Abstract
This paper studies the contribution of the workplace to the SES-health gradient. Our analysis is based on a unique dataset that tracks various health outcomes and workplace risks among healthcare workers during the first four months of the coronavirus 2019 (COVID-19) pandemic. The setting provides an exceptional opportunity to test for work-related disparities in health, while controlling for confounding determinants of the SES-health gradient. We find that low-SES nurses were systematically more likely to contract COVID-19 as a result of workplace exposure. These differentials existed in all healthcare institutions, but were particularly large in non-hospital settings. In contrast, we find no relationship between SES and nonwork-related infection rates. The differences in workplace infection rates are substantially larger than those implied by standard ‘task-based’ indices of transmission risk, and cannot be attributable to easily identifiable metrics of workplace risk. Together, our results show how subtle differences in work conditions or job duties can substantially contribute to the SES-health gradient.
Keywords: Socioeconomic status, Health inequality, COVID-19
1. Introduction
The positive relationship between socioeconomic status (SES) and health is one of the most well-established findings in social science (see Marmot & Wilkinson, 1999, for a review).1 Yet the sources of the gradient remain poorly understood. In economics, the empirical literature has documented a number of mediating factors in this relationship including differences in health knowledge and risky behavior (Cutler et al., 2011; de Walque, 2007; Grimard & Parent, 2007; Kenkel, 1999), access to healthcare (Currie & Gruber, 1996; Goodman-Bacon, 2018), and environmental conditions both at home and in the workplace (Currie & Stabile, 2003; Evans & Kantrowitz, 1996).2 Nevertheless, it has proven difficult to disentangle their respective contribution to the SES-health gradient, in part, because these various mediators often move in tandem (Cutler et al., 2008; Elo, 2009).
We assess the role of the workplace for the SES-health gradient among a specific population: frontline healthcare workers during the Coronavirus 2019 (COVID-19) pandemic. Our analysis draws on a dataset with information on workplace risks from COVID-19 exposure and worker health outcomes. This setting provides a unique opportunity to test for work-related disparities in health, holding constant all other potential mediators for the SES-health gradient.
Our analysis is based on an administrative dataset of healthcare workers in Montreal, Quebec, during the first four months of the pandemic. Montreal was a major COVID-19 hotspot during the first wave. The city had the highest rates COVID-19 cases in Canada, and had similar case rates to several major northeastern U.S. cities.3 The cross-sectional dataset covers healthcare workers in three different healthcare institutions: hospitals, long-term elder care facilities, and local community health centers. There is detailed information on a range of health-related outcomes, including whether individuals had a COVID-19 contact at work, self-assessed symptoms, and diagnostic test results. There is also detailed information on occupation, age, gender, location of work, and location of residence.
We focus on three narrowly defined occupation categories: Licensed Nurse Practitioners, Registered Nurses, and Nurse Clinicians. These occupations each have similar daily workplace tasks – they are all nurses – but have distinct educational requirements and widely varying pay scales.4 For the sake of clarity, we refer to these three occupations as Low-SES, Mid-SES and High-SES nurses.
We estimate the relative probability of infection across different SES nurses who were or were not exposed to COVID-19 in the workplace. These comparisons are based on workers with similar characteristics (age, gender, and residence ZIP code) who worked in the same 3-digit ZIP code location. The resulting estimates capture how heterogeneity in the SES-health risk gradient varies with underlying workplace conditions, holding constant all non-work drivers of COVID-19 infection. Thus, we are able to isolate the impact of the workplace on the relative risk of COVID-19 infection across different SES workers.
We find that Low-SES nurses were significantly more likely to test positive for COVID-19. This gradient is driven entirely by workplace exposure, and we find no significant difference in infection rates across nurses who were not exposed to COVID-19 in the workplace. The patterns are stable across a number of different specifications including models that control for workplace location fixed effects, suggesting that the observed SES gradient cannot be attributed to differences in underlying infection risk or safety protocols across healthcare facilities.
What explains the SES gradient in workplace-related COVID-19 infection rates? We find no significant differences in testing rates by SES group, suggesting that the results cannot be attributed to different workplace testing policies across the three occupational groups.5 Similarly, we find no clear differences in the levels of workplace risk across SES groups, as measured by either the duration of exposure or the probability of facing a high-risk contact. We also find systematic differences in the magnitude of the SES-infection gradient across different healthcare institutions, with effect sizes that are three times larger in non-hospital settings. These patterns align with documented shortages of personal protective equipment (PPE) and lack of infection control measures in Quebec's non-hospital institutions during the first wave of the pandemic (Rinfret, 2020). Finally, since immigrants and visible minorities were disproportionately employed as Low-SES nurses, our results may also reflect workplace-based racialized mechanisms (i.e., Boateng & Adams, 2016; Boateng et al., 2019), in which discriminatory treatment of minority nurses placed them at a higher risk of a work-related infection. Taken together, our results suggest that the observed SES-infection gradient was most likely driven by a combination of inadequate pandemic preparedness and worker training, as well as subtle differences in specific job responsibilities and working conditions across groups.
Our results complement a number of recent studies that use occupation-based measures of viral transmission risk during the COVID-19 pandemic. These measures have been used to measure the size and characteristics of at-risk populations (Baker et al., 2020; Baylis, L Beauregard, et al., 2020), to evaluate differential economic effects across workers (Beland et al., 2020; Beland et al., 2020), and to guide the policy response (Aum et al., 2020; Chopra et al., 2020). To measure viral transmission risk, researchers typically combine O*NET data that provide detailed information on a range of specific job requirements (such as physical proximity, frequency of face-to-face interactions, etc.) with assessments from health experts on the role of these factors for viral transmission risk (see Baylis, Devereux, et al., 2020; Beauregard et al., 2020). Although the ordering of the O*NET ‘task-based’ measure of infection risk aligns with our estimates of observed workplace infection risk, it drastically understates the disparities in infection risk across occupations that we observe in our sample, and it does not account for the large differences in infection risk across healthcare institutions. Our results show how large disparities in workplace infection risk can arise, even across workers in similar occupations with similar tasks. The findings provide a cautionary note for subjective task-based measures of infection risk, and highlight the critical need for data on incidence of workplace COVID-19 infections across a variety of occupations and industries.
More broadly, our research provides new insights into the drivers of the socioeconomic health gradient. These health disparities have only intensified during the COVID-19 pandemic (Baena-Diez et al., 2020; Chowkwanyun & Reed, 2020; Golestaneh et al., 2020; Kim et al., 2020). Previous research has documented how differences in underlying health conditions (Clay et al., 2019; Clark et al., 2020; CDC COVID-19 Response Team, 2020; Guan et al., 2020), exposure to air pollution (Clay et al., 2018; Wu et al., 2020), reliance on public transportation (Adda, 2016; McLaren, 2020; Medlock et al., 2021), and access to healthcare (Clay et al., 2020; Ji et al., 2020), can all exacerbate socioeconomic health disparities during periods of pandemic. There is also a growing literature showing significant differences across sociodemographic groups in the knowledge about the sources of COVID-19 transmission, trust in public health officials, and behaviors regarding its spread (Alsan et al., 2020; Simonov et al., 2020). Finally, lower SES workers are disproportionately concentrated in occupations with fewer opportunities for remote work (Bartik et al., 2020; Chandra et al., 2020; Dingel & Neiman, 2020), although without direct measures of COVID-19 infection rates across occupations it is impossible to assess how these differences contributed to workplace-related exposure to COVID-19. Our paper provides the first direct evidence on workplace-related COVID-19 infections across occupations. Our results demonstrate how large SES-based health disparities can emerge even in a common workplace environment amongst a subset of healthcare workers who were all trained about the sources of disease transmission.
2. Context
2.1. Nursing in Quebec
In Quebec, the vast majority of nurses are employed in three types of healthcare facilities: hospitals, local community health centers, and long term elder care facilities. Employment in nursing can be broadly classified into three distinct occupations: Licensed Nurses Practitioner (LNP), Registered Nurses (RN), and Nurse Clinicians (NC). These three occupations are all regulated by the provincial government.
The three occupations each have specific educational requirements. LNPs must complete a high school degree and an 1800-h training program. RNs must complete an additional year of education beyond high school and a 2100-h job training program. Meanwhile, NCs must complete a three year bachelor degree in Nursing Science.
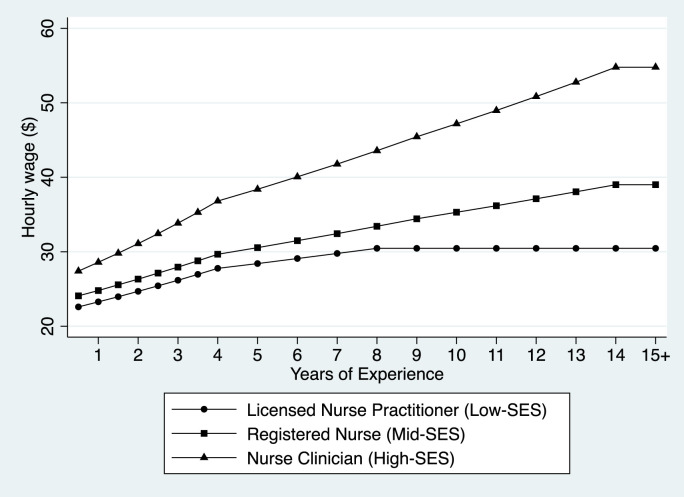
The salary profile also differs widely across the three occupations. Fig. 1 reports the hourly wage scale for the nurses each occupation. This scale is standard for all Quebec nurses who work in the public sector and set by a collective agreement negotiated by the main nurses’ union.6 The hourly wages vary according to years of work experience as well as the specific occupation (LNP, RN, or NC).7 For every level of experience, hourly wages are higher for NPs than RNs than LNPs. These wage differentials are smaller early at lower levels of experience. For example, among workers with less than 5 years of experience, all three occupations earn hourly wages within $10 of each other. The pay gaps increase with experience, so that an NP with at least 14 years of experience earns an hourly wage that is $25 higher than that of an LNP. For reference, the median employment income in Montreal was roughly $36,000 in 2016 (Statistics Canada, 2016), which is less than the annual salary of a full time worker in each of the nursing occupations at any level of experience.8
Fig. 1.
Hourly Wages of Low-SES, Mid-SES and High-SES Nurses
Notes: This figure reports the wage profiles for public sector nurses set by the 2016 FIQ collective agreement. In 2020, roughly 85 percent of Quebec nurses worked in the public sector. The wage profile is based on an 18-level pay scale, that changes every six months during the first four years of employment, and every year thereafter. The reported hourly wages are based on base pay rates that do not account for additional job responsibilities (i.e., team leader, assistant team leader, or instructor). Source:http://www.fiqsante.qc.ca/wp-content/uploads/2016/10/Echelles_salariales_Web_2016-2020_ANG.pdf.
Despite the wide differences in educational requirements and wages, all three occupations have overlapping job descriptions and responsibilities. Workers in each occupation are directly involved in patient care and common daily tasks include monitoring patient vital signs, administering treatments, providing comfort and hygiene to patients, and interacting with patient family members and friends (Avenir Santé Québec, 2020).
In March 2020, the provincial government declared a public health emergency and modified several provisions of healthcare workers' collective agreements.9 The government also authorized an 8 percent pay raise for all frontline healthcare workers. There were widespread accounts of inadequate pandemic preparation, particularly in senior living centers. Indeed, subsequent reporting documented inadequate worker training, an initial lack of PPE in many facilities, and healthcare staff that were heavily psychologically affected by the burden of the crisis (Rinfret, 2020). Frontline healthcare workers were disproportionately likely to contract COVID-19 during the first wave, accounting for 25 percent of all report COVID-19 cases between March 1 and June 15.
2.2. Potential influences of SES on workplace COVID-19 infections
There are a number of potential channels through which occupational status differences across nurses may have influenced the likelihood of a workplace-related COVID-19 infection. First, educational differences across the three nursing occupations may have directly affected workplace infection risk. Educational differences may have influenced workplace COVID-19 infections through tolerance towards risk (Cutler & Lleras-Muney, 2010), adoption of health-promoting behaviors (Link & Phelan, 1995; Phelan et al., 2010), or the ability to effectively cope with stressful environments (Ross & Mirowksky, 2010). Previous research has also documented a link between education and the level of knowledge about illness (Lange, 2011). For this mechanism to operate in our context, however, it must be the case that further medical training (beyond the 1800-h training obtained by all nurses) provides added information about the basic sources of disease transmission.
Second, the wide income disparities across nurses may have contributed to differences in workplace infection risk. There is a large literature documenting the relationship between income and health (see Smith, 1999, for a review).10 In our context, lower SES nurses may have been induced to work longer hours out of financial necessity, placing themselves at greater risk of a workplace COVID-19 contact. It is also possible that higher underlying stress levels among lower income workers may have contributed to infection risk, both directly through a depressed immune system response (e.g., McEwen, 1998a,b), or indirectly through stress-induced behavioral changes in the workplace (e.g., Cooper, 2005; Goldberger & Breznitz, 1993).
Third, differences in job control across occupations may have contributed to workplace infection risk. Researchers have argued that individuals in lower status occupations may experience psychosocial stress due to feelings of subordination and lack of control, which may contribute to a compromised immune system and poor health (Marmot, 2004; Wilkinson, 1999). In addition, workers in lower status occupations often have less control over their hours of work (Schneider & Harknett, 2019). Thus, lower-SES nurses may have been required to take on higher risk shifts. Alternatively, irregular scheduling or frequent overnight shifting may have led this group to be more susceptible to a COVID-19 infection due to workplace error stemming from fatigue.11
Finally, workplace infection rates may have differed across nurses in the three occupational groups as a result of distinct job responsibility and tasks. Although all three occupations share similar daily routines and job duties, it is possible that particular tasks required of lower SES nurses may have placed them at greater risk of infection. For example, they may have spent more time in direct contact with patients or worked in closer proximity to patients.
3. Data
We obtained an administrative dataset from the Human Resources department for nurses who worked in a subset of healthcare facilities in Montreal, Quebec from March 15 to July 1, 2020. These data provide information on all nurses who worked in healthcare facilities located in a particular area in Montreal that spans 16 3-digit ZIP codes. The cross-sectional dataset provides detailed health information on healthcare workers in the three nursing occupations: Licensed Nurses Practitioner (Low-SES), Registered Nurses (Mid-SES), and Nurse Clinicians (High-SES).12 For each worker, we observe whether she had a contact with a COVID-19 positive person in the workplace (either patient or coworker). For workers with a COVID-19 contact, there is information about whether exposure lasted more than 10 min and whether the exposure was deemed to be high-risk.13
We also have information on diagnostic testing of employees. For each worker, we observe whether or not a diagnostic test was conducted and, if so, the results of the test. We use this information to construct various measures of testing: indicators for whether a worker was ever tested and whether the worker ever tested positive. The dataset also provides information on self-assessed COVID-19 symptoms, which were reported by all nurses regardless of testing. We use this information to construct an indicator for whether a worker ever had COVID-19 symptoms.
The dataset contains information on worker demographics and workplace characteristics. We observe the age, gender, and 3-digit ZIP code of home residence for employees. The data also identify 16 distinct 3-digit ZIP code of the primary work location.14 We use the information on workplace ZIP code to construct an indicator variable ‘works in hospital’ that identifies whether a nurse worked in hospital versus non-hospital settings.15
In Table 1 , we report summary statistics across the three categories of nurses: Low-SES, Mid-SES and High-SES. Overall, there are 4,250 individuals in the sample. 24 percent are Low-SES, 39 percent are Mid-SES, and 37 percent are High-SES. The composition of the nursing workforce across occupations in our sample is reflective of the province-wide distribution.16
Table 1.
Summary statistics.
| Outcome |
Mean by Occupational Category |
|||
|---|---|---|---|---|
| All | Low-SES | Mid-SES | High-SES | |
| Panel A: Workplace Exposure to COVID-19 | ||||
| Contact at work | 0.30 | 0.35*** | 0.29 | 0.26* |
| Contact >10 min, if contact at work | 0.74 | 0.75 | 0.72 | |
| High-risk contact, if contact at work | 0.29 | 0.28 | 0.29 | |
| Panel B: COVID-19 Cases and Reported Symptoms | ||||
| Tested positive for COVID-19 | 0.10 | 0.15** | 0.09 | 0.08 |
| Tested positive for COVID-19, if contact at work | 0.27 | 0.37*** | 0.23 | 0.23 |
| Tested positive for COVID-19, if no contact at work | 0.030 | 0.038* | 0.031 | 0.024** |
| Had COVID-19 symptoms | 0.32 | 0.37*** | 0.31 | 0.29 |
| Panel C: Testing for COVID-19 | ||||
| Tested for COVID-19 | 0.37 | 0.43*** | 0.37 | 0.34* |
| Tested for COVID-19, if contact at work | 0.84 | 0.86 | 0.85 | 0.81 |
| Tested for COVID-19, if no contact at work | 0.18 | 0.19 | 0.17 | 0.18 |
| Panel D: Demographic Outcomes | ||||
| Works in hospital | 0.60 | 0.42*** | 0.70 | 0.60** |
| Age | 42.0 | 45.1*** | 41.1 | 40.8 |
| Female | 0.85 | 0.87 | 0.85 | 0.86 |
| Observations | 4,250 | 1,028 | 1,654 | 1,568 |
Notes: This table presents sample means across Low-SES Mid-SES and High-SES workers. We report asterisks for statistically significant differences in means relative to the Mid-SES group. These differences are calculated by pooling all observations and estimating the following regressions: , with standard errors clustered at the workplace ZIP code level. ***, **, * denote significance at the 1%, 5%, and 10% level.
Panel A shows a large and statistically significant SES gradient in workplace exposure, with the highest rates among Low-SES nurses. Conditional on workplace contact, however, the three groups appear to have faced similar levels of risk, as measured by both duration of exposure and whether the contact was deemed high-risk.
Panel B shows that 10 percent of nurses tested positive for COVID-19, substantially higher than the 1 percent city-wide diagnosis rate (SantéMontréal, 2020).17 The high rates of COVID-19 infection are driven by work-related risks. Indeed, the COVID-19 diagnosis rate jumps to 27 percent for nurses with a workplace contact. We also find systematically higher rates of COVID-19 diagnosis among Low-SES workers, particularly among nurses with a workplace contact. Low-SES nurses were 6 percentage points more likely to be diagnosed for COVID-19 and were significantly more likely to report COVID-19 symptoms. The gap in the positive case rate doubles when we restrict attention to nurses with a workplace contact. For nurses without a workplace contact, COVID-19 diagnosis rates were much lower and similar across SES groups.
Panel C shows that 37 percent of nurses were tested for COVID-19 during the sample period.18 COVID-19 tests appear to have been directed to higher risk workers: 84 percent of nurses with a workplace contact received a test. There is a monotonically decreasing relationship between COVID-19 testing rates and occupational ranking: 43 percent of Low-SES workers were tested, 37 percent of Mid-SES workers were tested, and 34 percent of High-SES workers were tested. Nevertheless, these differences appear to be driven by the differing rates of workplace exposure to COVID-19 (reported in Panel A). Among workers who faced a workplace contact, we find no significant differences in testing rates across the three SES groups. Similarly, for nurses who did not face workplace contact, the testing rates are virtually the same across the three occupations.
Panel D shows that the three groups also differed across several socioeconomic outcomes. Low-SES nurses were somewhat older and more likely to work in non-hospital settings. Importantly, in our estimation strategy, we control for both individual characteristics and workplace conditions.
4. Empirical strategy
Our estimation strategy compares health outcomes across nurses of different SES that did or did not have contact with a COVID-19 positive case in the workplace, controlling for demographic characteristics. We estimate the following equation:
| (1) |
where denotes the outcome for nurse , who belongs to one of three groups: Low-SES, Mid-SES, or High-SES (corresponding to the three occupations: Licensed Nurse Practitioner, Registered Nurse, and Nurse Clinician), at the workplace ZIP code, .. The main dependent variable is an indicator for whether or not the worker tested positive for COVID-19. We estimate equation (1) by OLS.19 Standard errors are clustered at the 3-digit ZIP code of the workplace to allow for within-group correlation in outcomes.20
The variables are indicators for Low-SES or High-SES (with Mid-SES left as the omitted reference group).21 is an indicator for whether worker experienced a workplace COVID-19 contact. The term denotes a vector of 16 workplace 3-digit ZIP code fixed effects to allow for differences in workplace risks that might vary across worksites throughout the city. Because these ZIP code fixed effects subsume the indicator for ‘works in hospital’, they should also control for differences in infection risk across hospital versus non-hospital settings.22
The term represents a set of individual covariates. These include an indicator for gender as well as a full vector of age fixed effects to control flexibly for age-based differences in infection risk. We also include a vector of fixed effects for 3-digit ZIP code of residence to allow for differences in infection risk according to non-workplace environmental conditions.
The coefficients and capture SES-based differentials in outcomes among nurses who did not experience a workplace COVID-19 contact. Specifically, identifies the difference in outcomes for non-contact Low-SES workers relative to non-contact Mid-SES workers (the omitted reference group), while captures the difference between non-contact High-SES workers and non-contact Mid-SES workers. Thus, these effects capture the underlying differences in health outcomes across SES groups that were unrelated to workplace risk. Meanwhile, the coefficient identifies the impact of a workplace COVID-19 contact on health outcomes for Mid-SES workers.
The main coefficients of interest, and , identify the extent to which workplace COVID-19 exposure differentially affected outcomes for different SES workers. Specifically, captures the differential impact of workplace exposure on outcomes for Low-SES workers relative to Mid-SES workers (the reference group). Similarly, captures the differential impact of workplace exposure on High-SES workers relative to Mid-SES workers. In many specifications, we partition the sample into just two groups: Low-SES workers versus Mid/High-SES workers, in which case the omitted reference group includes both Mid- and High-SES nurses. In these models, the coefficient captures the differential impact of workplace exposure for Low-SES workers relative to the impact of workplace exposure on Mid/High-SES workers. In all cases, the estimates are based on relative differences across exposed versus non-exposed nurses of different SES status. Thus, the analysis holds constant all nonwork sources of COVID-19 risk, thereby isolating the contribution of the workplace to the health gradient. These differential estimates across nurses with and without a workplace contact control for any cross-occupation differences in underlying susceptibility to COVID-19 infection.23
5. Results
5.1. Differences in workplace COVID-19 infections by SES
Table 2 reports the results from equation (1) for our main estimation, where the dependent variable is an indicator equal to 1 if and only if the person tested positive. Columns (1)–(4) report estimates of overall differences in diagnosis rates across SES groups. Columns (1)–(2) report the results when partition the sample into two groups to compare outcomes for Low-SES workers relative to the omitted category of Mid/High-SES workers. Columns (3)–(4) report the results when we partition the sample into all three occupations, so that we compare both Low- and High-SES workers relative to the omitted category of Mid-SES workers. Across the four specifications, we find that consistently higher rates of COVID-19 diagnosis among Low-SES nurses. Because these models control for workplace ZIP code fixed effects, these differences cannot be attributable to cross institution differences in workplace risk. The findings must reflect either within workplace differences in COVID-19 infection risk or various non-work risks or behavioral differences that are not captured by the demographic covariates.
Table 2.
SES differences in COVID-19 infections and workplace exposure.
| Dependent Variable: Tested Positive for COVID-19 |
||||||||
|---|---|---|---|---|---|---|---|---|
| Differences in COVID-19 Infection Rates by SES |
Differences in COVID-19 Infection Rates by SES and Workplace Exposure |
|||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Low-SES | 0.063** | 0.063** | 0.059** | 0.058** | 0.008 | 0.005 | 0.006 | 0.003 |
| (0.029) | (0.029) | (0.025) | (0.027) | (0.005) | (0.007) | (0.005) | (0.008) | |
| Low-SES Contact at Work | 0.122** | 0.123** | 0.124*** | 0.121** | ||||
| (0.052) | (0.053) | (0.041) | (0.043) | |||||
| High-SES | −0.008 | −0.011* | −0.003 | −0.004 | ||||
| (0.008) | (0.005) | (0.004) | (0.005) | |||||
| High-SES Contact at Work | 0.003 | −0.004 | ||||||
| (0.029) | (0.025) | |||||||
| Contact at Work | 0.204*** | 0.207*** | 0.203*** | 0.208*** | ||||
| (0.011) | (0.013) | (0.006) | (0.005) | |||||
| Workplace ZIP code FEs | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Demographic controls | No | Yes | No | Yes | No | Yes | No | Yes |
| R2 | 0.014 | 0.070 | 0.014 | 0.070 | 0.148 | 0.198 | 0.148 | 0.198 |
| # Clusters | 16 | 16 | 16 | 16 | 16 | 16 | 16 | 16 |
| # Observations | 4,250 | 4,250 | 4,250 | 4,250 | 4,250 | 4,250 | 4,250 | 4,250 |
| Mean Dependent Var. | 0.10 | 0.10 | 0.10 | 0.10 | 0.10 | 0.10 | 0.10 | 0.10 |
Notes: This table reports the results of the OLS regression of a binary variable equal to 1 if and only if the person is tested and positive, on binary variables of interest. Nurses are partitioned into three categories: Low-, Mid- or High-SES. The omitted reference group is Mid/High-SES nurses in columns 1, 2, 5 and 6, and Mid-SES in columns 3, 4, 7 and 8. “Contact at Work” is a binary variable equal to 1 if and only if the person was in contact with an infected person at work (patient or coworker). “Demographic controls” are indicator variables for age, sex, and ZIP code of residency. Observations are clustered at the workplace ZIP code level. ***, **, * denote significance at the 1%, 5%, and 10% level.
Columns (5)–(8) report the results from our main specification that interact occupational status with workplace contact. Columns (5)–(6) report the estimates when we partition into two groups (Low-vs. Mid/High-SES workers), while columns (7)–(8) report the results when we partition into all three occupations. The results demonstrate that the underlying differences in positive test rates across groups were driven entirely by workplace contact. The interaction effects for Low-SES are positive and statistically significant across the various specification, implying that workplace contact differentially increased the probability of testing positive among Low-SES nurses. In contrast, the main effects for Low-SES workers are all small and statistically insignificant, indicating no systematic differences in infection rates among individuals who were not exposed in the workplace. Similarly, we find no significant effects for High-SES nurses regardless of workplace exposure.24
The interaction effects reported in columns (5)–(8) are large in magnitude. Our preferred estimates (col. 6) imply that workplace-related infection rates were 53% (=0.123/0.23) higher for Low-SES nurses relative to the other two groups. The findings are consistent with the underlying differences in workplace-related COVID-19 diagnoses reported in Table 1. Notably, the regression results establish that these differentials persist, even after we account for cross-institution differences in infection risk and individual demographic factors.
One potential explanation for the observed patterns in Table 2 is differential testing rates across SES workers. For example, if Low-SES nurses were more likely to be tested following a workplace contact, the previous estimates could partly reflect lower rates of undiagnosed infection among this group of workers. In practice, decisions over employee testing were made at the institutional level, following the guidelines established by the provincial health authorities. These guidelines made no mention of nurses’ occupational standing, so it is unlikely that testing rates should differ across groups, conditional on underlying workplace risk. Nevertheless, we assess the extent to which group-specific testing policies may be driving the baseline findings.
Table 3 (cols. 1–2) shows no significant difference in the testing rates for Low-SES workers, regardless of workplace contact. The main interaction effects are positive, but small in magnitude, and statistically insignificant. The main results for COVID-19 diagnosis are similar to the baseline findings when we restrict the sample to individuals who received a COVID-19 tests (cols. 3–4). Similarly, we estimate a significant workplace-related SES gradient in the probably of reporting COVID-19 symptoms, regardless of whether a diagnostic test was conducted (cols. 5–6). Taken together, these results strongly suggest that the observed differentials in positive COVID-19 cases across nurses reflect actual differences in the likelihood of workplace-related infections and were not driven by SES-based differences in testing.
Table 3.
SES differences in COVID-19 testing.
|
Dependent Variable: |
Tested for COVID-19 |
COVID-19 positive, if tested = 1 |
Reported COVID-19 symptoms |
|||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Low-SES | 0.009 | 0.006 | 0.042 | 0.045 | −0.001 | −0.006 |
| (0.019) | (0.026) | (0.034) | (0.041) | (0.018) | (0.025) | |
| Low-SES Contact at Work | 0.014 | 0.019 | 0.100** | 0.097** | 0.061* | 0.068** |
| (0.039) | (0.038) | (0.034) | (0.033) | (0.029) | (0.031) | |
| Contact at Work | 0.657*** | 0.653*** | 0.122*** | 0.113*** | 0.542*** | 0.543*** |
| (0.017) | (0.015) | (0.016) | (0.015) | (0.017) | (0.020) | |
| Workplace ZIP code FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Demographic controls | No | Yes | No | Yes | No | Yes |
| Restricted sample to tested workers | Yes | Yes | ||||
| R2 | 0.393 | 0.429 | 0.051 | 0.193 | 0.308 | 0.351 |
| # Clusters | 16 | 16 | 16 | 16 | 16 | 16 |
| # Observations | 4,250 | 4,250 | 1,587 | 1,587 | 4,250 | 4,250 |
| Mean Dependent Var. | 0.37 | 0.37 | 0.27 | 0.27 | 0.32 | 0.32 |
Notes: This table reports the results of the OLS regression of a binary variable equal to 1 if and only if the person is tested (columns 1 and 2), or if and only if the person is tested and positive (columns 3 and 4), or if and only if the person reported COVID-19 symptoms (columns 5 and 6). In columns 3 and 4, the sample is restricted to nurses who were tested. Nurses are partitioned into three categories: Low-, Mid- or High-SES. The omitted reference group is Mid/High-SES nurses. “Contact at Work” is a binary variable equal to 1 if and only if the person was in contact with an infected person at work (patient or coworker). “Demographic controls” are indicator variables for age, sex, and ZIP code of residency. Observations are clustered at the workplace ZIP code level. ***, **, * denote significance at the 1%, 5%, and 10% level.
The absence of SES-based testing differentials is unsurprising, since employee occupational standing did not directly factor into the provincial testing guidelines. Nevertheless, these patterns are striking, given that a primary goal of workplace testing was to identify the maximum number of COVID-19 cases among workforce. According to this objective, tests should be allocated disproportionately to all identifiable group with higher underlying risk of COVID-19 infection. Instead, we find that Low-SES workers had significantly higher rates of workplace-related infection but were no more likely to be tested, suggesting that a reallocation of tests to Low-SES workers may have reduced the rates of undiagnosed infection.
The estimated differences in work-related COVID-19 infections reported in Table 2 are robust to a range of alternative specifications and controls. In Table A2 we report results from models with two-way clustered standard errors to allow for correlation in outcomes within both workplace and home ZIP code address, following the approach of Cameron et al. (2011). Statistical inference is unaffected. In Table A3, we report estimations from a logit model. The estimated odds ratios are similar in sign and significance to our baseline estimates.25 In Table A4 , we assess the sensitivity of the results to different covariates. For reference, column (1) reports the original coefficient estimates (corresponding to Table 2, col. 6), estimated with 10-year age group fixed effects. In columns (2) and (3), we control for a series of week of diagnosis fixed effects to capture potential changes in underlying COVID-19 prevalence over the sample period. We estimate these models for both the full sample (col. 2) and the restricted sample of tested workers (col. 3).26 Controlling for the week of testing does not affect the main estimates of interest.
Table 4.
SES differences in COVID-19 infection risk.
| Duration of Workplace Contact |
High-risk Workplace Contact |
Team Hierarchy |
|||||
|---|---|---|---|---|---|---|---|
| Dependent Variable: |
Contact >10 min |
COVID-19 positive |
High-risk contact |
COVID-19 positive |
COVID-19 positive |
||
| All | If contact = 1 | Include contact duration controls | All | If contact = 1 | Include high-risk contact controls | Include team leader controls | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Low-SES | 0.050*** | −0.019 | 0.006 | 0.018 | 0.001 | 0.005 | 0.006 |
| (0.014) | (0.033) | (0.006) | (0.011) | (0.026) | (0.007) | (0.007) | |
| Low-SES Contact at Work | 0.122** | 0.122** | 0.123** | ||||
| (0.056) | (0.052) | (0.053) | |||||
| Contact >10 min | 0.180*** | ||||||
| (0.021) | |||||||
| High-risk Contact | −0.089*** | ||||||
| (0.020) | |||||||
| Team Leader Contact at Work | 0.014 | ||||||
| (0.013) | |||||||
| Contact at Work | 0.072** | 0.232*** | 0.206*** | ||||
| (0.029) | (0.009) | (0.013) | |||||
| Full controls | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| R2 | 0.069 | 0.195 | 0.217 | 0.075 | 0.180 | 0.203 | 0.198 |
| # Clusters | 16 | 14 | 16 | 16 | 14 | 16 | 16 |
| # Observations | 4,250 | 1,252 | 4,250 | 4,250 | 1,252 | 4,250 | 4,250 |
| Mean Dependent Var. | 0.22 | 0.74 | 0.10 | 0.08 | 0.29 | 0.10 | 0.10 |
Notes: This table reports the results of the OLS regression of a binary variable equal to 1 if and only if the person was in contact for more than 10 min with a COVID-19 positive person at work (columns 1 and 2), if and only if the person is tested and positive (columns 3, 6 and 7), or if and only if the person had a contact classified as high-risk by its workplace (columns 4 and 5). In columns 2 and 5, the sample is restricted to nurses who were in contact with a COVID-19 positive person at work. Nurses are partitioned into two categories: Low-SES or Mid-/High-SES. The omitted reference group is Mid/High-SES nurses. “Contact at Work” is a binary variable equal to 1 if and only if the person was in contact with an infected person at work (patient or coworker). Full controls include workplace ZIP code and demographic controls reported in Table 2. The regression in column 7 also includes Team Leader fixed effects. Observations are clustered at the workplace ZIP code level. ***, **, * denote significance at the 1%, 5%, and 10% level.
Finally, in Table A5 , we explore whether Low-SES workers were more likely to test positive for COVID-19 following a nonwork contact.27 In columns (1) and (2), the estimates on ‘Low-SES Contact outside of work’ are both statistically insignificant, while the main estimates for ‘Low-SES Nurse’ are both positive and significant. Taken together these findings suggest that workplace as opposed to nonwork exposure was the key driver of the higher COVID-19 infection rates among Low-SES nurses.
Table 5.
SES differences in workplace COVID-19 infection risk across healthcare institutions.
|
Dependent Variable: |
COVID-19 positive |
COVID-19 positive, if tested = 1 |
Tested for COVID-19 |
|||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Low-SES Contact at Work Hospital | 0.062*** | 0.068*** | 0.030* | 0.044* | 0.012 | 0.011 |
| (0.011) | (0.013) | (0.016) | (0.023) | (0.017) | (0.016) | |
| Low-SES Contact at Work Non-hospital | 0.155*** | 0.151** | 0.137*** | 0.120** | 0.022 | 0.031 |
| (0.051) | (0.054) | (0.043) | (0.050) | (0.051) | (0.048) | |
| Workplace ZIP code FEs | Yes | Yes | Yes | Yes | Yes | Yes |
| Demographic controls | No | Yes | No | Yes | No | Yes |
| Restricted sample to tested workers | Yes | Yes | ||||
| R2 | 0.150 | 0.200 | 0.055 | 0.197 | 0.393 | 0.430 |
| # Clusters | 16 | 16 | 16 | 16 | 16 | 16 |
| # Observations | 4,250 | 4,250 | 1,587 | 1,587 | 4,250 | 4,250 |
| Mean Dependent Var. | 0.10 | 0.10 | 0.27 | 0.27 | 0.37 | 0.37 |
Notes: This table reports the results of the OLS regression of a binary variable equal to 1 if and only if the person is tested and positive (columns 1 to 4), or if and only if the person is tested (columns 5 and 6). In columns 3 and 4, the sample is restricted to nurses who were tested. Nurses are partitioned into two categories: Low- or Mid-/High-SES. The omitted reference group is Mid/High-SES nurses. “Contact at Work” is a binary variable equal to 1 if and only if the person was in contact with an infected person at work (patient or coworker). “Demographic controls” are indicator variables for age, sex, and ZIP code of residency. All models include double-interactions between Low-SES, hospital and non-hospital dummies as well as the direct effect of Contact at Work. Observations are clustered at the workplace ZIP code level. ***, **, * denote significance at the 1%, 5%, and 10% level.
5.2. Determinants of SES differentials in workplace COVID-19 infections
What explains the higher rates of COVID-19 infection among Low-SES workers? One possibility is that these nurses were given tasks that placed them at higher risk of infection. For example, they may have been more likely to spend longer periods of time caring for COVID-19 positive patients or may have been assigned to patients that posed higher risks to caregivers.
In Table 4, we assess whether different SES workers faced different levels of risk in the workplace. In columns 1–3 we explore whether there were systematic differences in the duration of workplace COVID-19 contact. Overall, Low-SES workers were more likely to experience an extended COVID-19 contact (col. 1). Conditional on contact, however, we find no significant differences in the length of time spent with COVID-positive patients (col. 2). Moreover, the inclusion of a control for contact duration has almost no impact on the main interaction estimates (col. 3). Similarly, we find no evidence that Low-SES workers had higher rates of high-risk workplace contact, and controlling for high-risk contact does not alter the main estimates (cols. 4–6).28
In the final column of Table 4, we assess whether the SES gradient can be attributed to the workplace hierarchy. We estimate a generalized version of equation (1), allowing the effect of workplace exposure to vary according to whether a nurse was the team leader. This framework allows us to test whether team leaders, who were more likely to be Mid- or High-SES nurses, assigned themselves less risky tasks. We estimate a positive (albeit statistically insignificant) interaction effect for team leaders, suggesting that head nurses were somewhat more likely to assign themselves to higher-risk patients. The inclusion of these covariates has little effect on the main interaction terms. These patterns suggest that differences occupational status or control at work are unlikely to be the drivers of the COVID-19 infection gradient.
Taken together, the results in Table 4 show no evidence that Low-SES nurses spent more time with COVID-19 patients, or were assigned to patients at higher risk of transmitting the virus. Instead, the results must reflect more subtle differences in the daily tasks performed by each group that placed some groups at systematically higher risk of infection.
To conclude the analysis, we explore heterogeneity in effects across different healthcare institutions. In Quebec, like many other jurisdictions, there were substantial differences in the effectiveness of the COVID-19 response across different healthcare institutions.29 The outbreak was particularly acute in long term elder living facilities, which accounted for more than 60 percent of province-wide deaths during the first wave. A widely publicized report by the Quebec ombudsman noted that “[long term elder care facilities] were a blind spot in preparing for the pandemic, with efforts massively concentrated on hospitals (Rinfret, 2020).” The report documented that there was a “lack of infection prevention and control culture in [long term elder care facilities]” and that “personal protective equipment was insufficient and unequally distributed.” Motivated by this evidence, we assess the extent to which the SES workplace infection gradient differed across hospital and non-hospital settings.
Table 5 reports the results from regressions that allow the Low-SES interaction effect to differ across hospital and non-hospital healthcare institutions. The estimates for COVID-19 diagnosis are positive and statistically significant in both hospital and non-hospital settings (cols. 1–2), suggesting that the SES gradient existed in both workplace settings. The estimates are more than twice as large in non-hospital institutions. These findings do not appear to have been driven by differential testing policies (cols. 5–6) and the differential effects remain even when we restrict the sample to tested workers (cols. 3–4).30
The fact that the SES-infection gradient is substantially larger in non-hospital settings suggest that something about particular workplaces (as opposed to workers) contributed to the gradient. In contrast, if the SES-gradient reflected pure behavioral differences or risk tolerance across groups (i.e. Cutler & Lleras-Muney, 2010), we would expect the infection risk gradient to be similar across both types of healthcare institutions. Taken together, these findings suggest that the costs of PPE shortages, poor preparedness, and inadequate worker training in many non-hospital healthcare facilities were disproportionately borne by Low-SES workers.
Finally, while our estimates cannot be attributed to higher underlying infection rates among minority populations, they may reflect unequal treatment of minority nurses within the workplace.31 Indeed, recent evidence suggests that minority nurses in Canada face higher rates of discriminatory treatment in the workplace (Boateng & Adams, 2016; Boateng et al., 2019). In our context, the higher rates of workplace COVID-19 infection among Low-SES workers could partly reflect differential treatment of minority nurses that may have manifested through either task-based discrimination, more stressful workplace interactions, or inadequate safety training. Unfortunately, without information on race or immigrant status, we are unable to explore this potential mechanism. Understanding the role of workplace discrimination on worker health disparities may be an useful avenue for future research.
6. Assessing the risks of COVID-19 transmission in the workplace
Policymakers in many countries have implemented partial lockdowns in which many businesses have been required to shut down or transition to home-based work to reduce the spread of the COVID-19 pandemic. These decisions have been highly controversial, and there has been considerable debate on both the scope of workplace shutdowns and which industries should be targeted. One reason for the controversy is the large uncertainty regarding the actual risks of workplace infection and how these risks vary across occupations.
In an effort to address these concerns, researchers have developed tools to assess the relative risk of workplace infection as a function of the specific daily tasks involved with various jobs. These models combine detailed data on specific job characteristics and tasks from the O*NET dataset with assessments from health experts on the associated risks of viral transmission. For example, a job that requires daily face-to-face discussions would be classified as higher risk than one that requires only weekly interactions. The vector of these various job attributes can then be combined to construct an index of viral transmission risk at the industry/occupation level. These tools have gained influence and have been applied in a number of studies.
A challenge for the ‘task-based’ approach to measuring workplace transmission risk is that the various indices have not been validated with actual COVID-19 infection rates. As a result, we do not know the extent to which the risks of transmission identified by public health experts align with actual rates of transmission. This concern is particularly relevant for the current pandemic, in which knowledge of sources of transmission continues to evolve.
We compare our estimates of relative transmission risk across licensed practitioner nurses and registered nurses to those implied by a standard occupational ‘task-based’ index (Baylis, Devereux, et al., 2020).32 We corroborate the ranking of these occupational groups: licensed practical nurses face higher risk of COVID-19 infection according to the ‘task-based’ index. Nevertheless, the magnitude of the differences in risk do not align. Our preferred estimates imply that the former group had a 50 percent higher risk of workplace-related infection. In contrast, the gap in infection risk on the 100 point ‘task-based’ index is 4 points, less than one third of the cross-occupation standard deviation in risk. Combining our estimated differences in infection risk with the occupation/industry risk index, we calculate that an implausible 98 percent of jobs carry zero risk of transmission risk.33 We also find that the occupational differences in workplace infection risk were three times higher in non-hospital settings that were not identifiable in occupational-based indices.
There are several limitations to these cross-occupation comparisons. They are calculated for just three occupations, and are made based infection rate estimates from a single city that was hit particularly hard during the first wave. Nevertheless, the wide discrepancies we uncover may provide a note of caution in the interpretation of ‘task-based’ occupational measures of transmission risk. There may be subtle differences across occupations that are not easily quantified but that may importantly impact transmission risk. Moreover, our finding that the SES gradient differs substantially across different institutions highlights the crucial role of specific worksite conditions for disease spread. Our results demonstrate the critical need for data on actual COVID-19 infection rates across a broader set of workers to better understand how workplace conditions contribute to disease transmission.
7. Conclusion
The positive relationship between socioeconomic status and health has been extensively documented. Many national governments have set ambitious targets to reduce these “health inequalities” (WHO, 2008; U.S. Dept. of Health and Human Services, 2010). although the effectiveness of government efforts will hinge on successfully identifying and addressing the underlying causes of the gradient.
Our study provides new evidence on the sources of health disparities among frontline healthcare workers during the COVID-19 pandemic. We find that large SES-based differences in COVID-19 infection rates. This gradient was driven entirely by work-related contact, and we find no differences infection rates among individuals who were not exposed to COVID-19 in the workplace.
We uncover wide differences in work-related COVID-19 infections, even among individuals within narrowly defined occupational categories who worked in the same healthcare institution. These differences are not easily captured by standard measures of workplace risk or ‘task-based’ indices of disease transmission. Instead, our results show how subtle differences in workplace conditions and job tasks can interact to generate large SES health disparities.
A defining feature of the coronavirus pandemic is its unequal burden across different socioeconomic groups. Our analysis highlights the critical role that the workplace can play for these health disparities. Future research might explore more deeply the underlying drivers of these workplace health disparities, and the extent to which they can be counteracted through targeted policy interventions. From a policy perspective, this analysis could shed light on how best to mitigate the pandemic's impact among lower status workers, and also offer potentially valuable insights into the drivers of “health inequalities” in more normal times.
Declaration of competing interest
None.
Acknowledgements
We thank Marcella Alsan, Gustavo Bobonis, Abel Brodeur, Fabian Lange, Mark Stabile, and seminar participants at Université de Montréal for valuable comments and suggestions. The authors acknowledge financial support from the Social Sciences and Research Council of Canada, Grant #430-2017-00307. Data can be obtained through an application process to the CIUSSS and the CISSS for the Greater Montreal Area.
Footnotes
The relationship holds across numerous health outcomes and risk factors, and has been observed in many countries and time periods (Cutler & Lleras-Muney, 2010; Link & Phelan, 1995).
Social scientists have also sought to understand the relative influence of various components of social class for health (Elo, 2009). While much of the literature has focused on the importance of education for health (Cutler & Lleras-Muney, 2010; Ross & Mirowksky, 2010; Schnittker, 2004), some scholars have argued that differences in income (McDonough et al., 1999; Wilkinson, 1990) and occupational standing (Marmot, 2004; Marmot et al., 1991; Marmot et al., 1987) are key determinants of the SES-gradient. See Section 2.2. for a discussion.
By July 1, the total number of diagnosed COVID-19 cases per 1,000 residents was 16 in Montreal, comparable to the rates in Baltimore (13), Washington D.C. (15), Philadelphia (17), and Boston (20), although lower than those in New York City (27) (Santé Montréal, 2020; Maryland Dept. of Health, 2020; Government of the District of Columbia, 2020; Philadelphia Dept. of Public Health, 2020; Massachusetts Dept. of Public Health, 2020; NY State Dept. of Health, 2020).
For example, among nurses with at least 14 years of experience, the hourly wage gap between Nurse Clinicians and Licensed Nurse Practitioners is 80 percent (FIQ, 2020).
The decision to test an employee was made at the institutional level following guidelines provided by the Institut National de Santé Publique du Québec (INSPQ). Occupation did not factor directly into this determination.
In Quebec, 95 percent of nurses are unionized, and almost all are represented by the Fédération Interprofessionnelle de la Santé de Québec (FIQ). Roughly 85 percent work in the public sector. The salaries for nurses in the private sector may differ depending on the individual employer.
The wage may also vary depending on an individual's license status (candidate for license, full license, or refresher period) as well as any additional job responsibility (i.e., team leader, assistant to team leader, or instructor).
The demographics of the nursing workforce also differ from the general population. In particular, women are far more likely to be employed in nursing (in our sample 85 percent of nurses are women). It has been documented that the share of minorities among nurses in Canada is larger than the share in the general population (Turcotte & Savage, 2020).
Modifications included the cancellation of vacations, allowances for extensions in work hours, and restrictions placed on job transfers.
A key challenge in establishing this link stems from the fact that low-income individuals may have other attributes that contribute to poor health. Nevertheless, evidence from large increases in the Earned Income Tax Credit shows positive effects on health as well as reduced stress among mothers (Evans & Garthwaite, 2014; Hoynes et al., 2015). The positive relationship between household income and health has also been documented in Canada, despite the existence of universal health insurance coverage for doctor and hospital services (Curtis et al., 2001).
Importantly, because our empirical analysis is based on comparisons across nurses who all experienced a workplace COVID-19 exposure, we are able to control for this type of difference in underlying workplace.
The dataset also information on orderlies. There is some information on doctors in these institutions, although most are classified as self-employed and not administered by the same Human Resources department.
The ‘high-risk’ classification was made at the discretion of hospital administrators based on a variety of factors including proximity to the COVID-19 positive individual, the use of PPE, and duration of contact.
The dataset does not report information on the specific institution of employment. On average there are four healthcare facilities by ZIP code.
All hospitals are located within a single ZIP code. Based on independent information on the workforce of these hospitals, we know that more than 95 percent of nurses associated with that ZIP code worked in a hospital. The indicator ‘works in hospital’ takes a value of one for nurses in that ZIP code and zero for nurses employed in the other 15 workplace ZIP codes.
Data on the total number of Licensed Nurse Practitioners (Low-SES) and Registered Nurses (Mid-SES) across Quebec align exactly with their relative shares in our sample (CIHI, 2021).
These disparities may reflect a combination of both the higher risk of infection among healthcare workers (Wu & McGoogan, 2020), and the high rates of testing that lowered the probability of undiagnosed infection (Benatia et al., 2020a,b).
In comparison, just 7 percent of the general population in the population had been tested by the end of the sample period (INSPQ, 2020).
In comparison to other models for limited dependent variables (i.e., probit or logit), the linear probability model does not impose any functional form assumption on the error terms, and the regression coefficient can be directly interpreted as marginal impacts without requiring any adjustments to the point estimates (Angrist & Pischke, 2009). In additional robustness analysis, we also report results from logit models.
We also estimate two-way clustered standard errors that allow for correlation within both workplace and home ZIP code addresses, following the approach of Cameron et al. (2011).
In many specifications, we partition the sample into two groups: Low-SES versus Mid/High-SES nurses, in which case the omitted reference group are Mid/High-SES nurses.
Because we lack information on specific institution of employment, we also cannot control for differences in workplace risks across long term elder care facilities and community-health centers.
For example, if individuals with underlying health conditions were more likely to select into the lowest tier occupations, we might expect them to experience higher overall rates of COVID-19 infection. Nevertheless, these health conditions should similarly impact the likelihood of COVID-19 infection in both workplace and non-workplace settings, so that we would not expect any systematic differences in the workplace-related infection gradient. A similar argument applies for any other demographic factors, such as race or immigration status, that might influence underlying susceptibility to infection.
Table A1 reports the corresponding estimates to Table 2, in which we report the coefficients for the demographic covariates. For ease of presentation, we have replaced the full vector of age fixed effects with 10-year age group fixed effects. The main estimates are unaffected by this change.
The magnitude of the log-odds estimates are not directly comparable to the marginal impacts reported in Table 2. We report the marginal effects from the logit model at the bottom of Table A3. For the full sample, the logit marginal effects are smaller than the OLS estimates, as often occurs when the mean of the dependent variable is small (Angrist & Pischke, 2009). Indeed, if we restrict the sample to people who are tested, as reported in the last two columns of Table A3, the logit marginal effects are similar to the corresponding OLS estimates (columns 3–4 of Table 3).
In column 2, we add an additional covariate for whether the individual was ever tested, so that nurses who were never tested (and thus cannot be assigned a testing date) are also included in the sample.
Nurses were required to disclose all known COVID-19 contacts, although there was likely considerable measurement error in the nonwork contact variable.
The negative direct effect of ‘High-risk Contact’ is likely a result of differential testing rates among workers whose exposure was deemed ‘high-risk’ (results available upon request). Differences in COVID-19 diagnosis rates across workers with high- and low-risk contacts reflect both average COVID-19 infection rates and differences in testing rates across each group. To the extent that the positivity rate decreases with the fraction of the population tested, this second selection effect may dominate.
For details on PPE shortages in U.S. elder care facilities see Murray (2020); Holroyd-Leduc and Laupacis (2020).
In these regressions, we are unable to identify the main effect of workplace exposure on COVID-19 diagnosis, since overall testing rates differed across hospital and non-hospital institutions.
In Canada, immigrant and non-white workers are disproportionately employed as Low-SES nurses (Statistics Canada, 2016). The findings cannot be driven by higher COVID-19 infection rates among minority populations, since our estimation strategy – based on relative infection rates across workplace and non-workplace settings – controls for the selection of workers with different underlying infection risk across occupations (see Section 4). We also find no differences in non-work related infections across SES categories.
Nurse clinicians were not separately identified in the O*NET data.
This large share is due to the implied steep decline in COVID-19 infection rates for jobs that had lower rankings on the index.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ssmph.2022.101124.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Adda J. Economic activity and the spread of viral diseases: Evidence from high frequency data. Quarterly Journal of Economics. 2016;131(2):891–941. [Google Scholar]
- Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Network Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angrist J., Pischke J. Princeton University Press; Princeton: 2009. Mostly harmless econometrics: An empiricist's companion. [Google Scholar]
- Aum S., Lee S.Y., Shin Y. 2020. Who should work from home during a pandemic? The wage-infection trade-off. NBER Working Paper #27908. [Google Scholar]
- Avenir Santé Québec 2020. http://avenirensante.gouv.qc.ca/en/carrieres
- Baena-Diez J., Barroso M., Cordeiro-Coelho S., Diaz J., Grau M. Impact of COVID-19 outbreak by income: Hitting hardest most deprived. Journal of Public Health. 2020;42(4):698–703. doi: 10.1093/pubmed/fdaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker M., Peckman T., Seixas N. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS One. 2020:489–493. doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartik A., Cullen Z., Glaeser E., Luca M., Stanton C. 2020. What jobs are being done at home during the COVID-19 crisis? Evidence from firm-level surveys. NBER Working Paper #27422. [Google Scholar]
- Baylis P., Devereux M., Fortin N., Gallipoli G., Green D.A., Cubillos P., Gyetvay S., Karimirad A., Lemieux T., Mukherji R., Simard-Duplain G., Siu H., Warman C. 2020. VSE COVID risk/reward assessment tool: User's guide.” vancouver school of economics COVID-19 nature of work risk team. [Google Scholar]
- Baylis P., L Beauregard P.-, Connolly M., Fortin N., Green D.A., Cubillos P.G., Gyetvay S., Haeck C., Molnar T.L., Simard-Duplain G., Siu H.E., teNyenhuis M., Warman C. 2020. The distribution of COVID-19 related risk. NBER Working Paper #27881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauregard P.-L., Connolly M., Haeck C. 2020. Professions et Industries: Quels sont les Risques de Transmission de la COVID-19? Un Outil pour Faire Face à la Deuxième Vague. Cirano Working Paper #2020PE-40. [Google Scholar]
- Beland L.-P., Brodeur A., Wright T. 2020. The short-term economic consequences of COVID-19: Exposure to disease, remote work and government response. IZA Working Paper #13159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benatia D., Godefroy R., Lewis J. Estimates of COVID-19 cases across four Canadian provinces. Canadian Public Policy. 2020;46(S3):203–216. doi: 10.3138/cpp.2020-035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benatia D., Godefroy R., Lewis J. 2020. Estimating COVID-19 prevalence in the United States: A sample selection model approach. medRxiv Working Paper. [Google Scholar]
- Boateng G., Adams T. Drop dead... I need your job’: An exploratory study of intra-professional conflict amongst nurses in two ontario cities. Social Science & Medicine. 2016;115:35–42. doi: 10.1016/j.socscimed.2016.02.045. [DOI] [PubMed] [Google Scholar]
- Boateng G., Schuster R., Boateng M. Uncovering a health and wellbeing gap among professional nurses: Situated experiences of direct care nurses in two Canadian cities. Social Science & Medicine. 2019;242 doi: 10.1016/j.socscimed.2019.112568. [DOI] [PubMed] [Google Scholar]
- Cameron C., Gelbach J., Miller D. Robust inference with multi-way clustering. Journal of Business & Economic Statistics. 2011;28:238–249. [Google Scholar]
- CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 – United States. Morbidity & Mortality Weekly Report. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A., Avery C., Spitzer A., McCormack G. Economic vulnerability of households with essential workers. JAMA. 2020;324(4):388–389. doi: 10.1001/jama.2020.11366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra A., Devereux M., Lahiri A. 2020. Pandemics through the lens of occupations. NBER Working Paper #27841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowkwanyun M., Reed A. Racial health disparities and covid-19 – caution and context. New England Journal of Medicine. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- CIHI . Canadian Institute for Health Information; Ottawa: 2021. Nursing in Canada, 2020 – data tables. [Google Scholar]
- Clark, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: A modelling study. Lancet Global Public Health. 2020;8:e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay K., Lewis J., Severnini E. Pollution, infectious disease, and mortality: Evidence from the 1918 Spanish influenza pandemic. The Journal of Economic History. 2018;78(4):1179–1209. [Google Scholar]
- Clay K., Lewis J., Severnini E. What explains cross-city variation in mortality during the 1918 influenza pandemic? Evidence from 438 U.S. Cities. Economics and Human Biology. 2019;35:42–50. doi: 10.1016/j.ehb.2019.03.010. [DOI] [PubMed] [Google Scholar]
- Clay K., Lewis J., Severnini E., Wang X. 2020. The value of health insurance during a crisis: Effects of medicaid implementation on pandemic influenza mortality. NBER Working Paper #27120. [Google Scholar]
- Cooper C. CRC; London: 2005. Handbook of stress medicine and health. [Google Scholar]
- Currie J., Gruber J. Health insurance eligibility, utilization of medical care, and child health. Quarterly Journal of Economics. 1996;111(2):431–466. [Google Scholar]
- Currie J., Stabile M. Socioeconomic status and health: Why is the relationship stronger for older children? The American Economic Review. 2003;93(5):1813–1823. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- Curtis L., Dooley M., Lipman E., Feeny D. The role of permanent income and family structure in the determination of child health in Canada. Health Economics. 2001;10(4):287–302. doi: 10.1002/hec.591. [DOI] [PubMed] [Google Scholar]
- Cutler D., Lange F., Meara E., Richards S., Ruhm C. The contribution of risk factors to the SES gradient in health: 1970-2000. Journal of Health Economics. 2011;30:1174–1187. doi: 10.1016/j.jhealeco.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D., Lleras-Muney A. Understanding differences in health behaviors by education. Journal of Health Economics. 2010;29(1):1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D., Lleras-Muney A., Vogl T. 2008. Socioeconomic status and health: Dimensions and mechanisms. NBER Working Paper #27908. [Google Scholar]
- Dingel J., Neiman B. How many jobs can Be done at home? Journal of Public Economics. 2020;189 doi: 10.1016/j.jpubeco.2020.104235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo I. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annual Review of Sociology. 2009;35:553–572. [Google Scholar]
- Evans W., Garthwaite C. Giving mom a break: The impact of higher EITC payments on maternal health. American Economic Journal: Economic Policy. 2014;6(2):258–290. [Google Scholar]
- Evans G., Kantrowitz E. Socioeconomic status and health: The potential role of environmental risk factors. Annual Review of Public Health. 1996;23:216–262. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- FIQ . 2020. Collective agreement: Salary scales and list of job titles.http://www.fiqsante.qc.ca/wp-content/uploads/2016/10/Echelles_ salariales_Web_2016-2020_ANG.pdf?download=1 July 2016 - March 2020. [Google Scholar]
- Goldberger L., Breznitz S. Free Press; New York: 1993. Handbook of stress: Theoretical and clinical aspects. [Google Scholar]
- Golestaneh L., Neugarten J., Fisher M., Billett H., Reyes Gil M., Johns T., Yunes M., Mokrzycki M., Coco M., Norris K., Perez H., Scott S., Kim R., Bellin E. The association of race and COVID-19 mortality. Lancet. 2020;25:100455. doi: 10.1016/j.eclinm.2020.100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman-Bacon A. Public health insurance and mortality: Evidence from medicaid implementation. Journal of Political Economy. 2018;126(1):216–262. [Google Scholar]
- Government of the District of Columbia . 2020. COVID-19 surveillance.https://coronavirus.dc.gov/data/ [Google Scholar]
- Grimard F., Parent D. Education and smoking: Were vietnam war draft avoiders also more likely to avoid smoking? Journal of Health Economics. 2007;26(5):896–926. doi: 10.1016/j.jhealeco.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D., Du B., Li L. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holroyd-Leduc J., Laupacis J. Continuing care and COVID-19: A Canadian tragedy that must not Be allowed to happen again. Canadian Medical Association Journal. 2020;192(23):E632–E633. doi: 10.1503/cmaj.201017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoynes H., Miller D., Simon D. Income, the earned income Tax Credit, and infant health. American Economic Journal: Economic Policy. 2015;7(1):172–211. [Google Scholar]
- INSPQ . 2020. Données COVID-19 au Québec.https://www.inspq.qc.ca/covid-19/donnees [Google Scholar]
- Ji Y., Ma Z., Peppelenbosch M., Pan Q. Potential association between COVID-19 mortality and healthcare resource availability. Lancet Global Health. 2020;8 doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenkel D. Health behavior, health knowledge, and schooling. Journal of Political Economy. 1999;99(2):287–305. [Google Scholar]
- Kim E., Marrast L., Conigliaro J. COVID-19: Magnifying the effect of health disparities. Journal of General Internal Medicine. 2020;35(8):2441–2442. doi: 10.1007/s11606-020-05881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange F. The role of education in complex health decisions: Evidence from cancer screening. Journal of Health Economics. 2011;30:43–54. doi: 10.1016/j.jhealeco.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Link B., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. Extra Issue: Forty Years of Medical Sociology: The State of the Art and Directions for the Future. [PubMed] [Google Scholar]
- Marmot M. Holt; New York, NY: 2004. The status syndrome: How social standing affects our health and longevity. [Google Scholar]
- Marmot M., Kogevinas M., Elston M. Social/economic status and disease. Annual Review of Public Health. 1987;8:111–135. doi: 10.1146/annurev.pu.08.050187.000551. [DOI] [PubMed] [Google Scholar]
- Marmot M., Smith G., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil servants: The whitehall II study. Lancet. 1991;337:1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Marmot M., Wilkinson R. Oxford University Press; Oxford: 1999. Social determinants of health. [Google Scholar]
- Maryland Dept of Health . 2020. Coronavirus disease 2019.https://coronavirus.maryland.gov/ [Google Scholar]
- Massachusetts Dept. of Public Health . 2020. Coronavirus updates and information.https://www.mass.gov/orgs/department-of-public-health/data/ [Google Scholar]
- McDonough P., Duncan G., Williams D., House J. Income dynamics and adult mortality in the United States, 1972 through 1989. American Journal of Public Health. 1999;87(9):1476–1483. doi: 10.2105/ajph.87.9.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen B. Stress, adaptation, and disease: Allostatis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McLaren J. 2020. Racial disparities in COVID-19 deaths: Seeking economic roots with census data. NBER Working Paper #27407. [Google Scholar]
- Medlock K., Temzedlides T., Hung S. COVID-19 and the value of safe transport in the United States. Scientific Reports. 2021;11 doi: 10.1038/s41598-021-01202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray T. U.S. PIRG Education Fund/Frontier Group; 2020. Nursing home safety during COVID: PPE shortages. [Google Scholar]
- NY State Dept of Health . 2020. Information on novel coronavirus.https://coronavirus.health.ny.gov/home [Google Scholar]
- Phelan J., Link B., Tehranifar P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior. 2010;51(1):S28–S40. doi: 10.1177/0022146510383498. supplement. [DOI] [PubMed] [Google Scholar]
- Philadelphia Dept. of Public Health . 2020. COVID-19 guidance and updates.https://www.phila.gov/departments/department-of-public-health/ [Google Scholar]
- Rinfret M. 2020. COVID-19 in CHSLDs during the first wave of the pandemic.” the Quebec Ombudsman's Status Report. [Google Scholar]
- Ross C., Mirowksky J. In: Handbook of medical sociology. 6th ed. Timmermans S., Fremont A., Conrad P., Bird C., editors. Vanderbilt University Press; Nashville, TN: 2010. Why education is the key to socioeconomic differentials in health. (Chapter 3), 33–51. [Google Scholar]
- Santé Montréal . 2020. Coronavirus COVID-19.https://www.santemontreal.qc.ca [Google Scholar]
- Schneider D., Harknett K. Consequences of routine work-schedule instability for worker health and well-being. American Sociological Review. 2019;84(1):82–114. doi: 10.1177/0003122418823184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker J. Education and the changing shape of the income gradient in health. Journal of Health and Social Behavior. 2004;45(3):286–305. doi: 10.1177/002214650404500304. [DOI] [PubMed] [Google Scholar]
- Simonov A., Szymon S., Dubé J.-P., Biswas S. 2020. The persuasive effects of fox news on compliance with social distancing during the covid-19 pandemic. NBER Working Paper #27237. [Google Scholar]
- Smith J. Healthy bodies and thick wallets: The dual relation between health and economic status. The Journal of Economic Perspectives. 1999;13(2):145–166. [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada . 2016. Census of population.https://www12.statcan.gc.ca/census-recensement/index-eng.cfm [Google Scholar]
- Turcotte M., Savage K. Statistics Canada; 2020. The contribution of immigrants and population groups designated as visible minorities to nurse aide, orderly, and patient service occupations. [Google Scholar]
- U.S. DHHS . U.S. Department of Health and Human Services; Washington, D.C: 2010. Health people 2020 framework. [Google Scholar]
- de Walque D. Does education affect smoking behaviors? Evidence using the vietnam draft as an instrument for college education. Journal of Health Economics. 2007;26:877–895. doi: 10.1016/j.jhealeco.2006.12.005. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva, Switzerland: 2008. CSDH final report: Closing the gap in a generation: Health equity through action on the social determinants of health. [Google Scholar]
- Wilkinson R. Income distribution and mortality: A ‘natural’ experiment. Sociology of Health & Illness. 1990;12:391–412. [Google Scholar]
- Wilkinson R. Health, hierarchy, and social anxiety. Annals of the New York Academy of Sciences. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Wu Z., McGoogan J. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1245. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Wu X., Nethery R., Sabath B., Braun D., Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Science Advances. 2020;6(45) doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.