SUMMARY
Multiple norovirus outbreaks following catered events in Auckland, New Zealand, in September 2010 were linked to the same catering company and investigated. Retrospective cohort studies were undertaken with attendees of two events: 38 (24·1%) of 158 surveyed attendees developed norovirus-compatible illness. Attendees were at increased risk of illness if they had consumed food that had received manual preparation following cooking or that had been prepared within 45 h following end of symptoms in a food handler with prior gastroenteritis. All food handlers were tested for norovirus. A recombinant norovirus GII.e/GII.4 was detected in specimens from event attendees and the convalescent food handler. All catering company staff were tested; no asymptomatic norovirus carriers were detected. This investigation improved the characterization of norovirus risk from post-symptomatic food handlers by narrowing the potential source of transmission to one individual. Food handlers with gastroenteritis should be excluded from the workplace for 45 h following resolution of symptoms.
Key words: Food safety, foodborne infections, hand hygiene, norovirus, outbreaks
INTRODUCTION
Norovirus is a common cause of gastroenteritis [1, 2] and although the illness is generally self-limiting and of short duration, it is associated with significant morbidity [3]. Norovirus is highly transmissible, having a low infectious dose and a multiplicity of transmission routes, including direct contact with an infected person [4], contact with fomites [5–7], consumption of contaminated food or water [8, 9], and exposure to airborne virus [10].
Similar to other foodborne pathogens, norovirus outbreaks have occurred following contamination of foods during primary production (e.g. shellfish [11] and fresh produce [12]). However, foodborne norovirus outbreaks are more likely than foodborne bacterial outbreaks to be associated with foods requiring handling but no subsequent heating, and more likely to have an infected food handler implicated [13]. Features of norovirus infection that increase the risk of transmission from infected food handlers include high concentrations of virus in stools, low infectious dose, and persistent shedding of viral particles in faeces following symptom cessation [14].
Food contamination by persons shedding virus in the immediate post-symptomatic period is potentially controllable by excluding food handlers with gastroenteritis from the workplace. Although current guidelines recommend a 48 h post-symptomatic exclusion period for food handlers with gastroenteritis [14–16], current experimental methods are inadequate to precisely determine the duration of infectivity following illness [17]. Recent empirical research suggests that norovirus RNA may be detectable in faeces for a median of 28 days after viral inoculation [18], although detection of norovirus by this method cannot be considered analogous to infectivity [19, 20]. Limited viral load estimations of norovirus infection in healthy adults suggest that viral loads decline rapidly within 2 weeks following onset of illness [19].
In the absence of experimental data verifying the temporal gradient of risk for transmitting norovirus following illness recovery, observational studies based on outbreaks add useful information to validate the risk assessment and support development of evidence-based preventive measures. However, interpretation of these studies can be problematic as transmission from the implicated index case may have occurred within the workplace before the detection of the outbreak [21], resulting in symptomatic or asymptomatic [22] infections among multiple food handlers, all of whom could have contaminated food. Unless full ascertainment of hazards in the food preparation environment has occurred, the contribution of a single food handler and the temporal relationship between symptoms and food contamination may be difficult to determine.
This report describes an outbreak of norovirus gastroenteritis in which complete ascertainment of symptoms and microbiological status of food handlers was obtained. On 22 and 23 September 2010 Auckland Regional Public Health Service received reports of gastrointestinal illness occurring in participants at two separate events (events 1 and 2) that had received food from the same caterer. Case-finding was extended to an additional four events (events 3–6) that had also been provided with food by the caterer during 20–22 September. This paper describes the investigations and actions following outbreak notification.
METHODS
This was a public health investigation to control a disease outbreak, and therefore did not require approval by an institutional review board.
Epidemiological investigation
The catering company provided a list of all catered events, menus and number catered for between 20 and 22 September.
Events 1 and 2
Retrospective cohort studies of events 1 and 2 were performed to identify risk factors associated with illness. Event 1 was a continuing professional development function held on 20 September, and provided one cohort. Event 2 was a 3-day trade fair held from 20 to 22 September that provided five cohorts: one cohort from those attending on 20 September; two cohorts from those attending on 21 September (attendees 10:00–11:45 hours, and attendees 15:00–17:10 hours); and two cohorts from those attending on 22 September (attendees 11:00–14:45 hours, and attendees 16:30–19:15 hours). These cohorts corresponded to separate batches of food received from the catering company. A questionnaire was developed that included questions about symptoms, onset and duration of illness (including illness prior to the event), items consumed, and contact with others with gastroenteritis prior to onset of symptoms. Event organizers provided names and contact details for event attendees. Questionnaires were either administered by phone interviews, or were emailed for self-completion. Non-responders were followed-up by phone.
A case was defined as a person who consumed food provided by the catering company and subsequently developed diarrhoea or vomiting and at least one other symptom (i.e. nausea, fever, chills, abdominal pain, backache and muscle aches). Incubation periods were defined as the time intervals between the consumption of implicated food and onset of diarrhoea or vomiting; those who had attended multiple times were excluded from these calculations. Demographic associations with illness were assessed by calculating the relative risk (RR) of becoming a case by age (based on two age groups: <40 years and >39 years) and sex. Risk of illness associated with date and time of exposure was assessed by calculating RR for persons exposed on 20 September or before 11:45 hours on 21 September compared to other attendees. Persons who had attended multiple functions were excluded from these calculations. A composite risk factor was created by coding event attendees to a binomial variable based on whether or not they had consumed food that had received substantial manual preparation (i.e. by having ingredients manually inserted within or applied to other ingredients) without further cooking. Food items that were cooked and then simply transferred to service trays were defined as not having been manually prepared after cooking. The RR for illness in the entire cohort (pooling event 1 and event 2 attendees) was calculated for this binomial variable.
Food risk factors were assessed within each of the six separate cohorts on the basis that each cohort received a single, separate batched delivery of food from the catering company. The RR was calculated for each food item served within each cohort, using data from all individuals who attended functions at which the particular food item was served, including those that attended multiple times. χ2 tests and P values were used to determine the statistical significance of RR. Multivariable log-binomial regression models were constructed for each cohort separately and for both events combined to assess independent association with illness where more than one variable in the cohort had significant univariate association with illness. Variables for different exposure days and for the composite variable for consumption of foods manually prepared without further cooking were tested only in the model comprising attendees from both events. For all models, risk factors with a P value <0·1 on univariate analysis were included initially; exposures with P > 0·1 were subsequently excluded from the models in a stepwise backwards procedure. Univariate analyses were undertaken using Epi Info 7·0·9·34 (CDC, USA); multivariate analysis was undertaken using R [23].
Events 3–6
Case-finding was undertaken among attendees of events 3–6. In events 3 and 4, catering was provided over 2 days for multiple meals to a single group for each event. In events 5 and 6, catering was provided to a single group for one meal only. Event organizers were asked whether any illness had occurred among attendees. If illness had occurred, attendees were asked to confirm by email whether they had experienced illness including diarrhoea and/or vomiting after the start of the event. Food and beverage exposure histories were not collected from individual attendees and no measures of association between risk factors and illness were calculated. Attack rates for each event were calculated using the same case definition as for the cohort studies.
Microbiological investigation
Faecal specimens were requested from event attendees with gastroenteritis and from all persons involved in food preparation at the catering company during the period 20–22 September. Environmental specimens were collected from interior surfaces of the food preparation premises using moist sterile cotton swabs. All specimens were submitted to the Institute of Environmental Science and Research Ltd (ESR). Faecal specimens were tested for bacterial pathogens associated with acute gastroenteritis. Faecal and environmental specimens were analysed for norovirus genogroup I and II (GI and GII) by real-time reverse transcription (RT)–qPCR using previously published primers and probes [24]. For genotyping of selected samples, noroviruses were first amplified using a primary RT–PCR that encompasses the polymerase region B (ORF-1) and capsid region C (ORF-2) to give a 523-bp product [25, 26]. Where necessary, to increase sensitivity, separate semi-nested PCRs using norovirus GII region B [25] and GII region C [26] primers were performed to give products of 213 bp and 344 bp, respectively. An RT–PCR specific for norovirus GII.4 P2 domain (794 bp product) was also performed [27]. All PCR products were purified using the ExoSAP-IT (Affymetrix, USA) followed by DNA sequencing in both directions using the Big Dye Terminator cycling methodology (Applied Biosystems Corp., USA) on an automated ABI 3130XL sequencer (Applied Biosystems). Consensus sequences in region B (172 bp), region C (283 bp) and the P2 domain (459 bp) were assembled using BioNumerics, version 5.10 (Applied Maths, Belgium) and compared to norovirus reference sequences using unweighted pair-group method with arithmetic mean (UPGMA) clustering. The Noronet web-based norovirus typing tool (accessed 12 January 2012) was also used to assist identification [28]. Phylogenetic analyses for each region were performed using MEGA version 5, with trees constructed using the neighbour-joining method, and evolutionary distances computed using the maximum composite likelihood method [29]. Bootstrap test (1000 replicates) was used for inferring confidence values (%) for each analysis. The norovirus sequence (region B–C) identified in this study was submitted to GenBank (JQ618020).
Environmental investigation
Investigation officers visited the catering company premises on 23 September and conducted interviews with the staff. Employees involved in food preparation during the period 20–22 September were identified and interviewed for history of gastrointestinal illness with onset between 13 and 23 September. Information was obtained on incidents of vomiting or diarrhoea at the premises for the same period. Food safety assessment was undertaken; principal ingredients were identified and food preparation processes determined for food items served. Cleaners employed at the venues for events 1 and 2 were interviewed.
RESULTS
Epidemiological investigation
In total, 354 persons attended events provided with food by the catering company between 20–22 September (Table 1). Nine persons who attended event 2 at multiple times are categorized in Table 1 based on their attendance time ranges.
Table 1.
Attack rates in groups of people who attended six events with food and beverage items prepared by a catering company, Auckland, 20–22 September 2010
| Event | Date(s) group exposed (timeperiod of exposure, if applicable) | Time of finalpreparation offood providedto group | Number withinformationon illness (totalnumber in group) | Cases | Number withconfirmednorovirusinfection | |
|---|---|---|---|---|---|---|
| n | Attack rate% (95% CI) | |||||
| 1 | 20 Sept. | 17:00 hours | 46 (53) | 13 | 28·3 (16·0–43·5) | 3 |
| 2 | 20 Sept. | 14:30 hours | 27 (27) | 8 | 29·6 (13·8–50·2) | 2 |
| 21 Sept. (10:00–11:45 hours) | 09:00 hours | 26 (26) | 9 | 34·6 (17·2–55·7) | 2 | |
| 21 Sept. (15:00–17:10 hours) | 14:00 hours | 11 (11) | 0 | 0 (0–28·5) | — | |
| 22 Sept. (11:00–14:45 hours) | 09:00 hours | 20 (20) | 2 | 10·0 (1·2–31·7) | 0 | |
| 22 Sept. (16:30–19:15 hours) | 14:00 hours | 19 (19) | 0 | 0 (0–17·6) | — | |
| 20 Sept. to 17:10 hours 21 Sept. | Multiple times | 2 (2) | 2 | 100 | 0 | |
| 20 Sept. to 22 Sept. | Multiple times | 1 (1) | 1 | 100 | 0 | |
| 21 Sept. (10:00 hours) to 22 Sept. | Multiple times | 5 (5) | 3 | 60·0 (14·7–94·7) | 0 | |
| 21 Sept. (15:00 hours) to 22 Sept. | Multiple times | 1 (1) | 0 | 0 (0–97·5) | — | |
| 20–22 Sept. | Multiple times | 1 (1) | 1 | 100 | 0 | |
| 3* | 20–21 Sept. | Multiple times | 9 (9) | 7 | 77·8 (40·0–97·2) | 1 |
| 4* | 21–22 Sept. | Multiple times | 25 (25) | 7 | 28·0 (12·1–49·4) | 1 |
| 5† | 22 Sept. | 17:00 hours | 0 (135) | — | 1 | |
| 6* | 22 Sept. | 16:00 hours | 0 (20) | — | 0 | |
| Total | 192 (354) | 52 | 27·1 (20·9–34·0) | 10 | ||
Aggregated information on illness in attendees of these events was collected by respective event organizers and provided to the investigation team.
Organizers of this event declined to permit investigation of attendees. However, one attendee reported illness, and was subsequently investigated.
Events 1 and 2
Event 1 was attended by 53 persons, 46 (86·8%) of whom completed questionnaires. Of these, 13 (28·3%) developed illness meeting the case definition. Event 2 was attended by 112 persons over the 20–22 September period. All attendees were interviewed; 25 (22·3%) developed illness meeting the case definition. Combining populations from both events, the overall attack rate was 24·1% (38/158); 28·8% (21/73) for persons who attended a function only on 20 September, 24·3% (9/37) for persons attending only on 21 September, and 5·1% (2/39) for persons attending only on 22 September. The median age of ill persons was 39 years (range 23–63 years); 82·1% were female. Neither age nor sex was significantly associated with illness meeting the case definition on univariate analysis. The median duration of symptoms was 31 h (range 1–110 h), and the median incubation period, excluding nine persons who had eaten food from functions on more than 1 day, was 36 h (range 8–85 h). Nausea was experienced by all 38 cases, diarrhoea by 84%, vomiting by 82%, fever by 73% and abdominal pain by 71%. Nine persons sought medical attention, none were hospitalized. The epidemic curve for events 1 and 2 is shown in Figure 1.
Fig. 1.
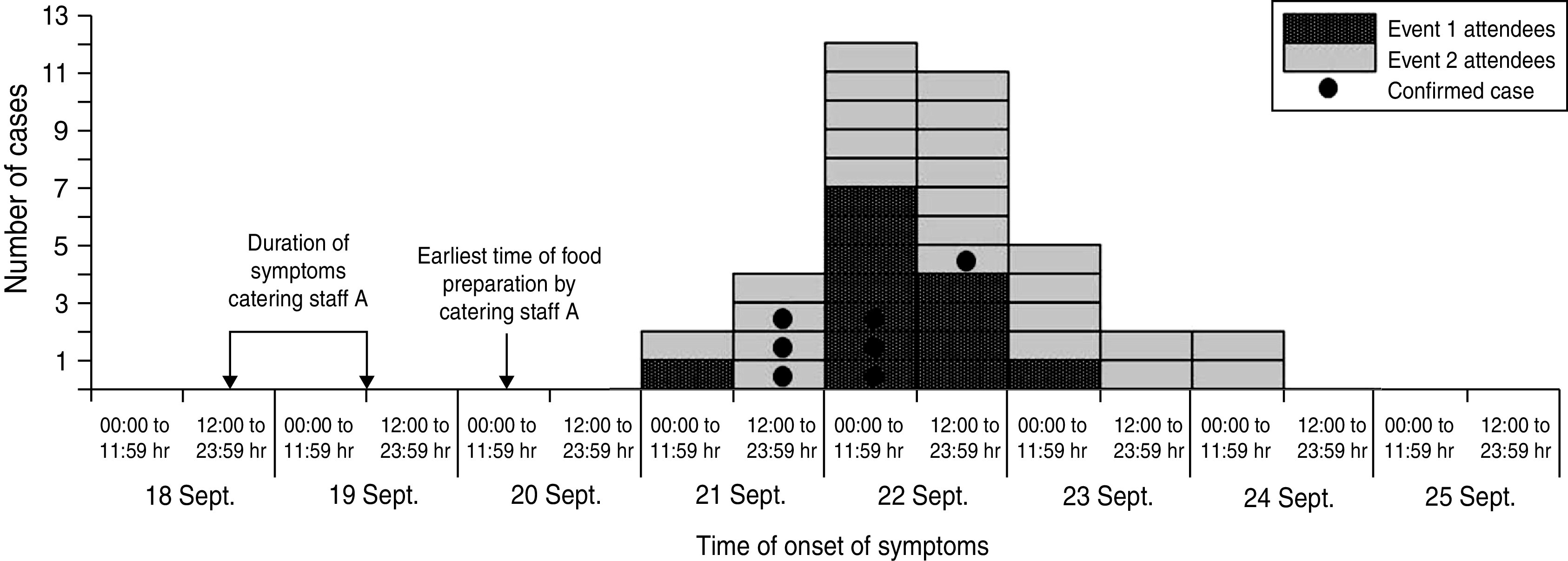
Cases of acute gastroenteritis, by date of symptom onset, in persons who attended either a medical continuing professional development event (event 1) or a trade fair event (event 2) and consumed food and/or beverage items provided by a single catering company between 20 and 22 September 2010. A case was defined as a person with an illness consisting of either vomiting or diarrhoea and one other gastroenteritis symptom.
Risk of illness meeting the case definition was significantly greater for those who attended events during the period 20 September to 11:45 hours on 21 September than for other attendees, and for those who consumed food that had received manual preparation after cooking (Table 2). The proportion of attendees who consumed food that had been manually prepared after cooking did not vary significantly in the period (odds ratio 1·2, 95% confidence interval 0·5–2·6, P = 0·8). No cases had a history of contact with others with gastroenteritis in the 2-week period prior to onset of their own illness.
Table 2.
Univariate and multivariable analyses of risk factors for illness in people attending either a medical continuing professional development event (event 1) or a trade fair event (event 2) supplied by a single catering company; Auckland, 20–22 September 2010*
| Exposure | Exposed | Not exposed | Univariate analysis | Multivariable analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Total | AR% | Cases | Total | AR% | RR | 95% CI | P | aRR | 95% CI | P | |
| Event 1 (20 September) | ||||||||||||
| Poached chicken sandwiches | 11 | 24 | 45·8 | 1 | 21 | 4·8 | 9·6 | 1·4–68·4 | 0·006 | |||
| Event 2 (20 September) | ||||||||||||
| Italian sushi (prosciutto-wrapped rice, parmesan, tomato) | 9 | 15 | 60·0 | 2 | 15 | 13·3 | 4·5 | 1·2–17·4 | 0·02 | 3·4 | 1·2–9·5 | 0·02 |
| Spiced chicken on cucumber noodle salad | 8 | 11 | 72·7 | 3 | 19 | 15·8 | 4·6 | 1·5–13·8 | 0·006 | 18·5 | 0·99–13·7 | 0·05 |
| Venison with tomato relish | 7 | 10 | 70·0 | 4 | 19 | 21·1 | 3·3 | 1·3–8·7 | 0·03 | |||
| Event 2 (21 September, 10:00–11:45 hours) | ||||||||||||
| Club sandwiches | 12 | 18 | 66·7 | 3 | 16 | 18·8 | 3·6 | 1·2–10·4 | 0·01 | |||
| Events 1 and 2 combined (20–22 September) | ||||||||||||
| Attended before 11:45 hours, 21 September† | 30 | 99 | 30·3 | 2 | 48 | 4·0 | 7·6 | 1·9–30·4 | 0·0005 | 7·2 | 2·4–43·2 | 0·005 |
| Consumed food with manual preparation without further cooking | 36 | 111 | 32·4 | 2 | 47 | 4·3 | 7·6 | 1·9–30·4 | 0·0003 | 6·6 | 2·2–39·2 | 0·007 |
AR, Attack rate; RR, crude relative risk; CI, confidence interval; aRR, relative risk adjusted for other risk factors shown for that cohort.
Exposures listed only if P < 0·1.
Includes persons attending functions of either event at any time on either 20 September or before 11:45 hours on 21 September; reference group were persons attending functions between 15:00 hours on 21 September and 19:15 hours on 22 September. Excludes eight persons who attended both before and after 11:45 hours on 21 September.
Different combinations of food items were available at and during each event. When attendees were grouped into separate cohorts defined by event and exposure day and time period, illness in event 1 attendees was statistically associated with consumption of poached chicken sandwiches (Table 2); for event 2 attendees, illness was associated with consumption of prosciutto-wrapped sushi, chicken on cucumber noodle salad and venison for those attending on 20 September, and with consumption of club sandwiches for those attending between 10:00 and 11:45 hours on 21 September. No items were statistically associated with illness in those who attended event 2 either after 15:00 hours on 21 September or on 22 September. Of the three food items with univariate associations with illness in event 2 attendees on 20 September, consumption of prosciutto-wrapped sushi and chicken on cucumber noodle salad were both independently associated with illness following multivariable analysis. No single main ingredient was common to each food item associated with illness, but complete ascertainment of minor ingredients (herbs, spices) did not occur for all food items.
Events 3–6
Attendees of events 3 and 4 were affected by illness, with attack rates of 77·8% (7/9) and 28·0% (7/25), respectively. The organizers of event 5 declined to circulate information on the investigation to event attendees or to provide details of event attendees; however, one attendee of this event submitted a specimen for analysis. No reports of illness were received from event 6, which received catering solely on 22 September.
Environmental investigation
All food items for the events were provided by the catering company. Most events received food served as single-serve canapés; two events (events 3 and 4) received filled bread rolls. Production of all food items provided by the catering company was performed on the company premises, distant from the event venues; items to be served hot were reheated onsite at the respective events. Food items were prepared on the day they were served and delivered in batches to event venues: final food preparation times for each batch are shown in Table 1.
The premises inspection identified that food handlers used tea towels tucked into their aprons for drying and wiping their hands during food preparation; no written policy was in place defining the exclusion period for staff following gastroenteritis symptoms. The catering company reported that 11 employees worked at the food preparation premises during 20–22 September. Of these, five were involved in food handling and preparation, one worked as a kitchen hand but did not prepare food, and one further person assisted in transporting food to events. All employees were interviewed during the investigation. Three employees reported experiencing gastrointestinal illness at some stage during the period 13–23 September. One of the chefs (catering staff A) reported becoming ill with vomiting and diarrhoea that commenced at 18:00 hours on 18 September and lasted until 12:00 hours on 19 September; this employee prepared food for all events in the 20–22 September period, making sandwiches and undertaking preparatory work on garnishes and salads. The interval between the cessation of catering staff A's symptoms and completion of food preparation work was about 45 h for food provided to event 2 guests attending between 10:00 and 11:45 hours on 21 September. A waiter (catering staff B) became ill with diarrhoea and vomiting at 03:00 hours on 22 September, and did not return to work on 22 September or 23 September; this employee was not involved in food preparation but had delivered food to events on 20–21 September. A kitchen hand (catering staff C) vomited once in the men's bathroom in the catering company premises at around 10:00 hours on 22 September and was immediately stood down from work; this employee was not involved in food preparation but cleaned cooking utensils, cleaned toilet facilities and delivered food to events. Neither catering staff A or B attended event venues; catering staff C briefly visited venues while delivering food but did not use venue kitchen or bathroom facilities. No other employees reported gastrointestinal symptoms in the period 13–24 September. Cleaners at the venues for events 1 and 2 had not been required to clean up vomitus at the venues in preceding weeks. Although event 2 extended over a 3-day period, no cases from event 2 attended the event venue after onset of symptoms. Four had attended the venue in the 14-h period prior to onset of illness, but in each of these cases attendance during this period overlapped only with functions held late in the afternoon of 22 September, and no others who attended at this time subsequently became cases.
Microbiological investigation
Faecal specimens were obtained and analysed from all 11 catering company employees who worked at the company's food preparation premises between 20 and 22 September, and from 13 event attendees who developed illness. The median specimen collection date from employees with illness was 1 day earlier than that of other employees. All specimens were negative for bacterial pathogens. Norovirus results from specimens collected from catering company employees and event attendees are shown in Table 3. Specimens from the three employees who had reported symptoms were positive for norovirus GII; norovirus was not detected in specimens from the remaining eight employees who had remained well. Specimens from ten event attendees were positive for norovirus GII: three who attended event 1 (20 September), four who attended event 2 (two on 20 September and two between 10:00 and 11:45 hours on 21 September), one attendee each from event 3 (20–21 September), event 4 (21–22 September) and event 5 (22 September). Eight environmental specimens were collected from frequently handled surfaces and objects in the catering company premises: of these, the specimen collected from the door handle of the men's toilet was positive for norovirus GII.
Table 3.
Norovirus results of tested faecal specimens collected in relation to a gastroenteritis outbreak; Auckland, 20–22 September 2010
| Ref. | Description | Symptomonset date | Specimencollectiondate | Norovirusresult |
|---|---|---|---|---|
| Catering company employees | ||||
| A | Chef | 18 Sept. | 24 Sept. | GII.e/GII.4 |
| B | Delivery assistant | 22 Sept. | 23 Sept. | GII.e/GII.4 |
| C | Kitchen hand | 22 Sept. | 26 Sept. | GII.e/GII.4 |
| D | Chef | No illness | 25 Sept. | Not detected |
| E | Chef | No illness | 26 Sept. | Not detected |
| F | Chef | No illness | 26 Sept. | Not detected |
| G | Chef | No illness | 25 Sept. | Not detected |
| H | Administrator | No illness | 24 Sept. | Not detected |
| I | Administrator | No illness | 25 Sept. | Not detected |
| J | Administrator | No illness | 24 Sept. | Not detected |
| K | Kitchen hand | No illness | 26 Sept. | Not detected |
| Event attendees | ||||
| 42 | Event 1, exposure 20 Sept. only | 22 Sept. | 23 Sept. | GII |
| 43 | Event 1, exposure 20 Sept. only | 22 Sept. | 25 Sept. | GII.e/GII.4 |
| 41 | Event 1, exposure 20 Sept. only | 22 Sept. | 27 Sept. | GII |
| 23 | Event 2, exposure 20 Sept. only | 21 Sept. | 23 Sept. | GII |
| 24 | Event 2, exposure 20 Sept. only | 22 Sept. | 25 Sept. | Not detected |
| 31 | Event 2, exposure 20 Sept. only | 21 Sept. | 24 Sept. | GII |
| 29 | Event 2, exposure 21 Sept., 10:00–11:45 hours | 21 Sept. | 25 Sept. | GII.e/GII.4 |
| 25 | Event 2, exposure 21 Sept., 10:00–11:45 hours | 22 Sept. | 24 Sept. | GII.e/GII.4 |
| 21 | Event 2, exposure 22 Sept. only | 25 Sept. | 28 Sept. | Not detected |
| 26 | Event 3, exposure 20–21 Sept. | Unknown | 27 Sept. | GII.e/GII.4 |
| 27 | Event 3, exposure 20–21 Sept. | Unknown | 5 Oct. | Not detected |
| 28 | Event 4, exposure 21–22 Sept. | 23 Sept. | 25 Sept. | GII.4 |
| 30 | Event 5, exposure 22 Sept. only | 24 Sept. | 26 Sept. | GII |
A norovirus classified as a recombinant GII.e/GII.4 was identified using the Noronet nomenclature system [28], although acknowledging that GII.e could be a more divergent member of GII.4 (P. White and J.-S. Eden, written communication). The norovirus was Osaka 2007-like (AB434770) in region B (Fig. 2) and distinct from other reported GII.4 variants in the capsid region (region C and P2 domain, Fig. 3). Indistinguishable sequences in region B (172 bp, Fig. 2) and region C (283 bp, data not shown) were identified in three positive specimens from catering company employees (catering staff A, B, C), four specimens from event attendees (attendees 25, 26, 29, 43) and an environmental swab. The norovirus GII from a fifth event attendee (attendee 28) was indistinguishable from the others in region C (283 bp, data not shown) but its identification in region B was not possible as the semi-nested PCR was negative for this sample. Further capsid sequencing in the P2 domain showed that sequences from the three catering staff A, B and C and two attendees (attendees 25 and 43) were indistinguishable from each other (Fig. 3), and were 1 bp different from those of two other attendees (attendees 26 and 28). The GII.4 P2 domain PCR assay was not performed on the environmental swab sample and attendee 29. The norovirus GII detected from five other attendees were not genotyped.
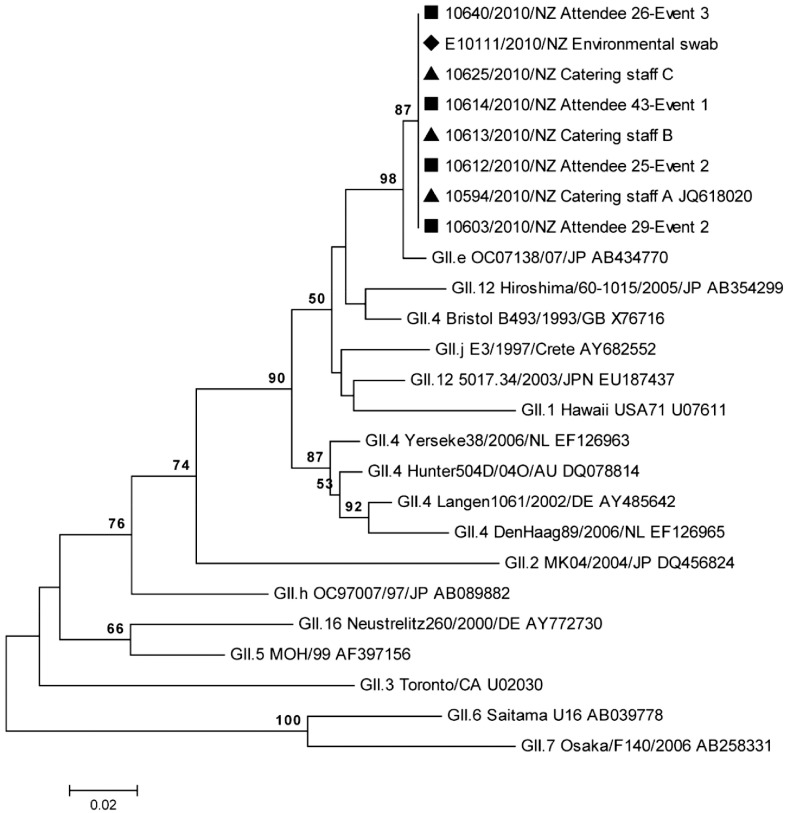
Fig. 2.
Neighbour-joining phylogenetic analysis of the norovirus partial polymerase region B (172 bp) showing the relationship between noroviruses identified in samples from attendees at events 1–3 (▪), catering staff A, B and C (▲), environmental swab (♦) and selected reference noroviruses. Indistinguishable norovirus sequences are represented on the same node. Bootstrap values from 1000 replicates are shown where greater than 50%.
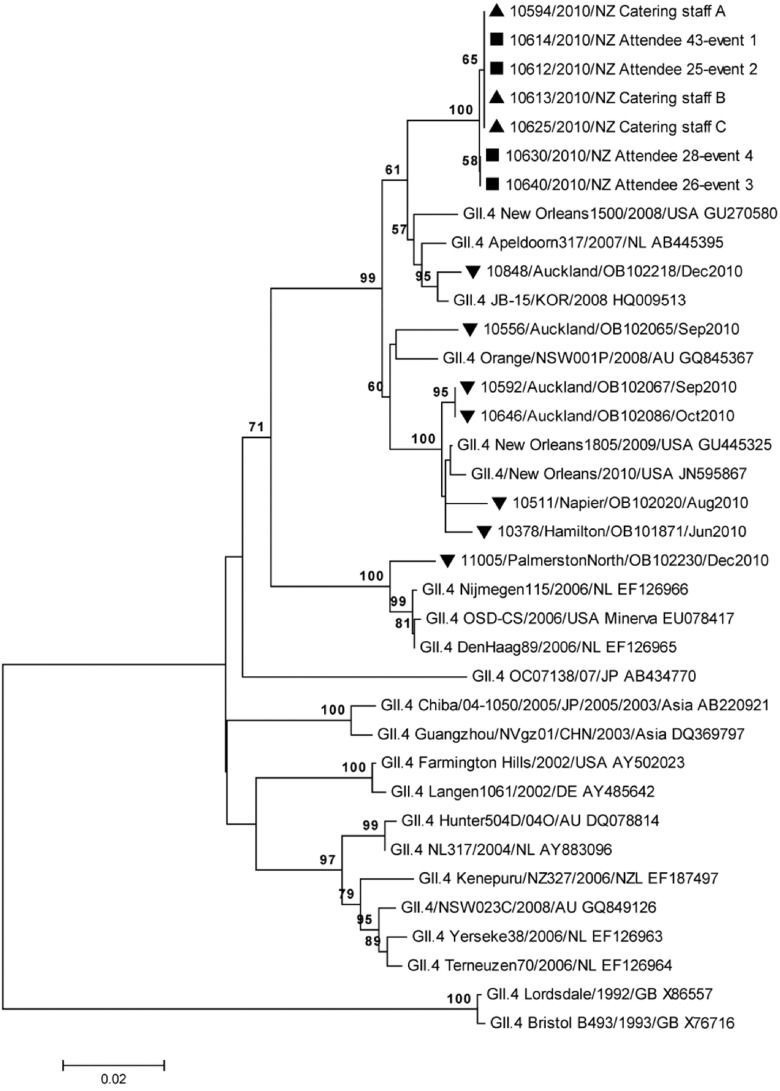
Fig. 3.
Neighbour-joining phylogenetic analysis of the norovirus P2 domain (459 bp) showing the relationship between noroviruses identified in samples from attendees at events 1–4 (▪), catering staff A, B and C (▲), selected reference norovirus GII.4 strains, and representative circulating norovirus GII.4 strains identified in New Zealand between June and December 2010. Strains are shown in the format: laboratory identity number/location/outbreak identity number/outbreak date (▼). Indistinguishable norovirus sequences are represented on the same node. Bootstrap values from 1000 replicates are shown where greater than 50%.
Outbreak control
Information was provided to all affected groups to prevent secondary spread. Summary recommendations included remaining away from work until symptoms had resolved, not undertaking any high-risk activities (in particular, food preparation for others) until 48 h had elapsed following resolution of symptoms, performing thorough hand hygiene and using appropriate cleaning products for toilet surfaces. Thorough cleaning of the catering company premises was performed using hypochlorite disinfectant. The catering company manager was advised to develop and enforce policies to stand-down sick food handlers until free of gastroenteritis symptoms for at least 48 h, and to implement a food safety programme from a nationally approved template [30].
DISCUSSION
This investigation reports an outbreak of norovirus gastroenteritis that affected five separate events supplied with food by a single catering company. Norovirus was detected in stool specimens collected from attendees at each affected event, from food handlers who had prepared food items for the events, and from an environmental surface at the catering company premises. Multiple food items were associated with illness at the different events, suggesting that contamination may have occurred through food preparation prior to distribution to event venues.
Norovirus genome sequencing in multiple regions allowed for both identification and determination of the genetic relationship of the noroviruses detected in specimens from the catering staff, attendees and the environmental swab. Genotyping determined by analysis of the commonly used norovirus regions B (ORF-1) and C (ORF-2) identified an unusual GII.e/GII.4 recombinant norovirus. Sequencing of the less conserved, hypervariable P2 domain for verification of the similarity between strains showed a minor difference (one base) in two of the attendees compared to the other noroviruses. This does not necessarily imply that the norovirus was not linked but is more likely to be due to a mutation [31].
All but two attendees of events 1 and 2 who developed illness had consumed food provided on 20 September or before 11:45 hours on 21 September. We consider that the source of contamination of food provided to these attendees was a single infected food handler (catering staff A) who was continuing to shed norovirus following cessation of symptoms. While two other catering company employees (catering staff B and C) were also confirmed with norovirus infection, food preparation for these attendees had been completed and food delivered to event venues at least 24 h before either catering staff B or C developed symptoms. As this interval is considerably longer than the 14-h period of norovirus shedding shown to occur before symptoms [18], neither were likely to have contaminated this food in their pre-symptomatic periods. Transmission from these employees to event attendees consuming food on 22 September cannot be excluded, although neither was directly involved in food preparation and both were stood down from work from the time of onset of their illness. The finding that the norovirus detected on the toilet door handle at the catering company was indistinguishable in regions B and C from the cases suggests possible transfer from the hands of an infected staff member, providing a further clue that virus was transmitted to food by hand contamination. No single main ingredient was common to all food items found to be associated with illness; however, contamination from a minor ingredient or cross-contamination between ingredients cannot be excluded.
Illness resulting from post-symptomatic norovirus shedding by food handlers has been noted previously [21, 32–39], although due to the observational nature of these studies it has not always been possible to exclude alternative explanations, even if recognized at the time [40]. Some of these outbreaks occurred in the context of pre-existing contamination of the food preparation environment by infected food handlers [32, 34, 35] or their family members [33], which may have been the source of food contamination. In other investigations, colleagues of the implicated food handler who were also involved in food preparation were either confirmed with asymptomatic norovirus infection [36] or did not have infection excluded through testing [21, 34, 35, 39], opening the possibility of transmission from asymptomatic norovirus carriers [41]. These concerns were addressed by our investigation. First, a detailed history of workplace contact was collected from catering staff A and corroborated against staffing records, indicating no contact with the workplace while symptomatic or in the likely period of pre-symptomatic norovirus shedding, and therefore no possibility of environmental contamination prior to the end of symptoms. Second, all catering company employees regardless of symptoms were tested for norovirus, and other than the three known symptomatic individuals none were found to be infected. Our failure to detect asymptomatic carriage was unlikely to have been because some samples were collected from some asymptomatic employees a few days later than those from their unwell colleagues, as norovirus shedding has been shown to continue for a median of 28 days after inoculation [18].
Other possible explanations for our findings are unlikely. The GII.e/GII.4 attributed to be the causative agent norovirus detected in this outbreak had not been previously identified in New Zealand. In addition, the noroviruses in these associated outbreaks were well defined and clearly distinguishable from other GII.4 variants detected in New Zealand from June to December 2010. This data supports the argument against coincidental and unrelated infection of event attendees and catering company workers. Norovirus contamination of a food ingredient prior to preparation by the catering company is an unlikely explanation for the outbreaks because food items with unrelated ingredients were associated with illness. Furthermore, the onset of illness in the first infected food handler preceded contact with ingredients used in preparation of food for the functions on 20 September.
Among attendees of events 1 and 2, the risk of norovirus infection was significantly increased in persons who consumed food prepared up to 45 h following cessation of catering staff A's symptoms. Three individuals became sick after eating food items prepared after this period; however, these items were prepared during the period of possible pre-symptomatic shedding by the last of the three infected employees and therefore may not be attributable to catering staff A alone. A number of factors may have been responsible for the reduction in risk to persons exposed to food prepared more than 45 h after the end of catering staff A's symptoms. The range of food prepared after this time may have required less manual preparation after cooking, and therefore less likely to have been contaminated; we attempted to assess this possibility and found that the proportion of attendees consuming food manually prepared after cooking did not vary significantly across the 3-day period of the events, and that the risk of illness associated with the time of food preparation remained significant despite adjustment for manual preparation of food items. It remains possible that catering staff A may have altered his food handling or hand hygiene practices from the afternoon of 21 September onward, improving food safety and reducing transmission, and although not reported at interview or detected in the investigation this cannot be excluded as a potential explanation for reduction in disease risk. We did not collect data on attendees' concurrent illness or medication use that may have altered susceptibility to infection, although we did not find any age or sex associations with illness. Finally, catering staff A may have been shedding less viable norovirus in the period following 45 h after symptom cessation, resulting in less virus transmission to food; however, this cannot be proven from these data. Contamination of food items prepared by an infected food handler more than 2 days after end of symptoms is thought to have occurred previously [36], although this occurred in the context where another food handler was found to have asymptomatic infection. Illness was also associated with consumption of food that had received manual preparation after cooking, which is consistent with findings that norovirus transfer to ready-to-eat food items can occur through manual handling [38, 42], and that virus inactivation is related to temperature and food matrix [43].
A total of 53 individuals in five different events were considered to have become ill as a result of this outbreak. Norovirus infection in food handlers working in centralized catering businesses has previously triggered outbreaks resulting in many cases of illness, both regionally [21, 37, 38] and nationally [8]. The outbreak reported here demonstrates the impact that a sole infected food handler may have in the catering setting, and reinforces the need for catering companies to adopt food safety programmes that enable workers who are recovering from gastrointestinal illness to cease food handling until at least 2 days have elapsed following cessation of symptoms. This requirement is not without challenges: for example, in New Zealand food service employees are typically required to draw down on their sick leave entitlement while stood down from work, and those on casual contracts may receive no income while absent from duties. Efforts to reduce financial disincentives faced by food workers on declaring that they have had illness are therefore desirable. At all times, effective hand hygiene should be practised by catering company workers.
ACKNOWLEDGEMENTS
We are grateful to the following individuals and organizations: Dawn Croucher, Malet Rivera-Aban and Laetitia Kaas, Institute of Environmental Science and Research Limited (ESR), for norovirus analysis. Dr Harry Vennema, National Institute for Public Health and the Environment, The Netherlands, and Peter White and John-Sebastian Eden, University of New South Wales, Australia, for advice and assistance with norovirus genotyping. Ministry for Primary Industries officials for environmental investigation reports; the organizations hosting the affected events, for making staff available to assist the investigation; the event attendees, for their participation; the catering company management, for their openness and willingness to support the investigation; and the anonymous peer reviewers, whose many helpful comments enabled us to greatly improve the manuscript.
Norovirus analysis was funded by the New Zealand Ministry of Health.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.de Wit MA, et al. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. American Journal of Epidemiology 2001; 154: 666–674. [DOI] [PubMed] [Google Scholar]
- 2.Phillips G, et al. Community incidence of norovirus-associated infectious intestinal disease in England: improved estimates using viral load for norovirus diagnosis. American Journal of Epidemiology 2010; 171: 1014–1022. [DOI] [PubMed] [Google Scholar]
- 3.Scallan E, et al. Foodborne illness acquired in the United States – major pathogens. Emerging Infectious Diseases 2011; 17: 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becker KM, et al. Transmission of Norwalk virus during football game. New England Journal of Medicine 2000; 343: 1223–1227. [DOI] [PubMed] [Google Scholar]
- 5.Kuusi M, et al. A prolonged outbreak of Norwalk-like calicivirus (NLV) gastroenteritis in a rehabilitation centre due to environmental contamination. Epidemiology and Infection 2002; 129: 133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones EL, et al. Role of fomite contamination during an outbreak of norovirus on houseboats. International Journal of Environmental Health Research 2007; 17: 123–131. [DOI] [PubMed] [Google Scholar]
- 7.Evans MR, et al. An outbreak of viral gastroenteritis following environmental contamination at a concert hall. Epidemiology and Infection 2002; 129: 355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson AD, et al. Multistate outbreak of Norwalk-like virus gastroenteritis associated with a common caterer. American Journal of Epidemiology 2001; 154: 1013–1019. [DOI] [PubMed] [Google Scholar]
- 9.Hewitt J, et al. Gastroenteritis outbreak caused by waterborne norovirus at a New Zealand ski resort. Applied and Environmental Microbiology 2007; 73: 7853–7857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marks PJ, et al. Evidence for airborne transmission of Norwalk-like virus (NLV) in a hotel restaurant. Epidemiology and Infection 2000; 124: 481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simmons G, et al. Raw oyster consumption and outbreaks of viral gastroenteritis in New Zealand: evidence for risk to the public's health. Australian and New Zealand Journal of Public Health 2001; 25: 234–240. [DOI] [PubMed] [Google Scholar]
- 12.Falkenhorst G, et al. Imported frozen raspberries cause a series of norovirus outbreaks in Denmark, 2005. Eurosurveillance 2005; 10: E050922.2. [DOI] [PubMed] [Google Scholar]
- 13.Widdowson M, et al. Norovirus and foodborne disease, United States, 1991–2000. Emerging Infectious Diseases 2005; 11: 95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moe CL. Preventing norovirus transmission: how should we handle food handlers? Clinical Infectious Diseases 2009; 48: 38–40. [DOI] [PubMed] [Google Scholar]
- 15.Food Standards Agency. Food handlers: fitness to work. Regulatory guidance and best practice advice for food business operators. London: Food Standards Agency, 2009, p. 9. [Google Scholar]
- 16.Communicable Diseases Network Australia. Guidelines for the public health management of gastroenteritis outbreaks due to norovirus or suspected viral agents in Australia. Canberra: Commonwealth of Australia, 2010, p. 33. [Google Scholar]
- 17.Centers for Disease Control and Prevention. Updated norovirus outbreak management and disease prevention guidelines. Morbidity and Mortality Weekly Report: Recommendations and Reports 2011; 60: 1–15. [PubMed] [Google Scholar]
- 18.Atmar RL, et al. Norwalk virus shedding after experimental human infection. Emerging Infectious Diseases 2008; 14: 1553–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aoki Y, et al. Duration of norovirus excretion and the longitudinal course of viral load in norovirus-infected elderly patients. Journal of Hospital Infection 2010; 75: 42–46. [DOI] [PubMed] [Google Scholar]
- 20.Karim MR, Pontius FW, LeChevallier MW. Detection of noroviruses in water–summary of an international workshop. Journal of Infectious Diseases 2004; 189: 21–28. [DOI] [PubMed] [Google Scholar]
- 21.Friedman DS, et al. An outbreak of norovirus gastroenteritis associated with wedding cakes. Epidemiology and Infection 2005; 133: 1057–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ozawa K, et al. Norovirus infections in symptomatic and asymptomatic food handlers in Japan. Journal of Clinical Microbiology 2007; 45: 3996–4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.R Development Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2011. (http://www.R-project.org). [Google Scholar]
- 24.Kageyama T, et al. Broadly reactive and highly sensitive assay for Norwalk-like viruses based on real-time quantitative reverse transcription-PCR. Journal of Clinical Microbiology 2003; 41: 1548–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson AD, et al. A waterborne outbreak of Norwalk-like virus among snowmobilers – Wyoming, 2001. Journal of Infectious Diseases 2003; 187: 303–306. [DOI] [PubMed] [Google Scholar]
- 26.Kojima S, et al. Genogroup-specific PCR primers for detection of Norwalk-like viruses. Journal of Virological Methods 2002; 100: 107–114. [DOI] [PubMed] [Google Scholar]
- 27.Xerry J, et al. Transmission events within outbreaks of gastroenteritis determined through analysis of nucleotide sequences of the P2 domain of genogroup II noroviruses. Journal of Clinical Microbiology 2008; 46: 947–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroneman A, et al. An automated genotyping tool for enteroviruses and noroviruses. Journal of Clinical Virology 2011; 51: 121–125. [DOI] [PubMed] [Google Scholar]
- 29.Tamura K, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Molecular Biology and Evolution 2011; 28: 2731–2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.New Zealand Food Safety Authority. Food control plan: food service and catering, 2011.
- 31.Verhoef L, et al. Selection of a phylogenetically informative region of the norovirus genome for outbreak linkage. Virus Genes 2012; 44: 8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White KE, et al. A foodborne outbreak of Norwalk virus gastroenteritis. Evidence for post-recovery transmission. American Journal of Epidemiology 1986; 124: 120–126. [DOI] [PubMed] [Google Scholar]
- 33.Iversen AM, et al. Two outbreaks of foodborne gastroenteritis caused by a small round structured virus: evidence of prolonged infectivity in a food handler. Lancet 1987; 2: 556–558. [DOI] [PubMed] [Google Scholar]
- 34.Reid JA, et al. Role of infected food handler in hotel outbreak of Norwalk-like viral gastroenteritis: implications for control. Lancet 1988; 2: 321–323. [DOI] [PubMed] [Google Scholar]
- 35.Patterson T, Hutchings P, Palmer S. Outbreak of SRSV gastroenteritis at an international conference traced to food handled by a post-symptomatic caterer. Epidemiology and Infection 1993; 111: 157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parashar UD, et al. An outbreak of viral gastroenteritis associated with consumption of sandwiches: implications for the control of transmission by food handlers. Epidemiology and Infection 1998; 121: 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Telfer B, et al. A large outbreak of norovirus gastroenteritis linked to a catering company, New South Wales, October 2003. New South Wales Public Health Bulletin 2004; 15: 168–171. [PubMed] [Google Scholar]
- 38.Malek M, et al. Outbreak of norovirus infection among river rafters associated with packaged delicatessen meat, Grand Canyon, 2005. Clinical Infectious Diseases 2009; 48: 31–37. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Multisite outbreak of norovirus associated with a franchise restaurant – Kent County, Michigan, May 2005. Morbidity and Mortality Weekly Report 2006; 55: 395–397. [PubMed] [Google Scholar]
- 40.Curry A, et al. Small round structured viruses and persistence of infectivity in food handlers. Lancet 1987; 2: 864–865. [DOI] [PubMed] [Google Scholar]
- 41.Barrabeig I, et al. Foodborne norovirus outbreak: the role of an asymptomatic food handler. BMC Infectious Diseases 2010; 10: 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daniels NA, et al. A foodborne outbreak of gastroenteritis associated with Norwalk-like viruses: first molecular traceback to deli sandwiches contaminated during preparation. Journal of Infectious Diseases 2000; 181: 1467–1470. [DOI] [PubMed] [Google Scholar]
- 43.Bertrand I, et al. The impact of temperature on the inactivation of enteric viruses in food and water: a review. Journal of Applied Microbiology 2012; 112: 1059–1074. [DOI] [PubMed] [Google Scholar]