SUMMARY
Enterotoxigenic Escherichia coli (ETEC) is now recognized as a common cause of foodborne outbreaks. This study aimed to describe the first ETEC O169 outbreak identified in Korea. In this outbreak, we identified 1642 cases from seven schools. Retrospective cohort studies were performed in two schools; and case-control studies were conducted in five schools. In two schools, radish kimchi was associated with illness; and in five other schools, radish or cabbage kimchi was found to have a higher risk among food items. Adjusted relative risk of kimchi was 5·87–7·21 in schools that underwent cohort studies; and adjusted odds ratio was 4·52–12·37 in schools that underwent case-control studies. ETEC O169 was isolated from 230 affected students, and was indistinguishable from the isolates detected from the kimchi product distributed by company X, a food company that produced and distributed kimchi to all seven schools. In this outbreak, we found that the risk of a kimchi-borne outbreak of ETEC O169 infection is present in Korea. We recommend continued monitoring regarding food safety in Korea, and strengthening surveillance regarding ETEC O169 infection through implementation of active laboratory surveillance to confirm its infection.
Key words: Foodborne infections, food safety, outbreaks
INTRODUCTION
Enterotoxigenic Escherichia coli (ETEC) infection is a self-limiting disease, characterized by diarrhoea, abdominal pain and vomiting, and typically affects persons served with processed foodstuffs [1, 2]. ETEC has been known previously as an important cause of bacterial gastroenteritis in the developing world and in travellers; however, it has been noted recently in foodborne outbreaks in developed countries [3–5]. Moreover, in various ETEC genotypes, ETEC O169 is increasingly recognized as the subtype that is frequently isolated from foodborne outbreaks. Earlier studies in Japan suggested that ETEC O169 outbreaks were associated with restaurants or catered events [4]. Reports from the USA indicate that raw vegetables and herbs are increasingly implicated as vehicles for ETEC O169 outbreaks [5].
In the Republic of Korea, profound change in the food environment and in individual eating habits has taken place over the past decade: consumption of foods prepared outside the home has increased greatly. An increase in the risk of foodborne infection outbreaks has been suggested in earlier studies where the number of foodborne outbreaks increased from 78 in 2002 to 259 in 2006 and the proportion of pathogenic E. coli in outbreak-related cases increased from 19% in 2003 to 26% in 2006 [6]. Hhowever, to date, serogroups of such ETEC pathogens isolated from outbreaks have not been clearly identified in Korea.
The recent introduction of pulse-field gel electrophoresis (PFGE) has provided an additional tool which can be used for foodborne outbreak investigation of E. coli in Korea. Although PFGE analysis of E. coli was first introduced in Korea in the mid-1990s, its routine use in the clinical setting is still not widely performed. However, in the public health setting, the value of PFGE in foodborne outbreak investigations has become more recognized. Furthermore, it is evident that earlier use of PFGE during an E. coli outbreak helps in identification of the transmission route of the pathogen.
In September 2012, clusters of ETEC O169 infection were detected in seven schools in Incheon, Korea, which subsequently were suspected to be linked to the same source of transmission by PFGE pattern analysis. These students developed gastrointestinal symptoms after eating food from the school cafeteria. This was the first isolation of ETEC O169 from a foodborne outbreak in Korea. In this report, we describe the investigation to identify the source of infection in the ETEC O169 outbreak which occurred in seven schools in Incheon, Korea.
METHODS
On 6 September 2012, a cluster of diarrhoeal illness was reported by four schools: A (elementary school), B (high school), C (elementary school) and D (elementary school). Subsequently on 7 September 2012, school F (elementary school), on 9 September, school E (girls' junior high school), and on 10 September, school G (high school) reported the occurrence of an increased number of students with diarrhoeal illness.
Due to limited human resources for conducting cohort studies in all the affected schools, retrospective cohort studies were performed in schools B and E, and case-control studies were conducted in schools A, C, D, F and G. Self-administered questionnaires were distributed to collect students' and teachers' demographics, clinical characteristics and history of food consumption during 1–10 September 2012. A case was defined as (1) a person who consumed food at the school cafeteria during 1–10 September; and (2) who developed vomiting, diarrhoea or abdominal pain after 3 September. All students, teachers and school workers who were exposed to the school cafeteria food items were enrolled in the retrospective studies in schools B and E. In schools A, C, D, F and G, control groups of asymptomatic students were selected randomly from school lists on a 1:1 ratio, frequency-matched by school grade.
The cafeterias and kitchens in the seven schools were inspected for environmental exposures to the pathogens. Processed food, unprocessed food and drinking water were collected and examined by Incheon City Health Environment Laboratory. Stool specimens were collected from identified cases for standard bacteriological and virological assessment. Inspection of food companies and interviews with food-handlers regarding food-handling practices and illnesses were conducted. From the food companies, more than six processed and un-processed food items each company were collected and examined. Clinical E. coli isolates were sent to the Korea Food and Drug Administration (KDFA) for PFGE subtyping with the use of restriction enzyme XbaI and standard PulseNet protocols.
We calculated food item-specific relative risks for schools B and E and odds ratios for schools A, C, D, F and G. The association between food items and the risk of developing symptoms was calculated using the χ2 test or Fisher's exact test; multivariable analysis was performed to calculate adjusted relative risks and odds ratios. A P value of <0·05 was considered statistically significant, and all statistical analyses were performed using SPSS software, version 16.0 (SPSS Inc., USA). Because outbreak response and investigational activities during public health emergencies are legally mandated by the government-operated infectious disease control system in Korea, institutional review board approval and informed consent were not required.
RESULTS
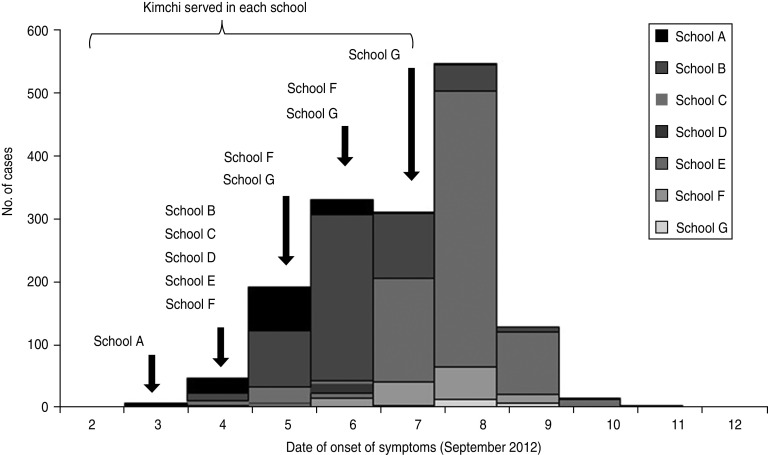
During the outbreak period, we identified 1642 potential cases of ETEC O169 infection. Dates of onset of symptoms ranged from 3 to 7 September 2012 (Fig. 1). Attack rate ranged between 3·0% and 62·2%, resulting in 17 cases in school D to 755 cases in school E (Table 1). The main symptoms in affected persons were: (1) diarrhoea (⩾3 loose stools a day; 22·2–94·4%), (2) abdominal pain (58·5–89·1%) and (3) fever (12·8–58·5%); whereas vomiting and mucoid or bloody diarrhoea were less common. Of all subjects, none experienced severe complications such as haemolytic uraemic syndrome or hospitalization. Mean incubation period ranged around 2–3 days (Table 1). The numbers of food samples taken were: school A (n = 24), school B (n = 42), school C (n = 30), school D (n = 25), school E (n = 26), school F (n = 29), and school G (n = 72) (Table 1). Of the food samples collected in all seven schools, ETEC O169 and enteropathogenic E. coli (EPEC) were isolated from cabbage or radish kimchi products.
Fig. 1.
Cases of enterotoxigenic Escherichia coli (ETEC) O169 enteritis associated with consumption of kimchi in multiple schools, Republic of Korea in 2012 (n = 1642), according to date of onset of symptoms.
Table 1.
Characteristics of enterotoxigenic Escherichia coli (ETEC) O169 enteritis outbreaks in seven schools, Republic of Korea in 2012 (n = 1642), according to site of outbreak occurrence
| Characteristics | Outbreak sites | ||||||
|---|---|---|---|---|---|---|---|
| School A | School B | School C | School D | School E | School F | School G | |
| No. of cases | 135 | 550 | 39 | 17 | 755 | 128 | 18 |
| Total exposure* | 920 | 1150 | 582 | 575 | 1,213 | 854 | 250 |
| Attack rate (%) | 14·7 | 47·8 | 6·7 | 3·0 | 62·2 | 15·0 | 7·2 |
| Symptom onset (date) | 3 Sept. | 4 Sept. | 4 Sept. | 5 Sept. | 4 Sept. | 6 Sept. | 7 Sept. |
| Symptoms, n (%) | |||||||
| Diarrhoea, ⩾3/day | 30 (22·2) | 316 (57·5) | 11 (28·2) | 7 (41·2) | 443 (58·7) | 66 (51·6) | 17 (94·4) |
| Mucoid diarrhoea | 9 (6·7) | 38 (6·9) | 1 (2·6) | 0 | 38 (5·0) | 12 (9·4) | 2 (11·1) |
| Bloody diarrhoea | 2 (1·5) | 9 (1·6) | 0 | 0 | 9 (1·2) | 2 (1·6) | 0 |
| Fever | 22 (16·4) | 126 (22·9) | 5 (12·8) | 10 (58·8) | 206 (27·3) | 19 (14·8) | 6 (33·8) |
| Vomiting | 10 (7·4) | 22 (4·0) | 1 (2·6) | 7 (41·2) | 68 (9·0) | 15 (11·7) | 0 |
| Abdominal pain | 79 (58·5) | 342 (62·2) | 26 (66·7) | 10 (58·8) | 582 (77·1) | 114 (89·1) | 16 (88·9) |
| Incubation time | |||||||
| Mean (days) | 2 | 3 | 2 | 2 | 2 | 3 | 2 |
| Range (h) | 17 | 20 | 13 | 5 | 14 | 20 | 10 |
| Food samples (n) | 24 | 42 | 30 | 25 | 26 | 29 | 72 |
| Isolated ETEC† | 69 | 60 | 35 | 11 | 20 | 27 | 8 |
Total exposure: number of individuals who ate at the school cafeteria.
Isolation from affected individuals.
In schools B and E, we conducted retrospective cohort studies by interviewing all persons who ate at the school cafeteria (Table 2). In school B, we interviewed 1150 individuals, and identified 550 (47·8%) with illness that fulfilled the case definition (Table 1). In univariable and multivariable analysis of all food items served between 1 and 10 September, radish kimchi was significantly associated with occurrence of illness (relative risk 2·47, adjusted relative risk 5·87) (Table 2). In school E, of 861 persons who ate radish kimchi, 644 (adjusted relative risk 7·21) became ill cases, whereas 75/209 persons (35·9%) who did not eat kimchi reported having symptoms. In the two schools, other items such as rice, sauced chicken, and sesame leaf had elevated relative risks, but radish kimchi had highest exposure in cases and highest relative risk. In school B, 60 ETEC O169, 14 enteroaggressive E. coli (EAEC), six EPEC and two Bacillus cereus were isolated from affected individuals; and in school E, 20 ETEC O169 and 15 EAEC were isolated from affected individuals (Table 1).
Table 2.
Relative risks of exposure to selected items in enterotoxigenic Escherichia coli (ETEC) O169 enteritis outbreaks in two schools, Republic of Korea in 2012, according to ingested food item
| Food item | Exposed | Non-exposed | Univariable | Multivariable | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Case | Total | (%) | Case | Total | (%) | RR | (95% CI) | aRR | (95% CI) | |
| School B | ||||||||||
| Rice | 534 | 1048 | (49·3) | 14 | 55 | (25·5) | 2·00 | (1·27–3·16) | 2·84 | (1·53–5·28) |
| Sauced chicken | 524 | 1058 | (49·5) | 24 | 80 | (30·0) | 1·65 | (1·18–2·32) | 2·29 | (1·40–3·75) |
| Fresh lettuce | 368 | 649 | (56·7) | 166 | 545 | (36·6) | 1·86 | (1·61–2·15) | 2·27 | (1·78–2·91) |
| Folded egg | 416 | 810 | (51·4) | 129 | 319 | (40·4) | 1·27 | (1·09–1·47) | 1·56 | (1·20–2·02) |
| Beef rib | 414 | 821 | (50·4) | 131 | 309 | (42·4) | 1·19 | (1·03–1·38) | 1·38 | (1·06–1·80) |
| Radish kimchi | 466 | 741 | (60·2) | 95 | 373 | (25·5) | 2·47 | (2·06–2·96) | 5·87 | (3·87–7·23) |
| School E | ||||||||||
| Rice | 756 | 1122 | (67·4) | 11 | 26 | (42·3) | 1·59 | (1·02–2·50) | 2·82 | (1·28–6·19) |
| Pork and vegetables | 733 | 1089 | (67·3) | 28 | 49 | (57·1) | 1·18 | (0·92–1·51) | 1·54 | (0·87–2·77) |
| Seasoned bracken | 386 | 554 | (69·7) | 319 | 507 | (62·9) | 1·12 | (1·02–1·21) | 1·35 | (1·05–1·75) |
| Sesame leaf | 419 | 595 | (70·4) | 252 | 419 | (60·1) | 1·17 | (1·07–1·29) | 1·58 | (1·21–2·05) |
| Eggplant | 262 | 371 | (70·6) | 440 | 685 | (64·2) | 1·10 | (1·00–1·20) | 1·34 | (1·02–1·76) |
| Radish kimchi* | 644 | 861 | (74·8) | 75 | 209 | (35·9) | 2·08 | (1·73–2·51) | 7·21 | (4·55–9·10) |
RR, Relative risk; aRR, adjusted relative risk; CI, confidence interval.
Enteroaggressive E. coli isolated from radish kimchi in school E.
Case-control studies were conducted in schools A, C, D, F and G (Table 3). In all schools, infection was significantly associated with eating cabbage kimchi or radish kimchi (Table 3). In school A, adjusted odds ratio for cabbage kimchi was 7·87 (95% confidence interval 3·50–23·09); with ETEC O169 and EPEC isolated from a cabbage kimchi specimen that was stored in the cafeteria. In school C, melon and broccoli salad had adjusted odds ratio of 4·37 and 2·59, respectively. In school D, shredded radish (the same product that was served as kimchi, although some was separately prepared as salad) showed adjusted odds ratio of 5·57; the same radish was also used for serving as radish kimchi. From affected students in school A, 69 ETEC O169, 39 EAEC, one EPEC and six B. cereus were isolated; in school C, 35 ETEC O169, seven EAEC, one EPEC and five B. cereus; in school D, 11 ETEC and seven EAEC; in school F, 27 ETEC, 14 EAEC and one B. cereus; in school G, eight ETEC and six EAEC were isolated, respectively (Table 1).
Table 3.
Selected exposures in cases vs. controls in enterotoxigenic Escherichia coli (ETEC) O169 enteritis outbreaks in five schools, Republic of Korea in 2012, according to ingested food item
| Food item | Case | Control | Univariable | Multivariable | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Exposed | Total | (%) | Exposed | Total | (%) | OR | (95% CI) | aOR | (95% CI) | |
| School A | ||||||||||
| Rice | 111 | 117 | (94·9) | 468 | 485 | (96·5) | 0·67 | (0·26–1·74) | 0·89 | (0·36–3·29) |
| Pine mushroom | 67 | 106 | (63·2) | 368 | 451 | (81·6) | 0·39 | (0·24–0·61) | 0·51 | (0·21–1·70) |
| Acorn jelly | 11 | 161 | (6·8) | 436 | 474 | (92·0) | — | — | — | — |
| Squid and vegetables | 95 | 120 | (79·2) | 416 | 472 | (88·1) | 0·51 | (0·30–0·86) | 0·74 | (0·58–1·87) |
| Cabbage kimchi* | 92 | 111 | (82·9) | 39 | 89 | (43·8) | 6·20 | (3·24–11·86) | 7·87 | (3·50–23·09) |
| School C | ||||||||||
| Rice | 38 | 38 | (100·0) | 94 | 97 | (96·9) | — | — | — | — |
| Melon | 38 | 39 | (97·4) | 87 | 97 | (89·7) | 4·37 | (0·54–35·34) | 4·76 | (0·81–37·42) |
| Broccoli salad | 32 | 37 | (86·5) | 69 | 94 | (73·4) | 2·32 | (0·81–6·61) | 2·59 | (0·99–6·85) |
| Radish kimchi | 36 | 38 | (94·7) | 72 | 92 | (78·3) | 5·00 | (1·11–22·58) | 6·27 | (1·37–20·12) |
| School D | ||||||||||
| Rice | 17 | 17 | (100·0) | 42 | 44 | (95·5) | — | — | — | — |
| Shredded radish | 16 | 17 | (94·1) | 36 | 44 | (81·8) | 3·56 | (0·41–30·85) | 5·57 | (0·45–38·89) |
| Beef | 15 | 17 | (88·2) | 41 | 44 | (93·2) | 0·55 | (0·08–3·61) | 0·87 | (0·01–3·89) |
| Radish kimchi | 16 | 17 | (94·1) | 37 | 44 | (84·1) | 3·03 | (0·34–23·66) | 4·52 | (0·77–22·52 |
| School F | ||||||||||
| Rice | 108 | 109 | (99·1) | 139 | 142 | (97·9) | 2·33 | (0·24–22·72) | 2·94 | (0·12–26·23) |
| Salad | 85 | 95 | (89·5) | 84 | 122 | (68·9) | 3·85 | (1·80–8·21) | 4·97 | (1·86–8·43) |
| Kimchi-fried rice | 106 | 108 | (98·1) | 131 | 143 | (91·6) | 4·85 | (1·06–22·17) | 5·60 | (1·11–29·23) |
| Cabbage kimchi | 104 | 109 | (95·4) | 102 | 140 | (72·9) | 7·75 | (2·93–20·47) | 9·52 | (3·21–21·26 |
| School G | ||||||||||
| Rice | 17 | 17 | (100·0) | 57 | 58 | (98·3) | — | — | — | — |
| Salad | 12 | 13 | (92·3) | 47 | 55 | (85·5) | 2·04 | (0·23–17·95) | 2·92 | (0·23–19·25) |
| Bean sprouts | 8 | 15 | (53·3) | 20 | 55 | (36·4) | 2·00 | (0·63–6·34) | 3·20 | (0·78–6·49) |
| Cabbage kimchi | 15 | 16 | (93·8) | 35 | 58 | (60·3) | 9·86 | (1·22–79·81) | 12·37 | (2·47–82·31 |
OR, Odds ratio; aOR, adjusted odds ratio; CI, confidence interval.
Enteropathogenic E. coli isolated from cabbage kimchi in school A.
We identified six food companies that supplied food items to the seven schools. Of these, company X was the only food distributor that supplied radish kimchi and cabbage kimchi to all seven schools. Specimens were collected from more than six food materials from each company and from food-handlers; however, pathogens were only isolated from unprocessed food materials. Of the food items prepared and stored by company X, ETEC O169 was isolated from radish; and EPEC was isolated from cabbage. Company X produced kimchi products made with cabbage and radish, which were harvested from company-affiliated farms, then distributed to institutions located in the western districts of Seoul and Incheon City, in less-fermented style. The farm that grew cabbage and radish was not visited for inspection.
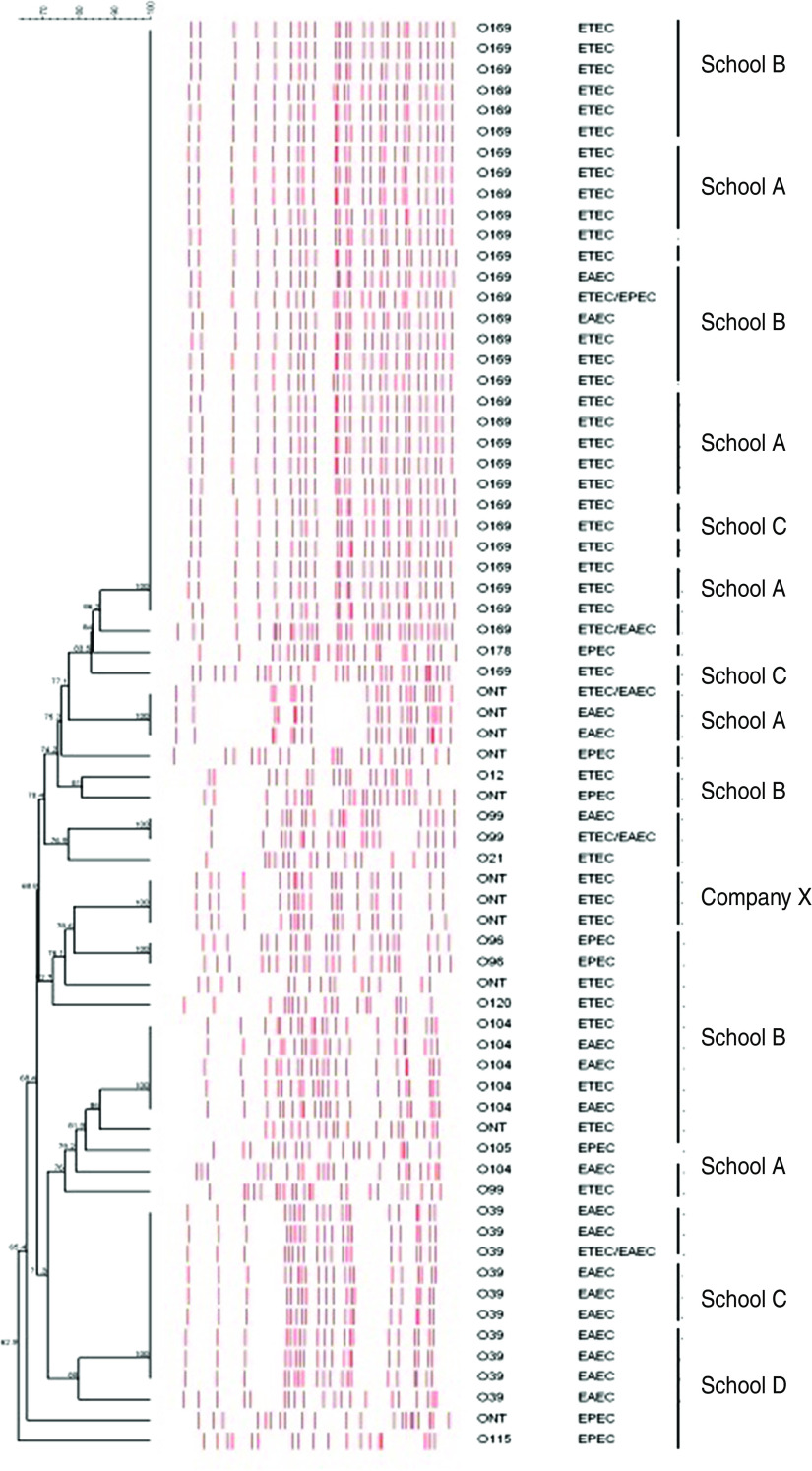
The school cafeterias in all seven schools were closed from 6 September, and drinking from water fountains was banned until microbiological test results became available. Active surveillance to monitor any patients with gastrointestinal symptoms and signs was initiated. When the results of the microbiological study became available, on 17 September, KFDA and Incheon City Department of Health jointly issued a press statement, on 19 September, notifying the public about the school ETEC O169 outbreak and the link to consumption of kimchi products from company X. Guidelines on how to prevent ETEC infection were also distributed. Figure 2 denotes phylogenetic analysis of multiple species of E. coli isolated from food specimens, stools, and foods from the schools and company X. The ETEC O169 outbreak isolates were closely related by PFGE analysis to the strain isolated from company X. Company X produced and delivered the same kimchi products to 14 other schools and five workplaces; however, no cases of ETEC occurring in students or workers in those places were identified and no cases were reported after 11 September 2012.
Fig. 2.
[colour online]. Cluster analysis of Enterotoxigenic Escherichia coli (ETEC) O169 enteritis outbreak isolates clustered by the unweighted method with pulsed-field gel electrophoresis patterns for available clinical and environmental isolates (n = 69), associated with consumption of kimchi in multiple schools, Republic of Korea in 2012.
DISCUSSION
In this report, we describe the first foodborne ETEC O169 enteritis outbreak identified in Korea. Eating kimchi, which was prepared in radish form (in schools B, C, D, E) or cabbage form (in schools A, F, G), was significantly associated with illness by both univariate and multivariate analyses. The outbreak affected 1642 individuals from seven schools in Incheon, and was linked to the consumption of contaminated kimchi products produced and delivered by a single food company. ETEC O169 isolates obtained from cases were indistinguishable by PFGE from isolates from kimchi products which were delivered to the schools.
The 2012 ETEC outbreak was different from the previous outbreak that occurred in Korea in two major aspects. First, active investigation with utilization of bacteriological tests and PFGE analysis was helpful in identifying the route of transmission and source of infection. Second, this outbreak illustrates the challenge posed by a single, food company-driven outbreak in catered school restaurants. Currently, in Korea, foods mostly come just a few central distribution companies and are widely distributed, indicating that a foodborne outbreak can spread quickly and widely. In this outbreak, the kimchi products were made by company X and were distributed to multiple different institutions comprising 21 schools and five workplaces, resulting in a large outbreak in seven schools within a relatively short period of time. Although the ultimate source of contamination in this outbreak is unknown, one possible hypothesis is that company X delivered kimchi that had not been processed after a sufficient period of ripening, hence there was increased opportunity for microbes to grow in the raw food materials such as cabbage and radish.
Kimchi is a traditional Korean dish made of fermented radish, cabbage or cucumber, with a mixture of seasonings. It is usually prepared during late autumn, stored in traditional jars underground or in special refrigerators designed for kimchi, then served as an everyday Korean dish throughout the year. If kimchi is properly fermented, the growth of microbiological pathogens is restricted; however, as seen in this outbreak, unfermented kimchi may cause bacterial overgrowth which may lead to kimchi-related outbreaks. In this outbreak, no other independent risk for food items other than kimchi was identified by multivariate analysis (except for rice and melon in some schools). The samples that yielded ETEC were the radish and cabbage forms of kimchi, not the raw vegetables. From the available information it is unclear whether raw food materials arrived at the plant already contaminated or if contamination occurred during the manufacturing of kimchi. Because kimchi is served almost every day with Korean meals, taking strong and specific action to identify and prevent contamination of raw kimchi materials by food companies is necessary for food safety control and prevention measures in Korea. Previously, other pathogens such as Shigella and norovirus have been reported as causes of kimchi-related outbreaks in Korea [7, 8].
Recently, other food materials such as salad, raw vegetables, and fruits are being recognized as sources of foodborne outbreaks in other cultures [9, 10]. The preparation of kimchi products requires the process of ripening and fermentation; insufficient ripening of kimchi may allow the pathogens to survive, emphasizing the need to define the exact criteria for the ripening process in kimchi-producing companies that supply products to schools and institutions. Unlike other E. coli subspecies, humans are known as the major reservoir of ETEC, and that contaminated hands or water are principal vehicles for its transmission [11]. Therefore, further studies on the manufacturing process and food handlers would be of importance in such kimchi-related ETEC outbreaks.
In Korea, ETEC was first detected in travellers with gastrointestinal symptoms who were investigated at an airport quarantine station [12]. The outbreak of ETEC was first observed in 2006, in a high school, through a contaminated water tank [13]. However, since ETEC infection is not a reportable infectious disease, the magnitude of its burden in Korea is not clearly understood. Furthermore, because isolation of ETEC has not been routinely performed in outbreak investigations, the recent increased number of outbreak reports may not represent the recent increase in the burden of ETEC in Korea.
PFGE analysis of E. coli became available in Korea in the mid-1990s, but is still not used widely in the clinical setting. However, in the public health sector PFGE is now recognized as a valuable tool for identifying the source of transmission, and has been widely applied in outbreak investigations. However, its use has not been described or systematically evaluated as an important public health tool for actual use in Korea. The current investigation sought to characterize and describe the utilization of PFGE during an ETEC outbreak, and discuss its usefulness in strengthening evidence that support epidemiological findings.
This investigation has a number of potential limitations. First, we used data collected through passive reporting, potentially under-estimating actual cases, which may lead to incorrect interpretation of relative risks and odds ratios. It is possible that a student with minor symptoms will not report to the public health authorities. Second, because more symptomatic infections are more likely to be reported, our data may not provide the proportion of actual clinical features in all ETEC-infected individuals. Despite these potential limitations, this investigation has certain strengths. First, active utilization and enhancing of laboratory testing led to the rapid identification of the outbreak and cause of illness. Second, rapid initiation of the outbreak investigation, and alerting consumers earlier than before, may have helped in preventing more illness in other exposed institutions.
In this report, we sought to describe an outbreak of ETEC O169 enteritis in multiple schools through summarizing epidemiological data, and to identify the source of infections. Our investigation indicates that the risk of a kimchi-borne outbreak of ETEC O169 infection is present in Korea, and highlights the need of further surveillance of food safety in schools and workplaces. Further, it remains important to assess the safety of foods served in schools and workplaces in order to increase public confidence in food safety outside the home. We recommend continued monitoring of food safety in Korea, and strengthening surveillance regarding ETEC O169 infection through the implementation of active laboratory surveillance to confirm its infection.
ACKNOWLEDGEMENTS
We are grateful to public health workers in Incheon City for their contribution to the investigation of this outbreak.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Kiers JL, et al. Effect of processed and fermented soyabeans on net absorption in enterotoxigenic Escherichia coli-infected piglet small intestine. British Journal of Nutrition 2006; 95: 1193–1198. [DOI] [PubMed] [Google Scholar]
- 2.Jain S, et al. An outbreak of enterotoxigenic Escherichia coli associated with sushi restaurants in Nevada, 2004. Clinical Infectious Diseases 2008; 47: 1–7. [DOI] [PubMed] [Google Scholar]
- 3.Dalton CB, et al. Outbreaks of enterotoxigenic Escherichia coli infection in American adults: a clinical and epidemiologic profile. Epidemiology and Infection 1999; 123: 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishikawa Y, et al. Epidemiology and properties of heat-stable enterotoxin-producing Escherichia coli serotype O169:H41. Epidemiology and Infection 1998; 121: 31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beatty ME, et al. Enterotoxin-producing Escherichia coli O169:H41, United States. Emerging Infectious Diseases 2004; 10: 518–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwun JW, Lee CH. Trends of recent food-borne disease outbreaks in Korea. Journal of Korean Medical Association 2007; 50: 573–81. [Google Scholar]
- 7.Min YS, et al. Epidemiologic investigation on an outbreak of shigellosis in Seongju-gun, Korea, 2003. Journal of Preventive Medicine and Public Health 2005; 38: 189–196. [PubMed] [Google Scholar]
- 8.Yu JH, et al. Epidemiology of foodborne Norovirus outbreak in Incheon, Korea. Journal of Korean Medical Science 2010; 25: 1128–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Little CL, Gillespie IA. Prepared salads and public health. Journal of Applied Microbiology 2008; 105: 1729–1743. [DOI] [PubMed] [Google Scholar]
- 10.Long SM, et al. General outbreaks of infectious intestinal disease linked with salad vegetables and fruit, England and Wales, 1992–2000. Communicable Disease and Public Health 2002; 5: 101–105. [PubMed] [Google Scholar]
- 11.Olsvik O, et al. Pathogenic Escherichia coli found in food. International Journal of Food Microbiology 1991; 12: 103–113. [DOI] [PubMed] [Google Scholar]
- 12.Jeon S, et al. Detection of the causative agents of traveler's diarrhea using a real-time PCR Screening Method. Korean Journal of Clinical Microbiology 2009; 12: 186–192. [Google Scholar]
- 13.Park S, et al. Enterotoxigenic Escherichia coli outbreak in a high school. Infection and Chemotherapy 2006; 38: 30–38. [Google Scholar]