Abstract
Background
The Coronavirus Disease 2019 (COVID-19) caused by the SARS-CoV-2 virus has taken the lives of more than 100,000 healthcare workers (HCWs) so far. Those who survived continuously work under immense physical and psychological pressure, and their quality of life (QoL) is impacted. The study aimed to assess the QoL among HCWs in Bangladesh who recovered from COVID-19.
Methods
This cross-sectional, telephonic interview-based study was conducted among 322 randomly selected HCWs from Bangladesh who were positive for COVID-19 and recovered from the infection before the interview. Data were collected from June to November 2020. We examined the impact of COVID on the QoL of the participants using the validated Bangladesh version of the World Health Organization (WHO) Quality of life questionnaire brief (WHOQOL-BREF). All analyses were done by STATA (Version 16.1).
Results
More than half of the health care professionals were male (56.0%), aged between 26–35 years (51%), and completed graduation (49%). The majority of the study participants in the four domains were married (n = 263, 81%) and living in Dhaka. The average score of the participants was 70.91 ± 13.07, 62.68 ± 14.99, 66.93 ± 15.14, and 63.56 ± 12.11 in physical, psychological, social relationship and environmental domains, respectively. HCWs in urban areas enjoyed 2.4 times better socially stable lives (OR: 2.42, 95% CI: 1.18–4.96) but 72% less psychologically satisfactory lives.
Conclusion
HCWs' post-COVID quality of life depended on variable interaction of demographic socioeconomic, including old age, female sex, graduation, and higher monthly income. The findings indicate the issues which should be addressed to improve the quality of life of frontline workers who fight against the pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-022-07961-z.
Keywords: Bangladesh, COVID-19, Quality of life (QoL), Healthcare workers, WHOQOL-BREF
Background
The Coronavirus Disease 2019 (COVID-19) caused by the SARS-CoV-2 virus was first identified in China in late 2019 as a cluster of unexplained pneumonia cases. Since then, it has spread worldwide and become a global public health concern by infecting millions of people and claiming hundreds and thousands of lives [1, 2]. With high transmission capability, numbers of mutations, and other associated factors, the impact of this virus outspreads physical health and encompasses mental health, social functioning, and environmental safety [3, 4]. Since its emergence, the pandemic is constantly putting tremendous pressure on healthcare systems worldwide. Healthcare workers (HCWs) are on the frontlines to combat this invisible enemy. Nevertheless, managing an exponentially expanding number of COVID-19 patients has placed them at a high risk of exposure [5].
A Chinese study reported 3000 HCWs infected (3.8%) with five deaths by early February 2020. In Italy, this rate jagged to 10.5% in late April, and 157 HCW deaths were documented in England until early May 2020 [6–8]. Hence, the fear of infection with its consequences and unforeseen interruptions to everyday life has put the front liners in a stressful situation. In Bangladesh, where there was a scarcity of HCWs from the very beginning (according to WHO, 3.05 doctors and 1.07 nurses are available per 10,000 populations in Bangladesh) [9], battle against COVID-19 with higher patient load in grinding [10]. Although exact data could not be extracted, various sources suggest that more than 5,000 HCWs have been infected, and more than 300 have died over one year since the first case was diagnosed in Bangladesh on March 8, 2020 [11]. Moreover, COVID-19 recovered HCWs suffered significant long-term symptoms that impaired their quality of life. Studies have revealed that, notwithstanding the long-term recovery, a few COVID-19 survivors experience long-term consequences such as lung fibrosis, debilitating chronic symptoms, and psychological issues, negatively impacting their quality of living [12–14].
According to World Health Organization (WHO), "an individual's perception of their position in life in the context of the culture and value systems in which they live and concerning their goals, expectations, standards, and concerns are defined as the quality of life" [15]. Previous researchers concluded that COVID-19 might lead to decreased health-related quality of life (HRQoL) by significantly impairing life's physical and psychological domain [16–18]. However, the importance of evaluating the QoL of HCWs during their recovery period was often overlooked and underreported. Nevertheless, HCWs may have poorer clinical outcomes than non-HCWs because they are exposed to high SARS-CoV-2 density environments, work longer hours, and are more prone to psychological trauma [19]. Long term clinical consequences of COVID-19 could be linked to disruption of HCWs’ professional, psychological, social and environmental wellbeing [20, 21]. HCWs have been reported to have a high mental health impact of COVID-19, requiring professional mental health support [20, 22–24].
A significant decline in QoL was observed among people who worked in healthcare facilities during previous pandemic periods [21]. However, the number of studies to explore the QoL among HCWs recovered from COVID-19 is limited. Identifying their QoL is essential to planning their early recovery and return to hospitals. Therefore, we undertook this study to evaluate the quality of life (QoL) and their related determinants among HCWs in Bangladesh who recovered from COVID-19.
Methods
Study design and participants
From June 2020 to November 2020, we conducted this research on the COVID-19 positive HCWs identified and confirmed to be such by Reverse Transcription-Polymerase Chain Reaction (RT-PCR) who had either improved clinically or tested negative for the virus. For three days, clinical recovery was classified as a consecutive absence of fever, cough, or respiratory distress for mild to moderate pneumonia patients and released with hospital advice. For the asymptomatic patients, passing 14 days after the first diagnosis was regarded as a clinically cure. The study excluded those treated for COVID-19, pregnant women, and the critically ill. In our earlier nationwide study, we collected a list of COVID-19 positive cases from the whole country [25]. We randomly approached 4584 patients and then completed an interview of 3,244 participants from the list. The detailed study methods were described elsewhere [25]. Among those 3,244 participants, we found 322 HCWs and considered them recruited in this analysis. As our study response rate was 60%, we had to approach a total of 527 HCWs, of whom 134 respondents refused, 45 individuals were unreachable, and 26 participants were left before completing the questionnaire at the time of the interview. We used the Bangla validated version of WHOQOL-BREF [26] to measure the quality of life of HCWs and questionnaires related to socio-demography developed by our research team.
Sociodemographic information, symptoms, and comorbidity profile
To assess the QoL of the HCWs, we collected participants' sociodemographic information, including age, gender, domicile, religion, educational attainment, marital status, and financial condition. In addition, we also recorded the details of their COVID-19 related hospitalization history, personal habits, presence of any chronic diseases such as heart disease, hypertension (HTN), asthma/chronic obstructive pulmonary disease (COPD), diabetes mellitus (DM), chronic kidney disease (CKD), and cancer. Symptoms that may arise or persist in the post-COVID period were also documented during the survey.
WHOQOL-BREF
We utilized WHOQOL-BREF, a brief validated version of the WHOQOL-100 quality of life assessment questionnaire [27], to assess the QoL of COVID-19 recovered HCWs. The WHOQOL Group collaborated with fifteen foreign field centres to develop the later instrument to create a QoL evaluation that could be used across cultures. This 26 item QOL instrument has shown good to excellent psychometric properties and is cross-culturally sensitive. The WHOQOL-BREF generates a profile and score for each of the 4 QOL domains; questions are centred around the meaning respondents attribute to each aspect of life and how problematic or satisfactory they perceive them. The Physical Health domain questions are based on daily activities, medical aid, energy, mobility, the extent of pain, sleeping pattern, and working capacity. The Psychological domain focuses on participants’ personal beliefs, positive and negative feelings, self-esteem, body image, thinking, and learning capabilities. The Social Relationships domain explores the respondent’s overall satisfaction with their personal and social life. Lastly, the environment domain comprises questions about safety and security, contentment with one's property and physical surroundings, finances (does one have enough money to satisfy one's requirements), access to the necessary care, information, and transport. Moreover, the questionnaire has two specific questions regarding participants’ opinions regarding their overall QoL and health. We used the Bangla validated version of the original WHOQOL-BREF [26] questionnaire.
Study procedure
Considering the present pandemic situation, we performed interviews over the phone. We approached all the randomly selected HCWs and recorded the response of those who felt comfortable participating in the survey. Besides, we informed the participants that there was no correct or wrong answer before the interview. Items that were misunderstood were replied, and interviewees were motivated to respond to the questions as they saw fit. The WHOQOL-BREF section of the questionnaire was scored following the manual [15]. The internal consistency of the WHOQOL-BREF questions was weighed using Cronbach's alpha. The strength of association of the questions was good among our respondents (Cronbach's alpha = 0.86).
Statistical analysis
We applied descriptive and inferential methods to describe the quality of life of the Covid-19 recovered healthcare workers and explore the determinants of QoL among them. Statistical software STATA (Version 16.1) was used for statistical analysis. QoL scores were explored separately in four domains: physical, psychological, social, and environmental. Analyzing variance (ANOVA) models and verifying the normality assumption allowed us to compare continuous variables across different categories. We performed an independent sample t-test to compare the means of two continuous variables. We used frequencies (percent) to describe the categorical variables and chi-square tests to determine the associations between groups. For binary logistic regression analysis, QoL scores were translated into binary scores by treating a value greater or equal to 50 as 1 ("good"), otherwise 0 ("poor"). All tests were two-tailed, and p-values less than or equal to 0.05 were considered statistically significant.
Results
Table 1 illustrates the sociodemographic variable of the study respondents. Among 322 health care professionals, more than half were male (n = 180, 56%), aged between 26–35 years (51%), and completed graduation (n = 158, 49%). Physicians accounted for 68% of our respondents, nurses for 27%, and others for 5% (such as laboratory technicians, pharmacists). The majority of the study participants were married (n = 263, 81%), urban dwellers (n = 247, 77%) and living in Dhaka (n = 154, 48%). According to the income distribution, most participants (n = 103, 35.64%) earned 20,000–40,000 BDT per month. Diabetes (16%), asthma/COPD (16%), and hypertension (15%) were the most prevalent comorbidities, followed by heart disease, cancer, and chronic kidney disease. One-fourth of the interviewee was smokers/past smokers (n = 80, 25%). Around 43% of HCW (n = 137, 42.55%) had to be hospitalized due to COVID-19 severity, while the other COVID-19 infected health care professionals were at home/institutional isolation during the whole infection period.
Table 1.
Socio-demographics variable of the study participants (n = 322)
| Name of Variable | Frequency (%) |
|---|---|
| Age group (in years) | |
| < 26 | 40 (12%) |
| 26–30 | 96 (30%) |
| 31–35 | 69 (21%) |
| 36–40 | 45 (14%) |
| 41–45 | 37 (12%) |
| 46 + | 35 (11%) |
| Gender | |
| Male | 180 (56%) |
| Female | 142 (44%) |
| Division | |
| Barisal | 32 (10%) |
| Chattogram | 70 (22%) |
| Dhaka | 154 (48%) |
| Khulna | 5 (2%) |
| Mymensingh | 18 (6%) |
| Rajshahi | 14 (4%) |
| Rangpur | 12 (4%) |
| Sylhet | 17 (5%) |
| Residence | |
| Rural | 44 (14%) |
| Urban | 247 (77%) |
| Semi-urban | 31 (9%) |
| Religion | |
| Muslim | 255 (79%) |
| Non-Muslim | 67 (21%) |
| Educational status | |
| Below Graduation (SSC/HSC) | 104 (32%) |
| Graduation | 158 (49%) |
| Post-graduation | 60 (19%) |
| Marital status | |
| Single | 57 (18%) |
| Married | 263 (81%) |
| others | 2 (1%) |
| Income (BDT) | |
| < 20,000 | 56 (19%) |
| 20,000–40,000 | 103 (36%) |
| 4000–60,000 | 56 (19%) |
| 60,000 + | 74 (26%) |
| Smoking status | |
| Never smoked | 242 (75%) |
| Current smoker | 58 (18%) |
| Past smoker | 22 (7%) |
| Chronic disease | |
| Hypertension | 48 (15%) |
| Diabetes | 51 (16%) |
| Asthma/ COPD | 50 (16%) |
| Heart disease | 23 (7%) |
| Chronic kidney disease | 9 (3%) |
| Cancer | 12 (4%) |
| Hospital admission (Yes) | 137 (43%) |
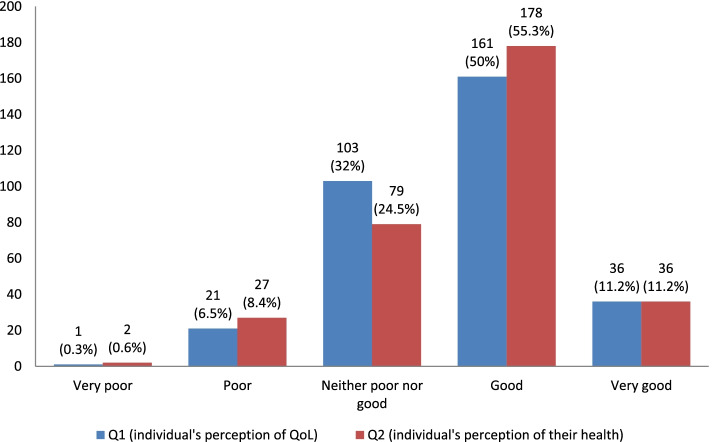
We found the mean score of individual's overall perception of QoL and their health (as assessed by Q1 and Q2, scored in a range of 1 to 5) were 3.65 ± 0.78 and 3.68 ± 0.81, respectively, which were slightly higher than the possible middle score (i.e., 3) (Fig. 1). The mean domain-specific scores of QoL were observed highest in the physical domain (70.91 ± 13.07), followed by social relationships (66.93 ± 15.14), environmental (63.56 ± 12.11), and psychological domain (62.68 ± 14.99) (Table 2).
Fig. 1.
Individual’s overall perception of QoL and health of the study respondents
Table 2.
Overall and domain specific score averages of the survey respondents
| WHOQOL-BREF | Overall mean | SD | |
|---|---|---|---|
| Overall 1 (Q1) | Individual’s overall perception of QoL | 3.65 | 0.78 |
| Overall 2 (Q2) | Individual’s overall perception of their health | 3.68 | 0.81 |
| Domain 1 | Physical | 70.91 | 13.07 |
| Domain 2 | Psychological | 62.68 | 14.99 |
| Domain 3 | Social relationships | 66.93 | 15.14 |
| Domain 4 | Environmental | 63.56 | 12.11 |
We observed a significant difference in the physical and psychological QoL scores among our HCW in different age groups (p = 0.001 and p = 0.0004, respectively) (Table 3). In both domains mean score of QoL deteriorated with the increase of age. We noticed average QoL score of Covid-19 recovered female HCWs was significantly lower than their male counterparts in psychological, social relationships, and environmental domains (p < 0.05). Interestingly, the mean scores of psychological, social relationships and environmental domains of HCWs differed significantly based on their corresponding division. Place of residence was a significant factor in modifying the social relationships domain (p < 0.05), and HCWs from urban areas scored highest in this sector. Respondents with a postgraduate level of education had a better environmental domain score than that of lower educational categories. While single HCW had a better physical and psychological QoL than married and divorced HCW, married respondents had a better social life. However, divorced/widowed HCWs lived the worst quality of life in both scenarios. As expected, study subjects hospitalized due to COVID-19 had a considerably lesser physical and psychological QoL than the home quarantined participants (p < 0.001). We observed proportionate deterioration of QoL scores due to chronic diseases in physical, psychological, and social relationships domains (p < 0.05). We also noticed the individual disease-specific worsening of QoL scores in each domain due to these chronic diseases. The analysis results were provided in the supplementary files (Supplementary 1).
Table 3.
Comparison of individual domains score against socio-demographics variables
| Variables | Physical | Psychological | Social | Environmental |
|---|---|---|---|---|
| Age group | ||||
| < 26 | 76.83 ± 11.72 | 66.88 ± 14.92 | 64.43 ± 15.90 | 60.15 ± 12.76 |
| 26 – 30 | 71.69 ± 13.74 | 65.76 ± 15.72 | 66.67 ± 16.91 | 64.10 ± 12.06 |
| 31 – 35 | 72.01 ± 12.72 | 62.84 ± 13.29 | 66.83 ± 14.10 | 62 ± 12.96 |
| 36 – 40 | 68.47 ± 11.07a | 59.47 ± 13.98 | 66.09 ± 15.07 | 65 ± 12.45 |
| 41 – 45 | 69.35 ± 12.63 | 53.84 ± 14.21abc | 68.57 ± 14.87 | 66.32 ± 12.32 |
| 46 + | 64.6 ± 13.40a | 62.6 ± 14.51 | 68.09 ± 11.65 | 64.29 ± 7.95 |
| p | 0.001 | 0.0004 | 0.832 | 0.206 |
| Gender | ||||
| Male | 72.03 ± 13.69 | 64.9 ± 15.06 | 69.22 ± 15.68 | 65.11 ± 12.86 |
| Female | 69.48 ± 12.14 | 59.87 ± 14.48 | 64.03 ± 13.95 | 61.60 ± 12.83 |
| p | 0.082 | 0.002 | 0.002 | 0.01 |
| Division | ||||
| Barisal | 71.5 ± 10.25 | 60.72 ± 9.01 | 62.5 ± 12.84 | 59.19 ± 11.55 |
| Chattogram | 74.11 ± 14.21 | 67.34 ± 14.87 | 67.77 ± 16.20 | 64.76 ± 10.17 |
| Dhaka | 70.52 ± 13.18 | 60.36 ± 15.77b | 68.46 ± 15.77 | 64.73 ± 12.72 |
| Khulna | 65.2 ± 16.45 | 49.8 ± 27.24 | 46.2 ± 12.13bc | 65 ± 9.57 |
| Mymensingh | 70.61 ± 10.27 | 68.83 ± 14.37 | 62.5 ± 11.56 | 64.11 ± 15.33 |
| Rajshahi | 68.07 ± 7.13 | 62.14 ± 8.02 | 65.64 ± 11.17 | 55.43 ± 6.99 |
| Rangpur | 62.58 ± 15.75 | 70.42 ± 11.31 | 62 ± .9.88 | 57.83 ± 9.34 |
| Sylhet | 70.29 ± 13.53 | 60.41 ± 13.29 | 73.24 ± 11.84d | 66 ± 13.01 |
| p | 0.14 | 0.003 | 0.005 | 0.023 |
| Residence | ||||
| Rural | 73.09 ± 12.72 | 66.73 ± 11.78 | 62.93 ± 16.64 | 63.73 ± 12.93 |
| Urban | 70.64 ± 12.99 | 61.79 ± 15.06 | 68.30 ± 14.89 | 63.83 ± 12.16 |
| Semi-urban | 69.90 ± 14.25 | 64 ± 17.71 | 61.71 ± 13.10 | 61.19 ± 10.51 |
| p | 0.471 | 0.116 | 0.012 | 0.52 |
| Religion | ||||
| Muslim | 71.46 ± 13.27 | 63.75 ± 15.16 | 66.77 ± 15.80 | 63.58 ± 12.46 |
| Non-Muslim | 68.81 ± 12.15 | 58.63 ± 13.72 | 67.52 ± 12.38 | 63.49 ± 10.73 |
| p | 0.14 | 0.013 | 0.719 | 0.958 |
| Educational status | ||||
| Below graduation (SSC/HSC) | 71.00 ± 12.84 | 62.56 ± 15.72 | 65.88 ± 14.66 | 62.60 ± 12.45 |
| Graduation | 70.91 ± 12.46 | 63.35 ± 13.89 | 66.53 ± 15.76 | 62.34 ± 11.71 |
| Post-graduation | 70.73 ± 15.1 | 61.13 ± 16.58 | 69.8 ± 14.14 | 68.45 ± 11.49e |
| p | 0.992 | 0.620 | 0.252 | 0.002 |
| Marital status | ||||
| Single | 75.19 ± 13.23 | 68.44 ± 14.35 | 62.96 ± 12.99 | 63.30 ± 12.08 |
| Married | 70.14 ± 12.79 | 61.77 ± 14.40a | 68.03 ± 15.21a | 63.63 ± 12.13 |
| Others | 50 ± 8.49ab | 18.5 ± 17.68ab | 34.5 ± 13.44ab | 62.5 ± 17.68 |
| p | 0.002 | 0.000 | 0.0006 | 0.975 |
| Income (BDT) | ||||
| < 20,000 | 71.68 ± 12.49 | 63 ± 14.77 | 63.52 ± 16.85 | 61.27 ± 13.80 |
| 20,000–40,000 | 71.22 ± 13.21 | 64.91 ± 13.87 | 65.90 ± 12.80 | 61.28 ± 10.07 |
| 4000–60,000 | 70.45 ± 12.85 | 63.68 ± 13.98 | 68.39 ± 17.95 | 64.54 ± 12.15 |
| 60,000 + | 70.28 ± 13.4 | 62.74 ± 16.52 | 66.84 ± 15.47 | 64.51 ± 12.85 |
| p | 0.920 | 0.77 | 0.393 | 0.158 |
| Hospital admission | ||||
| No | 73.59 ± 13.18 | 66.29 ± 14.45 | 67.97 ± 15.09 | 63.48 ± 12.25 |
| Yes | 67.28 ± 12.04 | 57.81 ± 14.37 | 65.52 ± 15.15 | 63.68 ± 11.96 |
| p | 0.000 | 0.000 | 0.151 | 0.881 |
| Smoking status | ||||
| No | 71.99 ± 13.05 | 63.81 ± 14.34 | 67.83 ± 14.49 | 62.40 ± 11.09 |
| Yes | 68.09 ± 12.33 | 57.9 ± 15.89a | 63.59 ± 15.88 | 67.86 ± 15.25a |
| Past smoker | 66.41 ± 13.64 | 62.82 ± 17.67 | 65.86 ± 19.17 | 65 ± 11.01 |
| p | 0.030 | 0.026 | 0.151 | 0.007 |
| Chronic disease | ||||
| 0 | 73.19 ± 12.25 | 64.45 ± 14.86 | 67.21 ± 14.47 | 62.51 ± 11.46 |
| 1 | 69.62 ± 14.24 | 62.59 ± 13.94 | 69.04 ± 15.49 | 65.21 ± 11.98 |
| 2 | 63.56 ± 9.33a | 54.31 ± 15.36a | 65.31 ± 9.73 | 65.44 ± 8.78 |
| 3 + | 57.75 ± 8.61ab | 51.1 ± 13.38ab | 57.2 ± 20.66ab | 66.8 ± 19.15 |
| p | 0.000 | 0.0001 | 0.018 | 0.188 |
Scores were expressed as mean ± standard deviation (SD)
p-value was determined by one-way ANOVA with Posthoc analysis by Tukey
p-value significant at < 0.05 level in comparison to a) first category, b) second category, c) third category and d) fourth category within a variable. Significant p-values are marked in bold
The results of the domain-specific univariate analysis were portrayed in Table 4, where we tried to detect the individual factors responsible for modifying the quality of life scores among HCWs. Participants living in urban areas enjoyed 2.4 times better socially stable lives (OR: 2.42, 95% CI: 1.18–4.96) but 72% less psychologically healthy (OR: 0.28, 95% CI: 0.10–0.81) than those respondents living in rural areas. HCWs who completed post-graduation degrees enjoyed 3.7 times more environmentally secured lives than HCWs who failed to complete graduation (3.67, 1.33–10.14). Eventually, married HCWs led to 57% less psychologically sound quality of life (0.43, 0.18–0.99) than single HCW. An almost similar trend (0.40, 0.17–0.95) was observed for respondents who earned more than 60,000 BDT per month. On the other hand, we noticed a positive trend among the HCWs in the environmental domain, making more than 40,000 BDT. As expected, participants admitted to hospitals during the infection period were 65% (0.35, 0.21–0.60) less likely to stay psychologically healthy than those who were not. Likewise, smokers were more at risk in terms of psychological (0.30, 0.16–0.56) and social (0.45, 0.24–0.87) quality of life than non-smokers. Notwithstanding, a significant deterioration of the patients' QoL was observed with comorbidities except in the environment domain.
Table 4.
Factors associated with each domain of WHOQOL-BREF among the study participants in univariate logistic regression analysis
| Variables | Physical | Psychological | Social relationships | Environmental | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age group | ||||||||
| < 26 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 26 – 30 | 0.25 | 0.03 – 2.02 | 0.88 | 0.32 – 2.44 | 1.29 | 0.57 – 2.91 | 2.14 | 0.96 – 4.78 |
| 31 – 35 | 0.42 | 0.04 – 3.86 | 0.64 | 0.22 -1.80 | 2.86 | 1.08 – 7.57 | 1.37 | 0.60 – 3.11 |
| 36 – 40 | 0.36 | 0.03 – 3.60 | 0.35 | 0.12 – 1.03 | 1.98 | 0.71 – 5.50 | 3.26 | 1.16 – 9.12 |
| 41 – 45 | 0.29 | 0.03 – 2.93 | 0.21 | 0.07 – 0.61 | 2.74 | 0.86 – 8.75 | 3.84 | 1.23 – 12.00 |
| 46 + | 0.07 | 0.01 – 0.62 | 1.06 | 0.29 – 3.82 | 2.07 | 0.68 – 6.28 | 6.4 | 1.67 – 24.58 |
| Gender | ||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 0.83 | 0.39 – 1.78 | 0.64 | 0.38 – 1.07 | 0.64 | 0.37 – 1.10 | 0.79 | 0.47 – 1.34 |
| Residence | ||||||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Urban | 0.51 | 0.12 – 2.27 | 0.28 | 0.10 – 0.81 | 2.42 | 1.18 – 4.96 | 1.53 | 0.75 – 3.14 |
| Semi-urban | 0.20 | 0.04 – 1.06 | 0.52 | 0.13 – 2.12 | 0.98 | 0.37 – 2.62 | 1.75 | 0.58 – 5.26 |
| Religion | ||||||||
| Muslim | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Non-Muslim | 1.29 | 0.47 – 3.51 | 0.57 | 0.32 – 1.05 | 2.08 | 0.94 – 4.60 | 1.25 | 0.64 -2.45 |
| Educational status | ||||||||
| Below graduation (SSC/HSC) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Graduation | 1.57 | 0.63 – 3.93 | 1.42 | 0.78 – 2.58 | 1.08 | 0.59 – 1.96 | 0.95 | 0.54 – 1.68 |
| Post-graduation | 0.60 | 0.23 – 1.58 | 0.78 | 0.38 – 1.58 | 1.85 | 0.77 – 4.43 | 3.67 | 1.33 – 10.14 |
| Marital status | ||||||||
| Single | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Married | 0.75 | 0.25 – 2.26 | 0.43 | 0.18 – 0.99 | 1.29 | 0.65 – 2.58 | 1.18 | 0.60 – 2.3 |
| Others | 0.08 | 0.003 – 1.45 | 1 | 0 | 1 | 0 | 0.33 | 0.02 – 5.55 |
| Income (BDT) | ||||||||
| < 20,000 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 20,000–40,000 | 0.43 | 0.12 – 1.59 | 1.04 | 0.43 -2.54 | 1.56 | 0.74 – 3.31 | 1.87 | 0.93 – 3.78 |
| 40,000–60,000 | 0.58 | 0.13 – 2.54 | 1 | 0.36 – 2.74 | 1.64 | 0.68 – 3.94 | 2.45 | 1.05 – 5.76 |
| 60,000 + | 0.64 | 0.15 – 2.69 | 0.40 | 0.17 – 0.95 | 1.45 | 0.65 – 3.23 | 2.82 | 1.26 – 6.31 |
| Hospital admission | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.49 | 0.23 – 1.06 | 0.35 | 0.21 – 0.60 | 0.63 | 0.37 – 1.1 | 1.31 | 0.76 – 2.24 |
| Smoking status | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 1.35 | 0.45 – 4.08 | 0.30 | 0.16 – 0.56 | 0.45 | 0.24 – 0.87 | 1.32 | 0.64 – 2.71 |
| Past smoker | 0.63 | 0.17 – 2.31 | 1.03 | 0.33 – 3.18 | 0.69 | 0.24 – 1.99 | 1.39 | 0.45 – 4.26 |
| Chronic disease | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 1 | 0.36 | 0.15 – 0.85 | 0.83 | 0.43 – 1.59 | 1.18 | 0.58 – 2.40 | 1.71 | 0.86 – 3.42 |
| 2 | 0.42 | 0.08 – 2.08 | 0.28 | 0.10 – 0.81 | 1.55 | 0.34 – 7.09 | 2.25 | 0.50 – 10.21 |
| 3 + | 0.24 | 0.07 – 0.84 | 0.12 | 0.04 – 0.32 | 0.15 | 0.06 – 0.39 | 0.60 | 0.23 – 1.57 |
OR (95% CI) shown in bold are statistically significant at p<0.05 level
We performed multivariable logistic regression analysis to analyze each variable against each domain to classify the critical factors related to QoL (Table 5). After adjusting the variables, we found that the participants over 46 years of age enjoyed better psychologically sound (AOR: 23.71, 95% CI: 1.31–430.32) and environmentally secure (AOR: 17.23, 95% CI: 1.88–165.52) life than the respondents aged below 26 years. Psychologically and socially, female HCWs were 74% and 59% less likely (0.24, 0.08–0.67; 0.41, 0.19–0.89) to have a good QoL than male HCWs, respectively. In urban areas, the HCW's chance of living a good-quality social life was 3.37 times higher than the rural participants (3.37, 1.37–8.30), while HCWs living in the semi-urban areas led physically impoverished life (0.07, 0.006–0.86). Besides, graduated HCWs had a 2.46 times greater probability of having a decent psychological (2.46, 1.06–5.68) QoL than those who failed to complete graduation. The participants who were married enjoyed better physical life than those single. The HCWs who earned more than 60,000 BDT monthly enjoyed better-secured lives than the participants who earned less than 20,000 BDT. Hospitalized HCWs were 86% less probability of enjoying a better QoL in the physical domain (0.14, 0.04–0.55) than those who were not. Environmental QoL was more favourable for ex-smokers than non-smokers (15.72, 1.28–192.46). Current smokers had a 76% lower chance (0.24, 0.07–0.85) of maintaining a good psychological QoL than never smoker participants. HCWs with three or more comorbidities had a worse QoL on psychological, social, and environmental measures than those without comorbidity. Finally, for each week since they recovered, people with COVID-19 were more likely to get a better physical quality of life (1.16, 1.035–1.309).
Table 5.
Factors associated with each domain of WHOQOL-BREF among the study participants in multivariable logistic regression analysis
| Variables | Physical | Psychological | Social | Environmental | ||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Age group | ||||||||
| < 26 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 26 – 30 | 0.07 | 0.005 – 1.06 | 0.93 | 0.25 – 3.49 | 0.90 | 0.32 – 2.55 | 1.39 | 0.51 – 3.91 |
| 31 – 35 | 0.07 | 0.004 – 1.23 | 0.81 | 0.18 – 3.64 | 1.25 | 0.36 – 4.26 | 0.87 | 0.29 – 2.63 |
| 36 – 40 | 0.12 | 0.005 – 2.84 | 0.43 | 0.08 – 2.17 | 1.49 | 0.37 – 5.93 | 1.52 | 0.38 – 6.10 |
| 41 – 45 | 0.10 | 0.003 – 3.73 | 0.30 | 0.05 – 1.60 | 1.72 | 0.37 – 7.92 | 2.00 | 0.46 – 8.77 |
| 46 + | 0.05 | 0.002 – 1.10 | 23.71 | 1.31 – 430.32 | 3.99 | 0.64 – 25.07 | 17.23 | 1.88 – 165.52 |
| Gender | ||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 1.15 | 0.34 – 3.87 | 0.24 | 0.08 – 0.67 | 0.41 | 0.19 – 0.89 | 1.04 | 0.52 – 2.08 |
| Residence | ||||||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Urban | 0.82 | 0.08 – 8.28 | 0.26 | 0.06 – 1.15 | 3.37 | 1.37 – 8.30 | 2.22 | 0.90 – 5.49 |
| Semi-urban | 0.07 | 0.006 – 0.86 | 0.25 | 0.04 – 1.64 | 1.05 | 0.32 – 3.43 | 2.54 | 0.69 – 9.38 |
| Religion | ||||||||
| Muslim | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Non-Muslim | 3.19 | 0.47 – 21.55 | 1.44 | 0.52 – 4.01 | 1.52 | 0.56 – 4.12 | 0.72 | 0.30 – 1.72 |
| Educational status | ||||||||
| Below graduation (SSC/HSC) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Graduation | 3.24 | 0.78 – 13.45 | 2.46 | 1.06 – 5.68 | 1.21 | 0.58 – 2.51 | 0.74 | 0.36 – 1.49 |
| Post-graduation | 0.86 | 0.14 – 5.20 | 2.76 | 0.67 – 11.40 | 1.29 | 0.35 – 4.77 | 2.77 | 0.63 – 12.16 |
| Marital status | ||||||||
| Single | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Married | 7.90 | 1.35 – 46.09 | 1.40 | 0.43 – 4.57 | 1.13 | 0.43 – 2.97 | 0.994 | 0.41 – 2.38 |
| Others | 0.28 | 0.004 – 20.42 | 1 | 0 | 1 | 0 | 0.06 | 0.001 – 1.94 |
| Income (BDT) | ||||||||
| < 20,000 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 20,000–40,000 | 0.47 | 0.08 – 2.86 | 1.26 | 0.38 – 4.16 | 1.38 | 0.55 – 3.43 | 1.70 | 0.72 – 3.98 |
| 4000–60,000 | 1.22 | 0.13 – 11.01 | 1.06 | 0.27 – 4.13 | 1.25 | 0.42 – 3.72 | 2.18 | 0.77 – 6.17 |
| 60,000 + | 0.46 | 0.06 – 3.31 | 0.42 | 0.13 – 1.37 | 1.90 | 0.65 – 5.57 | 2.94 | 1.09 – 7.89 |
| Hospital admission | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.14 | 0.04 – 0.55 | 0.46 | 0.20 – 1.03 | 0.66 | 0.32 – 1.37 | 1.39 | 0.68 – 2.86 |
| Smoking status | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 3.90 | 0.57 – 26.86 | 0.24 | 0.07 – 0.85 | 0.53 | 0.18 – 1.55 | 3.06 | 0.90 – 10.38 |
| Past smoker | 6.06 | 0.16 – 225.92 | 1 | 0 | 1.06 | 0.22 – 5.04 | 15.72 | 1.28 – 192.46 |
| Chronic disease | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 1 | 0.39 | 0.09 – 1.63 | 1.32 | 0.45 – 3.84 | 0.83 | 0.33 – 2.10 | 0.88 | 0.35 – 2.25 |
| 2 | 1.14 | 0.06 – 20.58 | 0.40 | 0.05 – 3.14 | 0.59 | 0.09 – 3.81 | 0.25 | 0.36 – 1.72 |
| 3 + | 0.29 | 0.03 – 3.06 | 0.08 | 0.01 – 0.55 | 0.05 | 0.01 – 0.23 | 0.06 | 0.01 – 0.32 |
| Durationa (Weeks) | 1.16 | 1.035—1.309 | 1.05 | 0.962—1.149 | 1.05 | 0.981—1.129 | 1.04 | 0.970—1.115 |
*p < 0.05
athe time (in weeks) passed between confirmation of COVID-19 and the date of interview
AOR (95% CI) shown in bold are statistically significant at p<0.05 level
Discussion
The extraordinary devastation induced by the COVID-19 pandemic has put millions of lives in danger and caused significant disruption to the financial system. Those who become infected with COVID-19 had to go through the most agonizing experiences. HCWs are the most vulnerable groups which render their service in front of the highest possible threat. So, assessing the quality of life of the COVID-19 recovered HCWs was a time-demanding necessity in the current situation.
We observed an improvement in the individuals' overall perception of QoL and their health (Q1 3.65 ± 0.78, Q2 3.68 ± 0.81) after getting recovered from the COVID-19. This positive observation was in harmony with four domains of QoL, where the physical domain scored the highest, shadowed by social relationship, environmental, and psychological domains, respectively. Eventually, the promising scores corresponding to each domain assert the overall improvement of the QoL among the HCWs.
Despite the recovered HCWs presenting with improved QoL, a variation in their domain-specific scores representing QoL was observed. To be specific, they showed significant variation concerning different sociodemographic variables, including age, gender, urban residence, higher educational attainment, marital status, higher income, past smoking and the presence of chronic disease. The findings of the earlier studies performed on the general population are congruent to the current study [16, 18, 28].
We noticed that the chance of having good psychological and environmental scores increased with increasing age when adjusted for other factors. The possible explanation for such findings is that HCWs start their careers later than other professions. Due to the lengthy education system, many HCWs do not begin earning substantial incomes until they are 45 or older, well after most of their peers from other professions [29]. Besides, with the increasing age, they find a balance between their profession and family life which he/she was initially thriving to adjust [30]. According to the medical economics report, the late establishment of the HCWs enabled them to acquire financial stability, freedom, physical safety and security, better accessibility to the wellbeing and social care, a good home environment as well as physical environment, and safe transportation in their later life [29]. As a result, despite their multimorbidity, the economic solvency of these older adults gives them a positive feeling by ruling out their negative esteem.
Our current study found that female HCWs are more vulnerable to observing a substandard psychological and social life than their male counterparts. Females experienced 31% deterioration in their psychological and social quality of life due to gender issues, in line with the previous studies conducted on normal adults of Bangladesh [31]. Furthermore, a study on Chinese HCWs [32] also discovered similar results. This might be because most of our female participants were frontline physicians or nurses who might have contracted SARS-CoV2 while treating patients and were still working for long diligent hours under high risk after recovery [33, 34]. Besides, due to the sudden COVID-19 outbreak, the government engaged junior physicians and nurses with fewer years of work experience, making their duties stressful and psychologically challenging [35–39]. During the SARS pandemic, research steered among HCWs in emergency rooms found that female HCWs were more prone than male HCWs to experience anxiety and behavioural disengagement [38].
Participants living in the urban areas had good social relationships domain scores than the rural participants. According to Shucksmith et al., rural communities led to a substantially poorer quality of life than metropolitan areas [40]. As in other countries [41], availability of modern amenities and treatment, good carrier growth, immediate social support from the surroundings, and a favourable environment might have been determinants of improved social QoL among the COVID-19 recovered urban HCWs [42]. We also found that COVID-19 recovered HCWs, residing in the semi-urban areas were significantly more prone to lead a substandard physical QoL than rural respondents. As our current study was carried out during the initial period of the pandemic, more cases were reported from the urban and semi-urban areas than the rural areas [43]. Our COVID-19 frontlines of semi-urban regions occupied inpatient management with low resources during the COVID-19 pandemic, where the patient surge was tremendous. The earlier study showed that uninterrupted workload could induce burnout among HCWs and diminish QoL [4]. In order to keep up with the ongoing surges in inpatient load, HCWs serving in COVID-19-designated units or hospitals had to deal with a dearth of skilled medical personnel and personal protective equipment, as well as inadequate training in the proper maintenance of PPE [44]. Therefore, these unexpected increases in load without adequate compensation and subsequent COVID-19 infection led to a decreased quality of life among the HCWs of semi-urban areas. The reciprocal relationships between psychological burnout, lack of resting time, and poor quality of life have been reported in HCWs managing the COVID-19 patients [8].
We found that married HCWs who recovered from COVID-19 enjoyed a better physical life than the single respondents. The presence of a person to look after during the COVID affected days might be the possible reason for their quick physical ailment in this particular domain.
A positive relationship was observed in the psychological domain between the QoL scores and the level of education among the study participants. Our findings were in line with the worldwide study conducted by Skevington et al. [45] and the study by Regidor et al. [46] performed on the Spanish population. They both reported that higher educational attainment was the key to acquiring better occupational prospects, unlocking financial stability, positive feelings, opportunities for upgrading skills, and overall a good quality of life. In line with this, we also found that graduate HCWs led 2.5 times better psychological QoL than the least educated group. However, it is plausible that graduate HCWs had more positive feelings of happiness and contentment due to their higher income, which secured a more positive environmental QoL. We can support this assumption because we noticed a positive association between the participants’ financial solvency and their environmental domain of QoL. Higher-income ensured access to better physical safety and security, excellent physical and social care accessibility, finer transportation, pollution, and a noise-free healthier environment. However, those with little education reported the worst health and financial resources and the worst overall quality of life [45].
HCWs admitted into the hospital due to COVID-19 had lower scores in the physical domain of the QoL index after recovery. The persistence of post-COVID-19 symptoms, functional disabilities, slow healing, and posttraumatic mental distress after severe infection might be the reason behind the declining physical quality of life. The persistence of symptoms after recovery was related to the patients’ low physical QoL [47], and impacted mental function [48]. Other studies found that the adverse impact on HCWs was marked compared to others [12].
As expected, we noticed that the active smokers participants were less likely to have a good score in the psychological domain of QoL. However, smoking did not affect catching the coronavirus [49] but was responsible for decreasing their self-esteem by creating negative feelings within themselves. Several studies also reported the negative effect of smoking on deteriorating QoL among the study participants [50–55]. We found that smoking quitters enjoyed a healthier environmental QoL than never smokers. The observed elevated QoL among the ex-smokers might be attributed to their self-determination, impetus from the behavioural change and improved sense of wellbeing. However, there is still the possibility of the unmeasured confounders influencing our analysis.
We observed that almost all of the six non-communicable comorbid diseases, namely HTN, DM, IHD, BA/COPD, CKD, and cancer, were responsible for significantly lower QoL scores in the physical health, psychological, and social relationship, and environmental domains of life among the HCWs. We found that the higher the number of comorbidities, the lower the chance of enjoying a satisfactory quality of life. Previous research conducted on COVID and non-COVID patients corroborates these findings [18, 49, 56–64]. As chronic diseases can exacerbate disease severity, provide a dire prognosis, and increase fatality in COVID-19 patients, the cumulative impact of COVID plus chronic disease might have led to our subjects' lower QoL even after recovery.
Lastly, the physical QoL of the COVID-19 recovered HCWs was found to be improved over time. As the physical domain solely depended on patients' physical wellbeing, the finding was relevant. On the other hand, it was evident from other research that COVID-19 exerted a tremendous negative impact on people's psychological domain [65]. Therefore, the time required to overcome psychological havoc could be a possible area to be explored in outlining a proper management plan for the patients’ early recovery.
The relatively limited number of individuals who gave data can be viewed as a drawback in the generalizability of the results. Future studies should reveal more generalizable findings by gathering data from a larger sample of HCWs. Given that the current study is a cross-sectional research case, longitudinal studies examining the pandemic's long-term impacts are warranted. The gender of the participant was found to have a substantial effect on the social and psychological QoL of the HCWs. Thus, additional gender-based comparative research examining the factors of HCWs' working conditions during the COVID-19 epidemic may better understand the issue.
Conclusions
HCWs' post-COVID QoL was affected by various demographic and socioeconomic determinants, including their age, gender, education, and monthly salary. One or more areas of QoL were significantly impacted when disease severity and the degree of comorbidities were considered. However, all the domains of QoL improved over the period where the physical domain had been found significant. Researchers in national and worldwide communities would surely be interested in our findings, which would lead policymakers in developing particular recuperation and rehabilitation plans, initiatives, and strategies for COVID-19-affected health care workers.
Supplementary Information
Additional file 1: Supplementary 1. Comparison of individual domain score by chronic disease status.
Acknowledgements
We would like to express our sincere thanks and gratitude to the study participants for their patience and cooperation during the telephone interview.
Abbreviations
- ANOVA
Analyzing variance
- AOR
Adjusted odds ratio
- COVID-19
Coronavirus disease 2019
- COPD
Chronic obstructive pulmonary disease
- CKD
Chronic kidney disease
- DM
Diabetes mellitus
- HCWs
Healthcare workers
- HRQoL
Health-related quality of life
- HSC
Higher secondary school certificate
- HTN
Hypertension
- OR
Odds ratio
- PPE
Personal protective equipment
- QoL
Quality of life
- RT-PCR
Reverse Transcription-Polymerase Chain Reaction
- SSC
Secondary School Certificate
- WHO
World health organization
- WHOQOL-BREF
World Health Organization Quality of life questionnaire brief
Authors’ contributions
MUR, MASK, MDHH, MHN and KD conceived and designed framework of this study. MUR, MASK, SKS, SYB, MH, MMAH, and MAH collected data. MASK, MUR, SKS, MMAH, MAH executed the statistical analysis. MUR, SKS, SYB, and MH drafted the manuscript. KD, MDHH, and MHN reviewed the manuscript critically. All authors read and approved the final manuscript.
Funding
Open access funding provided by Mid Sweden University. This research did not receive any funding from any agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Data could be available from Dr Mohammad Delwer Hossain Hawlader (mohammad.hawlader@northsouth.edu)
Declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Review Board (IRB)/Ethical Review Committee (ERC) of North South University (No:2020/OR-NSU/IRB-No.0801). The ethical criteria outlined in the 1964 Declaration of Helsinki and its subsequent revisions and equivalent ethical norms were observed. The ethical criteria outlined in the 1964 Declaration of Helsinki and its subsequent revisions, or equivalent ethical standards, were followed whenever needed. Verbal informed consent was obtained from all study respondents during the phone interview.
Consent for publication
N.A.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206–12. Available from: https://pubmed.ncbi.nlm.nih.gov/15324539 [DOI] [PMC free article] [PubMed]
- 2.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2):e100213. Available from: http://gpsych.bmj.com/content/33/2/e100213.abstract [DOI] [PMC free article] [PubMed]
- 3.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woon LS-C, Mansor NS, Mohamad MA, Teoh SH, Leong Bin Abdullah MFI. Quality of life and its predictive factors among healthcare workers after the end of a movement lockdown: the salient roles of COVID-19 stressors, psychological experience, and social support. Front Psychol. 2021;12:1164. doi: 10.3389/fpsyg.2021.652326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karlsson U, Fraenkel C-J. Covid-19: risks to healthcare workers and their families. BMJ. 2020;371:3944. doi: 10.1136/bmj.m3944. [DOI] [PubMed] [Google Scholar]
- 6.European Centre for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK – eighth update. ECDC Rapid Risk Assesment. 2020 [cited 8 Aug 2021]. 1–39. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-eighth-update-8-april-2020.pdf
- 7.Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID-19: the need for robust data and analysis. Anaesthesia. 2020;75:989–92. doi: 10.1111/anae.15116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stojanov J, Malobabic M, Stanojevic G, Stevic M, Milosevic V, Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int J Soc Psychiatry. 2021;67(2):175–181. doi: 10.1177/0020764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Global Health Workforce Alliance. Progress report on the Kampala Declaration and Agenda for Global Action (Bangladesh). World Health Organization. 2021 [cited 17 June 2021]. Available from: https://www.who.int/workforcealliance/countries/bgd/en/#:~:text=Bangladesh suffers from both a,based on MoHFW HRD 2011)
- 10.Hall VJ, Foulkes S, Charlett A, Atti A, Monk EJM, Simmons R, et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative healthcare workers in England: a large, multicentre, prospective cohort study (SIREN) Lancet (London, England) 2021;397(10283):1459–1469. doi: 10.1016/S0140-6736(21)00675-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sultana M. Covid-19: Fatality among doctors rising again. Dhaka Tribune. 2021 Apr 18; Available from: https://archive.dhakatribune.com/bangladesh/2021/04/18/covid-19-fatality-among-doctors-rising-again
- 12.Ngai JC, Ko FW, Ng SS, To K-W, Tong M, Hui DS. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15(3):543–50. doi: 10.1111/j.1440-1843.2010.01720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ng CK, Chan JWM, Kwan TL, To TS, Chan YH, Ng FYY, et al. Six month radiological and physiological outcomes in severe acute respiratory syndrome (SARS) survivors. Thorax. 2004;59(10):889–891. doi: 10.1136/thx.2004.023762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonanno GA, Ho SMY, Chan JCK, Kwong RSY, Cheung CKY, Wong CPY, et al. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Heal Psychol Off J Div Heal Psychol Am Psychol Assoc. 2008;27(5):659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- 15.Orley J. 1996. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment- Field Trial Version. Geneva. Available from: https://apps.who.int/iris/bitstream/handle/10665/63529/WHOQOL-BREF.pdf
- 16.Chen KY, Li T, Gong FH, Zhang JS, Li XK. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psychiatry. 2020;11(July):1–6. doi: 10.3389/fpsyt.2020.00668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slimani M, Paravlic A, Mbarek F, Bragazzi NL, Tod D. The relationship between physical activity and quality of life during the confinement induced by COVID-19 outbreak: a pilot study in Tunisia. Front Psychol. 2020;11(August):1–5. doi: 10.3389/fpsyg.2020.01882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Heal Res Perspect. 2020;11(5):296–302. doi: 10.24171/j.phrp.2020.11.5.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang F, Yang Z, Wang Y, Zhang W, Lin Y, Zeng L, et al. Health-Related Quality of Life and Influencing Factors of Pediatric Medical Staff During the COVID-19 Outbreak. Front Public Heal. 2020;8. Available from: 10.3389/fpubh.2020.565849 [DOI] [PMC free article] [PubMed]
- 20.Than HM, Nong VM, Nguyen CT, Dong KP, Ngo HT, Doan TT, et al. Mental health and health-related quality-of-life outcomes among frontline health workers during the peak of COVID-19 outbreak in Vietnam: a cross-sectional study. Risk Manag Healthc Policy. 2020;13:2927. doi: 10.2147/RMHP.S280749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suryavanshi N, Kadam A, Dhumal G, Nimkar S, Mave V, Gupta A, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;10(11):e01837. Available from: 10.1002/brb3.1837 [DOI] [PMC free article] [PubMed]
- 22.Xiong L-J, Zhong B-L, Cao X-J, Xiong H-G, Huang M, Ding J, et al. Possible posttraumatic stress disorder in Chinese frontline healthcare workers who survived COVID-19 6 months after the COVID-19 outbreak: prevalence, correlates, and symptoms. Transl Psychiatry. 2021;11(1):374. Available from: 10.1038/s41398-021-01503-7 [DOI] [PMC free article] [PubMed]
- 23.Liao T, Meng D, Xiong L, Wu S, Yang L, Wang S, et al. Long-term effects of COVID-19 on health care workers 1-year post-discharge in Wuhan. Infect Dis Ther. 2022;11(1):145–163. doi: 10.1007/s40121-021-00553-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawlader MDH, Rashid MU, Khan MAS, Ara T, Nabi MH, Haque MMA, et al. Quality of life of COVID-19 recovered patients in Bangladesh. PLoS One. 2021;16(10):e0257421. doi: 10.1371/journal.pone.0257421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Izutsu T, Tsutsumi A, Islam A, Matsuo Y, Yamada HS, Kurita H, et al. Validity and reliability of the Bangla version of WHOQOL-BREF on an adolescent population in Bangladesh. Qual life Res an Int J Qual life Asp Treat care Rehabil. 2005;14(7):1783–1789. doi: 10.1007/s11136-005-1744-z. [DOI] [PubMed] [Google Scholar]
- 27.THE WHOQOL GROUP Development of the World Health Organization WHOQOL-BREF quality of life assessment The WHOQOL Group. Psychol Med. 1998;28(3):551–8. doi: 10.1017/S0033291798006667. [DOI] [PubMed] [Google Scholar]
- 28.Algahtani FD, Hassan S-N, Alsaif B, Zrieq R. Assessment of the quality of life during COVID-19 pandemic: a cross-sectional survey from the kingdom of Saudi Arabia. Int J Environ Res Public Health. 2021;18(3):847. doi: 10.3390/ijerph18030847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sweeney JF. Physician retirement: Why it’s hard for doctors to retire. Med Econ J. 2019;96(4):12. Available from: https://www.medicaleconomics.com/view/physician-retirement-why-its-hard-doctors-retire
- 30.Aymes S. Work-life balance for physicians: The what, the why, and the how. Medical News Today [Internet]. 2020 Sep 22; Available from: https://www.medicalnewstoday.com/articles/physician-burnout-running-on-an-empty-tank
- 31.Tsutsumi A, Izutsu T, Kato S, Islam MA, Yamada HS, Kato H, et al. Reliability and validity of the Bangla version of WHOQOL-BREF in an adult population in Dhaka. Bangladesh Psychiatry Clin Neurosci. 2006;60(4):493–498. doi: 10.1111/j.1440-1819.2006.01537.x. [DOI] [PubMed] [Google Scholar]
- 32.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976–e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li L, Cheng S, Gu J. SARS infection among health care workers in Beijing. China JAMA. 2003;290(20):2662–2663. doi: 10.1001/jama.290.20.2662. [DOI] [PubMed] [Google Scholar]
- 34.Shih F-J, Gau M-L, Kao C-C, Yang C-Y, Lin Y-S, Liao Y-C, et al. Dying and caring on the edge: Taiwan’s surviving nurses’ reflections on taking care of patients with severe acute respiratory syndrome. Appl Nurs Res. 2007;20(4):171–180. doi: 10.1016/j.apnr.2006.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hasan S. Govt to recruit 2,000 more doctors; process ambiguous. The Daily Star. 2020;11. Available from: https://www.thedailystar.net/country/news/govt-recruit-2000-more-doctors-process-ambiguous-1926617
- 36.Chan S. Nurses fighting against severe acute respiratory syndrome (SARS) in Hong Kong. J Nurs Scholarsh. 2003;35(3):209. doi: 10.1111/j.1547-5069.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- 37.Tzeng H-M. Fighting the SARS epidemic in Taiwan: a nursing perspective. JONA J Nurs Adm. 2003;33(11):565–567. doi: 10.1097/00005110-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Wong TW, Yau JKY, Chan CLW, Kwong RSY, Ho SMY, Lau CC, et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med. 2005;12(1):13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Mok E, Chung BPM, Chung JWY, Wong TKS. An exploratory study of nurses suffering from severe acute respiratory syndrome (SARS) Int J Nurs Pract. 2005;11(4):150–160. doi: 10.1111/j.1440-172X.2005.00520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shucksmith M, Cameron S, Merridew T, Pichler F. Urban-rural differences in quality of life across the European union. Reg Stud. 2009;43(10):1275–1289. doi: 10.1080/00343400802378750. [DOI] [Google Scholar]
- 41.Rajbangshi PR, Nambiar D, Choudhury N, Rao KD. Rural recruitment and retention of health workers across cadres and types of contract in north-east India: a qualitative study. WHO South-East Asia J public Heal. 2017;6(2):51–59. doi: 10.4103/2224-3151.213792. [DOI] [PubMed] [Google Scholar]
- 42.Sadiq AS, Ahmed S. Understanding of individual rationality and institutional constraints: the case of deficiency of doctors in rural Bangladesh. J Glob Heal Reports. 2020;4:e2020056. [Google Scholar]
- 43.Directorate General of Health Services (DGHS). Press release COVID-19 from Integrated Control Room of DGHS. DGHS. 2021 [cited 27 June 2021]. Available from: https://corona.gov.bd/press-release
- 44.Hossain MA, Bin Rashid MU, Khan MAS, Sayeed S, Kader MA, Hawlader MDH. Healthcare workers’ knowledge, attitude, and practice regarding personal protective equipment for the prevention of COVID-19. J Multidiscip Healthc. 2021;14:229–38. doi: 10.2147/JMDH.S293717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skevington SM. Qualities of life, educational level and human development: an international investigation of health. Soc Psychiatry Psychiatr Epidemiol. 2010;45(10):999–1009. doi: 10.1007/s00127-009-0138-x. [DOI] [PubMed] [Google Scholar]
- 46.Regidor E, Barrio G, de la Fuente L, Domingo A, Rodriguez C, Alonso J. Association between educational level and health related quality of life in Spanish adults. J Epidemiol Community Heal. 1999;53(2):75–82. doi: 10.1136/jech.53.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taboada M, Moreno E, Cariñena A, Rey T, Pita-Romero R, Leal S, et al. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. Br J Anaesth. 2021;126(3):e110–e113. doi: 10.1016/j.bja.2020.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jacobs LG, Paleoudis EG, Di Bari DL, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020;15(12 December):1–14. doi: 10.1371/journal.pone.0243882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Health Organization (WHO). Smoking and COVID-19. WHO newsroom. 2020 [cited 30 June 2021]. Available from: https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19
- 50.Ahmed MS, Neyaz AN, Aslami A. Health-related quality of life of chronic obstructive pulmonary disease patients: Results from a community based cross-sectional study in Aligarh, Uttar Pradesh. India Lung India. 2016;33(2):148–153. doi: 10.4103/0970-2113.177438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coste J, Quinquis L, D’Almeida S, Audureau E. Smoking and health-related quality of life in the general population Independent relationships and large differences according to patterns and quantity of smoking and to gender. PLoS One. 2014;9(3):e91562. doi: 10.1371/journal.pone.0091562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking: A longitudinal investigation. Arch Gen Psychiatry. 1998;55(2):161–166. doi: 10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- 53.Haukkala A, Uutela A, Vartiainen E, Mcalister A, Knekt P. Depression and smoking cessation: the role of motivation and self-efficacy. Addict Behav. 2000;25(2):311–316. doi: 10.1016/S0306-4603(98)00125-7. [DOI] [PubMed] [Google Scholar]
- 54.Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998;88(10):1518–1522. doi: 10.2105/AJPH.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hurley LL, Taylor RE, Tizabi Y. Positive and negative effects of alcohol and nicotine and their interactions: a mechanistic review. Neurotox Res. 2012;21(1):57–69. doi: 10.1007/s12640-011-9275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Komalasari R, Nurjanah N, Yoche MM. Quality of life of people with cardiovascular disease: a descriptive study. Asian/Pacific Isl Nurs J. 2019;4(2):92–96. doi: 10.31372/20190402.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ferrer M, Alonso J, Morera J, Marrades RM, Khalaf A, Aguar MC, et al. Chronic obstructive pulmonary disease stage and health-related quality of life. The quality of life of chronic obstructive pulmonary disease study group. Ann Intern Med. 1997;127(12):1072–9. doi: 10.7326/0003-4819-127-12-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 58.Arne M, Lundin F, Boman G, Janson C, Janson S, Emtner M. Factors associated with good self-rated health and quality of life in subjects with self-reported COPD. Int J Chron Obstruct Pulmon Dis. 2011;6:511–519. doi: 10.2147/COPD.S24230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jones S, White S, Ormrod J, Sam B, Bull F, Pieh S, et al. Work-based risk factors and quality of life in health care workers providing maternal and newborn care during the Sierra Leone Ebola epidemic: findings using the WHOQOL-BREF and HSE management standards tool. BMJ Open. 2020;10(11):e032929. doi: 10.1136/bmjopen-2019-032929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Oga T. Stages of disease severity and factors that affect the health status of patients with chronic obstructive pulmonary disease. Respir Med. 2000;94(9):841–846. doi: 10.1053/rmed.2000.0804. [DOI] [PubMed] [Google Scholar]
- 61.Islam MZ, Riaz BK, Efa SS, Farjana S, Mahmood F. Health-related quality of life of adult COVID-19 patients following one-month illness experience since diagnosis: findings of a cross-sectional study in Bangladesh. medRxiv. 2021. 10.1101/2021.02.19.21252073. [DOI] [PMC free article] [PubMed]
- 62.Shavro SA, Ezhilarasu P, Augustine J, Bechtel JJ, Christopher DJ. Correlation of health-related quality of life with other disease severity indices in Indian chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2012;7:291–296. doi: 10.2147/COPD.S26405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aschalew AY, Yitayal M, Minyihun A. Health-related quality of life and associated factors among patients with diabetes mellitus at the University of Gondar referral hospital. Health Qual Life Outcomes. 2020;18(1):62. doi: 10.1186/s12955-020-01311-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dehkordi A, Heydarnejad MS, Fatehi D. Quality of life in cancer patients undergoing chemotherapy. Oman Med J. 2009;24(3):204–207. doi: 10.5001/omj.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arora T, Grey I, Östlundh L, Lam KBH, Omar OM, Arnone D. The prevalence of psychological consequences of COVID-19: A systematic review and meta-analysis of observational studies. J Health Psychol. 2022;27(4):805–24. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary 1. Comparison of individual domain score by chronic disease status.
Data Availability Statement
Data could be available from Dr Mohammad Delwer Hossain Hawlader (mohammad.hawlader@northsouth.edu)