SUMMARY
Epidemiological and virological studies indicate that noroviruses-contaminated groundwater was the primary source of four acute gastroenteritis outbreaks in South Korea between 2008 and 2012. Furthermore, cabbage kimchi was first identified as the vehicle of transmission between groundwater and infected patients in an outbreak in 2011. The proper treatment of groundwater sources prior to use for drinking or in food preparation is necessary to prevent further outbreaks.
Key words: Gastroenteritis, groundwater, norovirus
Noroviruses (NoVs) are recognized as the most common aetiological agents of acute gastroenteritis (AGE) outbreaks worldwide, due to their high stability in the environment and low infectious dose [1]. Groundwater is one potential vehicle for the transmission of NoVs, which results in AGE outbreaks [1–4]. Groundwater is defined as the water located beneath the soil that can be used for drinking, recreational purposes, food processing, and household use [1, 5, 6]. A recent study reported that NoVs contaminate about 20% of the groundwater in South Korea [5]. Matthews et al. found that 11% of reported NoV outbreaks were waterborne [7]. In this paper, we summarize the epidemiological and virological data from four AGE outbreaks suspected to be caused by NoV contamination of groundwater sources.
According to the epidemiological investigation guideline for waterborne and foodborne diseases published by the Korea Center for Disease Control & Prevention (KCDC), all AGE outbreaks should be promptly and thoroughly investigated by public officials to identify causal agents and prevent the spread of disease in South Korea. Between January 2008 and June 2012, following AGE outbreaks, faecal specimens were collected from Gyeonggi province, a highly populated area that houses 24% of the South Korean population. The samples were obtained from the KNRRC waterborne virus bank [8]. Faecal specimens were diluted to 10% with phosphate-buffered saline and clarified by centrifugation at 800 g for 15 min, and the supernatants were collected for measurement. Groundwater samples were collected immediately after epidemiological findings indicated that groundwater might have been the source of the outbreak. Groundwater sampling and concentration procedures were conducted using standard protocols [5, 9]. Total coliforms and Escherichia coli in groundwater were analysed using the Colilert kit (Idexx Laboratories, USA) according to the manufacturer's instructions [5]. Free chlorine was measured using a portable microprocessor HI96701C (Hanna Instruments, USA) according to the manufacturer's instructions. Viral RNA was extracted from the faecal supernatant and groundwater samples using the QIAamp viral RNA mini kit (Qiagen, Germany) according to the manufacturer's instructions. To detect NoVs, semi-nested reverse transcriptase–polymerase chain reaction (RT–PCR) was performed using specific primer sets (NV-GIF1M/NV-GIR1M/NV-GIF2 for NoV GI; NV-GIIF1M/NV-GIIR1M/NV-GIIF3M for NoV GII), targeting the capsid gene (region C) as described previously [4, 5]. Previously reported size-distinguishable products were used as positive control [10]. Final PCR products were purified and bi-directionally sequenced with nested PCR primers. MEGA software (version 4.0) was used for phylogenetic analysis.
From January 2008 to June 2012, 193 AGE outbreaks were reported in Gyeonggi province, South Korea. Viral aetiology revealed that NoVs were detected in 57 (29·5%) outbreaks, while group A rotaviruses were isolated from three (1·6%) outbreaks. Other viruses, including enteric adenovirus, astrovirus, and sapovirus, were not found in AGE outbreaks. Both epidemiological and virological evidence supported the view that groundwater was implicated in four NoV outbreaks. These data are summarized in Table 1.
Table 1.
Epidemiological features of four groundwater-borne norovirus-associated outbreaks in Gyeonggi province, South Korea between 2008 and 2012
| Outbreak no. | 2008-A* | 2011-B† | 2012-C | 2012-D |
|---|---|---|---|---|
| Epidemiological study | Retrospective cohort | Case-control | Retrospective cohort | Retrospective cohort |
| Outbreak setting | Water park | Five schools | Restaurant | Restaurant |
| Duration of exposure | 14 Jan. 2008 | 16–19 May 2011 | 23–25 May 2012 | 30 May 2012 to 1 June 2012 |
| Date of onset | 16 Jan. 2008 | 18–20 May 2011 | 25 May 2012 | 1 June 2012 |
| Median incubation time | 36 h | 24 h | 26 h | 41 h |
| Median age (range) | 12 yr (11–30 yr) | 16 yr (8–19 yr) | 19 yr (18–45 yr) | 16 yr (15–41 yr) |
| Outbreak-associated illnesses (no. ill/no. exposed) | 31·0% (67/216) | 5·9% (451/7605) | 75·9% (22/29) | 74·5% (76/102) |
| Suspected exposure route | Unknown | Cabbage kimchi | Unknown | Unknown |
| Relative risk or odds ratio | n.d. | 1·65–4·55 | n.d. | n.d. |
| Clinical specimens | ||||
| Total (n). | 3 | 149 | 22 | 39 |
| Norovirus positive (n) | 3 | 51 | 7 | 15 |
| Genotype (n) | GI.4 (3) | GI.3 (51) | GII.17 (7) | GII.2 (15) |
| Groundwater | ||||
| Date of collection | 21 Jan. 2008 | 20 May 2011 | 29 May 2012 | 4 June 2012 |
| Collection points (n) | Water park reservoir | Food plant groundwater (2) | Camp groundwater | Restaurant tap |
| Filtered volume (litres) | 670 | 436–640 | 505 | 531 |
| Norovirus genotype (n) | GI.4 | GI.3 (2) | GII.17 | GII.2 |
| Homology‡ | >98·9% | >99·4% | >96·6% | 100·0% |
| Disinfection system | Sand filtration, Chlorination | Ultraviolet light | None | Chlorination |
| Total coliforms | Positive | Positive | Positive | n.d. |
| E. coli. | Positive | Positive | Positive | n.d. |
| Distance to septic tank | n.d. | 10 m | 20 m | n.d. |
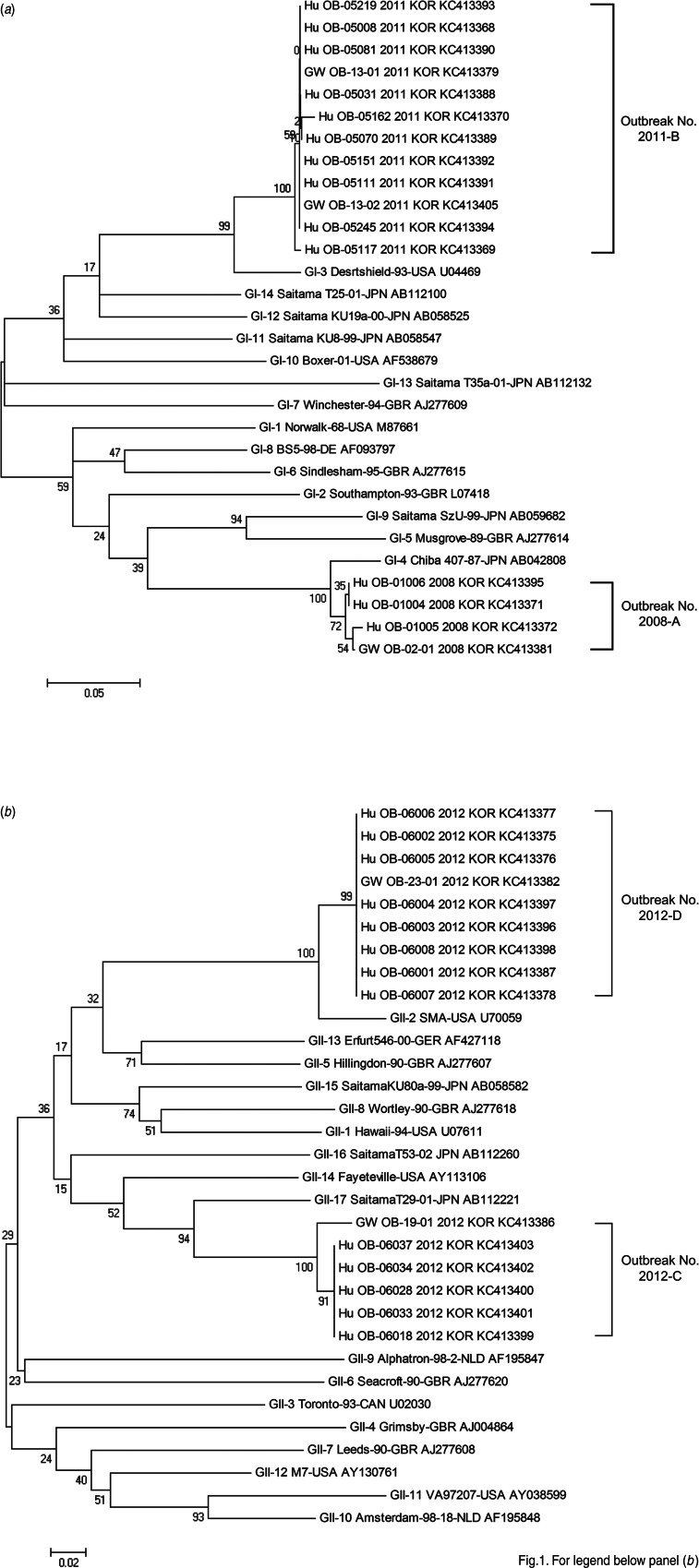
On 14 January 2008, 216 students and teachers visited a water park. On 16 January 2008, 67 (31·0%) individuals exhibited symptoms of AGE; this incident is referred to as outbreak 2008-A (Table 1) [11]. Three faecal specimens from patients were collected and NoVs were detected in all of the specimens. An epidemiological inspection on 18 January 2008 revealed that the outbreak could not be linked to any food items, but E. coli was detected in the groundwater supplied to the water park as recreational water, as well as drinking and food-preparation water supplied to an affiliated restaurant. On 21 January 2008, groundwater was collected from the reservoir tank in the water park. NoV GI.4 was detected in the groundwater and clinical specimens, with a sequence identity of 98·9–99·4% between the two sources (Fig. 1) [11].
Fig. 1.
A phylogenetic tree constructed using 178 nucleotide sequences from the capsid gene (region C) of norovirus GI (a) and GII (b) isolated from clinical specimens and groundwater samples associated with the four outbreaks. The ClustalW method and neighbour-joining method were used for DNA sequence alignments and dendrogram construction, respectively. GW, Groundwater; Hu, human patient; OB, outbreak.
Between 18 and 20 May 2011, five consecutive AGE outbreaks in five independent schools were reported, which are referred to as 2011-B (Table 1) [12]. Of the 7605 students, a total of 451 (5·9%) were affected by AGE symptoms. NoV GI.3 strains were identified in 51/149 faecal specimens. Epidemiological investigations examining the food supply revealed that the common factor was the cabbage ‘kimchi’ supplied through the food catering services to the five schools (Table 1). The cabbage kimchi was processed using groundwater in the food plant and distributed to the five schools over the same time period. A case-control study was performed using the asymptomatic students at the five schools as control subjects [12]. The controls were matched by age to the cases, at a ratio of at least 2:1 [12]. Higher adjusted odds ratios (ORs) were observed for the groups that had consumed cabbage kimchi at the three schools [OR 2·56, 95% confidence interval (CI) 1·07 − 6·09, P = 0·034; OR 1·65, 95% CI 1·04 − 2·63, P = 0·033; OR 4·55, 95% CI 1·55 − 17·22, P = 0·005) [12]. However, the ORs at the remaining two schools were not statistically significant (OR 1·86, 95% CI 0·58 − 8·66, P = 0·32; OR 0·57, 95% CI 0·27 − 1·25, P = 0·16). On 20 May 2011, two groundwater samples were collected from the food plant. NoV GI.3 strains were isolated from both groundwater samples and showed 99·4–100·0% identity to the clinical specimens (Fig. 1). Furthermore, NoV GI.3 was detected in cabbage kimchi, which was collected from the same food plant on 20 May 2011. The sequence similarity between the isolates from the kimchi and those from the groundwater samples was 100·0%, while sequence homology between the kimchi isolates and the clinical isolates was 99·6–100·0% (unpublished data, Korea Food and Drug Administration).
In the 2012-C outbreak, 29 high-school students and teachers visited a rural-experience camp between 23 and May 25. Twenty-two (75·9%) visitors exhibited AGE symptoms beginning on 25 May 2012. NoV GII.17 strains were identified in seven faecal specimens of the 22 samples collected. Epidemiological investigations were unable to statically associate any food items with the outbreak. However, a restaurant at which visitors consumed seven meals from 23 to 25 May 2012 used groundwater. The groundwater had not been disinfected for drinking purposes. The groundwater was collected on 29 May 2012, and the NoV GII.17 strain was detected, which shared >96·6% homology with the clinical sample strains (Fig. 1).
The 2012-D outbreak occurred on 1 June 2012 (Table 1). Epidemiological investigations revealed that 76 (74·5%) of 102 students and teachers visiting a river resort were affected by AGE symptoms. NoVs were identified in 15 samples of the 39 faecal specimens collected from patients. Although a retrospective cohort study showed that no food items were suspected, the affected individuals had six meals and consumed drinking water in a resort-affiliated restaurant in which chlorinated groundwater was used as drinking and food-preparation water. However, no free chlorine was detected in the groundwater on 4 June 2012, indicating that the automated chlorination system was out of order. NoV GII.2 was detected in the groundwater and clinical samples, and sequence identity between the viral strains detected in the two sources was 100·0% (Fig. 1).
NoVs are generally detected year-round in groundwater despite clinical winter seasonality [5]. Three outbreaks (2011-B, 2012-C, 2012-D) occurred in May, i.e. at the end of the warm spring in South Korea. This indicates that NoVs in groundwater may cause AGE outbreaks regardless of season [3, 4].
Faecal coliforms were detected in groundwater in the 2008-A, 2011-B, and 2012-C outbreaks, and the groundwater implicated in the 2011-B and 2012-C outbreaks was located relatively close to septic tanks (Table 1). Furthermore, groundwater from three outbreaks (2008-A, 2011-B, 2012-D) was supplied without the proper operation of disinfection systems. This suggests that inadequate management of contaminated groundwater can lead to exposure of NoVs, resulting in outbreaks [2, 3].
Epidemiological and phylogenetic evidence supports the view that groundwater was the primary source for the four outbreaks. However, epidemiological data from three of the outbreaks (2008-A, 2012-C, 2012-D), were insufficient to conclusively determine the route of transmission from groundwater to the infected patients, although food items eaten raw, direct consumption of non-disinfected groundwater, or person-to-person contact were suspected. Cabbage kimchi processed by NoV-contaminated groundwater was first identified as the route of exposure in the 2011-B outbreak although cabbage kimchi presumably contaminated by a food-handler was previously suspected as the source of a NoV outbreak in South Korea [12, 13]. Cabbage kimchi is prepared in the following manner: raw cabbage is irrigated with water, mixed with various seasonings, and typically stored at a low temperature until consumption. Therefore, groundwater-borne NoVs can survive in cabbage kimchi [6].
In conclusion, contaminated groundwater was very likely to have been the primary source for the four AGE outbreaks discussed in this study. To prevent further outbreaks, proper treatment of groundwater sources before use for drinking or in food preparation is necessary. In the event of a ‘food poisoning’ outbreak, the possibility that contaminated water used during food preparation may have been the source of the outbreak should always be considered.
The nucleotide sequences of clinical and environmental NoV isolates were submitted to the GenBank database with the following accession numbers: KC413368–KC413372, KC413375–KC413379, KC413381–KC413382, KC413386–KC413403 and KC413405.
ACKNOWLEDGEMENTS
This work was supported by the Mid-career Researcher Program (2012R1A2A2A01045078) through NRF grants funded by the MEST.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Hall AJ, et al. Updated norovirus outbreak management and disease prevention guidelines. Morbidity and Mortality Weekly Report. Recommemdations and Reports 2011; 60: 1–18. [PubMed] [Google Scholar]
- 2.Parshionikar SU, et al. Waterborne outbreak of gastroenteritis associated with a norovirus. Applied and Environmental Microbiology 2003; 69: 5263–5268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maunula L, Miettinen IT, von Bonsdorff CH. Norovirus outbreaks from drinking water. Emerging Infectectious Diseases 2005; 11: 1716–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim SH, et al. Outbreaks of gastroenteritis that occurred during school excursions in Korea were associated with several waterborne strains of norovirus. Journal of Clinical Microbiology 2005; 43: 4836–4839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee SG, et al. Nationwide groundwater surveillance of noroviruses in South Korea, 2008. Applied and Environmental Microbiology 2011; 77: 1466–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheong S, et al. Enteric viruses in raw vegetables and groundwater used for irrigation in South Korea. Applied and Environmental Microbiology 2009; 75: 7745–7751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matthews JE, et al. The epidemiology of published norovirus outbreaks: a review of risk factors associated with attack rate and genogroup. Epidemiology and Infection 2012; 140: 1161–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korean National Research Resource Centre. Waterborne virus bank (http://www.wava.or.kr/). Accessed 1 March 2009).
- 9.Fout GS, et al. ICR microbial laboratory manual. US Environmental Protection Agency, Washington DC, 1996. Publication no. EPA/600/R-95/178. [Google Scholar]
- 10.Lee SG, et al. Standardized positive controls for detection of norovirus by reverse transcription PCR. Virology Journal 2011; 8: 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koh SJ, et al. An outbreak of gastroenteritis caused by norovirus-contaminated groundwater at a waterpark in Korea. Journal of Korean Medical Science 2011; 26: 28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee MJ. et al. Epidemiological study of ground-waterborne norovirus GI.3-associated gastroenteritis outbreaks in Gyeonggi province of South Korea in May 2011. Journal of Bacteriology and Virology 2012; 42: 232–241. [Google Scholar]
- 13.Yu JH, et al. Epidemiology of foodborne Norovirus outbreak in Incheon, Korea. Journal of Korean Medical Science 2010; 25: 1128–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]