SUMMARY
Cryptosporidium infects millions of people worldwide causing acute gastroenteritis, but despite its remarkable epidemiological and economic impact, information on the epidemiological trends of human cryptosporidiosis is still scarce in most countries. Here we investigate a panel of 486 cases collected in Galicia (NW Iberian Peninsula) between 2000 and 2008, which sheds new light on the epidemiology in this region of the South Atlantic European façade. Incidence rates in Galicia are one order of magnitude higher than those reported in other regions of Spain, suggesting that this parasite remains largely underdiagnosed in this country, and are also larger than those typical of other European countries with available data. Two species dominate our dataset, Cryptosporidium hominis (65%) and C. parvum (34%). The sex ratio of patients infected by either species was 0·5, but C. hominis was significantly more common in younger males. C. parvum infections were more acute and required more specialized medical attention, which suggests a differential adaptation of each species to human hosts. The parasites display strong seasonal and geographical variation. C. parvum incidence peaked during summer and was mainly detected in rural areas while C. hominis infections were more frequent in autumn and exhibited a more even geographical distribution. Such differences probably reflect their distinct sources of infection – C. parvum is mainly zoonotic and C. hominis anthroponotic – and the effects of climatic variables, like temperature and rainfall.
Key words: Cryptosporidium, molecular epidemiology, seasonal variation, virulence
INTRODUCTION
Cryptosporidium is a genus of protozoan parasites that infect many vertebrate species and cause diarrhoeal diseases [1]. They affect humans worldwide and the increasing number of cases reported in the last decades has prompted the recognition of cryptosporidiosis as an emerging disease by the WHO [1–4]. This pathogen has a faecal–oral transmission route, and propagates through the ingestion of oocysts present in contaminated water supplies or food [2, 5–7]. Most human infections are caused by Cryptosporidium hominis and C. parvum, while other species are found only rarely [3, 8]. C. hominis is almost exclusively anthroponotic, in contrast to C. parvum, which is commonly detected in domestic animals such as cows and sheep [3].
Cryptosporidiosis is a matter of public health concern in many countries and has inspired a growing number of epidemiological surveys aimed at understanding its demographic and clinical features [9–14]. However, there is little data on the worldwide incidence of this parasite in humans and only a few South European countries have reported studies on its incidence and prevalence [15, 16]. Spain, in common with most countries, lacks a specific cryptosporidiosis surveillance system (notification of cases to the health authorities was not mandatory until 2009 except for outbreaks), which means that the disease is likely to be underdiagnosed and underreported. Thus, although there are some surveys involving Spanish human samples, most of them include a small number of patients and are devoted to the analysis of particular cases or isolated outbreaks [17–19].
In order to improve our understanding of cryptosporidiosis in Europe, we present the results of a large-scale epidemiological study performed on a panel of samples corresponding to all patients with gastrointestinal illness in the Santiago de Compostela health area (Galicia, NW Iberian Peninsula), over a 9-year period. All faecal samples received at the Servizo de Microbioloxía of the Complexo Hospitalario Universitario de Santiago (CHUS) were routinely checked for cryptosporidiosis and subsequently characterized at the species and subtype levels [20]. In order to ascertain relevant epidemiological patterns of cryptosporidiosis in the study region, incidence rates were combined with genetic (species and subtype), environmental (temperature, rainfall, humidity) geographical (location; rural vs. urban area), demographic (sex and age of patients) and clinical (medical care required, oocyst counts and stool consistency) data, and time-series analyses were performed. Our results can be taken as a proxy for the epidemiology of cryptosporidiosis in the NW Iberian Peninsula, and represent the largest-scale study of the whole South-Western European façade.
MATERIALS AND METHODS
Sample genotyping
Stool samples were collected from all patients suffering from diarrhoeal disease between January 2000 and December 2008 in the health district of Santiago de Compostela (Galicia, NW Iberian Peninsula), an area with 515 700 inhabitants (2004). Diarrhoea was defined as the passage of three unformed stools in 8 h or of >3 loose stools in 24 h in addition to the presence of one or more symptoms of an enteric infection [21]. Samples were checked for enteric pathogens by routine microbiological methods at the Microbiology and Parasitology Laboratory of CHUS. The presence of viral antigens (adenovirus, astrovirus, rotavirus, norovirus) was assessed by applying a commercial immunochromatography test (CerTest Biotec faecal antigen rapid test; CerTest Biotec, Spain), bacteria (Campylobacter, Escherichia, Salmonella, Shigella, Yersinia) were identified using conventional coproculture techniques [22] and protozoan parasites were visualized by microscope examination after concentrating the samples with a modification of the Ritchie method [23]. Coccidian oocysts were detected by fluorescence microscopy (100–400x magnification) after staining stool smears with phenol-auramine [22, 24]. The identification was conducted on the basis of size and shape (for details see the microscopic identification module in http://water.epa.gov/lawsregs/rulesregs/sdwa/lt2/lab_home.cfm#training) by two experienced microscopists from the Microbiology and Parasitology Laboratory of CHUS.
A total of 822 cases of cryptosporidiosis were reported during the study period. Those with enough stool to perform DNA extractions (486 cases) were genotyped by means of iPLEX™ technology (Agena Bioscience, USA) to determine the Cryptosporidium species and subtype present in each sample [20]. This method is based on the use of single base extension of a panel of selected single nucleotide variants (SNVs) [25], used as species and subtype markers, followed by sequencing by mass spectrometry (MALDI-TOF) [26].
Demographic and clinical data
All relevant demographic (municipality, age and sex) and clinical (observed co-infections, associated symptoms and immunocompromised status) data were collected from each patient's record. Medical records were kept confidential pursuant to current legislation. Other variables, like specimen collection date, reported outbreaks, recent foreign travel and patient's close contacts affected by enteric problems, i.e. relatives and classmates, were also compiled.
The stage of the parasitization process and clinical profile of each case were assessed by means of three parameters: (i) excretion rate, (ii) sought medical care and (iii) stool consistency. (i) The excretion rate, or parasitic load, was quantified by scoring the number of oocysts observed per microscope field in stained faecal smears using 100x magnification, and used to typify the stage of the illness [27]. Medical treatment is usually sought after the onset of the first symptoms, mainly within the first week of the infection. In this initial, or acute, stage there is an exponential growth of the parasite population, and oocysts are shed in large numbers (>50 oocysts/field). In the second stage of the infection, usually within the second and third weeks, the parasite population usually reaches a plateau and experiences a progressive reduction, along with the oocyst count (20–50 oocysts/field), and symptoms ameliorate. In the third stage, patients may still shed oocysts (5–20 oocysts/field) for a long period of time (up to 2 months after infection), prior to the final non-proliferative stage (<5 oocysts/field) (J. Llovo, unpublished data). These data were available for 482 samples (99% of the genotyped samples), which were divided into four groups (1–4) according to oocyst counts (<5, 5–20, 20–50, >50, respectively) [28]. (ii) Medical care, as defined according to the kind of medical assistance required by patients, was available for 480 samples (98% of the genotyped samples). It was classified as primary health care (PHC), emergency ward (EW) or hospital admission (HA) [29], following a criterion of increasing symptomatic seriousness. Patients treated at PHC are assumed to present less virulent infections than those who use the EW or are admitted into hospital, which obviously are the most severe cases. (iii) Stool consistency, categorized as formed, pasty, and liquid stools, was evaluated in 369 samples (76% of the genotyped samples) [30]. This parameter can be used as a proxy for the stage of the illness, since the production of loose faeces is more frequent in the acute phase of the infection [31], and it is also expected to be associated with the clinical profile, as watery diarrhoea has a stronger impact on patients (dehydration, weight loss, etc.) than the excretion of pasty or formed stools.
Environmental and climatic analyses
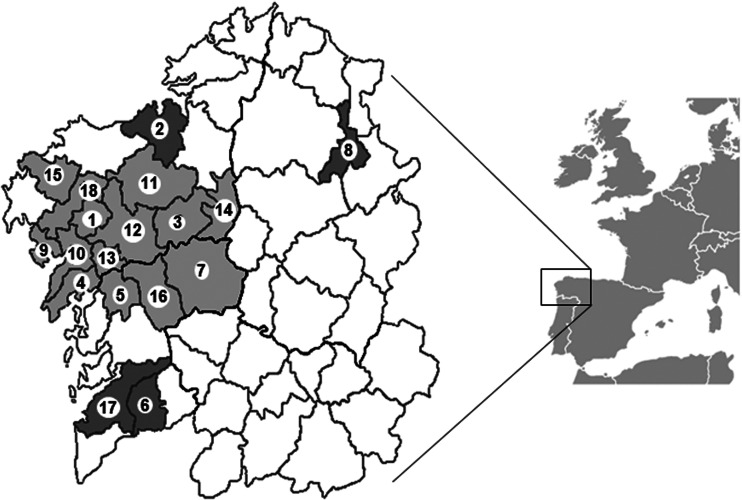
The health district of CHUS is distributed in 14 administrative regions called comarcas (analogous to shires; Fig. 1, Table 1), which include 58 lesser administrative units or parishes. A rural–urban index (RUI) was devised to represent the global environment of each comarca by combining four socioeconomic factors: (i) human density (population/km2), (ii) livestock abundance (number of cattle), (iii) availability of public water supply and (iv) sewerage services (fraction of the population with access to these services). Data were obtained from the Instituto Galego de Estatística (IGE; http://www.ige.eu/). To categorize each comarca, average values for each variable were compared with their corresponding average value at Galician level. Variables above the Galician average were counted as 0 (otherwise counted as 1), except for livestock abundance, where values were assigned the other way around. Finally the index for each comarca was estimated as the sum of the four variables. Thus, this index ranges from 0, which defines an urban comarca (high population density, low presence of cattle and high percentage of population with access to public water services) to 4, a rural comarca.
Fig. 1.
Comarcas included in Santiago de Compostela health district. Several patients from comarcas 2, 6, 8 and 17, which are not part of this health area (depicted in dark grey), received medical assistance at CHUS and were included in the analyses. Comarcas are: 1, A Barcala; 2, A Coruña; 3, Arzúa; 4, Barbanza; 5, Caldas; 6, Condado; 7, Deza; 8, Meira; 9, Muros; 10, Noia; 11, Ordes; 12, Santiago; 13, Sar; 14, T. Melide; 15, T. Soneira; 16, Tabeirós; 17, Vigo; 18, Xallas.
Table 1.
Demographic data
| Cryptosporidium species | C. hominis subtypes | C. parvum subtypes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Outcome | C. hominis | C. parvum | P | Ib | Id | P | IIa | IIn | P |
| Comarca* | 1. A Barcala (3) | 2 | 7 | <10−4 | 2 | — | 0·83 | 7 | — | 0·51 |
| 2. A Coruña (0) | — | 1 | — | — | 1 | — | ||||
| 3. Arzúa (4) | 3 | 10 | 1 | 1 | 8 | 2 | ||||
| 4. Barbanza (1) | 22 | 7 | 17 | 3 | 3 | 3 | ||||
| 5. Caldas (0) | 6 | 1 | 6 | — | 1 | — | ||||
| 6. Condado (1) | 1 | — | 1 | — | — | — | ||||
| 7. Deza (3) | 3 | 10 | 2 | 1 | 8 | 1 | ||||
| 8. Meira (3) | — | 1 | — | — | 1 | — | ||||
| 9. Muros (1) | 5 | 2 | 4 | — | 2 | — | ||||
| 10. Noia (2) | 11 | 5 | 10 | 1 | 5 | — | ||||
| 11. Ordes (4) | 8 | 24 | 7 | 1 | 20 | 3 | ||||
| 12. Santiago (1) | 213 | 62 | 199 | 13 | 57 | 4 | ||||
| 13. Sar (2) | 8 | 3 | 8 | — | 3 | — | ||||
| 14. T. Melide (4) | 2 | 7 | 2 | — | 7 | — | ||||
| 15. T. Soneira (3) | 1 | — | 1 | — | — | — | ||||
| 16. Tabeirós (3) | 29 | 5 | 26 | 2 | 4 | 1 | ||||
| 17. Vigo (0) | 1 | — | 1 | — | — | — | ||||
| 18. Xallas (4) | 2 | 17 | 2 | — | 17 | — | ||||
| Age groups†
(years) |
1–3 | 201 | 107 | 0·99 | 184 | 14 | 0·98 | 95 | 10 | 0·73 |
| 4–9 | 54 | 33 | 46 | 6 | 31 | 2 | ||||
| 10–19 | 18 | 7 | 17 | 1 | 5 | — | ||||
| 20–29 | 13 | 5 | 12 | 1 | 4 | 1 | ||||
| 30–39 | 8 | 3 | 7 | — | 3 | — | ||||
| 40–49 | 5 | 2 | 5 | — | 2 | — | ||||
| 50–59 | 3 | 1 | 3 | — | — | 1 | ||||
| 60–69 | 5 | 2 | 5 | — | 2 | — | ||||
| 70–79 | 8 | 3 | 7 | 1 | 3 | — | ||||
| ⩾80 | 2 | 1 | 2 | — | 1 | — | ||||
| Sex | Male | 164 | 82 | 0·74 | 149 | 13 | 0·65 | 72 | 8 | 0·58 |
| Female | 154 | 82 | 140 | 10 | 74 | 6 | ||||
All statistical analyses were performed using the χ2 test of homogeneity.
P values obtained with Yates' correction are in italics.
Values in parentheses are the rural–urban index for each comarca.
Unknown in three cases.
Unknown in one case.
Climatic data (i.e. monthly averages for humidity, rainfall and temperature [32]) were collected from the IGE and the Spanish National Institute of Statistics (INE; http://www.ine.es/) at two different weather stations located in Santiago de Compostela (Fig. 1, region 12), which were considered representative of all comarcas. The monthly data for each variable was calculated as the mean of the values from the two stations. For each variable, months were sorted according to the value of the variable and grouped into equal-sized bins (36 months in each bin), and the corresponding numbers of parasitized cases was obtained for each bin.
Statistical analyses
Time-series analyses were performed to characterize the seasonal component of the number of patients infected by C. parvum or C. hominis. The seasonal variation index (SVI), which quantifies the deviation of the number of cryptosporidiosis cases recorded each season relative to the overall mean, was estimated by applying the ratio-to-moving average method under a multiplicative time-series model. These calculations were performed with the aid of IBM SPSS software v. 20·0 (IBM Corp., USA).
Associations between Cryptosporidium species – and their corresponding subtypes – and demographical (age, sex, geographical distribution), clinical (excretion rates, medical care, stool consistency or symptoms) and environmental (seasonality, rainfall, humidity, temperature) parameters were evaluated by means of χ2 tests of homogeneity [33]. These were also used to investigate associations between clinical parameters, such as excretion rate, medical care and stool consistency. The distribution of parasites' species in age groups was assessed by means of a Mann–Whitney U test [33]. To do this, patients were grouped into 10-year bins. Given the large number of children, these were further divided into two age groups (0–3 and 4–9 years, respectively [10]). Spearman's rho (ρ) correlation coefficient [33] was used to evaluate associations between Cryptosporidium species and the regional development index (RUI). All statistical analyses were performed using Microsoft Excel (Microsoft Corp., USA) and IBM SPSS software v. 20·0 (IBM Corp., USA). In all cases, P values ⩽0·05 were considered significant.
RESULTS
The incidence rates of cryptosporidiosis in terms of number of cases per 100 000 population per year in the Santiago de Compostela health area (Galicia, NW Iberian Peninsula) were 9·44 (2000), 9·25 (2001), 17·57 (2002), 29·18 (2003), 13·96 (2004), 20·31 (2005), 27·64 (2006), 5·79 (2007) and 25·77 (2008), with an average (±s.e.) rate of 17·65±2·88, and 91·33 ± 7·44 cryptosporidiosis cases per year.
The epidemiological patterns were studied in a subset of these cases (N = 486), which were genotyped at the species and subtype levels [20]. Of these, 318 (65·43%) samples were confirmed as C. hominis, 164 (33·95%) as C. parvum, three (0·62%) as C. meleagridis and one (0·21%) as C. felis. The C. hominis samples corresponded to gp60 subtypes Ib (n = 289), Id (n = 23), Ia and Ie (n = 3, each). C. parvum samples were assigned to subtypes IIa (n = 146), IIn (n = 14), IId (n = 3) and one undetermined subtype. Of the three C. meleagridis samples, two were of subtype IIIf and one IIIb. Only the main species (C. hominis and C. parvum) and subtypes (IIa, IIn, Ib, Id) were used in the analyses (Table 1).
Demographic data analysis
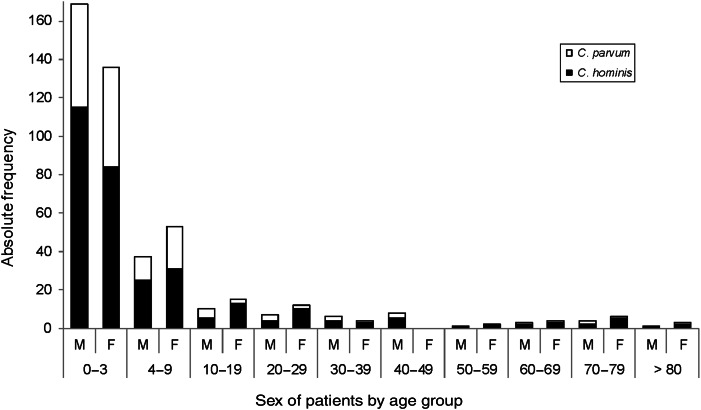
In our sample, Cryptosporidium mainly affects young children. The mean age of C. hominis patients (9·34 ± 17·58 years, range 1 month to 91 years, median 2 years, mode 1 year) was slightly higher than that of those infected by C. parvum (7·53±15·07 years, range 5 months to 80 years, median 2 years, mode 1 year), although the observed difference was not statistically significant by Mann–Whitney U test. No significant variation of the relative frequency of the two parasite species was observed across age bins (Table 1, Fig. 2).
Fig. 2.
Absolute frequencies of Cryptosporidium cases ranked by the sex and age group of patients.
The sex ratio of the patients was nearly 0·5 (239 females and 247 males, including three cases of parasitization with C. meleagridis and one with C. felis) and the distribution of parasite species across patients' sex did not depart from random expectations (P = 0·74, χ2 test; Table 1). But, if age groups are also considered, a differential incidence of C. hominis in males and females was detected (Fig. 2): there were more C. hominis cases in boys aged <3 years (115 cases) than in girls of the same age (84 cases), whereas this ratio was inverted in patients aged ⩾4 years (49 in males vs. 69 in females, respectively; P < 0·01, χ2 test; Fig. 2). This effect was not detected in C. parvum patients, with 54 and 52 cases in boys and girls, and 28 and 30 cases in older males and females, respectively (P = 0·74, χ2 test). No deviation from randomness was observed in the distribution of the major subtypes (Ib, Id, IIa, IIn) across sexes, considering their relative abundances (Table 1).
Clinical analysis
Seriousness of the infection
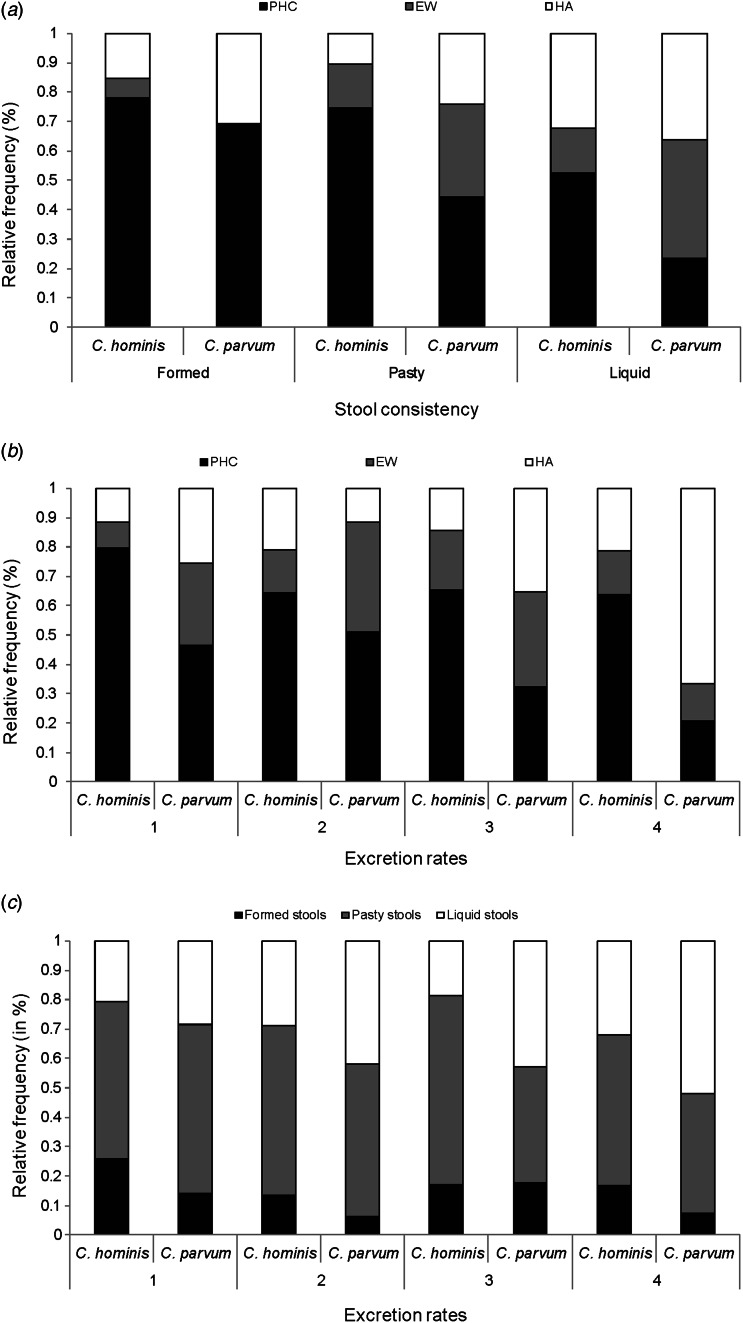
To check if the pathological course of the infections was in any way associated with the parasite species, we searched for associations between the abundance of the two Cryptosporidium species and three parameters which were used as proxies for the stage of the infection and its symptomatic seriousness: the type of medical attention required, the consistency of the stools and the parasitic load. Indeed, (i) C. parvum infections required HA in a larger proportion of cases than those caused by C. hominis (34·36% vs. 17·46%, respectively; P < 0·0001, χ2 test; Table 2), which were more often dealt with at PHC (67·62% of the C. hominis cases). No significant differences in required treatment were observed in within-species subtypes. (ii) Although Cryptosporidium infections usually presented pasty faeces (more than 50% of cases; Table 2), C. parvum were more often associated with liquid stools than C. hominis (41·23% vs. 25·59%, respectively; P < 0·01, χ2 test). This is interesting, because patients with formed or pasty stools were usually assisted at PHC, while those suffering from watery diarrhoea were mainly treated in the EW or were admitted to hospital (P < 0·0001, χ2 test; Fig. 3a, Supplementary Table S1). This was also observed within Cryptosporidium species when they were individually assessed (C. hominis, P < 0·01 and C. parvum, P < 0·05, χ2 test; Fig. 3a, Supplementary Table S1), which suggests that the association between stool consistency and medical care is independent of the infecting species. The same pattern was found for C. hominis subtype Ib (P < 0·01, χ2 test, data not shown).
Table 2.
Clinical data
| Cryptosporidium species | C. hominis subtypes | C. parvum subtypes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Outcome | C. hominis | C. parvum | P | Ib | Id | P | IIa | IIn | P | |
| Excretion rate* | 1 | 70 | 44 | 0·34 | 63 | 5 | 0·93 | 40 | 3 | 0·58 | |
| 2 | 76 | 43 | 69 | 6 | 36 | 6 | |||||
| 3 | 70 | 37 | 66 | 4 | 35 | 1 | |||||
| 4 | 99 | 39 | 88 | 8 | 34 | 4 | |||||
| Stool consistency† | Formed | 46 | 13 | <0·01 | 39 | 5 | 0·39 | 10 | 3 | 0·32 | |
| Pasty | 143 | 54 | 135 | 6 | 50 | 3 | |||||
| Liquid | 65 | 47 | 59 | 5 | 41 | 3 | |||||
| Medical care‡ | PHC | 213 | 62 | <10−4 | 196 | 12 | 0·14 | 52 | 9 | 0·10 | |
| EW | 47 | 45 | 44 | 3 | 39 | 4 | |||||
| HA | 55 | 56 | 46 | 8 | 54 | 1 | |||||
| Co-infections | Yes | 62 | 18 | <0·05 | 55 | 6 | 0·58 | 16 | 1 | 1·00 | |
| No | 256 | 146 | 234 | 17 | 130 | 13 | |||||
| Symptoms | Abdominal pain | Yes | 11 | 5 | 0·81 | 11 | — | 0·71 | 4 | — | 0·79 |
| No | 307 | 159 | 278 | 23 | 142 | 14 | |||||
| Fever | Yes | 14 | 9 | 0·60 | 11 | 2 | 0·56 | 8 | — | 0·80 | |
| No | 304 | 155 | 278 | 21 | 138 | 14 | |||||
| Vomiting | Yes | 8 | 11 | <0·05 | 8 | — | 0·90 | 11 | — | 0·61 | |
| No | 310 | 153 | 281 | 23 | 135 | 14 | |||||
| Nausea | Yes | 2 | — | 0·79 | 1 | 1 | 0·34 | — | — | — | |
| No | 316 | 164 | 288 | 22 | 146 | 14 | |||||
| Mucoid stools | Yes | 5 | 13 | <0·01 | 4 | 2 | 0·09 | 12 | 1 | 0·71 | |
| No | 313 | 151 | 285 | 21 | 134 | 13 | |||||
| Other symptoms§ | Yes | 6 | 3 | 0·76 | 5 | 1 | 0·93 | 4 | — | 0·79 | |
| No | 312 | 161 | 284 | 22 | 142 | 14 | |||||
| Immunocompromised | Yes | 6 | 4 | 0·94 | 6 | — | 0·93 | 4 | — | 0·79 | |
| No | 312 | 160 | 283 | 23 | 142 | 14 | |||||
| Outbreaks | Yes | 16 | — | <0·01 | 16 | — | 0·50 | — | — | — | |
| No | 302 | 164 | 273 | 23 | 146 | 14 | |||||
| Travel history | Yes | 6 | 1 | 0·48 | 2 | 4 | <10−4 | 1 | — | 0·14 | |
| No | 312 | 163 | 287 | 19 | 145 | 14 | |||||
| Family and school cases | Yes | 22 | 11 | 0·93 | 19 | 3 | 0·45 | 11 | — | 0·61 | |
| No | 296 | 153 | 270 | 20 | 135 | 14 | |||||
PHC, Primary health care; EW, emergency ward; HA, hospital admission.
All statistical analyses were performed by using the χ2 test of homogeneity.
P values obtained with Yates' correction are in italics.
Data available for 482 samples.
Data available for 480 samples.
Data available for 369 samples.
Weight loss, dehydration and food rejection.
Fig. 3.
Relationships in the three variables used to measure the virulence of each infection. (a) Stool consistency and type of medical assistance required by patients infected by C. hominis or C. parvum. (b) Excretion rates (parasitic load) and type of medical care required by patients infected by C. hominis or C. parvum. (c) Excretion rates (parasitic load) and stool consistency of patients infected by C. hominis or C. parvum.
Parasite loads (measured in terms of oocyst excretion rates) did not vary significantly across parasite species (Table 2). Patients with high loads required HA more frequently than those with lower excretion rates (P < 0·01, χ2 test, Fig. 3b, Supplementary Table S2). Markedly, this effect seems to be restricted to C. parvum infections (P < 0·0001, χ2 test), and it was not observed in C. hominis patients (P = 0·23, χ2 test; Fig. 3b, Supplementary Table S2). The main C. parvum subtype (IIa) displayed a similar pattern (P < 0·01, χ2 test, data not shown).
No significant association was found between oocyst excretion rates and stool consistency, neither for the whole dataset (P = 0·24, χ2 test; Fig. 3c, Supplementary Table S3) nor within either species (C. hominis, P = 0·32 and C. parvum, P = 0·49, χ2 test; Supplementary Table S3).
Associated co-infections
Enteropathogens other than Cryptosporidium were detected in 80 out of the 486 samples, including 11 different organisms. Eight samples had more than one concurrent pathogen. There were three cases of co-infection with either Endolimax nana, Cystoisospora belli or Pentatrichomonas hominis, two with noroviruses, two with Entamoeba histolytica, seven with rotaviruses, eight with adenoviruses, nine with Salmonella enterica, 13 with Campylobacter jejuni, 19 with Blastocystis hominis and 26 with Giardia lamblia. Some of these pathogens had previously been described as co-infective with Cryptosporidium [2, 34, 35]. Co-infections were more often associated with C. hominis (77·5% of the co-infection cases, P < 0·05, χ2 test; Table 2). No differences in subtypes were found.
Clinical symptoms, outbreaks and other factors
The classical symptoms of cryptosporidiosis are nausea, fever, abdominal pain, vomiting and mucus in the stool [36]. The latter two were more often associated with C. parvum infections (P < 0·05 and P < 0·01, respectively, χ2 test; Table 2). No differences were found in subtypes.
Immunocompromised patients, who required HA in 90% of the cases, did not show significant differences in the predominance of any Cryptosporidium species or subtype (Table 2).
Samples from a Cryptosporidium outbreak in the comarca of Tabeirós in autumn 2003, were genotyped as part of our survey. The outbreak was caused exclusively by C. hominis subtype Ib and affected hundreds of people, although only 16 cases were included in the study (Table 2).
The few cryptosporidiosis patients that reported a recent travel abroad or foreign origin were gathered and studied as a single group. These people came mainly from Africa (Ethiopia) and South America (Mexico, Bolivia, Ecuador). No significant interspecific differences were reported, although subtype Id was significantly more frequent in this group of patients (P < 0·0001, χ2 test; Table 2).
Finally, we observed that patients with C. hominis presented twice as many members of the same household or schoolmates with a gastroenteric problem than those suffering from C. parvum infections, although this difference was not statistically significant (Table 2).
Geographical distribution and environmental analysis
Spatial distribution of cases was different between species (P < 0·0001, χ2 test; Table 1). C. parvum incidence was positively associated with the RUI (Spearman's ρ correlation ρRUI-C.parvum = 0·552, P < 0·05), which indicates a significant association of this species with rural areas, while C. hominis infections were not associated with any particular social environment.
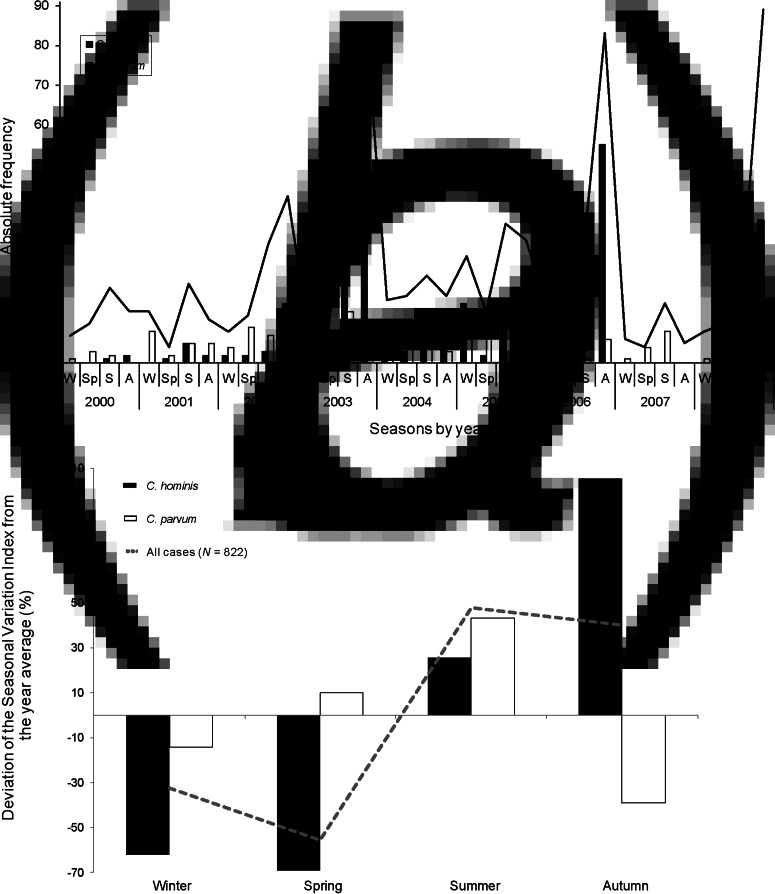
Seasonality and climatic analyses
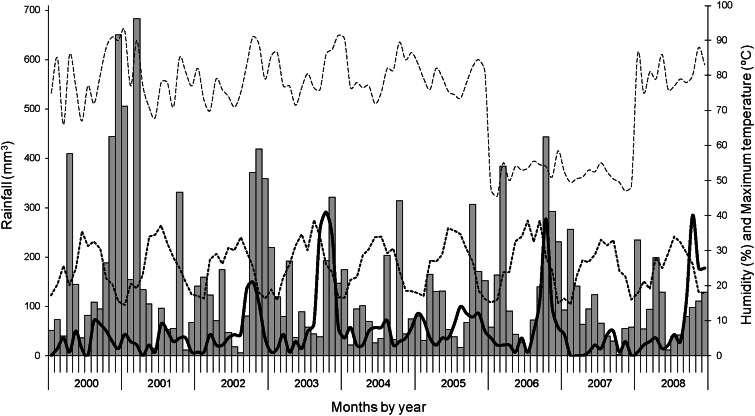
Time-series analyses of the whole dataset revealed a strong seasonal pattern of cryptosporidiosis incidence, with higher numbers in summer and particularly in autumn, as opposed to winter and spring, when incidence rates regularly fell below the yearly average (Fig. 4a). The two species displayed different seasonal structuration: the number of C. parvum cases experienced moderate seasonal variation, with a large increase in summer (SVI = 43%, Fig. 4b) and a sharp reduction in autumn (SVI = −39%). By contrast, seasonal variation of C. hominis was much greater, with a peak of cases in autumn (SVI = 105%), and below average incidences in winter and spring (−62% and −70%, respectively).
Fig. 4.
Seasonality of Cryptosporidium incidence. (a) Absolute frequencies of cryptosporidiosis cases across the study period. The continuous line represents the total number of cryptosporidiosis cases. (b) Seasonal patterns of variation of incidence rates (W, winter; Sp, spring, S, summer, A, autumn).
Potential associations of temporal patterns with climate parameters such as temperature, rainfall and humidity distributions were also investigated (Table 3). Monthly temperature was found not to be associated with the incidence of cryptosporidiosis at the species and subtype levels. However, since Galicia has a temperate climate, a role for monthly extreme temperatures (maximum and minimum) was also assessed [32]. Indeed, maximum monthly temperatures were associated with a higher incidence of both species (P < 0·01, χ2 test; Table 3). Humidity and rainfall also covaried with the incidence rates of both species, although they showed different patterns. C. hominis infections increased with rainfall and/or humidity (Figs 4a, 5), and the opposite pattern was observed for C. parvum, which was more common after dry periods (P < 0·0001, χ2 test; Table 3). In good agreement with these observations, only C. parvum cases were reported in 2007, which showed particularly low levels of rainfall in summer and autumn (seasons that usually display the highest number of C. hominis cases) and was one of the years with the lowest level of humidity reported (Figs 4a, 5). On the other hand, an increase in the number of infections caused by C. hominis was observed in 2003 and 2006, the warmest years of the temporal series (especially their summers and autumns) that also showed high rainfall rates (Figs 4a, 5).
Table 3.
Environmental data
| Cryptosporidium species | C. hominis subtypes | C. parvum subtypes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable* | Outcome | C. hominis | C. parvum | P | Ib | Id | P | IIa | IIn | P |
| Season | Winter | 29 | 36 | <10−4 | 28 | — | 0·07 | 29 | 4 | 0·87 |
| Spring | 17 | 42 | 25 | 2 | 37 | 5 | ||||
| Summer | 88 | 60 | 64 | 11 | 55 | 4 | ||||
| Autumn | 184 | 26 | 172 | 10 | 25 | 1 | ||||
| Humidity (%) | <74 | 95 | 51 | <10−4 | 95 | — | <0·01 | 43 | 8 | 0·22 |
| (73·6 ± 12·9) | 74–79·9 | 74 | 67 | 59 | 12 | 61 | 4 | |||
| >80 | 149 | 46 | 135 | 11 | 42 | 2 | ||||
| Rainfall (mm3) | <60 | 61 | 71 | <10−4 | 47 | 11 | <0·01 | 61 | 8 | 0·57 |
| (136·5 ± 132·6) | 60–140 | 102 | 49 | 98 | 3 | 45 | 2 | |||
| >140 | 155 | 44 | 144 | 9 | 40 | 4 | ||||
| Temperature (°C) | <10·4 | 60 | 35 | 0·39 | 57 | 1 | 0·13 | 29 | 3 | 0·98 |
| (13·2 ± 4·1) | 10·4–15·8 | 125 | 54 | 115 | 9 | 49 | 5 | |||
| >15·8 | 133 | 75 | 117 | 13 | 68 | 6 | ||||
| Max. temperature (°C) | <22 | 62 | 38 | <0·01 | 59 | 1 | <0·05 | 31 | 4 | 0·92 |
| (25·6 ± 6·8) | 22–29·4 | 165 | 57 | 154 | 10 | 52 | 5 | |||
| >29·5 | 91 | 69 | 76 | 12 | 63 | 5 | ||||
| Min. temperature (°C) | <1 | 87 | 45 | 0·90 | 82 | 3 | 0·13 | 40 | 3 | 0·70 |
| (3·6 ± 4·2) | 1–6 | 97 | 47 | 90 | 6 | 40 | 6 | |||
| >6 | 134 | 72 | 117 | 14 | 66 | 5 | ||||
All statistical analyses were performed by using the χ2 test of homogeneity.
P values obtained with Yates' correction are typed in italics.
Average monthly values ± standard error for climatic each variable are given in parentheses.
Fig. 5.
Cryptosporidiosis cases reported (continuous line, N = 822) and monthly averages of rainfall (bars), maximum temperature (dotted line) and humidity (segmented line). All lines follow the right axis.
DISCUSSION
This is one of the broadest epidemiological studies on cryptosporidiosis conducted in Southern Europe to date. The 822 cases reported in the 9-year period of analysis represent half of the cases reported elsewhere in Spain between 1995 and 2009 [17]. Considering that the population in the Santiago health area represents just about the 1·2% of the Spanish population, it seems clear that cryptosporidiosis cases were severely underdiagnosed in Spain during this period. In fact, the Microbiology and Parasitology Laboratory of CHUS is one of the few centres in Spain were all faecal samples from patients with enteric problems are routinely analysed for the presence of this and other pathogens. This high level of screening is reflected in the high incidence rates observed in our health area (17·65 ± 2·88 cases per 100000 population per year), that are far greater than those previously reported in most other large-scale surveys conducted in Europe [16, 17, 37, 38] or in the USA [12, 13]. In fact, only 2007 presented a lower incidence rate than those reported in Ireland (14·17), Great Britain (6·05) – countries that share climatic characteristics with Galicia – and some USA states [13, 38].
In the current dataset there was a strong predominance of C. hominis and C. parvum infections, involving the most common subtypes in humans (Ib and IIa, respectively) [3, 15, 39] and affecting mainly young children, as described worldwide [8, 10, 11]. As previously reported [11, 40], the number of cases decreased with age and no significant differences in the incidence of both species were observed.
In good agreement with data from other European countries, parasite species were equally distributed across sexes [10, 11]. However, in contrast to C. parvum, the fraction of C. hominis cases was usually larger in adult females than in males, suggesting human-to-human transmission that can probably be attributed to their greater involvement in childcare.
The analyses of various clinical variables showed differences in virulence between species; however, by contrast with previous studies [41–43], our results revealed that infections produced by C. parvum were more harmful than those caused by C. hominis, as they were significantly associated with more severe symptoms (vomiting or presence of mucous stools) that often required HA. These disparities in virulence suggest that humans could be better adapted to C. hominis infections, which seemed to have a milder effect on patient's physiology. Unlike previous studies [41, 42], the subtype families detected in our health area showed no significant differences in virulence.
Cryptosporidiosis caused by C. hominis exhibited clinical characteristics somewhat different to those caused by C. parvum. For instance, more than 75% of cases with concomitant enteropathogens were C. hominis infections. Moreover, the fact that C. hominis, and particularly its subtype Ib, is responsible for the majority of the outbreaks reported in Europe [3], as the one detected in Tabeirós in 2003, confirms the high infectivity of this species and its great capability of spreading both through rural or urban regions. On the contrary, subtype Id, which was found in a much smaller proportion in our panel of samples, was significantly more frequent in patients reporting recent foreign travel, reinforcing the assumption that it is not a typical European subtype [3, 15, 41, 42].
The results of the geographical and seasonal distribution of the Galician samples are concordant with previous studies showing that C. hominis displays a widespread distribution with seasonal peaks in autumn [e.g. 6, 10, 11, 40], while C. parvum was significantly more prevalent in rural areas [3, 11], with increments in the number of cases that coincided with lambing and calving activity peaks (usually in spring and summer). This could be the reason for the increase in oocyst concentrations observed in drinking water obtained from the river Tambre – the main water source that flows through the study area – in spring and summer of 2007 [44]. In fact, C. parvum subtypes identified in human samples were commonly detected in livestock stools, which further supports their zoonotic origin [20, 45].
Finally, it has been proposed that climate variables such as those analysed here modulate the incidence rate of cryptosporidiosis and, thus, are likely to play a role in the seasonal distribution of the species [32, 46, 47]. Regarding temperature, the intervals of highest incidence occurred consistently after the warmest periods [47], as described in other mid-latitude and temperate regions [46]. On the other hand, variations of rainfall and/or humidity might also contribute to the different incidence rates observed between species. A negative association between rainfall and the risk of infection by Cryptosporidium, such as the one observed for C. parvum, has been attributed to a reduction of oocyst concentration in the soil and surface water after rainy periods [48, 49]. However, this hypothesis does not seem to apply to C. hominis. An explanation of this might reside in the mechanisms of transmission of the two species. C. parvum is mainly zoonotic and is commonly found in rural areas, thus the spread of its oocysts is probably associated with rain levels in contrast to person-to-person transmission of C. hominis, which is expected to be more affected by seasonal changes in human activity, such as use of recreational water and consumption of fresh vegetables in warmer seasons, or initiation of nursery-primary school attendance of children in late summer.
ACKNOWLEDGEMENTS
We thank Dr Manuel del Valle (Dirección Provincial de Saúde Pública, A Coruña), as well as the anonymous referees who reviewed this work, for helpful suggestions and constructive comments on the manuscript. This work was supported by grant PGIDIT06PXIB228073PR from Xunta de Galicia, Spain, to C.B. J.L.A-F. was supported by a student fellowship co-financed by Xunta de Galicia, Spain, and the European Social Fund; X.M. was supported by a Programa Ramón y Cajal contract (Ministerio de Ciencia e Innovación, Spain) and C.B. was supported by a Programa Isidro Parga Pondal contract (Xunta de Galicia, Spain).
DECLARATION OF INTEREST
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268815000163.
click here to view supplementary material
REFERENCES
- 1.Mosier DA, Oberst RD. Cryptosporidiosis. A global challenge. Annals of the New York Academy of Sciences 2000; 916: 102–111. [DOI] [PubMed] [Google Scholar]
- 2.Meinhardt PL, Casemore DP, Miller KB. Epidemiologic aspects of human cryptosporidiosis and the role of waterborne transmission. Epidemiologic Reviews 1996; 18: 118–136. [DOI] [PubMed] [Google Scholar]
- 3.Xiao L. Molecular epidemiology of cryptosporidiosis: an update. Experimental Parasitology 2010; 124: 80–89. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Emerging issues in water and infectious disease. Geneva: WHO; 2003.
- 5.Freire-Santos F, et al. Detection of Cryptosporidium oocysts in bivalve molluscs destined for human consumption. Journal of Parasitology 2000; 86: 853–854. [DOI] [PubMed] [Google Scholar]
- 6.Semenza JC, Nichols G. Cryptosporidiosis surveillance and water-borne outbreaks in Europe. Eurosurveillance 2007; 12: E13–14. [DOI] [PubMed] [Google Scholar]
- 7.Craun GF, Calderón RL, Craun MF. Outbreaks associated with recreational water in the United States. International Journal of Environmental Health Research 2005; 15: 243–262. [DOI] [PubMed] [Google Scholar]
- 8.Elwin K, et al. The epidemiology of sporadic human infections with unusual cryptosporidia detected during routine typing in England and Wales, 2000–2008. Epidemiology and Infection 2011; 140: 673–683. [DOI] [PubMed] [Google Scholar]
- 9.Fournet N, et al. Simultaneous increase of Cryptosporidium infections in the Netherlands, the United Kingdom and Germany in late summer season, 2012. Eurosurveillance 2013; 18(2). [PubMed] [Google Scholar]
- 10.Chalmers RM, et al. Long-term Cryptosporidium typing reveals the aetiology and species-specific epidemiology of human cryptosporidiosis in England and Wales, 2000 to 2003. Eurosurveillance 2009; 14(2). [DOI] [PubMed] [Google Scholar]
- 11.Chalmers RM, et al. Epidemiology of anthroponotic and zoonotic human cryptosporidiosis in England and Wales, 2004–2006. Epidemiology and Infection 2011; 139: 700–712. [DOI] [PubMed] [Google Scholar]
- 12.Yoder JS, Beach MJ. Cryptosporidiosis surveillance – United States, 2003–2005. Morbidity and Mortality Weekly Report Surveillance Summaries 2007; 56: 1–10. [PubMed] [Google Scholar]
- 13.Yoder JS, Harral C, Beach MJ. Cryptosporidiosis surveillance - United States, 2006–2008. Morbidity and Mortality Weekly Report. Surveillance Summaries 2010; 59: 1–14. [PubMed] [Google Scholar]
- 14.Kotloff KL, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 2013; 382: 209–222. [DOI] [PubMed] [Google Scholar]
- 15.Alves M, et al. Distribution of Cryptosporidium subtypes in humans and domestic and wild ruminants in Portugal. Parasitology Research 2006; 99: 287–292. [DOI] [PubMed] [Google Scholar]
- 16.The ANOFEL Cryptosporidium National Network. Laboratory-based surveillance for Cryptosporidium in France, 2006–2009. Eurosurveillance 2010; 15: 19642. [PubMed] [Google Scholar]
- 17.Navarro-i-Martínez L, del Águila C, Bornay-Llinares FJ. Cryptosporidium: a genus in revision. The situation in Spain [in Spanish]. Enfermedades Infecciosas y Microbiología Clínica 2011; 29: 135–143. [DOI] [PubMed] [Google Scholar]
- 18.Artieda J, et al. Outbreak of cryptosporidiosis in a child day-care centre in Gipuzkoa, Spain, October to December 2011. Eurosurveillance 2012; 17(5). [DOI] [PubMed] [Google Scholar]
- 19.Soler P. Surveillance of cryptosporidiosis in Spain from 1995 to 2003. Eurosurveillance 2004; 8(10). [Google Scholar]
- 20.Abal-Fabeiro JL, et al. High-throughput genotyping assay for the large-scale genetic characterization of Cryptosporidium parasites from human and bovine samples. Parasitology 2014; 141: 491–500. [DOI] [PubMed] [Google Scholar]
- 21.DuPont HL, et al. The infectivity of Cryptosporidium parvum in healthy volunteers. New England Journal of Medicine 1995; 332: 855–859. [DOI] [PubMed] [Google Scholar]
- 22.Murray P, et al. Manual of Clinical Microbiology, 9th edn. Washington, DC: ASM Press, 2007. [Google Scholar]
- 23.Allen AV, Ridley DS. Further observations on the formol-ether concentration technique for faecal parasites. Journal of Clinical Pathology 1970; 23: 545–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nichols G, Thom B. Screening for Cryptosporidium in stools. Lancet 1984; 1: 734–735. [PubMed] [Google Scholar]
- 25.Gabriel S, Ziaugra L, Tabbaa D. SNP genotyping using the Sequenom MassARRAY iPLEX platform. Current Protocols in Human Genetics 2009; Chapter 2: Unit 2 12. [DOI] [PubMed]
- 26.Sauer S, Gut IG. Genotyping single-nucleotide polymorphisms by matrix-assisted laser-desorption/ionization time-of-flight mass spectrometry. Journal of Chromatography, B: Analytical Technologies in the Biomedical and Life Sciences 2002; 782: 73–87. [DOI] [PubMed] [Google Scholar]
- 27.Chappell CL, et al. Cryptosporidium parvum: intensity of infection and oocyst excretion patterns in healthy volunteers. Journal of Infectious Diseases 1996; 173: 232–236. [DOI] [PubMed] [Google Scholar]
- 28.Garcia LS, Brewer TC, Bruckner DA. Fluorescence detection of Cryptosporidium oocysts in human fecal specimens by using monoclonal antibodies. Journal of Clinical Microbiology 1987; 25: 119–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kendrick D, et al. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Social Science & Medicine 2005; 61: 1905–1915. [DOI] [PubMed] [Google Scholar]
- 30.Pereira SJ, et al. Pathogenesis of human and bovine Cryptosporidium parvum in gnotobiotic pigs. Journal of Infectious Diseases 2002; 186: 715–718. [DOI] [PubMed] [Google Scholar]
- 31.Franzen C, Muller A. Cryptosporidia and microsporidia – waterborne diseases in the immunocompromised host. Diagnostic Microbiology & Infectious Disease 1999; 34: 245–262. [DOI] [PubMed] [Google Scholar]
- 32.González-Moreno O, et al. Prevalence and climatic associated factors of Cryptosporidium sp. infections in savanna chimpanzees from Ugalla, Western Tanzania. Parasitology Research 2013; 112: 393–399. [DOI] [PubMed] [Google Scholar]
- 33.Sokal RR, Rohlf FJ. Biometry: the Principles and Practice of Statistics in Biological Research, 3rd edn. New York: W. H. Freeman, 1995, pp. 887. [Google Scholar]
- 34.Jex AR, et al. Detection of diarrhoeal pathogens in human faeces using an automated, robotic platform. Molecular and Cellular Probes 2012; 26: 11–15. [DOI] [PubMed] [Google Scholar]
- 35.Mengelle C, et al. Simultaneous detection of gastrointestinal pathogens with a multiplex Luminex-based molecular assay in stool samples from diarrhoeic patients. Clinical Microbiology and Infection 2013; 19: E458–465. [DOI] [PubMed] [Google Scholar]
- 36.Chalmers RM, Davies AP. Minireview: clinical cryptosporidiosis. Experimental Parasitology 2010; 124: 138–146. [DOI] [PubMed] [Google Scholar]
- 37.European Centre for Disease Prevention and Control. Annual epidemiological report on communicable diseases in Europe. Report of the status of communicable diseases in the EU and EEA/EFTA countries. Stockholm: ECDC, 2007.
- 38.European Centre for Disease Prevention and Control. Annual epidemiological report 2012. Reporting on 2010 surveillance data and 2011 epidemic intelligence data. Stockholm: ECDC, 2013.
- 39.Jex AR, Gasser RB. Analysis of the genetic diversity within Cryptosporidium hominis and Cryptosporidium parvum from imported and autochtonous cases of human cryptosporidiosis by mutation scanning. Electrophoresis 2008; 29: 4119–4129. [DOI] [PubMed] [Google Scholar]
- 40.Garvey P, McKeown P. Epidemiology of human cryptosporidiosis in Ireland, 2004–2006: analysis of national notification data. Eurosurveillance 2009; 14(8). [PubMed] [Google Scholar]
- 41.Cama VA, et al. Differences in clinical manifestations among Cryptosporidium species and subtypes in HIV-infected persons. Journal of Infectious Diseases 2007; 196: 684–691. [DOI] [PubMed] [Google Scholar]
- 42.Cama VA, et al. Cryptosporidium species and subtypes and clinical manifestations in children, Peru. Emerging Infectious Diseases 2008; 14: 1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hunter PR, et al. Health sequelae of human cryptosporidiosis in immunocompetent patients. Clinical Infectious Diseases 2004; 39: 504–510. [DOI] [PubMed] [Google Scholar]
- 44.Castro-Hermida JA, et al. Presence of Cryptosporidium spp. and Giardia duodenalis through drinking water. Science of the Total Environment 2008; 405: 45–53. [DOI] [PubMed] [Google Scholar]
- 45.Quílez J, et al. Cryptosporidium species and subtype analysis from dairy calves in Spain. Parasitology 2008; 135: 1613–1620. [DOI] [PubMed] [Google Scholar]
- 46.Jagai JS, et al. Seasonality of cryptosporidiosis: a meta-analysis approach. Environmental Research 2009; 109: 465–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Naumova EN, et al. Seasonality in six enterically transmitted diseases and ambient temperature. Epidemiology and Infection 2007; 135: 281–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schijven J, et al. A decision support tool to compare waterborne and foodborne infection and/or illness risks associated with climate change. Risk Analysis 2013; 33: 2154–2167. [DOI] [PubMed] [Google Scholar]
- 49.Tate KW, Pereira MD, Atwill ER. Efficacy of vegetated buffer strips for retaining Cryptosporidium parvum. Journal of Environmental Quality 2004; 33: 2243–2251. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268815000163.
click here to view supplementary material