Abstract
Objective
To evaluate the effectiveness of a comprehensive educational intervention in a hybrid model of cardiac rehabilitation in Spain during the COVID-19 pandemic.
Methods
In a prospective pretest-posttest pilot study a pooled sample of patients attending hybrid cardiac rehabilitation in Spain received a culturally-adapted education intervention for 6 weeks. Participants completed surveys at pre- and post-rehabilitation assessing disease-related knowledge, health literacy, adherence to the Mediterranean Diet and self-efficacy. Physical activity was measured by number of steps per day using wearable activity tracking devices. Satisfaction with the educational materials was also evaluated by a survey with a 10 point Likert-type scale and yes/no and open-ended questions.
Results
Eighty-one(99%) participants completed both assessments. There was significant improvement in disease-related knowledge(p < 0.001), physical activity(p < 0.001), and adherence to the diet(p = 0.005) post-rehabilitation. The number of participants that were classified as having “high health literacy skills” increased by 17%. Post-rehabilitation knowledge was associated with education level (ß = 0.430; p = 0.001),pre-rehabilitation knowledge (ß = 0.510; p = 0.002), and high health literacy skills (ß = 0.489; p = 0.01). Educational materials were highly satisfactory to participants.
Conclusion
Significant increases in disease-related knowledge and health behaviors in patients attending hybrid models of cardiac rehabilitation are encouraging results that support the value of implementing comprehensive educational initiatives to programs in Spain.
Innovation
This work presents preliminary evidence of the effectiveness of the first comprehensive education intervention that is open access and culturally adapted to people living with cardiovascular disease in Spain.
Key words: Cardiac rehabilitation; Patient education as topic/methods; Pilot projects; Process assessment, healthcare/methods; Health behaviour; Health knowledge, attitudes, practice
1. Introduction
Cardiovascular disease (CVD) is the leading cause of disability and death worldwide [1]. Coronary heart disease – the most common CVD – causes 1.8 million or 27% of all deaths in Europe [2], and its prevalence is estimated to increase by 18% by 2030 [3]. In Spain, CVD accounts for 1 in 4 deaths in men and one-third of deaths in women [4]. Spain has one of the world’s highest life expectancies at birth [5,6], which combined with other factors such as high proportion of immigrants result in challenges in the care of people living with CVD, including disability and healthcare cost [7,8]. Cardiac Rehabilitation (CR) is a cost-effective model of secondary prevention that can mitigate this burden [[9], [10], [11]].
CR aims to improve the functional capacity, wellbeing and health-related quality of life of CVD patients through exercise training, risk factor modification, psychosocial management and patient education and counselling [11,12]. Research has shown that the most effective way to deliver CR is comprehensively (i.e., including all core components) [13]. Despite well-established benefits, comprehensive CR has low availability and is underutilized [14,15]. The coronavirus disease 2019 (COVID-19) pandemic has contributed to a further reduction in availability and access to these programs [16].
Spain is among the countries worst hit by the Covid-19 pandemic, with one of the highest rate of infections and deaths per million inhabitants [17]. The limitations caused by the pandemic combined with the increasing need for CR led to programs lacking resources to offer comprehensive care for CVD patients. This situation forced programs to transition from traditional models of CR (i.e., delivered in a clinical setting with weekly visits for exercise, education and counselling over a period of several months) to alternative models of CR (i.e., community services, home support or individualized management, delivered isolated or combined with in-person visitations [i.e., hybrid model] using different types of communication such as paper, telephone, apps, email, text message, web pages, online meetings or direct contact) [18,19]. Although evidence suggests that the cost-effectiveness of the delivery of CR through telerehabilitation is similar to a centre-based program [20,21], programs were not prepared for such delivery when the pandemic started. In 2017, it was reported that alternative CR models were available in only one-quarter of countries globally and where offered, capacity was insufficient half the time [22]. In 2020, a global survey of the impacts of COVID-19 on CR delivery around the globe reported that over 60% of programs did not offer any remote model of CR delivery [16]. The lack of and imposed transition to alternative models led to various challenges during the pandemic, including the need for resources to deliver all core components of CR such as patient education [[23], [24], [25]]. Another gap highlighted by this survey was the availability of patient education resources to support the delivery of comprehensive CR using alternative models such as fully virtual and hybrid programming [16]. Due to the lack of resources, many programs cancelled education — a critical component of patient self-management. Cardiac College™, a patient-centered education website, bridged this gap for many programs across the world.
To our knowledge, Cardiac CollegeTM is the only evidence-based and theoretically-informed comprehensive educational program for CR. It is available open access in 8 languages, including Spanish [[26], [27], [28], [29]]. The goal of this curriculum is to educate patients about the nature of CVD and its medical management, how to get active and eat well, how to take care of their psychosocial well-being and be an active self-manager. It comprises 5 modules delivered in-person, in print and/or online. Although the effectiveness of Cardiac CollegeTM was confirmed in Spanish-speaking patients from Latin America [28], the delivery of this education as an intervention within a hybrid model of CR has not been previously assessed.
Therefore, the purpose of this pilot study was to evaluate the effectiveness of Cardiac CollegeTM in a hybrid model of CR in Spain during the COVID-19 pandemic, before implementing it more broadly. In the present study, we also investigated patients’ satisfaction with the materials used to deliver the education intervention.
2. Methods
2.1. Design
This was a prospective pretest-posttest pilot study. A pooled sample of cardiac patients attending hybrid CR received the comprehensive education intervention called Cardiac CollegeTM, with assessments carried out at baseline (pre-CR) and at CR discharge (post-CR). The study was conducted in the CR unit of the Hospital General Universitario Gregorio Marañón (Madrid, Spain) following the standards required by the Declaration of Helsinki and approved by the Hospital’s Ethics Committee (approval number: RCA20). All participants provided written informed consent. Data were collected between December/2020 and July/2021.
2.2. Setting and intervention
The Hospital General Universitario Gregorio Marañón is in Madrid, Spain. The CR program is located within the hospital and cares for approximately 500 patients annually. The healthcare team is comprised of a physical medicine and rehabilitation physician, two cardiologists, two nurses, one physiotherapist, one psychologist and one administrative assistant. CR participants were offered supervised exercise sessions twice a week for 6 weeks, and provided a home exercise prescription for the other days of the week. The educational intervention consisted of a weekly lecture covering the following topics: cardiovascular diseases, cardiovascular risk factors, medical therapy, healthy diet, exercise and physical activity, and CR phase III (i.e., community support to maintain or improve current health or cardiac patients).
Due to the COVID-19 pandemic, adaptations were made to the CR program due to government restrictions and to reduce transmission. Patients who were clinically stable or who could not attend face-to-face sessions underwent onsite personal training sessions with the healthcare team to exercise at home and follow the lesson plans for self-learning. Weekly contacts with the healthcare team were scheduled to support and educate these patients.
2.3. The Spanish version of Cardiac CollegeTM: culturally-adapted to people living in Spain
Cardiac CollegeTM was developed originally in English and followed a rigorous and theory-based process, by local and international CR experts and patient partners [30]. All content is written in plain language to ensure clear and actionable messaging for a diverse audience. The original version was translated to Spanish, culturally-adapted and tested in a group of 249 Spanish speaking patients attending onsite CR in three Latin American countries [28]. Significant improvements in disease-related knowledge, health literacy, self-efficacy, and health behaviours were identified [28].
Based on best practices in translation and adaptation [31,32], the Spanish version of Cardiac CollegeTM was adapted for use in Spain through two steps: (1) the original version of the materials and the Spanish translation were checked for consistency and terms were adapted to match the Spanish dialect spoken in Spain; and, (2) the material was given to a group of 8 experts in CR (two physical medicine and rehabilitation physicians, two cardiologists, two nurses, and one physiotherapist). These steps were following to harmonize and culturally adapt the material, making adaptations that addressed the guidelines and care CVD patients receive in Spain and eliminating any elements that might be conceptually inappropriate or could cause any confusion.
Culturally adapted materials for use in Spain were added to the Cardiac CollegeTM website and included the patient guide, lesson plans and 12 educational videos. The patient guide was comprised of 9 booklets organized into the five pillars of the Cardiac CollegeTM curriculum named treat heart disease (4 booklets), get active (1 booklet), eat healthy (1 booklet), feel well (2 booklets), and take control (1 booklet). PDFs of the booklets were available online for download at the Cardiac CollegeTM website and research participants received a printed copy of the booklets if requested. In addition, each participant of the study received six weekly lesson plans that provided a summary of all educational materials (including links) to support their 6-week educational program. Finally, 12 animated videos (mean duration of 5 minutes each) were also created.
2.4. Participants
Patients with coronary heart disease, heart failure, cardiomyophathy, valvular heart disease or arrhythmias recruited from a CR program were included. The exclusion criteria were: lack of Spanish-language proficiency, and any visual, cognitive or serious psychiatric condition that would preclude the participant from completing the surveys.
Previous studies using Cardiac CollegeTM that had disease-related knowledge as the primary outcome indicated that a sample size of 84 was sufficient to reach a small to moderate effect size (d = 0.25), with a statistical power of 0.95, and a 1-sided alpha of 0.025, including a 60% retention rate. Patients were recruited continuously until the desired sample size was achieved.
2.5. Procedures
Patients were invited to participate in the study during their initial assessment. Consenting patients completed an online survey (pre-CR survey) administered via REDCap and used a wearable activity tracker for 7 days. At the end of the 6-week CR program participants were invited to complete another online survey (post-CR survey) via REDCap and wore the activity tracker for another 7 days.
All participants received a printed version of the Cardiac CollegeTM guide or were instructed to download PDFs of these materials online. A schedule of education and 6 lesson plans were also available to participants in print or online. Participants received 7 educational sessions of 60 minutes in duration each, delivered once a week by the CR team onsite or through self-learning where patients were instructed to learn about specific topics at home. For self-learning sessions, there were weekly opportunities to ask questions about the educational topic. The education schedule is described in Appendix 1.
2.6. Outcome measures
Disease-related knowledge, health literacy, physical activity, adherence to the Mediterranean diet, and exercise self-efficacy were assessed at pre- and post-CR using Spanish versions of psychometrically-validated scales as outlined below. Pre-CR, all participants self-reported ethnicity, education level, marital and work status. Post-CR, they also completed a satisfaction survey about the educational materials, which included 10 Likert-type, yes/no and open-ended questions. Clinical characteristics (CR referral indication and cardiac risk factors) were extracted from medical records.
2.6.1. Disease-related knowledge
Assessed using the short version of the Coronary Artery Disease Education Questionnaire (CADE-Q SV) [33], which consists of 20 true/false/I don't know items about medical condition, risk factors, exercise, nutrition, and psychosocial risk. The maximum score possible is 20 overall, four for each domain, with higher scores indicating better knowledge. The Spanish version of CADE-Q SV has been psychometrically-validated [33].
2.6.2. Health literacy
Measured using three instruments named the BRIEF Health Literacy Screening Tool [34], the Medical Term Recognition Test (METER) [35], and the Newest Vital Sign (NVS) [36]. As health literacy has different dimensions, these multiple tools were used. The BRIEF measures health literacy skills by asking respondents to complete four questions using a 5-point Likert-type scale. Score ranges are 4-12 (inadequate), 13-16 (marginal), and 17-20 (adequate) [34]. The METER measures respondents’ prior reading experience by instructing them to mark actual medical terms in a list of 70 words. Score ranges are 0-20 (low), 21-34 (marginal), and 35-40 (functional health literacy) [35]. The NVS measures nutrition reading, comprehension, and numeracy through six questions regarding the information found on an accompanying nutrition label. Score ranges from 0-6, with scores ≥ 4 considered evidence of adequate health literacy [36]. A combined measure named “high health literacy skills” was created by combining the results obtained using the three instruments (i.e. BRIEF, METER and NVS). The criterion used for combining these measures was a simple approach that allowed the combination of adequate levels in all three skills. Therefore, when participants presented adequate health literacy measured by the BRIEF and NVS and functional health literacy by METER, they were classified as having high health literacy skills.
2.6.3. Physical activity
Measured by number of steps per day using wearable activity tracking devices. All participants were instructed to report their steps for seven consecutive days (before CR intake and at discharge) using a log provided. Mean steps per day were computed, with 7,500 steps corresponding to 150 minutes/week in chronic disease populations [37].
2.6.4. Adherence to the Mediterranean Diet (MD)
Assessed using the Mediterranean Diet Score (MDS) tool. This is a self-administered tool consisting of 13 questions about food consumption frequency and food intake habits related to the MD. Score ranges are 0-5 (low adherence to MD) and 10-13 (high adherence to MD) [38].
2.6.5. Exercise self-efficacy
Assessed using a modified version of the Bandura’s 18-item exercise self-efficacy (ESE) scale, which asked respondents “How confident are you that you can exercise most days of the week?” instead of three or more times per week as the original version. Participants responded on a 5-point Likert scale ranging from 1= “not confident at all” to 5= “very confident” [39].
2.7. Statistical analysis
First, descriptive statistics were computed to describe participants’ sociodemographic and clinical characteristics overall. Continuous variables are presented as mean ± standard deviation (SD) and discrete variables are presented as number (percentage) unless otherwise stated. Choice of hybrid CR model was considered: differences in the sociodemographic and clinical characteristics of participants that attended mostly sessions onsite vs home-based were tested using t-tests or chi-square as appropriate.
Second, descriptive statistics were also used to describe satisfaction with the educational materials. Pearson correlation coefficients were used to determine the associations between satisfaction, knowledge and health literacy. T-tests were used to test the difference in knowledge between participants that presented higher health literacy levels and satisfaction.
Third, paired t-tests were used to investigate outcome changes between assessments (i.e., pre- and post-CR). Given the effects of socioeconomic status, health literacy among other factors on disease-related knowledge, simple and multiple linear regression models were computed to investigate differences in overall post-CR knowledge (dependent variable) based on these characteristics.
Given that multiple tests were performed, a more conservative approach was taken to denote statistical significance: an adjusted p-value of less than 0.01 was considered significant [40]. All analysis was completed using SPSS version 28.0 (IBM Inc. 2021, NYC).
3. Results
3.1. Participants’ characteristics
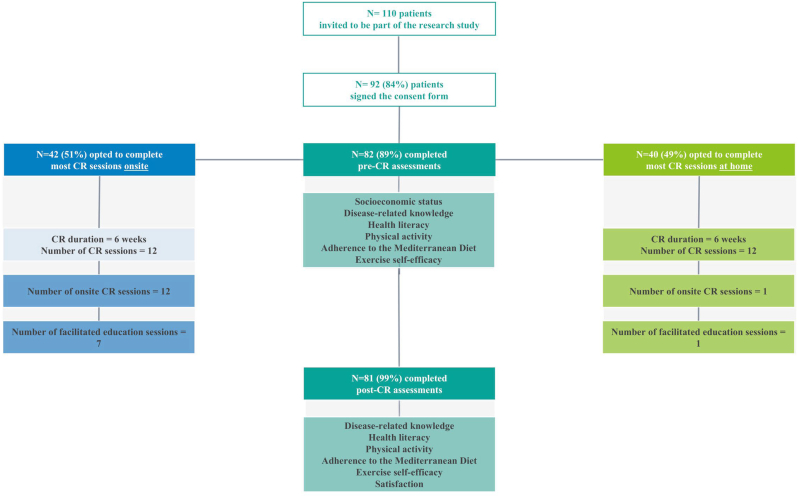
A flow diagram is shown in Fig. 1. Overall, 82 patients consented to participate in this study and completed the pre-CR survey; 81 (99%) participants completed both assessments. Table 1 presents the sociodemographic and clinical characteristics of these participants. A comparison of characteristics among those that completed most CR sessions onsite (n=42; 51%) vs. those that completed most sessions at home (n=40; 49%) is also found in Table 1. As shown, younger patients and those that had a diagnosis of cardiomyopathy were significantly more likely to choose to attend more sessions onsite as part of their hybrid CR model.
Fig. 1.
Flow diagram
Table 1.
Participants’ sociodemographic and clinical characteristics overall and by main component of hybrid CR model (n=82)
| Overall (n=82) | Main component of hybrid CR model |
|||
|---|---|---|---|---|
| Mean±SD / n (%) | Mostly onsite sessions (n=42) | Mostly home-based sessions (n=40) | p⁎ | |
| Sociodemographic characteristics | ||||
| Age | 57.2 ± 11.6 | 54.1 ± 12.2 | 60.4 ± 10.1 | 0.01 |
| Sex (% male) | 68 (83%) | 37 (54%) | 31 (46%) | 0.47 |
| Ethnicity (% European) | 75 (92%) | 37 (49%) | 38 (51%) | 0.90 |
| Education (% ≤ elementary school) | 32 (39%) | 18 (56%) | 14 (44%) | 0.48 |
| Work status (% retired) | 27 (33%) | 11 (41%) | 16 (59%) | 0.34 |
| Marital status (% married) | 52 (64%) | 25 (48%) | 27 (51%) | 0.78 |
| Clinical Characteristics | ||||
| Coronary artery disease | 64 (78%) | 28 (44%) | 14 (56%) | 0.32 |
| Percutaneous coronary intervention | 56 (68%) | 23 (41%) | 33 (59%) | 0.18 |
| Smoking (% current) | 53 (65%) | 33 (62%) | 20 (38%) | 0.07 |
| Dyslipidemia | 42 (51%) | 20 (48%) | 22 (52%) | 0.76 |
| Obesity | 40 (49%) | 20 (50%) | 20 (50%) | 1.00 |
| Hypertension | 39 (48%) | 19 (49%) | 23 (51%) | 0.87 |
| Angina | 21 (26%) | 12 (57%) | 9 (43%) | 0.51 |
| Diabetes type 2 | 16 (20%) | 10 (63%) | 6 (37%) | 0.32 |
| Heart failure | 14 (17%) | 10 (59%) | 4 (41%) | 0.11 |
| Cardiomyopathy | 11 (13%) | 10 (90%) | 1 (10%) | 0.007 |
| Family history of myocardial infarction | 10 (12%) | 8 (80%) | 2 (20%) | 0.06 |
| Alcohol consumption (% high) | 10 (12%) | 4 (40%) | 6 (60%) | 0.53 |
| Arrhythmia | 10 (12%) | 7 (70%) | 3 (30%) | 0.21 |
| Metabolic Syndrome | 8 (10%) | 5 (63%) | 3 (27%) | 0.48 |
| Sleep apnea | 8 (10%) | 3 (27%) | 5 (63%) | 0.48 |
| Coronary artery bypass graft surgery | 7 (9%) | 5 (70%) | 2 (3%) | 0.26 |
| Depression | 5 (6%) | 4 (80%) | 1 (20%) | 0.18 |
| Fibrillation | 4 (5%) | 3 (75%) | 1 (3%) | 0.32 |
| Valve disease | 3 (4%) | 2 (60%) | 1 (40%) | 0.56 |
Percentages in the different types of hybrid CR models are related to the number of participants identified by characteristic.
CR, cardiac rehabilitation; SD, standard deviation.
Difference between participants who attended different types of hybrid CR models.
3.2. Effectiveness of education intervention
Mean scores of all outcome measures at each assessment are presented in Table 2. As shown, there was a significant increase from pre- to post-CR in total disease-related knowledge (p<0.0001), as well as in 4 out of 5 specific knowledge areas. Risk Factors was the area with the highest knowledge at both assessment points. The biggest increase in knowledge post-CR was in the psychological risk area. With regards to health literacy, none of scores from the three instruments (i.e. BRIEF, METER and NVS) increased significantly at post-CR when compared to pre-CR. The number of participants that were classified as having “high health literacy skills” using the combined health literacy measure increased by 17%.
Table 2.
Disease-related knowledge, health literacy, physical activity, adherence to the Mediterranean Diet and exercise self-efficacy pre- and post-CR (n = 81)
| Outcome measures | Possible score range | Pre-CR | Post-CR | Change | p |
|---|---|---|---|---|---|
| Disease-related knowledge | |||||
| CADE-Q SV total scores (mean±SD) | 0–20 | 15.1 ± 2.8 | 17.6 ± 2.1 | +2.5 | <0.001 |
| Subscale: medical condition (mean±SD) | 0–4 | 3.1 ± 1.1 | 3.5 ± 0.8 | +0.4 | <0.001 |
| Subscale: risk factors (mean±SD) | 0–4 | 3.6 ± 0.7 | 3.8 ± 0.5 | +0.2 | 0.03 |
| Subscale: exercise (mean±SD) | 0–4 | 2.8 ± 0.8 | 3.4 ± 0.7 | +0.6 | <0.001 |
| Subscale: diet (mean±SD) | 0–4 | 3.2 ± 1.0 | 3.6 ± 0.4 | +0.4 | 0.002 |
| Subscale: physiological risk (mean±SD) | 0–4 | 2.3 ± 1.0 | 3.1 ± 0.9 | +0.8 | <0.001 |
| Health literacy | |||||
| BRIEF total scores (mean±SD) | 4–20 | 14.8 ± 2.4 | 15.2 ± 3.0 | +0.4 | 0.16 |
| Adequate health literacy, n (%) | 17–20 | 20 (25%) | 28 (35%) | +11% | - |
| METER total scores (mean±SD) | 0–40 | 35.9 ± 5.2 | 35.5 ± 5.6 | -0.4 | 0.46 |
| Functional health literacy, n (%) | 35–40 | 64 (79%) | 62 (76%) | -3% | - |
| NVS total scores (mean±SD) | 0–6 | 4.2 ± 2.0 | 4.3 ± 2.0 | +0.1 | 0.18 |
| Adequate health literacy, n (%) | 4–6 | 53 (65%) | 56 (69%) | +4% | - |
| High health literacy skills, n (%) | - | 10 (13%) | 25 (30%) | +17% | - |
| Physical activity | |||||
| Steps taken per day (mean±SD) | - | 9,991.2 ± 4,358.6 | 12,452.4 ± 4,594.6 | +2461.2 | <0.001 |
| Participants who reached ≥ 7,500 per day, n (%) | - | 61 (74%) | 70 (85%) | +11% | - |
| Adherence to the Mediterranean Diet | |||||
| MDS total scores (mean±SD) | 0–13 | 9.8 ± 1.7 | 10.8 ± 1.7 | +1.0 | 0.005 |
| Low adherence, n (%) | 0–5 | 1 (1%) | 0 (0%) | -1% | - |
| High adherence, n (%) | 6–13 | 48 (59%) | 56 (68%) | +9% | - |
| Exercise self-efficacy | |||||
| Bandura’s SE scale (mean±SD) | 0–5 | 3.33 ± 0.85 | 3.51 ± 0.73 | +0.18 | 0.02 |
CADE-Q SV, Coronary Artery Disease Education Questionnaire Short Version; CR, cardiac rehabilitation; MDS, Mediterranean Diet Score; METER, Medical Term Recognition Test; NVS, Newest Vital Sign; SD, standard deviation; SE self-efficacy.
With regards to physical activity, mean steps per day increased significantly from pre- to post-CR (p < 0.0001) and the number of participants that reached ≥ 7,500 steps per day increased by 11%. With regard to adherence to the Mediterranean Diet, MDS scores also increased significantly from pre- to post-CR (p=0.005), with the percentage of participants classified with high adherence increasing by 9% at post-CR. As also shown in Table 2, the increase in exercise self-efficacy scores was not considered significant at post-CR when compared to pre-CR scores (p = 0.02).
The regression models are presented in Table 3. Results suggested that education level, pre-CR knowledge and high health literacy skills are associated with post-CR knowledge. The multiple regression analysis model was significant (F = 10.40, p < 0.001) but with low power (R2 = 0.22); however, all factors remained associated with post-CR knowledge.
Table 3.
Simple and multiple regression analysis for disease-related knowledge total scores at post-CR
| Simple regression |
Multiple regression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | SE | p | 95% CI Lower Bound | 95% CI Upper Bound | β | SE | p | 95% CI Lower Bound | 95% CI Upper Bound |
| Age | –0.034 | 0.028 | 0.84 | –0.064 | 0.053 | - | - | - | - | - |
| Sex | –0.012 | 0.684 | 0.95 | –1.503 | 1.411 | - | - | - | - | - |
| Education level | 0.510 | 0.429 | 0.002 | 0.672 | 2.499 | 0.430 | 0.429 | 0.001 | 0.546 | 2.310 |
| Work status | 0.021 | 0.152 | 0.90 | -0.304 | 0.343 | - | - | - | - | - |
| Type of hybrid CR model⁎ | 0.015 | 0.429 | 0.91 | -0.872 | 0.967 | - | - | - | - | - |
| Pre-CR knowledge | 0.536 | 0.085 | 0.002 | 0.129 | 0.493 | 0.510 | 0.081 | 0.002 | 0.118 | 0.488 |
| High health literacy skills | 0.522 | 0.438 | 0.01 | –0.362 | 1.506 | 0.489 | 0.390 | 0.01 | –0.322 | 1.306 |
SE, standard error; CI, confidence interval; CR, cardiac rehabilitation.
More sessions onsite vs. more sessions at home.
3.3. Participants’ satisfaction with the educational materials
Overall, participants were satisfied with the educational materials intervention, thought they were useful to help the management of their condition, were often able to get the information they were looking for and understand the information, and mostly described the amount of information received by the materials as just right (Fig. 2). Fig. 2 also shows that most participants used the educational materials provided outside of CR sessions, with 53.8%, 46.8% and 39.4% reporting using the patient guide, lesson plans and short videos more than 10 times per month, respectively. The topic (see Appendix 1) with the highest satisfaction was “heart medicines” (mean = 2.5 ± 0.6/3; delivered on week 5) and the one with the lowest satisfaction was “questions and CR phase III” (mean = 1.9 ± 0.9/3; delivered on week 5). Finally, when asked what they would do if they had a question about heart disease, 22% of participants reported they would look for answers in the educational materials provided.
Fig. 2.
Satisfaction with educational materials
4. Discussion and conclusion
4.1. Discussion
Results of this pilot study demonstrate that delivery of a translated and culturally adapted comprehensive, evidence- and theoretically-based, patient-centered education intervention improved disease-related knowledge and healthy behaviors (i.e., physical activity and adherence to the Mediterranean diet) in participants of a hybrid CR model in Spain. Although effectiveness of this intervention has been confirmed by others [[26], [27], [28]], this study has for the first time shown the use of Cardiac CollegeTM in a hybrid CR model. These results are timely and can be useful beyond Spain, as many programs around the world have moved to a hybrid model of care with some in-person contact at the beginning of the program [16], as advocated by International CR Associations during the early stages of the pandemic [[41], [42], [43], [44], [45]]. In addition, a global survey on the impacts of COVID-19 pandemic on CR revealed a significant drop in the amount of patient education delivery due mainly to the lack of reliable resources [16]. This pilot data provides preliminary support that effective materials are available open access and could be a beneficial adjunct to CR programs in Spain.
Health literacy is an important concept for people living with chronic conditions as it helps them manage their condition and navigate the health care environment [46,47]. Its definition goes beyond the understanding of basic health information in medical situations and extends to skills and abilities to obtain, process and understand health information, as well as applying it when making decisions related to health [48]. In the present study, health literacy was measured using three instruments in order to incorporate these different abilities. This study has not identified increases in any health literacy skills after the education intervention which is in contrast to a previous study using the Spanish version of these educational materials in Latin America [28]. This may be because participants from this study already presented high levels of health literacy at baseline, as is commonly seen in studies from high income countries [46]. In addition, there is a complex relationship between health literacy, disease-related knowledge and education, which is influenced by personal, situational, and socioenvironmental factors such as socioeconomic level and place of living [47,49]. Regression analysis from this study confirmed this significant association between high health literacy skills and disease-related knowledge post educational intervention.
There are considerable gaps in the literature concerning cardiac patients’ preferences, information needs and satisfaction with educational interventions, especially within virtual learning. Understanding these characteristics and creating alternative CR models aligned to what patients want and need is paramount to increasing access and participation in these programs [50]. In this pilot study, it was identified that participants were satisfied overall with the educational materials (named patient guide, short videos and lesson plans) and used them often, even beyond the CR program. This study provides a starting point on this topic and invites researchers to investigate in depth participants’ preferences and needs about the delivery of core components in hybrid and virtual CR models.
While the present study provides preliminary evidence of the effectiveness of a comprehensive patient education intervention in a hybrid CR model in Spain, caution is needed when interpreting these results. First, this was not a randomized study, so no causal conclusions can be drawn. Also, there was no long-term follow-up after the intervention to establish whether benefits are sustained, although this has been confirmed by other studies using these educational materials [[26], [27], [28]]. Having a control group, blinding and multiple assessments, and including other CR models (e.g. onsite and virtual) and outcomes (e.g. functional capacity and motivation) should serve as the basis for future research. Second, generalizability of the findings is limited by some selection and retention biases in the sample. Most of the educational materials were only available online and not all patients have equal internet access at home. It is unknown how generalizable this intervention and the effects would be to other CR programs in Spain, as well as among Spanish-speaking patients attending other hybrid CR models around the world. Third, physical activity was assessed using wearable activity tracking devices and although participants were recommended to wear the activity tracker all day and to take it off only on specific occasions (e.g., while showering), it was not possible to supervise the wearing time. Fourth, the MDS tool used to assess adherence to the Mediterranean diet was not psychometrically validated to Spanish at the time of the research. Finally, due to restrictions imposed by the pandemic, it was not possible to collect data from our original target of 84 participants. However, our sample size was very close (n = 82; 98%).
4.2. Innovation
The COVID-19 pandemic has accelerated the need for patient education materials in CR, which in some programs was the only resource available to support patients during this delicate time [16]. Although there are numerous educational resources available for patients enrolled in CR programs, Cardiac CollegeTM is the only evidence-based, freely available and culturally adapted to people living in Spain. This intervention is comprised of multiple materials that can accommodate patient needs, learning preferences, health literacy levels, and learning abilities/limitations. Results from this pilot study have provided preliminary results that this innovative education intervention can be used in CR programs in Spain.
4.3. Conclusion
This pilot study provides preliminary results about the importance of structured education for patients attending CR programs in Spain. Significant increases in disease-related knowledge and health behaviors in patients attending hybrid models of CR are encouraging results that support the value of implementing comprehensive educational initiatives to CR programs in Spain. In addition, although more research is needed, the fact that this study happened during the first wave of the COVID-19 pandemic in one of the hardest-hit countries and that participants improved their outcomes and were satisfied amidst restrictions show that these educational interventions are valuable and should be made accessible to patients.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank all the participants who have contributed to the realization of this project.
We would also like to thank the entire cardiac rehabilitation team at Gregorio Marañón General University Hospital who participated in the study (physical medicine and rehabilitation physicians, cardiologists, nurses, psychologists and physiotherapists) for their help in translation, educational talks and other participations in this project.
Footnotes
This work has not been previously presented. The authors have no disclaimers.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2022.100054.
Appendix A. Supplementary data
Supplementary material
References
- 1.Vos T., Lim S.S., Abbafati C., Abbas K.M., Abbasi M., Abbasifard M., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timmis A., Townsend N., Gale C.P., Torbica A., Lettino M., Petersen S.E., et al. European society of cardiology: cardiovascular disease statistics 2019. Eur Heart J. 2020;41:12–85. doi: 10.1093/eurheartj/ehz859. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D., Benjamin E.J., Go A.S., Arnett D.K., Blaha M.J., Cushman M., et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 4.Bueno H., Pérez-Gómez B. Global rounds: cardiovascular health, disease, and care in Spain. Circulation. 2019;140:13–15. doi: 10.1161/CIRCULATIONAHA.119.038714. [DOI] [PubMed] [Google Scholar]
- 5.World Bank Life Expectancy at Birth in Spain, 1960-2019. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=ES (10 January 2022)
- 6.Billari F.C., Kohler H.P. Patterns of low and lowest-low fertility in Europe. Popul Stud (Camb) 2004;58:161–176. doi: 10.1080/0032472042000213695. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Alvarez E., Lanborena N., Borrell L.N. Cardiovascular disease risk factors in Spain: A comparison of native and immigrant populations. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lennon R.P., Claussen K.A., Kuersteiner K.A. State of the heart: an overview of the disease burden of cardiovascular disease from an epidemiologic perspective. Prim Care. 2018;45:1–15. doi: 10.1016/j.pop.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Buckley B.J.R., de Koning I.A., Harrison S.L., Fazio-Eynullayeva E., Underhill P., Kemps H.M.C., et al. Exercise-based cardiac rehabilitation vs. percutaneous coronary intervention for chronic coronary syndrome: impact on morbidity and mortality. Eur J Prev Cardiol. 2022;29(7):1074–1080. doi: 10.1093/eurjpc/zwab191. [published online: November 11, 2021] [DOI] [PubMed] [Google Scholar]
- 10.Dibben G., Faulkner J., Oldridge N., Rees K., Thompson D.R., Zwisler A.D., et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2021;11 doi: 10.1002/14651858.CD001800.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor R.S., Dalal H.M., McDonagh S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol. 2022;19(3):180–194. doi: 10.1038/s41569-021-00611-7. [published online: September 16, 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehra V.M., Gaalema D.E., Pakosh M., Grace S.L. Systematic review of cardiac rehabilitation guidelines: Quality and scope. Eur J Prev Cardiol. 2020;27:912–928. doi: 10.1177/2047487319878958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabboul N.N., Tomlinson G., Francis T.A., Grace S.L., Chaves G., Rac V., et al. Comparative Effectiveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J Clin Med. 2018;7:514. doi: 10.3390/jcm7120514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turk-Adawi K., Supervia M., Lopez-Jimenez F., Pesah E., Ding R., Britto R.R., et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine. 2019;13:31–45. doi: 10.1016/j.eclinm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abreu A., Pesah E., Supervia M., Turk-Adawi K., Bjarnason-Wehrens B., Lopez-Jimenez F., et al. Cardiac rehabilitation availability and delivery in Europe: How does it differ by region and compare with other high-income countries?: Endorsed by the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2019;26:1131–1146. doi: 10.1177/2047487319827453. [DOI] [PubMed] [Google Scholar]
- 16.Ghisi G.L.M., Xu Z., Liu X., Mola A., Gallagher R., Babu A.S., et al. Impacts of the COVID-19 pandemic on cardiac rehabilitation delivery around the world. Glob Heart. 2021;16:43. doi: 10.5334/gh.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.One World in Data COVID-19 Cases in Spain. https://ourworldindata.org/ (10 January 2022)
- 18.Clark R.A., Conway A., Poulsen V., Keech W., Tirimacco R., Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015;22:35–74. doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 19.Babu A.S., Arena R., Ozemek C., Lavie C.J. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol. 2020;36:792–794. doi: 10.1016/j.cjca.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang R., Morris N.R., Mandrusiak A., Bruning J., Peters R., Korczyk D., et al. Cost-utility analysis of home-based telerehabilitation compared with centre-based rehabilitation in patients with heart failure. Heart Lung Circ. 2019;28:1795–1803. doi: 10.1016/j.hlc.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Jin K., Khonsari S., Gallagher R., Gallagher P., Clark A.M., Freedman B., et al. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2019;18:260–271. doi: 10.1177/1474515119826510. [DOI] [PubMed] [Google Scholar]
- 22.de Melo Lima, Ghisi G., Pesah E., Turk-Adawi K., Supervia M., Lopez Jimenez F., et al. Cardiac rehabilitation models around the globe. J Clin Med. 2018;7(9) doi: 10.3390/jcm7090260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Besnier F., Gayda M., Nigam A., Juneau M., Bherer L. Cardiac rehabilitation during quarantine in COVID-19 pandemic: challenges for center-based programs. Arch Phys Med Rehabil. 2020;101:1835–1838. doi: 10.1016/j.apmr.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leochico C.F.D., Espiritu A.I., Ignacio S.D., Mojica J.A.P. Challenges to the emergence of telerehabilitation in a developing country: a systematic review. Front Neurol. 2020;11:1007. doi: 10.3389/fneur.2020.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cartledge S., Rawstorn J.C., Tran M., Ryan P., Howden E.J., Jackson A. Telehealth is here to stay but not without challenges: a consultation of cardiac rehabilitation clinicians during COVID-19 in Victoria, Australia. Eur J Cardiovasc Nurs. 2021 doi: 10.1093/eurjcn/zvab118. [published online: December 22, 2021] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghisi G.L.M., Rouleau F., Ross M.K., Dufour-Doiron M., Belliveau S.L., Brideau J.R., et al. Effectiveness of an education intervention among cardiac rehabilitation patients in canada: a multi-site study. CJC Open. 2020;2:214–221. doi: 10.1016/j.cjco.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghisi G.L.M., Chaves G.S.S., Ribeiro A.L., Oh P., Britto R.R., Grace S.L. Comprehensive cardiac rehabilitation effectiveness in a middle-income setting: a randomized controlled trial. J Cardiopulm Rehabil Prev. 2020;40:399–406. doi: 10.1097/HCR.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 28.Ghisi G.L.M., Grace S.L., Anchique C.V., Gordillo X., Fernandez R., Quesada D., et al. Translation and evaluation of a comprehensive educational program for cardiac rehabilitation patients in Latin America: A multi-national, longitudinal study. Patient Educ Couns. 2021;104:1140–1148. doi: 10.1016/j.pec.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xia L., Ghisi G.L.M., Meng S., Grace S.L., Shi W., Zhang L., et al. Establishing a process to translate and adapt health education materials for natives and immigrants: the case of Mandarin adaptations of cardiac rehabilitation education. Heart Lung. 2021;50:794–817. doi: 10.1016/j.hrtlng.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Ghisi G.L.M., Scane K., Sandison N., Maksymiu S., Skeffington V., Oh P. Development of and educational curriculum for cardiac rehabilitation patients and their families. J Clin Ex Cardiol. 2015;6:5. [Google Scholar]
- 31.Wild D., Grove A., Martin M., Eremenco S., McElroy S., Verjee-Lorenz A., et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 32.Yorkston K.M., Bourgeois M.S., Baylor C.R. Communication and aging. Phys Med Rehabil Clin N Am. 2010;21:309–319. doi: 10.1016/j.pmr.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghisi G.L.M., Fernandez R., Quesada D., Anchique C.V., Gordillo X., Loaiciga B.A., et al. Translation, adaptation, and psychometrically validation of an instrument to assess disease-related knowledge in Spanish-speaking cardiac rehabilitation participants: The Spanish CADE-Q SV. Heart Lung. 2021;50:129–135. doi: 10.1016/j.hrtlng.2020.07.016. [DOI] [PubMed] [Google Scholar]
- 34.Haun J., Luther S., Dodd V., Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun. 2012;17:141–159. doi: 10.1080/10810730.2012.712615. [DOI] [PubMed] [Google Scholar]
- 35.Rawson K.A., Gunstad J., Hughes J., Spitznagel M.B., Potter V., Waechter D., et al. The METER: a brief, self-administered measure of health literacy. J Gen Intern Med. 2010;25:67–71. doi: 10.1007/s11606-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weiss B.D., Mays M.Z., Martz W., Castro K.M., DeWalt D.A., Pignone M.P., et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tudor-Locke C., Craig C.L., Aoyagi Y., Bell R.C., Croteau K.A., De Bourdeaudhuij I., et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8:80. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghisi G.L.M., Mahajan A., da Silva Chaves G.S., Rouse V., Brum M., Ajwani F., et al. Validation of a self-administered version of the Mediterranean diet scale (MDS) for cardiac rehabilitation patients in Canada. Int J Food Sci Nutr. 2019;70:202–211. doi: 10.1080/09637486.2018.1486392. [DOI] [PubMed] [Google Scholar]
- 39.Bandura A. Information Age Publishing; Greenwich: 2006. Guide for constructing self-efficacy scales; pp. P307–P337. [Google Scholar]
- 40.Chen S.Y., Feng Z., Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis. 2017;9:1725–1729. doi: 10.21037/jtd.2017.05.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dawkes S., Hughes S., Ray S., Nichols S., Hinton S., Roberts C., et al. COVID-19 and cardiac rehabilitation: joint BACPR/BCS/BHF statement on cardiac rehabilitation services. Brit J Cardiol. 2020;27:50. doi: 10.5837/bjc.2020.019. [published online: June 1, 2020] [DOI] [Google Scholar]
- 42.Scherrenberg M., Wilhelm M., Hansen D., Völler H., Cornelissen V., Frederix I., et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020 doi: 10.1177/2047487320939671. 2047487320939671, [published online ahead of print, 2020 Jul 2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mureddu G.F., Ambrosetti M., Venturini E., La Rovere M.T., Mazza A., Pedretti R., et al. Cardiac rehabilitation activities during the COVID-19 pandemic in Italy. Position Paper of the AICPR (Italian Association of Clinical Cardiology, Prevention and Rehabilitation) Monaldi Arch Chest Dis. 2020;90 doi: 10.4081/monaldi.2020.1439. [DOI] [PubMed] [Google Scholar]
- 44.American Association of Cardiovascular Prevention and Rehabilitation (AACVPR) Returning With Care. 2020. http://www.aacvpr.org/covid19/reopening (10 January 2022)
- 45.Canadian Association of Cardiovascular Prevention and Rehabilitation (CACPR) CACPR Statement for COVID-19. 2020. https://cacpr.wildapricot.org/resources/Documents/CACPR%20Statement%20for%20Covid%20-%20final%20full%20-%20logo.pdf (10 January 2022)
- 46.Ghisi G.L.M., Chaves G.S.D.S., Britto R.R., Oh P. Health literacy and coronary artery disease: a systematic review. Patient Educ Couns. 2018;101(2):177–184. doi: 10.1016/j.pec.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 47.Dunn P., Conard S. Improving health literacy in patients with chronic conditions: A call to action. Int J Cardiol. 2018;273:249–251. doi: 10.1016/j.ijcard.2018.08.090. [DOI] [PubMed] [Google Scholar]
- 48.Rudd R.E. The evolving concept of Health literacy: New directions for health literacy studies. J Commun Healthc. 2015;8:7–9. [Google Scholar]
- 49.Chiu H.T., Tsai H.W., Kuo K.N., Leung A.Y.M., Chang Y.M., Lee P.H., et al. Exploring the influencing factors of health literacy among older adults: a cross-sectional survey. Medicina (Kaunas) 2020;56:330. doi: 10.3390/medicina56070330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ritchey M.D., Maresh S., McNeely J., Shaffer T., Jackson S.L., Keteyian S.J., et al. Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.119.005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material