Abstract
Background
Following surgery for benign nodular goiter, patients may experience neck and shoulder pain, neck pressure and tightness, choking sensation, altered voice function, and dysphagia leading to decreased short-term quality of life (QoL). This single-blinded randomized controlled trial investigated the effect of post-thyroidectomy rehabilitative neck stretching and movement exercises on these variables including QoL.
Methods
Patients undergoing thyroid lobectomy or total thyroidectomy were randomized to perform neck stretching and movement exercises three times daily in four weeks following surgery (intervention group) or conventional follow-up without exercises (control group). Outcome measures were scores in the following questionnaires: Disease-specific Thyroid-Related Patient-Reported Outcome (ThyPRO-39) involving symptoms of “sense of fullness in the neck,” “pressure in the throat,” and “discomfort swallowing” combined in the multi-item Goiter Symptom Scale, the Voice Handicap-Index-10 (VHI-10), neck and shoulder pain measurement by a numeric rating scale (NRS), and General measure of health (EQ-5D-5L). All scores were assessed prior to surgery and one, two, four weeks, and three months after surgery. Data were analyzed using a linear mixed model.
Results
Eighty-nine patients were included and randomized to the control (n = 45) or the intervention group (n = 44). At three months after surgery, both the control and the intervention group experienced large to moderate improvements in the Goiter symptom and Hyperthyroid symptom scale of the ThyPRO questionnaire (p < 0.004). No significant between-group differences were found in any of the other applied scales.
Conclusions
This study confirms that patients experience profound improvements in QoL after surgery for benign nodular goiter. However, early post-thyroidectomy neck stretching and movement exercises did not result in further QoL improvement, reduction in pain or less impacted subjective voice function for patients primarily undergoing thyroid lobectomy.
Trial Registration Number NCT04645056 (https://clinicaltrials.gov)
Introduction
Benign nodular goiter may result in a range of symptoms, including difficulties in swallowing and neck pressure symptoms [1–4]. Patients undergoing thyroidectomy often experience an improvement in quality of life (QoL) three to six months after surgery [5–7]. However, in the early postoperative phase numerous patients suffer from choking sensation, tightness, and pressure symptoms, discomfort in their neck and shoulders and a restricted laryngeal movement [8–10]. These factors are most likely caused by injury of the skin, extra-laryngeal muscles or nerves, or as a psychological reaction to neck surgery [8–10]. In addition, an altered voice function and impairment of swallowing may occur due to surgical edema, injury to the vocal folds from intubation, recurrent laryngeal nerve (RLN) palsy, or affection of the external branch of the superior laryngeal nerve, or damage to the anterior strap muscles [4, 11, 12]. Such symptoms are often temporary, but nevertheless they may reduce both disease-specific and generic QoL [13, 14].
Stretching exercises reduce muscle pain, improve range of motion, flexibility, functionality, and neuromuscular coordination after various types of surgery, e.g., thoracotomy, mastectomy, and orthopedic surgery, and such patients are routinely offered physiotherapeutic support [15–18]. Moreover, patients with voice dysfunction are treated with neck stretching techniques provided by speech-language-pathologists (SLP) [19, 20].
A few randomized trials, mostly using inadequately validated instruments, showed significantly reduced neck pain, neck stiffness, movement disability, and need for postoperative analgesics by applying neck and shoulder exercises after thyroidectomy [8, 21–23]. However, such measures have not been evaluated by randomized controlled trial employing validated disease-specific QoL instruments appropriate for measuring changes in neck pressure symptoms in patients with goiter. Thus, we aimed to investigate whether postoperative rehabilitative neck stretching exercises have short-term effects on goiter related symptoms, voice function, neck pain, and QoL in patients undergoing surgery due to a benign thyroid nodular disease.
Material and methods
Design and setting
This study was a single-blinded, randomized, controlled trial conducted at a tertiary surgical center. Adults (> 18 years old) undergoing elective thyroid lobectomy (TL) or total thyroidectomy (TT) and with a fine needle biopsy supporting the presence of benign thyroid disease were eligible. Patients were non-eligible in case of (1) recurrent laryngeal nerve (RLN) palsy, (2) current or previous voice disorders requiring treatment by surgery or SLP, or (3) neck or thyroid surgery within the last ten years. Participants were invited to participate two weeks prior to surgery using a secure e-mail system provided by the Danish authorities. Patients were randomized according to the week of surgery using block randomization. Thus, patients who were operated in weeks with even week numbers were allocated to the control group (CTL), while those being operated in weeks with odd numbers were allocated to intervention with physiotherapeutic instructions (INT). The surgical team was blinded to the study and only the physical trainer was aware of the group assignment before surgery. The patients in the CTL group had contact with the physical trainer regarding questionnaires, but were blinded toward the physiotherapeutic intervention in order to avoid any bias caused by not being offered the exercises.
Surgical procedure and intervention
The thyroidectomy was performed under general anesthesia by an experienced surgical team using a standard approach with a Kocher’s skin incision and an intra operative nerve monitoring during surgery [4, 12, 24]. All patients had at least one night stay at the hospital. After total thyroidectomy patients remained in-hospital until a normal and or near normal serum calcium level was ensured, which in most cases lasted one-to-two days after surgery.
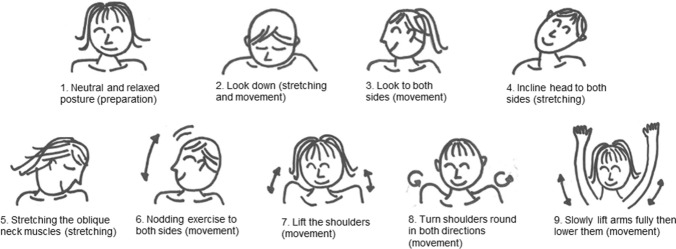
Patients in the INT group initiated the rehabilitation exercises the morning after surgery by instructions from an experienced physical trainer. Nine stretching and movement exercises were performed, with focus on the anterior and posterior neck musculature as well as the muscles around the shoulders. Stretching in the perpendicular direction to the incision was avoided (Fig. 1). One rehabilitation session lasted approximately 10–15 min, and the patient was encouraged to perform the exercises three times a day for a total of four weeks. No further instructions were given except from written information and a video demonstration of the rehabilitation program. For the control group, no information regarding training exercises was provided from nurses or surgeons. The program was developed with inspiration from previous studies and amended by an experienced SLP [8, 21]. The postoperative pain management regime included 1 g of paracetamol four times daily in combination with a non-steroidal anti-inflammatory drug of 400 mg ibuprofen three times daily. Only rarely was morphine used.
Fig. 1.
Illustration of neck stretching and movement exercises for the intervention group. Patients performed five repetitions to each side and a 10 s hold in the stretching exercises
One week after surgery, a telephone follow-up consultation was conducted for all participants by the physical trainer, including questions of the general well-being. For the INT group, the call also addressed the compliance to exercises. No further follow-up was conducted besides electronic questionnaires.
Outcome measures
The primary outcome was QoL and neck symptoms as assessed by the Goiter Symptom scale of the thoroughly validated disease-specific Thyroid-Related Patient-Reported Outcome (ThyPRO) questionnaire, which is currently recommended for evaluating for patients with thyroid disease [25]. The secondary outcomes were subjective voice dysfunction, neck and shoulder pain, and QoL assessed by the generic EuroQol-5-Domain (EQ-5D-5L) QoL questionnaire [7, 26–28]. Data were obtained two weeks prior to surgery, and one, two, four weeks, and three months after surgery through an electronic secure email system. Baseline demographic and surgical information of the participants were collected through hospital records.
Disease-specific QoL was measured by the short form of the ThyPRO containing 39 statements and labeled ThyPRO-39 [26, 29–32]. The ThyPRO questionnaire contains 11 scales, i.e., Goiter Symptom, Hyperthyroid Symptoms, Eye Symptoms, Tiredness, Cognitive Complaints, Anxiety, Depressivity, Emotional Susceptibility, Impaired Social Life, Impaired Daily Life and Appearance. Each statement was rated on a Likert scale from 0 to 4, with 0 point equaling no symptoms and 4 points equaling severe symptoms. The Goiter Symptom scale of the ThyPRO includes three items “sense of fullness in the neck,” “pressure in the throat,” and “discomfort swallowing” relevant for both preoperative and postoperative symptoms from goiter and thyroid surgery.
Subjective voice function was measured by the thoroughly validated Voice-Handicap-Index-10 (VHI-10) focusing on patients’ perception of voice quality [27, 33, 34]. VHI-10 comprises a list of ten statements regarding voice function evaluated by the patient on a five-point Likert scale (0–4 points), with four points indicating the most severe symptoms.
Discomfort and pain were measured using two numeric rating scales (NRS) from 0 to 10 points (0 representing “no pain” and 10 representing “worst pain ever”) in regard to (a) pain in the thyroid bed and (b) muscular pain in neck and shoulders [34].
The generic QoL was measured by the validated EQ-5D-5L questionnaire [7, 28, 35]. It contains a VAS score of the overall health status, ranging from 0 to 100, as well as five dimensions of health including mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, ranging from level 1 to 5 (1 indicating “no problems” and 5 indicating “unable to/extreme problems”) [36]. By including a generic QoL questionnaire, it is possible to compare QoL across different diseases. No change of trial outcomes was done after the trial was commenced.
As the Danish legislation does not require approval of questionnaire studies by the regional ethics committee, no such permission can be applied for or given. The trial was registered on www.ClinicalTrials.gov (NCT04645056).
Statistics
A sample size of 82 patients with 41 in each group was estimated from a five-point between-group difference in the Goiter Symptom score of the ThyPRO questionnaire, using an eight point’s standard deviation and a power of 80% [5, 6, 34, 37, 38].
An unpaired t-test was used to compare data obtained at baseline and at three months follow-up between the INT group and the CTL group. A few scales of ThyPRO needed log-transformation due to non-normality. A linear mixed model was used to analyze the effect of intervention on the ThyPRO scales, using weight of the surgical specimen as an independent dichotomous variable (i.e., above or below median weight). Effect sizes by Cohen were applied to the ThyPRO scores for comparison of values obtained at baseline and at three months. An effect size in the range 0.2–0.5 is considered as a “small effect,” 0.5–0.8 as a “moderate effect,” and a value > 0.8 as a “large effect” [7].
A Bonferroni correction was applied to adjust for multiple comparison. The ThyPRO scales required a p-value < 0.004 to reach significance, while the EQ-5D required a p-value < 0.01. The EQ-5D-5L dimension variables were dichotomized to “no problems” (level 1) and “any problem” (level 2–5) and were analyzed using linear mixed models [36].
All data were collected and stored in the secure database system RedCAP licensed to the Region of Southern Denmark by Vanderbilt University.
Results
Patient characteristics
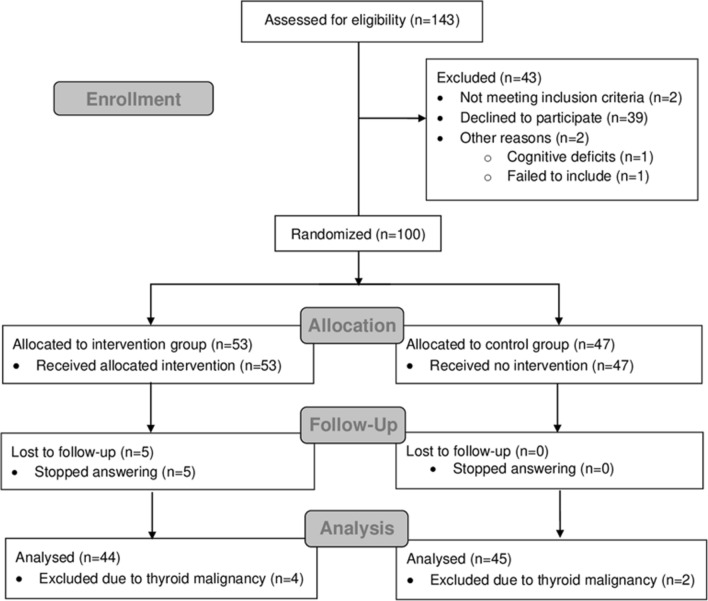
From April 2020 to April 2021, 143 patients were assessed for eligibility. Forty-three patients were excluded (n = 4) or declined to participate (n = 39), leaving 100 patients (response rate: 70%) to be randomly assigned to either INT or CTL (Fig. 2). The final analysis included 89 patients after deducting 11 patients due to either lost to follow-up or a diagnosis of thyroid malignancy, and all analyses were performed with this group of patients (Fig. 2). There was no difference regarding age, sex, or type of surgery between the included patients versus those declining to participate or being lost to follow-up. The majority of included patients were women (74%), and the mean age was 56.6 ± 13.6 years. Twelve patients underwent TT and 77 TL, with a median (range) specimen weight of 44 (6–258) gram, and with no significant difference between the CTL and the INT group. Basic characteristics of control and intervention groups are summarized in Table 1. No important harm or unintended effects were observed in either the CTL or INT groups.
Fig. 2.
CONSORT flowchart of the enrollment, randomization, follow-up, and analysis phase
Table 1.
Sociodemographic, surgical, and thyroid characteristics of participants in control and intervention group
| Cohort characteristics | Control group (n = 45) | Intervention group (n = 44) | p-value | |
|---|---|---|---|---|
| Age | Years, (mean ± SD) | 55.4 ± 12.5 | 57.7 ± 14.7 | 0.44 |
| Sex | Female, n (%) | 31 (69%) | 35 (80%) | 0.32 |
| Male, n (%) | 14 (31%) | 9 (21%) | ||
| Surgery | Total thyroidectomy, n (%) | 5 (11%) | 7 (16%) | 0.44 |
| Hemi-thyroidectomy, n (%) | 40 (89%) | 37 (84%) | ||
| Weight of thyroid specimen | Gram, median (range) | 44 (6–174) | 48 (14–258) | 0.67 |
| RLN paresis/palsy after surgery | (n) | 5 | 2 | 0.48 |
| TSHa | Before surgery (mean ± SD) | 1.2 ± 1.0 | 0.9 ± 0.8 | 0.19 |
| 4-weeks post-surgery (mean ± SD) | 3.6 ± 4.8 | 2.8 ± 2.3 | 0.30 |
aThyroid-stimulating hormone (TSH)
Thyroid-related patient-reported outcome (ThyPRO-39)
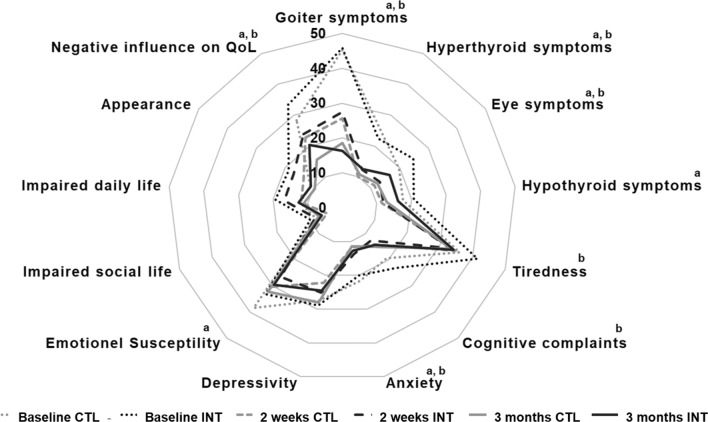
At baseline, no significant difference was observed between INT and CTL group in any of the 13 ThyPRO scales. In both groups, seven of the scales (Goiter-, Hyperthyroid- and Eye Symptoms, Anxiety, Hypothyroid Symptoms (CTL), Emotional Susceptibly (CTL), Tiredness (INT), Cognitive Complaints (INT), and Negative Influence on QoL) were significantly reduced (i.e., improved) three months after thyroidectomy (p < 0.004, Tables 2 and 3). Significant improvements in all the above scales were seen already at two weeks postoperatively (Tables 2 and 3). Comparing the CTL and the INT group, no significant difference was seen in any of the 13 ThyPRO scales during follow-up (Fig. 3).
Table 2.
Results of the ThyPRO QoL questionnaire in the control group
| Control group | Baseline median (range) | 1 week median (range) p-valuea | 2 weeks median (range) p-valuea | 4 weeks median (range) p-valuea | 3 months median (range) p-valuea | Effect sizeb |
|---|---|---|---|---|---|---|
| Goiter symptoms | 42 (0–100) | 33 (0–100) | 25 (0–75) | 21 (0–75) | 17 (0–75) | 1.10 |
| 0.92 | 0.00* | 0.00* | 0.00* | |||
| Hyperthyroid symptoms | 19 (0–75) | 6 (0–69) | 6 (0–63) | 6 (0–63) | 6 (0–75) | 0.73 |
| 0.00* | 0.00* | 0.00* | 0.00* | |||
| Eye symptoms | 8 (0–100) | 0 (0–92) | 0 (0–83) | 0 (0–67) | 8 (0–75) | 0.32 |
| 0.00* | 0.00* | 0.00* | 0.00* | |||
| Hypothyroid symptoms | 13 (0–88) | 6 (0–69) | 6 (0–81) | 6 (0–75) | 6 (0–81) | 0.24 |
| 0.00* | 0.00* | 0.004 | 0.003* | |||
| Tiredness | 33 (0–75) | 42 (0–67) | 33 (17–58) | 33 (8–83) | 33 (8–58) | 0.15 |
| 0.10 | 0.57 | 0.12 | 0.25 | |||
| Cognitive complaints | 8 (0–83) | 17 (0–75) | 8 (0–75) | 8 (0–67) | 8 (0–75) | 0.19 |
| 0.544 | 0.015 | 0.006 | 0.05 | |||
| Anxiety | 17 (0–75) | 8 (0–58) | 0 (0–50) | 0 (0–50) | 8 (0–67) | 0.47 |
| 0.00* | 0.00* | 0.00* | 0.00* | |||
| Depressivity | 25 (0–67) | 25 (0–50) | 25 (0–41) | 25 (0–50) | 25 (0–67) | − 0.05 |
| 0.01 | 0.01 | 0.02 | 0.72 | |||
| Emotional Susceptibility | 33 (0–67) | 33 (8–75) | 25 (0–58) | 33 (0–67) | 33 (17–58) | 0.44 |
| 0.002* | 0.00* | 0.00* | 0.001* | |||
| Impaired social life | 0 (0–50) | 0 (0–42) | 0 (0–33) | 0 (0–25) | 0 (0–42) | 0.08 |
| 0.67 | 0.03 | 0.02 | 0.52 | |||
| Impaired daily life | 0 (0–58) | 17 (0–75) | 8 (0–50) | 8 (0–42) | 0 (0–75) | 0.07 |
| 0.006 | 0.88 | 0.76 | 0.65 | |||
| Appearance | 8 (0–50) | 17 (0–83) | 8 (0–58) | 8 (0–42) | 8 (0–50) | 0.13 |
| 0.003* | 0.19 | 0.76 | 0.42 | |||
| Negative influence on QoL | 25 (0–100) | 25 (0–100) | 25 (0–75) | 0 (0–75) | 0 (0–75) | 0.46 |
| 0.44 | 0.12 | 0.001* | 0.00* |
Results from the disease-specific thyroid-specific patient-reported outcome measure (ThyPRO) of quality of life (QoL) for the control group
Bonforoni adjustments used to correct for multiple testing with significance levels *= p < 0.004.
ap-values represent the statistical significance compared to baseline.
bEffect sizes (ES) compare data from baseline and 3 months postoperatively. According to Cohen [7], ES are divided in small effect = 0.2–0.5, moderate effect = 0.5–0.8 and large effects > 0.8
Table 3.
Results of the ThyPRO QoL questionnaire in the intervention group
| Intervention group | Baseline median (range) | 1 week median (range) p-valuea | 2 weeks median (range) p-valuea | 4 weeks median (range) p-valuea | 3 months median (range) p-valuea | Effect sizeb |
|---|---|---|---|---|---|---|
| Goiter symptoms | 42 (0–100) | 33 (0–92) | 25 (0–92) | 17 (0–100) | 8 (0–75) | 1.02 |
| 0.39 | 0.00* | 0.00* | 0.00* | |||
| Hyperthyroid symptoms | 19 (0–69) | 13 (0–56) | 9 (0–44) | 6 (0–31) | 6 (0–50) | 0.59 |
| 0.00* | 0.00* | 0.00* | 0.00* | |||
| Eye symptoms | 17 (0–100) | 8 (0–58) | 8 (0–58) | 8 (0–83) | 8 (0–67) | 0.33 |
| 0.00* | 0.00* | 0.00* | 0.001* | |||
| Hypothyroid symptoms | 13 (0–100) | 13 (0–63) | 6 (0–56) | 6 (0–56) | 9 (0–75) | 0.21 |
| 0.007 | 0.00* | 0.00* | 0.03 | |||
| Tiredness | 38 (0–75) | 33 (8–67) | 33 (8–67) | 33 (17–67) | 33 (17–75) | 0.39 |
| 0.04 | 0.00* | 0.00* | 0.001* | |||
| Cognitive complaints | 17 (0–100) | 8 (0–83) | 8 (0–67) | 0 (0–75) | 4 (0–83) | 0.32 |
| 0.002* | 0.00* | 0.00* | 0.00* | |||
| Anxiety | 17 (0–75) | 8 (0–75) | 4 (0–58) | 4 (0–75) | 8 (0–67) | 0.33 |
| 0.02 | 0.006 | 0.008 | 0.001* | |||
| Depressivity | 25 (0–67) | 25 (0–50) | 25 (0–67) | 25 (0–67) | 25 (0–58) | 0.27 |
| 0.002* | 0.06 | 0.21 | 0.027 | |||
| Emotional susceptibility | 33 (0–67) | 33 (8–75) | 25 (0–50) | 25 (0–58) | 25 (8–58) | 0.24 |
| 0.00* | 0.001* | 0.04 | 0.07 | |||
| Impaired social life | 0 (0–50) | 0 (0–42) | 0 (0–50) | 0 (0–42) | 0 (0–58) | 0.25 |
| 0.83 | 0.39 | 0.19 | 0.04 | |||
| Impaired daily life | 13 (0–92) | 17 (0–75) | 8 (0–92) | 8 (0–75) | 8 (0–75) | 0.28 |
| 0.60 | 0.37 | 0.08 | 0.02 | |||
| Appearance | 8 (0–92) | 17 (0–83) | 8 (0–67) | 8 (0–92) | 8 (0–100) | 0.36 |
| 0.67 | 0.59 | 0.15 | 0.01 | |||
| Negative influence on QoL | 25 (0–100) | 25 (0–100) | 25 (0–100) | 13 (0–100) | 0 (0–100) | 0.48 |
| 0.06 | 0.009 | 0.00* | 0.00* |
Results from the disease-specific thyroid-specific patient-reported outcome measure (ThyPRO) of quality of life (QoL) for the intervention group
Bonforoni adjustments used to correct for multiple testing with significance levels *= p < 0.004.
ap-values represent the statistical significance compared to baseline.
bEffect sizes (ES) compare data from baseline and 3 months postoperatively. According to Cohen [7], ES are divided in small effect = 0.2–0.5, moderate effect = 0.5–0.8 and large effects > 0.8
Fig. 3.
Radar plots of mean ThyPRO scores comparing baseline, two weeks, and three months data in the control group (n = 44) and the intervention group (n = 45). Large scores indicate more severely affected quality of life. a Baseline vs. two weeks and three months in the control group (p < 0.004)
Regarding effect size [7], two scales (Goiter- and Hyperthyroid Symptoms) showed moderate or large improvement three months after surgery in both the CTL and the INT group (Tables 2 and 3).
Voice-Handicap-Index-10 (VHI-10) and numeric rating scales (NRS)
At baseline, the VHI-10 and NRS were similar in the CTL group and the INT group [VHI-10 median (range) scores: CTL 1(0–22) vs. INT 2(0–29) points; NRS scores: CTL 3(0–14) vs. INT 4(0–16) points]. Compared to baseline, no significant changes were observed in both items at one, two, four weeks and three months after surgery.
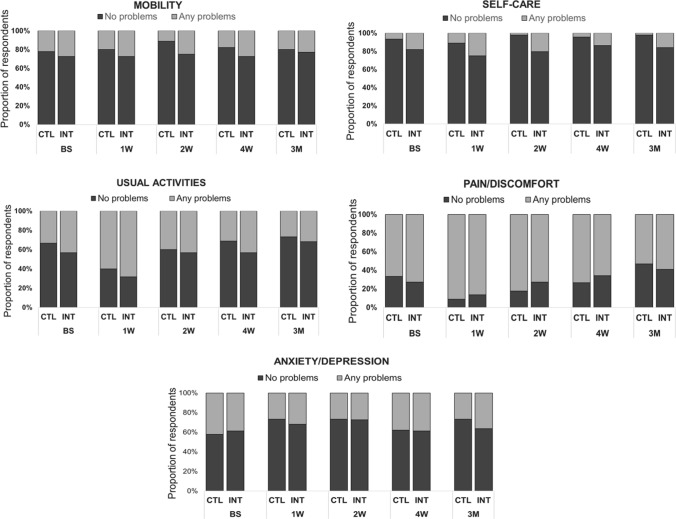
General health, EQ-5D questionnaire
Reflecting an improved general health, the EQ-5D VAS score increased significantly in both groups three months after surgery compared to baseline. No statistically significant difference was seen between groups, neither at baseline nor at three months after surgery (Fig. 4). Additionally, there was no significant difference between groups in any of the five health dimensions during follow-up (Fig. 5). Usual Activities in both groups and Pain/Discomfort in the CTL group showed a significantly worse state in the first week postoperatively (p < 0.01).
Fig. 4.
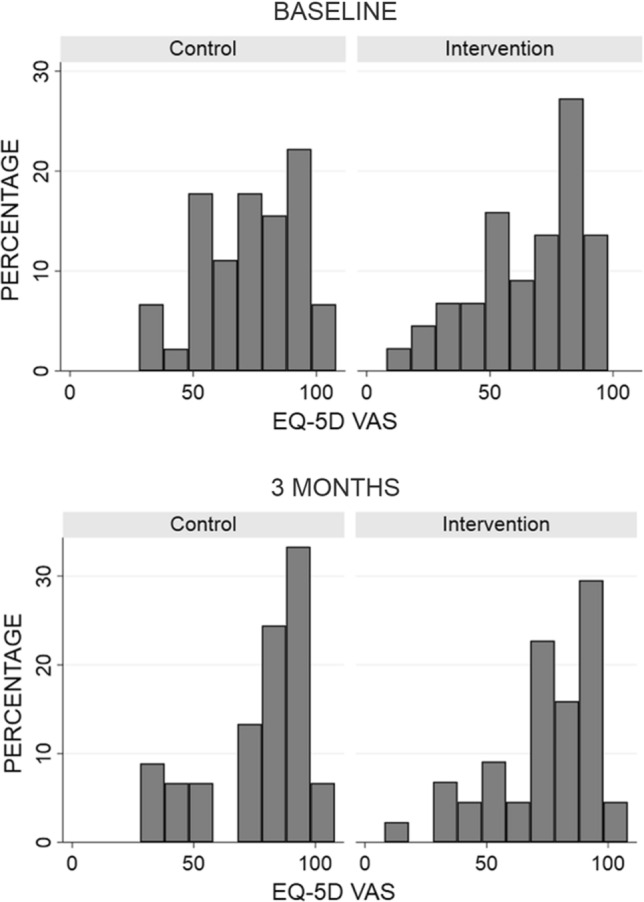
Generic quality of life measured by the instrument EQ-5D-5L. The figure shows the EQ-5D-5L VAS percentage distribution in the control (n = 45) and the intervention group (n = 44), at baseline (top) and at three months (bottom). Low scores indicate a reduced generic quality of life. None of the differences between groups were statistically significant at any point in time (level of significance p)
Fig. 5.
Proportion of responses divided in “no problems” or “any problems” for EQ-5D-5L dimensions at baseline, one week, two weeks, four weeks, and three months for the control group (CTL) (n = 45) and the intervention group (INT) (n = 44). No differences between the groups were statistically significant at any time during the follow-up (level of significance p < 0.05)
Discussion
Using well-validated questionnaires, this randomized single-blinded controlled trial revealed no significant effect of postoperative neck stretching and movement exercises on thyroid-specific-QoL, subjective voice function, neck and shoulder pain or the general subjective health. We assessed these outcomes at one, two, and four weeks, and three months after surgery. Although the intervention seemed to be of no benefit, the study confirmed that thyroid surgery profoundly improves the thyroid-specific-QoL, as measured by the ThyPRO instrument. The improvement was seen within the first two weeks postoperatively and persisted until the last assessment at three months. These findings are well in line with earlier studies of QoL [5, 6, 39].
Previous studies, using other outcome measures, also examined the impact of stretching exercises [8, 21–23]. Takamura et al. [8] found reduced neck discomfort and pain one year after thyroid surgery. In patients with goiter, Abdelmohsen et al. [22] found similar results as early as two weeks post-surgically. In contrast, Jang et al. [23] found no significant effect of early postoperative neck stretching exercises after thyroid surgery. None of these studies [8] used validated instruments. Using a validated questionnaire (Neck Pain and Disability Scale), Ayhan et al. [21] found significantly less “Neck Pain and Disability Score” one week postoperatively among patients who received neck stretching exercises, as compared with a control group. However, no effect was seen thereafter, suggesting only an immediate effect of the postoperative rehabilitation. These four studies were all hampered by either the lack of randomization or use of poorly validated questionnaires [8, 21–23].
In contrast to the present trial, previous studies included patients with thyroid malignancies [8, 21–23]. Such patients are mostly concerned with their malignant disease and may have less focus on minor issues such as neck pain [40] than patients with benign conditions do [41]. Additionally, thyroid malignancy often involves more extensive neck surgery, prolonged anesthesia, which potentially leads to more postoperative pain and other complaints. As only 13% of our patients underwent TT, our results are not directly comparable to previous studies in which the majority of operations were TT [8, 21–23].
As an enhanced patient satisfaction can be achieved by follow-up phone calls [42], it cannot be excluded that the phone call in the post-surgical period per se influenced the QoL among our patients, thereby confounding the effect of intervention. However, by including a control group, which also received a phone call, we tried to eliminate such an effect.
None of the above-mentioned studies examined subjective voice function [8, 21–23], even though stretching exercises can improve laryngeal function and voice-related QoL after thyroidectomy [14]. The lack of any effect of the intervention on the voice function likely reflects that thyroid lobectomy, being the dominant operation in our study, only has little impact on voice function. Further, only very few of our patients encountered a RLN paresis.
In a comparison with the Danish EQ-5D-5L population norms, our patients generally performed worse in all five EQ-5D-5L domains, both preoperatively and three months postoperatively. This may reflect that full recovery had not taken place at this point [43]. This assumption is supported by a previous study, in which no difference was found in the health-related EQ-5D-5L score between the general population and patients 12 months after thyroidectomy [44].
A few limitations of this study should be addressed. First, the trial was initiated in the spring 2020 where the Danish health care system was under pressure by the COVID-19 pandemic. This might have influenced the response rate of 70% negatively. In addition, the patient’s overall QoL may have been negatively affected by the national lockdown and a general concern of COVID-19 infection, which, however, applied to both groups.
In the present study, only one phone call after the operation was made to ensure compliance, whereas previous trials included several follow-up phone calls [21–23]. The less intensive follow-up of our patients could potentially have caused some of them to discontinue their exercises earlier than intended, and this would have attenuated any difference, if present, between the INT group and the CTL group. As the ThyPRO questionnaire is not validated for thyroid malignancies, the study did not include patients with thyroid cancer. Further, the negative outcome of our study cannot be generalized to patients with thyroid malignancies as these patients often have more extensive surgery. Finally, the study lacks long-term data, but we find it unlikely that any effect of intervention should emerge beyond three months following surgery.
We conclude that thyroid surgery profoundly improves QoL in patients with benign nodular goiter. However, as shown in this randomized controlled trial, early postoperative neck stretching and movement exercises did not result in further QoL improvement. Therefore, rehabilitative neck stretching exercises by a physical trainer in the investigated concept may not provide additional benefit for patients undergoing thyroid lobectomy.
Acknowledgements
A special thanks to Speech-and-Language-Pathologist Mette Lund Frank, University of Southern Denmark and Department of ORL Head & Neck Surgery, Odense University Hospital, for the instruction of patients in neck stretching and movement exercises.
Funding
This study was financially supported by a scholarship from University of Southern Denmark.
Declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
The study was performed in accordance with the Helsinki Declaration. According to Danish Law, the study did not require approval from the Research Ethics Committee.
Informed consent
Informed consent was obtained from all participants in this study.
Footnotes
The original online version of this article was revised: The authors' names were corrected.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/23/2022
A Correction to this paper has been published: 10.1007/s00268-022-06646-2
Contributor Information
Rikke Taudal Thorsen, Email: rikke.taudal.thorsen2@rsyd.dk.
Helle Døssing, Email: helle.doessing@rsyd.dk.
Steen Joop Bonnema, Email: steen.bonnema@rsyd.dk.
Thomas Heiberg Brix, Email: thomas.brix@rsyd.dk.
Christian Godballe, Email: christian.godballe@rsyd.dk.
Jesper Roed Sorensen, Email: jesper.roed.sorensen@rsyd.dk.
References
- 1.Carle A, Krejbjerg A, Laurberg P. Epidemiology of nodular goitre. Influence of iodine intake. Best Pract Res Clin Endocrinol Metab. 2014;28:465–479. doi: 10.1016/j.beem.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Sorensen JR, Bonnema SJ, Godballe C, et al. The Impact of goiter and thyroid surgery on goiter related esophageal dysfunction. Syst Rev Front Endocrinol (Lausanne) 2018;9:679. doi: 10.3389/fendo.2018.00679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sorensen JR, Lauridsen JF, Døssing H, et al. Thyroidectomy improves tracheal anatomy and airflow in patients with nodular goiter: a prospective cohort study. Eur Thyroid J. 2017;6:307–314. doi: 10.1159/000480348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sorensen JR, Printz T, Iwarsson J, et al. The impact of post-thyroidectomy paresis on quality of life in patients with nodular thyroid disease. Otolaryngol Head Neck Surg. 2019;161:589–597. doi: 10.1177/0194599819855379. [DOI] [PubMed] [Google Scholar]
- 5.Mishra A, Sabaretnam M, Chand G, et al. Quality of life (QoL) in patients with benign thyroid goiters (pre- and post-thyroidectomy): a prospective study. World J Surg. 2013;37:2322–2329. doi: 10.1007/s00268-013-2133-3. [DOI] [PubMed] [Google Scholar]
- 6.Sorensen JR, Watt T, Cramon P, et al. Quality of life after thyroidectomy in patients with nontoxic nodular goiter: a prospective cohort study. Head Neck. 2017;39:2232–2240. doi: 10.1002/hed.24886. [DOI] [PubMed] [Google Scholar]
- 7.Watt T, Cramon P, Frendl DM, et al. Assessing health-related quality of life in patients with benign non-toxic goitre. Best Pract Res Clin Endocrinol Metab. 2014;28:559–575. doi: 10.1016/j.beem.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Takamura Y, Miyauchi A, Tomoda C, et al. Stretching exercises to reduce symptoms of postoperative neck discomfort after thyroid surgery: prospective randomized study. World J Surg. 2005;29:775–779. doi: 10.1007/s00268-005-7722-3. [DOI] [PubMed] [Google Scholar]
- 9.Lee JS, Kim JP, Ryu JS, et al. Effect of wound massage on neck discomfort and voice changes after thyroidectomy. Surgery. 2018;164:965–971. doi: 10.1016/j.surg.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 10.Lombardi CP, Raffaelli M, De Crea C, et al. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery. 2009;146:1174–1181. doi: 10.1016/j.surg.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Vicente DA, Solomon NP, Avital I, et al. Voice outcomes after total thyroidectomy, partial thyroidectomy, or non-neck surgery using a prospective multifactorial assessment. J Am Coll Surg. 2014;219:152–163. doi: 10.1016/j.jamcollsurg.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 12.Ryu J, Ryu YM, Jung YS, et al. Extent of thyroidectomy affects vocal and throat functions: a prospective observational study of lobectomy versus total thyroidectomy. Surgery. 2013;154:611–620. doi: 10.1016/j.surg.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Lombardi CP, Raffaelli M, D'Alatri L, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006;140:1026–1032. doi: 10.1016/j.surg.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148:S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 15.Reeve J, Stiller K, Nicol K, et al. A postoperative shoulder exercise program improves function and decreases pain following open thoracotomy: a randomised trial. J Physiother. 2010;56:245–252. doi: 10.1016/S1836-9553(10)70007-2. [DOI] [PubMed] [Google Scholar]
- 16.Bonutti PM, Marulanda GA, McGrath MS, et al. Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:194–199. doi: 10.1007/s00167-009-0947-1. [DOI] [PubMed] [Google Scholar]
- 17.Chung C, Lee S, Hwang S, et al. Systematic review of exercise effects on health outcomes in women with breast cancer. Asian Nurs Res (Korean Soc Nurs Sci) 2013;7:149–159. doi: 10.1016/j.anr.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura K, Kodama T, Mukaino Y. Effects of active individual muscle stretching on muscle function. J Phys Ther Sci. 2014;26:341–344. doi: 10.1589/jpts.26.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu V, Wu C-W. Speech therapy after thyroidectomy. Gland Surg. 2017;6:501–509. doi: 10.21037/gs.2017.06.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Logemann JA. Dysphagia: evaluation and treatment. Folia Phoniatr Logop. 1995;47:140–164. doi: 10.1159/000266348. [DOI] [PubMed] [Google Scholar]
- 21.Ayhan H, Tastan S, Iyigün E, et al. The effectiveness of neck stretching exercises following total thyroidectomy on reducing neck pain and disability: a randomized controlled trial. Worldviews Evid Based Nurs. 2016;13:224–231. doi: 10.1111/wvn.12136. [DOI] [PubMed] [Google Scholar]
- 22.Abdelmohsen S, Ahmed N. Effect of teaching patients neck stretching exercises on neck pain and disability following thyroidectomy. J Nurs Educ Pract. 2017;8:107. doi: 10.5430/jnep.v8n1p107. [DOI] [Google Scholar]
- 23.Jang JY, Chang Y-S, Kim E, et al. Early neck exercises to reduce post-thyroidectomy syndrome after uncomplicated thyroid surgery: a prospective randomized study. J Korean Thyroid Assoc. 2014;7:70. doi: 10.11106/jkta.2014.7.1.70. [DOI] [Google Scholar]
- 24.Gal I, Solymosi T, Szabo Z, et al. Minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surg Endosc. 2008;22:2445–2449. doi: 10.1007/s00464-008-9806-2. [DOI] [PubMed] [Google Scholar]
- 25.Wong CK, Lang BH, Lam CL, et al. A systematic review of quality of thyroid-specific health-related quality-of-life instruments recommends ThyPRO for patients with benign thyroid diseases. J Clin Epidemiol. 2016;78:63–72. doi: 10.1016/j.jclinepi.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Watt T, Bjorner JB, Groenvold M, et al. Development of a short version of the thyroid-related patient-reported outcome ThyPRO. Thyroid. 2015;25:1069–1079. doi: 10.1089/thy.2015.0209. [DOI] [PubMed] [Google Scholar]
- 27.Nissen LS, Schultz J, Galili J, et al. Crosscultural Adaption and validation of the danish voice handicap index-10. J Voice. 2021;35:661.e7–e11. doi: 10.1016/j.jvoice.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 28.Stolk E, Ludwig K, Rand K, et al. Overview, update, and lessons learned from the international EQ-5D-5L valuation work: version 2 of the EQ-5D-5L valuation protocol. Value Health. 2019;22:23–30. doi: 10.1016/j.jval.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Watt T, Barbesino G, Bjorner JB, et al. Cross-cultural validity of the thyroid-specific quality-of-life patient-reported outcome measure, ThyPRO. Qual Life Res. 2015;24:769–780. doi: 10.1007/s11136-014-0798-1. [DOI] [PubMed] [Google Scholar]
- 30.Watt T, Hegedus L, Groenvold M, et al. Validity and reliability of the novel thyroid-specific quality of life questionnaire, ThyPRO. Eur J Endocrinol. 2010;162:161–167. doi: 10.1530/EJE-09-0521. [DOI] [PubMed] [Google Scholar]
- 31.Watt T, Bjorner JB, Groenvold M, et al. Establishing construct validity for the thyroid-specific patient reported outcome measure (ThyPRO): an initial examination. Qual Life Res Int J Qual Life Aspects Treat Care Rehabil. 2009;18:483–496. doi: 10.1007/s11136-009-9460-8. [DOI] [PubMed] [Google Scholar]
- 32.Watt T, Groenvold M, Deng N, et al. Confirmatory factor analysis of the thyroid-related quality of life questionnaire ThyPRO. Health Qual Life Outcomes. 2014;12:126. doi: 10.1186/s12955-014-0126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17–24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bukvic BR, Zivaljevic VR, Sipetic SB, et al. Improvement of quality of life in patients with benign goiter after surgical treatment. Langenbeck’s Arch Surg. 2014;399:755–764. doi: 10.1007/s00423-014-1221-7. [DOI] [PubMed] [Google Scholar]
- 35.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Foundation ER (2019) EQ-5D-5L-English-User-Guide
- 37.Zivaljevic VR, Bukvic Bacotic BR, Sipetic SB, et al. Quality of life improvement in patients with Hashimoto thyroiditis and other goiters after surgery: a prospective cohort study. Int J Surg. 2015;21:150–155. doi: 10.1016/j.ijsu.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 38.Torring O, Watt T, Sjolin G, et al. Impaired quality of life after radioiodine therapy compared to antithyroid drugs or surgical treatment for graves' hyperthyroidism: a long-term follow-up with the thyroid-related patient-reported outcome questionnaire and 36-item short form health status survey. Thyroid. 2019;29:322–331. doi: 10.1089/thy.2018.0315. [DOI] [PubMed] [Google Scholar]
- 39.Cramon P, Bonnema SJ, Bjorner JB, et al. Quality of life in patients with benign nontoxic goiter: impact of disease and treatment response, and comparison with the general population. Thyroid. 2015;25:284–291. doi: 10.1089/thy.2014.0433. [DOI] [PubMed] [Google Scholar]
- 40.Abdul-Sater L, Henry M, Majdan A, et al. What Are thyroidectomy patients really concerned about? Otolaryngol Head Neck Surg. 2011;144:685–690. doi: 10.1177/0194599811399556. [DOI] [PubMed] [Google Scholar]
- 41.Bajaj Y, De M, Thompson A. Fine needle aspiration cytology in diagnosis and management of thyroid disease. J Laryngol Otol. 2006;120:467–469. doi: 10.1017/S0022215106000703. [DOI] [PubMed] [Google Scholar]
- 42.Kingery MT, Hoberman A, Baron SL, et al. Day-of-surgery video calls and phone calls increase patient satisfaction with outpatient surgery experience: a randomized controlled trial of postoperative communication modalities. J Bone Joint Surg Am. 2021;103:243–250. doi: 10.2106/JBJS.20.00426. [DOI] [PubMed] [Google Scholar]
- 43.Sørensen J, Davidsen M, Gudex C, et al. Danish EQ-5D population norms. Scand J Public Health. 2009;37:467–474. doi: 10.1177/1403494809105286. [DOI] [PubMed] [Google Scholar]
- 44.Schmitz-Winnenthal FH, Schimmack S, Lawrence B, et al. Quality of life is not influenced by the extent of surgery in patients with benign goiter. Langenbeck’s Arch Surg. 2011;396:1157. doi: 10.1007/s00423-011-0822-7. [DOI] [PubMed] [Google Scholar]