SUMMARY
The aim of this study was to determine the seroprevalence of Toxoplasma gondii infection in free-range chickens from Uberlândia, Minas Gerais state, Brazil, and characterize the genotypic and phenotypic features of two isolates of this parasite, considering the importance of these hosts in the epidemiology of toxoplasmosis. Serum samples from 108 free-range chickens were obtained from ten different districts, and submitted to the modified agglutination test (MAT) for the presence of anti-T. gondii antibodies, and brain and heart tissue samples from infected chickens were processed for mouse bioassay. An overall seroprevalence of 71·3% was found and antibody titres ranged from 16 to 4096. After confirmation of seropositivity by mouse bioassay, the determination of the T. gondii genotypes of two isolates was performed by PCR–RFLP, using primers for the following markers: SAG1, SAG2, SAG3, BTUB, GRA6, c22–8, c29–2, L358, PK1, new SAG2, Apico and CS3. These T. gondii isolates, designated TgChBrUD1and TgChBrUD2, were obtained from heart samples of free-range chickens. The TgChBrUD1 isolate belonged to ToxoDB PCR–RFLP genotype 11 and the TgChBrUD2 isolate belonged to ToxoDB PCR–RFLP genotype 6. Both isolates demonstrated high virulence in a rodent model, with the TgChBrUD1 isolate able to induce brain cysts, in accord with its pattern of multiplication rates in human fibroblast culture. Taken together, these results reveal high prevalence of T. gondii infection in free-range chickens throughout Uberlândia, indicating an important degree of oocyst environmental contamination and the existence of considerable risk for T. gondii transmission to humans by consumption of free-range chicken as a food source.
Key words: Food protection, free-range chicken, phenotyping, tissue cyst, Toxoplasma gondii
INTRODUCTION
Toxoplasma gondii is an obligatory intracellular parasite of the phylum Apicomplexa with a worldwide distribution. This parasite infects all warm-blooded animals and causes opportunistic disease in humans. T. gondii has a complex life-cycle with an asexual phase in intermediate hosts and a sexual phase, not obligatory, occurring exclusively in the epithelial cells of the cat intestine [1]. Brazil has a very high rate of T. gondii infection in humans. Up to 50% of elementary school children and 50–80% of women of child-bearing age have antibodies to T. gondii. Furthermore, the risks for uninfected women to acquire toxoplasmosis during pregnancy and fetal transmission are high because the environment is highly contaminated with oocysts [2]. Toxoplasmosis is asymptomatic in most infected people, as the infection remains latent for an indeterminate time, except when some circumstances lead to an immunity impairment, which may result in reactivation of the infection [3]. Even though this disease is normally asymptomatic, there are immunocompetent patients that can present non-specific symptoms like lymphadenopathy, fever, muscle pain, fatigue, and headache. Serious cases of toxoplasmosis may occur in immunosuppressed patients or in congenitally infected newborns [1]. Toxoplasmosis can be acquired by consuming raw or undercooked meat containing bradyzoites within tissue cysts from infected animals such as pig, chicken, sheep, cow, and others, or by ingesting oocysts shed into the environment which contaminate soil or water, vegetables and fruits, or by transplacentary transmission [1].
The most likely source of T. gondii is food consumption of raw or undercooked meat contaminated with tissue cysts. Brazil is among the largest producers and exporters of chicken meat in the world [4], and there is a new trend in the production of free-range organic meat that could increase the risk of T. gondii contamination [5]. In the USA and Europe, it is estimated that toxoplasmosis is one of the main causes of death by foodborne pathogens [6, 7]. However, the pathogenicity is determined by several factors, including host susceptibility, the inoculum, strain virulence and parasite stage at the time of infection [8].
Research on T. gondii population structure has been conducted worldwide. T. gondii was previously considered clonal with very low genetic variability with three genetic types (I, II, III) in North America and Europe. Although differences among these three genotypes at genome sequence level is lower than 1%, they have markedly different virulence phenotypes in mice, with type I strains uniformly lethal in outbred mice with LD100 = 1. In contrast, types II and III strains are significantly less virulent with LD50 ⩾103–105 and LD50 > 105, respectively [9]. Recently, a fourth clonal type has been characterized in North America [10]. There is evidence suggesting that T. gondii clonal lineages are present in Europe, with type II being most prevalent. In South America, T. gondii isolates from a variety of animals from different geographical areas were intensively studied and high genetic variability was revealed based on restriction fragment length polymorphism (RFLP) associated to polymerase chain reaction (PCR) [9, 11]. Different studies with animals (most samples isolated from chickens, cats, dogs, goats, sheep, capybaras) revealed highly diverse populations [12–15]. In Brazil, various studies with T. gondii isolates from many animals from different geographical areas have shown that multiple isolates express high genetic diversity [16]. The three most common genotypes were 6, 8 and 11 and these major genotypes were previously designated as type BrI, BrIII and BrII, respectively [16, 17]. Analysis of mortality rates in infected mice indicated that type BrI is highly virulent, type BrIII is non-virulent, while type BrII and BrIV lineages are intermediately virulent [17].
Considering that there has been no previous study in free-range chickens in Uberlândia city, state of Minas Gerais, Brazil, as an indicator of soil contamination with T. gondii oocysts and the potential risk of infection by this parasite to humans by ingestion of this traditional food source, the main purpose of the present study was to isolate and characterize T. gondii occurring in this host by multilocus PCR–RFLP to better understand the epidemiology of toxoplasmosis in this city.
MATERIALS AND METHODS
Free-range chicken sample collection
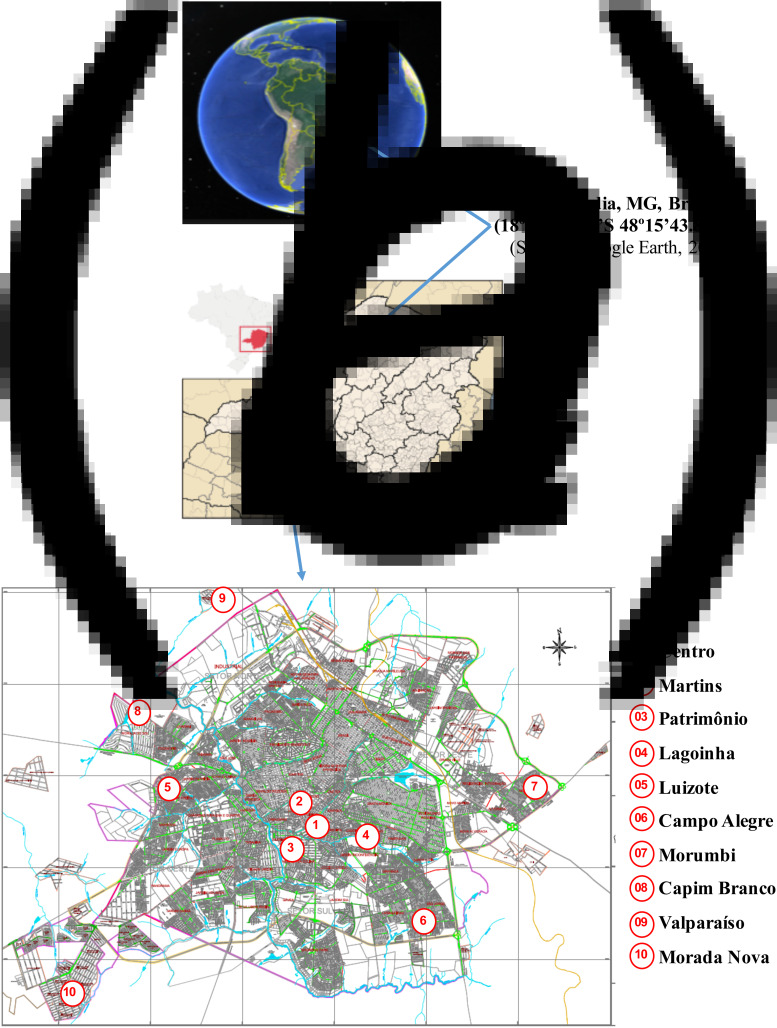
This cross-sectional study was carried out in Uberlândia (18° 54′ 40·70″ S, 48° 15′ 43·89″ W), located in the Triângulo Mineiro, Southwestern region of the state of Minas Gerais, Brazil (Fig. 1a,b), which has a population of approximately 604 103 inhabitants and 4 675 753 head of poultry according to the IBGE census of 2010 [18]. In the absence of any previous studies on chicken toxoplasmosis in Minas Gerais, a 50% expected prevalence (p) and a 90% confidence interval (Z = 1·645) with a 10% desired absolute precision (d) was considered necessary to arrive at the required sample size, using the formula: n = p(1 − p)Z2/d2 [19]. The sample size calculated was n = 68 and was increased for better accuracy. Serum samples from 108 free-range chickens (Gallus domesticus) were obtained in ten different districts of this city, eight of which were located in the urban area (Centro, Martins, Patrimônio, Lagoinha, Luizote, Campo Alegre, Morumbi, Capim Branco) and two in the suburban area (Valparaíso, Morada Nova) (Fig. 1c). Blood samples were collected from the wing vein and sera were stored at −20 °C until required for serological assay.
Fig. 1.
Location of the city where free-range chickens were sampled in the present study. Uberlândia is shown in the continent (a), followed by its position on the map of Brazil and in the state of Minas Gerais (b). The districts where the animals were sampled are also represented (c). (Source: Uberlândia City Council, 2015.)
Modified agglutination test (MAT)
Sera from chickens were tested for anti-T. gondii antibodies using the MAT, as described previously [13]. Antigen preparation consisted of tachyzoites collected from peritoneal exudate of Swiss mice previously infected with T. gondii RH strain. Parasite suspensions were washed four times (centrifugation at 720 g for 10 min at 4 °C) with phosphate-buffered saline (PBS; pH 7·2) and then fixed with 6% formalin under agitation for 12 min at 4 °C. After a new washing cycle, the parasites were quantified (1·2 × 108 tachyzoites/ml) and stored in carbonate buffer (pH 8–9) added from 2·8 mm β-mercaptoetanol and 0·004% Evans Blue. After the homogenization, the antigen was added (25 µl/well) to 96-well U-shaped microplates, followed by the addition (v/v) of the serum samples diluted twofold from 1:16 to 1:16·384 in PBS. The plates were incubated at 37 °C in a humid chamber for 12 h. As controls, human and mouse positive and negative serum samples were included in each reaction. The results were analysed considering as positive samples the presence of agglutination of the parasites and the formation of a button with defined contour for the negative samples.
Peptic digest of chicken tissues
Samples of brain and heart from seropositive chickens were collected and processed in accordance with a protocol described previously [20]. Samples were cut in small pieces, after adding 0·15 m NaCl to process the tissue homogenization. The same volume of 0·5% acid pepsin (pH 1·1–1·2) was added to the pre-warmed (37 °C) homogenate and incubated at 37 °C for 1 h under gentle shaking. The resulting preparation was filtered through two layers of gauze and centrifuged at 800 g for 10 min. The supernatant was discarded and the sediment was homogenized in PBS containing 25 µg/ml gentamycin, and further used in mouse bioassay.
Mouse bioassay
Processed brain and heart samples were inoculated (1 ml volume) in six mice (three for each sample) by the subcutaneous route. The animals were observed daily for mortality and serum samples were collected at 15, 30 and 60 days after inoculation to evaluate seroconversion by immunoenzymatic assays (ELISAs). Serum samples were also collected prior to the inoculation and served as negative control sera.
Mouse seroconversion assay
ELISAs were performed to evaluate the seroconversion of the mice used in bioassay experiments, as described previously [15], with modifications. Microtitre plates of polystyrene were coated with soluble antigen of T. gondii (10 µg/ml) in 0·06 m carbonate buffer (pH 9·6) overnight at 4 °C. The plates were washed three times with 0·05% PBS plus Tween 20 (PBS-T) and serum samples were added in duplicate, diluted 1:16 in PBS-T containing 5% non-fat milk (PBS-TM). After incubation for 1 h at 37 °C, the plates were washed six times with PBS-T and incubated with the anti-mouse IgG/peroxidase conjugate (Sigma Chemical Co., USA) diluted 1:2000 in PBS-TM for 1 h at 37 °C. After a new cycle of washing, the assay was developed by adding the enzyme substrate consisting of 0·03% H2O2 in chromogenic buffer (o-phenylenediamine – 1·0 mg/ml in 0·1 m citrate-phosphate buffer; pH 5·0). After incubation for 10 min at room temperature, the reaction was stopped by adding 2 n H2SO4. The optical density (OD) was read in a plate reader at 492 nm (Titertek Multiskan Plus, Flow Laboratories, Switzerland). Three positive and three negative control sera were included in each plate. The cut-off for a positive test was determined as the mean OD of negative control sera plus 3 standard deviations. Antibody titers were arbitrarily expressed as ELISA indexes (EI), according to the formula EI (%) = OD sample/cut-off × 100, as described previously [21]. EI values >1·1 were considered as positive.
Isolation of T. gondii
Brain from seropositive mice was collected and homogenized for the detection of tissue cysts and the peritoneal exudates were analysed for the presence of free tachyzoites by light microscopy. Brain samples containing cysts were inoculated by the intraperitoneal route (30 and 50 cysts) in six Swiss mice (three animals per dose). Tachyzoites of TgChBrUD1 and TgChBrUD2 strains were obtained initially from peritoneal exudates of previously infected Swiss mice and then maintained by serial passage in human foreskin fibroblast (HFF, ATCC no. CRL-1635, USA), in RPMI 1640 medium (Sigma Chemical Co.) in order to obtain the necessary numbers of parasites for genetic characterization. After total cell lysis, tachyzoites were collected, washed in PBS, filtered on 3 µm polycarbonate membrane (Millipore, France) and stored at −70 °C until genotyping. HFF cells infected with T. gondii isolates were also stored in liquid nitrogen.
Extraction of T. gondii genomic DNA
The extraction of DNA was performed following a protocol described previously [2]. Frozen tachyzoites were homogenized in PBS with 50 µl of extraction buffer (10 mm Tris–HCl, 100 mm NaCl, 25 mm EDTA, 1% SDS, 0·4 mg/ml proteinase K) and incubated overnight at 37 °C under gentle stirring. Next, phenol buffer was added to the sample (v/v) and centrifuged at 12 000 g for 5 min. The supernatant containing the aqueous phase was retrieved. To precipitate the extracted DNA, propanol (v/v) was added, homogenized, and incubated overnight at −20 °C. The samples were centrifuged at 12 000 g for 25 min at 4 °C, and the sediments were saved and added from 70% ethanol, repeating this step twice. The processed DNA samples were allowed to dry completely at room temperature, homogenized with 0·01 m Tris-EDTA (1/10), incubated at 56 °C for 10 min and stored at −20 °C until the amplification process.
Phenotyping of T. gondii isolates
Mice (Swiss, BALB/c and C57BL/6), gerbil (Meriones unguiculatus) and Cricetidea (Calomys callosus) were intraperitoneally inoculated with 102 tachyzoites from each T. gondii isolate with the purpose of determining the morbidity and the mortality indices in these animals in order to establish a comparison between the parasite virulence and burden in these animals.
Genotyping of T. gondii isolates
The determination of T. gondii genotypes in the obtained isolates was performed as described previously [22] by PCR, using primers for the three-way markers (SAG1, SAG2, new SAG2, SAG3, BTUB, GRA6, c22–8, c29–2, L358, PK1, Apico and CS3, for posterior analysis of polymorphism of the fragments of restriction (RFLP), as described elsewhere [17]. After the amplification of the fragments, the samples were submitted to enzymatic activity with endonucleases specific for each fraction. The endonuclease-treated amplified product was analysed in agarose gel at 2·5% and 3%.
Statistical analysis
The Kaplan–Meier method was used to estimate the percentage of mice surviving at each time point and survival curves were compared using the log-rank test. Results were considered significant at P < 0·05. The statistical analysis and the graphs were performed using GraphPad Prism v. 5.0 (GraphPad Software, USA). The profiles found after digestion with restriction endonucleases were compared with the profiles of the reference strains in a virtual database, the ToxoDB database (www.toxodb.org). The calculation of power sample size was performed using SigmaStat v. 3.5 software (http://sigmastat.software.informer.com/3.5/), and the study achieved 90% power at the 5% level.
Ethical approval
This study was approved by the Ethics Committee for Animal Experimentation from the Federal University of Uberlândia (CEUA-UFU), under Protocol CEUA/UFU No. 054/11, 20 December 2011. The care of experimental animals complied with the National Institutes of Health guidelines for the human use of laboratory animals. Rodents were maintained in individual cages at animal facilities from this institution, and received food and water ad libitum.
RESULTS
Detection of seropositive free-range chickens
Antibodies against T. gondii were found in 77 (71·3%) of 108 serum samples, with antibody titre ⩾16 as determined by MAT. The antibody titres varied from 16 to 4096, but the titre most frequently found was 32 (Table 1). Six seropositive chickens were selected for the isolation and genetic characterization of T. gondii based on the presence of antibody titres varying from 64 to 512.
Table 1.
Antibody titres for Toxoplasma gondii determined by the modified agglutination test (MAT) in serum samples from free-range chickens in different districts of Uberlândia, Minas Gerais, Brazil
| No. of reactive samples/no. of tested samples | Anti-T. gondii antibody titre | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| District | 16 | 32 | 64 | 128 | 256 | 512 | 1024 | 2048 | 4096 | |
| Martins | 1/4 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Campo Alegre | 8/10 | 7 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Capim Branco | 5/6 | 3 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Centro | 7/9 | 2 | 2 | 2 | 0 | 1 | 0 | 0 | 0 | 0 |
| Lagoinha | 11/11 | 1 | 5 | 2 | 0 | 2 | 1 | 0 | 0 | 0 |
| Luizote | 5/7 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 0 |
| Morada Nova | 24/31 | 3 | 7 | 5 | 2 | 6 | 1 | 0 | 0 | 0 |
| Morumbi | 2/10 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patrimônio | 4/10 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Valparaíso | 10/10 | 0 | 2 | 1 | 0 | 3 | 1 | 2 | 0 | 1 |
| Total (%) |
77/108 (71·3) |
19 (24·7) |
21 (27·3) |
12 (15·6) |
5 (6·5) |
13 (16·9) |
3 (3·9) |
3 (3·9) |
0 (0) |
1 (1·3) |
Isolation of T. gondii from free-range chickens
Two T. gondii isolates were obtained from six seropositive chicken samples bioassayed in mice. T. gondii infection was evidenced through clinical signs (respiratory fatigue, ruffled coat, inappetence, apathy) of the mice used in bioassay and confirmed by seroconversion of the animals inoculated with heart and brain samples of naturally infected free-range chickens selected for this purpose (Table 2). After 30 days inoculation, the serological analyses by ELISA indicated the seroconversion of four mice that had been inoculated with brain (100% mortality) and heart (33% mortality) samples (chicken no. 808). Another heart sample (chicken no. 880) also induced seroconversion (mortality) in 100% of the mice inoculated. The two new isolates were designated TgChBrUD1 and TgChBrUD2 (where Tg = T. gondii, Ch = chicken, Br = Brazil, UD = Uberlândia and the isolates were numbered according to the chronological order in which isolation was performed).
Table 2.
Toxoplasma gondii isolates in free-range chickens (Gallus domesticus) from Uberlândia, Minas Gerais, Brazil
| Chicken identification number | District | Antibody titre in MAT | Mice inoculated with brain from free-range chickens | Mice inoculated with heart from free-range chickens | Mortality range from day post-infection | Isolate designation | ||
|---|---|---|---|---|---|---|---|---|
| Mice, n | Mortality (%) | Mice, n | Mortality (%) | |||||
| 853 | Morumbi | 64 | 3 | 0 | 3 | 0 | 0 | — |
| 808 | Patrimônio | 128 | 3 | 3 (100) | 3 | 1 (33·3) | 45–60 days | TgChBrUD1 |
| 833 | Luizote | 128 | 3 | 0 | 3 | 0 | 0 | — |
| 883 | Luizote | 256 | 3 | 0 | 3 | 0 | 0 | — |
| 880 | Morada Nova | 512 | 3 | 0 | 3 | 3 (100) | 30–60 days | TgChBrUD2 |
| 836 | Morada Nova | 64 | 3 | 0 | 3 | 0 | 0 | — |
The presence of cysts was also detected in the brain of these seropositive animals; however, free tachyzoites were not found in these mouse peritoneal exudates. Afterwards, the cerebral cysts were inoculated in Swiss mice for in vivo maintenance of the isolates. By observing the mortality and morbidity of the mice, the constant presence of tachyzoites in the peritoneal exudate of these animals was noticed. The tachyzoite forms of TgChBrUD1 and TgChBrUD2 were used to perform successive passages every 2 or 3 days via the intraperitoneal route to maintain the isolates in an in vivo model.
Phenotyping of T. gondii isolates
Both T. gondii isolates showed different characteristics in HFF cultures, as the time of disruption and infection of neighbouring cells. The TgChBrUD1 isolate presented slow multiplication rate compared to the TgChBrUD2 isolate. It was observed that 4 days were necessary to lyse the majority of HFF cells infected with the TgChBrUD1isolate, while this only took 2 days in cells infected with the TgChBrUD2 isolate (data not shown). Additional biological features were also observed between both isolates. The TgChBrUD1 isolate induced brain cysts in Swiss mice after 20 days inoculation and a small amount of free tachyzoites in the peritoneal exudate was found after the first passage in Swiss mice. However, the majority of animals used during the bioassay died after 6 and 7 days inoculation, even though they presented occasionally a small number of free tachyzoites in the peritoneal exudate. In contrast, the TgChBrUD2 isolate induced a high number of free tachyzoites in the peritoneal exudate of Swiss mice after 3, 4 or 5 days inoculation (data not shown).
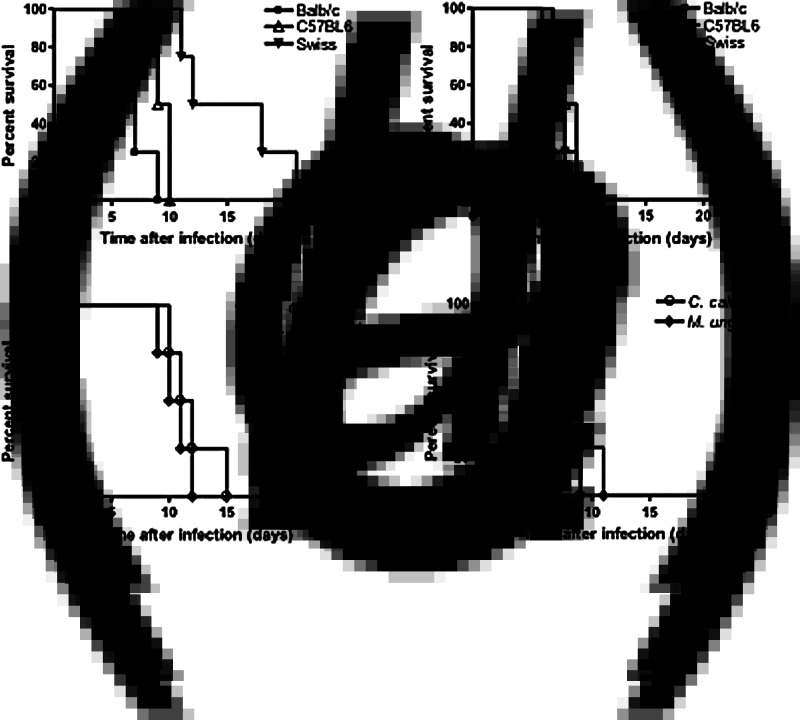
When analysing the experimental infections in mice from different genetic backgrounds, as allogenic (Swiss) or isogenic (BALB/c or C57BL/6), survival curves of BALB/c and C57BL/6 mice were very short, particularly if the isolate came from TgChBrUD1 (Fig. 2a) or from TgChBrUD2 (Fig. 2b), with 100% mortality around 10 days after infection. In Swiss mice, however, the time to death was more prolonged, with 100% mortality after 20 days infection with the TgChBrUD1 isolate (Fig. 2a), compared to the TgChBrUD2 isolate, which induced 100% mortality after 9 days infection (Fig. 2b). Likewise, the time to death was short in other rodents, such as gerbils (Meriones unguiculatus) that presented 100% mortality at around 12 days infection with either of the isolates (Fig. 2c,d), whereas Cricetidae (Calomys callosus) showed a slightly higher time to death (100% mortality at 15 days infection) with the TgChBrUD1 isolate (Fig. 2c), than the TgChBrUD2 isolate (100% mortality at 9 days infection) (Fig. 2d).
Fig. 2.
Survival rates among mice (BALB/c, C57BL6 and Swiss) and other rodents (Meriones unguiculatus and Calomys callosus), inoculated with 102 tachyzoites of TgChBrUD1 (a, c) or TgChBrUD2 (b, d) isolates from free-range chickens in Uberlândia, Minas Gerais, Brazil.
Genotyping of T. gondii isolates
After 12 successive passages in mice, tachyzoites from both isolates were cultured in vitro using HFF cells and characterized through 12 genotypically different primers. The typing analysis of the samples for the enzymatic activity with endonucleases was evaluated through the bands found in the agarose gel. The isolates differed between each other for the markers New SAG2, BTUB, GRA6, c22–8, c29–2, PK1 and Apico. The TgChBrUD1 isolate exhibited ToxoDB PCR–RFLP genotype 11, also known as type BrII. The TgChBrUD2 isolate exhibited ToxoDB PCR–RFLP genotype 6, also known as type BrI Africa 1 (Table 3).
Table 3.
Multilocus genotyping of Toxoplasma gondii isolates in free-range chickens (Gallus domesticus) from Uberlândia, MG, Brazil
| PCR–RFLP markers | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Isolate identification | SAG1 | SAG2 | SAG2 (5΄ + 3΄) | SAG2 New | SAG3 | BTUB | GRA6 | c22–8 | c29–2 | L358 | PK1 | Apico | CS3 | Genotype† | Reference |
| TgChBrUD1 | I | I | I | II | III | III | III | I | III | I | II | III | I | 11 (BrII) | Pena et al. [17] |
| TgChBrUD2 | I | I | I | I | III | I | II | u-1* | I | I | I | I | I | 6 (BrI AfricaI) | Pena et al. [17] |
u-1, New allele that is different from clonal type I, II and III alleles.
ToxoDB PCR–RFLP genotype number.
DISCUSSION
Studies involving the analysis strain diversity of T. gondii have constituted an important issue in recent decades. Highly abundant clonal genotypes were found in North America and Europe, while recent studies using multilocus markers showed high genetic diversity in South America, where strains show greater evidence of recombination [11]. Chickens are indicators of T. gondii strain prevalence in a domestic or peridomestic environment and several studies have examined the distribution of T. gondii genotypes in chickens in many countries, including Brazil [14, 23]. The yearly poultry meat consumption per capita in Brazil is estimated to be 31·66 kg and the importance of these studies is because the toxoplasmosis pathogenicity is also determined by T. gondii strain virulence, with repercussions for the quality of life in the population, among other foodborne pathogens, as has been demonstrated in the USA [24–26].
In the present study, the detection of antibodies against T. gondii in free-range chickens was conducted by MAT, which was standardized in microtitre plates. The assay parameters were established to avoid the prozone effect due to excess of antibodies that could cause false-negative results. Results described in previous studies using free-range chickens as model of natural T. gondii infection had proven the validity of MAT for this type of study [27]. The high seropositivity (71%) found in free-range chickens in our study indicates a high soil contamination with T. gondii oocysts in Uberlândia. From six naturally infected chickens, two T. gondii isolates were obtained from heart or brain by mouse bioassay. The success of the isolation of both new T. gondii isolates was dependent on the number of mice inoculated, the amount of infected tissues used in the bioassay, and the concentration of parasites in the samples [27]. Further, the ELISA serological test was used to detect mouse seroconversion, since it has higher sensitivity and the reading of the results is objective in comparison with MAT [27]. The genotyping of the isolated parasites was performed by the multilocus PCR–RFLP method [28], which allows the identification of T. gondii isolates with high resolution. Recent studies of nine T. gondii isolates from human patients in French Guiana and 53 isolates from chickens in Brazil suggested the occurrence of high rates of transmission and out-crossing [29]. When applied to strains from South America, markers designed to detect DNA polymorphisms in isolates from North America and Europe reveal patterns resembling mixtures of types I and III alleles with a lower frequency of type II allele [30]. These genotypes I and II were considered exotic in the past, but some of them turned out to be common lineages in South America, and appear unusual only by comparison to the previously studied clonal lineages from North America and Europe [29].
In Brazil, a study of T. gondii isolates from a variety of animals from different geographical areas showed that multiple isolates identified from different hosts and locations are considered the common clonal lineages in Brazil. The three most common genotypes were 6, 8 and 11 and these major genotypes were previously designated as types BrI, BrIII and BrII, respectively [17]. These results indicate that the T. gondii population in Brazil is highly diverse with a few successful clonal lineages expanded into wide geographical areas [17]. Analysis of mortality rates in infected mice indicated that type BrI is highly virulent, type BrIII is non-virulent, while type BrII and BrIV lineages are intermediately virulent. In the present study, two T. gondii isolates from free-range chickens were genotyped. The comparison between both isolates demonstrated distinct biological features, as the TgCHBrUD2 isolate was revealed to be more virulent than the TgCHBrUD1 isolate. The TgCHBrUD2 (genotype 6 type BrI Africa 1) isolate presented nine type I alleles out of 12 genetic markers and killed all infected animals in a short period of time (100% mortality at 9 days after infection) with the absence of brain tissue cysts in mice of different genetic backgrounds characterizing a virulent strain [17]. In contrast, the TgCHBrUD1 (genotype 11 type BrII) isolate showed five markers with the type I allele, two of type II alleles and five markers of type III alleles. The time to death was more prolonged, since it induced mouse brain cysts with the time to death (100% mortality) being around 10 days after infection in BALB/c mice and up to 20 days after infection in Swiss mice, characterizing an intermediate virulent strain [17]. These genotypes were previously identified from domestic animals and have a geographical distribution clearly widespread in Minas Gerais, Brazil. Genotype 11 type BrII is associated with congenital toxoplasmosis in this state [17, 31].
It has been suggested that distinct combinations of alleles in several loci may be responsible for the heterogeneity observed in the virulence phenotype of T. gondii strains [32]. Early studies recognized that T. gondii strains display vastly different levels of virulence in mice, as defined by survival after acute infection [33], and subsequent molecular analyses revealed that they could be genetically similar or not [17, 34]. Thus, virulence seems not to be the result of specific alleles at a few dominant loci but rather the result of allelic combinations from many loci [17]. In a previous genetic mapping and linkage analysis study, marker CS3 on chromosome VIIa of T. gondii has been shown to be strongly linked to acute virulence in mice [35]. Most of the isolates obtained and genotyped from cats in São Paulo state, Brazil for the CS3 locus, indicate that isolates with alleles I and II at the CS3 locus are strongly associated with mortality in infected mice, while isolates with allele III at CS3 is strongly associated with survival of infected mice [17]. In the present study, we observed allele I at the CS3 locus for both isolates and it can be responsible for acute virulence in the animals evaluated.
In the present study it was possible to observe that BALB/c mice were significantly more susceptible than Swiss mice when inoculated with the TgCHBrUD1 isolate. Likewise, both isogenic mouse lineages (BALB/c and C57BL/6) presented a higher susceptibility compared to Swiss allogenic mice, Meriones unguiculatus and Calomys callosus, when inoculated with the TgCHBrUD1 isolate. In the murine model of toxoplasmosis, C57BL/6 mice are considered to be more susceptible to T. gondii infection than BALB/c mice, when they are inoculated with type I (C56) or type II (ME-49) strains [36]. In contrast, genetically resistant lineages [e.g. BALB/c (H-2d)] can control T gondii infection, developing latent chronic infection, as do immunocompetent humans [37].
On the other hand, the mortality rates in mice inoculated with the TgCHBrUD2 isolate did not show significant differences between all animal groups, indicating that this isolate is highly virulent and leads to the animal's death independent of the host species. Based on the results obtained, it can be concluded that the diversity of T. gondii strains are also present in Uberlândia. Moreover, as this approach has not been investigated previously, our results can lead to a better understanding between genotype and phenotype of these new isolates, perhaps making it possible to establish a stronger link between the genetic structure and virulence of this parasite at the feto-maternal interface. Further studies on the genetic variability and biological features of new isolates to be conducted in additional cities from this region of Triângulo Mineiro, Minas Gerais, Brazil, will be necessary to supply more detailed information on the gene evolution, the level of genetic exchange and the structure of T. gondii population worldwide.
It has been described that the increased practice of modern confinement production could decrease T. gondii's contamination of meat, but a new tendency in the production of free-range-reared animals for meat could increase the risk of contamination [38]. This is also true in Brazil, particularly in street markets where free-range chickens are available to purchase throughout the country.
The production of free-range organic meat is a new trend, and this practice increases the chances of meat containing tissue cysts from T. gondii. In summary, the present study identified two T. gondii isolates in free-range chickens showing variable degrees of virulence, as demonstrated by phenotypic and genotypic characterization, which highlights the importance of controlling food quality as chicken meat consumption can be an important foodborne pathogen for humans.
ACKNOWLEDGEMENTS
We are indebted to Dr Chunlei Su from The Department of Microbiology, The University of Tennessee, Knoxville, TN, USA, who provided us with his expertise to genotype the parasite isolates. We thank Antonio Tomaz Junior for his technical assistance. This work was financially supported by Brazilian research agencies (Conselho Nacional de Desenvolvimento Científico e Tecnológico-CNPq, Fundação de Amparo à Pesquisa do Estado de Minas Gerais-FAPEMIG, and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-CAPES).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Cenci-Goga BT, et al. Toxoplasma in animals, food, and humans: an old parasite of new concern. Foodborne Pathogens Disease 2011; 8: 751–762. [DOI] [PubMed] [Google Scholar]
- 2.Dubey JP, et al. Toxoplasmosis in humans and animals in Brazil: high prevalence, high burden of disease, and epidemiology. Parasitology 2012; 139: 1375–1424. [DOI] [PubMed] [Google Scholar]
- 3.Dubey J, Jones J. Toxoplasma gondii infection in humans and animals in the United States. International Journal for Parasitology 2008; 38: 1257–1278. [DOI] [PubMed] [Google Scholar]
- 4.Nääs IA, et al. Brazilian chicken meat production chain: a 10-year overview. Brazilian Journal of Poultry Science 2015; 17: 87–94. [Google Scholar]
- 5.Jones JL, Dubey JP. Foodborne toxoplasmosis. Clinical Infectious Diseases 2012; 55: 845–851. [DOI] [PubMed] [Google Scholar]
- 6.Mead PS, et al. Food-related illness and death in the United States. Emerging Infectious Diseases 1999; 5: 607–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meerburg BG, Kijlstra A. Changing climate-changing pathogens: Toxoplasma gondii in North-Western Europe. Parasitology Research 2009; 105: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubremetz JF, Lebrun M. Virulence factors of Toxoplasma gondii. Microbes and Infection 2012; 14: 1403–1410. [DOI] [PubMed] [Google Scholar]
- 9.Howe DK, Sibley LD. Toxoplasma gondii comprises three clonal lineages: correlation of parasite genotype with human disease. Journal of Infectious Diseases 1995; 172: 1561–1566. [DOI] [PubMed] [Google Scholar]
- 10.Khan A, et al. Genetic analyses of atypical Toxoplasma gondii strains reveal a fourth clonal lineage in North America. International Journal for Parasitology 2011; 41: 645–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sibley LD, Ajioka JW. Population structure of Toxoplasma gondii: clonal expansion driven by infrequent recombination and selective sweeps. Annual Review of Microbiology 2008; 62: 329–351. [DOI] [PubMed] [Google Scholar]
- 12.Cavalcante CR, et al. Virulence and molecular characterization of Toxoplasma gondii isolated from goats in Ceará, Brazil. Small Ruminant Research 2007; 69: 79–82. [Google Scholar]
- 13.Da Silva RC, et al. Genotypic characterization of Toxoplasma gondii in sheep from Brazilian slaughterhouses: new atypical genotypes and the clonal type II strain identified. Veterinary Parasitology 2011; 175: 173–177. [DOI] [PubMed] [Google Scholar]
- 14.Dubey JP, et al. New Toxoplasma gondii genotypes isolated from free-range chickens from the Fernando de Noronha, Brazil: unexpected findings. Journal of Parasitology 2010; 96: 709–712. [DOI] [PubMed] [Google Scholar]
- 15.Mineo JR, Camargo ME, Ferreira AW. Enzyme-linked immunosorbent assay for antibodies to Toxoplasma gondii polysaccharides in human toxoplasmosis. Infection and Immunity 1980; 27: 283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubey JP, et al. Toxoplasmosis in humans and animals in Brazil: high prevalence, high burden of disease, and epidemiology. Parasitology 2012; 139: 1375–1424. [DOI] [PubMed] [Google Scholar]
- 17.Pena HFJ, et al. Population structure and mouse-virulence of Toxoplasma gondii in Brazil. International Journal for Parasitology 2008; 38: 561–569. [DOI] [PubMed] [Google Scholar]
- 18.IBGE-Brazilian Institute of Geography and Statistics. Censo demográfico 2010. 2015. (http://www.cidades.ibge.gov.br/xtras/perfil.php?lang=&codmun=317020&search=minas-gerais|uberlandia|infograficos:-informacoes-completas). Accessed 1 September 2015.
- 19.Thrusfield M. Veterinary Epidemiology, 3rd edn. London: Blackwell Science, 2007. [Google Scholar]
- 20.Dubey JP. Refinement of pepsin digestion method for isolation of Toxoplasma gondii from infected tissues. Veterinary Parasitology 1998; 74: 75–77. [DOI] [PubMed] [Google Scholar]
- 21.Silva DO, et al. Heterologous antibodies to evaluate the kinetics of the humoral immune response in dogs experimentally infected with Toxoplasma gondii RH strain. Veterinary Parasitology 2002; 107: 181–195. [DOI] [PubMed] [Google Scholar]
- 22.Derouin F, Howe DK, Honore S. Determination of genotypes of Toxoplasma gondii strains isolated from patients with toxoplasmosis. Journal of Clinical Microbiology 1997; 35: 1411–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubey JP, et al. Molecular and biological characterization of Toxoplasma gondii isolates from free-range chickens from Guyana, South America, identified several unique and common parasite genotypes. Parasitology 2007; 134: 1559–1565. [DOI] [PubMed] [Google Scholar]
- 24.Durmuş İ, et al. Poultry meat consumption and consumer trends in Turkey. Bitlis Eren University Journal of Science and Technology 2012; 2: 10–14. [Google Scholar]
- 25.Batz MB, Hoffmann S, Morris JG Jr.. Ranking the disease burden of 14 pathogens in food sources in the United States using attribution data from outbreak investigations and expert elicitation. Journal of Food Protection 2012; 75: 1278–1291. [DOI] [PubMed] [Google Scholar]
- 26.Hoffmann S, Batz MB, Morris JG Jr.. Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. Journal of Food Protection 2012; 75: 1292–1302. [DOI] [PubMed] [Google Scholar]
- 27.Dubey JP, et al. Biologic and genetic characteristics of Toxoplasma gondii isolates in free-range chickens from Costa Rica, Central America. Veterinary Parasitology 2006; 139: 29–36. [DOI] [PubMed] [Google Scholar]
- 28.Su C, et al. Moving towards an integrated approach to molecular detection and identification of Toxoplasma gondii. Parasitology 2010; 137: 1–11. [DOI] [PubMed] [Google Scholar]
- 29.Khan A, et al. Recent transcontinental sweep of Toxoplasma gondii driven by a single monomorphic chromosome. Proceedings of the National Academy of Sciences USA 2007; 104: 14872–14877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferreira Ade M, et al. Genetic analysis of natural recombinant Brazilian Toxoplasma gondii strains by multilocus PCR–RFLP. Infection, Genetics and Evolution 2006; 6: 22–31. [DOI] [PubMed] [Google Scholar]
- 31.Carneiro ACAV, et al. Genetic characterization of Toxoplasma gondii revealed highly diverse genotypes for isolates from newborns with congenital toxoplasmosis in Southeastern Brazil. Journal of Clinical Microbiology 2013; 51: 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grigg ME, et al. Unusual abundance of atypical strains associated with human ocular toxoplasmosis. Journal of Infectious Diseases 2001; 184: 633–639. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman HE, et al. Strain differences of Toxoplasma gondii. Journal of Parasitology 1959; 45: 189–190. [PubMed] [Google Scholar]
- 34.Dardé ML, Bouteille B, Pestre-Alexandre M. Isoenzyme analysis of 35 Toxoplasma gondii isolates and the biological and epidemiological implications. Journal of Parasitology 1992; 78: 786–794. [PubMed] [Google Scholar]
- 35.Khan A, et al. Composite genome map and recombination parameters derived from three archetypal lineages of Toxoplasma gondii. Nucleic Acids Research 2005; 33: 2980–2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suzuki Y, et al. Induction of tumor necrosis factor-α and inducible nitric oxide synthase fails to prevent toxoplasmic encephalitis in the absence of interferon-γ in genetically resistant BALB/c mice. Microbes and Infection 2000; 2: 455–462. [DOI] [PubMed] [Google Scholar]
- 37.Suzuki Y, et al. MHC class I gene(s) in the D/L region but not the TNF-alpha gene determines development of toxoplasmic encephalitis in mice. Journal of Immunology 1994; 153: 4649–4654. [PubMed] [Google Scholar]
- 38.Jones JL, Parise ME, Fiore AE. Neglected parasitic infections in the United States: toxoplasmosis. American Journal of Tropical Medicine and Hygiene 2014; 90: 794–799. [DOI] [PMC free article] [PubMed] [Google Scholar]