Abstract
BACKGROUND
Depression is the most common type of depressive disorder. The most common sleep disorder associated with depression is insomnia. Insomnia and depression are closely related.
AIM
To investigate the relationship of designed questionnaire items and depression, and analyze the related factors with depression.
METHODS
Questionnaire included Patient Health Questionnaire-9 (PHQ-9) and Pittsburgh sleep quality index (PSQI), 12 kinds of diseases, 8 general characteristics, and 20 insomnia characteristics, totally 56 items were filled out by 411 patients enrolled.
RESULTS
All the 9 items of PHQ-9, 6 components of PSQI (except sleep duration), education, living situation, exercise, years of insomnia, western medicine treatment, Chinese medicine treatment, psychotherapy, kinds of insomnia, treatment expected to treat insomnia, psychological counseling, habit of 1 h before bed, habit of lunch break, diagnosed depression, coronary heart disease, mental illness showed significant difference between without and with depression group. By univariate analysis and multivariate analysis. The odds ratio of education, exercise, kinds of insomnia, habit of 1 h before bed, diagnosed depression, coronary heart disease (P = 0.01) showed significant difference. Their odds ratios were 0.71 (0.55, 0.93), 2.09 (1.32, 3.31), 0.76 (0.63, 0.91), 0.89 (0.81, 0.98), 0.32 (0.17, 0.60), 0.43 (0.23, 0.79).
CONCLUSION
We demonstrated that education, exercise, kinds of insomnia, habit of 1 h before bed, diagnosed depression and coronary heart disease affect the depression.
Keywords: Depression, Patient Health Questionnaire-9, Pittsburgh sleep quality index, Sleep, Insomnia
Core Tip: Depression is the most common type of depressive disorder, manifesting as single or repeated episodes, with a high risk of recurrence. Depression affects the functions of the energy and digestive system and can also lead to varying degrees of sleep difficulties, insomnia, sleep arousal and other sleep disorders. In this study, we aimed to evaluate the related factor with depression, to provide theoretical support for detection and depression therapy.
INTRODUCTION
Depression is the most common type of depressive disorder, manifesting as single or repeated episodes, with a high risk of recurrence. There can be significant emotional, cognitive, and physical symptoms during episodes, and symptoms can resolve between episodes[1]. The main clinical manifestation is depression, which is not commensurate with the situation. It can range from sullenness to grief and even stupor. Some patients will have obvious anxiety and motor agitation. In severe cases, psychotic symptoms such as hallucinations and delusions may occur. Some patients suffer from self-injury, suicidal behavior, and even death[2]. With the accelerating pace of society, study pressure, work pressure, and life pressure increase, and the incidence of depression shows a significant upward trend. Depression has become the most important cause of the ten causes of disability-adjusted life years in every country in the world. The lifetime prevalence of depression is estimated to be 5% among adults[3,4]. Depressive disorders have a high prevalence and high disease burden, but the treatment rates are low, with less than 10% of these patients receiving effective treatment in many countries; however, the medical prevention and treatment of depression in China still has a low recognition rate[5]. Hospitals above the prefecture-level city have a recognition rate of less than 20%, and less than 10% of patients receive relevant drug treatment. At the same time, the incidence of depression has begun to show a trend of younger age (college and even primary and secondary school students). The popularization, prevention and treatment of depression need urgent attention[6].
Depression affects the functions of the energy and digestive system and can also lead to varying degrees of sleep difficulties, insomnia, sleep arousal and other sleep disorders. Changes in sleep are one of the diagnostic criteria for depression. The probability of sleep disturbance in patients with depression is as high as 70%, which manifests as insomnia, lethargy, nightmares and disturbance of the sleep-wake cycle[7]. The most common sleep disorder associated with depression is insomnia. Insomnia and depression are closely related and share a bidirectional relationship with each other[8]. Insomnia is a demonstrated and a relative risk factor for depression. Treatment can improve or prevent major depressive episodes. The early identification of insomnia may also improve the outcomes of depression[9]. Insomnia and depression are heterogeneous processes, and the diagnostic components of insomnia and depression are likely to lead to translational progress at their nexus[10,11]. Studies have shown that poor sleep quality can lead to a decline in executive function, making it difficult to avoid negative thoughts, increasing nighttime unpleasantness, and triggering rumination, and repeated negative thoughts lead to increased suicide risk. In addition to insomnia, depressive patients may also experience somnolence during the course of the disease. Approximately 7%-8% of patients with major depressive disorder have somnolence and excessive sleep time, and approximately 25% of patients have both insomnia and somnolence[12]. More severe depression has now been shown to be associated with higher rates of substance use disorder and suicide attempts[13]. In addition, general characteristics, such as marital status and smoking, can affect subjective sleep quality. The relationship between marital status and sleep in women with depression showed that marital status was related to sleep efficiency. Married women had better sleep quality and significantly lower sleep delay than unmarried women. Compared with divorced or widowed patients, married depressed patients had better sleep quality; the stress of marriage breakdown and the loss of a partner had an important impact on sleep, and the occurrence of an unhappy marriage and depressive symptoms caused changes in physical function, causing alcoholism and lack of sleep[14]. Smokers were reported to have more severe sleep problems than nonsmokers. Nicotine patches led to abnormal sleep, a lack of sleep, shortened sleep latency, and reduced nighttime sleep[15].
In our study, by the questionnaire designed by our team, which included a total of 56 items, we aimed to investigate the relationship between the designed questionnaire items and depression and analyze the factors related to depression.
MATERIALS AND METHODS
Study subjects
With written informed consent, this study was approved by the Fuxing Hospital affiliated with the Capital Medical University Institution Review Board. A total of 424 patients with insomnia in Yuetan Community Health Service Center and its subordinate community health service stations were enrolled as the research subjects in our study. Thirteen patients were excluded because they did not have a qualified questionnaire. Finally, 411 patients were included for further analysis. The inclusion criteria included the following items: (1) Patients who met the diagnostic points of nonorganic insomnia: their main complaints were difficulty falling asleep, difficulty maintaining sleep, or poor sleep quality; this sleep disorder occurred at least three times a week and lasted for one month or more. Focusing on sleep day and night, worrying too much about the consequences of insomnia, and dissatisfaction with sleep quantity and/or quality causes obvious distress or affects social and occupational functions. This criterion was met as long as dissatisfaction with the quantity and/or quality of sleep was the patient's only complaint; (2) Patients who had contacted their family doctor; and (3) Patients aged between 40 and 70 years old. The exclusion criteria included the following items: (1) Patients with insomnia as only one of multiple symptoms of a mental disorder or physical condition were excluded; insomnia was limited to the main mental or physical disorder; and (2) Patients with severe mental disorder were excluded.
The Patient Health Questionnaire-9 (PHQ-9) and the Pittsburgh Sleep Quality Index (PSQI) were included in our questionnaires. In addition, the questionnaires also included 12 kinds of diseases, including diagnosed depression, chronic diseases, high blood pressure, diabetes, coronary heart disease, cerebrovascular disease, enlarged prostate, cancer, mental illness, tuberculosis, chronic hepatitis, and cirrhosis. Eight general characteristics, including sex, age, education level, marital status, living situation, occupational status, income (yuan) per month and exercise, were analyzed. The percentage of sex, education level, marital status, living situation, occupational status, income (yuan) per month and exercise. The 20 insomnia characteristics included the following: years of insomnia; Western medicine treatmen; Chinese medicine treatment; psychotherapy; kind of insomnia; events related to insomnia; treatment expected to treat insomnia; traditional Chinese medicine foot baths; acupressure; psychological counseling; medicated diet; Tai Chi; traditional Chinese medicine; other traditional Chinese medicines; habit of 1 h before bed; habit of drinking tea; habit of drinking coffee; habit of drinking spirits; habit of smoking; and habit of taking a lunch break.
Survey method and quality control
Questionnaires designed by our study team were distributed to respondents by uniformly trained investigators, and the relevant contents of the questionnaires were explained to the respondents face-to-face. Then, the questionnaires were investigated and completed. After taking back the questionnaires, unqualified questionnaires with missing items were eliminated, and valid questionnaires were sorted and numbered. Quality control was carried out at the stages of data collection, data collation and result analysis. The questionnaires were completed by trained investigators instructing the subjects one-on-one. Data were entered and reviewed by trained personnel to ensure the accuracy of data entry.
Depression severity degree assessed by the PHQ-9
The PHQ-9 consists of 9 items as follows: "little interest or pleasure in doing things”; “feeling down, depressed, or hopeless”; “trouble falling or staying asleep, or sleeping too much”; “feeling tired or having little energy”; “poor appetite or overeating”; “feeling bad about yourself or that you are a failure or have let yourself or your family down”; “trouble concentrating on things, such as reading the newspaper or watching television”; “moving or speaking so slowly that other people could have noticed or being so fidgety or restless that you have been moving a lot more than usual”; and “thoughts that you would be better off dead, or thoughts of hurting yourself in some way”. This questionnaire was used to evaluate depression and grade the severity of symptoms[16]. Higher PHQ-9 scores are related to decreased functional status and increased symptom-related difficulties. A PHQ-9 score of 0–4 represents no depression. Scores of 5–9 represent mild depression, 10–14 represent moderate depression, and 15–19 represent moderately severe depression. Scores of 20–27 represent severe depression.
Sleep quality assessed by the PSQI
The PSQI was used to assess the sleep quality of the subjects in the last month. It consists of 19 self-assessment items and 5 other assessment items, of which the 19th self-assessment item and the 5 other assessment items are not included in the scoring. Only the remaining 18 self-assessment items are included in the scoring. The 18 items consist of the following 7 components: subjective sleep, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction; each component is scored on a scale of 0 to 3. The cumulative score of each component is the total PSQI score, and the total score ranges from 0 to 21. The higher the score, the worse the sleep quality. It took the subjects 5 to 10 minutes to complete the questionnaire. Scores of 0–5 represent that sleep quality is very good; scores of 6–10 represents that sleep quality is okay; scores of 11–15 represent that sleep quality is average; and scores of 16–21 represent that sleep quality is poor[17].
Statistical analysis
SPSS 22.0 was used for data analysis. Excel and GraphPad Prism were used to draw the figures. Measurement data are expressed as the mean ± SD. Count data are expressed as n (%). The measurement data that conformed to a normal distribution were compared by two independent sample t tests or analysis of variance; the measurement data that did not conform to a normal distribution were compared by the rank sum test. Count data were compared by the χ2 test. Principal component analysis (PCA) was used to analyze the contributing rate to depression. The correlation between the 9 PHQ-9 items was analyzed by Pearson correlation regression. Univariate and multivariate logistic regression was used to analyze the factors significantly associated with depression. A P < 0.05 was considered a statistically significant difference.
RESULTS
Relationship of the PHQ-9 items and depression
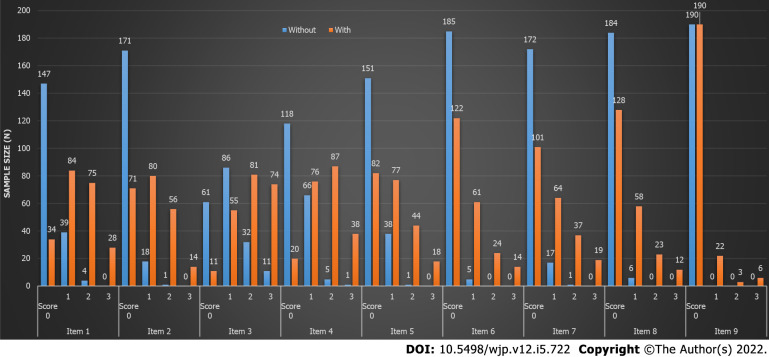
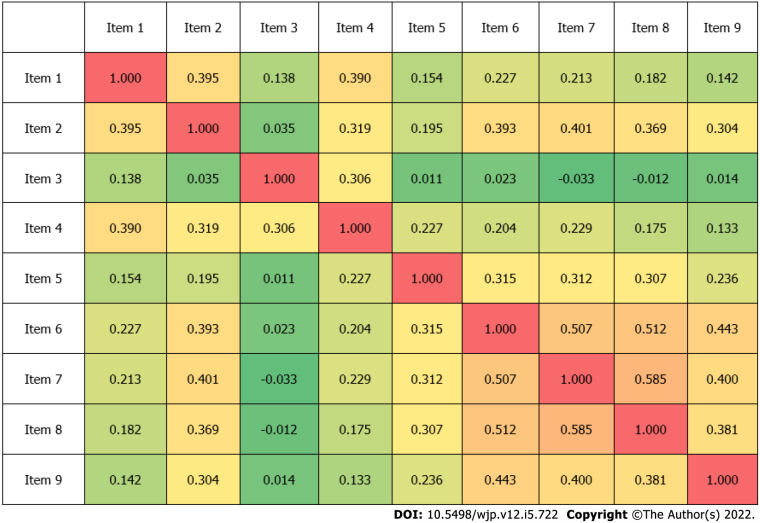
According to their PHQ-9 scores, the individuals enrolled in our study were divided into a without depression group (n = 190) and a depression group (n = 221), which included mild (n = 139), moderate (n = 49), moderately severe (n = 22), and severe depression (n = 11). First, the 9 items, including “little interest or pleasure in doing things” (Item 1), “feeling down, depressed, or hopeless” (Item 2), “trouble falling or staying asleep, or sleeping too much” (Item 3), “feeling tired or having little energy” (Item 4), “poor appetite or overeating” (Item 5), “feeling bad about yourself or that you are a failure or have let yourself or your family down” (Item 6), “trouble concentrating on things, such as reading the newspaper or watching television” (Item 7), “moving or speaking so slowly that other people could have noticed, or so fidgety or restless that you have been moving a lot more than usual” (Item 8), and “thoughts that you would be better off dead, or thoughts of hurting yourself in some way” (Item 9), were compared between the without depression group and with depression group. As shown in Figure 1, the 9 items in the without depression group and with depression group were compared, and all 9 items showed significant differences (P < 0.001). Then, the 9 items were compared for the mild depression, moderate depression, moderately severe depression, and severe depression groups, as shown in Table 1. All 9 items also showed significant differences (P < 0.001). PCA was used to analyze the 9 items contributing to depression. As shown in Figure 2, the contributing rates of Items 1-9 were 36.00%, 15.59%, 9.96%, 9.09%, 7.32%, 6.18%, 5.94%, 5.40% and 4.53%, respectively. This item contributed the most to the depression analysis. In addition, the correlation coefficients of the 9 items were also analyzed. As shown in Figure 3, Item 7 and Item 8 showed the highest positive correlation coefficient, which was 0.585, but Item 7 and Item 3 showed the highest negative correlation coefficient, which was -0.033.
Figure 1.
Comparison of the 9 items of Patient Health Questionnaire-9 in the without depression group and with depression group.
Table 1.
Relationship of Patient Health Questionnaire-9 items and depression
|
PHQ-9 item
|
Score
|
Mild (n = 139)
|
Moderate (n = 49)
|
Moderately severe (n = 22)
|
Severe (n = 11)
|
||||
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
||
| Item 1 | 0 | 32 | 23.02 | 2 | 4.08 | 0 | 0.00 | 0 | 0.00 |
| 1 | 67 | 48.20 | 11 | 22.45 | 5 | 22.73 | 1 | 9.09 | |
| 2 | 36 | 25.90 | 27 | 55.10 | 10 | 45.45 | 2 | 18.18 | |
| 3 | 4 | 2.88 | 9 | 18.37 | 7 | 31.82 | 8 | 72.73 | |
| Item 2 | 0 | 62 | 44.60 | 8 | 16.33 | 1 | 4.55 | 0 | 0.00 |
| 1 | 62 | 44.60 | 14 | 28.57 | 4 | 18.18 | 0 | 0.00 | |
| 2 | 15 | 10.79 | 24 | 48.98 | 14 | 63.64 | 3 | 27.27 | |
| 3 | 0 | 0.00 | 3 | 6.12 | 3 | 13.64 | 8 | 72.73 | |
| Item 3 | 0 | 10 | 7.19 | 0 | 0.00 | 0 | 0.00 | 1 | 9.09 |
| 1 | 41 | 29.50 | 12 | 24.49 | 2 | 9.09 | 0 | 0.00 | |
| 2 | 52 | 37.41 | 19 | 38.78 | 9 | 40.91 | 1 | 9.09 | |
| 3 | 36 | 25.90 | 18 | 36.73 | 11 | 50.00 | 9 | 81.82 | |
| Item 4 | 0 | 17 | 12.23 | 3 | 6.12 | 0 | 0.00 | 0 | 0.00 |
| 1 | 66 | 47.48 | 9 | 18.37 | 1 | 4.55 | 0 | 0.00 | |
| 2 | 48 | 34.53 | 28 | 57.14 | 10 | 45.45 | 1 | 9.09 | |
| 3 | 8 | 5.76 | 9 | 18.37 | 11 | 50.00 | 11 | 100.00 | |
| Item 5 | 0 | 69 | 49.64 | 10 | 20.41 | 3 | 13.64 | 0 | 0.00 |
| 1 | 49 | 35.25 | 20 | 40.82 | 5 | 22.73 | 3 | 27.27 | |
| 2 | 19 | 13.67 | 17 | 34.69 | 7 | 31.82 | 1 | 9.09 | |
| 3 | 2 | 1.44 | 2 | 4.08 | 7 | 31.82 | 7 | 63.64 | |
| Item 6 | 0 | 102 | 73.38 | 16 | 32.65 | 2 | 9.09 | 2 | 18.18 |
| 1 | 32 | 23.02 | 24 | 48.98 | 5 | 22.73 | 0 | 0.00 | |
| 2 | 4 | 2.88 | 9 | 18.37 | 10 | 45.45 | 1 | 9.09 | |
| 3 | 1 | 0.72 | 0 | 0.00 | 5 | 22.73 | 8 | 72.73 | |
| Item 7 | 0 | 85 | 61.15 | 15 | 30.61 | 1 | 4.55 | 0 | 0.00 |
| 1 | 44 | 31.65 | 17 | 34.69 | 2 | 9.09 | 1 | 9.09 | |
| 2 | 9 | 6.47 | 14 | 28.57 | 12 | 54.55 | 2 | 18.18 | |
| 3 | 1 | 0.72 | 3 | 6.12 | 7 | 31.82 | 8 | 72.73 | |
| Item 8 | 0 | 105 | 75.54 | 17 | 34.69 | 6 | 27.27 | 0 | 0.00 |
| 1 | 28 | 20.14 | 25 | 51.02 | 5 | 22.73 | 0 | 0.00 | |
| 2 | 5 | 3.60 | 6 | 12.24 | 9 | 40.91 | 3 | 27.27 | |
| 3 | 1 | 0.72 | 1 | 2.04 | 2 | 9.09 | 8 | 72.73 | |
| Item 9 | 0 | 134 | 96.40 | 40 | 81.63 | 13 | 59.09 | 3 | 27.27 |
| 1 | 5 | 3.60 | 7 | 14.29 | 5 | 22.73 | 5 | 45.45 | |
| 2 | 0 | 0.00 | 2 | 4.08 | 2 | 9.09 | 1 | 9.09 | |
| 3 | 0 | 0.00 | 0 | 0.00 | 2 | 9.09 | 2 | 18.18 | |
PHQ-9: Patient Health Questionnaire-9.
Figure 2.
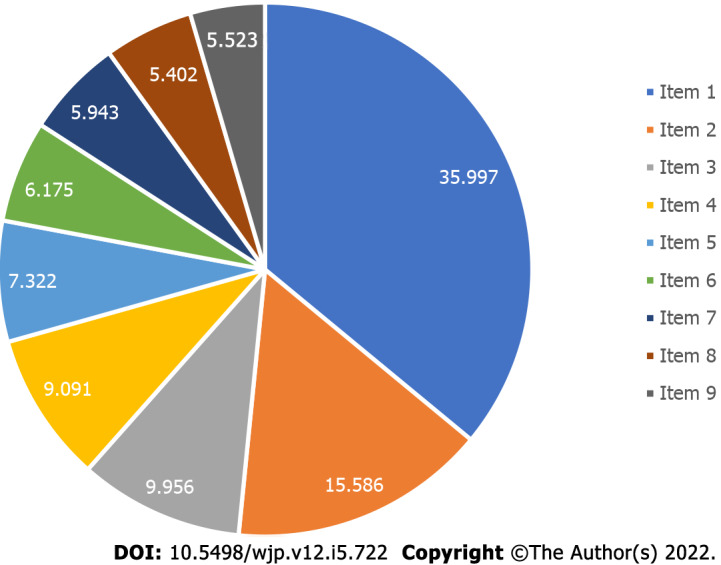
The contributing rate of 9 items of Patient Health Questionnaire-9 to depression (%).
Figure 3.
The correlation coefficient of the 9 items of Patient Health Questionnaire-9.
Relationship of the PSQI components and depression
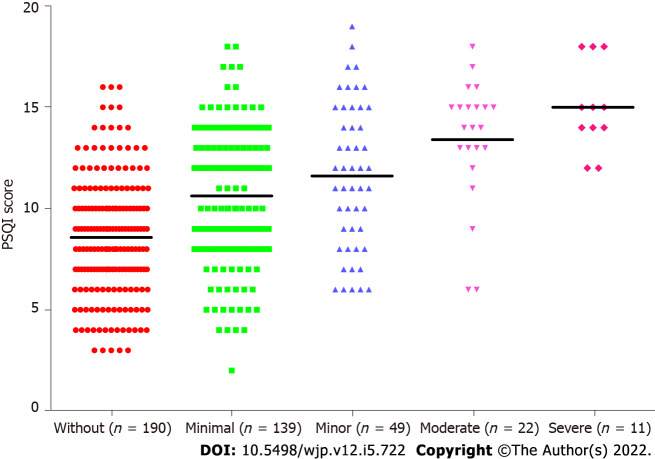
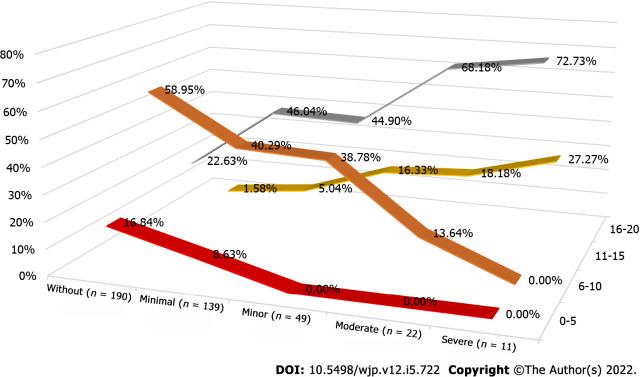
As shown in Table 2, the 7 PSQI components, which were subjective sleep, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction, were compared for the without depression group (n = 190) and the with depression group (n = 221), which included mild (n = 139), moderate (n = 49), moderately severe (n = 22), and severe depression (n = 11). After comparison, subjective sleep (P < 0.001), sleep latency (P < 0.001), habitual sleep efficiency (P = 0.001), sleep disturbances (P < 0.001), use of sleep medications (P = 0.001), and daytime dysfunction (P < 0.001) showed significant differences between the depression groups; however, sleep duration showed no significant difference (P = 0.054). As shown in Figure 4, the mean PSQI scores in the without depression group (n = 190), mild depression group (n = 139), moderate depression group (n = 49), moderately severe depression group (n = 22), and severe depression group (n = 11) were 8.58, 10.63, 11.61, 13.41 and 15.00, respectively. With the progression of depression severity, the PSQI score also showed a significant increase (P < 0.001). In addition, the degrees of depression for the very good sleep quality (0-5), okay sleep quality (6-10), average sleep quality (11-15), and poor sleep quality (16-21) groups were also analyzed. As shown in Figure 5, for the 0–5 and 6–10 sleep quality groups, the percentages of the without depression group (n = 190), mild depression group (n = 139), moderate depression group (n = 49), moderately severe depression group (n = 22), and severe depression group (n = 11) were 16.84%, 8.63%, 0%, 0%, 0% and 58.95%, 40.29%, 38.78%, 13.64%, 0%, respectively. The percentage of depression degree de-escalated. In the 11–15 and 16–20 sleep quality groups, the percentages of the without depression group (n = 190), mild depression group (n = 139), moderate depression group (n = 49), moderately severe depression group (n = 22), and severe depression group (n = 11) were 1.58%, 5.04%, 16.33%, 18.18%, 27.27% and 22.63%, 46.04%, 44.90%, 68.18%, 72.73%, respectively. The percentage of depression degree escalated.
Table 2.
Relationship of Pittsburgh sleep quality index components and depression
|
PSQI index
|
Score
|
Without (n = 190)
|
With (n = 221)
|
Mild (n = 139)
|
Moderate (n = 49)
|
Moderately severe (n = 22)
|
Severe (n = 11)
|
||||||
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
n
|
Percent
|
||
| Subjective sleep quality | 0 | 0 | 0.00 | 3 | 1.36 | 2 | 1.44 | 1 | 2.04 | 0 | 0.00 | 0 | 0.00 |
| 1 | 87 | 45.79 | 27 | 12.22 | 22 | 15.83 | 4 | 8.16 | 1 | 4.55 | 0 | 0.00 | |
| 2 | 94 | 49.47 | 146 | 66.06 | 94 | 67.63 | 33 | 67.35 | 11 | 50.00 | 8 | 72.73 | |
| 3 | 9 | 4.74 | 45 | 20.36 | 21 | 15.11 | 11 | 22.45 | 10 | 45.45 | 3 | 27.27 | |
| Sleep latency | 0 | 9 | 4.74 | 8 | 3.62 | 3 | 2.16 | 4 | 8.16 | 1 | 4.55 | 0 | 0.00 |
| 1 | 52 | 27.37 | 31 | 14.03 | 23 | 16.55 | 5 | 10.20 | 3 | 13.64 | 0 | 0.00 | |
| 2 | 77 | 40.53 | 69 | 31.22 | 45 | 32.37 | 13 | 26.53 | 8 | 36.36 | 3 | 27.27 | |
| 3 | 52 | 27.37 | 113 | 51.13 | 68 | 48.92 | 27 | 55.10 | 10 | 45.45 | 8 | 72.73 | |
| Sleep duration | 0 | 46 | 24.21 | 39 | 17.65 | 27 | 19.42 | 6 | 12.24 | 4 | 18.18 | 2 | 18.18 |
| 1 | 62 | 32.63 | 68 | 30.77 | 42 | 30.22 | 19 | 38.78 | 4 | 18.18 | 3 | 27.27 | |
| 2 | 59 | 31.05 | 60 | 27.15 | 39 | 28.06 | 13 | 26.53 | 8 | 36.36 | 0 | 0.00 | |
| 3 | 23 | 12.11 | 54 | 24.43 | 31 | 22.30 | 11 | 22.45 | 6 | 27.27 | 6 | 54.55 | |
| Habitual sleep efficiency | 0 | 64 | 33.68 | 48 | 21.72 | 34 | 24.46 | 10 | 20.41 | 3 | 13.64 | 1 | 9.09 |
| 1 | 44 | 23.16 | 42 | 19.00 | 27 | 19.42 | 10 | 20.41 | 4 | 18.18 | 1 | 9.09 | |
| 2 | 41 | 21.58 | 48 | 21.72 | 28 | 20.14 | 12 | 24.49 | 4 | 18.18 | 4 | 36.36 | |
| 3 | 41 | 21.58 | 83 | 37.56 | 50 | 35.97 | 17 | 34.69 | 11 | 50.00 | 5 | 45.45 | |
| Sleep disturbances | 0 | 3 | 1.58 | 2 | 0.90 | 1 | 0.72 | 1 | 2.04 | 0 | 0.00 | 0 | 0.00 |
| 1 | 154 | 81.05 | 135 | 61.09 | 99 | 71.22 | 25 | 51.02 | 8 | 36.36 | 3 | 27.27 | |
| 2 | 32 | 16.84 | 79 | 35.75 | 37 | 26.62 | 22 | 44.90 | 13 | 59.09 | 7 | 63.64 | |
| 3 | 1 | 0.53 | 5 | 2.26 | 2 | 1.44 | 1 | 2.04 | 1 | 4.55 | 1 | 9.09 | |
| Use of sleeping medications | 0 | 85 | 44.74 | 90 | 40.72 | 63 | 45.32 | 19 | 38.78 | 6 | 27.27 | 2 | 18.18 |
| 1 | 28 | 14.74 | 15 | 6.79 | 9 | 6.47 | 4 | 8.16 | 1 | 4.55 | 1 | 9.09 | |
| 2 | 43 | 22.63 | 40 | 18.10 | 32 | 23.02 | 8 | 16.33 | 0 | 0.00 | 0 | 0.00 | |
| 3 | 34 | 17.89 | 76 | 34.39 | 35 | 25.18 | 18 | 36.73 | 15 | 68.18 | 8 | 72.73 | |
| Daytime dysfunction | 0 | 161 | 84.74 | 94 | 42.53 | 71 | 51.08 | 18 | 36.73 | 5 | 22.73 | 0 | 0.00 |
| 1 | 27 | 14.21 | 84 | 38.01 | 53 | 38.13 | 18 | 36.73 | 9 | 40.91 | 4 | 36.36 | |
| 2 | 2 | 1.05 | 37 | 16.74 | 14 | 10.07 | 12 | 24.49 | 6 | 27.27 | 5 | 45.45 | |
| 3 | 0 | 0.00 | 6 | 2.71 | 1 | 0.72 | 1 | 2.04 | 2 | 9.09 | 2 | 18.18 | |
PSQI: Pittsburgh sleep quality index.
Figure 4.
The mean Pittsburgh sleep quality index score. The mean Pittsburgh sleep quality index score in the without depression group (n = 190), mild (n = 139), moderate (n = 49), moderately severe depression (n = 22), and severe depression (n = 11) was 8.58, 10.63, 11.61, 13.41 and 15.00. PSQI: Pittsburgh sleep quality index.
Figure 5.
The percentage of Pittsburgh sleep quality index group. The percentage of Pittsburgh sleep quality index group in without depression group (n = 190), mild (n = 139), moderate (n = 49), moderately severe depression (n = 22), and severe depression (n = 11).
Comparison of disease status between the without depression and with depression groups
As shown in Table 3, the disease status of the without depression and with depression groups was analyzed. Twelve kinds of diseases, including diagnosed depression, chronic diseases, high blood pressure, diabetes, coronary heart disease, cerebrovascular disease, enlarged prostate, cancer, mental illness, tuberculosis, chronic hepatitis, and cirrhosis, were compared between the without depression and with depression groups. Diagnosed depression (P < 0.001), coronary heart disease (P = 0.03), and mental illness (P = 0.01) showed significant differences between the two groups. The percentages of diagnosed depression in the without depression and with depression groups were 8.95% and 23.53%, respectively. The percentages of coronary heart disease and mental illness in the two groups were 11.05% and 19.00%, and 0.53% and 5.43%, respectively. The other 9 kinds of diseases, including chronic diseases, high blood pressure, diabetes, cerebrovascular disease, enlarged prostate, cancer, tuberculosis, chronic hepatitis, and cirrhosis, showed no significant differences (P > 0.05).
Table 3.
Comparison of diseases status between without depression and with depression groups, n (%)
|
Diseases
|
Status
|
Without depression
|
With depression
|
P
value
|
| Diagnosed depression | Yes | 17 (8.95) | 52 (23.53) | < 0.001 |
| No | 173 (91.05) | 169 (76.47) | ||
| Chronic diseases | Yes | 60 (31.58) | 68 (30.77) | 0.86 |
| No | 130 (68.42) | 153 (69.23) | ||
| High blood pressure | Yes | 100 (52.63) | 114 (51.58) | 0.83 |
| No | 90 (47.37) | 107 (48.42) | ||
| Diabetes | Yes | 49 (25.79) | 58 (26.24) | 0.92 |
| No | 141 (74.21) | 163 (73.76) | ||
| Coronary heart disease | Yes | 21 (11.05) | 42 (19) | 0.03 |
| No | 169 (88.95) | 179 (81) | ||
| Cerebrovascular disease | Yes | 14 (7.37) | 25 (11.31) | 0.17 |
| No | 176 (92.63) | 196 (88.69) | ||
| Enlarged prostate | Yes | 9 (4.74) | 14 (6.33) | 0.48 |
| No | 181 (95.26) | 207 (93.67) | ||
| Cancer | Yes | 6 (3.16) | 8 (3.62) | 0.80 |
| No | 184 (96.84) | 213 (96.38) | ||
| Mental illness | Yes | 1 (0.53) | 12 (5.43) | 0.01 |
| No | 189 (99.47) | 209 (94.57) | ||
| Tuberculosis | Yes | 0 (0) | 1 (0.45) | 0.35 |
| No | 190 (100) | 220 (99.55) | ||
| Chronic hepatitis | Yes | 1 (0.53) | 3 (1.36) | 0.39 |
| No | 189 (99.47) | 218 (98.64) | ||
| Cirrhosis | Yes | 3 (1.58) | 2 (0.9) | 0.53 |
| No | 187 (98.42) | 219 (99.1) |
Comparison of general characteristics between the without depression and with depression groups
Eight general characteristics, including sex, age, education, marital status, living situation, occupational status, income (yuan) per month and exercise, were analyzed. The percentages of sex, education level, marital status, living situation, occupational status, income (yuan) per month and exercise in the without depression and with depression groups were compared by the chi-square test. As shown in Table 4, age was compared by the independent t test. Education level (P = 0.04), living situation (P=0.002), and exercise (P < 0.001) showed significant differences between the two groups. The other 5 general characteristics showed no significant differences (P > 0.05). The most significant general characteristic was exercise; the percentages in the without depression and with depression groups were 78.95% and 62.44%, respectively. The percentages of elementary school education and below, junior high school education, secondary school or high school education, university education and above in the two groups were 1.05%, 13.16%, 38.42%, 47.37% and 1.81%, 23.53%, 29.86%, 44.80%, respectively. The percentages of living alone, living with a husband or wife, living with children, and others in the two groups were 5.79%, 59.47%, 32.11%, and 2.63% and 16.29%, 50.68%, 27.15%, and 5.88%, respectively.
Table 4.
Comparison of general characteristics between without depression and with depression groups, n (%)
|
Characteristics
|
Status
|
Without depression
|
With depression
|
P
value
|
| Gender | Male | 51 (26.84) | 55 (24.89) | 0.65 |
| Female | 139 (73.16) | 166 (75.11) | ||
| Age (yr) | 59.36 ± 7.46 | 59.66 ± 8.36 | 0.71 | |
| Education | Elementary school and below | 2 (1.05) | 4 (1.81) | 0.04 |
| Junior high school | 25 (13.16) | 52 (23.53) | ||
| Secondary school or high school | 73 (38.42) | 66 (29.86) | ||
| University and above | 90 (47.37) | 99 (44.8) | ||
| Marital status | Unmarried | 6 (3.16) | 10 (4.52) | 0.05 |
| Married | 170 (89.47) | 178 (80.54) | ||
| Divorced | 5 (2.63) | 18 (8.14) | ||
| Widowed | 9 (4.74) | 15 (6.79) | ||
| Living situation | Living alone | 11 (5.79) | 36 (16.29) | 0.002 |
| Live with husband or wife | 113 (59.47) | 112 (50.68) | ||
| Live with children | 61 (32.11) | 60 (27.15) | ||
| Other | 5 (2.63) | 13 (5.88) | ||
| Occupational | On-the-job | 55 (28.95) | 49 (22.17) | 0.29 |
| Retire | 130 (68.42) | 166 (75.11) | ||
| Unemployed | 5 (2.63) | 6 (2.71) | ||
| Income (yuan) | 0-2000 | 4 (2.11) | 9 (4.07) | 0.09 |
| 2000-4000 | 53 (27.89) | 81 (36.65) | ||
| 4000-6000 | 71 (37.37) | 78 (35.29) | ||
| ≥ 6000 | 62 (32.63) | 53 (23.98) | ||
| Exercise | Yes | 150 (78.95) | 138 (62.44) | < 0.001 |
| No | 40 (21.05) | 83 (37.56) |
Comparison of insomnia-related characteristics between the without depression and with depression groups
Years of insomnia, Western medicine treatment, Chinese medicine treatment, psychotherapy, kind of insomnia, events related to insomnia, treatment expected to treat insomnia, traditional Chinese medicine foot baths, acupressure, psychological counseling, medicated diet, Tai Chi, traditional Chinese medicine, other traditional Chinese medicines, habit of 1 h before bed, habit of drinking tea, habit of drinking coffee, habit of drinking spirits, habit of smoking, and habit of taking a lunch break were analyzed. As shown in Table 5, among the 20 insomnia-related characteristics, years of insomnia (P < 0.001), Western medicine treatment (P = 0.02), Chinese medicine treatment (P < 0.001), psychotherapy (P = 0.002), kind of insomnia (P < 0.001), treatment expected to treat insomnia (P < 0.001), psychological counseling (P < 0.001), habit of 1 h before bed (P < 0.001), and habit of taking a lunch break (P < 0.001) showed significant differences between the two groups. The other 11 characteristics showed no significant differences (P > 0.05). The years of insomnia in the without depression and with depression groups were 5.21 ± 6.06 years and 7.35 ± 7.48 years, respectively.
Table 5.
Comparison of insomnia related characteristics between without depression and with depression groups, n (%)
|
Indicator
|
Status
|
Without depression
|
With depression
|
P
value
|
| Years of insomnia | 5.21 ± 6.06 | 7.35 ± 7.48 | < 0.001 | |
| Western medicine treatment | Yes | 102 (53.68) | 143 (64.71) | 0.02 |
| No | 88 (46.32) | 78 (35.29) | ||
| Chinese medicine treatment | Yes | 82 (43.16) | 143 (64.71) | < 0.001 |
| No | 108 (56.84) | 78 (35.29) | ||
| Psychotherapy | Yes | 6 (3.16) | 25 (11.31) | 0.002 |
| No | 184 (96.84) | 196 (88.69) | ||
| Kinds of insomnia | Difficult to fall asleep | 89 (46.84) | 140 (63.35) | < 0.001 |
| Difficult to deep sleep | 20 (10.53) | 16 (7.24) | ||
| Easy to wake up | 53 (27.89) | 36 (16.29) | ||
| Wake up early | 28 (14.74) | 29 (13.12) | ||
| Events related to insomnia | Work pressure | 42 (22.11) | 40 (18.1) | 0.10 |
| Family life | 58 (30.53) | 66 (29.86) | ||
| Disease related | 49 (25.79) | 82 (37.1) | ||
| Sleep environment | 37 (19.47) | 31 (14.03) | ||
| Interpersonal communication | 4 (2.11) | 2 (0.9) | ||
| Treatment expected to treat insomnia | Western medicine | 53 (27.89) | 36 (16.29) | < 0.001 |
| Traditional Chinese Medicine | 97 (51.05) | 133 (60.18) | ||
| Psychotherapy | 14 (7.37) | 36 (16.29) | ||
| Other | 26 (13.68) | 16 (7.24) | ||
| Traditional Chinese medicine foot bath | Yes | 50 (26.32) | 49 (22.17) | 0.33 |
| No | 140 (73.68) | 172 (77.83) | ||
| Acupressure | Yes | 51 (26.84) | 50 (22.62) | 0.32 |
| No | 139 (73.16) | 171 (77.38) | ||
| Psychological counseling | Yes | 1 (0.53) | 19 (8.6) | < 0.001 |
| No | 189 (99.47) | 202 (91.4) | ||
| Medicated diet | Yes | 16 (8.42) | 28 (12.67) | 0.17 |
| No | 174 (91.58) | 193 (87.33) | ||
| Tai Chi | Yes | 11 (5.79) | 5 (2.26) | 0.07 |
| No | 179 (94.21) | 216 (97.74) | ||
| Traditional Chinese medicine | Yes | 93 (48.95) | 120 (54.3) | 0.28 |
| No | 97 (51.05) | 101 (45.7) | ||
| Other traditional Chinese medicine | Yes | 17 (8.95) | 16 (7.24) | 0.53 |
| No | 173 (91.05) | 205 (92.76) | ||
| Habit of 1 hour before bed | Electronic products | 79 (41.58) | 125 (56.56) | < 0.001 |
| Reading news or papers | 31 (16.32) | 22 (9.95) | ||
| Chat | 7 (3.68) | 10 (4.52) | ||
| Fitness | 0 (0) | 1 (0.45) | ||
| None | 12 (6.32) | 26 (11.76) | ||
| Watch TV | 61 (32.11) | 37 (16.74) | ||
| Habit of drinking tea | Yes | 57 (30) | 81 (36.65) | 0.16 |
| No | 133 (70) | 140 (63.35) | ||
| Habit of drinking coffee | Yes | 38 (20) | 35 (15.84) | 0.27 |
| No | 152 (80) | 186 (84.16) | ||
| Habit of drinking spirits | Yes | 3 (1.58) | 10 (4.52) | 0.09 |
| No | 187 (98.42) | 211 (95.48) | ||
| Habit of smoking | Yes | 24 (12.63) | 19 (8.6) | 0.18 |
| No | 166 (87.37) | 202 (91.4) | ||
| Habit of lunch break | Yes | 52 (27.37) | 82 (37.1) | < 0.001 |
| No | 138 (72.63) | 139 (62.9) |
Logistic analysis of depression and the significant characteristics
After comparing the disease status, general characteristics, and insomnia-related characteristics between the without depression and with depression groups, education level, living situation, exercise, years of insomnia, Western medicine treatment, Chinese medicine treatment, psychotherapy, kind of insomnia, treatment expected to treat insomnia, psychological counseling, habit of 1 h before bed, habit of taking a lunch break, diagnosed depression, coronary heart disease, and mental illness, which showed significant differences between the two groups, were further analyzed by logistic regression. As shown in Table 6, by univariate analysis, the ORs of education level (P = 0.02), exercise (P = 0.02), kind of insomnia (P = 0.01), habit of 1 h before bed (P = 0.04), diagnosed depression (P = 0.03), and coronary heart disease (P = 0.02) showed significant differences. Their odds ratios (ORs) were 0.71 (0.54, 0.94), 1.81 (1.11, 2.95), 0.79 (0.65, 0.95), 0.90 (0.81, 1.00), 0.48 (0.24, 0.94), and 0.46 (0.25, 0.86), respectively. Then, the characteristics that showed significant differences in the univariate analysis were further analyzed by multivariate analysis. The ORs of education level (P = 0.01), exercise (P < 0.001), kind of insomnia (P < 0.001), habit of 1 h before bed (P = 0.02), diagnosed depression (P < 0.001), and coronary heart disease (P = 0.01) were significantly different. Their ORs were 0.71 (0.55, 0.93), 2.09 (1.32, 3.31), 0.76 (0.63, 0.91), 0.89 (0.81, 0.98), 0.32 (0.17, 0.60), and 0.43 (0.23, 0.79), respectively.
Table 6.
Logistic analysis of depression and the significant characteristics
|
Characteristics
|
Univariate analysis
|
Multivariate analysis
|
||||||||
|
Wals
|
P
value
|
OR
|
95% CI of OR
|
Wals
|
P
value
|
OR
|
95% CI of OR
|
|||
|
Lower
|
Upper
|
Lower
|
Upper
|
|||||||
| Education | 5.58 | 0.02 | 0.71 | 0.54 | 0.94 | 6.08 | 0.01 | 0.71 | 0.55 | 0.93 |
| Living situation | 0.38 | 0.54 | 0.91 | 0.67 | 1.23 | |||||
| Exercise | 5.63 | 0.02 | 1.81 | 1.11 | 2.95 | 9.89 | < 0.001 | 2.09 | 1.32 | 3.31 |
| Years of insomnia | 3.40 | 0.07 | 1.03 | 1.00 | 1.07 | |||||
| Western medicine treatment | 1.05 | 0.31 | 0.79 | 0.50 | 1.24 | |||||
| Chinese medicine treatment | 0.70 | 0.40 | 1.20 | 0.78 | 1.82 | |||||
| Psychotherapy | 1.30 | 0.25 | 0.53 | 0.18 | 1.57 | |||||
| Kinds of insomnia | 5.95 | 0.01 | 0.79 | 0.65 | 0.95 | 8.79 | < 0.001 | 0.76 | 0.63 | 0.91 |
| Treatment expected to treat insomnia | 0.74 | 0.39 | 1.12 | 0.87 | 1.44 | |||||
| Psychological counseling | 2.96 | 0.09 | 0.15 | 0.02 | 1.30 | |||||
| Habit of 1 hour before bed | 3.97 | 0.04 | 0.90 | 0.81 | 1.00 | 5.48 | 0.02 | 0.89 | 0.81 | 0.98 |
| Habit of lunch break | 0.12 | 0.73 | 1.08 | 0.68 | 1.71 | |||||
| Diagnosed depression | 4.64 | 0.03 | 0.48 | 0.24 | 0.94 | 12.94 | < 0.001 | 0.32 | 0.17 | 0.60 |
| Coronary heart disease | 5.91 | 0.02 | 0.46 | 0.25 | 0.86 | 7.43 | 0.01 | 0.43 | 0.23 | 0.79 |
| Mental illness | 2.87 | 0.09 | 0.16 | 0.02 | 1.34 | |||||
OR: Odds ratio.
DISCUSSION
Education level was a protective factor against depression and the OR was 0.71 (0.55, 0.93). Studies have found that academic achievement can influence employment, health care, and social communication[18-20]. The relationship between depression and academic achievement has drawn increasing attention. An overall negative association between depression and academic achievement for both sexes was demonstrated. Several studies have examined the associations between depression and academic achievement[21,22]. Our study results were consistent with these studies. People with higher education levels have good learning abilities, receive health-related knowledge, and have stronger abilities to cope with and solve problems, which may have a positive effect on obtaining better sleep quality. Some studies have shown that the number of years of education were associated with the recurrence of depression, and the shorter the years of education, the greater the possibility of depression recurrence[23,24]. Considering that years of education indirectly affect the sleep quality of patients through depressive symptoms, the relationship among the three factors needs to be further explored. There are some opposite results between depression and education level. On the one hand, educational attainment protects individuals from depression and improves their symptoms; however, individuals with higher education levels are more likely to suffer severe and recurrent episodes of major depression than individuals with low levels of education[25,26].
In our study, patients who did not exercise had an OR of 2.09 (1.32, 3.31) compared with the patients who did exercise. We demonstrated that exercise was a protective factor against depression. The protective effects of exercise and its mechanism on depression have been demonstrated in many studies[27] and support that physical exercise can reduce depression symptoms in patients[28,29]. In patients with depression (aged 18–60 years) who performed aerobic exercise or stretching exercises, there were significant short-term time effects for improving depression severity[30]. A meta-analysis study including 1452 depression patients found a protective effect on depression, regardless of the mode of exercise[31]. However, there are still some studies that found that there is no protective effect of exercise on treating depression. The provision of advice and encouragement for exercise did not improve the depression therapeutic effect when compared to regular care[32]. In another study, 1-week high cadence cycling did not improve depression symptoms[33]. Recently, exercise was not only used as a single treatment for depression but also an adjunct intervention therapeutic method for depression[34]. When exercise was used as a single therapy method, depression-related symptoms were significantly decreased after moderate aerobic exercise for 8 wk[35]. In addition, exercise was also recognized as an intervention with significant effects that can be used as an adjuvant therapy for depression[36]. The mechanisms underlying the antidepressant effects of exercise are closely related to psychological and physiological factors. Psychosocial and cognitive factors after exercise may include self-worth, self-esteem, self-efficacy, self-confidence, sleep quality, and life satisfaction[37-39]. Anti-inflammatory and antioxidant factors (interleukin-18, interleukin-1β, interleukin-6, tumor necrosis factor-α, caspase-1) were also demonstrated to be closely related to depression and anxiety[40-42]. The antidepressant effects of exercise are also related to elevated neurogenesis because of brain-derived neurotrophic factors[43-45].
This study found that the kind of insomnia was related to depression. Patients with major depressive disorder in the community had poor subjective sleep quality, prolonged sleep latency, short sleep duration, low sleep efficiency, sleep disturbances, and impaired daytime functioning[46]. These subjective sleep quality abnormalities were consistent with the objective measurements of sleep[47,48]. Some studies have shown that the polysomnography of patients with major depressive disorder shows that the rapid eye movement latency period is shortened, and the time of the first rapid eye movement period after falling asleep moves forward, which increases the proportion of rapid eye movement sleep and reduces the time of slow wave sleep[49-51]. Possible mechanisms include hyperexcitability of the hypothalamic–pituitary–adrenal axis; a glutamate deficiency, which plays an important role in both depression and sleep regulation; a marked reduction in plasma melatonin levels; alterations in the serotonergic system; and some increases in systemic markers of inflammation. The sleep quality of people with depression disorder in the past is different from that of the normal population[51,52]. The depressive symptoms disappear, but their sleep problems still persist. Some people think that persistent sleep disorder is a manifestation of the residual period of major depressive disorder. Depressive symptoms in patients with previous depressive disorder were not related to current sleep quality, while residence, years of education, work status and mental health were significantly correlated with sleep quality in patients with a previous depressive disorder[53,54]. Depressed patients living in rural areas were twice as likely to have good sleep quality compared with patients with previous depressive disorders living in urban areas. In our study, the absence of coronary heart disease was also demonstrated to be a protective factor against depression. Recently, the relationship between coronary heart disease and depression has received increased attention[55]. Patients with coronary heart disease are more likely to suffer from depression because they often endure unpleasant symptoms without warning and are required to take many medications for their lifestyle[55], leading to negative emotions such as anxiety or depression[56]. Approximately 20%–30% of patients with heart diseases are diagnosed with anxiety or depression. However, the percentage of patients affected with anxiety and depression was reported to be elevated to 15%–43% during the first 12 mo after an acute cardiac event[55]. Compared to depression, self-reported depression is more strongly related to cardiac morbidity and mortality[57].
Although we systematically analyzed the factors related to depression, including a depression evaluation, a sleep quality evaluation, general characteristics, and diagnosed disease status, there are still some limitations in this study. First, the sample size was relatively small. Some group sample sizes may affect the statistical results and lead to bias in the results. Second, although patients with depression in the past and patients who had been recently diagnosed with depression were enrolled in our study, the sample sizes of the two groups were small, and we did not compare their relative factors. Third, different therapeutic methods for depression were not performed. In our future study, we will perform a study that compares the therapeutic effects of different methods for treating depression.
CONCLUSION
In conclusion, we demonstrated that education level, exercise, kind of insomnia, habit of 1 h before bed, diagnosed depression and coronary heart disease were the factors related to depression, which may provide some implications for the clinical practice of depression.
ARTICLE HIGHLIGHTS
Research background
Depression and sleep quality were demonstrated to be affected each other. In addition, the other factor, including diseases, general and insomnia characteristics also affect depression.
Research motivation
The relationship of depression and sleep quality, diseases and general characteristics and depression should be systemically investigated.
Research objectives
In this study, we aimed to investigate the relationship of depression and sleep quality, diseases and general characteristics.
Research methods
Questionnaire included Patient Health Questionnaire-9 (PHQ-9) and Pittsburgh sleep quality index (PSQI), 12 kinds of diseases, 8 general characteristics, and 20 insomnia characteristics, totally 56 items were filled out by 411 patients enrolled.
Research results
All the 9 items of PHQ-9, 6 components of PSQI (except sleep duration), 12 kinds of diseases, 3 general characteristics, and 9 insomnia characteristics showed significant difference between without and with depression group. By univariate analysis and multivariate analysis. The odds ratio of education, exercise, kinds of insomnia, habit of 1 h before bed, diagnosed depression, coronary heart disease showed significant difference.
Research conclusions
Education, exercise, kinds of insomnia, habit of 1 h before bed, diagnosed depression and coronary heart disease are the related factor with depression.
Research perspectives
Larger sample size and long-time span study should be designed and performed in the future study. Different therapeutic methods for depression should also be performed.
Footnotes
Institutional review board statement: The study was reviewed and approved by the Fuxing Hospital affiliated to Capital Medical University Institution Review Board.
Informed consent statement: All study participants or their legal guardian provided written informed consent prior to study enrollment.
Conflict-of-interest statement: We declare that we have no financial or personal relationships with other individuals or organizations that can inappropriately influence our work and that there is no professional or other personal interest of any nature in any product, service and/or company that could be construed as influencing the position presented in or the review of the manuscript.
STROBE statement: The authors have read the STROBE Statement – checklist of items, and the manuscript was prepared and revised according to the STROBE Statement – checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: January 24, 2022
First decision: March 13, 2022
Article in press: April 28, 2022
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Benham S, United States; Gunlu A, Turkey; Kalnak N, Sweden; Mazza M, Italy; Therasse E, Canada S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
Contributor Information
Yan Jiang, Yuetan Community Health Service Center Fuxing Hospital, Capital Medical University, Beijing 100045, China.
Tao Jiang, Department of Medicine Innovation Research, Chinese PLA General Hospital, Beijing 100853, China.
Li-Tao Xu, Yuetan Community Health Service Center Fuxing Hospital, Capital Medical University, Beijing 100045, China.
Lan Ding, Yuetan Community Health Service Center Fuxing Hospital, Capital Medical University, Beijing 100045, China. dinglan@ccmu.edu.cn.
Data sharing statement
No data is needed to share.
References
- 1.Malhi GS, Mann JJ. Depression. Lancet. 2018;392:2299–2312. doi: 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- 2.Wang J, Wu X, Lai W, Long E, Zhang X, Li W, Zhu Y, Chen C, Zhong X, Liu Z, Wang D, Lin H. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open. 2017;7:e017173. doi: 10.1136/bmjopen-2017-017173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreno-Agostino D, Wu YT, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. J Affect Disord. 2021;281:235–243. doi: 10.1016/j.jad.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 4.Remes O, Mendes JF, Templeton P. Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature. Brain Sci. 2021;11 doi: 10.3390/brainsci11121633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Z, Ruan M, Chen J, Fang Y. Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neurosci Bull. 2021;37:863–880. doi: 10.1007/s12264-021-00638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satinsky EN, Kakuhikire B, Baguma C, Rasmussen JD, Ashaba S, Cooper-Vince CE, Perkins JM, Kiconco A, Namara EB, Bangsberg DR, Tsai AC. Adverse childhood experiences, adult depression, and suicidal ideation in rural Uganda: A cross-sectional, population-based study. PLoS Med. 2021;18:e1003642. doi: 10.1371/journal.pmed.1003642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yan T, Qiu Y, Yu X, Yang L. Glymphatic Dysfunction: A Bridge Between Sleep Disturbance and Mood Disorders. Front Psychiatry. 2021;12:658340. doi: 10.3389/fpsyt.2021.658340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020;45:74–89. doi: 10.1038/s41386-019-0411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alvaro PK, Roberts RM, Harris JK. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep. 2013;36:1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayer G, Happe S, Evers S, Hermann W, Jansen S, Kallweit U, Muntean ML, Pöhlau D, Riemann D, Saletu M, Schichl M, Schmitt WJ, Sixel-Döring F, Young P. Insomnia in neurological diseases. Neurol Res Pract. 2021;3:15. doi: 10.1186/s42466-021-00106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ragnoli B, Pochetti P, Raie A, Malerba M. Comorbid Insomnia and Obstructive Sleep Apnea (COMISA): Current Concepts of Patient Management. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18179248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao J, Liu H, Wu Z, Wang Y, Cao T, Lyu D, Huang Q, Zhu Y, Wu X, Chen J, Su Y, Zhang C, Peng D, Li Z, Rong H, Liu T, Xia Y, Hong W, Fang Y. Clinical features of the patients with major depressive disorder co-occurring insomnia and hypersomnia symptoms: a report of NSSD study. Sleep Med. 2021;81:375–381. doi: 10.1016/j.sleep.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Ruggieri V. [Autism, depression and risk of suicide] Medicina (B Aires) 2020;80 Suppl 2:12–16. [PubMed] [Google Scholar]
- 14.Buckman JEJ, Saunders R, Stott J, Arundell LL, O'Driscoll C, Davies MR, Eley TC, Hollon SD, Kendrick T, Ambler G, Cohen ZD, Watkins E, Gilbody S, Wiles N, Kessler D, Richards D, Brabyn S, Littlewood E, DeRubeis RJ, Lewis G, Pilling S. Role of age, gender and marital status in prognosis for adults with depression: An individual patient data meta-analysis. Epidemiol Psychiatr Sci. 2021;30:e42. doi: 10.1017/S2045796021000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mendelsohn C. Smoking and depression--a review. Aust Fam Physician. 2012;41:304–307. [PubMed] [Google Scholar]
- 16.Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, Aguglia A, Belvederi Murri M, Brakoulias V, Amore M, Ghaemi SN, Amerio A. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review. J Affect Disord. 2021;279:473–483. doi: 10.1016/j.jad.2020.09.131. [DOI] [PubMed] [Google Scholar]
- 17.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Witt K, Milner A, Evans-Whipp T, Toumbourou JW, Patton G, LaMontagne AD. Educational and Employment Outcomes among Young Australians with a History of Depressive Symptoms: A Prospective Cohort Study. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18073376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyake Y, Tanaka K, Arakawa M. Employment, income, and education and prevalence of depressive symptoms during pregnancy: the Kyushu Okinawa Maternal and Child Health Study. BMC Psychiatry. 2012;12:117. doi: 10.1186/1471-244X-12-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang A, Wang K, DuVall AS. Examining the Pathoplastic Moderating Role of Education on the Association between Depressive Mood and Self-Rated Health among Cancer Survivors: A Population-Based Study. Curr Oncol. 2021;28:4042–4052. doi: 10.3390/curroncol28050343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riglin L, Petrides KV, Frederickson N, Rice F. The relationship between emotional problems and subsequent school attainment: a meta-analysis. J Adolesc. 2014;37:335–346. doi: 10.1016/j.adolescence.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 22.Veldman K, Bültmann U, Stewart RE, Ormel J, Verhulst FC, Reijneveld SA. Mental health problems and educational attainment in adolescence: 9-year follow-up of the TRAILS study. PLoS One. 2014;9:e101751. doi: 10.1371/journal.pone.0101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preventing recurrent depression: long-term treatment for major depressive disorder. Prim Care Companion J Clin Psychiatry. 2007;9:214–223. [PMC free article] [PubMed] [Google Scholar]
- 24.Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deb S, Banu PR, Thomas S, Vardhan RV, Rao PT, Khawaja N. Depression among Indian university students and its association with perceived university academic environment, living arrangements and personal issues. Asian J Psychiatr. 2016;23:108–117. doi: 10.1016/j.ajp.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Ahmed G, Negash A, Kerebih H, Alemu D, Tesfaye Y. Prevalence and associated factors of depression among Jimma University students. A cross-sectional study. Int J Ment Health Syst. 2020;14:52. doi: 10.1186/s13033-020-00384-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie Y, Wu Z, Sun L, Zhou L, Wang G, Xiao L, Wang H. The Effects and Mechanisms of Exercise on the Treatment of Depression. Front Psychiatry. 2021;12:705559. doi: 10.3389/fpsyt.2021.705559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Micheli L, Ceccarelli M, D'Andrea G, Tirone F. Depression and adult neurogenesis: Positive effects of the antidepressant fluoxetine and of physical exercise. Brain Res Bull. 2018;143:181–193. doi: 10.1016/j.brainresbull.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Imboden C, Gerber M, Beck J, Eckert A, Pühse U, Holsboer-Trachsler E, Hatzinger M. Effects of Aerobic Exercise as Add-On Treatment for Inpatients With Moderate to Severe Depression on Depression Severity, Sleep, Cognition, Psychological Well-Being, and Biomarkers: Study Protocol, Description of Study Population, and Manipulation Check. Front Psychiatry. 2019;10:262. doi: 10.3389/fpsyt.2019.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imboden C, Gerber M, Beck J, Holsboer-Trachsler E, Pühse U, Hatzinger M. Aerobic exercise or stretching as add-on to inpatient treatment of depression: Similar antidepressant effects on depressive symptoms and larger effects on working memory for aerobic exercise alone. J Affect Disord. 2020;276:866–876. doi: 10.1016/j.jad.2020.07.052. [DOI] [PubMed] [Google Scholar]
- 31.Nebiker L, Lichtenstein E, Minghetti A, Zahner L, Gerber M, Faude O, Donath L. Moderating Effects of Exercise Duration and Intensity in Neuromuscular vs. Endurance Exercise Interventions for the Treatment of Depression: A Meta-Analytical Review. Front Psychiatry. 2018;9:305. doi: 10.3389/fpsyt.2018.00305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams CF, Bustamante EE, Waller JL, Davis CL. Exercise effects on quality of life, mood, and self-worth in overweight children: the SMART randomized controlled trial. Transl Behav Med. 2019;9:451–459. doi: 10.1093/tbm/ibz015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harper SA, Dowdell BT, Kim JH, Pollock BS, Ridgel AL. Non-Motor Symptoms after One Week of High Cadence Cycling in Parkinson's Disease. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16122104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toups MS, Greer TL, Kurian BT, Grannemann BD, Carmody TJ, Huebinger R, Rethorst C, Trivedi MH. Effects of serum Brain Derived Neurotrophic Factor on exercise augmentation treatment of depression. J Psychiatr Res. 2011;45:1301–1306. doi: 10.1016/j.jpsychires.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olson RL, Brush CJ, Ehmann PJ, Alderman BL. A randomized trial of aerobic exercise on cognitive control in major depression. Clin Neurophysiol. 2017;128:903–913. doi: 10.1016/j.clinph.2017.01.023. [DOI] [PubMed] [Google Scholar]
- 36.Ross RE, VanDerwerker CJ, Newton JH, George MS, Short EB, Sahlem GL, Manett AJ, Fox JB, Gregory CM. Simultaneous aerobic exercise and rTMS: Feasibility of combining therapeutic modalities to treat depression. Brain Stimul. 2018;11:245–246. doi: 10.1016/j.brs.2017.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tu RH, Zeng ZY, Zhong GQ, Wu WF, Lu YJ, Bo ZD, He Y, Huang WQ, Yao LM. Effects of exercise training on depression in patients with heart failure: a systematic review and meta-analysis of randomized controlled trials. Eur J Heart Fail. 2014;16:749–757. doi: 10.1002/ejhf.101. [DOI] [PubMed] [Google Scholar]
- 38.Danielsson L, Kihlbom B, Rosberg S. "Crawling Out of the Cocoon": Patients' Experiences of a Physical Therapy Exercise Intervention in the Treatment of Major Depression. Phys Ther. 2016;96:1241–1250. doi: 10.2522/ptj.20150076. [DOI] [PubMed] [Google Scholar]
- 39.Schuch FB, Dunn AL, Kanitz AC, Delevatti RS, Fleck MP. Moderators of response in exercise treatment for depression: A systematic review. J Affect Disord. 2016;195:40–49. doi: 10.1016/j.jad.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Boucher D, Monteleone M, Coll RC, Chen KW, Ross CM, Teo JL, Gomez GA, Holley CL, Bierschenk D, Stacey KJ, Yap AS, Bezbradica JS, Schroder K. Caspase-1 self-cleavage is an intrinsic mechanism to terminate inflammasome activity. J Exp Med. 2018;215:827–840. doi: 10.1084/jem.20172222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim TK, Kim JE, Choi J, Park JY, Lee JE, Lee EH, Lee Y, Kim BY, Oh YJ, Han PL. Local Interleukin-18 System in the Basolateral Amygdala Regulates Susceptibility to Chronic Stress. Mol Neurobiol. 2017;54:5347–5358. doi: 10.1007/s12035-016-0052-7. [DOI] [PubMed] [Google Scholar]
- 42.Reddy VS, Harskamp RE, van Ginkel MW, Calhoon J, Baisden CE, Kim IS, Valente AJ, Chandrasekar B. Interleukin-18 stimulates fibronectin expression in primary human cardiac fibroblasts via PI3K-Akt-dependent NF-kappaB activation. J Cell Physiol. 2008;215:697–707. doi: 10.1002/jcp.21348. [DOI] [PubMed] [Google Scholar]
- 43.Gujral S, Aizenstein H, Reynolds CF 3rd, Butters MA, Erickson KI. Exercise effects on depression: Possible neural mechanisms. Gen Hosp Psychiatry. 2017;49:2–10. doi: 10.1016/j.genhosppsych.2017.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Laske C, Banschbach S, Stransky E, Bosch S, Straten G, Machann J, Fritsche A, Hipp A, Niess A, Eschweiler GW. Exercise-induced normalization of decreased BDNF serum concentration in elderly women with remitted major depression. Int J Neuropsychopharmacol. 2010;13:595–602. doi: 10.1017/S1461145709991234. [DOI] [PubMed] [Google Scholar]
- 45.Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. J Affect Disord. 2013;148:12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 46.Choi YH, Yang KI, Yun CH, Kim WJ, Heo K, Chu MK. Impact of Insomnia Symptoms on the Clinical Presentation of Depressive Symptoms: A Cross-Sectional Population Study. Front Neurol. 2021;12:716097. doi: 10.3389/fneur.2021.716097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin CH, Yen YC, Chen MC, Chen CC. Depression and pain impair daily functioning and quality of life in patients with major depressive disorder. J Affect Disord. 2014;166:173–178. doi: 10.1016/j.jad.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 48.Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16:375. doi: 10.1186/s12888-016-1075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blasco-Serra A, Escrihuela-Vidal F, González-Soler EM, Martínez-Expósito F, Blasco-Ausina MC, Martínez-Bellver S, Cervera-Ferri A, Teruel-Martí V, Valverde-Navarro AA. Depressive-like symptoms in a reserpine-induced model of fibromyalgia in rats. Physiol Behav. 2015;151:456–462. doi: 10.1016/j.physbeh.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 50.Wang YQ, Li R, Zhang MQ, Zhang Z, Qu WM, Huang ZL. The Neurobiological Mechanisms and Treatments of REM Sleep Disturbances in Depression. Curr Neuropharmacol. 2015;13:543–553. doi: 10.2174/1570159X13666150310002540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steiger A, Pawlowski M. Depression and Sleep. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20030607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Plante DT. The Evolving Nexus of Sleep and Depression. Am J Psychiatry. 2021;178:896–902. doi: 10.1176/appi.ajp.2021.21080821. [DOI] [PubMed] [Google Scholar]
- 53.Norell-Clarke A, Hagström M, Jansson-Fröjmark M. Sleep-Related Cognitive Processes and the Incidence of Insomnia Over Time: Does Anxiety and Depression Impact the Relationship? Front Psychol. 2021;12:677538. doi: 10.3389/fpsyg.2021.677538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Obuobi-Donkor G, Nkire N, Agyapong VIO. Prevalence of Major Depressive Disorder and Correlates of Thoughts of Death, Suicidal Behaviour, and Death by Suicide in the Geriatric Population-A General Review of Literature. Behav Sci (Basel) 2021;11 doi: 10.3390/bs11110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhou Y, Zhu XP, Shi JJ, Yuan GZ, Yao ZA, Chu YG, Shi S, Jia QL, Chen T, Hu YH. Coronary Heart Disease and Depression or Anxiety: A Bibliometric Analysis. Front Psychol. 2021;12:669000. doi: 10.3389/fpsyg.2021.669000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu Y, Chen Z, Duan J, Huang K, Zhu B, Yang L, Zheng L. Serum Levels of FGF21, β-Klotho, and BDNF in Stable Coronary Artery Disease Patients With Depressive Symptoms: A Cross-Sectional Single-Center Study. Front Psychiatry. 2020;11:587492. doi: 10.3389/fpsyt.2020.587492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zuidersma M, Conradi HJ, van Melle JP, Ormel J, de Jonge P. Self-reported depressive symptoms, diagnosed clinical depression and cardiac morbidity and mortality after myocardial infarction. Int J Cardiol. 2013;167:2775–2780. doi: 10.1016/j.ijcard.2012.07.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data is needed to share.