SUMMARY
Using polymerase chain reaction (PCR) to detect faecal hepatitis A virus (HAV) can be a useful tool for investigating HAV outbreaks, especially in low-endemic countries. We describe the use of faecal HAV PCR as a non-invasive tool for screening. Two Dutch children visiting different daycare centres were diagnosed with hepatitis A in 2011. A systematic contact investigation was started in the daycare centres and relevant contacts were screened. The faecal HAV PCR test was used to screen the children. The employees were screened with a serum IgM. The faecal HAV PCR test proved to be an appropriate tool for screening. The screening of a total of 135 children and employees in the daycare centres resulted in evidence of eight asymptomatic infections and transmission to three related daycare centres. Control measures were taken including immunization. Compared to an epidemiological investigation without screening, 144 extra contacts were vaccinated based on the screening results. This most likely led to improved prevention of expansion of the outbreak.
Key words: Hepatitis A, infectious disease control, laboratory tests, molecular typing methods, outbreaks
INTRODUCTION
Hepatitis A virus (HAV) is a vaccine-preventable, acute inflammatory liver disease causing little or no symptoms of infection in young children, whereas it may result in severe morbidity and even mortality in adults [1, 2]. HAV is transmitted via the faecal–oral route in person-to-person contact or via contaminated water and food. Clinical cases are considered to be infectious from 1 to 2 weeks before the onset of symptoms to 1–2 weeks after. However, recent studies have reported cases with high faecal excretion of HAV during at least the first month of illness, suggesting some patients may be infectious for a longer period than currently assumed [3, 4]. The diagnostic gold standard for an acute HAV infection is the detection of anti-HAV immunoglobulin M (anti-HAV IgM) or the detection of HAV RNA in serum [3]. Alternative media for viral detection have been studied and saliva and faeces have proved to be effective non-invasive media for HAV RNA detection [5–8].
Low HAV prevalence in industrialized countries makes all age groups susceptible to infection [9, 10]. Introduction of HAV in daycare centres in these countries may easily cause outbreaks because HAV has a long incubation period and children show little or no signs of infection. Moreover, transmission between children occurs via various routes such as direct contact, sharing of toys, sharing of food or poor toilet hygiene [5, 8, 11]. In such outbreaks an epidemiological investigation of the outbreak followed by mass immunization of the people identified as being at risk is the cornerstone of outbreak management [5, 8, 11–13].
However, identification of the vaccination target group can be difficult. At time of notification the duration and the extent of viral circulation is usually uncertain and parents of young or special-needs children may hesitate to participate because they perceive mass vaccination as child-unfriendly. In such a situation screening of the direct contacts may complement the epidemiological investigation: it may identify asymptomatic cases and thus enable fine tuning of the vaccination target group [6, 14]. Viral detection on faecal samples can be an alternative screening tool to serological screening. Using polymerase chain reaction (PCR) for detection of faecal HAV has important benefits over serological screening. It is an accessible and child-friendly technique that overcomes the difficulties and objections related to collecting blood from children. The samples can be collected at home by the parents and can be sent to the laboratory by regular mail. The sample collection does not require any trained staff.
In this context we report on an outbreak of hepatitis A involving several daycare centres, where faecal HAV PCR was used to define the children at risk and the related vaccination target group.
In January 2011 the Municipal Health Service (MHS) in the rural part of the Dutch province of Utrecht managed a HAV outbreak involving several daycare centres. The outbreak started with the notification of a total of seven hepatitis A infections within one family of Dutch-Moroccan descent. The diagnoses resulted from active case-finding by the general practitioner following the HAV infection in a 21-year-old family member who suffered from jaundice since the last week of December 2010 (Fig. 1). This report focuses on two family members who were linked to daycare centres.
Fig. 1.
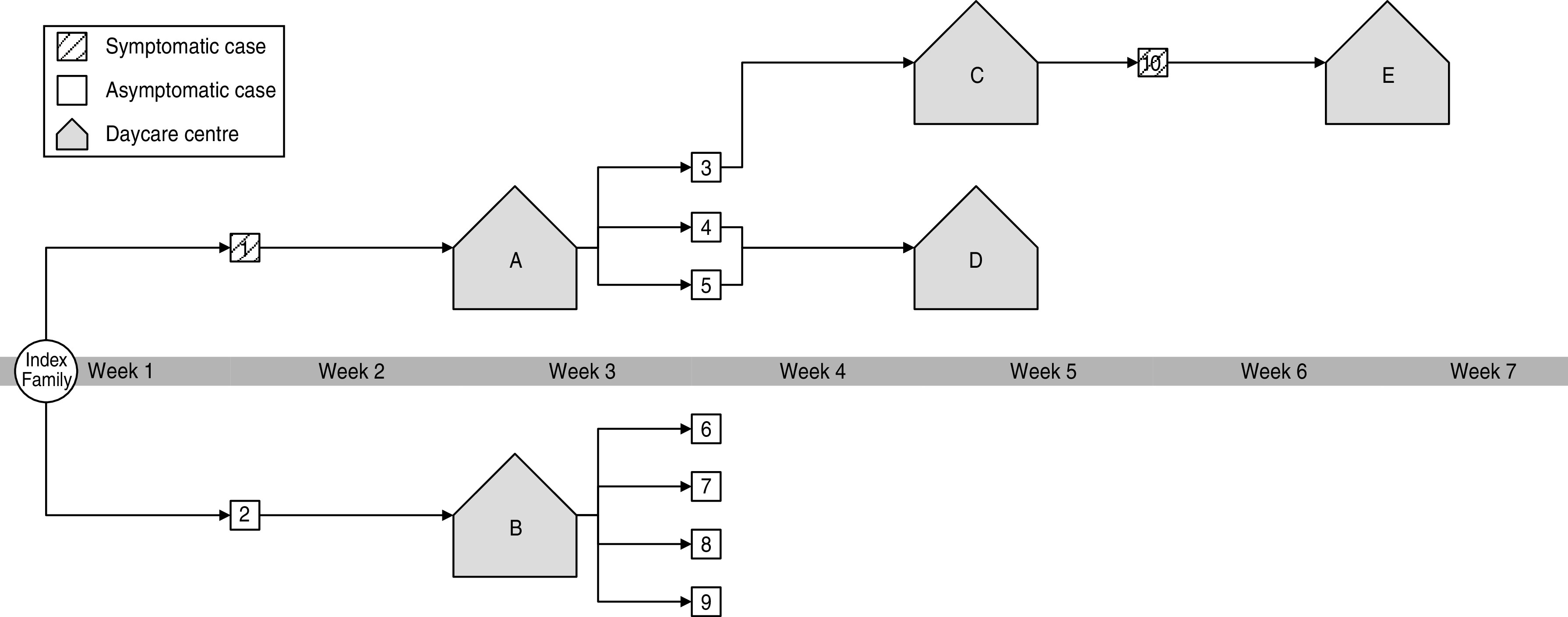
The outbreak overview.
The first was an 18-year-old girl (case 1, centre A; Fig. 1) who visited a special-needs school for children aged 4–21 years. She had been symptomatic since the second week of December 2010. The second was a 3-year-old boy (case 2, centre B; Fig. 1). He remained asymptomatic and visited a nursery for children aged 0–4 years.
In case of HAV introduction, the Dutch national guidelines recommend mass vaccination of all contacts that share toilet facilities in daycare centres. However, we decided to first screen the direct contacts before identifying the vaccination target group. We chose this approach for two reasons: (1) the jaundice of case 1 started in the second week of December 2010 suggesting a longer period of viral circulation; (2) within the daycare centres the role of toilet facilities in transmission was unclear: in centre A the index was in nappies and thus did not share toilet facilities with the direct group members and in centre B the toddler toilets were alternately used by another daycare group, but direct contact between case 2 and the children of the other group did not occur.
Because of the relatively new use of the faecal HAV PCR test as a tool for screening in outbreak management, we consider a discussion of our experiences to be valuable.
METHODS
As soon as the MHS was notified about the infections, a systematic contact investigation was started. All high-risk contacts were offered screening, i.e. cases 1 and 2, centres A, and B (Fig. 1).
A high-risk contact was defined as a ‘group member’ or ‘sharing toilet/changing facilities’ with a case during the infectious period (Fig. 2). The infectious period for a symptomatic IgM-positive case was defined as 1 week prior to the onset of symptoms. An asymptomatic case was considered infectious 4 weeks prior to serum IgM detection or 18 days prior to HAV RNA detection in faeces. These periods were pragmatically selected based on the information on HAV excretion in the Dutch National Guidelines.
Fig. 2.
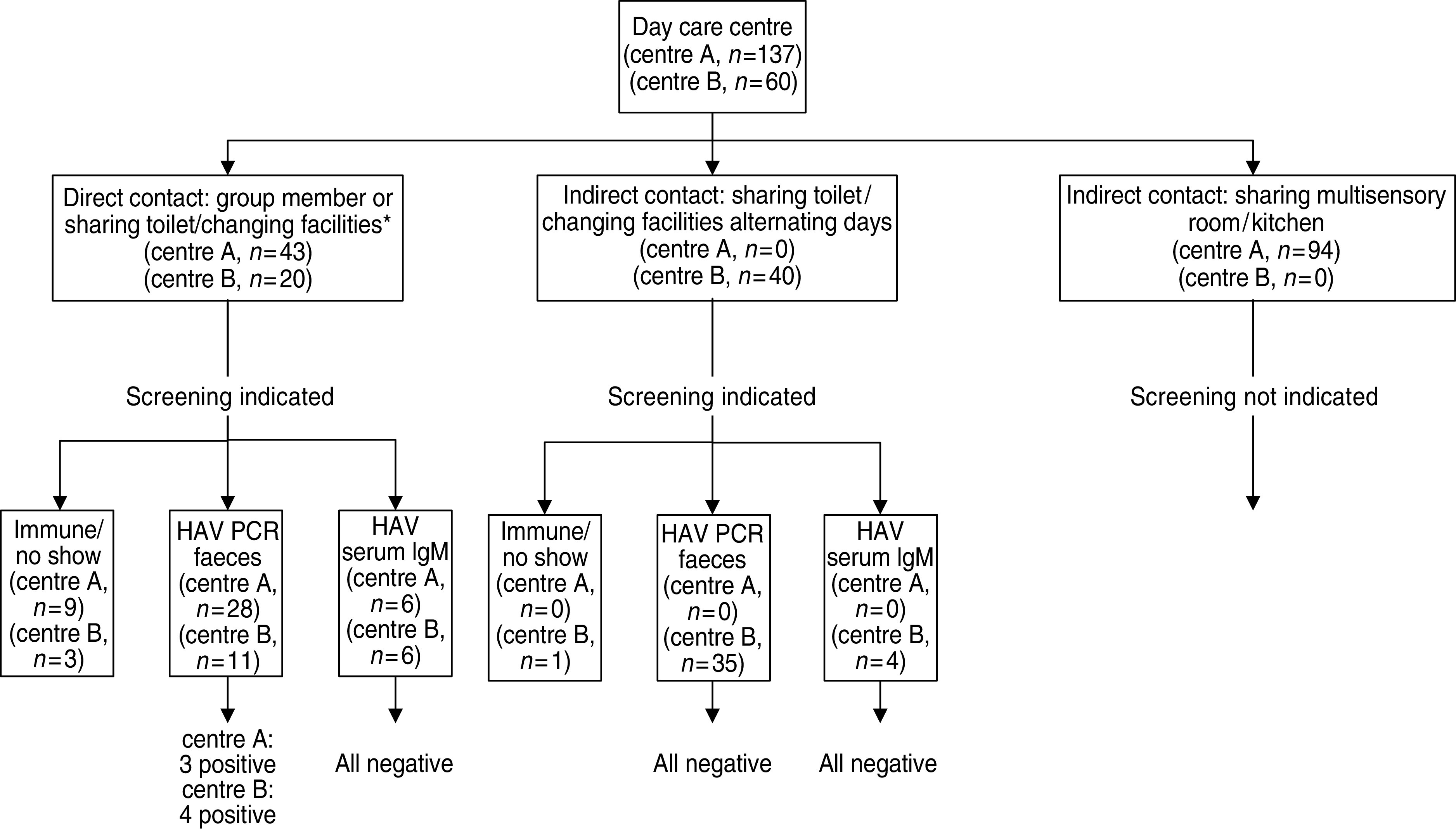
Method of outbreak investigation in centres A and B. * In centre A the index case was in nappies and therefore did not share toilet facilities with the direct group members who used the toilet facilities.
Each time the screening identified a positive case a new contact investigation was started and each time the investigation linked a new daycare centre, the screening was repeated (centres C and D; Fig. 1). When the newly identified case was an employee linked to a new daycare centre, the screening was not repeated because transmission through employees was considered less likely (case 10, centre E; Fig. 1).
HAV RNA detection in faecal material was used for the screening of children. The faecal samples were collected by the parents and sent to the laboratory by regular mail, in properly packaged sample collection tubes. All HAV RNA detection was performed by the National Institute of Public Health and the Environment (RIVM) in The Netherlands. A real-time reverse transcription–polymerase chain reaction (RT–PCR) was used to detect HAV RNA in total nucleic acid extracted from faecal samples and serum using a procedure similar to one described previously [15]. Positive samples were further analysed to determine the HAV genotype by comparing the sequence to a database of reference sequences. Employees were screened through classic serum IgM by commercial enzyme immunoassay (EIA) via the individual general practitioners and related laboratories. IgM-positive samples were sent to the RIVM for further analyses to determine the HAV genotype.
The estimated attack rate was calculated by dividing the number of hepatitis A cases (asymptomatic and symptomatic) by the total number of persons screened, multiplied by 100.
RESULTS
In this outbreak a total of 173 high-risk contacts were identified of which 135 contacts were screened for HAV (Table 1). This resulted in the identification of eight additional HAV infections (cases 3–10; Fig. 1) and linked three additional centres to this outbreak (centres C, D, E; Fig. 1). HAV RNA was detected in seven faecal samples of children and anti-HAV IgM was detected in the serum of one employee. All children were asymptomatic, the employee reported malaise but jaundice was not observed. The estimated AR in this outbreak was 5·9 (8/135 × 100).
Table 1.
Number of contacts screened per daycare centre
The overall participation in the screening was high: 90% chose to participate. Of the risk contacts 55% (96/173) were screened with faecal HAV PCR (children), 23% (39/173) with HAV serology (employees), 12% (21/173) were already immune to HAV (with a history of vaccination or living in an endemic area) and 10% (17/173) chose not participate in the screening (Table 1).
Figure 2 shows that the toilet facilities were not the primary transmission route at the daycare centres. At centre A screening resulted in the identification of a total of three hepatitis A cases in direct group members who were linked to the index case by group contact only: the index case was in nappies and therefore did not share toilet facilities with these three cases who used the toilet facilities. In centre B screening showed no viral circulation in children that shared the toilet facilities on alternate days but did not have direct contact with the index case (Fig. 2).
Table 2 compares the epidemiological approach and the screening approach and shows that 144 extra contacts were vaccinated based on the screening results. In centre A additional screening led to a larger vaccination target group and in centre B to a smaller vaccination target group. Contacts in centres C, D and E were linked to the outbreak by the results of the screening only and would therefore not have been vaccinated in an epidemiological approach without additional screening.
Table 2.
Number of contacts in the vaccination target group in the outbreak investigation without screening compared to outbreak investigation and additional screening
| Centre | Outbreak investigation | Outbreak investigation and additional screening | Target group for vaccination identified through additional screening |
|---|---|---|---|
| A | 43 | 137 | 94 |
| B | 60* | 40† | −20 |
| C + E | 0 | 30 | 30 |
| D | 0 | 40 | 40 |
| Total | 103 | 247 | 144 |
Direct contacts and contacts sharing toilet facilities.
Direct contacts only.
This outbreak is most likely caused by a ‘seeding event’ related to Morocco. Apart from the seven infections within the index family and the eight transmissions found in the outbreak investigation, no further notifications of HAV infections were reported to the MHS. The three family members mentioned here (index case and cases 1 and 2; Fig. 1) did not travel abroad but three other asymptomatic family members visited Morocco in the third week of October 2010. This epidemiologically links the incubation period of the first symptomatic family case (case 1; Fig. 1) to Morocco.
The sequence analysis confirms this: two viral strains from the family were genotyped as type 1A with a sequence most similar to sequences found in travellers returning from Morocco.
The suggestion is that these children subsequently transmitted the HAV virus to the daycare centres. However, this could not be confirmed by sequence analysis of the virus because the HAV viral titre in the faecal samples in this outbreak was not sufficient for genotyping.
DISCUSSION
In this hepatitis A outbreak, faecal HAV PCR was shown to be an appropriate screening tool. Additional screening in an epidemiological approach identified eight additional cases and linked three additional daycare centres. This led to the assumption that toilet facilities were not the primary transmission route and resulted in a vaccination target group that differed considerably from the target group in the epidemiological approach.
We do not know the number of cases of HAV that have been prevented by the additional screening and the related vaccination target group, since the attack rates from previously published outbreaks are too heterogeneous to allow for estimations. Previously published outbreak attack rates range from 2·8 to 42 and these outbreaks differ in terms of settings and age profiles [16, 17].
Faecal HAV PCR has important benefits over serological screening. The collection and transport of material does not require trained staff, making it an accessible technique. Contrary to serological screening, the technique is non-invasive and therefore very suitable for outbreaks involving children.
Compared to serological testing, HAV RNA detection will find more (a)symptomatic HAV prevalence since HAV RNA is present before anti-HAV IgM [6].
A positive faecal HAV PCR test shows the presence of viral RNA but remains inconclusive on the question of whether this RNA is able to form cultivatable virus strains that replicate in vivo and infect others. The objective of screening in HAV outbreaks involving daycare centres is not to identify infectious cases, but to determine the likelihood of HAV viral circulation. Considering the presence of HAV viral RNA in the number of children involved in this outbreak, viral circulation within the centres is implicit and it is likely that further transmission to the population has been prevented by the vaccination intervention.
It may be expected that additional screening will increase the number of vaccinations. However, in this outbreak the number of vaccinations in centre B decreased. This was caused by the fact that the Dutch national guidelines advise mass vaccination of all contacts that share toilet facilities in case of a child with hepatitis A in a daycare centre. However, the outbreak investigation in centre B showed no viral circulation among the toddlers that shared toilet facilities but did not have any direct contact with case 2. Consequently we concluded that the children only sharing toilet facilities and not having any direct contact were not at risk and could therefore be excluded from vaccination.
An additional advantage of the use of screening (both molecular and serological) in outbreak management is that it yields material for genetic typing of the virus. This may lead to useful insights on the sources of infection and on transmission routes [18, 19]. Moreover it may help to discriminate between real outbreaks and pseudo-outbreaks that are caused by multiple unrelated viral introductions [20].
Seven out of eight cases detected via screening in this outbreak were asymptomatic. Studies about infectiousness of asymptomatic cases are rare despite their relevance for outbreak management [5]. Further research is needed on the relevance of asymptomatic cases for the continuation of an outbreak. Many outbreak reports suggest continued transmission in the community by asymptomatic cases [5, 8, 12]. Outbreaks in The Netherlands are reported to remain small after the vaccination of the contacts that are considered to be at risk in epidemiological investigation without screening [18, 21, 22].
The costs of screening in HAV outbreak management are an important limitation. We cannot estimate the cost effectiveness of our intervention, since we were unable to give a realistic estimation of the number of cases prevented by the identification of the eight asymptomatic cases and the related vaccination intervention. Furthermore, estimates of the costs of an outbreak of hepatitis A must be interpreted conservatively because of difficulties in describing and valuing all costs generated by an outbreak [23]. The costs of this outbreak should include direct costs, such as medical resources and costs of outbreak control, as well as indirect costs of non-medical resources such as lost time at work. Intervention in a HAV outbreak, however, is reported to be cost effective [23]. Direct costs related to the management of an hepatitis A outbreak are reported to be high and are usually underestimated [17, 23]. Post-exposure prophylaxis is the major cost factor in HAV outbreak management [23]. The costs of screening will add up to the cost of vaccination and must be compared with the prevented morbidity.
In conclusion, the faecal HAV PCR test is a new, non-invasive tool appropriate for screening that may well complement the epidemiological investigation. Further research is needed on the relevance of asymptomatic cases for outbreak management and on the cost-effectiveness of the method.
ACKNOWLEDGEMENTS
We thank the employees, the parents and the children of the daycare centres for their kind cooperation that made the screening possible.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Hadler SC, et al. Hepatitis A in day-care centers. A community-wide assessment. New England Journal of Medicine 1980; 302: 1222–1227. [DOI] [PubMed] [Google Scholar]
- 2.Lednar WM, et al. Frequency of illness associated with epidemic hepatitis A virus infections in adults. American Journal of Epidemiology 1985; 122: 226–233. [DOI] [PubMed] [Google Scholar]
- 3.Amado LA, et al. Comparison between serum and saliva for the detection of hepatitis A virus RNA. Journal of Virological Methods 2008; 148: 74–80. [DOI] [PubMed] [Google Scholar]
- 4.Tjon GM, et al. High and persistent excretion of hepatitis A virus in immunocompetent patients. Journal of Medical Virology 2006; 78: 1398–1405. [DOI] [PubMed] [Google Scholar]
- 5.Morais LM, et al. Early infection and asymptomatic spread of hepatitis A virus in a public child care center in Rio de Janeiro, Brazil: should attending children under two years of age be vaccinated? Memórias do Instituto Oswaldo Cruz 2006; 101: 401–405. [DOI] [PubMed] [Google Scholar]
- 6.de Paula VS, et al. Detection of hepatitis A virus RNA in serum during the window period of infection. Journal of Clinical Virology 2004; 29: 254–259. [DOI] [PubMed] [Google Scholar]
- 7.van Steenbergen JE, et al. Two years' prospective collection of molecular and epidemiological data shows limited spread of hepatitis A virus outside risk groups in Amsterdam, 2000–2002. Journal of Infectious Diseases 2004; 189: 471–482. [DOI] [PubMed] [Google Scholar]
- 8.McFarland N, et al. An outbreak of hepatitis A affecting a nursery school and a primary school. Epidemiology and Infection 2011; 139: 336–343. [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine 2010; 28: 6653–6657. [DOI] [PubMed] [Google Scholar]
- 10.Verhoef L, et al. Changing risk profile of hepatitis A in The Netherlands: a comparison of seroprevalence in 1995–1996 and 2006–2007. Epidemiology and Infection 2011; 139: 1172–1180. [DOI] [PubMed] [Google Scholar]
- 11.Payne L, Coulombier D. Hepatitis A in the European Union: responding to challenges related to new epidemiological patterns. Eurosurveillance 2009; 14: 2–3. [PubMed] [Google Scholar]
- 12.Hrivniakova L, Slacikova M, Kolcunova S. Hepatitis A outbreak in a Roma village in eastern Slovakia, August–November 2008. Eurosurveillance 2009; 14: 11–13. [PubMed] [Google Scholar]
- 13.Roberts RJ, Palmer SR. Exposure to school children as a risk factor in a community outbreak of hepatitis A in young adults: a case control study. Epidemiology and Infection 2006; 134: 803–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumbang J, et al. Outbreak of hepatitis A in an extended family after importation by non-immune travellers. Epidemiology and Infection. Published online: 6 December 2011. doi: 10.1017/S0950268811002561. [DOI] [PubMed] [Google Scholar]
- 15.Jothikumar N, et al. Development and evaluation of a broadly reactive TaqMan assay for rapid detection of hepatitis A virus. Applied and Environmental Microbiology 2005; 71: 3359–3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matin N, et al. Hepatitis A surveillance in England – how many cases are not reported and does it really matter? Epidemiology and Infection 2006; 134: 1299–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taylor-Robinson DC, et al. Exploration of cost effectiveness of active vaccination in the control of a school outbreak of hepatitis A in a deprived community in the United Kingdom. Eurosurveillance 2007; 12: E5–6. [DOI] [PubMed] [Google Scholar]
- 18.Tjon G, et al. Different transmission patterns of hepatitis A virus for two main risk groups as evidenced by molecular cluster analysis. Journal of Medical Virology 2007; 79: 488–494. [DOI] [PubMed] [Google Scholar]
- 19.Tjon GM, et al. Molecular epidemiology of hepatitis A in Noord-Brabant, The Netherlands. Journal of Clinical Virology 2005; 32: 128–136. [DOI] [PubMed] [Google Scholar]
- 20.Bruisten SM, et al. The molecular epidemiology of hepatitis A in The Netherlands; the usefulness of typing isolated viral strains [in Dutch]. Nederlands Tijdschrift voor Geneeskunde 2007; 151: 2779–2786. [PubMed] [Google Scholar]
- 21.Sonder GJ, et al. Hepatitis A virus immunity and seroconversion among contacts of acute hepatitis A patients in Amsterdam, 1996–2000: an evaluation of current prevention policy. Amercian Journal of Public Health 2004; 94: 1620–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tjon G, et al. Different transmission patterns of hepatitis A virus for two main risk groups as evidenced by molecular cluster analysis. Journal of Medical Virology 2007; 79: 488–494. [DOI] [PubMed] [Google Scholar]
- 23.Luyten J, Beutels P. Costing infectious disease outbreaks for economic evaluation: a review for hepatitis A. Pharmacoeconomics 2009; 27: 379–389. [DOI] [PubMed] [Google Scholar]


