Abstract
Introduction and hypothesis
Studies on the prevalence of urinary incontinence (UI) among CrossFit practitioners are on the rise. This systematic review with meta-analysis was aimed at determining the prevalence of UI among CrossFit practitioners.
Methods
A systematic review of the literature was performed by searching MEDLINE/PubMed, Scopus, and SPORTDiscus through January 2021. The search strategy included the keywords CrossFit, urine incontinence, exercise, high impact and pelvic floor dysfunction. The inclusion criterion was any study with a sample of CrossFit practitioners and results separated from the other fitness modalities analysed. The subjects were women with no restriction of age, parity, experience or frequency of training. Quality assessment of the studies included was conducted using the Oxford Centre of Evidence-Based Medicine scale and the Newcastle–Ottawa Scale (NOS) adapted for cross-sectional studies.
Results
Thirteen studies (6 comparative and 7 non-comparative) were included for the systematic review, all using a cross-sectional design. The level of evidence was 4, with their quality ranging from poor (n = 10) to fair (n = 3). A total of 4,823 women aged 18 to 71 were included, 91.0% participated in CrossFit, and 1,637 presented UI, which indicates a prevalence of 44.5%. Also, 55.3% and 40.7% presented mild or moderate UI respectively. Stress UI was the most common type reported (81.2%).
Conclusions
The factors that increased the likelihood of UI were age, body mass index and parity. Exercises based on jumps were commonly associated with urine leakage. CrossFit practitioners presented higher UI than control groups.
Keywords: Fitness, High-intensity functional training, Pelvic floor, Stress incontinence, Women's health
Introduction
CrossFit is an exercise regimen that has become the biggest fitness trend of the twenty-first century, and it is now considered a multi-million-dollar industry [1]. Despite its growing success and reported beneficial effects, current literature has questioned the safety of CrossFit practice based on a considerable injury risk owing to the high intensity at which exercises must be performed [2].
Regrettably, the potentially harmful effects of CrossFit practice might not end here. This fitness modality proposes the performance of high-intensity exercises executed repeatedly that demand high-impact movements. This training pattern may cause an increase in intra-abdominal pressure that in turn leads to an overload on the pelvic muscle floor [3, 4]. In addition, as there are few or no rest pauses during and between CrossFit workouts, neuromuscular fatigue is relatively present. This combination of increased intra-abdominal pressure, neuromuscular fatigue, and overloaded pelvic floor musculature due to strenuous exercise might lead to involuntary urine leakage, i.e. urinary incontinence (UI) [5]. Besides, other training characteristics common in CrossFit practitioners, such as the volume of weekly practice or the performance of heavy weightlifting exercises, can also be considered a predisposing factor for UI, especially among competitors [6, 7].
Studies on CrossFit users' profiles have indicated the existence of a high body mass index (BMI) among them, with mean values around 25 kg·m-2, and have also shown that people up to 58 years old are involved in its practice [8]. Similarly, there seems to be a considerable prevalence of multiparous women among CrossFit athletes [9]. As age and BMI have been identified as risk factors for sustaining UI, alongside parity, it is plausible that CrossFit could be associated with urine leakage among some practitioners [10].
Urinary incontinence may cause embarrassment and affect performance and quality of life [11]. It can also discourage people from participating in sport and exercise [7]. Thus, quality and up-to-date information concerning the existing risk of UI among CrossFit practitioners should be available to CrossFit trainers and sports fitness advisors in general. This goal can be achieved by conducting systematic reviews that synthesize and summarize the scientific evidence on the subject. Although several systematic reviews on the prevalence of UI among sports practitioners have been published [4, 5, 11–14], to our knowledge, none of them has provided specific information or have particularly focused on CrossFit so far. In the light of all the above issues, this systematic review and meta-analysis was aimed at determining the prevalence of UI and associated risk factors among CrossFit practitioners.
Materials and methods
A systematic review was carried out following the latest Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. The PRISMA 2020 27-item checklist is presented in Appendix 1. A protocol for this review is registered with the Open Science Framework (OSF), 10.17605/OSF.IO/EQ4YX.
Table 5.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 27-item checklist
| Section and topic | Item # | Checklist item | Page/document |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review | Title page |
| Abstract | |||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist | 1–2 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge | 3–4 |
| Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses | 4 |
| Methods | |||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses | 4–5 |
| Information sources | 6 | Specify all databases, registers, websites, organisations, reference lists and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted | 26 |
| Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used | 4, Appendix 2 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process | 5 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and if applicable, details of automation tools used in the process | 5 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g. for all measures, time points, analyses), and if not, the methods used to decide which results to collect | 5 |
| 10b | List and define all other variables for which data were sought (e.g. participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information | 5 | |
| Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the studies included, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process | 5 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g. risk ratio, mean difference) used in the synthesis or presentation of results | 5–6 |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g. tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)) | NR |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics, or data conversions | NR | |
| 13c | Describe any methods used to tabulate or visually display results of individual studies and syntheses | NR | |
| 13d | Describe any methods used to synthesise results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) used to identify the presence and extent of statistical heterogeneity, and the software package(s) used | 5–6 | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g. subgroup analysis, meta-regression) | 6 | |
| 13f | Describe any sensitivity analyses conducted to assess the robustness of the synthesised results | NR | |
| Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases) | NR |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome | NR |
| Results | |||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram | 6, Fig. 1 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded | 6 | |
| Study characteristics | 17 | Cite each study included and present its characteristics | 6, Table 3–Table 4 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each study included | 7, Table 1–Table 2 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g. confidence/credible interval), ideally using structured tables or plots | Table 3–Table 4 |
| Results of syntheses | 20a | For each synthesis, briefly summarise the characteristics and risk of bias among contributing studies | 8 |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g. confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect | 8, Fig. 2 | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results | NR | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesised results | NR | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed | NR |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed | NR |
| Discussion | |||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence | 10–12 |
| 23b | Discuss any limitations of the evidence included in the review | 12 | |
| 23c | Discuss any limitations of the review processes used | 12 | |
| 23d | Discuss the implications of the results for practice, policy and future research | 10–12 | |
| Other information | |||
| Registration and protocol | 24a | Provide registration information for the review, including register name and registration number, or state that the review was not registered | 4 |
| 24b | Indicate where the review protocol can be accessed, or state that a protocol was not prepared | 4 | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol | NR | |
| Support | 25 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review | 13 |
| Competing interests | 26 | Declare any competing interests of review authors | 13 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from the studies included; data used for all analyses; analytic code; any other materials used in the review | 13 |
From: Page et al. [15]. For more information, visit: http://www.prisma-statement.org
NR not reported
Search strategy
The following electronic databases were searched from their respective inceptions through January 2022: MEDLINE/PubMed, SPORTDiscus and Scopus. The following search terms, Boolean operators, and combinations were used: “CrossFit” (keyword alone) OR “Urine Incontinence” AND “Exercise” OR “Urine Incontinence” AND “High Impact” OR “Pelvic floor dysfunction” AND “Exercise”. Search strategies can be found in Appendix 2.
Eligibility criteria
To be selected for further analysis, the studies had to meet the following selection criteria:
To include CrossFit practitioners in their sample regardless of their age and sex.
To provide information on UI prevalence, severity and/or associated risk factors.
To be an observational or cross-sectional investigation.
Studies were excluded if:
The sample included athletes from several fitness or sport modalities and separate results were no provided for CrossFit practitioners.
The full text of the study was not available.
The research was not published in a peer-reviewed journal written in English, Portuguese or Spanish language.
The research was a review, a case report, a doctoral thesis, a letter to the editor or a conference abstract.
Study selection
Titles and abstracts of search results were screened for relevance, with full-text versions of potentially relevant articles obtained and assessed for inclusion. Eligibility was assessed independently by two authors with discrepancies resolved through discussion with a third researcher. The reference lists of the selected articles, as well as studies that quoted them, were checked for potential articles eligible for this review.
Data extraction
Information on CrossFit practitioners (mean age, parity, number of years performing CrossFit, recreational/competitive status), variables assessed (prevalence, severity and type of UI), associated factors with UI and outcomes were extracted from the original reports by one researcher and checked by a second investigator. Missing data were obtained from the study authors whenever possible.
Quality appraisal
According to a previous study [12], two researchers independently rated the quality of evidence according to the Oxford Centre of Evidence-Based Medicine (OCEBM) scale [16]. The assessment considered the thematic area and the type of the study, grading the evidence based on the best design for the “symptom prevalence study” scenario. Moreover, the quality of the included studies was evaluated as good, fair or poor based on thresholds described previously [17], using the Newcastle–Ottawa Scale adapted for cross-sectional studies [18]. The inconsistencies in coding process and quality assessment between the two researchers were resolved by consensus.
Statistical analysis
Data extracted from the articles were processed in an Excel spreadsheet, and we performed the statistical analysis using RevMan v5.4.1 software. We calculated the odds ratio (OR) with 95% confidence interval (CI) for dichotomous variables using a random-effects Mantel–Haenszel model. We used inverse variance or generic inverse variance to report mean differences for continuous data and their 95% CIs. We assessed heterogeneity using the Chi-squared test and I2 test.
Results
Study selection
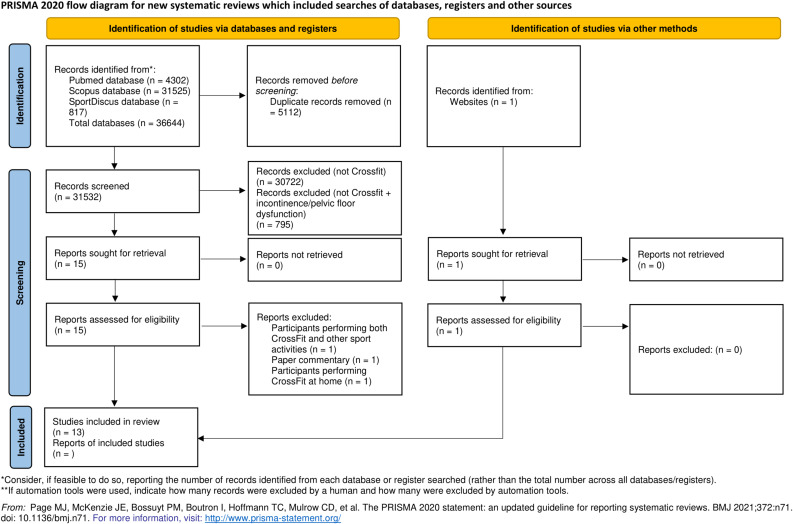
On the one hand, in identifying studies via databases and registers, 36,644 records were found (PubMed, Scopus and SPORTDiscus). After eliminating duplicates, 31,532 records were selected, of which 30,723 were excluded based on their title and abstracts. Thereafter, 15 full-text documents were reviewed, and 3 more documents were excluded. One was a commentary on a paper by Forner et al., entitled “Do women runners report more pelvic floor symptoms than women in CrossFit? A cross-sectional survey” [19]. Further, the study by Lúdvíksdóttir et al. [20] did not clarify whether CrossFit practitioners performed other sports activities concurrently. Another study analysed CrossFit training during the COVID-19 quarantine [21], so their participants were conditioned by the availability of home equipment. On the other hand, an additional record was identified through a website and assessed for eligibility. In the last stage, a total of 13 articles were included for the systematic review (Fig. 1).
Fig. 1.
Flow diagram of the search and selection process for the inclusion of articles
Designs and samples
The studies were categorised into comparative (n = 6) [22–27] and non-comparative (n = 7) [7, 9, 28–32]. All of them used a cross-sectional design. The pooled sample size was 4,823 individuals with 91% in the CrossFit group; all participants were females. The sample was composed of adults (18–71 years of age), and the mean age was 31.1 years.
Methodological quality assessment
Table 1 details the design of the studies, if they performed sample calculation and their sources of bias. It also reflects that all studies showed a level of evidence 4, because they were cross-sectional studies. Thus, the respective grade of recommendation is C, based on the criteria set forth by the OCEBM [16].
Table 1.
Methodological quality assessment
| Reference | OCEBM level of evidence | Study design | Sample size calculation | Sources of bias |
|---|---|---|---|---|
| Comparative studies | ||||
| Elks et al. [22] | 4 | Cross-sectional | Yes | Selection bias (i.e. voluntary response); unequal group size; self-reported data; exercise intensity was not controlled; inability to assess the survey participation rate |
| Forner et al. [23] | 4 | Cross-sectional | No | Selection bias (i.e. voluntary response); unequal group size; self-reported data; lack of questions about urine leakage during CF exercises; inability to assess the survey participation rate |
| Khowailed et al. [27] | 4 | Cross-sectional | No | Selection bias (i.e. voluntary response); small sample size; self-reported data; multigravida women were not adequately controlled; inability to assess the survey participation rate |
| De Machado et al. [26] | 4 | Cross-sectional | Yes | Selection bias (i.e. only nulliparous women aged between 18 and 35 years with a body mass index ≤ 30 kg/m2 were included; the folder disclosure was carried in a single institution of higher education); small sample size; sample size calculation based on a measure not used in the study; self-reported data; the recruitment rate was not assessed |
| Middlekauff et al.[25] | 4 | Cross-sectional | Yes | Selection bias (i.e. only nulliparous women aged between 18 and 35 years were included); self-reported data; the recruitment rate was not assessed |
| Yang et al. [24] | 4 | Cross-sectional | No | Selection bias (i.e. regional sample; voluntary response; some women did not participate in specific exercises); small sample size; unequal group size; self-reported data; the recruitment rate was not assessed |
| Non-comparative studies | ||||
| Poli De Araújo et al. [28] | 4 | Cross-sectional | Yes | Selection bias (i.e. voluntary response; heterogeneity of CF training experience); questionnaire not validated; self-reported data; inability to assess the survey participation rate |
| Dias et al. [29] | 4 | Cross-sectional | No | Selection bias (i.e. recruitment from a single CF centre; voluntary response; included women with only 1 month of CF practice); small sample size; the recruitment rate was not assessed |
| High et al. [9] | 4 | Cross-sectional | No | Selection bias (i.e. voluntary response); self-reported data; inability to assess the survey participation rate |
| Lopes et al. [30] | 4 | Cross-sectional | No | Selection bias (i.e. recruitment from only two CF centres; only women aged between 18 and 35 years were included; voluntary response; the majority of the sample had less than 1 year of experience in CF training); small sample size; self-reported data; the recruitment rate was not assessed |
| Pisani et al. [31] | 4 | Cross-sectional | No | Selection bias (i.e. voluntary response); self-reported data; inability to assess the survey participation rate |
| Pisani et al. [32] | 4 | Cross-sectional | No | Selection bias (i.e. voluntary response); self-reported data; inability to assess the survey participation rate |
| Wikander et al. [7] | 4 | Cross-sectional | No | Selection bias (i.e. competitive women CF participants were included; voluntary response); self-reported data; inability to assess the survey participation rate |
Abbreviations: CF CrossFit, OCEBM Oxford Centre of Evidence-Based Medicine, UI urinary incontinence
Furthermore, a summary of the quality assessment using the Newcastle–Ottawa Scale adapted for cross-sectional studies is shown in Table 2. The 13 included studies obtained fair or poor ratings. In the selection domain, ascertainment of exposure was well demonstrated across all studies. On the contrary, none of the included studies disclosed the response rate. Seven studies were considered somewhat representative of the average in the target population; however, the remaining six were based on a selected group of users. Also, only six studies conducted power analysis for sample size estimation or justified their sample size. Regarding comparability, controlling for age was deemed the most important factor, followed by parity or body mass index. Six of the studies controlled for a combination of these factors, whereas the other seven studies lacked adjustment for possible confounders. In the outcome domain, the 13 studies performed well in assessment of the UI outcomes. Finally, seven of the studies did not perform well in statistical tests, as they did not provide confidence intervals. Overall, 10 out of 13 studies achieved a poor quality rating, whereas 3 studies received a fair quality rating.
Table 2.
Newcastle–Ottawa Scale, adapted for quality assessment of cross-sectional studies
| Reference | Selection (maximum 5 stars) | Comparability (maximum 2 stars)a | Outcome (maximum 3 stars) | Quality rating (maximum 10 stars)b | ||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of the sample (☆) | Sample size (☆) | Non-respondents (☆) | Ascertainment of the exposure (☆☆) | Based on design and analysis (☆☆) | Assessment of the outcome (☆☆) | Statistical test (☆) | ||
| Elks et al. [22] | ☆ | ☆ | ☆ | ☆☆ | ☆ | Poor (6/10 stars) | ||
| Forner et al. [23] | ☆ | ☆ | ☆ | Poor (3/10 stars) | ||||
| Khowailed et al. [27] | ☆ | ☆ | Poor (2/10 stars) | |||||
| De Machado et al. [26] | ☆ | ☆ | ☆ | Poor (3/10 stars) | ||||
| Middlekauff et al.[25] | ☆ | ☆ | ☆ | ☆ | Poor (4/10 stars) | |||
| Yang et al. [24] | ☆ | ☆☆ | ☆ | ☆ | Poor (5/10 stars) | |||
| Poli De Araújo et al. [28] | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | Fair (7/10 stars) | |
| Dias et al. [29] | ☆ | ☆ | Poor (2/10 stars) | |||||
| High et al. [9] | ☆ | ☆ | ☆☆ | ☆ | ☆ | Poor (6/10 stars) | ||
| Lopes et al. [30] | ☆ | ☆ | ☆ | Poor (3/10 stars) | ||||
| Pisani et al. [31] | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | Fair (7/10 stars) | |
| Pisani et al. [32] | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | Fair (7/10 stars) | |
| Wikander et al. [7] | ☆ | ☆ | Poor (2/10 stars) | |||||
Abbreviations: max, maximum aOne ☆ was allocated if the study adjusted for age, with an additional ☆ given if adjusted for parity or body mass index
bScores were allocated for urinary incontinence outcomes. Good quality: 4–5 stars in the selection domain, 1–2 stars in the comparability domain, and 2–3 stars in the outcome domain. Fair quality: 3 stars in the selection domain, 1–2 stars in the comparability domain and 2–3 stars in the outcome domain. Poor quality: 1–2 stars in the selection domain or 0 stars in the comparability domain or 0–1 star(s) in the outcome domain
Overview of study characteristics
Ten studies (77%) were aimed at determining the prevalence of UI among CrossFit practitioners, whereas the remaining three (23%) analysed prevalence data as a secondary outcome. Great heterogeneity was detected, mainly because different questionnaires were used and because of the lack of a standardised definition of UI. The severity and type of UI were analysed in five and six investigations respectively. Again, heterogeneity was observed in the questionnaires and classifications employed to collect data. Only two out of the five studies that included UI severity as an outcome used a standard definition, which was adapted from the International Urogynecological Association and the International Continence Society. Four investigations administered the Incontinence Symptoms Severity Index, whereas the remaining study used the International Consultation of Incontinence Questionnaire-Short Form (ICIQ-SF). All studies included parity information, and only one article reported data on the prevalence of UI before the beginning of CrossFit practice.
The following variables related to CrossFit practice were included in the scientific literature: training load (n = 10), CrossFit experience (n = 9), most common exercises associated with UI (n = 6) and competitive experience (n = 2). Hardly any associations between these factors and UI were found, except for the type of exercise performed. A total of seven investigations revealed that CrossFit exercises based on jumps (single jump rope and double unders, as well as box jumps) increased the likelihood of urine leakage. The characteristics and main findings of the studies reviewed are depicted in Table 3 (comparative studies) and Table 4 (non-comparative studies).
Table 3.
Comparative studies assessing urinary incontinence (UI) among female CrossFit practitioners (CFG) and control participants (CG)
| Reference, country and sample | Variables (tools) | Participants with UI, severity and type | Factors associated with UI | Comparative results CFG-CG |
|---|---|---|---|---|
| Elks et al. [22], USA | ||||
| 423 women (mean age; range): | Prevalence: | Women with UI (n): | Multiparity | Prevalence (proportion of each group; p value): |
| CFG: n = 322 (38; 30–45 years) | UDI-6 | CFG: 256 | Vaginal delivery | UI: CFG 84% vs CG 48%; p < 0.001 |
| CG: n = 101 (31; 26.5–39.5 years) | POPDI-6 | Severity (n): | Postmenopausal status | Severity (proportion of each group; p value): |
| Parity (n): | Severity: | Slight: 133 | Body mass index | Slight: CFG 44% vs CG 34%; p < 0.001 |
| CFG: 3 | ISI | Moderate: 116 | Pelvic surgery | Moderate: CFG 38% vs CG 14%; p < 0.001 |
| CG: 3 | Type: | Severe: 7 | CF exercises (n; proportion of CFG): | Severe: CFG 2% vs CG 0%; p < 0.001 |
| CF experience: NR | Specific items | Type (n): | Jump rope DU: 166; 65% | Type (proportion of each group; p value): |
| Competitive status: NR | SUI: 186 | SUI: CFG 73% vs CG 47%; p < 0.001 | ||
| UUI: 140 | UUI: CFG 55% vs CG 42%; p = 0.02 | |||
| MUI: 128 | MUI: CFG 50% vs CG 31%; p < 0.001 | |||
| Forner et al. [23], Australia | ||||
| 1,379 women (mean age ± SD): | Prevalence: | Women with UI: NR | Parity | Prevalence (proportion of each group): |
| CFG: n = 858 (38.5 ± 8.8 years) | UDI-6 | Severity: NR | UI: CFG 50.4 % vs CG 51.6 % | |
| CG: n = 521 (38.4 ± 9.2 years) | CRADI-8 | Type (n): | Severity: NR | |
| Parity (n): | POPDI-6 | SUI: 355 | Type (proportion of each group; p value): | |
| CFG: 433 | Severity: NR | UUI: 208 | SUI: | |
| CG: 295 | Type: | MUI: 410 | Parous: CFG 51.5% vs CG 8.1%; p = 0.362 | |
| CF experience: NR | UDI-6 | Nulliparous: CFG 30% vs CG 23.9 %; p = 0.098 | ||
| Competitive status: NR | UUI: | |||
| Parous: CFG 29% vs CG 36.3%; p = 0.037 | ||||
| Nulliparous: CFG 19% vs CG 21.7%; p = 0.413 | ||||
| MUI: | ||||
| Parous: CFG 57.3% vs CG 57.3%; p = 0.997 | ||||
| Nulliparous: CFG 37.2% vs CG 34.5%; p = 0.502 | ||||
| Khowailed et al. [27], USA | ||||
| 14 women (mean age; range) | Prevalence: | Women with UI (n): | Parity | Prevalence (proportion of each group; p value): |
| CFG: n = 9 (29; 18–40 years) | Carls’ UI survey | CFG: 6 | CF exercises (n; proportion of CFG): | CFG > CG; p = 0.023 |
| CG: n = 5 (29; 18–40 years) | Severity: NR | CG: 2 | Jumps: 7; 77.8% | Severity: NR |
| Parity (n): 4 | Type: NR | Severity: NR | Running: 6; 66.7% | Type: NR |
| CF experience: NR | Type: NR | Lifting: 3; 33.3% | ||
| Competitive status: NR | ||||
| De Machado et al. [26], Brazil | ||||
| 41 women (mean age ± SD) | Prevalence: | Women with UI (n): | CF exercises (n): | Prevalence (proportion of each group; p value): |
| CFG: n = 20 (27.4 ± 3.7 years) | ICIQ-SF | CFG: 12 | Jumps: NR | UI: CFG 60% vs CG 9.5%; p < 0.001 |
| CG: n = 21 (25.8 ± 3.4 years) | Severity: | Severity (n): | Lifting: NR | Severity (proportion of each group): |
| Parity (n): 0 | ICIQ-SF | Mild: 2 | Mild: CFG 9.5% vs CG 0% | |
| CF experience (mean; range): | Type: NR | Moderate: 10 | Moderate: CFG 50% vs CG 9.5% | |
| 22; 6–60 months | Severe: 0 | Severe: 0 | ||
| Competitive status (n): | Very severe: 0 | Very severe: 0 | ||
| CFG = 12 | Type: NR | Type: NR | ||
| Middlekauff et al.[25],, USA | ||||
| 70 women (mean age ± SD) | Prevalence: | Women with UI (n): | No statistically significant associations were found | Prevalence (proportion of each group): |
| CFG: n = 35 (26.8 ± 3.8 years) | EPIQ and POP-Q | CFG: 9 | UI: CFG 27.7% vs CG 8.5% | |
| CG: n = 35 (22.7 ± 3.9 years) | Severity: NR | Severity: NR | Severity: NR | |
| Parity (n): 0 | Type: NR | Type: NR | Type: NR | |
| CF experience (mean ± SD): | ||||
| 22.1 ± 12.3 months | ||||
| Competitive status: NR | ||||
| Yang et al. [24], USA | ||||
| 149 women (mean age): | Prevalence: | Women with UI (n): | Parity | Prevalence (proportion of each group): |
| CFG: n = 105 (36.9 years) | ISSI | CFG: 53 | Vaginal delivery | UI: CFG 55.6% vs CG 31.8% |
| CG: n = 44 (29.0 years) | Severity: | Severity (n): | CF exercises (n; proportion of CFG): | Severity: NR |
| Parity (n): | ISSI | Mild: 34 | Jump rope DU: 50; 94.3% | Type: NR |
| CFG: 67 | Type: NR | Moderate to severe: 19 | Jump rope SU: 43; 81.1% | |
| CF experience: NR | Type: NR | Box jump: 30; 56.6% | ||
| Competitive status: NR | ||||
Abbreviations: CF CrossFit, CRADI-8 Colorectal–Anal Distress Inventory-8, DU double unders, EPIQ Epidemiology of Prolapse and Incontinence Questionnaire, ISI Incontinence Severity Index, ISSI Incontinence Symptom Severity Index, MUI mixed urinary incontinence, NR not reported, POPDI-6 Pelvic Organ Prolapse Distress Inventory-6, POP-Q Pelvic Organ Prolapse Quantifications System, SU single unders, SUI stress urinary incontinence, UDI-6 Urinary Distress Inventory-6, UUI urgency urinary incontinence
Table 4.
Non-comparative studies assessing urinary incontinence (UI) among female CrossFit practitioners
| Reference, country and sample | Variables (tools) | Participants with UI, severity and type | Risk factors |
|---|---|---|---|
| Poli De Araújo et al. [28], Brazil | |||
| 551 women | Prevalence: NR | Women with UI (n): 165 | Age |
| Mean age ± SD; range: 31.8 ± 7.4; 16–64 years | Severity: NR | Severity: NR | CF exercises (n; proportion of those with UI): |
| Parity (n): 175 | Type: NR | Type: NR | Jump rope DU: 111; 67.3% |
| CF experience of parous women (n): | Jump rope SU: 44; 26.7% | ||
| < 6 months: 38 | |||
| 7–23 months: 20 | |||
| 24+ months: 117 | |||
| Competitive status: NR | |||
| Dias et al. [29], Brazil | |||
| 34 women | Prevalence: | Women with UI (n): 5 | Multiparity |
| Mean age ± SD: 30.3 ± 6.4 years | Questionnaire by researchers | Severity: NR | Vaginal delivery |
| Parity (n): 8 | Severity: NR | Type (n): | CF training frequency |
| CF experience (n): | Type: | UUI: 3 | |
| < 6 months: 8 | Questionnaire by researchers | ||
| 7–23 months: 20 | |||
| 24+ months: 6 | |||
| Competitive status: NR | |||
| High et al. [9], USA | |||
| 314 women | Prevalence: | Women with UI (n): 82 | Parity |
| Mean age ± SD; range: 36 ± 10; 20–71 years | PFDI-20 | Severity: NR | Vaginal delivery |
| Parity (n): 180 | IIQ | Type (n): | Age |
| CF experience (mean ± SD): 46 ± 30 months | ICIQ-SF | SUI: 49 | |
| Competitive status: NR | Severity: NR | UUI: 42 | |
| Type: ICIQ-SF | |||
| Lopes et al. [30], Brazil | |||
| 50 women | Prevalence: | Women with UI (n): 10 | No statistically significant associations were found |
| Mean age ± SD; range: 28.6 ± 4.5; 18–35 years | ICIQ-SF | Severity: NR | |
| Parity (n): 3 | Severity: NR | Type (n): | |
| CF experience (n): | Type: | SUI: 8 | |
| < 12 months: 29 | ICIQ-SF | UUI: 1 | |
| 12–24 months: 9 | MUI: 1 | ||
| 24+ months: 12 | |||
| Competitive status: NR | |||
| Pisani et al. [31], Brazil | |||
| 828 women | Prevalence: | Women with UI (n): 298 | Gestation |
| Mean age ± SD: 31.4 ± 7.6 years | ICIQ-SF | Severity of urine loss amount (n): | Multigravida |
| Parity (n): 98 | Severity: NR | Small: 268 | History of: |
| CF experience (n): | Type: | Moderate: 25 | Sexual dysfunction |
| < 6 months: 37 | ICIQ-SF | Large: 5 | Pelvic organ prolapses |
| 6–12 months: 60 | Type (n): | Vaginismus | |
| 12–24 months: 115 | SUI: 263 | Dyspareunia | |
| 24+ months: 86 | UUI: 16 | ||
| Competitive status: NR | MUI: 19 | ||
| Pisani et al. [32], Brazil | |||
| 828 women | Prevalence: | Women with UI (n): 298 | Vaginal delivery: ×2.1 risk |
| Mean age ± SD: 30.6 ± 6.6 years | ICIQ-SF | Severity: NR | CF training frequency >5/week: ×3 risk |
| Parity (n): 212 | Severity: NR | Type (n): | CF exercises (n; proportion of those with UI): |
| CF experience (n): | Type: | SUI: 263 | Jump rope DU: 152; 51.0% |
| < 6 months: 98 | ICIQ-SF | UUI: 16 | Jump rope SU: 100; 33.6% |
| 6–12 months: 173 | MUI: 19 | Box jump: 63; 21.1% | |
| 12–24 months: 313 | Running: 38; 12.8% | ||
| 24+ months: 244 | Front squat: 30; 10.0% | ||
| Competitive status (n): | |||
| 0 participations/year: 499 | |||
| 1 participations/year: 174 | |||
| 2 participations/year: 101 | |||
| >2 participations/year: 54 | |||
| Wikander et al. [7], Australia | |||
| 452 women | Prevalence: NR | Women with UI (n): 208 | Multiparity |
| Mean age ± SD; range: 36 ± 9; 20–63 years | Severity: | Severity (n)c: | Exercises (n; proportion of those with UI): |
| Parity: NR | ISI | Slight: 89 | Jump rope SU: 177; 85.1% |
| CF experience: | Type: NR | Moderate: 83 | Jump rope DU: 167; 80.8% |
| Type 1 (n = 44)a: 4.4 ± 2.5 years | Severe: 6 | Running: 93; 44.7% | |
| Type 2 (n = 36)b: 3.7 ± 2.4 years | Very severe: 5 | Box jump: 85; 40.9% | |
| Competitive status: NR | Type: NR | Deadlift: 62; 29.8% | |
| Previous UI (n; proportion): 189; 41.8% | Back squat: 57; 27.4% | ||
| Front squat: 54; 26.0% | |||
Abbreviations: CF CrossFit, DU double unders, ICIQ-SF International Consultation on Incontinence Questionnaire Short-Form, ISI Incontinence Severity Index, IIQ Incontinence Impact Questionnaire, MUI mixed urinary incontinence, NR not reported, PFDI-20 Pelvic Floor Distress Inventory Short Form-20, SU single unders, SUI stress urinary incontinence, UUI urgency urinary incontinence
aUI prior to CF practice, during daily activities but not during training or competitions
bUI prior to CF practice, not during daily activities but during training
cThe total number of participants reporting the severity of their UI (n = 183) differs from the total number of participants reporting UI (n = 208)
Prevalence, severity and types of UI among CrossFit practitioners
From a total of 3,682 CrossFit practitioners assessed, 1,637 presented UI, which indicates a prevalence of 44.46%. The severity of UI was noted in five studies. A total of 55.3% and 40.7% of the cases were deemed as mild or moderate UI respectively. Stress UI (SUI) was the most common type reported (81.2%) based on the six studies that provided data on this matter.
Meta-analysis
Findings from the six comparative studies indicated that participants were younger in control groups than in CrossFit groups, with a mean difference of 2.11 years (95% CI 1.38–2.83, p < 0.001), and had a lower BMI, with a mean difference of 1.03 kg·m−2 (95% CI 0.67–1.39, p < 0.001). In both cases there was substantial heterogeneity among studies (I2 = 92% for age and I2 = 81% for BMI, p < 0.001 for both comparisons).
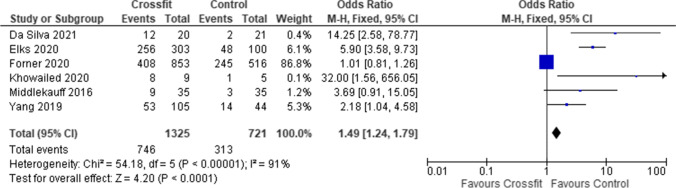
When comparing the prevalence of UI, higher odds of presenting UI in the CrossFit groups than in the control groups (OR 1.49; 95% CI 1.24–1.79, p < 0.001) were identified. A considerable heterogeneity among studies was found (I2 = 91%, p < 0.001; Fig. 2).
Fig. 2.
Total prevalence of urinary incontinence among CrossFit practitioners
The meta-analysis performed by pooling data from CrossFit practitioners showed that those reporting UI were older, with a mean difference of 2.02 years (95% CI 1.24–2.80, p < 0.001; moderate heterogeneity, I2 = 46%, p = 0.14). Also, CrossFit practitioners presenting UI had a higher BMI, with a mean difference of 0.31 kg·m−2 (95% CI 0.02–0.60, p = 0.03; substantial heterogeneity, I2 = 78%, p = 0.003). Parity was also related to UI, as athletes reporting UI had higher odds of having an antecedent of parity (OR 2.58, 95% CI 2.05–3.26; p < 0.001; moderate heterogeneity, I2 = 51%, p = 0.13).
Discussion
This systematic review was aimed at synthesising and critically revising the currently available scientific evidence regarding the prevalence of UI among CrossFit practitioners. The results obtained mainly came from studies that showed a low to fair methodological quality, limiting the applicability of the data analysed. Nevertheless, some interesting findings are worthy of discussion.
After pooling the data of the 13 investigations reviewed, a UI prevalence of around 45% was revealed in the first place. Studies on the presence of UI among the general female population have shown a wide range of prevalence rates. For instance, judging from the data presented in the review by Hunskaar et al. [33], UI affected between 12–42% of women below the age of 60 years, whereas, based on the results of the epidemiological survey performed by Hannestad et al. [34], a mean prevalence of around 25% was reported. A more recent review indicated a prevalence of UI ranging from 5% to 70% after analysing several population studies from different countries [35]. This disparity in UI prevalence can be attributed to differences in the methodological design and especially to different UI definitions. For instance, according to relevant and well-designed studies on the epidemiology of UI that used standardised definitions and validated questionnaires, the prevalence of UI was around 25–27% [36], which would indicate that CrossFit practitioners are more likely to present UI than women in general.
Nevertheless, prevalence rates are also affected by the target population's characteristics. Therefore, data obtained from studies with similar samples enable a more accurate discussion of the prevalence of UI observed in the present review. In this regard, population-based studies in women of around the same age interval as in the reviewed investigations indicated a prevalence ranging from 6% [37] to 42.5% [38]. Findings from meta-analyses on female athletes have pointed out a weighted average of 26–36% of UI prevalence [5, 13]. According to the data obtained in the present review, CrossFit seems to exhibit a moderate prevalence rate that somehow falls between sports with low percentages such as cycling (10%) or swimming (15%) and high-impact modalities such as volleyball (57.5%), gymnastics (61%) or trampoline (>80%) [11, 12].
Strenuous exercise has been cited as a risk factor for developing symptoms of SUI [14]. The pooled data confirmed that SUI was the most prevalent type, according to previous findings in female athletes [39] and among women who exercised regularly [40].
Our meta-analysis also showed that CrossFit practitioners had higher odds of presenting UI in comparison with the control groups included in the comparative studies reviewed. The latter is somehow an expected finding, previously reported in investigations comparing female athletes with the general population [12, 13, 41]. However, the OR results must be interpreted cautiously as significant differences in age and body composition were found between the two groups. Therefore, no causal relationship can be extracted from the data analysed as significant differences in age and body composition were found between the groups. Moreover, only one of the studies reviewed informed the prevalence of UI before women started CrossFit practice.
Age, parity and BMI are well-known risk factors for UI for several reasons. The striated urethral sphincter, which is considered a major contributor to urinary continence control (since it provides a direct closure force at the mid-urethra), experiences a decline in its function with age owing to a decrease in its relative volume [42]. Parity is consistently related to UI because of disruption of pelvic floor structures and to denervation, which cause a drop in the pelvic muscle floor functionality, especially after the first vaginal delivery [43]. Body mass index has been linked to intra-abdominal pressure and intravesical pressure, which overcomes urethral closing pressure and leads to incontinence [44]. In addition, oxidative stress from visceral adipose tissue is likely to have a negative effect on the collagen and supportive structures of the pelvic floor, which confer continence [45]. Our meta-analysis indicates that these three factors are associated with UI among CrossFit practitioners. These results can help trainers to identify women who are more prone to presenting this problem and to develop preventive strategies. In this regard, controlling contributing factors such as eating disorders, smoking or caffeine and alcohol consumption are recommended. Athletes should also be encouraged to avoid excessive fluid consumption and void shortly before training and include specific exercises to strengthen the pelvic floor musculature in their routines [46].
Trainers should also pay attention to the selection of exercises for each workout of the day. This review revealed that specific CrossFit exercises, mainly those based on jumps, were frequently associated with UI. This fact might be the consequence of an increase in intra-abdominal pressure resulting from the performance of high-impact activities that, in turn, overload the pelvic floor. In addition, the force reaction of the feet with the ground transfers that shock to the pelvic organs, predisposing them to UI [13].
Several limitations should be accounted for when interpreting the findings of this review. First, considerable heterogeneity was detected in the studies. Second, data mostly came from cross-sectional designs through convenience sampling. Third, information on several confounding factors such as the use of hormones, types of birth or gynaecological surgeries was seldom given. Fourth, studies included only women. Finally, the existence of certain methodological limitations inherent to the review design (e.g. language restrictions, not having reviewed grey literature or publication bias) should be considered as well, as they may have conditioned the present results.
In summary, the prevalence of UI among CrossFit practitioners was found to be around 45%. Age, body mass index and parity appeared to be factors that increased the likelihood of UI, whereas exercises based on jumps were commonly associated with urine leakage. In comparison with control groups, CrossFit practitioners showed higher odds of presenting UI. Nevertheless, it should be taken into account that the scientific evidence found came from observational studies with great heterogeneity and wide confidence intervals. These features can result in inconsistency and imprecision in the reported outcomes. In addition, limitations with the design and execution of the study were also present as not all the investigations included a comparison group. Moreover, in very few studies, the prevalence of UI was compared before and after undergoing a CrossFit training program. Thus, the current findings must be interpreted within the context of a low quality of evidence [47]. According to the above issues, it is very difficult to draw solid conclusions to confirm whether the practice of CrossFit should not be recommended based on an increased risk of sustaining UI Table 5.
Appendix 1
Appendix 2
Search strategy #1 in PubMed—263 results
(CrossFit [Title/Abstract])
Search strategy #2 in Scopus—1,271 results
(CrossFit [Title/Abstract])
Search strategy #3 in SPORTDiscus—523 results
(CrossFit [Title/Abstract])
Search strategy #4 in PubMed—4,039 results
((incontinence urinary AND exercise [Title/Abstract]) OR (incontinence urinary AND high impact [Title/Abstract]) OR (pelvic floor dysfunction AND exercise [Title/Abstract]))
Search strategy #5 in Scopus—30,254 results
((incontinence urinary AND exercise [Title/Abstract]) OR (incontinence urinary AND high impact [Title/Abstract]) OR (pelvic floor dysfunction AND exercise [Title/Abstract]))
Search strategy #6 in SPORTDiscus—294 results
((incontinence urinary AND exercise [Title/Abstract]) OR (incontinence urinary AND high impact [Title/Abstract]) OR (pelvic floor dysfunction AND exercise [Title/Abstract]))
Author’s participation
E. Dominguez-Antuña: data collection, data analysis, manuscript writing; J.C. Diz: data analysis, manuscript writing; D. Suárez-Iglesias: data analysis, manuscript writing/editing; C. Ayán: project development, data analysis, manuscript writing.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Conflicts of interest
None.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dawson MC. CrossFit: fitness cult or reinventive institution? Int Rev Sociol Sport. 2015;52(3):361–379. doi: 10.1177/1012690215591793. [DOI] [Google Scholar]
- 2.Barranco-Ruiz Y, Villa-González E, Martínez-Amat A, Da Silva-Grigoletto ME. Prevalence of injuries in exercise programs based on CrossFit®, cross training and high-intensity functional training methodologies: a systematic review. J Hum Kinet. 2020;73(1):265. doi: 10.2478/hukin-2020-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gephart LF, Doersch KM, Reyes M, Kuehl TJ, Danford JM. Intraabdominal pressure in women during CrossFit exercises and the effect of age and parity. Baylor Univ Med Cent Proc. 2018;31(3):289–293. doi: 10.1080/08998280.2018.1446888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bø K. Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sport Med. 2004;34(7):451–464. doi: 10.2165/00007256-200434070-00004. [DOI] [PubMed] [Google Scholar]
- 5.Pires T, Pires P, Moreira H, Viana R. Prevalence of urinary incontinence in high-impact sport athletes: a systematic review and meta-analysis. J Hum Kinet. 2020;73(1):288. doi: 10.2478/hukin-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Da Roza T, Brandão S, Mascarenhas T, Jorge RN, Duarte JA. Urinary incontinence and levels of regular physical exercise in young women. Int J Sports Med. 2015;36(9):776–780. doi: 10.1055/s-0034-1398625. [DOI] [PubMed] [Google Scholar]
- 7.Wikander L, Kirshbaum MN, Gahreman DE. Urinary incontinence and women CrossFit competitors. Int J Womens Health. 2020;12:1189–1195. doi: 10.2147/IJWH.S278222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sprey JWC, Ferreira T, de Lima MV, Duarte A, Jorge PB, Santili C. An epidemiological profile of CrossFit athletes in Brazil. Orthop J Sport Med. 2016;4(8):2325967116663706. doi: 10.1177/2325967116663706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.High R, Thai K, Virani H, Kuehl T, Danford J. Prevalence of pelvic floor disorders in female CrossFit athletes. Female Pelvic Med Reconstr Surg. 2020;26(8):498–502. doi: 10.1097/SPV.0000000000000776. [DOI] [PubMed] [Google Scholar]
- 10.Xie X, Chen Y, Khan A, Long T, Li S, Xie M. Risk factors for urinary incontinence in Chinese women: a cross-sectional survey. Female Pelvic Med Reconstr Surg. 2021;27(6):377–381. doi: 10.1097/SPV.0000000000000871. [DOI] [PubMed] [Google Scholar]
- 11.Rial Rebullido T, Gómez-Tomás C, Faigenbaum AD, Chulvi-Medrano I. The prevalence of urinary incontinence among adolescent female athletes: a systematic review. J Funct Morphol Kinesiol. 2021;6(1):12. doi: 10.3390/jfmk6010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Mattos Lourenco TR, Matsuoka PK, Baracat EC, Haddad JM. Urinary incontinence in female athletes: a systematic review. Int Urogynecol J. 2018;29(12):1757–1763. doi: 10.1007/s00192-018-3629-z. [DOI] [PubMed] [Google Scholar]
- 13.Teixeira RV, Colla C, Sbruzzi G, Mallmann A, Paiva LL. Prevalence of urinary incontinence in female athletes: a systematic review with meta-analysis. Int Urogynecol J. 2018;29(12):1717–1725. doi: 10.1007/s00192-018-3651-1. [DOI] [PubMed] [Google Scholar]
- 14.Almousa S, Bandin Van Loon A. The prevalence of urinary incontinence in nulliparous female sportswomen: a systematic review. J Sports Sci. 2019;37(14):1663–1672. doi: 10.1080/02640414.2019.1585312. [DOI] [PubMed] [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):1–11. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.OCEBM Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine [Internet]. Accessed 6 March 2022. Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence
- 17.Anthony M, Lin F. A systematic review for functional neuroimaging studies of cognitive reserve across the cognitive aging spectrum. Arch Clin Neuropsychol. 2018;33(8):937–948. doi: 10.1093/arclin/acx125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13(1):1–17. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koch M. Commentary on ‘Do women runners report more pelvic floor symptoms than women in CrossFit? A cross-sectional survey’ by Forner et al. Int Urogynecol J. 2021;32(2):303. doi: 10.1007/s00192-020-04602-z. [DOI] [PubMed] [Google Scholar]
- 20.Lúdvíksdóttir I, Hardardóttir H, Sigurdardóttir P, Ulfarsson GF. Comparison of pelvic floor muscle strength in competition-level athletes and untrained women. Laeknabladid. 2018;104(3):133–138. doi: 10.17992/lbl.2018.03.177. [DOI] [PubMed] [Google Scholar]
- 21.De AMP, Brito LGO, Pochini ADC, Ejnisman B, Sartori MGF, Girão MJBC. Prevalence of urinary incontinence in CrossFit practitioners before and during the COVID-19 quarantine and its relationship with training level: an observational study. Rev Bras Ginecol Obstet. 2021;43(11):847–852. doi: 10.1055/s-0041-1739463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elks W, Jaramillo-Huff A, Barnes KL, Petersen TR, Komesu YM. The Stress Urinary Incontinence in CrossFit (SUCCeSS) Study. Female Pelvic Med Reconstr Surg. 2020;26(2):101–106. doi: 10.1097/SPV.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 23.Forner LB, Beckman EM, Smith MD. Do women runners report more pelvic floor symptoms than women in CrossFit®? A cross-sectional survey. Int Urogynecol J. 2020;32(2):295–302. doi: 10.1007/s00192-020-04531-x. [DOI] [PubMed] [Google Scholar]
- 24.Yang J, Cheng JW, Wagner H, Lohman E, Yang SH, Krishingner GA, et al. The effect of high impact CrossFit exercises on stress urinary incontinence in physically active women. Neurourol Urodyn. 2019;38(2):749–756. doi: 10.1002/nau.23912. [DOI] [PubMed] [Google Scholar]
- 25.Middlekauff ML, Egger MJ, Nygaard IE, Shaw JM. The impact of acute and chronic strenuous exercise on pelvic floor muscle strength and support in nulliparous healthy women. Am J Obstet Gynecol. 2016;215(3):316.e1–316.e7. doi: 10.1016/j.ajog.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 26.Da Machado LS, Marques Cerentini T, Laganà AS, Viana da Rosa P, Fichera M, Telles da Rosa LH. Pelvic floor evaluation in CrossFit® athletes and urinary incontinence: a cross-sectional observational study. Women Health. 2021;61(5):490–499. doi: 10.1080/03630242.2021.1927288. [DOI] [PubMed] [Google Scholar]
- 27.Khowailed IA, Pinjuv-Turney J, Lu C, Lee H. Stress incontinence during different high-impact exercises in women: a pilot survey. Int J Environ Res Public Health. 2020;17(22):1–9. doi: 10.3390/ijerph17228372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poli De Araújo M, Brito LGO, Rossi F, Garbiere ML, Vilela ME, Bittencourt VF. Prevalence of female urinary incontinence in CrossFit practitioners and associated factors: an Internet population-based survey. Female Pelvic Med Reconstr Surg. 2020;26(2):97–100. doi: 10.1097/SPV.0000000000000823. [DOI] [PubMed] [Google Scholar]
- 29.Dias M, de Melo VL, Ferreira L, Roussenq SC, Lenzi J, dos Santos JM, et al. Is the frequency of CrossFit practice correlated with stress urinary incontinence? A transversal study of prevalence/A frequência da prática de crossfit está correlacionada com a incontinência urinária de esforço? um estudo transversal de prevalência. Braz J Dev. 2021;7(5):47084–47095. [Google Scholar]
- 30.Lopes E, Apolinário A, Barbosa L, Moretti E. Frequency of urinary incontinence in women who practice CrossFit: a cross-sectional study. Fisioter Pesqui. 2021;27(3):287–292. doi: 10.1590/1809-2950/19028227032020. [DOI] [Google Scholar]
- 31.Pisani GK, de Sato TO, de Carvalho DHT, Carvalho C. Impact of urinary incontinence on quality of life in female CrossFit practitioners: a cross-sectional study. Eur J Obstet Gynecol Reprod Biol. 2022;1(268):56–61. doi: 10.1016/j.ejogrb.2021.11.424. [DOI] [PubMed] [Google Scholar]
- 32.Pisani GK, de Oliveira ST, Carvalho C. Pelvic floor dysfunctions and associated factors in female CrossFit practitioners: a cross-sectional study. Int Urogynecol J. 2021;32(11):2975–2984. doi: 10.1007/s00192-020-04581-1. [DOI] [PubMed] [Google Scholar]
- 33.Hunskaar S, Arnold EP, Burgio K, Diokno AC, Herzog AR, Mallett VT. Epidemiology and natural history of urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(5):301–319. doi: 10.1007/s001920070021. [DOI] [PubMed] [Google Scholar]
- 34.Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT Study. J Clin Epidemiol. 2000;53(11):1150–1157. doi: 10.1016/S0895-4356(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 35.Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217–222. doi: 10.1080/13697137.2018.1543263. [DOI] [PubMed] [Google Scholar]
- 36.Serati M, Ghezzi F. The epidemiology of urinary incontinence: a case still open. Ann Transl Med. 2016;4(6):123. doi: 10.21037/atm.2016.03.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samuelsson E, Victor A, Tibblin G. A population study of urinary incontinence and nocturia among women aged 20–59 years. Acta Obstet Gynecol Scand. 1997;76(1):74–80. doi: 10.3109/00016349709047789. [DOI] [PubMed] [Google Scholar]
- 38.Schreiber Pedersen L, Lose G, Høybye MT, Elsner S, Waldmann A, Rudnicki M. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017;96(8):939–948. doi: 10.1111/aogs.13149. [DOI] [PubMed] [Google Scholar]
- 39.Rodríguez-López ES, Calvo-Moreno SO, Basas-García Á, Gutierrez-Ortega F, Guodemar-Pérez J, Acevedo-Gómez MB. Prevalence of urinary incontinence among elite athletes of both sexes. J Sci Med Sport. 2021;24(4):338–344. doi: 10.1016/j.jsams.2020.09.017. [DOI] [PubMed] [Google Scholar]
- 40.Thomaz RP, Colla C, Darski C, Paiva LL. Influence of pelvic floor muscle fatigue on stress urinary incontinence: a systematic review. Int Urogynecol J. 2018;29(2):197–204. doi: 10.1007/s00192-017-3538-6. [DOI] [PubMed] [Google Scholar]
- 41.Carvalhais A, Natal Jorge R, Bø K. Performing high-level sport is strongly associated with urinary incontinence in elite athletes: a comparative study of 372 elite female athletes and 372 controls. Br J Sports Med. 2018;52(24):1586–1590. doi: 10.1136/bjsports-2017-097587. [DOI] [PubMed] [Google Scholar]
- 42.Falah-Hassani K, Reeves J, Shiri R, Hickling D, McLean L. The pathophysiology of stress urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2021;32(3):501–552. doi: 10.1007/s00192-020-04622-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hirsch AG, Minassian VA, Dilley A, Sartorius J, Stewart WF. Parity is not associated with urgency with or without urinary incontinence. Int Urogynecol J. 2010;21(9):1095–1102. doi: 10.1007/s00192-010-1164-7. [DOI] [PubMed] [Google Scholar]
- 44.Aune D, Mahamat-Saleh Y, Norat T, Riboli E. Body mass index, abdominal fatness, weight gain and the risk of urinary incontinence: a systematic review and dose–response meta-analysis of prospective studies. BJOG. 2019;126(12):1424–1433. doi: 10.1111/1471-0528.15897. [DOI] [PubMed] [Google Scholar]
- 45.Doumouchtsis SK, Loganathan J, Pergialiotis V. The role of obesity on urinary incontinence and anal incontinence in women: a review. BJOG. 2022;129(1):162–170. doi: 10.1111/1471-0528.16848. [DOI] [PubMed] [Google Scholar]
- 46.Goldstick O, Constantini N. Urinary incontinence in physically active women and female athletes. Br J Sports Med. 2014;48(4):296–298. doi: 10.1136/bjsports-2012-091880. [DOI] [PubMed] [Google Scholar]
- 47.Meader N, King K, Llewellyn A, Norman G, Brown J, Rodgers M, et al. A checklist designed to aid consistency and reproducibility of GRADE assessments: development and pilot validation. Syst Rev. 2014;3(1):1–9. doi: 10.1186/2046-4053-3-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.