SUMMARY
This study aimed to describe Toxoplasma gondii prevalence in Polish pregnant women and the incidence rates of congenital infections in their neonates observed between 2004 and 2012. Serological tests for T. gondii-specific IgG and IgM antibodies were performed on serum samples of 8281 pregnant women treated at the Polish Mother's Memorial Hospital Research Institute in Lodz. The yearly seroconversion rate for T. gondii IgG antibodies was estimated using a mathematical model to determine the dependency between age and prevalence. Mean prevalence of IgG antibodies between 2004 and 2012 in pregnant women was 40·6% [95% confidence interval (CI) 39·6–41·7] and increased with age with a yearly seroconversion rate of 0·8% (95% CI 0·6–1·0, P < 0·001). Assuming a T. gondii materno-fetal transmission rate of 30% gave an estimate of 1·80/1000 neonates as congenitally infected. The increased mean age (28·7 vs 26·7 years, P < 0·001) of pregnant women was probably the most important factor in abolishing the effect of falling prevalence rates.
Key words: IgG, IgM, materno-fetal transmission, pregnancy, prevalence, Toxoplasma gondii, toxoplasmosis
INTRODUCTION
Infections with Toxoplasma gondii are distributed globally in people and animals such as rats, dogs, cats, sheep, hens and pigs [1, 2]. Contamination with this parasite is usually long-lasting and asymptomatic [3]. However, it causes serious clinical symptoms such as congenital ocular and neurotoxoplasmosis and affects immunosuppressed patients [3]. Particularly dangerous are primary infections in pregnant women, causing transmission of T. gondii through the placenta to the fetus and congenital infections with a severe, sometimes fatal course [4]. The consumption of raw or undercooked meat and unwashed raw vegetables or fruits were reported as eating habits being important risk factors for toxoplasmosis [1, 5]. Enhanced risk of T. gondii infection is also associated with older gestational age at the time of maternal infection, although the risk of serious consequences then decreases [6]. Of socioeconomic risk factors determined were occupational exposure to parasite tissue cysts and oocysts, health status, living in urban or rural areas, frequent exposure to feline faeces, and low educational level [1, 7].
Prevalence of T. gondii varies between and within different countries depending on both region and ethnicity [8, 9]. Prevalence rates in seropositive pregnant women have been reported from 4% to 100% with values over 60% in Central and South America, Africa and Asia [8, 9]. Serological analyses conducted in people living in Polish regions showed high prevalence rates in women of Przodkowo commune from Pomorskie province (54·4%), forestry workers from Pomorskie and Warmińsko-Mazurskie provinces (62·5%) and in pregnant women (41·3%) [10–12]. The past few decades brought a considerable decrease in prevalence of T. gondii observed in different countries worldwide [8]. In Poland a similar trend in seroprevalence was found, with a significant decrease from 45·4% in 1998 to 39·4% in 2003, with an annual decline of 1% observed in pregnant women [10]. Of 1920 pregnant women treated in 1998 the prevalence of T. gondii IgG without IgM antibodies was 43·4% [13].
Toxoplasmosis is severe threat during pregnancy. Seroepidemiological monitoring of pregnant women is undoubtedly needed to develop educational programmes on risk of T. gondii infections in pregnant women and strategies to prevent congenital toxoplasmosis [14, 15]. In this study, we investigated the prevalence of specific T. gondii IgG antibodies in a group of pregnant women from Poland admitted to the Polish Mother's Memorial Hospital Research Institute in Lodz between 2004 and 2012.
MATERIALS AND METHODS
During a 9-year period (2004–2012) a total of 8281 pregnant women treated at the Polish Mother's Memorial Hospital Research Institute in Lodz, participated in this study. The patients came from Lodzkie province and other Polish regions, as the Institute is a specialist perinatal care centre. Currently, the Polish Society of Gynecology recommends serological testing for T. gondii infections for pregnant women within the first trimester and in negative individuals in the third trimester. However, screening for T. gondii is still not mandatory in Poland.
Serological tests
Blood samples were taken from all pregnant women participating in the study by venepuncture during the first visit to the Institute. Serum fractions were gained by centrifugation and stored at 4°C until analysis within 2 days. Serological tests were performed in the Department of Clinical Microbiology at the Institute.
Screening for T. gondii IgG antibodies was performed with an enzyme-linked fluorescent assay (ELFA) (Vidas Toxo IgG II, bioMérieux, France), using 4 IU/ml as the cut-off point. Detection of IgM antibodies was performed with an ELFA assay (Vidas Toxo IgM, bioMérieux). Samples with indexes ⩾0·65 were considered as positive. Determination of T. gondii IgG avidity was performed using an ELFA assay (Vidas Toxo IgG Avidity, bioMérieux). Samples with indexes <0·200 were interpreted as low avidity, 0·200–0·300 as borderline avidity, and ⩾0·300 as high avidity.
Statistical analysis
The yearly seroconversion rate for T. gondii IgG antibodies was estimated using a mathematical model to determine the dependency between age and prevalence. The linear trend for age was calculated by binomial regression with identity link. Departures from the linear trend for age were performed using quadratic orthogonal trend for age. For prevalence, 95% confidence intervals (CIs) were estimated, assuming binomial distribution. We tested the interaction between age and period for prevalence between 2004 and 2012. We included main effect for age group (18–25, 26–35, 36–47 years) and continuous period, and their interaction. Differences in prevalence rates and age of pregnant women, observed between 1998–2003 and 2004–2012 periods were tested using interaction term in binomial regression. Period variable was categorical and age was continuous.
All results were determined as statistically significant at the significance level P ⩽ 0·05 for main effects and P ⩽ 0·1 for interaction terms. Data were analysed using Stata v. 11 software (StataCorp., USA).
RESULTS
Prevalence rates in pregnant women of different age
T. gondii IgG antibodies were identified in 40·6% (3364/8281, 95% CI 39·6–41·7) of pregnant women aged between 18 and 47 years (mean age 28·7 years).
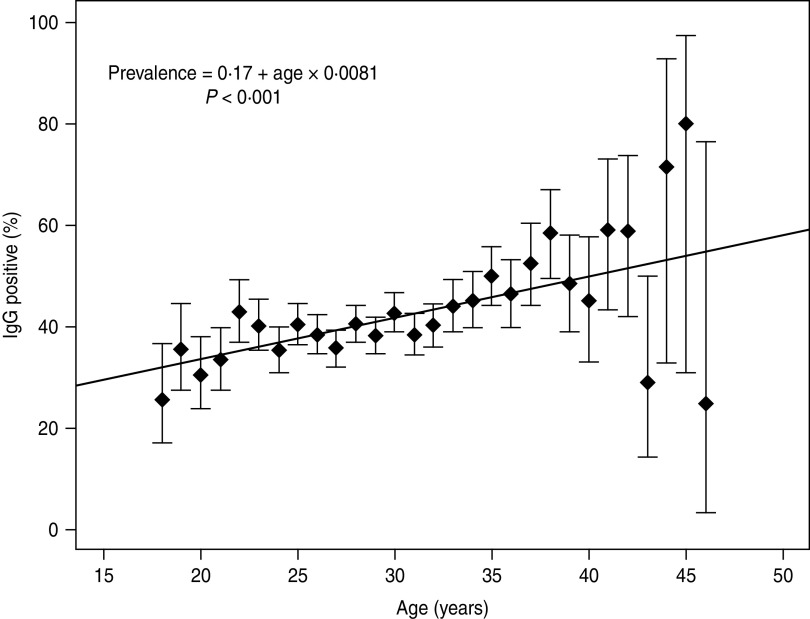
The prevalence of IgG antibodies related to age is indicated in Figure 1. The incidence rate of T. gondii IgG increased significantly with a yearly seroconversion rate of 0·8% (95% CI 0·6–1·0, P ⩽ 0·001). Departure from the linear trend was not significant (P = 0·117). The highest mean prevalence was observed for women aged 45 years (80%, 95% CI 30·9-97·3); however, the number of pregnant women aged >40 years was smaller compared to other studied patients (114 vs. 8167) (Fig. 1). In the group of older pregnant women (n = 114), the wider 95% CIs for prevalence ranged from 24·3% to 72·8%. For women aged <40 years (n = 8167) the mean prevalence values for particular age groups were between 25·7% and 48·6% and for prevalence the 95% CIs ranged from 7·0% to 19·8% (Fig. 1).
Fig. 1.
Incidence rate of Toxoplasma gondii IgG in 8281 pregnant women; estimation model based on the dependency between age and prevalence, with a yearly seroconversion rate of 0.8%.
The estimation of morbidity
Taking into account a yearly seroconversion rate of 0·8%, the estimated risk of primary infection with T. gondii was 0·6% (0·8% × (9/12)). Hence, the risk of acquiring infection during pregnancy was 6/1000 pregnancies. For the whole studied cohort of pregnant women we estimated 49·7 cases to be primary infections during pregnancy.
It is estimated that about 14%, 29% and 59% of newborns of mothers with T. gondii primary infection within the first, second and third trimester of pregnancy, respectively, would be infected [6]. Hence, in the analysed population seven (0·85/1000), 14·4 (1·74/1000) and 29·3 (3·54/1000) neonates would be infected in utero during the first, second and third trimester of pregnancy, respectively. Considering that the reported materno-fetal adjusted mean transmission rate of 19·5% occurred from 3 to 34 weeks of pregnancy, 9·7 neonates (1·17/1000) would be expected to have congenital toxoplasmosis in the studied group [6]. However, the transmission rate after 34 weeks of pregnancy should also be considered, therefore we took into account the mean materno-fetal transmission rate of 30% as the most accurate coefficient and calculated that 14·9 neonates (1·80/1000) would be congenitally infected [16].
Assuming 95% CIs for a yearly seroconversion rate of 0·8%, the calculated rate ranged from 0·6 to 1·0. Considering this range the risk for primary infection during pregnancy would be 0·45-0·75% that means that 4·5–7·5 primary-infected pregnant women per 1000 treated individuals. Hence, in the analysed group from 37·3 to 62·2 pregnant women would have a primary infection. Considering a materno-fetal transmission rate of 30%, about 11·2 (1·4/1000) to 18·7 (2·3/1000) newborns would be infected in utero.
Prevalence rates between 2004 and 2012
Between 2004 and 2012 the prevalence of T. gondii decreased from 41·8% (95% CI 37·7-46·1) to 37·8% (95% CI 32·3-43·5) (Table 1). A decreasing, but not significant trend in prevalence of T. gondii was observed (4%, P = 0·103). It was observed in particular for pregnant women aged 20–35 years. After adjustment for age the annual decline was higher and significant (5%, P = 0·025). For particular age groups the trend ranged from −0·010 to −0·001. However, the yearly trend was homogenous across age groups (P = 0·490). A continuously increasing age of pregnant women (from 28·0 to 29·7 years, mean 28·7 years) was observed.
Table 1.
Prevalence of Toxoplasma gondii IgG antibodies in pregnant women tested in Lodz, Poland, between 2004 and 2012
| Year | Study population | IgG positive | Mean age (years) | ||
|---|---|---|---|---|---|
| n | % | 95% CI | |||
| 2004 | 526 | 220 | 41·8 | 37·7–46·1 | 28·0 |
| 2005 | 1262 | 518 | 41·0 | 38·4–43·8 | 28·3 |
| 2006 | 1191 | 481 | 40·4 | 37·6–43·2 | 28·2 |
| 2007 | 1048 | 453 | 43·2 | 40·2–46·2 | 28·7 |
| 2008 | 1050 | 435 | 41·4 | 38·5–44·4 | 28·8 |
| 2009 | 1013 | 380 | 37·5 | 34·6–40·5 | 28·9 |
| 2010 | 899 | 389 | 43·3 | 40·1–46·5 | 29·0 |
| 2011 | 1006 | 380 | 37·8 | 34·8–40·8 | 29·2 |
| 2012 | 286 | 108 | 37·8 | 32·3–43·5 | 29·7 |
| Total | 8281 | 3364 | 40·6 | 39·6–41·7 | 28·7 |
n, Number of women; CI, confidence interval.
Prevalence of IgM antibodies
T. gondii IgM antibodies were identified in 9·7% of studied pregnant women (95% CI 9·1–10·3). Of these women 0·3% were IgM positive without IgG and 9·4% were IgM positive with IgG.
Prevalence rates occurring between 1998–2003 and 2004–2012
Compared to our earlier results, obtained for pregnant women treated between 1998 and 2003 at the same Institute and admitted to the study based on the same criteria, the current yearly seroconversion rate of T. gondii IgG antibodies between 2004 and 2012, was a little higher (0·8% vs. 0·7%) [10]. These small discrepancies were not significant (P = 0·528). Simultaneously, we observed a significantly higher prevalence of T. gondii IgM antibodies (9·7 vs. 4·9%, P ⩽ 0·001). The mean age of pregnant women treated between 2004 and 2012 was also significantly higher compared to patients from the earlier period (28·7 vs 26·7 years, P ⩽ 0·001, data not shown).
DISCUSSION
In women at childbearing age T. gondii prevalence differs from 9% in the UK, 12% in Eastern Spain, 21% in Italy, 24% in the North of Portugal to 41% in Poland, 44% in France and 49% in Albania [9, 17–22]. In this study we observed the prevalence rate to be 40·6% of 8281 pregnant women. Taking into account data obtained for pregnant women treated at the same Institute from 1998 to 2003 (41·3%), current prevalence rates were slightly lower, but still high compared to other European countries [10]. A similarly low decreasing trend was observed in Croatia, where a prevalence of 29·1% was observed for pregnant women treated from 2005 to 2009 was similar to that of 31·4% described in 2002 [23]. However, for the period between 2004 and 2012, we observed a decreased IgG prevalence from 41·8% to 37·8%. The decreasing trend was not significant, but after adjustment for age of pregnant women, the annual decline was higher (5% vs. 4%) and significant. Decrease in toxoplasmosis seropositivity was also observed for other European countries like Austria (from 48% to 50% at the end of the 1970s to 31-35% in recent years), North of Portugal (31·4% in 2005 to 24·4% in 2010), Italy (31·4% in 2001 to 21·4% in 2005) and The Netherlands (35·2% in 1995/1996 to 18·5% in 2006/2007) [18, 21, 24–26].
Considering the age of the studied pregnant women, we calculated a yearly T. gondii IgG seroconversion rate of 0·8%. Based on the estimation model, the prevalence rates increased with age in a linear manner. A similar association between age and seroprevalence was also observed in our earlier study (seroconversion rate of 0·7%) and in other countries [8, 10]. The linear trend remained in accordance with changes observed for pregnant women treated in Upper Austria between 2000 and 2007 [26]. However, in that population, the seroconversion rate was lower than observed in our study (0·5% vs. 0·8%). It should be noted that the median age of Austrian women (28·3 years) was comparable to the mean age of the Polish pregnant women (28·7 years) [26]. A similar mean age of pregnant women was also observed in other populations including Spaniards (29·9 years for native-born, 28·4 for migrants), French (29·5 years), Hungarians (27·7 years), and Albanians (27 years) [9, 19, 27, 28]. Compared to our study from 2006, the currently observed mean age of pregnant women was significantly higher (28·7 vs. 26·7 years) [10]. Hence, it is plausible that in the Polish population the effect of falling prevalence rates is abolished by the elevated age of pregnant women.
Simultaneously to a decrease in the IgG prevalence rate, we observed significantly elevated prevalence of IgM antibodies (9·7% vs. 4·9%). This is similar to that described in pregnant women in Austria and Kosovo [24, 29]. In pregnant women from Austria the IgG prevalence decreased from 48% to 50% and then to 35% which was accompanied by an increase in IgM prevalence from 0·4% to 0·83% [24]. In pregnant women in Kosovo the IgG seroprevalence of 29·4%, lower than found in other European countries, was observed in parallel with a relatively high IgM seropositivity of 4·1% [29]. The IgM prevalence observed in Polish pregnant women is much higher compared to the incidence from other countries including rates of 2% or 4·1% in North of Portugal, 0·8% in central Italy and 0·9% or 1·2% in Legnano in Italy [18, 21, 30]. The much lower estimated incidence of primary infection compared to the observed IgM prevalence (9·7% vs. 0·6%) probably results from the persistence of IgM antibodies for at least 1 year after contamination [10]. The frequency of IgM-positive women without specific IgG was much lower than for those with IgG (0·3% vs. 9·4%). In the population studied in this work, the unexpected increased prevalence rate of IgM antibodies observed simultaneously with the increasing age of pregnant women, and the IgG prevalence elevated with age, indicate increasing age of pregnant women as the most important factor affecting the prevalence rate in pregnant women from Poland. High prevalence of IgM antibodies probably results from their persistence in the host organism for several years after primary infection. We also think that discrepancies between our current and earlier studies might result from differential serological tests used to identification of IgM antibodies. Before March 2000, the serological status of IgM was determined with Platelia Toxo-M assay (Diagnostics Sanofi Pasteur, France). Of four different tests, including two used in our studies, the currently applied Vidas Toxo IgM (bioMérieux) was shown to provide the highest positive predictive value (80·8%) and specificity (99·3%) [31].
We calculated that for the studied Polish pregnant women about 14·9 neonates would be congenitally infected, that means 1·80 infected newborns for every 1000 live births. To date, various mother-to-child transplacental T. gondii transmission rates have been reported, ranging from 0% in case of maternal infection acquired before gestation to 67%, when infection was acquired between weeks 31 and 34 [6]. Hence, similar to our earlier study, we assumed the mean transmission rate of 30% as the most accurate coefficient for calculation of congenital infection incidence. Compared to limited data from other European countries, the estimated incidence rate of congenital toxoplasmosis in Polish neonates is lower than that found in Italy (9–35/1000), The Netherlands (2·2/1000) or Kosovo (0·2–2·0/1000), but higher than in France (0·3/1000), Austria (0·1/1000) or Ireland (0·1/1000) [22, 24, 25, 29, 30, 32, 33]. Based on our results, the incidence of congenital toxoplasmosis in neonates in Poland is still unfortunately high. The current calculated higher morbidity rate in neonates compared to values from our earlier study (1·80% vs. 1·50%) might be reasoned from the origin of samples, which were collected at a referral centre in Poland as well as from the altered sensitivity of applied serological tests.
T. gondii prevalence in pregnant women in Poland is still high, although a decreasing linear trend in age-adjusted IgG prevalence was found. The observed increased prevalence of IgM antibodies is of particular concern, as it might reflect the elevated level of primary infections in pregnant women during recent years. Both the use of primary prophylactics to increase the awareness of the risk of T. gondii infections in Polish women of childbearing age and secondary prevention by serological testing are absolutely necessary to prevent further spread of the pathogen in future mothers and the development of congenital infections in their babies.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Bojar I, Szymanska J. Environmental exposure of pregnant women to infection with Toxoplasma gondii – state of the art. Annals of Agricultural and Environmental Medicine 2010; 17: 209–214. [PubMed] [Google Scholar]
- 2.Pezzoli L, et al. Toxoplasmosis in Italian pregnant women: results of a survey on perception of foodborne risks. Journal of Food Protection 2009; 72: 680–684. [DOI] [PubMed] [Google Scholar]
- 3.Silva CH, et al. Early diagnosis of congenital toxoplasmosis in newborn infants using IgG subclasses against two Toxoplasma gondii recombinant proteins. Memórias do Instituto Oswaldo Cruz 2012; 107: 342–347. [DOI] [PubMed] [Google Scholar]
- 4.Nowakowska D, et al. Too late prenatal diagnosis of fetal toxoplasmosis: a case report. Fetal Diagnosis and Therapy 2005; 20: 190–193. [DOI] [PubMed] [Google Scholar]
- 5.Gao XJ, et al. Toxoplasma gondii infection in pregnant women in China. Parasitology 2012; 139: 139–147. [DOI] [PubMed] [Google Scholar]
- 6.Remington JS, et al. Toxoplasmosis. In: Remington JS, Klein JO, eds. Infectious Diseases of the Fetus and Newborn Infant. Philadelphia: Saunders, 2011, pp. 918–1041. [Google Scholar]
- 7.Alvarado-Esquivel C, Estrada-Martinez S, Liesenfeld O. Toxoplasma gondii infection in workers occupationally exposed to unwashed raw fruits and vegetables: a case control seroprevalence study. Parasites & Vectors 2011; 4: 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. International Journal of Parasitology 2009; 39: 1385–1394. [DOI] [PubMed] [Google Scholar]
- 9.Ramos JM, et al. Seroprevalence of Toxoplasma gondii infection among immigrant and native pregnant women in Eastern Spain. Parasitology Research 2011; 109: 1447–1452. [DOI] [PubMed] [Google Scholar]
- 10.Nowakowska D, et al. Prevalence and estimated incidence of Toxoplasma infection among pregnant women in Poland: a decreasing trend in the younger population. Clinical Microbiology and Infection 2006; 12: 913–917. [DOI] [PubMed] [Google Scholar]
- 11.Holec-Gasior L, Kur J. Epidemiological studies of toxoplasmosis among women from Przodkowo commune. Przegląd Epidemiologiczny 2009; 63: 311–316. [PubMed] [Google Scholar]
- 12.Holec-Gasior L, et al. Occurrence of Toxoplasma gondii specific antibodies in group of forestry workers from Pomorskie and Warminsko-Mazurskie provinces. Wiadomości Parazytologiczne 2008; 54: 231–236. [PubMed] [Google Scholar]
- 13.Nowakowska D, et al. Anti – T. gondii antibody concentration in sera of pregnant women in the sample of Lodz population. Wiadomości Parazytologiczne 2001; 47 (Suppl. 1): 83–89. [PubMed] [Google Scholar]
- 14.Gollub EL, et al. Effectiveness of health education on Toxoplasma-related knowledge, behaviour, and risk of seroconversion in pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology 2008; 136: 137–145. [DOI] [PubMed] [Google Scholar]
- 15.Benard A, et al. Survey of European programmes for the epidemiological surveillance of congenital toxoplasmosis. Eurosurveillance 2008; 13: 18834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Remington JM, et al. Toxoplasmosis. In: Remington JS, Klein JO, eds. Infectious Diseases of the Fetus and Newborn Infant. Philadelphia: Saunders, 2001, pp. 204–346. [Google Scholar]
- 17.De PM, et al. Implementation of screening for Toxoplasma gondii infection in pregnancy. Journal of Clinical Medicine Research 2010; 19: 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopes AP, et al. Seroepidemiology of Toxoplasma gondii infection in women from the North of Portugal in their childbearing years. Epidemiology and Infection 2012; 140: 872–877. [DOI] [PubMed] [Google Scholar]
- 19.Maggi P, et al. Surveillance of toxoplasmosis in pregnant women in Albania. New Microbiologica 2009; 32: 89–92. [PubMed] [Google Scholar]
- 20.Nash JQ, et al. Risk factors for toxoplasmosis in pregnant women in Kent, United Kingdom. Epidemiology and Infection 2005; 133: 475–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pinto B, et al. Seroprevalence for toxoplasmosis in individuals living in north west Tuscany: access to Toxo-test in central Italy. European Journal of Clinical Microbiology and Infectious Diseases 2012; 31: 1151–1156. [DOI] [PubMed] [Google Scholar]
- 22.Villena I, et al. Congenital toxoplasmosis in France in 2007: first results from a national surveillance system. Eurosurveillance 2010; 15: 19600. [DOI] [PubMed] [Google Scholar]
- 23.Vilibic-Cavlek T, et al. Seroprevalence of TORCH infections in women of childbearing age in Croatia. Journal of Maternal-Fetal and Neonatal Medicine 2011; 24: 280–283. [DOI] [PubMed] [Google Scholar]
- 24.Edelhofer R, Prossinger H. Infection with Toxoplasma gondii during pregnancy: seroepidemiological studies in Austria. Zoonoses. Public Health 2010; 57: 18–26. [DOI] [PubMed] [Google Scholar]
- 25.Hofhuis A, et al. Decreased prevalence and age-specific risk factors for Toxoplasma gondii IgG antibodies in The Netherlands between 1995/1996 and 2006/2007. Epidemiology and Infection 2011; 139: 530–538. [DOI] [PubMed] [Google Scholar]
- 26.Sagel U, Kramer A, Mikolajczyk RT. Incidence of maternal Toxoplasma infections in pregnancy in Upper Austria, 2000–2007. BMC Infectious Diseases 2011; 11: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beke A, et al. Comparison of prevalence of toxoplasma and cytomegalovirus infection in cases with fetal ultrasound markers in the second trimester of pregnancy. Prenatal Diagnosis 2011; 31: 945–948. [DOI] [PubMed] [Google Scholar]
- 28.Cornu C, et al. Factors affecting the adherence to an antenatal screening programme: an experience with toxoplasmosis screening in France. Eurosurveillance 2009; 14: 21–25. [PubMed] [Google Scholar]
- 29.Dentico P, et al. Toxoplasmosis in Kosovo pregnant women. New Microbiologica 2011; 34: 203–207. [PubMed] [Google Scholar]
- 30.De PM, et al. Seroprevalence and incidence of Toxoplasma gondii infection in the Legnano area of Italy. Clinical Microbiology and Infection 2008; 14: 186–189. [DOI] [PubMed] [Google Scholar]
- 31.Hofgartner WT, et al. Detection of immunoglobulin G (IgG) and IgM antibodies to Toxoplasma gondii: evaluation of four commercial immunoassay systems. Journal of Clinical Microbiology 1997; 35: 3313–3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferguson W, et al. Lack of awareness of risk factors for primary toxoplasmosis in pregnancy. Irish Journal of Medical Science 2011; 180: 807–811. [DOI] [PubMed] [Google Scholar]
- 33.Ricci M, et al. Screening and prevention of congenital toxoplasmosis: an effectiveness study in a population with a high infection rate. Journal of Maternal-Fetal and Neonatal Medicine 2003; 14: 398–403. [DOI] [PubMed] [Google Scholar]