SUMMARY
Cryptosporidium is the leading aetiology of waterborne disease outbreaks in the United States. This report briefly describes the temporal and geographical distribution of US cryptosporidiosis cases and presents analyses of cryptosporidiosis case data reported in the United States for 1995–2012. The Cochran–Armitage test was used to assess changes in the proportions of cases by case status (confirmed vs. non-confirmed), sex, race, and ethnicity over the study period. Negative binomial regression models were used to estimate rate ratios (RR) and 95% confidence intervals (CI) for comparing rates across three time periods (1995–2004, 2005–2008, 2009–2012). The proportion of confirmed cases significantly decreased (P < 0·0001), and a crossover from male to female predominance in case-patients occurred (P < 0·0001). Overall, compared to 1995–2004, rates were higher in 2005–2008 (RR 2·92, 95% CI 2·08–4·09) and 2009–2012 (RR 2·66, 95% CI 1·90–3·73). However, rate changes from 2005–2008 to 2009–2012 varied by age group (Pinteraction < 0·0001): 0–14 years (RR 0·55, 95% CI 0·42–0·71), 15–44 years (RR 0·99, 95% CI 0·82–1·19), 45–64 years (RR 1·47, 95% CI 1·21–1·79) and ⩾65 years (RR 2·18, 95% CI 1·46–3·25). The evolving epidemiology of cryptosporidiosis necessitates further identification of risk factors in population subgroups. Adding systematic molecular typing of Cryptosporidium specimens to US national cryptosporidiosis surveillance would help further identify risk factors and markedly expand understanding of cryptosporidiosis epidemiology in the United States.
Key words: Cryptosporidium, water-borne infections
INTRODUCTION
Cryptosporidiosis is an infectious gastrointestinal disease caused by the parasite Cryptosporidium [1]. Illness is typically characterized by profuse, watery, non-bloody diarrhoea; other symptoms can include weight loss, abdominal pain or cramps, anorexia, fatigue, headache, fever, and vomiting [1]. In 2004, nitazoxanide became the first and only drug the U.S. Food and Drug Administration (FDA) has approved for the treatment of cryptosporidiosis in immunocompetent children aged 1–11 years [2]. In 2005, the FDA expanded this approval for all immunocompetent persons aged ⩾1 year [3]. Annually, approximately 8500 cases of cryptosporidiosis are reported in the United States [4], although an estimated 748 000 cases occur [5].
Cryptosporidiosis gained national recognition as a waterborne disease during massive drinking-water associated outbreaks in Texas in 1984 and Milwaukee in 1993 [6, 7], with the latter resulting in >400 000 cases. Consequently, national reporting of cryptosporidiosis cases began in 1995 [8]. Cryptosporidium is the leading aetiology of waterborne disease outbreaks in the United States (2001–2012) and has contributed to the significant increase in the incidence of recreational water-associated outbreaks [9, 10]. Since the first US pool-associated outbreak of cryptosporidiosis was detected in Los Angeles in 1988 [11], the parasite has caused many recreational water-associated outbreaks, particularly those associated with halogenated (i.e. chlorinated or brominated) recreational water venues. The most notable of these outbreaks occurred in New York in 2005 [12], Utah in 2007 [13], and Texas in 2008 [14], each of which affected thousands of people. Transmission is facilitated via treated drinking and recreational water because Cryptosporidium oocysts are extremely halogen tolerant [15–17], immediately infectious upon excretion, small enough in size (species predominantly infecting humans are approximately 4·5 × 5·5 µm) to bypass traditional filters, and have a low infectious dose. Foodborne, person-to-person, and animal-to-person transmission of Cryptosporidium can also occur. Investigations of foodborne outbreaks have implicated multiple sources [18], including produce [19], and unpasteurized milk [20, 21] and apple cider [22, 23]. Person-to-person transmission, particularly in childcare settings [24, 25], and zoonotic transmission, particularly involving livestock such as bovine calves, have also lead to cryptosporidiosis outbreaks [26–28].
In the United States, cryptosporidiosis surveillance data are typically analysed and published biennially [4, 29–33]. These data suggest that the epidemiology of cryptosporidiosis in the United States is evolving. For example, 2005 marked the first year for which >8000 cases were reported, compared to <4000 annually in previous years [29, 32, 33]. More cases were reported in females than males for the first time in 2005, and then consistently since 2007 [4, 29–33]. In 2011–2012, there was a substantial increase in the rates of reported non-confirmed cases; and for the first time, age-specific rates were higher in elderly adults than children aged 5–9 years [4, 29–33]. However, biennial analyses of cryptosporidiosis data preclude longitudinal analyses of how cryptosporidiosis epidemiology in the United States might be evolving over time. Given the emergence of Cryptosporidium as a pathogen of major public health importance in the United States and worldwide [34], it is critical to fill the gap in knowledge regarding its evolving epidemiology. The purpose of this study was to further elucidate the epidemiology of cryptosporidiosis in the United States by examining 18 years of cryptosporidiosis case data, focusing on differences across three time periods (1995–2004, 2005–2008, 2009–2012).
METHODS
Data
National cryptosporidiosis data reported to the U.S. Centers for Disease Control and Prevention (CDC) via the National Notifiable Diseases Surveillance System (NNDSS) were analysed. These data were voluntarily reported by public health agencies in the 50 states, the District of Columbia, and New York City for 1995–2012. At the time of analysis, 2012 was the last year for which finalized and complete data were available. NNDSS case reports include data on year of report; whether the case was associated with a detected outbreak; case-patient's county and state of residence, race, ethnicity, sex, and age; and case status (whether the case met criteria of the national case definition for confirmed, probable, suspect, or unknown classification). Age was categorized into four groups based on exposure commonalities: 0–14 years (children, for whom swimming is the most popular sports activity [35]), 15–44 years (older teenagers and young adults, where females are of childbearing age), 45–64 years (middle-aged adults), and ⩾65 years (senior citizens). Case status was dichotomized into confirmed and non-confirmed (probable, suspect, and unknown) cases. Risk factor data are not reported to NNDSS. National, systematic molecular typing of clinical Cryptosporidium specimens is currently not performed in the United States.
Analysis
NNDSS data for 1995–2012 were analysed using SAS v. 9.3 (SAS Institute Inc., USA). Annual incidence rates (cases/100 000 population) were calculated by dividing the number of reported incident cryptosporidiosis cases by each year's mid-year census estimate and multiplying by 100 000 [36]. Maps were created to display rates of cryptosporidiosis by county across four time periods: (1995–1999, 2000–2004, 2005–2008, and 2009–2012), using ArcGIS v. 10 (ESRI, USA); average annual cryptosporidiosis incidence rates/100 000 population for these time periods were calculated by summing each county's case counts over given years, dividing this sum by the sum of mid-year census estimates for each county over the given years, and then multiplying by 100 000.
To examine trends in binomial proportions of case status (confirmed vs. non-confirmed), sex, race, and ethnicity over time, the Cochran–Armitage test for trend was used [37, 38]. This test is appropriate for assessing trends in binomial proportions across the levels of an ordinal variable (i.e. year). The null hypothesis was that there was no change in proportion of non-confirmed, female, white, or non-Hispanic cases over time.
To examine changes in cryptosporidiosis rates during the study period, overall and by age group, count response models were used. Case counts were aggregated into three time periods selected based on availability of a drug approved to treat cryptosporidiosis, due to the hypothesized influence that drug availability might have on diagnosis. These time periods were: 1995–2004 (prior to availability of nitazoxanide), 2005–2008 (the first 4 years after nitazoxanide licensure) and 2009–2012 (the second 4 years after nitazoxanide licensure); data were aggregated over several years to increase stability and to simplify analysis and presentation. The negative binomial distribution was used because the data were overdispersed relative to the Poisson distribution. Model results were summarized as average annual incidence rates/100 000 population, and as incidence rate ratios (RR) and 95% confidence intervals (CI) to compare modelled cryptosporidiosis rates across time periods. The null hypothesis was that there was no change in cryptosporidiosis rates across time periods. To assess the age composition of case-patients across time periods, a time period × age group interaction was tested in the regression models. Subset analyses in non-outbreak cases were conducted to assess the potential impact of large outbreaks on changes in national reporting.
RESULTS
A total of 102 835 cases of cryptosporidiosis were reported to CDC for 1995–2012; 13·6% (n = 13 958) were outbreak-associated (Table 1). Annual overall incidence rates/100 000 population ranged from a low of 0·9 in 1997 to a high of 3·9 in 2007 (Fig. 1). During 1995–1999, the reported cryptosporidiosis rates were highest in the upper Midwest, the Northeast, and New Mexico (Fig. 2). During 2000–2004, cryptosporidiosis reporting remained highest in the upper Midwest and the Northeast, and incrementally increased in other parts of the country. During 2005–2008, there was a clear increase in cryptosporidiosis reporting throughout the United States, which persisted and continued to expand during 2009–2012.
Table 1.
Number of reported cryptosporidiosis cases, by outbreak-associated status and year, United States, 1995–2012 (N = 102 835)
| Outbreak-associated status | ||
|---|---|---|
| Year | Yes, n (%) | No/unknown*, n (%) |
| 1995 | 502 (16·9) | 2470 (83·1) |
| 1996 | 456 (16·1) | 2371 (83·9) |
| 1997 | 244 (9·5) | 2322 (90·5) |
| 1998 | 290 (7·6) | 3503 (92·4) |
| 1999 | 353 (12·7) | 2416 (87·3) |
| 2000 | 421 (13·5) | 2707 (86·5) |
| 2001 | 384 (10·1) | 3403 (89·9) |
| 2002 | 197 (6·5) | 2819 (93·5) |
| 2003 | 127 (3·6) | 3379 (96·4) |
| 2004 | 165 (4·5) | 3471 (95·5) |
| 2005 | 3431 (41·5) | 4840 (58·5) |
| 2006 | 519 (8·0) | 5960 (92·0) |
| 2007 | 3372 (28·9) | 8285 (71·1) |
| 2008 | 2031 (19·3) | 8469 (80·7) |
| 2009 | 201 (2·6) | 7455 (97·4) |
| 2010 | 298 (3·3) | 8653 (96·7) |
| 2011 | 544 (5·8) | 8769 (94·2) |
| 2012 | 423 (5·3) | 7585 (94·7) |
| Total | 13 958 (13·6) | 88 877 (86·4) |
Almost half (49·2%, n = 50 625) of all cases were reported not to be associated with an outbreak. Outbreak status was unknown for 38 250 (37·2%) cases and not reported for two (0·0%) cases. These two cases were included in those reported not to be associated with an outbreak and with unknown outbreak status.
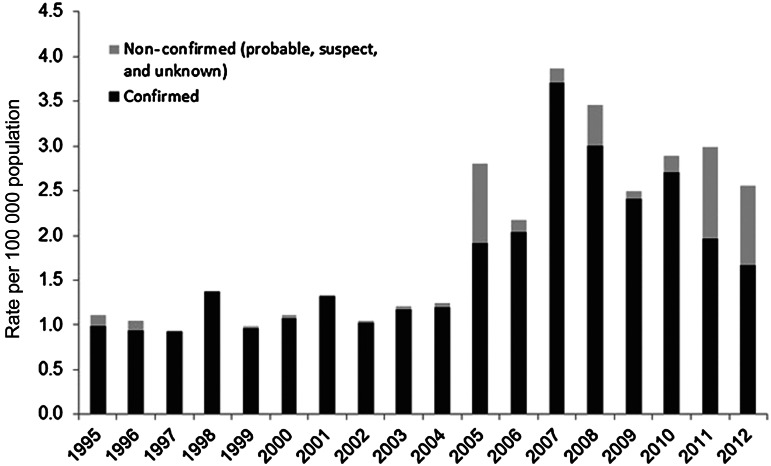
Fig. 1.
Incidence rate of reported cryptosporidiosis, by case status and year, United States, 1995–2012 (N = 102 835).
Fig. 2.
Incidence rate of reported cryptosporidiosis/100 000 population, by county, United States, 1995–2012. (a) 1995–1999, (b) 2000–2004, (c) 2005–2008, (d) 2009–2012.
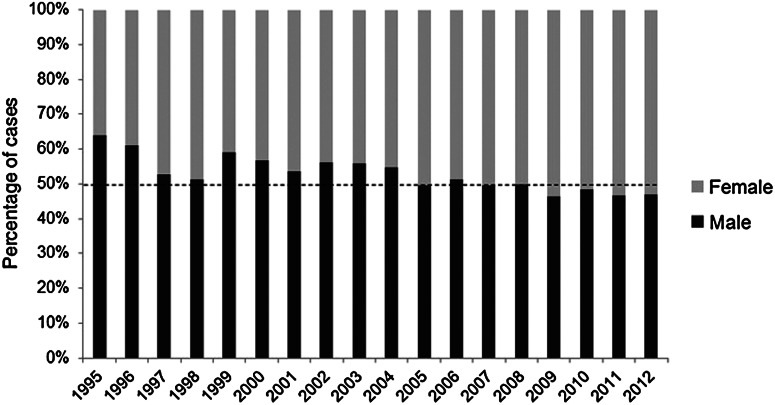
During 1995–2012, the majority (n = 89933, 87·5%) of reported cryptosporidiosis cases were confirmed. Although the total number of confirmed cases increased over time, the proportion of confirmed cases significantly decreased (Cochran–Armitage Z statistic: −58·77, P < 0·0001) (Fig. 1). During 1995–2012, the total number of reported cases in males and females was approximately equal. However, the ratio of male to female cases changed over time (Cochran–Armitage Z statistic: −23·94, P < 0·0001), and there was a crossover from male to female predominance which occurred in 2009 (Fig. 3). During 1995–2012, in cryptosporidiosis cases for which race was reported, the majority were in white patients (n = 61302, 83·7%), with a small but significant increase in the proportion of case reports in white patients over time (Cochran–Armitage Z statistic: 15·72, P < 0·0001); however, nearly one third (n = 29629, 28·8%) of case reports were missing race data during the study period. Similarly, in cryptosporidiosis cases for which ethnicity was reported, the majority were in non-Hispanic patients (n = 54043, 88·8%), with a small but significant increase in the proportion of case reports in non-Hispanic patients over time (Cochran–Armitage Z statistic: 9·92, P < 0·0001); however, over one third (n = 41978, 40·8%) of case reports were missing ethnicity data during the study period.
Fig. 3.
Percentage* of reported cryptosporidiosis cases, by sex and year, United States, 1995–2012. [* N = 101 823 cases: missing sex data for n = 1012 (1·0%) cases.]
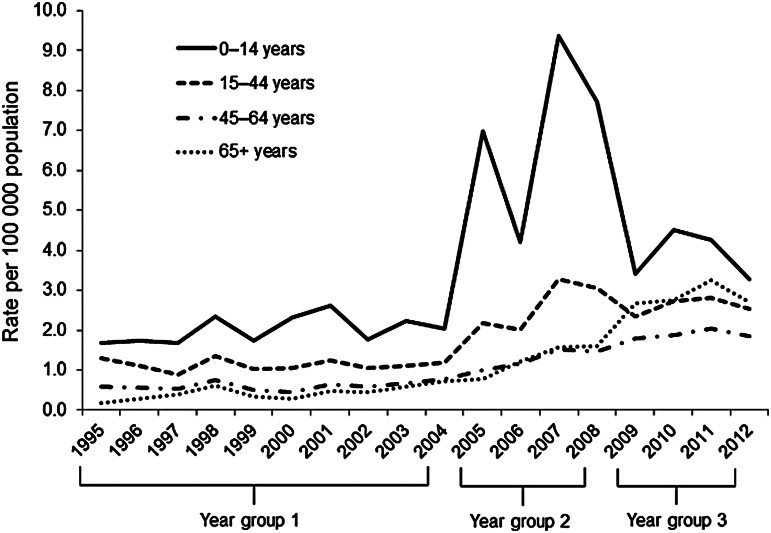
Cryptosporidiosis rates by time period and age group are displayed in Figure 4. Compared to 1995–2004, cryptosporidiosis rates were higher in 2005–2008 and 2009–2012. Across all time periods, rates were highest in children aged 0–14 years, followed by people aged 15–44 years in 1995–2004 and 2005–2008. During 2009–2012, rates were second highest in adults aged ⩾65 years.
Fig. 4.
Incidence rate of reported cryptosporidiosis, by county, by age group and year, United States, 1995–2012 (N = 102 835).
The changes in rates across the three time periods varied by age group (Pinteraction < 0·0001) (Fig. 4, Table 2). Compared to 1995–2004, rates in 2005–2008 and 2009–2012 increased overall (all ages combined) and within each age group. Compared to rates in 2005–2008, rates in 2009–2012 significantly decreased in children aged 0–14 years, did not significantly change in persons aged 15–44 years, and significantly increased in adults aged 45–64 years and ⩾65 years. After excluding outbreak-associated cases, rates were lower, but most rate ratios revealed similar patterns (Table 3). Excluding outbreak-associated cases had the greatest impact on rates in 2005–2008. The overall 2005–2008 rate was 25·7% lower, decreasing from 3·07/100 000 population (when outbreak-associated cases were included) to 2·28/100 000 population (when outbreak-associated cases were excluded). The rate in children aged 0–14 years decreased 34·7%, from 7·07 to 4·62/100 000 population. Additionally, the overall rate ratio for 2009–2012 vs. 2005–2008 was 0·91 when outbreak-associated cases were included in analyses but 1·17 when outbreak-associated cases were excluded.
Table 2.
Cryptosporidiosis incidence rates and rate ratios from negative binomial regression models, by age group and year group, United States, 1995–2012
| Age group (years) | Year group | Rate/100 000 population per year | RR (95% CI) (vs. 1995–2004) | RR (95% CI) (vs. 2005–2008) |
|---|---|---|---|---|
| All ages | 1995–2004 | 1·05 | 1·00 | |
| 2005–2008 | 3·07 | 2·92 (2·08–4·09) | 1·00 | |
| 2009–2012 | 2·80 | 2·66 (1·90–3·73) | 0·91 (0·61–1·37) | |
| 0–14 | 1995–2004 | 2·01 | 1·00 | |
| 2005–2008 | 7·07 | 3·51 (2·81–4·37) | 1·00 | |
| 2009–2012 | 3·87 | 1·92 (1·54–2·39) | 0·55 (0·42–0·71) | |
| 15–44 | 1995–2004 | 1·14 | 1·00 | |
| 2005–2008 | 2·64 | 2·32 (1·98–2·71) | 1·00 | |
| 2009–2012 | 2·61 | 2·29 (1·95–2·68) | 0·99 (0·82–1·19) | |
| 45–64 | 1995–2004 | 0·61 | 1·00 | |
| 2005–2008 | 1·29 | 2·10 (1·77–2·48) | 1·00 | |
| 2009–2012 | 1·89 | 3·09 (2·61–3·65) | 1·47 (1·21–1·79) | |
| ⩾65 | 1995–2004 | 0·44 | 1·00 | |
| 2005–2008 | 1·30 | 2·94 (2·10–4·12) | 1·00 | |
| 2009–2012 | 2·84 | 6·41 (4·59–8·97) | 2·18 (1·46–3·25) |
RR, Rate ratio; CI, confidence interval.
Table 3.
Cryptosporidiosis incidence rates and rate ratios from negative binomial regression models, by age group and year group, excluding outbreak-associated cases, United States, 1995–2012
| Age group (years) | Year group | Rate/100 000 population per year | RR (95% CI) (vs. 1995–2004) | RR (95% CI) (vs. 2005–2008) |
|---|---|---|---|---|
| All ages | 1995–2004 | 0·94 | 1·00 | |
| 2005–2008 | 2·28 | 2·42 (1·78–3·30) | 1·00 | |
| 2009–2012 | 2·68 | 2·84 (2·08–3·87) | 1·17 (0·81–1·70) | |
| 0–14 | 1995–2004 | 1·74 | 1·00 | |
| 2005–2008 | 4·62 | 2·66 (2·11–3·35) | 1·00 | |
| 2009–2012 | 3·54 | 2·04 (1·62–2·57) | 0·77 (0·58–1·01) | |
| 15–44 | 1995–2004 | 1·05 | 1·00 | |
| 2005–2008 | 2·12 | 2·03 (1·73–2·39) | 1·00 | |
| 2009–2012 | 2·50 | 2·39 (2·04–2·81) | 1·18 (0·97–1·43) | |
| 45–64 | 1995–2004 | 0·57 | 1·00 | |
| 2005–2008 | 1·16 | 2·02 (1·65–2·46) | 1·00 | |
| 2009–2012 | 1·87 | 3·26 (2·67–3·97) | 1·62 (1·28–2·05) | |
| ⩾65 | 1995–2004 | 0·42 | 1·00 | |
| 2005–2008 | 1·24 | 2·96 (2·05–4·28) | 1·00 | |
| 2009–2012 | 2·82 | 6·73 (4·67–9·70) | 2·27 (1·47–3·50) |
RR, Rate ratio; CI, confidence interval.
DISCUSSION AND CONCLUSION
This report presents the first examination of the evolving epidemiology of US cryptosporidiosis case-report data for 1995–2012. Analyses reveal a significant increase in reporting of cryptosporidiosis accompanied by an evolving composition of reported cases, particularly in the geographical distribution and status of cryptosporidiosis cases as well as the sex and age distribution of cases. These findings underscore the need to further characterize the epidemiology of cryptosporidiosis in the United States.
Overall, rates of reported cryptosporidiosis significantly increased during the study period. The marked increase in reporting and spread of cryptosporidiosis throughout the United States, in particular from 2005 to 2008, was apparently driven, at least in part, by large outbreaks that occurred during the study period [12–14]. The substantial impact of recreational water-associated outbreaks such as those that occurred in New York (2005), Utah (2007), and Texas (2008) can be seen in the sensitivity analyses. When all outbreak-associated cases were removed, the 2005–2008 rates were expectedly much lower while non-outbreak rates continued to increase from 2005–2008 to 2009–2012. The increases in reporting might be due to increased pathogen transmission following these outbreaks; increased investment in states' capacity to detect, investigate, and report cases following outbreaks; or an artifact of changes in healthcare providers' awareness, diagnosis, and treatment of cryptosporidiosis associated with drug licensure. The significant increase in rates seen after 2004 coincides with the 2005 FDA licensure of nitazoxanide to treat cryptosporidiosis in immunocompetent case-patients aged ⩾1 year. The availability of a drug to treat cryptosporidiosis might have increased healthcare providers' awareness of the disease or motivated them to order diagnostic testing for cryptosporidiosis.
It cannot be determined from NNDSS data alone whether the observed changes in geographical distribution seen in this study reflect regional differences in Cryptosporidium ecology and transmission, or jurisdictional differences in the capacity to detect, investigate, or report cases. The increased reporting in the upper Midwest region could be a consequence of possible increased Cryptosporidium transmission following the 1993 Milwaukee drinking water-associated outbreak or it could be a consequence of higher cattle density in this region compared with other regions; this increased cattle density could be a proxy for increased contact with pre-weaned calves [39, 40]. Additionally, the Milwaukee outbreak in 1993 might have led to increased regional awareness of cryptosporidiosis or increased regional investment in capacity to detect, investigate, and report cases.
Changes in the proportion of cases classified as confirmed or non-confirmed could be due to a variety of factors. The increase in the proportion of non-confirmed cases in 2005 can be directly attributed to the New York recreational water-associated outbreak that occurred in that year, as most of the >2000 cases associated with that outbreak were reported as probable. In contrast, the increasing proportion of non-confirmed cases starting in 2011 is more likely a result of recent revisions in the case definition for national surveillance of cryptosporidiosis and possible changes in diagnostic testing practices. Since 1995, the case definition for national surveillance has changed four times: 1998, 2009, 2011, and 2012 [8, 41–44]; these changes have largely been in response to innovations in laboratory methods to detect Cryptosporidium [45–47]. In recent years, immunochromatographic card tests have been increasingly utilized because they do not require a trained microbiologist or parasitologist to administer or interpret results. However, failure to follow manufacturers' directions when running these tests (e.g. storing them outside the specified temperature range or reading results after the specified time) can lead to false positives [48]. The issues with immunochromatographic card tests prompted the 2011 revision of confirmed cryptosporidiosis cases to include only those cases diagnosed by laboratory methods with a high positive predictive value [44]. Before this change, all cases with laboratory evidence of Cryptosporidium were classified as confirmed, regardless of type of diagnostic test used [8]. The most recent 2012 revision specifies which diagnostic tests (i.e. direct fluorescent antibody test, polymerase chain reaction (PCR), enzyme immunoassay, or light microscopy of stained specimen) are required to meet the criteria for confirmed case status. Since test type might not be known, this would increase the number of non-confirmed cases reported. These alterations to the case definition for national surveillance present challenges to interpreting changes in national cryptosporidiosis data over time.
Although the overall proportion of males and females was roughly equal throughout the study, an analysis by time period revealed that the ratio of male to female case-patients changed from male predominance (1995–2004) to female predominance (2009–2012). One explanation for this crossover might be that in earlier years, Cryptosporidium circulated as an opportunistic pathogen in HIV-infected individuals [49], who were predominantly male. However, the incidence of cryptosporidiosis in HIV-infected persons has decreased since the introduction of highly active antiretroviral therapy for HIV infection [50, 51]. This hypothesis cannot be tested with NNDSS data since HIV status is not reported to NNDSS. Furthermore, since 2005, Cryptosporidium has emerged as the leading aetiology of recreational water-associated outbreaks [9], which disproportionately affect young children as suggested here and shown elsewhere [13]. Consequently, the risk for infection via person-to-person transmission might have increased in females. As caregivers to young children both inside and outside of the home (e.g. in childcare facilities), females of childbearing age could potentially be at increased risk for infection resulting from person-to-person transmission due to the lack of or nascent toileting skills in young children and poor hygiene (e.g. inadequate hand washing) in caregivers and young children [24, 52]. Challenges in maintaining proper hygiene, combined with exposure to recreational water and childcare settings, place both young children and their caregivers at increased risk for cryptosporidiosis [52–54].
Consistent with previously reported research [4], in our study, reported rates of cryptosporidiosis were highest in children across all time periods. Rate changes in national surveillance data did not occur uniformly across all age groups. Rather, cryptosporidiosis rates increased earlier (2005–2008) in the two youngest groups, likely driven by the three large recreational water-associated outbreaks mentioned previously, while incidence rates increased later in the two older groups (2009–2012). Rates in adults aged ⩾65 years increased starting in 2005. It is unclear why; however, 2005 is the year that the FDA licensure of nitazoxanide first included treatment of cryptosporidiosis in immunocompentent patients aged ⩾12 years. It is possible that the availability of a new treatment contributed to an increase in reported cryptosporidiosis incidence rates in adults, as opposed to an actual increase in the occurrence of disease in this population; however, risk factors for cryptosporidiosis in elderly adults have not been reported in the literature and need to be explored further.
Our analysis is subject to several limitations. Due to underreporting (only 2% of estimated cryptosporidiosis cases are reported annually in the United States), our findings might not be generalizable to all cryptosporidiosis cases occurring in the United States [4, 5]. All infected persons do not have symptoms; all of those with disease do not seek healthcare; and all those who do seek healthcare do not have the necessary diagnostic testing. This is a typical limitation of national surveillance data for diseases caused by infectious enteric pathogens [5], and might be partially overcome with the introduction of multiplex molecular assays for the detection and identification of enteric diseases. Next, although changes observed in national surveillance might reflect the general epidemiology of cryptosporidiosis in the United States, variability in surveillance capacity and reporting requirements across reporting jurisdictions over time could limit our ability to compare cryptosporidiosis rates over time. Additionally, the lack of data on race and ethnicity [which were captured in NNDSS, but a high percentage (>25%) of case reports were missing these data]; potential exposures or risk factors (e.g. immune status, swallowing contaminated water, contact with livestock, or caring for an infected person); and the Cryptosporidium species that caused each specific case (which were not captured in NNDSS), limits further characterization of cryptosporidiosis epidemiology in the United States. The data suggested that there might have been an increase in the proportion of reports of cases in white and non-Hispanic patients over time; however, the high proportion of missing data limit the conclusions that can be drawn about racial and ethnic changes in the epidemiology of cryptosporidiosis over the study period. Finally, misclassification of outbreak-associated cases as non-outbreak-associated cases, due to limited ability to detect epidemiological links in cases, would limit the ability to exclude all true outbreak-associated cases from sensitivity analyses.
Unlike the UK, the United States does not perform systematic molecular characterization of Cryptosporidium specimens nationally. A molecular typing-based surveillance system could help answer some of the questions posed herein [4]. Human cryptosporidiosis is predominantly caused by C. hominis (primarily transmitted anthroponotically) and C. parvum (transmitted zoonotically or anthroponotically), which are morphologically indistinguishable [55, 56]. Thus, knowing the species and subtype can help identify the exposure that led to infection in a given case-patient and epidemiological links in cases [56, 57]. Molecular typing results can also be used in conjunction with traditional epidemiological data to geographically and temporally characterize the distribution of species and subtypes and to ultimately differentiate risk factors for disease in the population. For example, a recent case-control study conducted in the UK revealed that risk factors for cryptosporidiosis differed by species; travelling abroad and changing diapers of children aged <5 years were risk factors for disease caused by C. hominis, while contact with farm animals was a risk factor for disease caused by C. parvum [53]. Currently in the United States, CDC uses nested PCR-restriction fragment length polymorphism (RFLP) to speciate, and DNA sequencing of the 60-kDa glycoprotein (gp60) gene to subtype, Cryptosporidium specimens typically collected during outbreak investigations and submitted by state public health partners, i.e. confirming cryptosporidiosis outbreaks [58]. CDC is currently collaborating with state partners to implement these molecular techniques in state public health laboratories. This step is the first of many, with the ultimate goal being national systematic whole-genome sequencing of all clinical Cryptosporidium specimens and reporting of standard risk factor data.
CONCLUSION
This study identified multiple shifts in national-level cryptosporidiosis surveillance data and raises a number of research questions. Further research is needed to better explain increases in reporting after 2004, particularly in years without large recreational water-associated outbreaks; geographical distribution of cases; cryptosporidiosis risk factors, particularly in females and older adults; and how the use of immunochromatographic card tests and nitazoxanide availability has influenced surveillance of cryptosporidiosis.
ACKNOWLEDGEMENTS
The findings and conclusions in this paper are those of the authors, and do not necessarily represent the official position of the U.S. CDC.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Warren C, Guerrant R. Clinical disease and pathology. In: Fayer R, Xiao L, eds. Cryptosporidium and Cryptosporidiosis, 2nd edn. Boca Raton, FL: CDC Press, 2008, pp. 235–254. [Google Scholar]
- 2.U.S. Food and Drug Administration. Alinia (nitazoxanide) label approved 21 July 2004.
- 3.U.S. Food and Drug Administration. Alinia (nitazoxanide) label approved 16 June 2005.
- 4.Painter JE, et al. Cryptosporidiosis surveillance – United States, 2011–2012. Morbidity and Mortality Weekly Report. Surveillance Summaries 2015; 64: 1–14. [Google Scholar]
- 5.Scallan E, et al. Foodborne illness acquired in the United States – major pathogens. Emerging Infectious Diseases 2011; 17: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Antonio RG, et al. A waterborne outbreak of cryptosporidiosis in normal hosts. Annals of Internal Medicine 1985; 103: 886–888. [DOI] [PubMed] [Google Scholar]
- 7.Mac Kenzie WR, et al. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. New England Journal of Medicine 1994; 331: 161–167. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Centers for Disease Control and Prevention. Cryptosporidiosis (Cryptosporidium) 1995 case definition. 1995.
- 9.Hlavsa MC, et al. Outbreaks of illness associated with recreational water – United States, 2011–2012. Morbidity and Mortality Weekly Report 2015; 64: 668–672. [PMC free article] [PubMed] [Google Scholar]
- 10.Hlavsa MC, et al. Recreational water-associated disease outbreaks – United States, 2009–2010. Morbidity and Mortality Weekly Report 2014; 63: 6–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Sorvillo FJ, et al. Swimming-associated cryptosporidiosis. American Journal of Public Health 1992; 82: 742–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoder JS, et al. Surveillance for waterborne disease and outbreaks associated with recreational water use and other aquatic facility-associated health events – United States, 2005–2006. Morbidity and Mortality Weekly Report Surveillance summaries 2008; 57: 1–29. [PubMed] [Google Scholar]
- 13.U.S. Centers for Disease Control and Prevention. Communitywide cryptosporidiosis outbreak – Utah, 2007. Morbidity and Mortality Weekly Report 2008; 57: 989–993. [PubMed] [Google Scholar]
- 14.Cantey PT, et al. Outbreak of cryptosporidiosis associated with a man-made chlorinated lake – Tarrant County, Texas, 2008. Journal of Environmental Health 2012; 75: 14–19. [PubMed] [Google Scholar]
- 15.Chappell CL, et al. Cryptosporidium hominis: experimental challenge of healthy adults. American Journal of Tropical Medicine and Hygiene 2006; 75: 851–857. [PubMed] [Google Scholar]
- 16.Okhuysen PC, et al. Virulence of three distinct Cryptosporidium parvum isolates for healthy adults. Journal of Infectious Diseases 1999; 180: 1275–1281. [DOI] [PubMed] [Google Scholar]
- 17.Shields JM, et al. Inactivation of Cryptosporidium parvum under chlorinated recreational water conditions. Journal of Water and Health 2008; 6: 513–520. [DOI] [PubMed] [Google Scholar]
- 18.Robertson LJ, Chalmers RM. Foodborne cryptosporidiosis: is there really more in Nordic countries? Trends in Parasitology 2013; 29: 3–9. [DOI] [PubMed] [Google Scholar]
- 19.Painter JA, et al. Attribution of foodborne illnesses, hospitalizations, and deaths to food commodities by using outbreak data, United States, 1998–2008. Emerging Infectious Diseases 2013; 19: 407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harper CM, et al. Outbreak of Cryptosporidium linked to drinking unpasteurised milk. Communicable Diseases Intelligence Quarterly Report 2002; 26: 449–450. [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal M, et al. Notes from the field: cryptosporidiosis associated with consumption of unpasteurized goat milk – Idaho, 2014. Morbidity and Mortality Weekly Report 2015; 64: 194–195. [PMC free article] [PubMed] [Google Scholar]
- 22.Blackburn BG, et al. Cryptosporidiosis associated with ozonated apple cider. Emerging Infectious Diseases 2006; 12: 684–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Millard PS, et al. An outbreak of cryptosporidiosis from fresh-pressed apple cider. Journal of the American Medical Association 1994; 272: 1592–1596. [PubMed] [Google Scholar]
- 24.Cordell RL, Addiss DG. Cryptosporidiosis in child care settings: a review of the literature and recommendations for prevention and control. Pediatric Infectious Diseases Journal 1994; 13: 310–317. [PubMed] [Google Scholar]
- 25.Turabelidze G, et al. Communitywide outbreak of cryptosporidiosis in rural Missouri associated with attendance at child care centers. Archives of Pediatrics and Adolescent Medicine 2007; 161: 878–883. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Centers for Disease Control and Prevention. Outbreak of cryptosporidiosis associated with a firefighting response – Indiana and Michigan, June 2011. Morbidity and Mortality Weekly Report 2012; 61: 153–156. [PubMed] [Google Scholar]
- 27.Gormley FJ, et al. Zoonotic cryptosporidiosis from petting farms, England and Wales, 1992–2009. Emerging Infectious Diseases 2011; 17: 151–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Webb LM, et al. Outbreak of cryptosporidiosis among responders to a rollover of a truck carrying calves – Kansas, April 2013. Morbidity and Mortality Weekly Report 2014; 63: 1185–1188. [PMC free article] [PubMed] [Google Scholar]
- 29.Yoder JS, Beach MJ. Cryptosporidiosis surveillance – United States, 2003–2005. Morbidity and Mortality Weekly Report. Surveillance Summaries 2007; 56: 1–10. [PubMed] [Google Scholar]
- 30.Yoder JS, Harral C, Beach MJ. Cryptosporidiosis surveillance – United States, 2006–2008. Morbidity and Mortality Weekly Report. Surveillance Summaries 2010; 59: 1–14. [PubMed] [Google Scholar]
- 31.Yoder JS, et al. Cryptosporidiosis surveillance – United States, 2009–2010. Morbidity and Mortality Weekly Report. Surveillance Summaries 2012; 61: 1–12. [PubMed] [Google Scholar]
- 32.Dietz VJ, Roberts JM. National surveillance for infection with Cryptosporidium parvum, 1995–1998: what have we learned? Public Health Reports 2000; 115: 358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hlavsa MC, Watson JC, Beach MJ. Cryptosporidiosis surveillance – United States 1999–2002. Morbidity and Mortality Weekly Report. Surveillance Summaries 2005; 54: 1–8. [PubMed] [Google Scholar]
- 34.Checkley W, et al. A review of the global burden, novel diagnostics, therapeutics, and vaccine targets for Cryptosporidium. Lancet Infectious Diseases 2015; 15: 85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau. U.S. Census Bureau, Statistical Abstract of the United States: 2012. 2012.
- 36.U.S. Census Bureau. Annual estimates of the population for the United States, Regions, States, and Puerto Rico: 1 April 2010 to 1 July 2012. 2012.
- 37.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics 1955; 11: 375–386. [Google Scholar]
- 38.Cochran WG. Some methods for strengthening the common χ2 tests. Biometrics 1954; 10: 417–451. [Google Scholar]
- 39.Jagai JS, et al. Patterns of protozoan infections: spatiotemporal associations with cattle density. EcoHealth 2010; 7: 33–46. [DOI] [PubMed] [Google Scholar]
- 40.Xiao L, et al. Distribution of Cryptosporidium parvum subtypes in calves in eastern United States. Parasitology Research 2007; 100: 701–706. [DOI] [PubMed] [Google Scholar]
- 41.U.S. Centers for Disease Control and Prevention. Cryptosporidiosis (Cryptosporidium) 1998 case definition. 1998.
- 42.U.S. Centers for Disease Control and Prevention. Cryptosporidiosis (Cryptosporidium) 2009 case definition. 2009.
- 43.U.S. Centers for Disease Control and Prevention. CDC. Cryptosporidiosis (Cryptosporidium) 2011 case definition. 2011.
- 44.U.S. Centers for Disease Control and Prevention. Cryptosporidiosis (Cryptosporidium) 2012 case definition. 2012.
- 45.Garcia LS, Shimizu RY. Detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal specimens using the ColorPAC combination rapid solid-phase qualitative immunochromatographic assay. Journal of Clinical Microbiology 2000; 38: 1267–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garcia LS, et al. Commercial assay for detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal specimens by rapid solid-phase qualitative immunochromatography. Journal of Clinical Microbiology 2003; 41: 209–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnston SP, et al. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. Journal of Clinical Microbiology 2003; 41: 623–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robinson TJ, et al. Evaluation of the positive predictive value of rapid assays used by clinical laboratories in Minnesota for the diagnosis of cryptosporidiosis. Clinical Infectious Diseases 2010; 50: e53–55. [DOI] [PubMed] [Google Scholar]
- 49.Moore RD, Chaisson RE. Natural history of opportunistic disease in an HIV-infected urban clinical cohort. Annals of Internal Medicine 1996; 124: 633–642. [DOI] [PubMed] [Google Scholar]
- 50.Brady MT, et al. Declines in mortality rates and changes in causes of death in HIV-1-infected children during the HAART era. Journal of Acquired Immune Deficiency Syndromes 2010; 53: 86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaplan JE, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clinical Infectious Diseases 2000; 30 (Suppl. 1): S5–14. [DOI] [PubMed] [Google Scholar]
- 52.Roy SL, et al. Risk factors for sporadic cryptosporidiosis among immunocompetent persons in the United States from 1999 to 2001. Journal of Clinical Microbiology 2004; 42: 2944–2951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hunter PR, et al. Sporadic cryptosporidiosis case-control study with genotyping. Emerging Infectious Diseases 2004; 10: 1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robertson B, et al. Case-control studies of sporadic cryptosporidiosis in Melbourne and Adelaide, Australia. Epidemiology and Infection 2002; 128: 419–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xiao L, et al. Cryptosporidium taxonomy: recent advances and implications for public health. Clinical Microbiology Reviews 2004; 17: 72–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chalmers RM, et al. Epidemiology of anthroponotic and zoonotic human cryptosporidiosis in England and Wales, 2004–2006. Epidemiology and Infection 2011; 139: 700–712. [DOI] [PubMed] [Google Scholar]
- 57.Cama VA, et al. Cryptosporidium species and subtypes and clinical manifestations in children, Peru. Emerging Infectious Diseases 2008; 14: 1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xiao L, et al. Subtype analysis of Cryptosporidium specimens from sporadic cases in Colorado, Idaho, New Mexico, and Iowa in 2007: widespread occurrence of one Cryptosporidium hominis subtype and case history of an infection with the Cryptosporidium horse genotype. Journal of Clinical Microbiology 2009; 47: 3017–3020. [DOI] [PMC free article] [PubMed] [Google Scholar]