SUMMARY
We studied the association between drinking water, agriculture and sporadic human campylobacteriosis in one region of British Columbia (BC), Canada. We compared 2992 cases of campylobacteriosis to 4816 cases of other reportable enteric diseases in 2005–2009 using multivariate regression. Cases were geocoded and assigned drinking water source, rural/urban environment and socioeconomic status (SES) according to the location of their residence using geographical information systems analysis methods. The odds of campylobacteriosis compared to enteric disease controls were higher for individuals serviced by private wells than municipal surface water systems (odds ratio 1·4, 95% confidence interval 1·1–1·8). In rural settings, the odds of campylobacteriosis were higher in November (P = 0·014). The odds of campylobacteriosis were higher in individuals aged ⩾15 years, especially in those with higher SES. In this region of BC, campylobacteriosis risk, compared to other enteric diseases, seems to be mediated by vulnerable drinking water sources and rural factors. Consideration should be given to further support well-water users and to further study the microbiological impact of agriculture on water.
Key words: Agriculture, Campylobacter, epidemiology, geographical information systems, water (safe)
INTRODUCTION
Campylobacteriosis is the most commonly reported bacterial enteric infection in humans throughout the world [1]. It causes severe abdominal pain, diarrhoea of several days' duration and can lead to Guillain–Barré syndrome, reactive arthritis, irritable bowel syndrome and, rarely, death [2]. About 50% of human cases are attributable to the consumption and handling of contaminated poultry; an additional 10–25% of cases are attributable to poultry through direct (e.g. animal contact) and indirect (e.g. drinking water) means [3–6]. Recent models propose various complex transmission pathways of Campylobacter from animals and the environment to humans [1, 7].
In Canada, the province of British Columbia (BC) (population 4·5 million) reported an annual average of 38·0/100000 cases of campylobacteriosis between 2005 and 2009, among the highest in the country [8]. In BC, several epidemiological studies have considered the role of the environment in human Campylobacter infection. One study showed the risk of sporadic campylobacteriosis to be eight times higher in people living in areas serviced by private single-dwelling wells compared to those on municipal water systems [9]. Another study found the risk of campylobacteriosis was higher in urban areas and areas with high poultry density [10]. Finally, comparing locally acquired and travel-associated Campylobacter infections found higher odds of local infection in males, older people, those living in rural areas or close to Agricultural Land Reserves (ALRs), and in the warmer months [11]. Some of these results are contradictory, which may be due to the fact that exposures have not yet been considered in combination or sequentially.
We conducted a study to improve our understanding of the non-foodborne transmission pathways of Campylobacter. We studied the combined effects of geographical factors, including drinking water and proximity to agriculture, associated with sporadic human campylobacteriosis in one region of BC, taking into account sociodemographic factors that may bias such associations. We hypothesized that campylobacteriosis is associated with exposure to undertreated drinking water contaminated through agricultural animal sources.
METHODS
A case-case design was used to compare reported cases of campylobacteriosis to other cases of reportable enteric diseases, referred to as enteric disease controls. All laboratory-confirmed cases of reportable enteric disease are reported from local BC laboratories to local health authorities and then to the BC Centre for Disease Control (BCCDC). Epidemiological data transferred on each case to the provincial level include age, sex, address of residence and ‘episode date’ (the earliest of onset, collection or reporting date). We did not have access to interview-based exposure information such as travel status, drinking water consumed or whether cases were part of a known outbreak.
We extracted all cases reported between 2005 and 2009 in the Fraser Health Authority (FHA) from the provincial database. This region encompasses 1·6 million people in an area east of the City of Vancouver and includes urban, semi-rural and rural settings [12]. It is the major poultry-growing region of the province. The drinking water supply includes 19 municipal systems and 450 smaller systems using surface, ground or mixed sources. These municipal and small water systems serve 95% and 1% of the population, respectively. The remaining 4% of the population obtain their drinking water primarily from ground water sources (private wells), for which owners are responsible for testing and treating [13].
In order to determine drinking water at patient's address of residence, we geocoded (assigned geographical coordinates to) cases and drinking water systems. All geocoding, spatial data analysis, and spatial database management were performed using ArcGIS v. 10·0 (ESRI, USA). Cases were geocoded by exact address of residence at the time of illness using a reference land parcel database [14]. If exact address matching could not be accomplished, street address range interpolation or six-digit postal code geocoding was performed.
A spatial database was created to assign drinking water data to each case, via their address of residence, using spatial overlay and join functions, according to a previous study [9]. Drinking water system management data (i.e. whether the water was on a municipal or a private system) were acquired for every land parcel from the 19 municipalities and two regional districts in the region. We excluded non-residential land parcels. Households that were not on a municipal or specific private system were deemed to have a private well. This was verified using the BC WELLS database [15]. We obtained information on the source of water for each system from FHA. A drinking water index was created taking into account system management (municipal or private) and drinking water source (ground, surface or mixed). Drinking water treatment data were assessed but deemed incomplete and not included in the analysis.
Geographical information systems (GIS)-based analyses were used to calculate proximity to the nearest ALR and nearest abattoir. ALR data were obtained from the Provincial Agricultural Land Commission, and abattoir data from the Canadian Food Inspection Agency and the BCCDC [16, 17]. Cases and controls were classified as living within or further than 2 km from an ALR, as previously validated [11, 18]. Distance to the nearest poultry abattoir and the nearest red meat abattoir was calculated for each case and control. An urban environment was defined as having a minimum population concentration of 1000 and a population density of > 400/km2; all other areas were defined as rural [19]. The material component of the 2006 Deprivation Index (DI) for Health Planning, based on education, employment and income indicators, was divided into tertiles and used as the socioeconomic status (SES) measure at the dissemination area census geographical unit [20, 21]. We assigned rural/urban environment and SES to each household using GIS-based spatial join functions.
Univariate analyses and multivariate logistic regression were conducted using SAS v. 9·3 (SAS Institute Inc., USA). Univariate comparisons between cases and controls were based on likelihood ratio χ2 tests (comparing proportions) and t tests allowing unequal variance (comparing continuous measures). Multivariate analyses treated ‘status’ (campylobacteriosis case or control enteric disease) as the binary dependent variable and included water index (surface/municipal, mixed/municipal, ground-well/municipal, ground-well/private), age (0–14 or ⩾15 years), sex (male/female), urban area (yes/no), DI, average distance to the nearest abattoir, distance to nearest ALR (0–2 km or > 2 km) and month as categorical explanatory variables. The best fit model was based on backwards stepwise elimination of non-significant (alpha = 0·05) effects from the full model, which included all main effects and two-way interactions. At each step, goodness-of-fit statistics (Akaike's Information Criterion) were examined to confirm adequacy of model fit. This approach analyses the odds of campylobacteriosis infection relative to all other enteric diseases and assesses statistical significance using the likelihood ratio χ2 statistic.
Ethics approval was received from the University of British Columbia (certificate no. H11-00430).
RESULTS
Between 2005 and 2009, 2992 campylobacteriosis cases and 4816 enteric disease controls were reported in FHA and included in the study. Enteric disease controls included cases of amoebiasis (n = 603), cryptosporidiosis (n = 209), cyclosporiasis (n = 76), shiga-toxigenic E. coli infection (n = 261), giardiasis (n = 1244), listeriosis (n = 16), salmonellosis (n = 1410), shigellosis (n = 372), Vibrio infection (n = 38), and yersiniosis (n = 587). During this period, 1800 Campylobacter isolates from across BC were speciated by the BC Public Health Microbiology and Reference Laboratory (BCPHMRL): 91·3% were C. jejuni, 5·8% were C. coli and 2·9% were other species (personal communication, 20 Dec. 2013: Dr Linda Hoang, Program Head, Public Health Advanced Bacteriology/Mycology Laboratory, BCPHMRL). There were no known outbreaks of waterborne disease or Campylobacter infection in this region during the study period.
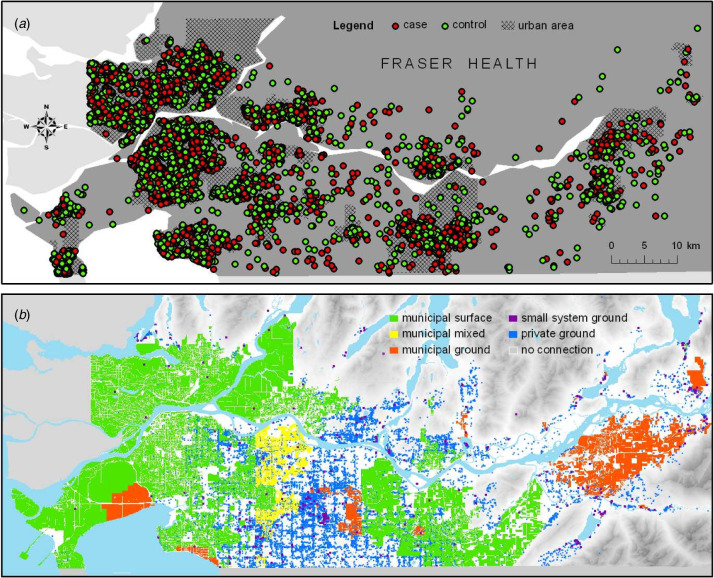
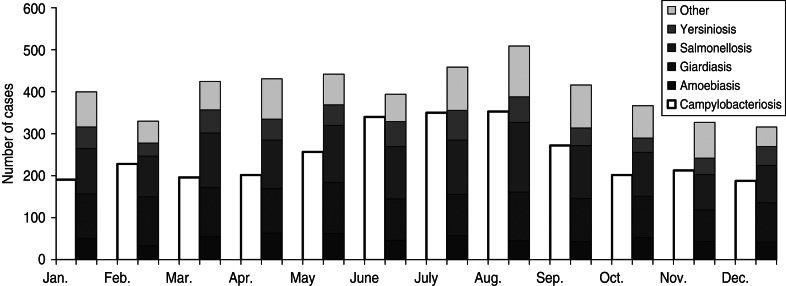
Univariate analysis showed that campylobacteriosis patients were on average older (37·2 vs. 32·6 years) than enteric disease controls, with a greater proportion aged ⩾15 years (Table 1). Further, the proportion and odds of campylobacteriosis were noticeably higher for the ⩾15 years age group compared to enteric disease controls; thus, we dichotomized the age variable into 0–14 and ⩾15 years. The sex distribution was similar, but a greater proportion of campylobacteriosis cases had a lower DI (or higher SES) (40·0% vs. 30·6% of controls). Campylobacteriosis patients were more likely to live in rural settings (8·2% vs. 6·8% of controls) and closer to an ALR (57·3% vs. 53·3% of controls) as well as to live on land parcels serviced by private wells (6·8% vs. 4·8% of controls) (Fig. 1). Campylobacteriosis cases did not seem to live closer to abattoirs than controls. Finally, campylobacteriosis cases showed a peak in June-August whereas control enteric disease cases showed a less pronounced peak in August and a decrease in autumn (Fig. 2). Individual control enteric diseases showed a similar pattern or stable numbers throughout the year.
Table 1.
Characteristics of campylobacteriosis and control enteric disease cases, Fraser Health Authority, BC, Canada, 2005–2009
| Characteristics | Campylobacteriosis cases (N = 2992) | Control enteric disease cases (N = 4816) | P value |
|---|---|---|---|
| Age (years) | |||
| Mean (range) | 37·2 (0–96) | 32·6y (0–100) | <0·001 |
| ⩾15 | 2531 (84·6%) | 3474 (72·1%) | <0·001 |
| Sex | |||
| Female | 1413 (47·2%) | 2267 (47·1%) | 0·89 |
| Male | 1579 (52·8%) | 2549 (52·9%) | |
| Deprivation index* | |||
| Low | 1053 (40·0%) | 1436 (30·6%) | <0·001 |
| Medium | 971 (33·2%) | 1365 (29·1%) | <0·001 |
| High | 905 (30·9%) | 1892 (40·3%) | <0·001 |
| Residence | |||
| Urban | 2747 (91·8%) | 4489 (93·2%) | 0·02 |
| Rural | 245 (8·2%) | 327 (6·8%) | |
| Proximity to ALR | |||
| ⩽2 km | 1715 (57·3%) | 2567 (53·3%) | <0·001 |
| >2 km | 1277 (42·7%) | 2249 (46·7%) | |
| Average (range) distance to nearest poultry abattoir (n = 8) | 8012 m (230–97 393) | 7747 m (210–57 652) | 0·05 |
| Average (range) distance to nearest red meat abattoir (n = 5) | 12 708 m (479–73 438) | 13 014 m (310–32 667) | 0·04 |
| Water index | |||
| Municipal surface | 2481 (82·9%) | 4157 (86·3%) | <0·001 |
| Municipal mixed | 120 (4·0%) | 141 (2·9%) | 0·01 |
| Municipal ground | 184 (6·2%) | 285 (5·9%) | 0·67 |
| Private surface | 3 (0·1%) | 1 (0·0%) | 0·14 |
| Private mixed | 2 (0·1%) | 2 (0·0%) | 0·64 |
| Private ground | 202 (6·8%) | 230 (4·8%) | <0·001 |
ALR, Agricultural Land Reserve.
Deprivation index data were suppressed from 186 cases because of small population size in certain areas.
Fig. 1.
Spatial distribution of campylobacteriosis cases, enteric disease controls and water system characteristics, Fraser Health Authority, BC, Canada, 2005–009. Cases have been randomly offset by up to 250 m to prevent re-identification by location. The eastern and northern regions of Fraser Health Authority are not shown in the map extent.
Fig. 2.
Campylobacteriosis cases and control enteric disease cases by month, Fraser Health Authority, BC, Canada, 2005–2009.
One-hundred eighty-six individuals were excluded from further analyses because their SES data were suppressed due to a small population size. Private surface and private mixed water categories were also excluded from further analyses since the number of cases and controls on such systems was small (four individuals in each of the two categories).
Preliminary multivariate analyses showed that proximity to abattoirs did not have a consistent effect on the odds of campylobacteriosis and that excluding these variables improved model fit. Further, distance to the nearest ALR border was excluded from the multivariate analyses due to its collinearity with the urban/rural variable, which better explained the odds of campylobacteriosis.
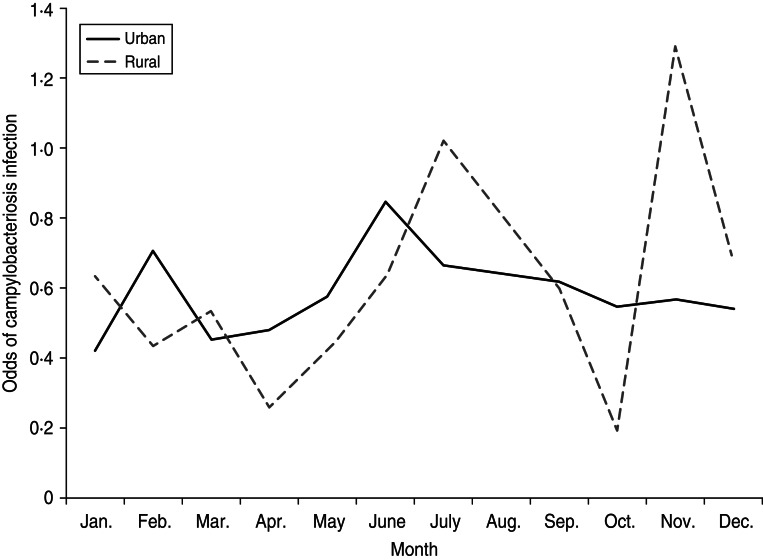
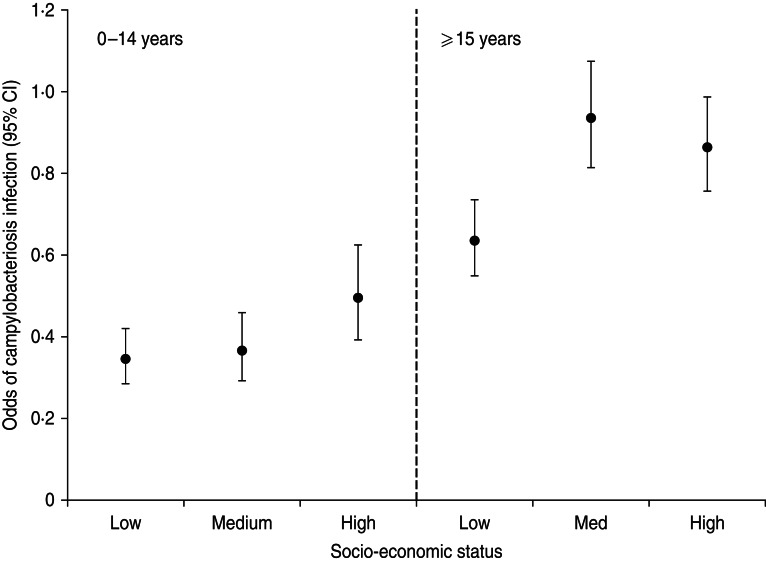
The final multivariate model showed a significant effect of water index on the odds of campylobacteriosis compared to enteric disease control (P = 0·025), as well as significant interactions for rural area by month (P = 0·004) and age by DI (P = 0·033) (Table 2). Specifically, the odds of campylobacteriosis compared to enteric disease controls was higher for individuals serviced by private wells than municipal surface water systems (OR 1·4, 95% CI 1·1–1·8). In rural settings, the odds of campylobacteriosis were lower in October (P = 0·007) and higher in November (P = 0·014) compared to urban settings (Fig. 3). After peaking in July, the number of campylobacteriosis cases in rural areas dropped considerably in October and increased again for a single month (November), whereas the number of cases of other enteric diseases stayed relatively constant between June and October in rural areas and then dropped to a stable winter level starting in November (data not shown). The odds of campylobacteriosis were higher in individuals aged ⩾15 years, especially in those with a low and medium DI (Fig. 4).
Table 2.
Multivariate regression model
| Variable | Likelihood ratio χ2 | P value |
|---|---|---|
| Age | 131·45 | <0·001 |
| Sex | 0·29 | 0·590 |
| Deprivation index | 21·29 | <0·001 |
| Month | 39·49 | <0·001 |
| Rural area | 0·18 | 0·675 |
| Water index | 9·36 | 0·025 |
| Age*Deprivation Index | 6·80 | 0·033 |
| Month*rural area | 27·37 | 0·004 |
Fig. 3.
Odds of campylobacteriosis as compared to enteric disease controls by month and by residence in rural or urban settings, Fraser Health Authority, BC, Canada, 2005–2009.
Fig. 4.
Odds of campylobacteriosis as compared to enteric disease controls by age and socioeconomic status, Fraser Health Authority, BC, Canada, 2005–2009. Low socioeconomic status refers to a high deprivation index and vice versa.
DISCUSSION
We built a model to explain the possible transmission of Campylobacter from the environment to humans in a region of BC, Canada, comparing campylobacteriosis cases to cases of other enteric diseases. We found that private well water, living in a rural environment at certain times of the year and older age in conjunction with higher SES (lower DI) increased the odds of campylobacteriosis.
The main advantage of the case-case design is its ability to limit selection and information biases: controls have similar symptoms, are identified through the same system and are subject to the same recall biases as cases [22–24]. In addition, this design is inexpensive and efficient, especially given that our hypothesis did not require interviewing cases and that we had access to enteric disease case data. A disadvantage of the case-case design is that controls differ from the general population in at least one significant way (their source of illness) and perhaps in general ways (host factors which increase their risk of illness) which limits the generalizability of results [22]. As suggested by McCarthy & Giesecke we used a variety of cases as controls to limit the impact that any single disease's exposures would have on the results [22]. We included as controls enteric diseases that are travel-associated, locally acquired or both because they all represent the population at risk of campylobacteriosis. Another disadvantage is that the case-case design underestimates the odds of disease when control diseases have similar exposures (e.g. both campylobacteriosis and giardiasis are associated with untreated drinking water) [23, 24]. However, 48·0% of controls were cases of salmonellosis, yersiniosis, shiga-toxigenic E. coli infection, Vibrio infection and listeriosis which are infections considered to be mainly foodborne [25, 26]. The fact that we nonetheless found significant associations supports the hypothesis that transmission of Campylobacter is indeed modulated by the environment, including drinking water.
The odds of Campylobacter infection were higher than enteric disease controls for individuals living on land parcels serviced by a single-user private well as compared to municipal surface water. This has been reported previously for one of the FHA communities and by others [9, 27–29]. Private wells in our study region and elsewhere are often untreated (personal communication: M. Zubel, FHA, 2013) and can be at risk of contamination from sewage or agricultural runoff [30]. A 2004 survey conducted in our study region found up to 8·4% of private wells contained faecal coliforms [31]. Contamination was localized to a few specific wells associated with shallow construction, disrepair and lack of proper seal and was deemed to be due to local contamination from agricultural runoff. The proportion of wells contaminated was higher in August (7·9%) and October (8·4%) than in February (1·4%). In addition, the Sumas-Abbotsford aquifer which covers 91 km2 (0·6%) of our study region contains high levels of nitrates, which researchers attribute to manure spreading on agricultural land [31–33].
We did not find that the higher odds of campylobacteriosis associated with private wells as opposed to enteric disease controls was mediated by proximity to ALR, residence in a rural area, or by season, which would be expected if agricultural runoff is the transmission pathway between the animal reservoir and human infection [34]. This may be because the enteric disease controls we compared to have similar risk factors, had insufficient power to detect complex interactions (e.g. the role of drinking water may be influenced simultaneously by season and residence in a rural area), the association is explained by other factors (e.g. private wells are contaminated by human sewage rather than agricultural runoff), the presence of a private well is a proxy for another, unmeasured factor, such as animal contact. Although farm animal count data are available, the data are not sufficiently detailed for a valid assessment (e.g. urban areas are included in certain animal dense consolidated census subdivisions leading to misclassification of exposure) [11].
The odds of Campylobacter infection compared to enteric disease controls differed by rural/urban residence depending on month of the year. In rural areas, the odds of campylobacteriosis were lower in October and higher in November than in urban settings. Many studies have found an increased risk of campylobacteriosis in rural areas and have attributed this to direct animal contact and the impact of animal waste on drinking water and the environment [35–39]. Many other studies have shown an increased risk of campylobacteriosis in the warmer months [40–42]. The increased rate and odds of campylobacteriosis in rural areas in November is a novel finding; this was consistent throughout all 5 years of our study and cannot be explained by a known outbreak. When data from the rest of the province were reviewed, this trend was not observed (data not shown).
The reason for this seasonal pattern is unclear. Although we did not have travel status for most cases in this study, previous research has shown that most travel-related enteric disease in BC, including campylobacteriosis and salmonellosis, occurs in the winter and early spring months [43]. We hypothesize that the increased odds in November may be associated with agricultural runoff in an animal dense rural environment. The start of the rainy season in October and the end of the period when manure spreading is allowed in late September may lead to an increased exposure to Campylobacter via the environment, including drinking water especially in poorly maintained drinking water systems [44, 45] (personal communication: O. Schmidt, BC Ministry of Agriculture, 2013). Febriani et al. also found an association between precipitation in autumn and an increased risk of acute gastrointestinal illness 3 weeks later [46]. It is not clear why the odds of campylobacteriosis were lower in rural areas in October.
Rural residence was a stronger predictor of campylobacteriosis than proximity to an ALR. Residing in a rural area may represent factors other than proximity that are important, such as direct farm or wild animal contact, potentially contaminated drinking water and food choices. In addition, ALR includes animal growing, produce growing, and forested regions and therefore may be less specific to the hypothesized route of transmission between farm animals and humans [47].
In a preliminary analysis, we included distance to the nearest poultry abattoir because we hypothesized such facilities could increase the risk of campylobacteriosis to nearby residents (through environmental contamination by animal waste) or to abattoir workers [39, 48–50]. However, distance to the nearest abattoir was not a significant factor and did not improve the model fit. In fact, most FHA abattoirs were located in urban settings and probably discharged their waste into the municipal sewage system.
We found that the odds of campylobacteriosis were higher in individuals aged ⩾15 years with medium and high SES (middle and low DI) as opposed to enteric disease controls. In BC, as elsewhere, the incidence of campylobacteriosis is highest in children aged 1–4 years and in adults aged 20–29 years [8]. The risk in children is attributed to behaviours increasing exposure as well as to a lack of immunity; the specific risk factors for young adults remain unclear [51]. Many authors have found an increased risk of campylobacteriosis in individuals with higher SES [35, 36, 52, 53]. This could be explained by greater health-seeking behaviour, more frequent restaurant meals, a greater exposure to fresh (as opposed to frozen) chicken meat, travel to endemic countries or other factors. However, a review of travel exposure on a subset of our data (cases occurring in 2008) did not support increased travel in campylobacteriosis cases with higher SES (data not shown).
We could not account for exposures that may have occurred in locations other than the place of residence, but this applied to cases and controls. We were not able to quantify specific exposures such as water ingested and contact with animals. However, other data support our explanatory variables as indicators of exposure. For example, sources show that most (79%) residents in a FHA town drink their tap water (regardless of source) [54]. Few (15%) residents in three urban and semi-rural FHA towns have farm animal contact (unpublished report: Fraser Health, Campylobacter risk factor and exposure analysis, 2012).
We did not have access to drinking water quality data to validate our water index. However, many authors have found private well water to be at higher risk [9, 27–29]. We collected the most recently available drinking water distribution data; it is possible that residences connected to municipal water systems after illness onset would have been misclassified. However, we do not believe this would affect cases and controls differently. Most (85%) individuals in our study are served by a single municipal surface water system, whereas only 3–6% of individuals used each of the other water systems. Thus, our estimates of the odds of campylobacteriosis are less precise for non-municipal surface water systems. Nevertheless, we were still able to find statistically significant differences in the odds of campylobacteriosis by water index. For the small water systems (n = 450), we relied on the x,y location coordinates of the drinking water system intake and number of users but lacked a detailed list of land parcels connected to it (as opposed to the parcels connected to the municipal water systems). This may have led to non-differential misclassification of cases and controls.
We conducted a case-case epidemiological study using individually assigned characteristics (e.g. age) as well as aggregate-level characteristics assigned to individuals (e.g. SES). The latter may be misclassified at the individual level, thereby introducing a bias in the estimate. However, this method allowed an efficient assessment of multiple environmental exposures (and possible confounders) associated with a case's place of residence. Some of the findings from this study, such as the increased odds of campylobacteriosis associated with private well water, are probably generalizable to other areas because they are widely supported in the literature. Others, such as the finding of varied risk associated with rural residence in autumn, need to be reproduced and explained further. All findings are relative to other enteric pathogens and may not represent the true population risk.
CONCLUSIONS
In conclusion, we found that the odds of campylobacteriosis were higher than other enteric diseases for those residing on land parcels serviced by private well water, independent of known confounders, but we were not able to show that this was mediated through food animal sources. Nonetheless, the odds of campylobacteriosis were lower in October and higher in November for rural residents, perhaps through exposure to agricultural runoff at the onset of the rainy season. Consideration should be given to further educate and support private well-water users against the risks of enteric diseases. Further work needs to be done to assess the role of agriculture on ground water and the ensuing risk of campylobacteriosis and other enteric diseases. Such studies and real-time surveillance of risk would greatly benefit from a central provincial repository of drinking water data so that province-wide data are accessible for study. In addition, further work is needed to understand the difference in Campylobacter transmission pathways in rural when compared to urban settings.
ACKNOWLEDGEMENTS
The authors acknowledge the financial support provided by the Public Health Agency of Canada. We thank the participating municipalities for providing access to drinking water data and Loretta Bogert O'Brien for obtaining and managing the drinking water data. Thanks also to BC laboratories for the diagnosis and reporting of cases and to the BC Enteric Policy Working Group for its support.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.World Health Organisation. The global view of campylobacteriosis: Report of an expert consultation, Utrecht, Netherlands, 9–11 July 2012. Geneva, Switzerland, 2013. [Google Scholar]
- 2.Nachamkin I, Szymanski C, Blaser M. Campylobacter, 3rd edn. Washington, DC: ASM Press, 2008. [Google Scholar]
- 3.Mullner P, et al. Source attribution of food-borne zoonoses in New Zealand: a modified Hald model. Risk Analysis 2009; 29: 970–984. [DOI] [PubMed] [Google Scholar]
- 4.Sheppard SK, et al. Campylobacter genotyping to determine the source of human infection. Clinical Infectious Diseases 2009; 48: 1072–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.European Food Safety Authority. Scientific opinion on Campylobacter in broiler meat production: Control options and performance objectives and/or targets at different stages of the food chain. EFSA Panel on Biological Hazards (BIOHAZ). EFSA Journal 2011; 9, 2105. [Google Scholar]
- 6.Mughini Gras L, et al. Risk factors for campylobacteriosis of chicken, ruminant, and environmental origin: a combined case-control and source attribution analysis. PLoS One 2012; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arsenault J, Epidemiologie spatiale de la campylobacteriose au Quebec [Dissertation]. Montreal, Canada: Université de Montréal, 2010, 1–299. [Google Scholar]
- 8.BC Centre for Disease Control. British Columbia annual summary of reportable diseases 2011. 2012. (http://www.bccdc.ca/NR/rdonlyres/B24C1DFD-3996-493F-BEC7-0C9316E57721/0/2011_CD_Annual_Report_Final.pdf). Accessed 30 August 2013.
- 9.Uhlmann S, et al. Where's the pump? Associating sporadic enteric disease with drinking water using a geographic information system, in British Columbia, Canada, 1996–2005. Journal of Water and Health 2009; 7: 692–698. [DOI] [PubMed] [Google Scholar]
- 10.Laberge K, Michel P, Galanis E. High animal density and urban environments increase the risk of campylobacteriosis in BC, Canada. Zoonoses and Public Health 2007; 54 (Suppl. 1): 24. [Google Scholar]
- 11.Kuo ME et al. Comparison of risk factors for locally-acquired versus travel-related human campylobacteriosis in BC, Canada. Proceedings of the 16th International Workshop on Campylobacter, Helicobacter and Related Organisms, 2011, p. 121.
- 12.BC Stats. Population estimates. Updated 2013 (http://www.bcstats.gov.bc.ca/StatisticsBySubject/Demography/PopulationEstimates.aspx). Accessed 30 August 2013.
- 13.Fraser Health Authority. Drinking Water Annual Report 2010/2011. 2012 Feb. (http://www.fraserhealth.ca/media/DrinkingWaterAnnualReport_2010-11.pdf). Accessed 30 August 2013.
- 14.Strickland MJ, et al. Quantifying geocode location error using GIS methods. Environmental Health 2007; 4: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.BC Ministry of Environment. WELLS: Ground water wells and aquifer database. Updated 2013 (http://www.env.gov.bc.ca/wsd/data_searches/wells/). Accessed 30 August 2013.
- 16.Canadian Food Inspection Agency. List of federally registered meat establishments and their licensed operators. Updated 1 September 2006 (http://www.bccdc.ca/NR/rdonlyres/161B504B-8E5D-43BA-B111-684DA64996C6/0/MeatPlantEstablishmentWEBVERSIONDec1812.pdf.) Accessed 1 November 2012.
- 17.BC Centre for Disease Control. Provincially licensed class A and B meat plants. Updated 26 June 2013 (http://www.bccdc.ca/NR/rdonlyres/161B504B-8E5D-43BA-B111-684DA64996C6/0/MeatPlantEstablishmentWEBVERSIONDec1812.pdf). Accessed 2 September 2013.
- 18.Turgeon P, et al. Fecal contamination of recreational freshwaters: The effect of time-independent agroenvironmental factors. Water Quality, Exposure and Health 2011; 3: 109–118. [Google Scholar]
- 19.Statistics Canada. Urban area. Updated 5 September 2007 (http://www12.statcan.gc.ca/census-recensement/2006/ref/dict/geo049-eng.cfm). Accessed 27 May 2013.
- 20.Pampalon R, et al. A deprivation index for health planning in Canada. Chronic Diseases in Canada 2009; 29: 178–191. [PubMed] [Google Scholar]
- 21.Statistics Canada. 2006 census of population. Updated 8 March 2013 (http://www12.statcan.gc.ca/census-recensement/2006/index-eng.cfm). Accessed 2 September 2013.
- 22.McCarthy N, Giesecke J. Case-case comparisons to study causation of common infectious diseases. International Journal of Health and Geography 1999; 28: 764–768. [DOI] [PubMed] [Google Scholar]
- 23.Gillespie IA, et al. A case-case comparison of Campylobacter coli and Campylobacter jejuni infection: a tool for generating hypotheses. Emerging Infectious Diseases 2002; 8: 937–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson N, et al. Case-case analysis of enteric diseases with routine surveillance data: Potential use and example results. Epidemiological Perspectives and Innovation 2008; 5: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scallan E, et al. Foodborne illness acquired in the United State: major pathogens. Emerging Infectious Diseases 2011; 17: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas M, et al. Estimates of the burden of foodborne illness in Canada for 30 specified pathogens and unspecified agents, circa 2006. Foodborne Pathogens and Disease 2013; 10: 639–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kapperud G, et al. Factors associated with increased and decreased risk of Campylobacter infection: a prospective case-control study in Norway. American Journal of Epidemiology 2003; 158: 234–242. [DOI] [PubMed] [Google Scholar]
- 28.Nygard K, et al. Association between environmental risk factors and campylobacter infections in Sweden. Epidemiology and Infection 2004. April; 132: 317–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schonberg-Norio D, et al. Swimming and Campylobacter infections. Emerging Infectious Diseases 2004. August; 10: 1474–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clark CG, et al. Characterization of waterborne outbreak-associated Campylobacter jejuni, Walkerton, Ontario. Emerging Infectious Diseases 2003. October; 9: 1232–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hii B et al. Abbotsford-Sumas Aquifer, British Columbia, Canada: 2004. Groundwater Quality Survey – Nitrate and Bacteria, September 2006.
- 32.Mitchell RJ, et al. Nitrate distributions and source identification in the Abbotsford-Sumas Aquifer, northwestern Washington State. Journal of Environmental Quality 2003; 32: 789–800. [DOI] [PubMed] [Google Scholar]
- 33.Carey B, Cummings R. Sumas-Blaine Aquifer Nitrate Contamination Summary. Olympia, WA: Washington State Department of Ecology, 2012. Report No.: 12-03-026.
- 34.Febriani Y, et al. Association between indicators of livestock farming intensity and hospitalization rate for acute gastroenteritis. Epidemiology and Infection 2009; 137: 1073–1085. [DOI] [PubMed] [Google Scholar]
- 35.Spencer SE, et al. The spatial and temporal determinants of campylobacteriosis notifications in New Zealand, 2001–2007. Epidemiology and Infection 2012; 140: 1663–1677. [DOI] [PubMed] [Google Scholar]
- 36.Bessell PR, et al. Geographic determinants of reported human Campylobacter infections in Scotland. BMC Public Health 2010; 10: 423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Green CG, Krause DO, Wylie JL. Spatial analysis of campylobacter infection in the Canadian province of Manitoba. International Journal of Health and Geography 2006; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kabore H, et al. Association between potential zoonotic enteric infections in children and environmental risk factors in Quebec, 1999–2006. Zoonoses and Public Health 2010. December; 57: e195–e205. [DOI] [PubMed] [Google Scholar]
- 39.Arsenault J, et al. Environmental characteristics associated with campylobacteriosis: accounting for the effect of age and season. Epidemiology and Infection 2012; 140: 311–322. [DOI] [PubMed] [Google Scholar]
- 40.Fleury M, et al. A time series analysis of the relationship of ambient temperature and common bacterial enteric infections in two Canadian provinces. International Journal of Biometeorology 2006; 50: 385–391. [DOI] [PubMed] [Google Scholar]
- 41.Lal A, et al. Seasonality in human zoonotic enteric diseases: a systematic review. PLoS One 2012; 7: e31883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nylen G, et al. The seasonal distribution of campylobacter infection in nine European countries and New Zealand. Epidemiology and Infection 2002; 128: 383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor M, et al. The impact of international travel on the epidemiology of enteric infections, British Columbia, 2008. Canadian Journal of Public Health 2010; 101: 332–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ministry of Agriculture. Manure spreading advisories. Updated 3 June 2013. (http://www.agf.gov.bc.ca/resmgmt/ManureAdvisory/). Accessed: 10 July 2013.
- 45.Environment Canada. National climate data and information archive. Updated 4 February 2013 (http://climate.weatheroffice.gc.ca/climateData/canada_e.html). Accessed 13 May 2013.
- 46.Febriani Y, et al. The association between farming activities, precipitation, and the risk of acute gastrointestinal illness in rural municipalities of Quebec, Canada: a cross-sectional study. BMC Public Health 2010; 10: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agricultural Land Commission. Agricultural Land Reserve. Updated 1 May 2013 (http://www.alc.gov.bc.ca/alr/alr_main.htm). Accessed 13 May 2013.
- 48.Jones K, Betaieb M, Telford DR. Correlation between environmental monitoring of thermophilic campylobacters in sewage effluent and the incidence of Campylobacter infection in the community. Journal of Applied Bacteriology 1990; 69: 235–240. [DOI] [PubMed] [Google Scholar]
- 49.Koenraad P, et al. Survey of Campylobacter spp. in sewage plants in the Netherlands. Food Microbiology 1994; 11: 65–73. [Google Scholar]
- 50.Wilson IG. Airborne Campylobacter infection in a poultry worker: case report and review of the literature. Communicable Disease and Public Health 2004; 7: 349–353. [PubMed] [Google Scholar]
- 51.Nelson W, Harris B. Campylobacteriosis rates show age-related static bimodal and seasonality trends. New Zealand Medical Journal 2011; 124: 33–39. [PubMed] [Google Scholar]
- 52.Arsenault J, et al. Environmental and demographic risk factors for campylobacteriosis: do various geographical scales tell the same story? BMC Infectious Diseases 2012; 12: 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simonsen J, Frisch M, Ethelberg S. Socioeconomic risk factors for bacterial gastrointestinal infections. Epidemiology 2008; 19: 282–290. [DOI] [PubMed] [Google Scholar]
- 54.Teschke K, et al. Water and sewage systems, socio-demographics, and duration of residence associated with endemic intestinal infectious diseases: a cohort study. BMC Public Health 2010; 10: 767. [DOI] [PMC free article] [PubMed] [Google Scholar]