SUMMARY
The child day-care centre (DCC) is often considered as one risk factor for gastroenteritis (GE) rather than a complex setting in which the interplay of many factors may influence the epidemiology of GE. This study aimed to identify DCC-level risk factors for GE and major enteropathogen occurrence. A dynamic network of 100 and 43 DCCs participated in a syndromic and microbiological surveillance during 2010–2013. The weekly incidence of GE events and weekly prevalence of five major enteropathogens (rotavirus, norovirus, astrovirus, Giardia lamblia, Cryptosporidium hominis/parvum) were modelled per DCC using mixed-effects negative binomial/Poisson regression models. Sixteen hundred children were surveyed up to 3 years, during which 1829 GE episodes were reported and 5197 faecal samples were analysed. Identified risk factors were: large DCC capacity, crowding, having animals, nappy changing areas, sandpits, paddling pools, cleaning potties in normal sinks, cleaning vomit with paper towels (but without cleaner), mixing of staff between child groups, and staff members with multiple daily duties. Protective factors were: disinfecting fomites with chlorine, cleaning vomit with paper towels (and cleaner), daily cleaning of bed linen/toys, cohorting and exclusion policies for ill children and staff. Targeting these factors may reduce the burden of DCC-related GE.
Key words: Epidemiology, gastroenteritis, gastrointestinal infections, paediatrics, public health
INTRODUCTION
Child day-care centres (DCCs) represent crowded facilities with a high in- and out-flow of children that are immunologically immature, have limited toilet training and understanding of hygiene behaviours. These characteristics may facilitate circulation of infectious agents in the DCC environment, including those with the ability to cause gastroenteritis (GE). These agents are transmitted either directly via person-to-person contact between children/staff members or indirectly via contact with a contaminated environment, including inanimate objects (fomites) such as communal toys and other classroom objects, water or food. Numerous studies, mainly from the United States, Scandinavian countries and The Netherlands, have consistently shown that children cared for at a DCC are at increased risk of acquiring GE compared to children cared for at home [1]. Such increased risk constitutes an important cause of childhood morbidity, rivalling that of acute respiratory infections [1], which impacts on parents and caregivers as it causes significant societal costs via increased expenditures on healthcare services for care and treatment [2].
There has been consensus since 1986 on the need to study the epidemiological characteristics of DCCs in order to design effective intervention programmes that limit the implications of DCC-associated GE, both for the child and society [3]. Yet, most studies on risk factors for diarrhoeal illness in DCCs do not focus on factors associated with the DCC setting itself, but rather on factors related to the attending child and their household environments. These studies therefore consider the DCC as an ‘abstract’ risk factor rather than a complex setting in which the interplay of many factors influences the occurrence of GE. There are also studies focusing on outbreaks at DCCs [4]. However, risk factors associated with transmission of enteropathogens during outbreaks might differ from those associated with the occurrence of the majority of DCC-related GE events, which are of sporadic and mild nature.
To our best knowledge, the only other investigation that has involved a long-term prospective evaluation of GE illness in DCCs was carried out in Iceland [5], where child-care practices are markedly different from The Netherlands. In The Netherlands, child-care services are utilized for an average of 2·5 days per week, reflecting the high level of part-time employment of parents, whereas in Iceland child-care services are mainly provided full time. Similar to an Australian study on diarrhoeal outbreaks at DCCs [4] the Icelandic study did not identify risk factors related to DCC characteristics themselves. Finally, studies have not yet explored specific DCC-related risk factors for circulating enteropathogens. The fact that DCC characteristics could increase the risk for GE episodes to occur in the attending child population has not been formally studied leaves the majority of recommendations in current international guidelines for infection control in DCCs as expert- rather than evidence-based [6].
Here we focus our attention on the characteristics of the Dutch DCC environment, and the interaction between these characteristics, in order to identify (general and pathogen-specific) putative risk factors for GE in their child population in order to gain knowledge essential for reducing the burden of DCC-associated GE. These characteristics included DCCs' socio-demographics, facility design, and policies for hygiene and disease control. Besides GE as a whole, risk factors for the prevalence of the enteropathogens rotavirus, norovirus, astrovirus, Giardia lamblia, and Cryptosporidium hominis were investigated, as these enteropathogens have been identified as significant contributors to GE in DCCs in a previous study [7]. To this end, we used data from the KIzSS network, which encompasses 100 DCCs participating in infectious disease surveillance in The Netherlands from 2010 to 2013.
METHODS
Participants
In The Netherlands, there are two major types of formal out-of-home child-care facilities that provide government-regulated, paid, non-custodial care for children aged 0–4 years: the day-care centre (DCC) and the day-care home. Day-care homes care for 1–6 children, whereas DCCs provide care for >5 and up to a few hundred children. In this study, we focus on DCCs. A DCC is usually open from 07:30 to 18:00 hours on weekdays, although some also provide care during the weekends. Although a DCC often provides full-time services, the majority of children attend the DCC for only 2 or 3 days per week, which is reflected in the high level of part-time employment of Dutch parents [8]. Only 4% of Dutch children have formal arrangements for more than 30 h per week [8]. In March 2010, 2011 and 2012, all DCCs registered in the Dutch national database maintained by the Ministry of Social Affairs and Employment in The Netherlands were invited to participate in a dynamic DCC network for the surveillance of GE in their child populations. A detailed description of the DCC network design, methodology and definitions is reported in a previous open-access article [9].
Study design
Syndromic surveillance network
Surveillance started in March 2010 and ended in March 2013 (3 years). Two types of data were collected. First, DCCs used study-designed calendars to indicate the daily occurrence of pre-defined GE episodes in their 0- to 4-year-old population that resulted in ⩾1 days of absence from the DCC (incidence numerator). DCCs were also asked to report the total number of attending children per week (incidence denominator). Incidence numerators and denominators were reported by DCCs via a web-based registration tool to the Dutch National Institute for Public Health and the Environment (RIVM) [10]. This tool enabled two-way communication between each DCC and the RIVM's research team for sending periodic reminders to the DCCs to submit their reports as well as to clarify and/or amend incomplete or inconsistent reports. Children were reported as ill either by their respective parents/caregivers or by the DCC staff if the children became ill at the DCC. We defined an episode of GE as an acute onset of ⩾3 episodes of watery stools per day or an acute onset of ⩾3 episodes of vomiting per day. A child had to be fully recovered for at least 7 days before being reported ill again. As children do not attend DCCs every day of the week, we adjusted for GE episodes missed due to children becoming ill and recovering during days of scheduled non-attendance at DCCs, as reported elsewhere [1]. Weeks in which a DCC reported the number of children attending the DCC during that week, but did not report the corresponding number of GE episodes observed during that week, were considered free from GE for that week. Weeks in which a DCC did not report either the number of attending children or the corresponding number of GE episodes were treated as missing observations and were not considered further.
Laboratory surveillance network
A subset of DCCs were instructed to take one faecal sample from 10 randomly chosen children each month (one sample per child), regardless of whether or not these children experienced gastrointestinal symptoms at the time of sampling and regardless of the size of the DCC. Repeated sampling of the same child within the same month was not allowed. All faecal samples were tested for the presence of 16 enteropathogenic bacteria, viruses and parasites using multiple, internally controlled, quantitative real-time multiplex polymerase chain reactions. Enteropathogens tested were: (1) viruses: adenovirus (enteropathogenic types 30 and 40/41), astrovirus, norovirus, rotavirus and sapovirus. (2) Bacteria: Salmonella enterica, Campylobacter jejuni, Shiga toxin-producing Escherichia coli (STEC), Shigella spp./enteroinvasive Escheria coli (EIEC), Clostridium difficile, enteroaggregative E. coli (EAEC), typical and atypical enteropathogenic E. coli (EPEC) and Yersinia enterocolitica. (3) Parasites: Cryptosporidium hominis/parvum, Dientamoeba fragilis and G. lamblia. As a previous study based on the same dataset used here showed that only rotavirus, norovirus, astrovirus, G. lamblia and C. hominis/parvum were those associated with GE incidence in DCC attendees [7], we considered here only these five pathogens. Together, these enteropathogens accounted for 39% of GE incidence experienced by children in DCCs (11% by rotavirus, 10% by norovirus, 8% by G. lamblia, 7% by astrovirus, 3% by C. hominis), whereas none of the bacterial enteropathogens were significantly associated with GE incidence [7]. For a detailed description of the laboratory analyses performed, we referred to a previous paper [9].
Risk factors and definitions; socio-demographics, facility design and policies for disease control
At enrolment in the network, all DCCs were asked to complete a retrospective questionnaire regarding three major categories of characteristics: socio-demographics, facility design and policies for hygiene and disease control. Questions regarding socio-demographics included the socioeconomic status, degree of urbanization, average number of enrolled staff members and children per week, group structure arrangements, child/staff ratio and crowding. The socioeconomic status was expressed as a normalized score (−4 to +4) based on income, employment and educational level per postal code area; a high score indicating a low socioeconomic status. The degree of urbanization was categorized by addresses per km2 as ‘highly urbanized’ (>2000 addresses/km2), ‘urbanized’ (1500–2000), ‘moderately urbanized’ (1000–1500), ‘lowly urbanized’ (500–1000) and ‘rural’ (<500). Group structure arrangements referred to whether the child groups of a DCC were organized either horizontally (children of a child group are of similar age; 0–2 or 2–4 years), vertically (children of a child group are of dissimilar age), or both. The child/staff ratio was defined as the average weekly number of employed staff members divided by the average weekly number of attending children. Crowding was expressed as the inverse of the ratio between the maximum number of DCC-attending children per day and the overall DCC capacity times 100. Facility set-up addressed questions about the presence (yes/no) of indoor and outdoor sandpits and paddling pools, child toilets/sinks, nappy changing areas, paper towels, and farm and pet animals. Hygiene and disease control policies were assessed by asking questions about hand-washing behaviours of staff and children (expressed as ‘always’ washing hands before food preparation, before and after eating, after changing nappy, or after toilet visit, vs. ‘sometimes/never’ doing so), mixing of staff members and child groups during the day (yes/no) and cleaning frequency of DCC toilets, kitchens, toys and beds (more or less frequent than daily). Finally, we asked DCCs about their exclusion and cohorting policies during a GE outbreak. Questions included whether staff or children were prevented from entering the DCC upon presentation of gastrointestinal symptoms (yes/no), whether children were assigned to separate toilets when ill (yes/no), whether staff where allowed to mix in different child groups (yes/no), whether toys were cleaned more often during outbreaks (yes/no) and whether public health authorities were notified in case of a suspected outbreak (yes/no).
Statistical analysis
We modelled the weekly number of GE episodes per DCC (outcome variable) using mixed-effects negative binomial regression models. These models included a random effect at the level of DCC to account for any clustered or serial non-independency in the data due to the repeated measurements made over time on the same DCCs. The underlying population at risk, i.e. the weekly total number of children attending the DCC, was included in the models as an offset term.
First, we assessed the association of each putative risk factor with GE occurrence in a baseline model together with confounders, including the socioeconomic status and degree of urbanization of the DCCs, as well as the season and year of surveillance. Season was categorized as spring (March 21 to June 21); summer (June 21 to September 21); autumn (September 21 to December 21) and winter (December 21 to March 21). Finally, years were defined as the periods between 21 March 2010 to 21 March 2011; 21 March 2011 to 21 March 2012 and 21 March 2012 to 21 March 2013. Next, all factors showing a P value ⩽0·1 in the ‘single-variable’ models were selected for inclusion in a multivariable model. A manual backward stepwise selection procedure was applied, dropping variables one by one starting from the one with the largest non-significant P value and then adding back all dropped variables if they later appeared to be significant. In addition, the effect of removing and adding variables on the associations of the other variables included in the model was monitored. Variables with a P value <0·05 were retained in the final model. Associations were expressed as adjusted incidence rate ratios (aIRRs) and corresponding 95% confidence intervals (95% CIs). After establishing the main model, all plausible two-way interactions between the significant factors, including the control variables (season, degree of urbanization, etc.), were tested for significance. The final model was therefore expanded to include the significant interaction terms, if present. The same analytical procedure was applied in the pathogen-specific analysis. In this analysis, we modelled the weekly number of positive samples for rotavirus, norovirus, astrovirus, G. lamblia and C. hominis/parvum, with the total number of tested samples being the offset term. Mixed-effects Poisson, rather than negative binomial, regression models were used to model these pathogens as the over-dispersion parameter alpha was not significantly different from zero in any of the pathogen-specific models, indicating that the Poisson distribution was appropriate.
The models assessed whether the estimated weekly GE incidence and enteropathogen prevalence was significantly lower or higher in DCCs with specific characteristics. The multivariate shared relationships between the significant risk factors and the occurrence of the five enteropathogens were explored altogether using canonical correlation analysis (CCA). CCA is a multivariate exploratory statistical method that allows for the combined analysis of linear interrelationships between two sets of variables, which in our study were the obtained significant risk factors and the five series of enteropathogen-positive samples. The plot of the first variate (on the horizontal axis) and the second variate (on the vertical axis) visualizes the position of DCCs according to their common risk variable groupings and enteropathogen occurrences [11]. While the regression analysis in this study was used to formally test the ‘many-to-one’ associations between the risk factors and (each) pathogen prevalence at a time, CCA was used to corroborate whether these associations where consistent when using a ‘many-to-many’ approach, i.e. when relating all risk factors with all pathogens together. As only ten faecal samples were collected per DCC per month, our study could not differentiate between enteropathogens that were introduced in the DCC (but not transmitted within the DCC environment) and enteropathogens that were transmitted within the DCC environment itself. This was particularly true for those DCCs and weeks in which a given enteropathogen was detected only once.
Ethical statement
The Dutch Central Committee on Research involving Human Subjects in Utrecht, The Netherlands, gave permission to conduct this study (protocol no.: 09–196/C). Given that limited subject-identifiable data were generated and the surveillance activities implied no risk or burden for any individuals, the committee judged that no specific ethical permission was required for institutional or individual consent. Although not required, parents or caregivers of children attending the participating DCCs were informed by letter about the purpose and design of the study and a form was attached so that parents could return it if they did not want to let their children participate to the study.
RESULTS
Participation rate and population at risk
One hundred DCCs participated in the syndromic surveillance, of which 43 DCCs also participated in the microbiological surveillance. The average participation rate, defined as the number of DDCs that reported at least the incidence denominator each week and/or submitted faecal samples compared to the total number of participating DCCs, was over 80% for both surveillance networks. A median population of 1600 children per week was followed in the network during the study period, during which 1829 GE episodes were reported (Table 1). In 990 out of 5197 tested faecal samples, rotavirus, norovirus, astrovirus, G. lamblia and/or C. hominis/parvum were detected (Table 2). Depending on the enteropathogen in question, the weekly probability of not detecting the enteropathogen per DCC ranged from 74·6% (norovirus) to 96·6% (C. hominis/parvum). The weekly probability of detecting an enteropathogen once ranged from 2·4% (C. hominis/parvum) to 14·2% (norovirus), whereas the weekly probability of detecting an enteropathogen twice or more ranged from 1·0% (C. hominis/parvum) to 11·2% (norovirus, Table 3).
Table 1.
Denominator characteristics of the syndromic surveillance component of the Dutch day care-based surveillance system (2010–2013, 100 day-care centres)
| Cases | Population size mean/week (2·5–97·5 percentiles) | Incidence mean/1000 child-years (2·5–97·5 percentiles) | ||
|---|---|---|---|---|
| Study year | Total | Mean/week (2·5–97·5 percentiles) | ||
| 2010–2011 | 483 | 9 (8–11) | 1435 (1333–1 536) | 360 (290–430) |
| 2011–2012 | 517 | 10 (8–12) | 1279 (1221–1 338) | 399 (331–467) |
| 2012–2013 | 829 | 16 (14–18) | 2125 (1969–2 280) | 411 (356–468) |
| Mean/year | 610 | 12 (10–14) | 1613 (1553–1 770) | 389 (53–427) |
Table 2.
Denominator characteristics of the laboratory surveillance component of the Dutch day-care-based surveillance system (2010–2013, 43 day-care centres)
| Samples | ||
|---|---|---|
| Study year | Total | Mean/week (2·5–97·5 percentiles) |
| 2010–2011 | 1914 | 40 (38–42) |
| 2011–2012 | 1739 | 37 (35–38) |
| 2012–2013 | 1544 | 33 (31–34) |
Table 3.
Prevalence characteristics of the five enteropathogens detected during laboratory surveillance (2010–2013, 43 DCCs)
| Enteropathogens | Total no. of detections | Average probability of detection per week and DCC | Average probability of detecting 0 per week and DCC | Average probability of detecting 1 per week and DCC | Average probability of detecting >1 per week and DCC |
|---|---|---|---|---|---|
| Rotavirus | 175 | 10·6 (8·6–12·5) | 89·4 (87·5–91·3) | 6·9 (5·3–8·5) | 3·7 (2·5–4·8) |
| Norovirus | 504 | 25·4 (22·6–28·0) | 74·6 (71·2–77·3) | 14·2 (12·0–16·4) | 11·2 (7·2–13·1) |
| Astrovirus | 150 | 8·4 (6·7–10·1) | 91·6 (89·9–93·3) | 5·6 (4·1–7·0) | 2·8 (1·8–3·9) |
| Giardia lamblia | 225 | 16·0 (13·7–18·3) | 84·0 (81·7–86·3) | 11·4 (9·5–13·4) | 4·6 (3·3–5·9) |
| Cryptosporidium hominis | 45 | 3·4 (2·3–4·6) | 96·6 (95·4–97·7) | 2·4 (1·4–3·4) | 1·0 (0·4–1·6) |
DCC, Day-care centre.
Values given are % (95% confidence intervals).
Risk factors for GE and enteropathogens
The main characteristics of the participating DCCs are shown in Table 4 together with the results of the regression models.
Table 4.
Characteristics of day-care centres (DCCs) participating in the surveillance network. Adjusted incidence rate rations (aIRRs) represent the associations between DCC characteristics and the occurrence of gastroenteritis, rotavirus, norovirus, astrovirus, G. lamblia and C. hominis in DCC attendees
| % DCCs with specific characteristicsa or their median valuesb (95% CI) | Gastroenteritis aIRRc (95% CI) | Rotavirus aIRRc (95% CI) | Norovirus aIRRc (95% CI) | Astrovirus aIRRc (95% CI) | G. lamblia aIRRc (95% CI) | C. hominis aIRRc (95% CI) | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Median DCC capacity (no. of children) | 78·8 (12·0–172·0)* | 1·001 (1·001–1·003) | 1·001 (1·001–1·002) | ||||
| Crowding of DCC environment (%)d | 43·1 (35·3–71·4)* | 1·007 (1·006–1·021) | |||||
| Children/staff member ratio | 5·7 (2·4–8·3)* | ||||||
| Mixing of staff members in child groups (%) | 16·5 (15·8–17·3) | 1·8 (1·0–3·6) | |||||
| Vertical child group structure (% DCCs) | 35·7 (47·1–66·9) | ||||||
| Facility design | |||||||
| Presence of sandpit(s) | 59·0 (49·2–68·9) | 1·9 (1·3–2·8) | 3·2 (1·9–5·1) | ||||
| Presence of paddling pool(s) | 30·4 (20·8–39·1) | 1·5 (1·3–1·9) | |||||
| Presence of dedicated child toilet(s) and/or sink(s) | 77·3 (76·2–78·7) | ||||||
| Presence of dedicated nappy-changing area(s) | 37·2 (27·4–46·7) | 2·2 (1·7–2·8) | |||||
| Presence of dedicated clothes washing area(s) | 45·8 (35·0–46·6) | ||||||
| Presence of paper towels | 46·5 (36·1–55·9) | ||||||
| Ownership of animalse | 8·9 (2·65–12·4) | 2·5 (1·2–5·3) | |||||
| In summer | − | 18·2 (8·9–37·4) | |||||
| In spring, autumn or winter | − | 8·4 (4·6–15·6) | |||||
| Staff members with multiple daily duties | 77·6 (68·6–85·4) | 2·7 (1·0–7·7) | |||||
| Policies for disease control | |||||||
| Hand/food hygiene for childrenf | 37·5 (27·6–47·3) | ||||||
| Hand/food hygiene for personnelf | 31·6 (21·8–40·2) | ||||||
| Cleaning with chlorine tablets | 7·0 (2·0–12·1) | 0·1 (0·04–0·3) | |||||
| Cleaning vomit with paper towels and cleanerg | 62·0 (52·3–61·6) | 0·6 (0·4–0·7) | |||||
| Cleaning vomit with paper towels and no cleanerg | 38·0 (47·7–38·4) | 1·3 (1·0–1·6) | |||||
| Cleaning children's potty in normal sink | 29·65 (20·36–38·93) | 1·9 (1·2–3·0) | |||||
| Daily cleaning of | |||||||
| Kitchen | 93·94 (87·27–97·74) | ||||||
| Toilet | 91·58 (84·08–96·29) | ||||||
| Toys | 15·38 (8·67–24·46) | 0·5 (0·2–0·9) | |||||
| Bed linen | 69·47 (59·18–78·51) | 0·7 (0·5–0·9) | |||||
| Measures undertaken during suspected outbreak | |||||||
| Ill children have separate toilet | 12·03 (6·36–20·02) | 0·4 (0·2–0·8) | |||||
| No mixing of staff members | 64·35 (53·78–73·36) | 0·6 (0·5–0·9) | |||||
| Excluding personnel with gastroenteritis | 8·7 (2·5–13·2) | 0·5 (0·4–0·7) | 0·5 (0·3–0·8) | ||||
| Extra cleaning of toys | 69·18 (58·97–77·87) | 0·4 (0·2–0·7) | |||||
| Excluding children with gastroenteritis | 16·4 (4·5–28·1) | 0·4 (0·2–0·6) | |||||
| Notification to local health authorities | 35·1 (25·5–44·5) | 1·7 (1·1–2·7) |
CI, Confidence interval.
Adjusted for year, season, socioeconomic status and degree of urbanization.
Calculated as: [1 – (maximum number of DCC-attending children per day/overall DCC capacity)]×100.
For dummy variables.
For numerical variables.
Present at DCCs: cats, dogs, rabbits, rodents, goats, cows, pigs, horses and birds.
Calculated as the percentage of DCCs that always wash the hands of children/staff before and after eating and after a visit to the toilet.
Compared to cleaning with a cloth.
2·5th and 97·5th percentiles, not 95% CIs.
Risk factors for GE
Five risk factors were associated with a higher incidence of GE in DCC-attending children in the final multivariable model, whereas one factor was associated with a lower GE incidence (Table 4). For each additional child enrolled for day care, the GE incidence increased by 0·1% (aIRR 1·001, 95% CI 1·000–1·003), meaning that if a DCC with whatever number of children enrolled decides on enrolling an additional child, it is expected to experience, on average, a 0·1% significant increase in its GE weekly incidence compared to when it did not have that additional child enrolled, and this is true while holding all other variables included in the model constant. Similarly, for each percent increase in crowding rate of the DCC environment, the GE incidence increased by 0·7% (aIRR 1·007, 95% CI 1·003–1·011). The GE incidence was higher in DCCs with a dedicated nappy-changing area compared to those DCCs without such an area (aIRR 2·2, 95% CI 1·7–2·8). Owning one or more (pet or farm) animals in the DCC was associated with an increase in incidence of GE (aIRR 2·5, 95% CI 1·2–5·3). Cleaning vomit with paper towels (and cleaner), rather than cloth towels, was associated with a decrease in GE incidence (aIRR 0·6, 95% CI 0·4–0·7). Excluding DCC personnel experiencing GE from working was significantly associated with a lower GE incidence (aIRR 0·5, 95% CI 0·4–0·7).
Risk factors for rotavirus
We identified five factors significantly associated with rotavirus occurrence in DCCs; all of which were related to policies for disease prevention and control (Table 4). Mixing of staff members in different child groups was associated with higher rotavirus prevalence (aIRR 1·8, 95% CI 1·0–3·6). Cleaning children's potties in a sink, rather than in a dedicated washing station, was also a risk factor for higher rotavirus prevalence (aIRR 1·9, 95% CI 1·2–3·0), while having a separate toilet for ill children was protective (aIRR 0·4, 95% CI 0·2–0·8). Finally, excluding children with GE symptoms upon entering or during day care was associated with lower rotavirus prevalence (aIRR 0·4, 95% CI 0·2–0·6).
Risk factors for norovirus
With each additional child enrolled in day care, the prevalence of novovirus increased by 0·1% (aIRR 1·001, 95% CI 1·000–1·002). Having indoor or outdoor sandpits and paddling pools was associated with higher prevalence of norovirus in DCCs (aIRR 1·9, 95% CI 1·3–2·8 and aIRR 1·5, 95% CI 1·3–1·9, respectively) (Table 4). Cleaning vomit with paper rather than with cloth towels (but no cleaner) was associated with an increase in norovirus prevalence (aIRR 1·3, 95% CI 1·0–1·6). Cleaning bed linen every day (compared to less often than once a day/cleaning only when visibly contaminated) was associated with lower norovirus prevalence (aIRR 0·7, 95% CI 0·5–0·9).
Risk factors for astrovirus
Only two DCC characteristics were significantly associated with astrovirus occurrence (Table 4). Cleaning toys every day was associated with lower astrovirus prevalence (aIRR 0·5, 95% CI 0·2–0·9). Furthermore, DCCs that always contacted the local public health authorities in case of a suspected GE outbreak had a higher risk of detecting astrovirus (aIRR 1·7, 95% CI 1·1–2·7).
Risk factors for G. lamblia
There was a strong significant interaction between the presence of animals in the DCC and season on the occurrence of G. lamblia: the aIRR was significantly higher in the summer (aIRR 18·21, 95% CI 8·9–37·4) than in the other seasons (aIRR 8·4, 95% CI 4·6–15·3) (Table 4). G. lamblia occurrence was also positively associated with the presence of sandpits (aIRR 3·5, 95% CI 2·0–5·9) in the DCC. Cleaning with chlorine detergents (aIRR 0·1, 95% CI 0·05–0·3), excluding personnel with GE (aIRR 0·5, 95% CI 0·3–0·8), and cleaning toys more often during a suspected GE outbreak (aIRR 0·4, 95% CI 0·3–0·9) were all associated with a lower prevalence of G. lamblia.
Risk factors for C. hominis/parvum
C. hominis/parvum was mainly detected during the autumn of 2012. Typing revealed that all detections were of the anthroponotic C. hominis type. Thus, hereafter we will refer to this pathogen as C. hominis only. Compared to DCCs in which a dedicated group of caregivers was present, DCCs in which staff members had multiple daily duties had a higher occurrence of C. hominis (aIRR 2·6, 95% CI 1·0–7·7)
Canonical correlation analysis
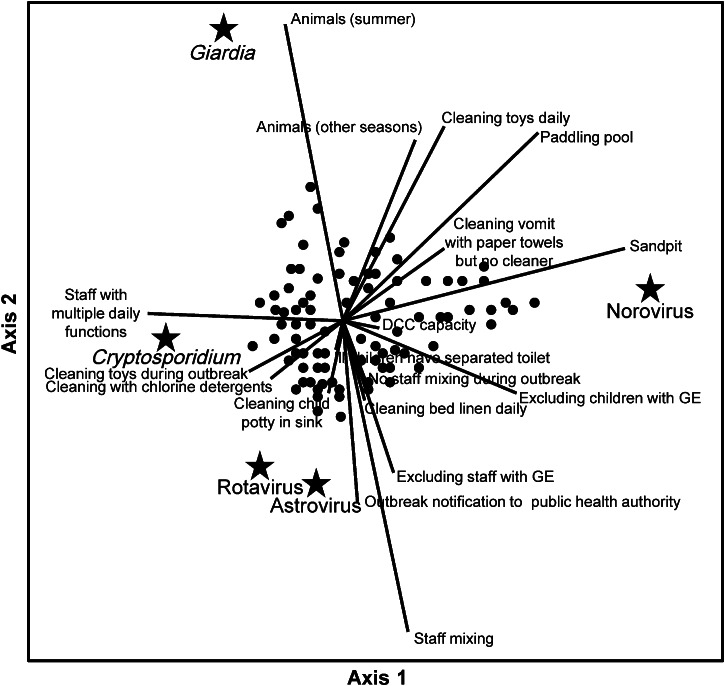
Figure 1 shows the plot of the first vs. the second canonical variate obtained from the CCA. The dots represent the DCCs. Those DCCs positioned in the centre of the plot have the commonest co-occurrence of the five enteropathogens, whereas those DDCs located on the peripheral areas of the plot have specific enteropathogens (i.e. the closest ones) that occur more often than others and risk factors as depicted accordingly. The multivariate-shared relationships of the 17 significant risk factors with the occurrence of the five enteropathogens are depicted as arrows radiating from the centre of the plot and directed to where their correlations with the pathogens are maximal. Figure 1 therefore illustrates that, for instance, higher G. lamblia occurrence in DCC attendees was associated with owning animals especially in summertime, while higher occurrence of C. hominis was associated with DCC staff having multiple daily duties. Outbreak notification to the local health authority and cleaning children's potties in a sink showed an association with higher rotavirus and astrovirus occurrence. Higher norovirus occurrence in DCC attendees was mostly associated with having access to sandpits and paddling pools. The CCA therefore summarized and confirmed all the main associations found in the regression analysis.
Fig. 1.
The first two canonical dimensions of the canonical correlation analysis. Factors significantly associated with rotavirus, norovirus, astrovirus, G. lamblia and C. hominis occurrence in day-care centre (DCC) attendees are represented as arrows directed to where their correlations with the pathogen prevalence are maximal. Adjusted for year, season, socioeconomic status and degree of urbanization. GE, gastroenteritis.
DISCUSSION
This study was performed to identify factors associated with increased/decreased incidence of GE as a whole and with increased/decreased prevalence of specific GE-causing enteropathogens at the DCC level in order to find potential targets for reducing the burden of DCC-related GE.
We report an increase in GE incidence as the overall number of children attending a DCC, as well as its crowding rate, increased. The fact that a child's potential for peer exposure to infectious agents in the DCC setting is largely influenced by the size of the facility and crowding therein has been described before [12]. A densely populated DCC may indeed provide more opportunities for inter-child transmission. Surprisingly, the presence of a dedicated nappy-changing area was significantly associated with increased incidence of GE in DCC attendees. As most children have to pass through these areas several times a day, they could be considered as ‘hubs’ for transmission of enteropathogens if/when they become contaminated; and in every day's routine activities there might be many occasions in which they might become so. Our questionnaire, however, did not cover the cleaning regimens of these nappy-changing areas, or the compliance towards these regimens, to assess whether this ‘hub hypothesis’ is true. Nonetheless, extra care about the hygienic standards of these dedicated areas seems recommendable when a DCC decides on centralizing nappy-changing operations. Previous research found high recovery rates for influenza from such nappy-changing areas [13]. Another peculiarity was the high prevalence of astrovirus if the DCC indicated it always notified the local public health authorities in case of a suspected GE outbreak. A possible explanation is that this ‘risk factor’ merely reflects those DCCs that always seek attention from the local public health authority because they have (had) problems in effectively controlling such infection with their own means. This task is indeed hampered by the fact that astrovirus, in addition to rotavirus and norovirus, can be excreted for several weeks even by immunocompetent children during outbreak situations [14].
Increased DCC capacity was also a specific risk factor for higher norovirus prevalence, further reflecting the high potential for anthroponotic transmission of this virus [6]. Similarly, mixing of staff members between child groups almost doubled rotavirus prevalence. Staff movements between different child groups should, therefore, be minimized as much as possible, particularly during suspected GE outbreaks. Such policies have been recommended for other settings, including hospitals [15], households [16] and nursing homes [17]. Interestingly, we found no relationship between high prevalence of any of the pathogens and the child/staff ratio or structure of the child groups at the DCC. One study observed that a higher child/staff ratio reduces the ability of individual staff to supervise hygiene; thereby increasing a child's exposure to circulating enteropathogens [18]. We did not find such an association in this study, probably because the child/staff ratio is fixed at around four children per staff member in The Netherlands, regardless of the size of the DCC facility.
The zoonotic potential of G. lamblia was reflected by the marked increase in its occurrence in DCC attendees when farm and/or pet animals were kept (for leisure) in or around the DCC. This increase was especially apparent in the summer, when the odds increased by 18-fold compared to not keeping animals at all. This may be due to increased or more substantial contact with these animals during the warm season, especially when kept outdoor. The proportion of G. lamblia infections in DCC attendees that have contact with animals has been described before by several studies, but so far no statistical association has been identified [19]. DCCs should therefore be aware that owning animals might significantly increase a child's exposure to G. lamblia, which may in turn increase the risk of developing GE. C. parvum, like Giardia lamblia, also has zoonotic potential. However, in this study we only found C. hominis, which is a non-zoonotic type, which transmits directly via person-to-person contact or indirectly via water or food. This would explain why C. hominis was not significantly associated with holding animals at the DCC. Banning animals from day care is unnecessary, but our results do suggest that the management of, and interaction with, these animals should be more carefully supervised. Before any recommendation can be made, future studies should better investigate the zoonotic potential of G. lamblia from several types of animals to children attending day care. Such studies should also corroborate whether such zoonotic potential exists within the DCC or rather takes place within the household environment, as parents with fondness for animals might be more prone to enrol their children in DCCs that also have animals. Moreover, G. lamblia assemblages from dogs and cats (D and C) are not infectious for humans, but human assemblages (A and B) are infectious for dogs and cats only, and little is known about the zoonotic potential of G. lamblia types in common DCC pets such as rabbits [20]. Animals like chicken are unlikely to be of importance for zoonotic transmission of G. lamblia or Cryptosporidium spp. since they harbour other subtypes.
Our study indicates that DCCs that had a sandpit or a paddling pool had an increased prevalence of norovirus and G. lamblia. A Japanese survey reported that 68% of sandpits in public parks were contaminated with faecal coliforms [21]. Moreover, playing in sandpits has been identified as a risk factor for infection with other pathogens, such as Yersinia enterocolitica [22], Salmonella enterica [22] and Toxocara [23]. Cleaning the sand with bleach has been proposed as a protective measure, but was concluded to be insufficient to decrease the enteropathogen contamination [24]. It is evident that sandpits can easily become contaminated by animal faeces, especially when situated outdoors, and even by the children themselves in cases of vomiting or faecal accidents. This is particularly relevant for norovirus, as vomit can contain a very high viral load, with production of easily spreadable aerosolized particles. The risk posed by sandpits holds also for paddling pools. Recreational water has indeed been reported to act as a vehicle for (inter-human) transmission of several enteropathogens, including norovirus [25], which is believed to be the single largest cause of waterborne outbreaks. Giardia is also known to be able to survive in water for a long time, especially at lower temperatures [26]. Remarkably, we did not identify the paddling pool as a risk factor for C. hominis, as water is one of the main transmission routes for this enteropathogen. The fact that we only detected C. hominis coincides with an increase of C. hominis in The Netherlands in the summer of 2012 [27]. Conversely, having staff members with multiple daily duties was a risk factor for C. hominis occurrence, suggesting that factors beyond (water) sanitation should be considered for this parasite. Enforcement of adequate hygienic measures and staff training, including covering of sandpits and paddling pools when not in use, are necessary to ensure both sandbox, playground and recreational water safety.
Contaminated hands are an important route of transmission of several enteropathogens and therefore toys might also play a major role as fomites because children frequently put them into their hands and mouths [28]. G. lamblia cysts, for example, can survive on fomites for several days, and have been recovered from chairs and tables in DCCs [29]. This would explain the protective effect of extra cleaning of toys during suspected outbreaks on the lower prevalence of G. lamblia we observed, especially since such protective effect seemed to be further increased if chlorine, in addition to regular cleaner, was used as disinfectant. Inactivation of protozoan parasites on fomites by chlorine is a common and effective process widely employed in the food industry [30] and recommended in many guidelines for disease control in DCCs, including those in The Netherlands. Although cleaning fomites with chlorine seemed to be protective against G. lamblia in DCC attendees, this effect was not observed for norovirus or C. hominis. This might be explained by the fact that both norovirus and C. hominis are highly resilient to chlorine, whereas G. lamblia is not [31].
Rotavirus, norovirus and G. lamblia have been identified as the most common agents involved in GE outbreaks in DCCs [30]. Several control measures for GE outbreaks at DCCs that have been reported by other studies were identified in our study as measures associated with a lower prevalence of certain enteropathogens, including the exclusion of children and personnel with GE from the DCC [32], no mixing of staff [33], and providing children with GE with their own toilet [34]. In The Netherlands, cohorting or exclusion of children with GE is not necessarily part of current infectious disease control policies for DCCs. This is irrespective of whether or not an infectious disease outbreak is suspected. Rather, DCCs usually indicate that they exclude ill children from participating in daily DCC activities [1]. Educating DCCs about the apparent benefits of these exclusion or cohorting policies for the sake of children and the DCC itself might increase their compliance, as education has been proved successful in increasing compliance to hand hygiene routines [35]. However, whether increased compliance also leads to increased effectiveness of reducing GE remains to be seen. Exclusion of ill children from day care poses significant problems to working parents whose absenteeism to care for their ill child may jeopardize employment [32]. Strict DCC exclusion policies might even encourage infected children to be placed elsewhere in the DCC community where the disease control policies are less strict. Furthermore, many infectious agents of GE are excreted prior to onset of clinical symptoms (which provide the criteria for exclusion), or are spread by asymptomatic carriers or by individuals with only mild symptoms [36]. The fact that the previously mentioned outbreak-related control measures seemed to lower the prevalence of some enteropathogens suggests that transmission of these enteropathogens is primarily caused by symptomatic, not asymptomatic cases; even though the latter group can shed enteropathogens over prolonged periods [37].
In this study, reports of proper hand-washing practices of children and DCC staff members were not associated with lower GE incidence, nor with lower prevalence of any of the enteropathogens studied. The absence of this protective effect could have at least three explanations. First, hygiene standards might have been too uniformly high to be explored, although this seems unlikely as only 37·5% of participating DCCs had indeed indicated implementation of washing the hands of children before and after eating and after toilet visits. Second, enteropathogens may also be transmitted via routes other than hands, including fomites. Thus, there may be several circumstances where these ‘alternative’ routes in the DCC pose a higher risk than that which can be prevented by always washing hands compared to not always washing hands. Finally, some prevarication bias cannot be excluded because, for example, a DCC may subconsciously provide answers pleasing to the interviewer or even deliberately misreport their hand hygiene polices [38]. Other hygiene policies were significantly associated with a lower incidence of GE and prevalence of some enteropathogens. These were cleaning children's potties in a dedicated washing basin (rather than in a regular sink), and daily cleaning of bed linen. These practices have self-evident reasons to be beneficial and should therefore be encouraged.
Our study has some limitations. Only 2% of DCCs active in The Netherlands participated to our study. Therefore, even though the representativeness and diversity of the DCC surveillance network was confirmed in an earlier study showing that the variation of KIzSS cohort participants reflected the national variation in DCC characteristics in terms of organization, facility design and hygiene policies very well [1], some selection bias cannot be excluded. For instance, as the participating DCCs were enrolled on a voluntary basis, they could represent a self-selected group of particularly motivated DCCs with generally higher hygienic and managerial standards.
Another limitation of our study is that we used a self-administered questionnaire to monitor DCC risk factors. Although it is unlikely that DCCs would have reported facility characteristics other than those actually in place, it is possible that discrepancies have occurred between the perceived and actual behaviour of some policies, e.g. hand hygiene; especially since the questionnaire might in some instances have been completed by the head of the DCC and not by the actual child caregivers. Such differences have been observed before in other studies [39]. We could not explore directly how hygiene measures at the DCC were actually pursued. In addition, DCC risk factors were assumed constant over the study period, and some of them might well have changed due, for instance, changes in policies or internal renovations.
We had no information on the exposure of children in their home settings. Household characteristics such as income and education level of the parents, number of additional siblings, etc. might be even stronger predictors of GE than the DCC characteristics, and may have even confounded, to some extent, the associations found here. Furthermore, we did not identify common risk factors in our regression analysis for the viruses studied here, even though they seem to share similar modes of transmission. Epidemiologically speaking, this is surprising. It might be that either we detected unique (significant) correlates of these viruses or that we just failed to detect the common factors due to predominantly temporal, rather than spatial (i.e. within the same DCCs), co-increase in prevalence. In this regard, the CCA provided an important advantage as it might best honour the multifactorial reality of pathogen circulation within the DCC setting, with multiple relationships taken at a glance. This provided a general overview of the simultaneous effects of the significant risk factors on the occurrence of the different pathogens, an approach that limits the known inefficiencies of conventional multiple testing (e.g. type-1 error) and variable selection based on statistical significance, and helps overcome problems of multicollinearity. The resulting procedure also provided an indication of the underlying common associations between pathogens and DCC characteristics that may have not passed the formal statistical testing because of marginal significance but still had some valuable predictive information for the pathogens in question. This might be the case of, for instance, rotavirus and astrovirus, which were notably closer to each other than to other pathogens in the CCA space, suggesting that their individual risk exposures are in fact simultaneously contributing to this relationship.
We focused on five enteropathogens that appeared to be significant contributors to GE incidence at DCCs in a previous study [7]. However, as stated earlier, they could explain altogether only 39% of such incidence. It is therefore clear that factors associated with the occurrence of any of these five enteropathogens may not be reflected in the occurrence of GE also, as there are other causes (perhaps of non-infectious origin) that contribute to the remainder of GE incidence. For instance, in the specific case of nappy-changing areas being associated with increased GE incidence, this variable was not significantly associated with increased prevalence of any of the five enteropathogens studied, suggesting that nappy-changing areas would increase GE incidence via enteropathogens other than those shown here.
As faecal samples were obtained from children while they were attending DCC and not from children who were absent because they were ill, selection bias in enteropathogen prevalence estimates has probably occurred. However, our sampling scheme is likely to have detected enteropathogens in the pre- and/or post-symptomatic phase. Indeed, because none of the enteropathogens included in the study were bacterial, these were unlikely to have been eradicated by antimicrobial treatments, so children may have continued to shed them upon re-entering the DCC. Besides, antibiotic treatment of children with GE in The Netherlands is extremely rare, as fewer than 1% of children visiting a general practitioner for GE usually receive an antibiotic treatment [1].
Although DCCs were asked to sample children at random, no formal randomization method was provided to them. Given that sampling was quite labour-intensive and there were constraints on budget and laboratory capacity, the monthly number of submittable samples was limited to 10 per DCC, and DCCs were allowed to decide on their randomization charts, if any; differences between DCCs were then meant to be accounted for by the random effect during analysis. Therefore, while we can state that repeated sampling of the same child within the same month is highly unlikely to have occurred, we cannot exclude the possibility that some samples were collected not completely at random. For instance, it can be speculated that sampling of children still in nappies would be easier than that of children with some toilet training, although children in DCCs rarely defecate directly into the toilet, but rather use potties, which are easier to sample. Thus, although sampling was at random by design, for logistic reasons some convenience sampling might also have occurred during implementation.
Finally, it is worth noting that we estimated the GE incidence and enteropathogen prevalence over a long period of time in DCCs with different characteristics, which allowed us to explore the effect of a comprehensive set of putative risk factors that may provide leads to the control of these enteropathogens within the DCC setting itself. However, our study could not investigate how the DCC characteristics contributed to the actual transmission of these enteropathogens because our sampling scheme did not allow for differentiation between enteropathogens that were introduced in the DCC environment (but not transmitted) and enteropathogens that were transmitted within the DCC environment. Doing so would have required testing all children, personnel, and the local environment within the framework of a pre-/post-intervention setting, studying one or a combination of interventions at a time. In that respect, our study was a compromise between precision and logistic feasibility.
CONCLUSION
This is the first large-scale longitudinal study that explored DCC socio-demographic, facility- and policy-related factors associated with GE incidence as a whole and with the prevalence of specific enteropathogens in DCC attendees. Sixteen hundred children were followed in 100 DCCs for up to 3 years, during which time more than 1800 GE episodes occurred and 5197 faecal samples were analysed. Several risk factors were identified, including high DCC capacity and crowding, owning farm/pet animals, having a dedicated nappy-changing area, presence of sandpits and/or paddling pool, cleaning children's potties in a non-dedicated sink, cleaning vomit with paper towels (but without cleaner), mixing of staff members between different child groups, and allowing staff members to have multiple daily duties. Identified protective factors were cleaning vomit with paper towels and cleaner, using chlorine as disinfectant for fomites, daily cleaning of bed linen and toys, and having formal policies for cohorting and exclusion for ill children and staff. We previously demonstrated that there is ample space for improvement of regular hygiene routines and adherence to disease control [1], and that 39% of the GE in Dutch DCCs could be attributed to the five enteropathogens studied here. Targeting the at-risk characteristics of DCCs identified in this study could, therefore, result in a significant reduction of the burden of DCC-related GE. Our results will prove useful in supporting the ever-present DCC responsibility to provide children with a safe, hygienically sound environment, as explicitly required by Dutch law since 2005.
ACKNOWLEDGEMENTS
The authors thank Jeroen Roelfsema and Sietze Brandes for excellent laboratory assistance and Tizza Zomer for critically reviewing the manuscript and Albert Wong for providing statistical feedback. We also acknowledge the directors and staff in all the participating DCCs, without whom this work would not have been possible.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Enserink R, et al. Infectious disease burden related to child day care in the Netherlands. Pediatric Infectious Disease Journal 2013; 32: e334–340. [DOI] [PubMed] [Google Scholar]
- 2.Friesema IH, et al. Costs of gastroenteritis in the Netherlands, with special attention for severe cases. European Journal of Clinical Microbiology & Infectious Diseases 2012; 31: 1895–1900. [DOI] [PubMed] [Google Scholar]
- 3.Davis JP, Pfeiffer JA. Surveillance of communicable diseases in child day care settings. Reviews of Infectious Diseases 1986; 8: 613–617. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson JK, et al. Prospective study of diarrhoeal outbreaks in child long-daycare centres in western Sydney. Medical Journal of Australia 1995; 163: 137–140. [DOI] [PubMed] [Google Scholar]
- 5.Gudnason T, et al. Does hygiene intervention at day care centres reduce infectious illnesses in children? An intervention cohort study. Scandinavian Journal of Infectious Diseases 2013; 45: 397–403. [DOI] [PubMed] [Google Scholar]
- 6.Janssen A. Prevention of norovirus infection in schools and childcare facilities. Stockholm: European Centre for Disease Control (ECDC), 2012.
- 7.Enserink R, et al. Gastroenteritis attributable to 16 enteropathogens in children attending day care. significant effects of rotavirus, norovirus, astrovirus, Cryptosporidium and Giardia. Pediatric Infectious Disease Journal (in press). [DOI] [PubMed]
- 8.Meulders D, et al. The provision of childcare services – a comparative review of 30 European countries. Brussels: European Commission, 2009.
- 9.Enserink R, et al. The KIzSS network, a sentinel surveillance system for infectious diseases in day care centers: study protocol. BMC Infectious Diseases 2012; 12: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward M, et al. Electronic reporting improves timeliness and completeness of infectious disease notification, The Netherlands, 2003. Eurosurveillance 2005; 10: 27–30. [PubMed] [Google Scholar]
- 11.Härdle W, Simar L. Applied Multivariate Statistical Analysis. Berlin, Heidelberg, Dordrecht and New York: Springer, 2007. [Google Scholar]
- 12.Augustine JM, Crosnoe RL, Gordon R. Early child care and illness among preschoolers. Journal of Health and Social Behavior 2013; 54: 315–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boone SA, Gerba CP. The occurrence of influenza A virus on household and day care center fomites. Journal of Infection 2005; 51: 103–109. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell DK, et al. Virologic features of an astrovirus diarrhea outbreak in a day care center revealed by reverse transcriptase-polymerase chain reaction. Journal of Infectious Diseases 1995; 172: 1437–1444. [DOI] [PubMed] [Google Scholar]
- 15.Chadwick PR, et al. Management of hospital outbreaks of gastro-enteritis due to small roundstructured viruses. Journal of Hospital Infection 2000; 45: 1–10. [DOI] [PubMed] [Google Scholar]
- 16.de Wit MA, Koopmans MP, van Duynhoven YT. Risk factors for norovirus, Sapporo-like virus, and group A rotavirus gastroenteritis. Emerging Infectious Diseases 2003; 9: 1563–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Enserink R, et al. Absence of influenza A(H1N1) during seasonal and pandemic seasons in a sentinel nursing home surveillance network in the Netherlands. Journal of the American Geriatrics Society 2011; 59: 2301–2305. [DOI] [PubMed] [Google Scholar]
- 18.Taylor M, Adams CL, Ellis A. Gatekeepers of health: a qualitative assessment of child care centre staff's perspectives, practices and challenges to enteric illness prevention and management in child care centres. BMC Public Health 2008; 8: 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sagebiel D, et al. Giardiasis in kindergartens: prevalence study in Berlin, Germany, 2006. Parasitology Research 2009; 105: 681–687. [DOI] [PubMed] [Google Scholar]
- 20.Overgaauw PA, et al. Zoonotic parasites in fecal samples and fur from dogs and cats in The Netherlands. Veterinary Parasitology 2009; 163: 115–122. [DOI] [PubMed] [Google Scholar]
- 21.Matsuo J, Nakashio S. Prevalence of fecal contamination in sandpits in public parks in Sapporo City, Japan. Veterinary Parasitology 2005; 128: 115–119. [DOI] [PubMed] [Google Scholar]
- 22.Mughini-Gras L, et al. Risk factors for human salmonellosis originating from pigs, cattle, broiler chickens and egg laying hens: a combined case-control and source attribution analysis. PLoS ONE 2014; 9: e87933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paludo ML, et al. Frequency of Toxocara infection in children attended by the health public service of Maringa, south Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo 2007; 49: 343–348. [DOI] [PubMed] [Google Scholar]
- 24.Carabin H, et al. Effectiveness of a training program in reducing infections in toddlers attending day care centers. Epidemiology 1999; 10: 219–227. [PubMed] [Google Scholar]
- 25.Podewils LJ, et al. Outbreak of norovirus illness associated with a swimming pool. Epidemiology and Infection 2007; 135: 827–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hilfman MM. Giardia in Leningrad [in Dutch]. Nederlands Tijdschrift voor Geneeskunde 1975; 119: 1872. [Google Scholar]
- 27.Fournet N, et al. Simultaneous increase of Cryptosporidium infections in the Netherlands, the United Kingdom and Germany in late summer season, 2012. Eurosurveillance 2013; 18: 3–7. [PubMed] [Google Scholar]
- 28.Weniger BG, et al. Fecal coliforms on environmental surfaces in two day care centers. Applied and Environmental Microbiology 1983; 45: 733–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cody MM, Sottnek HM, O'Leary VS. Recovery of Giardia lamblia cysts from chairs and tables in child day-care centers. Pediatrics 1994; 94: 1006–1008. [PubMed] [Google Scholar]
- 30.Lyman WH, et al. Prospective study of etiologic agents of acute gastroenteritis outbreaks in child care centers. Journal of Pediatrics 2009; 154: 253–257. [DOI] [PubMed] [Google Scholar]
- 31.Tuladhar E, et al. Residual viral and bacterial contamination of surfaces after cleaning and disinfection. Applied and Environmental Microbiology 2012; 78: 7769–7775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson M, et al. Evidence base of incubation periods, periods of infectiousness and exclusion policies for the control of communicable diseases in schools and preschools. Pediatric Infectious Disease Journal 2001; 20: 380–391. [DOI] [PubMed] [Google Scholar]
- 33.Barros AJ, et al. Preventing acute respiratory infections and diarrhoea in child care centres. Acta Paediatrica 1999; 88: 1113–1118. [DOI] [PubMed] [Google Scholar]
- 34.Brady MT. Infectious disease in pediatric out-of-home child care. American Journal of Infection Control 2005; 33: 276–285. [DOI] [PubMed] [Google Scholar]
- 35.Zomer TP, et al. Sociocognitive determinants of observed and self-reported compliance to hand hygiene guidelines in child day care centers. American Journal of Infection Control 2013; 41: 862–867. [DOI] [PubMed] [Google Scholar]
- 36.Pickering LK, et al. Asymptomatic excretion of rotavirus before and after rotavirus diarrhea in children in day care centers. Journal of Pediatrics 1988; 112: 361–365. [DOI] [PubMed] [Google Scholar]
- 37.Sukhrie FH, et al. Nosocomial transmission of norovirus is mainly caused by symptomatic cases. Clinical Infectious Diseases 2012; 54: 931–937. [DOI] [PubMed] [Google Scholar]
- 38.Hiebert R, Nordin M. Methodological aspects of outcomes research. European Spine Journal 2006; 15 (Suppl. 1): S4–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O'Boyle CA, Henly SJ, Larson E. Understanding adherence to hand hygiene recommendations: the theory of planned behavior. American Journal of Infection Control 2001; 29: 352–360. [DOI] [PubMed] [Google Scholar]