SUMMARY
This study was conducted to examine the incidence trend of campylobacteriosis in Michigan over a 10-year period and to investigate risk factors and clinical outcomes associated with infection. Campylobacter case data from 2004 to 2013 was obtained from the Michigan Disease Surveillance System. We conducted statistical and spatial analyses to examine trends and identify factors linked to campylobacteriosis as well as ecological associations using animal density data from the National Agricultural Statistics Service. An increasing trend of Campylobacter incidence and hospitalization was observed, which was linked to specific age groups and rural residence. Cases reporting ruminant contact and well water as the primary drinking source had a higher risk of campylobacteriosis, while higher cattle density was associated with an increased risk at the county level. Additional studies are needed to identify age-specific risk factors and examine prevalence and transmission dynamics in ruminants and the environment to aid in the development of more effective preventive strategies.
Key words: Campylobacter, epidemiology, foodborne infections, surveillance
INTRODUCTION
Campylobacter, a Gram-negative zoonotic pathogen, is one of the most widespread infectious agents in the world [1]. It is not only the leading cause of gastroenteritis in humans, but it can also cause serious long-term sequelae like Guillain–Barré syndrome, reactive arthritis, and inflammatory bowel disease [2]. The annual incidence of campylobacteriosis varies between countries, but the numbers of reported cases have been increasing worldwide in the past decade [1]. Importantly, estimated burden of disease is considerable, as it is estimated to cost US$1.7 billion/year in the United States alone [3].
Chicken consumption and handling have been identified as major risk factors for campylobacteriosis [4] as broiler chickens are frequently colonized with C. jejuni. Recent studies have also reported attributable rates for cattle in up to 19·3% of Campylobacter cases [5, 6], suggesting that cattle serve as another important source for human infections. Indeed, raw milk and cheese have been implicated in several outbreaks [7]. Campylobacter is also widespread in the environment including water and soil, where it has been found to survive for several months [8, 9]. Water, especially, has been identified as an important source for Campylobacter infections and has been linked to outbreaks as well [10, 11]. Human-to-human transmission via the faecal–oral route has been reported; however, zoonotic or foodborne transmission is the predominant mode. With the high prevalence of campylobacteriosis reported throughout the world, foreign travel has also emerged as an important risk factor [12].
Seasonal variation has been described for Campylobacter infections. A significantly higher incidence of campylobacteriosis has been reported in warmer seasons in different countries and from different sources such as animals and water [13, 14]. The reason behind this seasonality is not known, but has been suggested to be the result of multiple factors including longer survival of Campylobacter sp. in the environment, increased shedding levels in animal reservoirs [15], and changes in human behaviour [16]. Spatial determinants such as urban vs. rural settings, have also been linked to campylobacteriosis incidence [17, 18], suggesting the need to assess environmental factors when conducting risk-factor analyses.
In the United States, the Foodborne Diseases Active Surveillance Network (FoodNet), which monitors incidence trends of foodborne pathogens, reported an increase in the incidence of campylobacteriosis, from 12·3 cases/100 000 in 2009 to 14·2 cases/100 000 in 2012 [19]. This increasing trend may be partly due to improvements in detection methods and enhanced surveillance, although other risk factors such as geographical location are also likely to be important. Considerable variation in campylobacteriosis incidence was observed among FoodNet sites throughout the surveillance period, ranging from 7 cases/100 000 in Tennessee to 34·3 cases/100 000 in California [19]. Because no significant differences were identified for key risk factors, medical care-seeking behaviour, or medical practices between sites, it is probable that site-specific risk factors like climate or number of animal reservoirs are also contributing to the variable rates [20].
Because Michigan is not a FoodNet site, we sought to calculate the incidence of campylobacteriosis over a 10-year period using data collected via the Michigan Department of Health and Human Services (MDHHS) and identify risk factors associated with disease. We hypothesized that the incidence of Campylobacter infections has increased temporally and specific factors are associated with increasing incidence. We also investigated clinical outcomes and demographics to assess the disease burden of campylobacteriosis in Michigan and identify characteristics associated with increased risk of infection. Ongoing surveillance efforts are vital to monitor incidence trends and investigate risk factors for disease in different geographical locations in order to more effectively define preventive measures.
METHODS
Campylobacteriosis is a reportable disease in Michigan. A total of 7182 laboratory-confirmed cases were reported to MDHHS with an onset date between 1 January 2004 and 31 December 2013. Demographic, clinical, and epidemiological data for each case were extracted from the Michigan Disease Surveillance System (MDSS) managed by the MDHHS. Season was categorized based on the onset date and travel was considered only when the travel period was within 1 week prior to the onset of symptoms. Data involving history of food consumption and animal contact were systematically collected from 2011 and thus, only the last 3 years of data were used in the analysis. The water source at home was categorized into well, municipal, bottled and other, which included various combinations of the different sources. Data was considered missing for all variables lacking data or that were reported as ‘unknown’.
Age-adjusted incidence rates (cases/100 000) were calculated using the Bridged-Race Population Estimates 1990–2013 dataset [21] and U.S. 2010 standard population by the U.S. Census Bureau [22]. Statistical analyses were performed using SAS v. 9·3 (SAS Institute Inc., USA). Differences in the frequencies of campylobacteriosis across variables were examined using χ2 tests; P < 0·05 was considered significant. Additional analyses were conducted to investigate the association between demographic characteristics and foreign travel history, where the prevalence ratio was compared between individuals with and without a travel history. Multivariate analyses for hospitalization and rural vs. urban residence were performed using logistic regression while adjusting for independent variables with a P value of <0·2 and biologically plausible variables that could represent confounders (e.g. age, sex). The multivariate model was constructed using a forward stepwise method with the requirement for a significance level of P⩽0·1 to remain in the model.
A Geographical Information System (GIS) map was generated in ArcGIS v. 10·2·2 (ESRI, USA) using data from the National Center for Health Statistics (NCHS), the bridged-race population estimates, and the case numbers in this study. Based on the NCHS classification system [23], ten Michigan counties with large metropolitan areas were classified as urban, while the remaining 73 counties were defined as rural. All protocols were approved by the Institutional Review Boards at Michigan State University (IRB no. 10-736SM) and MDHHS (842-PHALAB).
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
RESULTS
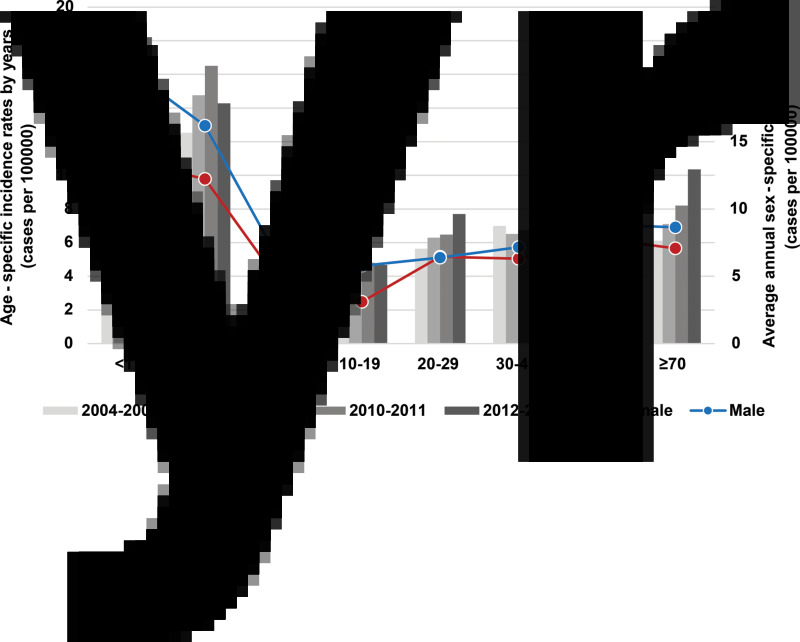
The average age-adjusted annual incidence was 7·22 (cases)/100 000, ranging from 6·26 in 2004 to 8·35 in 2013. An increasing trend was observed over time with average incidence rates increasing from 6·58/100 000 in 2004–2006 to 7·37/100 000 in 2007–2010 and 7·65/100 000 in 2011–2013. The average annual incidence was higher for men (7·89/100 000) than women (6·56/100 000), with an incidence rate ratio of 1·2 (P < 0·01). The highest incidence rate was reported in children aged <5 years (14·86/100 000) compared to other age groups (6·76/100 000, P < 0·01). When stratified by sex, boys aged <1 year had the highest incidence (20·5/100 000), although an overall increasing trend in incidence was observed after 5–19 years, particularly for cases aged between 20–29 and >50 years (Fig. 1).
Fig. 1.
Average annual sex-specific campylobacteriosis incidence rate by age group and the trend of age-specific incidence rates by year, 2004–2013.
Caucasians comprised 85% of the total cases in Michigan and Campylobacter incidence was significantly higher (6·51/100 000) in this group compared to Asians (4·47/100 000) and African Americans (1·56/100 000) (P < 0·05). Cases self-reporting as Asian were more likely to have a history of foreign travel [prevalence ratio (PR) 4·3], while the opposite was observed in individuals self-reporting as African American (PR 0·7) (Table 1). Travel destinations were also correlated with race, as 52·4% of Asian travellers visited Asia and 47·1% of African American travellers visited Africa. By age, individuals between 20 and 39 years were more likely to develop a Campylobacter infection following foreign travel (PR 1·6), while the opposite was observed in children aged <5 years (PR 0·3) and in the elderly (aged ⩾80 years) (PR 0·1) (Table 1).
Table 1.
Demographic characteristics of Campylobacter cases in Michigan (2004–2013) by foreign-travel status
| Total with known foreign-travel status* | Foreign-travel associated cases | Domestic cases | Prevalence ratio | |||
|---|---|---|---|---|---|---|
| Characteristic | No. | No. | % | No. | % | |
| Sex† | ||||||
| Male | 3524 | 489 | 58·9 | 3035 | 52·4 | 1·1 |
| Female | 3094 | 341 | 41·1 | 2753 | 47·6 | 0·9 |
| Age group (years)‡ | ||||||
| <1 | 181 | 10 | 1·2 | 171 | 3 | 0·4 |
| 1–4 | 628 | 26 | 3·1 | 602 | 10·4 | 0·3 |
| 5–19 | 884 | 90 | 10·9 | 794 | 13·7 | 0·8 |
| 20–39 | 1437 | 267 | 32·2 | 1170 | 20·2 | 1·6 |
| 40–59 | 2067 | 314 | 38·2 | 1753 | 30·3 | 1·3 |
| 60–79 | 1186 | 117 | 14·1 | 1069 | 18·5 | 0·8 |
| ⩾80 | 240 | 5 | 0·6 | 235 | 4·0 | 0·2 |
| Race | ||||||
| Caucasian | 4952 | 566 | 68·3 | 4386 | 75·7 | 0·9 |
| African American | 196 | 17 | 2·1 | 179 | 3·1 | 0·7 |
| Asian | 109 | 42 | 5·1 | 67 | 1·2 | 4·3 |
| Others | 553 | 69 | 8·3 | 484 | 8·4 | 1 |
| Unknown | 815 | 135 | 16·3 | 680 | 11·7 | 1·4 |
| Total | 6625 | 830 | 12·5 | 5795 | 87·5 | |
Only the cases with travel information (n = 6625) were included.
Sex was unknown in seven cases.
Age was unknown in two cases.
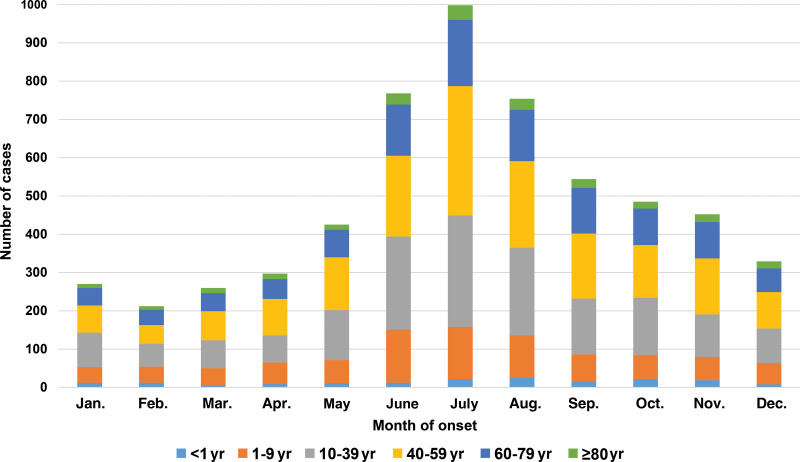
Different seasonal trends were observed for domestic cases (n = 5795) compared to cases with a recent history of foreign travel (n = 830). Domestic cases were more common in the summer months of June and July [odds ratio (OR) 1·6, 95% confidence interval (CI) 1·3–1·9], while cases with foreign travel history were more common in January and February (OR 1·8, 95% CI 1·3–2·4). For domestic cases, the seasonality in summer (June–August) was more prominent for individuals aged 10–59 years, especially compared to the <1 year and ⩾80 years (OR 1·3, 95% CI 1·1–1·6) age groups (Fig. 2).
Fig. 2.
Seasonality of Campylobacter cases reported in Michigan by age group, 2004–2013.
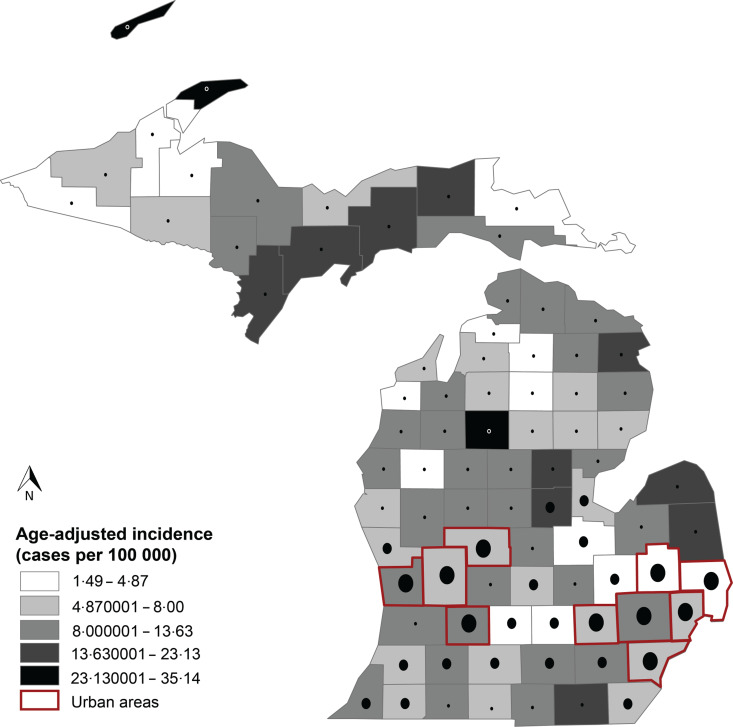
Geographical variation in the age-adjusted incidence was observed in the 83 Michigan counties (Fig. 3). Using data from the NCHS system, ten of the counties were defined as urban and the remainder were rural. The incidence was significantly higher in rural (7·78/100 000) compared to urban areas (6·70/100 000, P < 0·05). Furthermore, the incidence increased by 41·5% from 6·45/100 000 in 2004 to 9·27/100 000 in 2013 in rural cases, relative to a 26·2% increase among urban cases (6·13/100 000 in 2004 to 7·65/100 000 in 2013).
Fig. 3.
Age-adjusted incidence of Campylobacter reported in Michigan by county, 2004–2013. Based on the classification by the National Center for Health Statistics (NCHS) data system [23], ten counties, which represent large metropolitan areas, were classified as urban (red outlines) and the remaining 73 counties were classified as rural. The black circles represent the population size of each county.
To investigate the possibility that geographical variation is linked to factors specific to rural areas, we conducted a case-case analysis between the urban and rural domestic cases. The age-specific incidence was higher for rural cases compared to urban cases, especially for groups aged 10–19 years [incidence rate ratio (IRR) 1·6], 20–39 years (IRR 1·3), and >80 years (IRR 1·3). Univariate analyses demonstrated that contact with animals (i.e. ruminants, poultry, domestic pets) was significantly more common for rural cases compared to urban cases as well as consumption of raw milk, ground meat, and frozen chicken (Table 2). The most notable difference, however, was the water source at home as rural cases were significantly more likely to drink only well water (OR 7·3, 95% CI 5·6–9·4). Multivariate logistic regression controlling for age and sex identified contact with ruminants (OR 1·6, 95% CI 1·0–2·5), consumption of ground meat (OR 1·4, 95% CI 1·1–1·7), and well water at home (OR 5·4, 95% CI 3·9–7·4) to be independently associated with Campylobacter infection in rural areas.
Table 2.
Univariate and multivariate analyses of risk factors in rural cases (n = 1035) compared to urban cases (n = 880)
| Risk factors | Rural | Urban | Univariate analysis: rural vs. urban | ||||
|---|---|---|---|---|---|---|---|
| Cases* | % | Cases* | % | OR | 95% CI† | P value‡ | |
| Contact with animals§ | |||||||
| Ruminants | 190/970 | 19·59 | 59/827 | 7·13 | 3·17 | 2·31–4·39 | <0·0001 |
| Birds | 192/966 | 19·88 | 103/823 | 12·52 | 1·73 | 1·33–2·27 | <0·0001 |
| Domestic pets | 730/987 | 73·96 | 508/828 | 61·35 | 1·79 | 1·46–2·20 | <0·0001 |
| Reptile | 47/961 | 4·89 | 28/823 | 3·40 | 1·46 | 0·89–2·45 | 0·12 |
| Aquatic pets | 94/955 | 9·84 | 62/820 | 7·56 | 1·33 | 0·94–1·90 | 0·0905 |
| Other | 89/922 | 9·65 | 52/820 | 6·34 | 1·58 | 1·10–2·30 | 0·0114 |
| Food consumption | |||||||
| Chicken prepared at home | 474/858 | 55·24 | 388/694 | 55·91 | 0·97 | 0·79–1·20 | 0·7938 |
| Frozen chicken | 256/862 | 29·7 | 167/697 | 23·96 | 1·34 | 1·01–1·68 | 0·0113 |
| Outside chicken | 248/883 | 28·09 | 223/719 | 31·02 | 0·87 | 0·70–1·08 | 0·2006 |
| Ground meats | 505/750 | 67·33 | 372/629 | 59·14 | 1·42 | 1·14–1·79 | 0·0016 |
| Raw milk | 49/971 | 5·05 | 13/796 | 1·64 | 3·20 | 1·69–6·48 | 0·0001 |
| Water source at home | |||||||
| Well | 487/998 | 48·80 | 96/826 | 11·62 | 7·25 | 5·63–9·37 | <0·0001 |
| Multivariate analysis adjusted for age and sex: rural vs. urban | |||||||
| Risk factors | OR | 95% CI|| | P value¶ | ||||
| Ruminants | 1·57 | 1·01–2·46 | 0·0468 | ||||
| Domestic pets | 1·26 | 0·96–1·66 | 0·0954 | ||||
| Frozen chicken | 1·30 | 0·97–1·72 | 0·0749 | ||||
| Ground meats | 1·43 | 1·09–1·72 | 0·0089 | ||||
| Raw milk | 1·89 | 0·85–4·20 | 0·1176 | ||||
| Well | 5·39 | 3·95–7·35 | <0·0001 | ||||
OR, Odds ratio; CI, confidence interval.
Only the cases with onset date between 2011and 2013 (n = 1915) are included due to the high proportion of missing data in previous years.
95% confidence interval for odds ratio.
Likelihood ratio χ2 test.
Animal contact was defined as positive when there was a report of direct contact with reptiles (e.g. snake, lizards), ruminants (e.g. cattle, goats, sheep), birds (e.g. chickens, turkeys, ducks, parrots), aquatic pets (e.g. fish, turtles), domestic pets (e.g. dogs, cats) and other animals. High-risk food exposure was evaluated by consumption history of ground meat (e.g. turkey, chicken, beef, pork), chicken, (i.e. prepared at home, frozen, or at a restaurant), and unpasteurized milk or cheese within a week. Frozen chicken was defined as chicken items that are sold frozen (i.e. breaded, pre-browned, stuffed). The water source at home was categorized into well, municipal, bottled and other, which included combinations of different sources.
Wald confidence interval.
Wald χ2 test.
Given the association with campylobacteriosis and ruminants, we evaluated the ecological association between animal density (i.e. cattle, chickens, goats, sheep, pigs) and disease incidence by county using data from the National Agricultural Statistics Service for 2012 [24]. Counties with <1% of the total number of each animal species in the state were classified as low-density counties, while counties with ⩾1% were classified as high density. Notably, 12 counties with the highest incidence rates of campylobacteriosis (13·6–35·1/100 000), all of which were also defined as rural areas (Fig. 3), were more likely to have a high cattle density (OR 2·5, 95% CI 2·1–2·9). No significant associations were observed for other animal species including chicken.
Clinical outcomes also varied in cases over time; the hospitalization rate increased from 23·3% in 2004 to 29·5% in 2013. Cases aged ⩾60 years had a significantly higher likelihood of hospitalization than other age groups (OR 2·5, 95% CI 2·2–2·8), while bloody diarrhoea was more common in children aged <5 years (OR 2·5, 95% CI 2·1–2·9). Based on these prior associations, we also sought to determine whether there were differences in hospitalization status among cases in rural vs. urban areas and after stratifying by travel history. Both urban and domestic cases were more frequently hospitalized compared to rural cases and those with foreign travel history (Table 3). Multivariate analyses demonstrated that age ⩾60 years (OR 2·4, 95% CI 2·1–2·7), lack of foreign travel (OR 2·6, 95% CI 2·1–3·2), and urban residence (OR 1·2, 95% CI 1·1–1·4), were independently associated with hospitalization.
Table 3.
Univariate and multivariate analyses of characteristics associated with hospitalization due to campylobacteriosis
| Characteristic | Total cases* | No. (%) hospitalized | OR (95% CI)† | P value‡ |
|---|---|---|---|---|
| Age (years) | ||||
| <10 | 1131 | 162 (14·3) | ||
| 10–59 | 4140 | 957 (23·1) | ||
| ⩾60 | 1447 | 576 (34·0) | 2·45 (2·16–2·78) | <0·0001 |
| Gender | ||||
| Male | 3644 | 891 (24·5) | ||
| Female | 3181 | 836 (26·3) | 0·91 (0·81–1·01) | 0·08 |
| Foreign travel | ||||
| Yes | 818 | 104 (12·7) | ||
| No | 5686 | 1533 (23·6) | 2·53 (2·04–3·17) | <0·0001 |
| Season | ||||
| Spring | 1249 | 304 (24·3) | ||
| Summer | 2881 | 748 (26·0) | 1·06 (0·95–1·19) | 0·29 |
| Autumn | 1713 | 447 (26·1) | ||
| Winter | 989 | 230 (23·3) | ||
| Residence | 3264 | 879 (27·0) | ||
| Urban | 3568 | 850 (23·8) | ||
| Rural | 1·18 (1·06–1·32) | 0·0032 |
OR, Odds ratio; CI, confidence interval.
Total number differs between variables due to missing information.
95% confidence interval for odds ratio.
Likelihood ratio χ2 test.
Wald confidence interval.
Multivariate logistic regression.
DISCUSSION
This study represents the first temporal report of campylobacteriosis incidence in Michigan and highlights an increasing incidence trend in the last decade. This increase may be partly due to enhanced awareness and changes in detection practices [25], although other factors are also likely to be important. When stratifying incidence by age, for example, different trends were observed. Increased incidence in cases aged between 20–29 and >50 years suggests that age-specific risk factors such as diet or other lifestyle factors, may be important for disease. Indeed, a higher attributable risk was observed for foreign travel in individuals aged between 20 and 39 years compared to other age groups, while higher disease frequencies occurred in the summer months for those aged between 10 and 59 years, especially compared to the <1 and ⩾80 years age groups. This finding suggests that seasonality could be impacted by summer-related behaviours including camping, swimming, or outdoor grilling, but also that these behaviors may be important risk factors for individuals aged between 10 and 59 years. Additional epidemiological studies are warranted, however, to fully investigate age-specific risk factors for the design of novel public health interventions.
Other factors associated with Campylobacter seasonality may include humidity and temperature [26] as high humidity and temperature levels enhance pathogen survival and proliferation, potentially increasing the load in animal reservoirs [9, 15]. Insect vectors like flies can also facilitate transmission of Campylobacter sp. between animal reservoirs, as well as to humans, when there is increased ventilation and airflow during months with warmer weather [27, 28]. In our study, only domestic cases showed a marked increase in incidence in the summer months, supporting the idea that factors important for seasonality are linked to geographical location or specific environments.
A significant difference in Campylobacter incidence was observed by geographical location, particularly when counties were classified as urban or rural. The higher incidence observed in rural cases in this study is most likely due to more frequent contact with animals and environmental exposures such as well water. Similar findings have been reported previously, as direct contact with farm animals [29, 30], swimming in lakes and rivers [31], and drinking untreated water [32], were associated with a higher risk of campylobacteriosis in rural settings. The steep increasing rate observed in rural areas of Michigan is concerning and warrants a further investigation to identify the source of infection in these areas.
Although chickens are a major reservoir for Campylobacter sp. and a prior Michigan study noted a correlation between poultry density and campylobacteriosis incidence [33], poultry density was not significantly associated with incidence in our study. Indeed, only four of the 83 counties were classified as having high chicken densities and one of these counties comprised 96·3% of the total layers in Michigan. Broilers were the dominant poultry type in the other three counties. The fact that poultry farming was confined to only four Michigan counties may have limited our ability to detect an association between poultry density and campylobacteriosis.
By contrast, 30 counties were classified as high cattle counties, in which the number of dairy cows was 3·6 times higher than beef cows. Compared to another prior Michigan study conducted in 2003 [34] that reported poultry husbandry as the key risk factor for campylobacteriosis in rural residents, only ruminant contact was a risk factor in rural cases compared to urban cases in our study. Although cattle contact would be expected to be more common and frequent in rural residents, it is plausible that the elevated risk for rural cases with well water may be suggestive of faecal contamination of source waters. Of rural cases, those in counties with high cattle densities were more likely to have well water as the only water source compared to cases from low-cattle-density counties (OR 1·6, 95% CI 1·2–2·1). Nonetheless, further studies are warranted to elucidate the genetic relatedness of isolates recovered from humans and cattle as well as the environment, including private wells, to better address questions involving source attribution and transmission dynamics. Additional studies are also needed to better assess associations between disease and food handling, preparation and consumption practices. Even though we initially observed an association between disease and frozen chicken consumption in the univariate analysis for rural cases, this association was no longer significant in the multivariate analysis.
Population distribution by race may also affect the overall incidence of Campylobacter in a given area. In this study, Caucasians had significantly higher rates relative to individuals of other races, especially African Americans, although different patterns were observed when foreign travel status was compared by race. These data suggest that risk factors may vary by race, which is similar to a prior study that reported a different level of risk for travel-related Campylobacter infections by the travel destination [35]. More specifically, they observed higher levels of infection following travel to Southeast Asia (32·4%), South Asia (7·8%), Africa (4·6%), and Latin America (2·5%). Another study also observed an association between a higher socioeconomic status and a higher campylobacteriosis notification rate [36], thereby warranting future studies aimed at examining the association between racial/ethnic background and disease while taking socioeconomic status into account as a confounding factor.
Similar to studies conducted in Hungary [37] and the UK [38], we observed a significant association between age and severe symptoms as children aged <5 years more frequently reported bloody diarrhoea. Since these findings are consistent across geographical locations with distinct strains in circulation, we expect that an immature intestinal mucosal immune system may contribute to more severe complications in young children [38, 39] and this is not the result of ascertainment bias. Although the association with hospitalization identified in the study is important, it may represent a ‘healthy travellers effect’ [40] as limited access to medical facilities may have contributed to lower hospitalization rates in travellers and rural cases. Nonetheless, the increasing rate of hospitalization in individuals aged ⩾60 years is concerning and may be due to the increasing Campylobacter incidence in this population.
In summary, the incidence of campylobacteriosis has increased in Michigan over time, and considerable variation was observed in the spatial distribution of cases and in factors associated with infection. Continuous monitoring of incidence is warranted, while additional studies must attempt to identify those individuals who are most susceptible to campylobacteriosis and more severe clinical outcomes. Designing target-specific preventive measures for the most susceptible population and identifying major environmental sources may be a key to decreasing infection rates and the disease burden in specific geographic locations.
ACKNOWLEDGEMENTS
This study was funded by the National Institutes of Health Enterics Research Investigational Network (ERIN) Cooperative Research Center at Michigan State University (S.D.M., grant number AI090872) and the United States Department of Agriculture, National Institute of Food and Agriculture (S.D.M., grant no. 2011-67005-30004).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Kaakoush NO, et al. Global epidemiology of Campylobacter infection. Clinical Microbiology Reviews 2015; 28: 687–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keithlin J, et al. Systematic review and meta-analysis of the proportion of Campylobacter cases that develop chronic sequelae. BMC Public Health 2014; 14: 1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Batz MB, Hoffmann S, Morris JG. Ranking the disease burden of 14 pathogens in food sources in the United States using attribution data from outbreak investigations and expert elicitation. Journal of Food Protection 2012; 75: 1278–1291. [DOI] [PubMed] [Google Scholar]
- 4.Harris N V, Weiss NS, Nolan CM. The role of poultry and meats in the etiology of Campylobacter jejuni/coli enteritis. American Journal of Public Health 1986; 76: 407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boysen L, et al. Source attribution of human campylobacteriosis in Denmark. Epidemiology and Infection 2014; 142: 1599–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kittl S, et al. Source attribution of human Campylobacter isolates by MLST and fla-typing and association of genotypes with quinolone resistance. PLoS One 2013; 8: e81796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Interagency Food Safety Analytics Collobaration. Foodborne illness source attribution Estimates for salmonella, Escherichia coli O157 (E. coli O157), Listeria monocytogenes, and Campylobacter using outbreak surveillance data. Interagency food safety analytics collaboration project, 2015.
- 8.Pitkänen T. Review of Campylobacter sp. in drinking and environmental waters. Journal of Microbiological Methods 2013; 95: 39–47. [DOI] [PubMed] [Google Scholar]
- 9.Jones K. Campylobacters in water, sewage and the environment. Journal of Applied Microbiology 2001; 90: 68S–79S. [DOI] [PubMed] [Google Scholar]
- 10.Taylor EV, et al. Common source outbreaks of Campylobacter infection in the USA, 1997–2008. Epidemiology and Infection 2013; 141: 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark CG, et al. Characterization of waterborne outbreak-associated Campylobacter jejuni, Walkerton, Ontario. Emerging Infectious Diseases 2003; 9: 1232–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kendall ME, et al. Travel-associated enteric infections diagnosed after return to the United States, Foodborne Diseases Active Surveillance Network (FoodNet), 2004–2009. Clinical Infectious Diseases 2012; 54: S480–S487. [DOI] [PubMed] [Google Scholar]
- 13.Rind E, Pearce J. The spatial distribution of campylobacteriosis in New Zealand, 1997–2005. Epidemiology and Infection 2010; 138: 1359–1371. [DOI] [PubMed] [Google Scholar]
- 14.Kovats RS, et al. Climate variability and Campylobacter infection: an international study. International Journal of Biometeorology 2005; 49: 207–214. [DOI] [PubMed] [Google Scholar]
- 15.Jore S, et al. Trends in Campylobacter incidence in broilers and humans in six European countries, 1997–2007. Preventive Veterinary Medicine 2010; 93: 33–41. [DOI] [PubMed] [Google Scholar]
- 16.Carrique-Mas J, et al. Risk factors for domestic sporadic campylobacteriosis among young children in Sweden. Scandinavian Journal of Infectious Diseases 2005; 37: 101–110. [DOI] [PubMed] [Google Scholar]
- 17.Spencer SEF, et al. The spatial and temporal determinants of campylobacteriosis notifications in New Zealand, 2001–2007. Epidemiology and Infection 2012; 140: 1663–1677. [DOI] [PubMed] [Google Scholar]
- 18.Green CG, Krause DO, Wylie JL. Spatial analysis of Campylobacter infection in the Canadian province of Manitoba. International Journal of Health Geographics 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Foodborne Disease Active Surveillance Network (FoodNet): FoodNet Surveillance Report for 2012. Atlanta, GA; 2014.
- 20.Ailes E, et al. Do differences in risk factors, medical care seeking, or medical practices explain the geographic variation in campylobacteriosis in Foodborne Diseases Active Surveillance Network (FoodNet) sites? Clinical Infectious Diseases 2012; 54 (Suppl. 5): S464–S471. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics. Vintage 2013 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010-July 1, 2013), by year, county, single-year of age (0, 1, 2, …, 85 years and over), bridged race, Hispanic origin, and sex. (http://www.cdc.gov/nchs/nvss/bridged_race.htm). Accessed 10 June 2015.
- 22.Howden LM, Meyer JA. 2010 Census briefs, age and sex composition: 2010 U.S. Department of Commerce Economics and Statistics Administration. U.S. Census Bureau (http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf). Accessed 18 June 2015.
- 23.National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties (http://www.cdc.gov/nchs/data_access/urban_rural.htm#urbancountries2013). Accessed 20 June 2015.
- 24.United States Department of Agriculture National Agricultural Statistics Service. The 2012 Census of Agriculture (http://www.agcensus.usda.gov/Publications/2012/Full_Report/Volume_1,_Chapter_2_County_Level/Michigan/). Accessed 28 Oct 2015.
- 25.Hurd S, et al. Clinical laboratory practices for the isolation and identification of Campylobacter in Foodborne Diseases Active Surveillance Network (FoodNet) sites: baseline information for understanding changes in surveillance data. Clinical Infectious Diseases 2012; 54 Suppl 5:S440–S445. [DOI] [PubMed] [Google Scholar]
- 26.White ANJ, et al. Environmental determinants of campylobacteriosis risk in Philadelphia from 1994 to 2007. Ecohealth 2009; 6: 200–208. [DOI] [PubMed] [Google Scholar]
- 27.Hald B, et al. Flies and Campylobacter infection of broiler flocks. Emerging Infectious Diseases 2004; 10: 1490–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nichols GL. Fly transmission of Campylobacter. Emerging Infectious Diseases 2005; 11: 361–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaboré H, et al. Association between potential zoonotic enteric infections in children and environmental risk factors in Quebec, 1999–2006. Zoonoses and Public Health 2010; 57: e195–e205. [DOI] [PubMed] [Google Scholar]
- 30.Gilpin BJ, et al. The transmission of thermotolerant Campylobacter sp. to people living or working on dairy farms in New Zealand. Zoonoses and Public Health 2008; 55: 352–360. [DOI] [PubMed] [Google Scholar]
- 31.Dale K, et al. Reported waterborne outbreaks of gastrointestinal disease in Australia are predominantly associated with recreational exposure. Australian New Zealand Journal of Public Health 2010; 34: 527–530. [DOI] [PubMed] [Google Scholar]
- 32.Karagiannis I, et al. A waterborne Campylobacter jejuni outbreak on a Greek island. Epidemiology and Infection 2010; 138: 1726–1734. [DOI] [PubMed] [Google Scholar]
- 33.Potter RC, Kaneene JB, Gardiner J. A comparison of Campylobacter jejuni enteritis incidence rates in high- and low-poultry-density counties: Michigan 1992–1999. Vector Borne and Zoonotic Diseases 2002; 2: 137–143. [DOI] [PubMed] [Google Scholar]
- 34.Potter RC, Kaneene JB, Hall WN. Risk factors for sporadic Campylobacter jejuni infections in rural michigan: a prospective case-control study. American Journal of Public Health 2003; 93: 2118–2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mughini-Gras L, et al. Campylobacteriosis in returning travellers and potential secondary transmission of exotic strains. Epidemiology and Infection 2014; 142: 1277–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bemis K, Marcus R, Hadler JL. Socioeconomic status and campylobacteriosis, Connecticut, USA, 1999–2009. Emerging Infectious Diseases 2014; 20: 1240–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sonnevend Á, et al. Lack of correlation between the 257C-to-T mutation in the gyrA gene and clinical severity of Campylobacter jejuni infection in a region of high incidence of ciprofloxacin resistance. Scandinavian Journal of Infectious Diseases 2011; 43: 905–911. [DOI] [PubMed] [Google Scholar]
- 38.Gillespie IA, et al. Investigating vomiting and/or bloody diarrhoea in Campylobacter jejuni infection. Journal of Medical Microbiology 2006; 55: 741–746. [DOI] [PubMed] [Google Scholar]
- 39.Davies EG. Immunodeficiency. In: AGM Campbell, N McIntosh, eds. Textbook of Pediatrics, 5th edn. London: Churchill Livingstone, 1988, pp. 1231–1272. [Google Scholar]
- 40.Ternhag A, et al. Mortality following Campylobacter infection: a registry-based linkage study. BMC Infectious Diseases 2005; 5: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]