SUMMARY
In May 2011, an outbreak of Shiga toxin-producing Escherichia coli (STEC) O157 was reported from Yamagata Prefecture, Japan. Investigations, including a case-control study, revealed that the outbreak was linked to two varieties of rice cakes produced by a local manufacturer between 2 and 7 May. Active and passive surveillance identified 136 suspected cases, 142 confirmed cases, 26 asymptomatic cases, and 25 secondary cases. While no environmental samples taken from the manufacturing premises tested positive for STEC, other than a stool sample taken from one employee, on-site and epidemiological investigations indicated that STEC was introduced during the manufacturing process of rice cakes rather than through contamination of raw materials. This was the first reported outbreak of STEC associated with cakes and confectionery in Japan, which indicates that contamination and outbreaks of STEC can occur in any food unless proper precautions are taken.
Key words: Japan, rice cakes, Shiga toxin-producing Escherichia coli
INTRODUCTION
Since the first report from the USA in 1983 [1], a number of outbreaks associated with Shiga toxin-producing Escherichia coli (STEC) O157 have been reported from many parts of the world [2–11]. From 1996 to 2010, a total of 351 foodborne outbreaks associated with STEC O157, resulting in 13364 cases and 22 deaths, have been officially reported in Japan [12]. Of particular note is the 1996 Sakai City outbreak involving more than 7000 cases, which remains the largest outbreak linked to STEC O157 ever reported [13]. Beef and beef-related foods have been the main vehicles for STEC infection in Japan and abroad [14]. Other foods, such as sprouts and green vegetables, as well as contaminated water, have also been implicated as vehicles for STEC infection [15, 16]. Direct animal and human contact can also generate STEC outbreaks [14, 17].
On 7 May 2011, the Murayama Public Health Centre in Yamagata Prefecture, Japan, was informed of clusters of cases of a suspected foodborne illness. The initial investigation revealed that there were four distinct clusters (pupils and staff at a nursery, festival participants, child sports team members, and college student club members); all had consumed rice cakes produced by a single local manufacturer (manufacturer A). We describe the joint investigation conducted by the Murayama Public Health Centre and the National Institute of Infectious Diseases (NIID) to identify the source and route of infection, as well as to assess the overall impact of the outbreak.
METHODS
Initial investigation and hypothesis generation
The investigation team responded on the respective reported days by conducting face-to-face and telephone interviews with individuals in the four clusters to generate hypotheses regarding exposure vehicles. The interviews consisted of three components: (i) whether the interviewee attended the respective suspected gathering event, (ii) whether the interviewee developed abdominal pain, diarrhoea, or bloody diarrhoea, within 7 days after the respective event, and (iii) what food items the interviewee consumed at the respective event. The interview did not include food items consumed outside of the respective suspected event and symptoms recorded were at the time of the interview date. The parents of small children involved were interviewed on their children's behalf.
Microbiological investigation
Stool samples taken from cluster and sporadic cases were tested by the Murayama Public Health Centre or healthcare facilities and their contracted private laboratories. At the Murayama Public Health Centre, samples were cultured on chromogenic agar (CHROMagar) and MacConkey sorbitol agar with cefixime and tellurite (CTSMAC) for detection and isolation of the strain. Serotyping was performed using commercially available antisera (Denka Seiken Co. Ltd, Japan) for serotype O and polymerase chain reaction (PCR) for serotype H. The presence of genes encoding Stx1 (stx1) and Stx2 (stx2) was tested on isolates of a cultured strain using PCR with the MK primer [18]. The presence of other virulence factor genes encoding Intimin (eae), AggR (aggR), InvE (invE), LT (elt), ST (est), and EAST1 (astA), as well as enteropathogenic Escherichia coli (EPEC) adherence factor (EAF) plasmid, were tested using multiplex PCR on selected samples. Further, the public health laboratory at Yamagata Prefecture and NIID performed pulsed-field gel electrophoresis (PFGE) on selected isolates from different clusters and sporadic cases to compare genetic relatedness of the strains. PFGE protocols and data analysis of E. coli O157:H7 isolates were performed using the restriction endonucleases XbaI following the standardized PulseNet methods from the United States Centre for Disease Control AND Prevention (CDC, USA) [19].
Traceback and environmental investigations
Manufacturer A was a small family-owned shop with three staff engaged in rice cake production. One staff member was primarily engaged in rice dough production, another in syrup pasting and packaging, and the third in wrapping. An environmental investigation was undertaken to identify the possible source and route of contamination. Environmental samples were taken on 8 and 12 May from various sources on the premises, including production machines, utensils, and ingredients. Since no final products had been stored by the manufacturer, a left-over rice cake produced on 3 May was recovered from a garbage bin in a patient's house on 8 May. Stool samples were taken from the three staff members and thorough face-to-face interviews were conducted with each staff member.
Case-control study
In order to statistically examine the generated hypothesis and exclude other possible sources, a case-control study was conducted. Taking into consideration the commonality in background characteristics, such as age and the ability to adequately respond to survey questions, we selected the members of a college student club out of the four clusters as the target population for the study. Cases were defined as ‘those who are members of the college student club and presented with abdominal pain, diarrhoea, or bloody diarrhoea, between 7 and 15 May’. Controls were defined as ‘those who are members of the college student club and did not present with the above-mentioned symptoms during the same period’. Controls were selected from those who participated in a club training activity on 26 May. Face-to-face interviews were conducted by the Murayama Public Health Centre and NIID staff using a standard survey questionnaire, primarily on 26 May. Odds ratios (ORs) with 95% confidence intervals (CIs) and P values were calculated based on Fisher's exact test using Epi Info (CDC, USA) to identify risk factors (gathering events and food items). A P value <0·05 was considered statistically significant.
Impact assessment of the outbreak
The Food Sanitation Law in Japan requires physicians to immediately report suspected foodborne illnesses to the nearest public health centre. Further, the Infectious Disease Control Law in Japan requires physicians to immediately report to the nearest public health centre when diagnosing STEC cases. In addition to cases related to the four clusters, the Murayama Public Health Centre was notified of sporadic cases through such systems and conducted the appropriate investigations. These data were collated and analysed to assess the overall impact of the outbreak using the case definitions described below:
Suspected
Those who presented with abdominal pain, diarrhoea, or bloody diarrhoea, within 7 days after consumption of rice cakes produced by manufacturer A since mid-April 2011.
Confirmed
Those who presented with abdominal pain, diarrhoea, or bloody diarrhoea, within 7 days after consumption of rice cakes produced by manufacturer A since mid-April 2011, and whose stool samples contained STEC O157 by laboratory testing.
Asymptomatic
Those who consumed rice cakes produced by manufacturer A but did not present with abdominal pain, diarrhoea, or bloody diarrhoea, since mid-April 2011, and whose stool samples contained STEC O157 by laboratory testing.
Secondary
Those who did not consume rice cakes produced by manufacturer A since mid-April 2011, or who consumed rice cakes but did not present with the above-mentioned symptoms within 7 days after consumption, and had close contact with confirmed cases, and whose stool samples contained STEC O157 by laboratory testing.
RESULTS
Initial investigation and hypothesis generation
The results of the initial investigations into the four clusters are summarized in Table 1. Two different types of rice cakes produced by manufacturer A between 2 and 7 May were implicated as common vehicles: kashiwamochi (round rice cake with red bean paste inside and wrapped in an oak leaf), and dango [skewered five small round rice cakes with one of four different kinds of syrup on top (soy sauce, sesame, green bean paste, or red bean paste)].
Table 1.
Summary of initial investigation findings into the four clusters
| Pupils and staff at a nursery | Festival participants | Child sports team members | College student club members | |
|---|---|---|---|---|
| Suspected gathering event | Lunch and snack time | Seasonal town festival | Basketball game | Lunch for recruitment |
| Date of the event | 2 May | 3 May | 3 May | 7 May |
| Food items served during the event | Rice cakes (kashiwamochi) and ready-made lunch box | Rice cakes [dango (soy sauce and green bean paste)], hamburger, and ready-made lunch box | Rice cakes [dango (soy sauce, sesame, green bean paste, and red bean paste)] and rusk | Rice cakes [dango (green bean paste)], hors d'oeuvres, and other foods listed in Table 2 |
| Date of initial reporting | 8 May | 7 May | 7 May | 12 May |
| Date of interview | 9–11 May | 8 May | 8–13 May | 12, 26 May |
| Number of people interviewed | 156 | 138 | 25 | 57 |
| Number of people who attended the event | 113 | 138 | 22 | 41 |
| Number of people who complained of abdominal pain, diarrhoea, or bloody diarrhoea within 7 days* | 28 | 89 | 21 | 12 |
| Number of people who complained of the above symptoms and had consumed rice cakes | 28 | 89 | 21 | 10 |
| Number of people who complained of the above symptoms, had consumed rice cakes, and tested positive for STEC O157 infection | 20 | 42 | 9 | 4 |
Kashiwamochi is a round rice cake with red bean paste inside and wrapped in an oak leaf. Dango is skewered, five small round rice cakes with one of four different types of syrup on top (soy sauce, sesame, green bean paste, or red bean paste).
Symptoms were at the time of the interview and the possibility of excluding patients who presented symptoms after the interview cannot be discounted.
Based upon the data collected on 8 May, the Murayama Public Health Centre hypothesized that the rice cakes produced by manufacturer A was the common source of infection, and manufacturer A was requested to halt its operation on 8 May. On 12 May, a fourth cluster of cases was reported from college club members who apparently had consumed rice cakes produced by manufacturer A on 7 May. The details of this cluster are described in the case-control study section below.
Microbiological investigation
Laboratory testing revealed that the outbreak was caused by STEC O157:H7. Of the 127 samples that tested positive for STEC O157 and whose Shiga-toxin genes were subtyped, 121 possessed both stx1 and stx2, and six possessed only stx1. PFGE on 35 selected samples from four different clusters and 14 sporadic cases showed that all strains were identical, except for one band which was thought to encode stx2 (i.e. non-existent for stx1 only strain). In addition to stx genes, multiplex PCR of selected samples revealed that the strains also possessed the virulence factor gene eae.
Traceback and environmental investigation
A stool sample taken from one of the staff members of manufacturer A, who was primarily engaged in syrup pasting and packaging, tested positive for STEC O157 on 13 May and the strain matched those taken from cluster and sporadic cases, as determined by PFGE. The staff member was not ill during the course of the outbreak. Stool samples taken from the remaining two staff as well as environmental samples taken from the premises of manufacturer A tested negative for STEC O157. A left-over rice cake (dango) recovered from a garbage bin in a patient's house was rotten and did not yield STEC O157 by culture on chromogenic agar media.
The environmental investigation of manufacturer A's premises revealed that, in addition to kashiwamochi and dango, at least two more rice cake varieties were produced between 2 and 7 May. These were daifuku (sticky rice cake with red bean paste inside) and yubeshi (steamed rice cake); they were not implicated in outbreaks of STEC O157. Manufacturer A was increasing its production level from late April to early May due to the holiday season in Japan.
Case-control study
The case-control study of college club members consisted of 57 subjects (12 cases, 45 controls). The age range of the cases was 18–20 years (median 19 years), while that of the controls was 18–21 years (median 19 years) (P = 0·63, Mann–Whitney U test). Of the 12 cases, four were confirmed as STEC O157 infection by laboratory testing, while no samples were taken from the remaining eight. All cases developed diarrhoea, ten developed abdominal pain, and three developed bloody diarrhoea. Twelve events were identified where two or more members of the college club had meals together between 1 and 12 May. Only one event, a recruitment lunch for new members on 7 May, had statistically significant participation by cases (P < 0·01). Of the 57 subjects, a total of 41 (12 cases, 29 controls) participated in the recruitment event. A total of 27 food and drink items were served during the event and only one food item, a rice cake (dango with green bean paste) produced by manufacturer A, was consumed by cases with statistical significance (OR 43·3, 95% CI 4·9–547·5, P < 0·01) (Table 2). Of the 12 cases in the case-control study, two had not consumed rice cakes produced by manufacturer A. While samples were not tested in both cases, neither developed symptoms that were strongly suggestive of STEC infection.
Table 2.
Case-control study food items provided at a recruitment lunch event on 7 May 2011
| Food items | Cases (n = 12) | Controls (n = 29)† | OR (95% CI) | P value | ||
|---|---|---|---|---|---|---|
| Exposed | Unexposed | Exposed | Unexposed | |||
| Fried shrimp | 3 | 9 | 8 | 21 | 0·88 (0·14–5·0) | 1 |
| Tartar sauce | 1 | 11 | 3 | 26 | 0·79 (0·03–10·3) | 1 |
| Fried chicken | 8 | 4 | 13 | 14 | 2·2 (0·43–11·3) | 0·47 |
| Fried wing | 1 | 11 | 7 | 22 | 0·29 (0·01–2·9) | 0·4 |
| Chicken nugget | 5 | 7 | 10 | 17 | 1·2 (0·24–6·0) | 1 |
| Fried ham | 1 | 11 | 3 | 26 | 0·79 (0·03–10·4) | 1 |
| Fried squid | 7 | 5 | 7 | 21 | 4·2 (0·82–22·9) | 0·07 |
| Fried fish | 0 | 11 | 3 | 25 | 0 (0–6·2) | 0·55 |
| Croquette | 1 | 11 | 6 | 21 | 0·32 (0·01–3·4) | 0·4 |
| Baked egg | 4 | 7 | 4 | 25 | 0·5 (0·09–2·5) | 0·55 |
| Sausage | 3 | 8 | 8 | 19 | 0·89 (0·14–5·3) | 1 |
| Sweetened potato | 3 | 9 | 8 | 20 | 0·83 (0·13–4·8) | 1 |
| Potato and cheese | 5 | 2 | 7 | 3 | 1·1 (0·08–14·5) | 1 |
| Waffles | 2 | 10 | 13 | 16 | 0·25 (0·03–1·6) | 0·15 |
| Sandwiches | 8 | 3 | 22 | 7 | 0·85 (0·14–5·4) | 1 |
| Rice cake (dango, green bean paste) | 10 | 2 | 3 | 26 | 43·3 (4·9–547·5) | <0·01 |
| Rice cake (dango, red bean paste)* | 3 | 9 | 8 | 21 | 0·88 (0·14–5·0) | 1 |
| Rice cake (dango, sesame)* | 2 | 10 | 14 | 15 | 0·21 (0·03–1·4) | 0·08 |
| Rice cake (dango, soy sauce)* | 5 | 7 | 10 | 19 | 1·4 (0·28–6·6) | 0·73 |
| Rice cake (dango, coloured)* | 6 | 4 | 14 | 14 | 1·5 (0·28–8·3) | 0·72 |
| Potato chips | 7 | 5 | 19 | 10 | 0·74 (0·15–3·6) | 0·73 |
| Cheese and fish | 6 | 5 | 9 | 20 | 2·7 (0·52–14·1) | 0·27 |
| Rice cracker and peanuts | 3 | 8 | 10 | 19 | 0·71 (0·12–4·0) | 1 |
| Other snacks | 5 | 7 | 15 | 14 | 0·93 (0·22–4·0) | 0·83 |
| Tea | 8 | 4 | 24 | 4 | 0·33 (0·05–2·1) | 0·21 |
| Juice | 8 | 4 | 19 | 10 | 1·05 (0·21–5·5) | 1 |
| Other drinks | 8 | 4 | 10 | 18 | 3·6 (0·71–19·3) | 0·15 |
OR, Odds ratio; CI, confidence interval.
Dango is skewered, five small round rice cakes with one of four different types of syrup on top (soy sauce, sesame, green bean paste, or red bean paste).
These rice cakes were produced by manufacturers other than manufacturer A.
Controls are limited to those who attended the recruitment event on 7 May.
Impact assessment of the outbreak
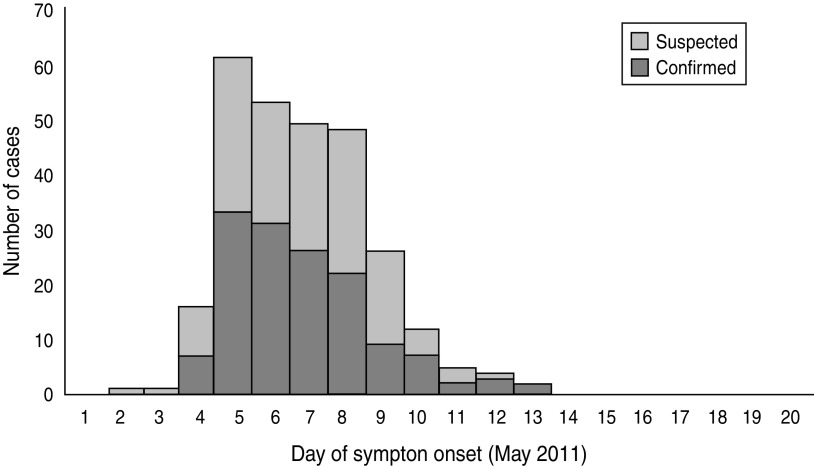
Active and passive surveillance identified 136 suspected cases, 142 confirmed cases, and 26 asymptomatic cases. An analysis of the 278 total suspected and confirmed cases, which consisted of 149 cluster and 129 sporadic cases, revealed that the age range was 1–94 years (median 32 years), the female ratio was 55·4%, 87 (31%) cases were hospitalized, five (1·8%) cases developed haemolytic uraemic syndrome, and one (0·36%) case died. The incubation period ranged from 0–7 days (median 3 days). The outbreak began on 2 May, peaked on 5 May, and the last case developed symptoms on 13 May (Fig. 1).
Fig. 1.
Epidemic curve of the outbreak; 278 suspected and confirmed cases.
An investigation into 84 families where at least one confirmed case had been reported identified 25 secondary cases from 18 families. A further analysis of 56 families where all of the family members submitted stool samples revealed that there were 118 primary cases, 17 secondary cases, and 127 negative cases (secondary attack rate 11·8%). It also revealed that all of the primary cases whose links to secondary cases were identified were young children (13 transmissions: eight from a child to a parent, one from a child to a grandparent, and four from a child to a child).
DISCUSSION
To our knowledge, this is the first reported STEC O157 outbreak associated with cakes and confectionery in Japan. Outside Japan, we found only one report through a PubMed search describing an outbreak in the USA associated with ready-to-bake, commercial, pre-packaged cookie dough where case patients consumed the cookie dough uncooked [20].
The results of the initial investigation strongly suggested rice cakes as a vehicle of the outbreak and this was later statistically supported by a case-control study targeting one cluster. Through extensive interviews with 57 college students, the case-control study identified only one food item, a rice cake (dango with green bean paste), at a single event, as a vehicle with statistical significance. The PFGE results also provided strong evidence connecting the four distinct clusters to the manufacturer, particularly because the strain was unique and had not been previously reported in Japan.
The symptoms of 278 suspected and confirmed cases were typical of those commonly seen in STEC O157 outbreaks [14]. The PFGE results indicate that the outbreak originated from the same strain, some of which lost the stx2-converting phage over the course of the outbreak [21].
The secondary attack rate in a household (11·8%) was within the range of previous reports [22]. The finding that all of the secondary transmission whose epidemiological links were confirmed originated from young children reflects the increased transmission risk in such groups, as reported previously [23, 24].
While no environmental samples taken from the manufacturing site were positive for STEC O157, the fact that only two varieties of rice cakes out of four produced between 2 and 7 May were related to the outbreak provided us with evidence to identify the possible source and route of contamination. Dango was pasted with one of four different types of syrup on top after the rice dough was rolled and immediately before packaging. The fact that dango with all types of syrup generated cases while one of the syrups, red bean paste, was also used for rice cakes which did not generate cases (daifuku), indicates that it was rice dough, rather than syrup, that caused the outbreak. After investigating the manufacturing process of rice cakes, we confirmed that all products underwent a high-temperature steaming process for more than half an hour when the rice powder was made into rice dough. This indicates that contamination of the raw materials, if any, is unlikely to be the cause of the outbreak, and that contamination probably occurred after this process [25, 26]. We found one difference in the process for making rice dough between the products that generated cases (kashiwamochi and dango) and those did not (daifuku and yubeshi) (data not shown). The cooling process used for kashiwamochi and dango rice dough involved immersing the dough into a bucket of tap water. The dough was then pounded with a pounding machine again. Theoretically, once the water was contaminated with STEC O157, all dough exposed to the water could become evenly and extensively contaminated through this process. While the tap water was chlorinated, it was considered ineffective in this situation, where heated rice dough was repeatedly immersed in the bucket, since chlorine rapidly dissipates with time, high temperatures, and contact with organic substances [27]. Interviews with the manufacturer indicated that the bucket was not routinely and thoroughly cleaned with soap and hot water. Without such measures, it is plausible that contamination of the bucket and water continued to contaminate rice dough for six consecutive days. We believe that the reason the environmental samples taken from the bucket and water were negative for STEC is probablyy because the premises was cleaned by the manufacturer prior to sample collection on 12 May.
Of the suspected and confirmed cases who consumed rice cakes manufactured on 2 May, the probable initial day of contamination, all had consumed kashiwamochi, but not dango, although 174 sets of dango had been produced and sold on the same day. This indicates that the initial contamination probably occurred between the processes of manufacturing kashiwamochi and manufacturing dango on 2 May. While a stool sample from one staff member engaged in syrup pasting and packaging was positive for STEC O157, and the strain matched those taken from cases confirmed by PFGE, we could not conclude whether the staff member was an origin of contamination because the staff also consumed rice cakes between 2 and 7 May. Further investigation did not provide evidence as to how STEC O157 was introduced into the rice cakes.
Passive surveillance also detected six confirmed cases of STEC O157 infection in the same prefecture as the outbreak cases in May 2011 that had no epidemiological links to each other. PFGE revealed that five of six cases had identical strains to those found in the outbreak. Considering the uniqueness of this strain, there was probably an original source of infection in the same area that eventually contaminated the rice cake production process and infected these five cases through other routes. Although we were unable to identify such an original source despite thorough interviews with these five individuals, this investigation indicates the importance of maintaining surveillance beyond outbreak cases to identify an original source of infection.
CONCLUSIONS
We described the investigation of the first reported STEC outbreak associated with cakes and confectionery in Japan. The initial investigation, as well as the case-control study, clearly identified two varieties of rice cakes as the cause of the outbreak. While no environmental samples were positive for STEC, apart from the stool sample obtained from one staff member of the manufacturer, an investigation into the manufacturing process, as well as epidemiological information, provided us with reasonable evidence to infer a route of contamination. This outbreak is indicative of the fact that contamination with STEC, which results in outbreaks, can occur in any food, and can continuously contaminate food over days unless proper precautions and routine, thorough cleaning practices are in place.
ACKNOWLEDGMENTS
The authors express sincere appreciation to the local government of Yamagata Prefecture, Tokyo Metropolitan, Saitama Prefecture, Fukushima Prefecture, Saitama City, Iwaki City, and Sendai City, as well as the hospitals and clinics in these jurisdictions, for their significant contributions to the epidemiological, laboratory, clinical, and environmental investigations during this outbreak. The authors are also grateful to Yamagata University, particularly Professor Hitoshi Togashi and the members of the college student club, for their cooperation in conducting a case-control study, and colleagues in the Murayama Public Health Centre and NIID for their support throughout the investigation.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Riley LW, et al. Hemorrhagic colitis associated with a rare Escherichia coli serotype. New England Journal of Medicine 1983; 308: 681–685. [DOI] [PubMed] [Google Scholar]
- 2.Sartz L, et al. An outbreak of Escherichia coli O157:H7 infection in southern Sweden associated with consumption of fermented sausage; aspects of sausage production that increase the risk of contamination. Epidemiology and Infection 2008; 136: 370–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Effler E, et al. Factors contributing to the emergence of Escherichia coli O157 in Africa. Emerging Infectious Diseases 2001; 7: 812–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woodward DL, et al. Verotoxigenic Escherichia coli (VTEC): a major public health threat in Canada. Canadian Journal of Infectious Diseases 2002; 13: 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, et al. Epidemiological study on an outbreak caused by E. coli O157:H7 in Jiangsu province [in Chinese]. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 2004; 25: 938–940. [PubMed] [Google Scholar]
- 6.Smith-Palmer A, et al. Cluster of E. coli O157 infections in Scottish tourists returning from southwest Turkey, July–August 2005. Eurosurveillance 2005; 10: E050818.2. [DOI] [PubMed] [Google Scholar]
- 7.Jensen C, et al. First general outbreak of Verocytotoxin-producing Escherichia coli O157 in Denmark. Eurosurveillance 2006; 11: 55–58. [PubMed] [Google Scholar]
- 8.Doorduyn Y, et al. Shiga toxin-producing Escherichia coli (STEC) O157 outbreak, The Netherlands, September–October 2005. Eurosurveillance 2006; 11: 182–185. [PubMed] [Google Scholar]
- 9.Mannix M, et al. Large outbreak of E. coli O157 in 2005, Ireland. Eurosurveillance 2007; 12: 54–56. [Google Scholar]
- 10.Sigmundsdottir G, et al. STEC O157 outbreak in Iceland, September–October 2007. Eurosurveillance 2007; 12: E071101.2. [DOI] [PubMed] [Google Scholar]
- 11.Ihekweazu C, et al. Large outbreak of verocytotoxin-producing Escherichia coli O157 infection in visitors to a petting farm in South East England, 2009. Epidemiology and Infection 2011; 18: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Government of Japan Ministry of Health, Labour, and Welfare. Information on food poisoning (http://www.mhlw.go.jp/topics/syokuchu/). Accessed 31 May 2012.
- 13.Michino H, et al. Massive outbreak of Escherichia coli O157:H7 infection in schoolchildren in Sakai City, Japan, associated with consumption of white radish sprouts. American Journal of Epidemiology 1999; 150: 787–796. [DOI] [PubMed] [Google Scholar]
- 14.Pennington H. Escherichia coli O157. Lancet 2010; 376: 1428–1435. [DOI] [PubMed] [Google Scholar]
- 15.Verma A, et al. An outbreak of E. coli O157 associated with a swimming pool: an unusual vehicle of transmission. Epidemiology and Infection 2007; 135: 989–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittaker PJ, et al. A national outbreak of verotoxin-producing Escherichia coli O157 associated with consumption of lemon-and-coriander chicken wraps from a supermarket chain. Epidemiology and Infection 2009; 137: 375–382. [DOI] [PubMed] [Google Scholar]
- 17.Payne CJI, et al. Vero cytotoxin-producing Escherichia coli O157 gastroenteritis in farm visitors, North Wales. Emerging Infectious Diseases 2003; 9: 526–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karch H, Meyer T. Single primer pair for amplifying segments of distinct Shiga-like-toxin genes by polymerase chain reaction. Journal of Clinical Microbiology 1989; 27: 2751–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribot EM, et al. Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathogens and Disease 2006; 3: 59–67. [DOI] [PubMed] [Google Scholar]
- 20.Neil KP, et al. A novel vehicle for transmission of Escherichia coli O157:H7 to humans: multistate outbreak of E. coli O157:H7 infections associated with consumption of ready-to-bake commercial prepackaged cookie dough – United States, 2009. Clinical Infectious Diseases 2011; 54: 511–518. [DOI] [PubMed] [Google Scholar]
- 21.Murase T, Yamai S, Watanabe H. Changes in pulsed-field gel electrophoresis patterns in clinical isolates of enterohemorrhagic Escherichia coli O157:H7 associated with loss of Shiga toxin genes. Current Microbiology 1999; 38: 48–50. [DOI] [PubMed] [Google Scholar]
- 22.Snedeker KG, et al. Primary and secondary cases in Escherichia coli O157 outbreaks: a statistical analysis. BMC Infectious Diseases 2009; 9: 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seto EYW, Soller JA, Colford JM. Strategies to reduce person-to-person transmission during widespread Escherichia coli O157:H7 outbreak. Emerging Infectious Diseases 2007; 13: 860–866. [DOI] [PubMed] [Google Scholar]
- 24.Werber D, et al. Preventing household transmission of Shiga toxin-producing Escherichia coli O157 infection: promptly separating siblings might be the key. Clinical Infectious Diseases 2008; 46: 1189–1196. [DOI] [PubMed] [Google Scholar]
- 25.Lee SY, et al. Survival and growth of foodborne pathogens during cooking and storage of oriental-style rice cakes. Journal of Food Protection 2006; 69: 3037–3042. [DOI] [PubMed] [Google Scholar]
- 26.Okahisa N, et al. Evaluation and control of the risk of foodborne pathogens and spoilage bacteria present in Awa-Uirou, a sticky rice cake containing sweet red bean paste. Foodborne Pathogens and Disease 2008; 5: 351–359. [DOI] [PubMed] [Google Scholar]
- 27.Friedman MS, et al. Escherichia coli O157:H7 outbreak associated with an improperly chlorinated swimming pool. Clinical Infectious Diseases 1999; 29: 298–303. [DOI] [PubMed] [Google Scholar]