36.718 |
| CS | −0.493 | .001 | −0.568 | −0.418 |
| STS | 0.242 | .001 | 0.155 | 0.328 |
| Characteristics of work | 2.531 | .001 | 1.575 | 3.487 |
| STS | ||||
| (Constant) | −19.306 | .001 | −28.535 | −10.076 |
| Profession* | 3.696 | .001 | 2.165 | 5.226 |
| CS | 0.285 | .001 | 0.136 | 0.434 |
| BO | 0.568 | .001 | 0.367 | 0.77 |
| Characteristics of work | 1.572 | .050 | −0.04 | 3.184 |
| Business travel or meetings | 1.421 | .007 | 0.398 | 2.444 |
| Clarity of objectives | 1.441 | .034 | 0.108 | 2.775 |
Abbreviations: CS, Compassion Satisfaction; BO, Burnout, STS, Secondary traumatic stress.
Physician = 0, nurses = 1.
Discussion
To our knowledge, this is the first empirical study assessing the degree of stress emerging from the work environment and impacting health professionals’ ProQoL during the COVID-19 pandemic in Greece.
Our ProQoL results revealed that a high percentage of health professionals stated moderate CS, BO, and STS levels. This could be explained by their willingness to efficiently provide their services and the satisfaction they receive by offering them to people in need, especially during these stressful times. Gender, professional experience and educational level seem to be factors that significantly influence health professionals’ ProQoL. More specifically, women as well as health professionals with longer work experience indicated high CS levels, while those with higher education seemed to cope better with STS. Health professionals working in emergency and COVID-19 units were found to be more likely to report high levels in all ProQoL dimensions. Furthermore, physicians indicated higher levels of STS compared to nurses. This finding could be explained by comparing the responsibilities of the 2 groups of health professionals (physicians and nurses) as well as their exposure to extremely stressful events, such as the care of COVID-19 patients.
As concerns job stress, our results showed that health professionals felt moderate stress originating from hard working conditions, heavy workload and multiple responsibilities. This is an expected finding, given the fact that the Greek health care system has been recovering from a long lasting economic crisis43,45 and there are shortages in both human and financial resources. This status, in combination with the stressful conditions of the pandemic, brought ambiguity in the working roles of health professionals. Finally, it is worth mentioning that job stress was positively correlated with burnout and secondary traumatic stress.
The moderate levels in both CS and BO and the moderate and low levels in STS found in our study, may seem as a paradox concerning the interpretation of ProQoL. To explain this, the higher the level of CS is, the better the ProQoL, while the higher the level of BO and STS, the worse the ProQoL is. However, health professionals exposed to COVID-19 experienced both negative and positive psychological outcomes simultaneously. This contradiction could be explained by the fact that, during the coronavirus pandemic, health professionals were feeling exhausted from the workload and saddened by the unpredictable number of deaths but, at the same, they were satisfied with the services toward their patients, aiming to improve their health. Our findings are almost consistent with a study conducted by Cuartero-Castañer in the United States. 14 However, other studies in Spain, Italy and China19,24,48,49 showed that health professionals scored higher levels in the same dimensions. This could partly be explained by the early outbreak as well as the impact of COVID-19 in the aforementioned countries.
Moreover, several studies revealed that health professionals, who are providing care to COVID-19 patients in need of immediate admission and are on the frontline facing large numbers of deaths and managing high-risk procedures, were found to be more likely to report higher levels in all CS, BO and STS.50-52 Additionally, a study conducted in Greece reported that the prevalence of post-traumatic stress symptoms was high mainly in health professionals who are greatly exposed to the virus. 53 Furthermore, various international studies demonstrated an increase in negative psychological consequences relating to working conditions during the COVID-19 outbreak.54-56
Despite the fact that women are prone to develop depression, prior to 40 and during the pandemic, 12 our results showed high levels of CS in female health professionals. This finding is in accordance with 2 studies conducted by Dosil et al. 57 and Ozamiz-Etxebarria et al. in Spain, 58 however the latter only focused on the general population. This was an expected result given the social role that women have with respect to caregiving.24,59 Another similar finding is that health professionals indicate high levels of CS when they have long work experience. 60
An association between health professionals’ occupational stress and BO and STS has also been demonstrated by other researchers. This is a finding negatively impacting their ProQoL. There are numerous studies reporting that the pandemic exposes health professionals not only to biological factors, but also to occupational, social and other factors, thus making occupational stress a major public health issue.61,62 Various studies conducted prior to the COVID-19 outbreak, also reported that health professionals are prone to high levels of stress and consequently, to low levels of ProQoL.63,64
There are various measures which could be implemented in response to the health crisis such as, mobilizing the existing workforce, changing working patterns, calling on volunteers and non-governmental entities and recruiting health professionals. 65 Protecting their mental health and well-being through adequate training could also help in maintaining the health workforce and especially those who suffer from work exhaustion or psychological distress. Shorter work schedules, regular rest periods and rotating shifts for staff who work in high-risk environments can be considered. 66 Furthermore, support from colleagues and supervisors, clear communication of directives and precautionary measures can reduce psychiatric symptoms. 67
Apart from the above-mentioned managerial measures, mindfulness-based therapy could cultivate compassion and foster psychological resilience. This could ultimately enable professionals to cope with suffering and death and prevent burnout and work stress. 68 Additionally, online psychological interventions such as cognitive behavior therapy (CBT), enhancement of team spirit and praise of valuable outcomes could also work toward supporting and strengthening HPs well-being.66,69
Limitations
Evidence that has emerged from this study should be interpreted in light of some limitations. First, the data has been obtained from a cross-sectional design study, which did not determine the causality of the variables analyzed. Prospective longitudinal studies might inform on causal long-term effects of COVID-19 on health professionals. Moreover, a convenient sample was used in order to collect data in a timely manner regarding the COVID-19 outbreak. This makes it difficult to generalize results to the broader population of health professionals in Greece, despite the fact that participants are working in one of the largest general hospitals and COVID-19 reference units in the country. Thus, further investigations in larger scale studies should be performed to provide more representative findings. Also, the subjectivity and bias of the sample responses should be taken into consideration, due to the fact that the questionnaire was self-administered.
Conclusions
During the COVID-19 pandemic, professional quality of life and occupational stress of health professionals of the specific hospital seemed to be moderate and are associated with their socio-demographic and occupational characteristics. The higher the occupational stress, the higher the burnout and secondary traumatic stress. Our findings brought to light the necessity of decision makers’ immediate interventions aiming to support health professionals’ quality of life and strengthen the capacity of the healthcare system. Health professionals’ continuing education initiatives as well as strategies for coping with stress and psychological resilience, should be included in health systems’ internal control assessments. Furthermore, it would be useful to conduct in-depth research through face-to-face interviews with HPs and focus groups, with the aim to examine their needs and provide personalized and integrated support in times of crisis. Despite the psychological burden that the COVID-19 pandemic has brought to Greek health professionals, it is acknowledged that they remain the most valuable and compassionate resource addressing the COVID-19 outbreak.
Supplemental Material
Supplemental material, sj-docx-1-his-10.1177_11786329221096042 for Professional Quality of Life and Occupational Stress in Healthcare Professionals During the COVID-19 Pandemic in Greece by Dimitra Latsou, Fevronia-Maria Bolosi, Lorena Androutsou and Mary Geitona in Health Services Insights
Acknowledgments
We want to express our thanks to the staff and office of the General Hospital of Athens “Evangelismos,” for their support throughout this study.
Footnotes
Author Contributions: All authors contributed and provided input in the study design and data collection, analysis of the results and the writing of the manuscript.
Disclaimer: The information and views set out in this article are those of the author and do not necessarily reflect the official opinion of the European Commission.
Ethical Approval/Patient Consent: The study was approved by the Scientific Council of the “Evangelismos” hospital (protocol number 478/15.10.2020). Health professionals were informed about the aim of the study and their agreement for participation was requested, providing an informed verbal consent. The survey was voluntary and anonymous, with a withdrawal option at any stage. The questionnaires were collected in a closed envelope submitted to the secretariat of each department.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dimitra Latsou  https://orcid.org/0000-0002-9451-0102
https://orcid.org/0000-0002-9451-0102
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2020 (COVID-19) Situation Report—93. World Health Organization; 2020. Accessed August 28, 2021. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [Google Scholar]
- 2. Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. 2021;35:293-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19 – implications for the health care system. New Engl J Med. 2020;383:1483-1488. [DOI] [PubMed] [Google Scholar]
- 5. Androutsou L, Latsou D, Geitona M. Health Systems’ challenges and responses for recovery in the pre and post COVID-19 era. J Serv Sci Manag. 2021;14:444-460. [Google Scholar]
- 6. Geerts JM, Kinnair D, Taheri P, et al. Guidance for health care leaders during the recovery stage of the COVID-19 Pandemic. JAMA Netw Open. 2021;4:e2120295. [DOI] [PubMed] [Google Scholar]
- 7. Allain-Dupré D, Chatry I, Kornprobst A, et al. The Territorial Impact of COVID-19: Managing the Crisis Across Levels of Government. OECD Policy Responses to Coronavirus (COVID-19). 2021. Accessed September 15, 2021. https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/
- 8. Tran BX, Ha GH, Nguyen LH, et al. CM, Studies of novel Coronavirus Disease 19 (COVID-19) pandemic: a global analysis of Literature. Int J Environ Res Public Health. 2020;17:4095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, et al. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36:e00054020. [DOI] [PubMed] [Google Scholar]
- 10. Liu CH, Zhang E, Wong GT, Hyun S, Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Res. 2020;290:113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mendez-Lopez A, Stuckler D, McKee M, Semenza JC, Lazarus JV. The mental health crisis during the COVID-19 pandemic in older adults and the role of physical distancing interventions and social protection measures in 26 European countries. SSM Popul Health. 2022;17:101017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang C, Tee M, Roy AE, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16:e0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee Y, Lui LMW, Chen-Li D, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. 2021;290:364-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ceban F, Nogo D, Carvalho IP, et al. Association between Mood Disorders and risk of COVID-19 infection, hospitalization, and Death: a systematic review and meta-analysis. JAMA Psychiatr. 2021;78:1079-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chutiyami M, Cheong AMY, Salihu D, et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: a meta-review of Systematic Reviews. Front Psychiatry. 2021;12:804525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Halcomb E, McInnes S, Williams A, et al. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J Nurs Scholarsh. 2020;52:553-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323:2133-2134. [DOI] [PubMed] [Google Scholar]
- 19. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Carmona-Rega MI, Sánchez-Ruiz MJ, Ortega-Galán ÁM. Professional quality of life, self-compassion, resilience, and empathy in healthcare professionals during COVID-19 crisis in Spain. Res Nurs Health. 2021;44:620-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mahmud S, Hossain S, Muyeed A, Islam MM, Mohsin M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: a rapid systematic review and meta-analysis. Heliyon. 2021;7:e07393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cuartero-Castañer ME, Hidalgo-Andrade P, Cañas-Lerma AJ. Professional Quality of life, engagement, and self-care in healthcare professionals in Ecuador during the COVID-19 Pandemic. Healthcare. 2021;9:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ortega-Galán ÁM, Ruiz-Fernández MD, Lirola MJ, et al. Professional Quality of Life and Perceived Stress in Health Professionals Before COVID-19 in Spain: Primary and Hospital Care. Vol. 8. Healthcare (Basel); 2020:484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Roney LN, Acri MC. The cost of caring: an exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. J Pediatr Nurs. 2018;40:74-80. [DOI] [PubMed] [Google Scholar]
- 26. Stamm HB. Professional Quality of life: Compassion Satisfaction and Fatigue Version 5 (ProQOL). 2009. Accessed 20 August, 2020. www.proqol.org
- 27. Hegney DG, Craigie M, Hemsworth D, et al. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J Nurs Manag. 2014;22:506-518. [DOI] [PubMed] [Google Scholar]
- 28. Yadollahi M, Razmjooei A, Jamali K, Niakan MH, Ghahramani Z. The relationship between professional quality of life (ProQol) and general health in Rajaee Trauma Hospital staff of shiraz, Iran. Shiraz E Medical J. 2016;17:e39253. [Google Scholar]
- 29. Zhang YY, Han WL, Qin W, et al. Extent of compassion satisfac-tion, compassion fatigue and burnout in nursing: A meta-analysis. J Nurs Manag. 2018;26:810-819. [DOI] [PubMed] [Google Scholar]
- 30. Amin AA, Vankar JR, Nimbalkar SM, Phatak AG. Perceived stress and professional quality of life in neonatal intensive care unit nurses in Gujarat, India. Indian J Pediatr. 2015;82:1001-10015. [DOI] [PubMed] [Google Scholar]
- 31. Alyahya S, AboGazalah F. Work-related stressors among the healthcare professionals in the fever clinic centers for individuals with symptoms of COVID-19. Healthcare. 2021;9:548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Al-Omar B. Sources of work-stress among hospital-staff at the Saudi MOH. J King Abdulaziz Univ-Econ Adm. 2003;17:3-16. [Google Scholar]
- 33. Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int. 2021;28:8791-8801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Huang Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211-224. [DOI] [PubMed] [Google Scholar]
- 35. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chua SE, Cheung V, Cheung C, et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391-393. [DOI] [PubMed] [Google Scholar]
- 37. Poon E, Liu KS, Cheong DL, Lee CK, Yam LY, Tang WN. Impact of severe respiratory syndrome on anxiety levels of front-line health care workers. Hong Kong Med J. 2004;10:325-330. [PubMed] [Google Scholar]
- 38. Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Longterm psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245-1251. [PMC free article] [PubMed] [Google Scholar]
- 40. Su T, Lien T, Yang C, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007;41:119-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Giannoglou D, Meimeti E, Provatopoulou X, et al. Predictors of mortality in hospitalized COVID-19 patients in Athens. Iran Red Crescent Med J. 2020. [Google Scholar]
- 42. Worldometers.info. 2021; Accessed 15 December 2021. https://www.worldometers.info/coronavirus/country/greece/
- 43. Geitona M. Assessing the value of medicinal innovation in an era of increasing austerity. Soc Cohes Dev. 2016;7:39-51. [Google Scholar]
- 44. Economou C, Kaitelidou D, Kentikelenis A, et al. The Impact of the Crisis on the Health System and Health in Greece. In Economic Crisis, Health Systems and Health in Europe: Country Experience. European Observatory on Health Systems and Policies. 2014; Accessed 15 November 2021. https://www.euro.who.int/__data/assets/pdf_file/0010/279820/Web-economic-crisis-health-systems-and-health-web.pdf [Google Scholar]
- 45. Souliotis K, Papadonikolaki J, Papageorgiou M, et al. The impact of crisis on health and health care: thoughts and data on the Greek case. Arch Hell Med. 2018;35:9-16. [Google Scholar]
- 46. Professional Quality of Life Scale (ProQOL) Version 5 (2009). Professional Quality of Life. Accessed August 20, 2020. https://proqol.org/proqol-measure
- 47. Sakketou A, Galanakis M, Varvogli L, Chrousos G, Darviri C. Validation of the Greek version of the “Job Stress Measure”. Psychology. 2014;05:1527-1535. [Google Scholar]
- 48. Buselli R, Corsi M, Baldanzi S, et al. Professional quality of life and mental health outcomes among health care workers exposed to Sars-Cov-2 (Covid-19). Int J Environ Res Public Health. 2020;17:6180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Li WW, West C, Xie G. The reflective risk assessment model of professional quality of life in Chinese nurses. J Nurs Manag. 2021;29:767-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wallace CL, Wladkowski SP, Gibson A, White P. Grief during the COVID-19 pandemic: considerations for palliative care providers. J Pain Symptom Manag. 2020;60:e70-e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Doherty M., Hauser J. Care of the dying patient. In: Waldman E, Glass M. eds. A Field Manual for Palliative Care in Humanitarian Crises. Oxford University Press; 2019;1-17. [Google Scholar]
- 52. Yin Q, Sun Z, Liu T, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. 2020;27:384-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Blekas A, Voitsidis P, Athanasiadou M, et al. COVID-19: PTSD symptoms in Greek health care professionals. Psychol Trauma Theory Res Pract Policy. 2020;12:812-819. [DOI] [PubMed] [Google Scholar]
- 54. Giusti EM, Pedroli E, D’Aniello GE, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ng QX, De Deyn MLZQ, Lim DY, Chan HW, Yeo WS. The wounded healer: A narrative review of the mental health effects of the COVID-19 pandemic on healthcare workers. Asian J Psychiatr. 2020;54:102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nochaiwong S, Ruengorn C, Awiphan R, et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine. 2020;99:e20751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dosil M, Ozamiz-Etxebarria N, Redondo I, Picaza M, Jaureguizar J. Psychological symptoms in health professionals in Spain after the first wave of the COVID-19 pandemic. Front Psychol. 2020;11:606121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ozamiz-Etxebarria N, Idoiaga Mondragon N, Dosil Santamaría M, Picaza Gorrotxategi M. Psychological symptoms during the two stages of lockdown in response to the covid-19 outbreak: an investigation in a sample of citizens in northern Spain. Front Psychol. 2020;11:1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Portero de la Cruz S, Cebrino J, Herruzo J, Vaquero-Abellán M. A multicenter study into burnout, perceived stress, job satisfaction, coping strategies, and General Health among Emergency Department Nursing Staff. J Clin Med. 2020;9:1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Billings J, Ching BCF, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res. 2021;21:923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Orsini A, Corsi M, Santangelo A, et al. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurol Sci. 2020;41:2353-2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Buselli R, Carmassi C, Corsi M, et al. Post-traumatic stress symptoms in an Italian cohort of subjects complaining occupational stress. CNS Spectr. 2021;26:513-520. [DOI] [PubMed] [Google Scholar]
- 63. Dolan SL, Ameringen MR, Corbin S, Arsenault A. Lack of professional latitude and role problems as correlates of propensity to quit amongst nursing staff. J Adv Nurs. 1992;17:1455-1459. [DOI] [PubMed] [Google Scholar]
- 64. Mosadeghrad AM, Ferlie E, Rosenberg D. A study of relationship between job stress, quality of working life and turnover intention among hospital employees. Health Serv Manage Res. 2011;24:170-181. [DOI] [PubMed] [Google Scholar]
- 65. World Health Organization. Regional Office for Europe. Strengthening the Health Systems Response to COVID-19: Technical Guidance #2: Creating Surge Capacity for Acute and Intensive Care. WHO; 2020. https://apps.who.int/iris/handle/10665/332562 [Google Scholar]
- 66. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of Coronavirus Disease 2019 (COVID-19) beyond paranoia and panic. Ann Acad Med Singap. 2020;49:155-160. [PubMed] [Google Scholar]
- 67. Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. 2004;54:190-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Duarte J, Pinto-Gouveia J, Cruz B. Relationships between nurses’ empathy, self-compassion and dimensions of professional quality of life: a cross-sectional study. Int J Nurs Stud. 2016;60:1-11. [DOI] [PubMed] [Google Scholar]
- 69. Frenkel MO, Pollak KM, Schilling O, et al. Stressors faced by healthcare professionals and coping strategies during the early stage of the COVID-19 pandemic in Germany. PLoS One. 2022;17:e0261502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-his-10.1177_11786329221096042 for Professional Quality of Life and Occupational Stress in Healthcare Professionals During the COVID-19 Pandemic in Greece by Dimitra Latsou, Fevronia-Maria Bolosi, Lorena Androutsou and Mary Geitona in Health Services Insights