SUMMARY
An anecdotal increase in C. perfringens outbreaks was observed in the North East of England during 2012–2014. We describe findings of investigations in order to further understanding of the epidemiology of these outbreaks and inform control measures. All culture-positive (>105 c.f.u./g) outbreaks reported to the North East Health Protection Team from 1 January 2012 to 31 December 2014 were included. Epidemiological (attack rate, symptom profile and positive associations with a suspected vehicle of infection), environmental (deficiencies in food preparation or hygiene practices and suspected vehicle of infection) and microbiological investigations are described. Forty-six outbreaks were included (83% reported from care homes). Enterotoxin (cpe) gene-bearer C. perfringens were detected by PCR in 20/46 (43%) and enterotoxin (by ELISA) and/or enterotoxigenic faecal/food isolates with indistinguishable molecular profiles in 12/46 (26%) outbreaks. Concerns about temperature control of foods were documented in 20/46 (43%) outbreaks. A suspected vehicle of infection was documented in 21/46 (46%) of outbreaks (meat-containing vehicle in 20/21). In 15/21 (71%) identification of the suspected vehicle was based on descriptive evidence alone, in 5/21 (24%) with supporting evidence from an epidemiological study and in 2/21 (10%) with supporting microbiological evidence. C. perfringens-associated illness is preventable and although identification of foodborne outbreaks is challenging, a risk mitigation approach should be taken, particularly in vulnerable populations such as care homes for the elderly.
Key words: Clostridium perfringens, epidemiology, food poisoning, outbreaks
INTRODUCTION
Clostridium perfringens is a Gram-positive spore forming anaerobic bacterium which is widely distributed in the natural environment and can be found in the intestinal tract of both animals and humans [1] as well as in food such as raw meats, dehydrated soups and sauces, raw vegetable and spices [2]. There are five types of C. perfringens (A, B, C, D, E) based on the toxins they produce [1]. Some strains of C. perfringens type A are also able to produce an enterotoxin (CPE) and to cause food poisoning and diarrhoeal illness. Spores of such strains are resistant to high temperatures and can therefore survive cooking procedures [3]. Growth of C. perfringens occurs at temperatures of 12–54 °C which may occur during cooling, reheating and hot holding of cooked foods [4]. Following germination of spores and in the appropriate environment, the cells multiply in large numbers without competition, as most bacteria would have been destroyed during the cooking process. Food poisoning occurs when high numbers of vegetative enterotoxigenic C. perfringens cells [usually >105 colony-forming units (c.f.u.)/g] are consumed. CPE, produced when the vegetative cells sporulate in the intestinal tract, is directly responsible for the gastrointestinal symptoms that occur. C. perfringens food poisoning is commonly associated with a mild and transient diarrhoeal illness, but may occasionally result in more serious complications such as necrotizing enteritis [5–7]. Fatalities are very rare and occur in 0·1% of cases [8]. C. perfringens type A can also cause CPE-mediated infectious [9] or antibiotic-associated diarrhoea [10] which is generally more profuse and of a longer duration than the classical food poisoning illness. This form of the disease occurs generally in the elderly population and hospital-acquired cases are often associated with antibiotic treatment [11].
It has been estimated that C. perfringens is the third most frequent cause of bacterial foodborne disease in England and Wales [12]. Outbreaks of food poisoning due to C. perfringens have been described in a number of settings [5, 13–17] and are commonly associated with high protein foods of animal origin [14]. In the UK the primary cause of C. perfringens outbreaks is reported to be poor temperature control and storage of meat dishes [18].
The diagnosis of C. perfringens mediated illness is, however, challenging. While there is little evidence that healthy humans are a reservoir for C. perfringens food poisoning [19, 20], non-enterotoxigenic C. perfringens can be part of the normal gut flora in humans and is therefore frequently isolated from faecal specimens of healthy human subjects [21–23]. Although lower numbers of organisms (typically <104–105 c.f.u./g) are generally found in normal human faeces compared to specimens from those with C. perfringens-associated illness [24], high counts of C. perfringens may also be observed in well individuals in certain groups such as elderly populations [22, 25]. In addition, spore count in sporadic cases of C. perfringens diarrhoea can be <105 c.f.u./g [9]. Therefore further microbiological testing in addition to quantitative measures such as culture is required.
In the North East of England, suspected outbreaks of C. perfringens are identified by local Health Protection or Environmental Health teams based on the presence of consistent clinical symptoms in cases that are epidemiologically linked in place or time, or by reported increases in laboratory-confirmed cases. Those outbreaks thought likely to be foodborne in origin are voluntarily reported to Public Health England's (PHE) Department of Gastrointestinal, Emerging and Zoonootic Infections via the Electronic Foodborne and Non-Foodborne Gastrointestinal Outbreak Surveillance System (eFOSS). Between 2012 and 2014, 31 outbreaks of infectious intestinal disease associated with C. perfringens were reported to eFOSS across England and Wales, 14 of which were reported by the North East PHE Centre (PHEC). Anecdotally, an increase in the number of C. perfringens outbreaks reported to the North East PHEC between 2012 and 2014 had also been observed when compared with previous years. We summarize epidemiological and microbiological findings following investigation of these outbreaks in order to develop further understanding of the epidemiology of C. perfringens outbreaks and inform local control measures.
METHODS
A suspected outbreak of C. perfringens is defined by the North East Health Protection Team as two or more cases of illness with an aetiology suggestive of a toxin-mediated infection (point source distribution of cases with a predominance of diarrhoea and short duration of illness) and identification of a plausible source of C. perfringens exposure (based on the judgement of the investigating Environmental or Health Protection team), or culture of C. perfringens from one or more faecal specimens. Faecal specimens are requested from affected cases and cultured for C. perfringens at the local laboratory. If >105 c.f.u. C. perfringens/g are detected, the cultures are sent for confirmation of identity, detection of the enterotoxin gene by PCR and molecular typing by fluorescent amplified fragment length polymorphism (fAFLP) at the National Reference Laboratory (NRL) of PHE. Faeces can also be sent to the NRL for detection of enterotoxin by ELISA. Where obtained, food specimens are cultured at PHE's Food Water and Environmental (FWE) Microbiology Laboratories and the isolates sent to the NRL. All outbreaks are recorded on PHE's case management system, HPZone. Information collected following a report of a potential outbreak includes the number, age, gender and symptom profile of affected individuals, the population at risk of exposure and the number of affected individuals who have been hospitalized or have died. Environmental Health teams are notified by the North East PHEC of all suspected outbreaks and where an inspection of food preparation practices is carried out, key findings and suspected vehicles of infection are documented.
All outbreaks entered into the case management system, HPZone, between 1 January 2012 and 31 December 2014 where the suspected infectious agent was specified as C. perfringens were identified. The following variables were extracted from the HPZone record and verified as necessary with paper records: date outbreak reported, population at risk, number of affected individuals, number of hospitalized cases and number of deaths. The number of cases confirmed by (i) culture (>105 c.f.u./g), (ii) identification of enterotoxigenic C. perfringens by PCR and (iii) detection of enterotoxin by ELISA were identified from paper copies of microbiology results along with any molecular profiling of isolated organisms. The same parameters were also documented for any food specimens obtained during the outbreak investigation.
Of the suspected outbreaks, only those with supporting microbiological evidence were included in any further analysis and were classified as follows:
Possible: C. perfringens isolated on culture (>105 c.f.u./g) from the faecal specimen of one or more individuals.
Probable: C. perfringens isolated on culture (>105 c.f.u./g) and cpe gene-bearer isolates detected by PCR in one or more individuals.
Confirmed: Enterotoxin detected by ELISA in the faeces of one or more individuals or C. perfringens with an indistinguishable molecular profile isolated from the faeces of one or more individuals and/or from food known to have been consumed by the affected group.
Descriptive analysis was undertaken describing the number of confirmed, probable and possible outbreaks, the number of outbreaks from which descriptive epidemiological evidence, analytical epidemiological evidence and/or microbiological evidence was available, and the key findings reported from epidemiological (including attack rate, symptom profile and evidence of any positive association with a suspected vehicle of infection), environmental (including deficiencies in food preparation or hygiene practices and suspected vehicle of infection) and microbiological investigations.
RESULTS
Descriptive epidemiology
Between 2012 and 2014, a total of 1072 outbreaks of gastrointestinal illness or food poisoning were reported to the North East PHEC (serving a population of approximately 2·6 million), of which 50 (5%) were suspected to be associated with C. perfringens [14/406 (3%) in 2012, 10/310 (3%) in 2013, 26/356 (7%) in 2014]. Four of the 50 suspected C. perfringens outbreaks were excluded from any further analysis since there was no microbiological evidence of C. perfringens. A summary of the characteristics of the 46 included outbreaks is outlined in Table 1.
Table 1.
Characteristics of outbreaks by year in which outbreak started*, North East England, 2012–2014
| Characteristic | 2012 | 2013 | 2014 | Total (2012–2014) |
|---|---|---|---|---|
| Total no. outbreaks | 12 (100%) | 9 (100%) | 25 (100%) | 46 (100%) |
| Setting† | ||||
| Care home | 12 (100%) | 8 (89%) | 18 (72%) | 38 (83%) |
| Food outlet | 0 | 0 | 4 (16%) | 4 (9%) |
| Private caterer | 0 | 1 (12%) | 3 (12%) | 4 (9%) |
| Symptoms | ||||
| Diarrhoea only | 6 (50%) | 4 (45%) | 16 (64%) | 26 (57%) |
| Diarrhoea and vomiting | 6 (50%) | 5 (56%) | 9 (36%) | 20 (43%) |
| Associated illness | ||||
| Total cases‡ | 176 (100%) | 102 (100%) | 384 (100%) | 662 (100%) |
| Median no. per outbreak (IQR) | 16 (10–19) | 11 (9–16) | 12 (9–15) | 13 (9–18) |
| Median attack rate (IQR)§ | 21 (15–24) | 12 (10–14)) | 15 (10–33) | 15 (11–23) |
| No. cases hospitalized | 7 (4%) | 0 | 1 (0·3%) | 8 (1%) |
| No. deaths | 3 (2%) | 0 | 1 (0·3%) | 4 (0·6%) |
IQR, Interquartile range.
Defined as the date of onset of illness in the first case at the time of reporting.
† Care home defined as a residential or nursing home for elderly or mentally infirm individuals. Food outlet defined as a premise at which food is regularly served, e.g. restaurant/pub/takeaway/mobile food van. Private caterer as an individual or business providing food on an ad hoc basis at an external event, e.g. wedding/festival.
‡ Defined on the basis of clinical symptoms.
§ Median attack rate only calculated for those outbreaks in which there was a clearly defined population at risk (n = 43).
Table 2 outlines the number of outbreaks classified as confirmed, probable or possible. In four outbreaks, one or more organisms other than C. perfringens were also isolated from affected individuals (outbreak 1: astrovirus n = 1, norovirus n = 3; outbreak 2: rotavirus n = 1; outbreak 3: Campylobacter n = 1; outbreak 4: norovirus n = 1) (Table 2).
Table 2.
Classification of outbreaks (2012–2014), by symptom profile, North East England, 2012–2014
| Symptom profile | All | ||
|---|---|---|---|
| Diarrhoea only | Diarrhoea and vomiting | ||
| Confirmed | 5 (19%) | 7 (35%) | 12 (26%) |
| Probable | 12 (46%) | 8 (40%) | 20 (43%) |
| Possible | 9 (35%) | 5 (25%) | 14 (30%) |
| No. of outbreaks where organisms other than C. perfringens isolated | 1 (4%) | 3 (15%) | 4 (9%) |
| Total no. of outbreaks | 26 (100%) | 20 (100%) | 46 (100%) |
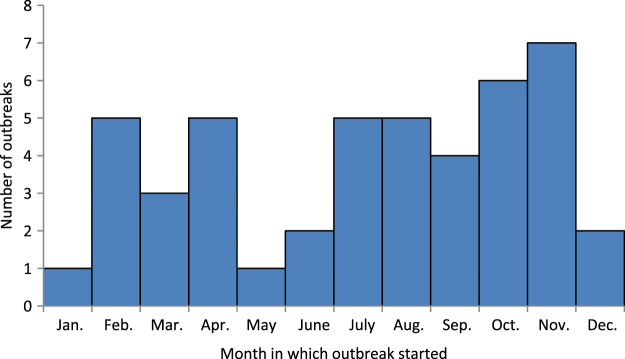
The distribution of reported outbreaks in time is shown in Figure 1.
Fig. 1.
Number of outbreaks (2012–2014, n = 46) by month of start date (defined as the date of onset of illness in the first case at the time of reporting).
Analytical epidemiology
An analytical study was carried out for eight of the 46 outbreaks and in five of these a statistically significant positive association was found with one or more food item thought to be a plausible vehicle of infection (Table 3).
Table 3.
Number of outbreaks by category of supporting evidence, North East England, 2012–2014
| 2012 | 2013 | 2014 | Total 2012–2014 | |
|---|---|---|---|---|
| No. of outbreaks | 12 (100%) | 9 (100%) | 25 (100%) | 46 (100%) |
| Analytical study | 4 (33%) | 1 (11%) | 3 (12%) | 8 (17%) |
| Positive, significant association with a specific food item | 2 (17%) | 0 | 3 (12%) | 5 (11%) |
| Food isolates | 0 | 0 | 4 (16%) | 4 (9%) |
| Matching molecular profile for food and faecal isolates | 0 | 0 | 2 (8%) | 2 (4%) |
| Environmental Health team visit | 12 (100%) | 9 (100%) | 21 (84%) | 42 (91%) |
| Specific concerns about temperature control | 7 (58%) | 4 (44%) | 9 (36%) | 20 (43%) |
Microbiology
The microbiological findings following testing of human faecal specimens are summarized by year in which outbreak started (defined as the date of onset of illness in the first case at the time of reporting) in Table 4.
Table 4.
Number of cases and microbiological findings by year in which outbreaks started*, North East England, 2012–2014
| 2012 | 2013 | 2014 | Total (2012–2014) | |
|---|---|---|---|---|
| No. of cases† | 176 (100%) | 102 (100%) | 384 (100%) | 662 (100%) |
| No. specimens cultured for C. perfringens | 62 (35%) | 22 (22%) | 109 (28%) | 193 (29%) |
| No. culture positive | 43 (24%) | 19 (19%) | 76 (20%) | 138 (21%) |
| No. of specimens culture cpe positive | 21 (11%) | 11 (11%) | 54 (14%) | 86 (13%) |
| No. of specimens tested for enterotoxin | 6 (3%) | 0 | 16 (4%) | 22 (3%) |
| No. of specimens enterotoxin positive | 6 (3%) | 0 | 4 (1%) | 10 (2%) |
Defined as the date of onset of illness in the first case at the time of reporting.
† Defined on the basis of clinical symptoms.
A total of 55 isolates from 15 different outbreaks (eight in 2014, two in 2013, five in 2012) were typed. In 12 of these outbreaks, C. perfringens isolates from two or more affected individuals with an indistinguishable fAFLP profile were detected. In two of the outbreaks reported in care homes, more than one fAFLP profile was detected among the isolates tested and no suspected vehicle of infection was identified. It is possible that these may represent non-food poisoning related illness.
C. perfringens was cultured from one or more food specimens in four different outbreaks and the isolate(s) were found to be enterotoxigenic in three of them. Food isolates from two of these outbreaks had an indistinguishable fAFLP profile from one or more associated faecal isolates (Table 3).
Environmental investigation
Environmental investigation is undertaken following discussion with the Health Protection Team. A visit from the Environmental Health team was documented in almost all outbreaks. In those where there was no documented visit, either single cases of C. perfringens had been identified or the food history obtained from the premise did not identify any potential issues with food hygiene or preparation. Specific concerns about temperature control (i.e. prolonged cooling or inadequate re-heating of foods) which would create ideal conditions for growth of C. perfringens were documented in just under half of the outbreaks described (Table 3). In addition, concerns about premises producing larger than normal volumes of food were documented in two outbreaks.
Identification of suspected vehicle of infection
A suspected vehicle of infection was documented in 21/46 (46%) outbreaks. In all but one of these the suspected source was meat (roast meat n = 12, curried stewed or minced meat n = 5, frozen sausages n = 1, ribs n = 1, chicken breast n = 1). Vegetable soup (made with a powdered chicken bouillon) was identified as the most likely source in the remaining outbreak.
The type of evidence available to inform assessment of the suspected vehicle is summarized in Table 3. In 15/21 (71%) outbreaks where a suspected source had been documented, this was based on descriptive evidence alone (e.g. described food handling practices such as inadequate re-heating or prolonged cooling of a potential vehicle of infection). In 5/21 (24%) outbreaks where there was a suspected source of infection, the descriptive evidence was supported by epidemiological evidence from an analytical study. In three of these outbreaks C. perfringens was cultured from the suspected food source and in two of these the C. perfringens isolates were of an fAFLP profile which matched one or more isolates from affected patients. C. perfringens was cultured from the suspected source of infection in one further outbreak in which no analytical study had been carried out, but the fAFLP profile of this isolate did not match that of any of the associated faecal isolates.
DISCUSSION
C. perfringens outbreaks were frequently reported to the North East PHEC between 2012 and 2014. The majority (83%) of outbreaks occurred in care homes. This may in part reflect a reporting bias, since care homes are specifically advised in the Health and Social Care Act (2008) to report all suspected outbreaks of gastrointestinal illness to Health Protection teams, whereas identification of outbreaks in other settings relies upon voluntary reporting. The typically mild nature of C. perfringens illness may mean that cases in other settings are unlikely to seek healthcare and thus be reported to Public Health teams. The frequency with which outbreaks are reported from care homes is nevertheless important, since these may easily be overlooked as food business operators.
A typical symptom profile of diarrhoea only was described in 57% (26/46) of the outbreaks reported, the remaining ‘atypical’ outbreaks having a mixture of both diarrhoea and vomiting. Outbreaks with an ‘atypical’ symptom profile did not appear any less likely to be classified as confirmed or probable outbreaks when compared with those with a more typical symptom profile (Table 2) and although other organisms were isolated from a higher proportion of these outbreaks, the overall number of outbreaks from which other organisms were isolated was small. Viral pathogens were isolated from one or more cases in two of the three outbreaks in which ‘atypical’ symptoms were observed. Infection with such viral pathogens may result in a greater propensity for vomiting and as such it is possible that these may represented mixed pathogen outbreaks or that there may have been detection of cases with co-incidental background illness resulting in misclassification of C. perfringens related illness. It is, however, difficult to disentangle this further on the basis of the evidence available, further emphasising the challenges in classifying outbreaks.
Relatively few hospitalised cases or fatalities were described. All of the described hospitalisations or fatalities occurred amongst symptomatic residents of care homes who were not necessarily confirmed cases of C. perfringens illness, and their diarrhoeal illness was thought unlikely to be the main factor contributing to their admission or death (although this was not verified further). This perhaps reflects the typically mild nature of symptoms associated with C. perfringens illness although there is no standard guidance as to what is recorded as a hospitalised case or fatality during an outbreak and as such this is likely to be an unreliable source of data There was no discernible pattern of temporal distribution, with outbreaks reported in every month of the year. Similar findings have been made in other reviews of C. perfringens outbreaks [26].
Although C. perfringens was isolated from one or more specimens in all of the outbreaks described, not all isolates had the potential to cause diarrhoea (as indicated by detection of the cpe gene) and not all of those that did were necessarily associated with illness. Just over a quarter of the reported outbreaks met the case definition for a confirmed outbreak. This may reflect challenges in obtaining sufficient microbiological evidence, such as a lack of leftover food or storage of leftover foods in conditions which result in the destruction of viable cells. The detection of CPE in the faeces of symptomatic individuals is useful in providing evidence of C. perfringens diarrhoea since the CPE is not a normal constituent of human faeces. CPE is usually detected using an ELISA [9], although may be rapidly eliminated from the host during the short symptomatic period [27]. The relative infrequency with which enterotoxin was detected in faeces in this outbreak series may reflect delays between onset of symptoms and specimen collection, or variation in testing practices such as an insufficient volume of specimen being available for further testing. It is much more difficult to ascertain whether reported cases in probable or possible outbreaks were likely to have occurred as a result of food poisoning. As previously described, C. perfringens may be frequently isolated from the faeces of healthy individuals particularly amongst elderly populations [20]. Distinction between enterotoxigenic and non-enterotoxigenic C. perfringens isolated from food or symptomatic individuals is essential to determine the aetiology of the diarrhoea and can be done by detecting the gene coding for CPE (cpe) by PCR assay [28, 29]. Although presence of the cpe gene is indicative of the potential to produce enterotoxin, it may also be present in faecal isolates from healthy individuals [30], and detection of enterotoxigenic strains may be hampered by the contiguous presence of non-toxigenic strains. Recent molecular studies suggest that cpe strains responsible for food poisoning may have distinct genetic characteristics [30], but such detail is unlikely to be available through routine microbiological testing. Other studies have also suggested that foodborne outbreaks of C. perfringens may be associated with cpe-negative strains which produce other toxins [31].
Consideration of supporting environmental and epidemiological evidence is therefore paramount in identifying likely foodborne outbreaks. Such evidence was, however, infrequently available in the outbreaks described in this study and this reflects the challenges in obtaining this type of evidence. It may for example be necessary to observe food preparation processes in real-time in order to identify relevant deficiencies in practice. This is often infeasible in practice since preparation has already occurred by the time an outbreak is reported. Environmental investigations are therefore reliant upon retrospective reporting of documented practices. The difficulties associated with using this type of information have been highlighted in other outbreak investigations [13]. Outbreaks may occur in settings which appear, based on the documentation available, to have good food handling practices in place, particularly where processes may have temporarily changed, e.g. they are catering for a larger number of customers than usual. Indeed this was identified as a specific concern in two of the outbreaks described here. Analytical epidemiological evidence may also be challenging to obtain, particularly where there is no clear hypothesis for a potential source of infection. Studies are often affected by difficulty in obtaining exposure histories and by recall bias which may be particularly challenging in elderly populations. They may also be hampered by lack of power due to small numbers of identified cases.
Despite the challenges in identifying and clearly defining foodborne outbreaks of C. perfringens, associated illness is preventable and as such a risk mitigation approach should be taken. This is particularly important in vulnerable populations such as residents of elderly care homes where there is potential for more severe illness. Given the ubiquitous presence of C. perfringens in the environment, elimination of contamination is likely to be difficult to achieve. Efforts should therefore focus on reducing the potential for proliferation should contamination be present. Consideration should be given to:
Examining awareness of the potential for C. perfringens outbreaks among Public Health and Environmental Health teams in order to facilitate recognition and direct timely investigation appropriately.
Examining awareness of C. perfringens food poisoning among food handlers and food business operators (particularly those which may be easily overlooked such as in care homes) in order to ensure appropriate processes (e.g. cooling/re-heating practices) are in place particularly when operating outside normal practices. Deficiencies in the level of understanding of food handlers about appropriate temperature control of foods have been identified in studies from other areas [32].
Developing protocols for collecting and testing of faecal and/or food specimens including the need for timely collection of specimens following onset of symptoms and appropriate storage.
Developing guidelines for interpreting complex microbiological findings which may be difficult to understand.
CONCLUSION
C. perfringens outbreaks are frequently reported in the North East of England. Microbiological, epidemiological and environmental information gathered during outbreak investigation is varied and often limited, most likely reflecting the challenges in obtaining and interpreting different sources of evidence. Although this may result in difficulties in confirming and clearly defining likely foodborne outbreaks, information gathered during outbreak investigation may be used to direct risk mitigation practices. Further consideration should be given to examining awareness of the potential for C. perfringens outbreaks amongst Public and Environmental Health professionals and food handlers in order to prevent future illness.
ACKNOWLEDGEMENTS
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Rood JI, Cole ST. Molecular genetics and pathogenesis of Clostridium perfringens. Microbiology and Molecular Biology Reviews 1991; 55: 621–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhodehamel EJ, Harmon SM. Bacteriological Analytical Manual. Chapter 16. Clostridium perfringens (http://www.fda.gov/Food/FoodScienceResearch/LaboratoryMethods/ucm070878.htm).
- 3.Hobbs BC, et al. Clostridium welchii food poisoning. Journal of Hygiene 1953; 51: 75–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, McClane BA. Further comparison of temperature effects on growth and survival of Clostridium perfringens type A isolates carrying a chromosomal or plasmid-borne enterotoxin gene. Applied and Environmental Microbiology 2006; 72: 4561–4568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bos J, et al. Fatal necrotizing colitis following a foodborne outbreak of enterotoxigenic Clostridium perfringens type A infection. Clinical Infectious Diseases 2005; 40: e78–e83. [DOI] [PubMed] [Google Scholar]
- 6.Schalch B, et al. Molecular typing of Clostridium perfringens form a food-borne disease outbreak in a nursing home: ribotyping versus pulsed-field gel electrophoresis. Journal of Clinical Microbiology 2003; 41: 892–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.BBC News. Christmas Day diner dies after food poisoning bug found (http://www.bbc.co.uk/news/uk-england-london-20908427). Accessed 3 March 2015.
- 8.Scallan E, et al. Foodborne illness acquired in the United States – unspecified agents. Emerging Infectious Diseases 2011; 17: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mpamugo O, Donocan T, Brett MM. Enterotoxigenic Clostridium perfringens as a cause of sporadic cases of diarrhoea. Journal of Medical Microbiology 1995; 43: 442–445. [DOI] [PubMed] [Google Scholar]
- 10.Borriello SP, et al. Enterotoxigenic Clostridium perfringens: a possible cause of antibiotic-associated diarrhoea. Lancet 1984; 323: 305–307. [DOI] [PubMed] [Google Scholar]
- 11.McLauchlin J, Grant KA. Clostridium botulinum and Clostridium perfringens. In: Simjee S, ed. Foodborne Diseases. Totowa, New Jersey: Humana Press, 2007, pp. 41–78. [Google Scholar]
- 12.Adak GK, Long SM, O'Brien SJ. Trends in indigenous foodborne disease and deaths, England and Wales: 1992 to 2000 Gut 2002; 51; 832–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simone B, et al. Investigation an outbreak of Clostridium perfringens gastroenteritis in a school; using smartphone technology, London, March 2013. Eurosurveillance 2014; 19: pii=20799. [DOI] [PubMed] [Google Scholar]
- 14.Eriksen J, et al. Clostridium perfringens in London, July 2009: two weddings and an outbreak. Eurosurveillance 2010; 15: pii=19598. [DOI] [PubMed] [Google Scholar]
- 15.Moffatt CRM, Howard PJ, Burns T. A mild outbreak of gastroenteritis in long-term, care facility residents due to Clostridium perfringens, Australia 2009. Foodborne Pathogens and Disease 2011; 8: 791–795. [DOI] [PubMed] [Google Scholar]
- 16.Wahl E, Romma S, Granum PE. A Clostridium perfringens outbreak traced to temperature-abused beef stew, Norway, 2012. Eurosurveillance 2013; 18: pii=20408. [PubMed] [Google Scholar]
- 17.Tallis G, Ng S, Ferreira C. A nursing home outbreak of Clostridium perfringens associated with pureed food. Australian and New Zealand Journal of Public Health 1999; 23: 421–423. [DOI] [PubMed] [Google Scholar]
- 18.Foodborne Disease Strategy. 2010. –15. Version 1.0. Published May 2011 (http://www.food.gov.uk/sites/default/files/multimedia/pdfs/fds2015.pdf). Accessed 4 February 2015.
- 19.Carman RJ, et al. Clostridium perfringens toxin genotypes in the feces of healthy North Americans. Anaerobe 2008; 14: 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang I, Wang J, Shih D. The level of faecal carriage and the toxic potential of Clostridium perfringens in the feces of a Taiwan subpopulation. Journal of Food and Drug Analysis 2006; 14: 89–92. [Google Scholar]
- 21.Nakamura H, et al. Usefulness of a combination of pulsed-field gel electrophoresis and enrichment culture in laboratory investigation of a foodborne outbreak due to Clostridium perfringens. Diagnostic Microbiology and Infectious Disease 2003; 47: 471–475. [DOI] [PubMed] [Google Scholar]
- 22.Stringer MF, Watson GN, Gilbert RJ. Faecal carriage of Clostridium perfringens. Journal of Hygiene 1985; 95: 277–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vela M, et al. DNA probe analysis for the carriage of enterotoxigenic Clostridium perfringens in faeces of a Mexican subpopulation. Diagnostic Microbiology and Infectious Disease 1999; 35: 101–104. [DOI] [PubMed] [Google Scholar]
- 24.PHE. Standards Unit, Microbiology Services, UK Standards for Microbiology Investigations. 2014 Bacteriology; B30(8.1), pp. 1–41 (https://www.gov.uk/government/uploads/system/uploads/attachmFent_data/file/343955/B_30i8.1.pdf). Accessed 30 March 2015.
- 25.Birkhead G, et al. Characterization of an outbreak of Clostridium perfringens food poisoning by quantitiative fecal culture and fecal enterotoxin measurement. Journal of Clinical Microbiology 1998; 26: 471–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grass JE, Gould LH, Mahon BE. Epidemiology of foodborne disease outbreaks caused by Clostridium perfringens, United States, 1998–2010. Foodborne Pathogens and Disease 2013; 10: 131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bartholomew BA, et al. Development and application of an enzyme linked immunosorbent assay for Clostridium perfringens type A enterotoxin. Journal of Clinical Pathology 1985; 38: 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fach P, Popoff MR. Detection of entreotoxigenic Clostridium perfringens in food and fecal samples with a duplex PCR and the slide latex agglutination test. Applied and Environmental Microbiology 1997; 63: 4232–4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grant KA, et al. The identification and characterization of Clostridium perfringens by real-time PCR, location of enterotoxin gene, and heat resistance. Foodborne Pathogens and Disease 2008; 5: 629–639. [DOI] [PubMed] [Google Scholar]
- 30.Miyamoto K, Li J, McLane BA. Enterotoxigenic Clostridium perfringens: detection and identification. Microbes and Environments 2012; 27: 343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Monma C, et al. Four foodborne disease outbreaks caused by a new type of enterotoxin-producing Clostridium perfringens. Journal of Clinical Microbiology 2015; 53: 859–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Panchal PK, Bonhote P, Dworkin MS. Food safety knowledge among restaurant food handlers in Neuchatel, Switzerland. Food Protection Trends 2013; 33: 133–144. [Google Scholar]