SUMMARY
In September 2009, an outbreak of Salmonella enterica serovar Enteritidis affected 327 of 1419 inmates at a London prison. We applied a cohort design using aggregated data from the kitchen about portions of food distributed, aligned this with individual food histories from 124 cases (18 confirmed, 106 probable) and deduced the exposures of those remaining well. Results showed that prisoners eating egg cress rolls were 26 times more likely to be ill [risk ratio 25·7, 95% confidence interval (CI) 15·5–42·8, P<0·001]. In a case/non-case multivariable analysis the adjusted odds ratio for egg cress rolls was 41·1 (95% CI 10·3–249·7, P<0·001). The epidemiological investigation was strengthened by environmental and microbiological investigations. This paper outlines an approach to investigations in large complex settings where aggregate data for exposures may be available, and led to the development of guidelines for the management of future gastrointestinal outbreaks in prison settings.
Key words: Epidemiology, outbreaks, Salmonella
INTRODUCTION
Salmonella spp. are the most common cause of foodborne outbreaks in the UK [1], the greatest proportion of which are caused by a particular Salmonella enterica serovar, Enteritidis [2]. Although the number of cases of Salmonella Enteritidis (SE) reported has declined in the UK since the 1990s [3], outbreaks continue to occur.
SE outbreak investigations across the UK have helped inform the development of control and prevention strategies [4]. Outbreaks have been reported in a variety of settings (including functions [5–7], fast food outlets [8] and restaurants [9, 10]) and from many different sources (including raw shell eggs [5, 7, 9], chicken [10] and frozen food [6]). SE outbreaks are more commonly reported in schools, private residences and residential institutions where a high number of persons may be exposed to a common contaminated food source, thus resulting in larger outbreaks [11]. Prisons are a similar such setting where large populations are at risk of developing foodborne illness [12]. In Japan, an Escherichia coli O6:H16 outbreak affected 1310 inmates [13]. Cieslak et al. completed a review of foodborne outbreaks in prisons in two US states (Georgia, Delaware) from 1974 to 1991. The authors found Salmonella was the most common cause reported, accounting for 37% (15/41) of outbreaks where the cause was known [14]. More recent reports from the USA include a Clostridium perfringens outbreak in 1994 which affected 40% of residents in a juvenile detention facility [15] and an outbreak in South Carolina, affecting a total of 688 out of 2317 inmates across four prisons, reportedly the largest outbreak of SE in the USA in 2001 [16].
Outbreaks in a prison setting pose a unique challenge to public health, where decisions on control and intervention must be balanced against external pressures from the judicial system. In this study we report an outbreak of SE in one of the largest prisons in Europe. We present the results of our microbiological, environmental and epidemiological investigations and highlight key considerations for the control and management of foodborne outbreaks in prison settings.
METHODS
Prison setting
The outbreak took place in a category B prison with up to 1680 male inmates and about 700 staff members present at time of the outbreak. Category B prisons house adult male prisoners (aged >21 years) who are a risk to the public but do not need the highest level of security [17]. The average length of stay in the prison was 6–12 months, before transfer or release, and about 30 prisoners per day attend court.
Outbreak notification and control
On 15 September 2009, healthcare staff in the prison identified six cases of diarrhoea and vomiting among prisoners. On 16 September 2009 the prison informed the local Health Protection Unit that about 70 prisoners were reporting gastrointestinal illness. Cases were found across all wings of the prison and a number of staff were affected. An Outbreak Control Team was convened on 17 September 2009 and a full investigation was conducted to identify the extent of the outbreak, the probable vehicle of infection and to advise on appropriate control measures.
Epidemiological investigation
A cross-sectional symptom surveillance questionnaire was completed daily by all prisoners from 17 to 21 September 2009. On the 17 September prisoners were also asked about symptoms over the period 14–16 September 2009. The information collected was used within the prison to determine the total number of prisoners affected each day and to identify symptomatic prisoners who required medical care.
All prisoners who ever reported one or more gastrointestinal symptom (diarrhoea, vomiting, high temperature) on the prison cross-sectional symptom surveillance questionnaire and those who tested positive for SE after providing a stool sample for microbiological testing, were asked to self-complete a structured ‘study questionnaire’ which included demographic details, clinical history and specific food exposures for the period 12–15 September 2009.
Case definition
Diarrhoea was defined as ⩾3 loose stools during a 24-h period. A confirmed case was defined as a prisoner who had diarrhoea with onset date after 13 September 2009 and had a laboratory-confirmed isolate of SE from a stool sample. A probable case was defined as a prisoner who had diarrhoea with onset after 13 September 2009, in the absence of microbiological confirmation. A secondary case was defined as an individual who had diarrhoeal illness and who shared a cell or had contact with a symptomatic individual (index) and whose symptom onset date was >2 days after the date of onset in the index case.
Analytical studies
(i) Cohort study
A retrospective cohort study was completed among prisoners, comparing food consumed by individual cases to aggregated totals of the food consumed by the prisoner population in general. Exposure data for all prisoners were sought from the kitchen where records had been kept of the number of servings (portions of food) prepared and distributed across the entire prison site each day. The total number of servings of each menu item prepared by the prison kitchen for lunch and dinner from 12 to 15 September 2009 was used to establish exposures of all prisoners based on an assumption that any prisoner eating a given food item would eat just one portion. For each food item, we used individual data from the study questionnaire to determine the number of exposed and unexposed cases, we then used information on the total number of portions available to deduce the number of those remaining well who were exposed and unexposed.
(ii) Case/non-case study
To enable adjustment for confounding, a case/non-case analysis was completed. Of those who completed the study questionnaire, individuals who met the confirmed or probable case definition were compared to non-cases (i.e. those who were identified from the prison cross-sectional symptom surveillance questionnaire as reporting diarrhoea, vomiting or high temperature, but who on completion of the study questionnaire described themselves as being asymptomatic).
Exclusions
Staff were excluded from the study population.
Data entry and analysis
The study questionnaire data was double-entered (to reduce data input error) into EpiData (EpiData Association, Denmark). In the cohort study univariate risk ratios and 95% confidence intervals (CI) were estimated using binary regression commands in Stata (StataCorp, USA). For the case/non-case analysis, univariate food-specific odds ratios for illness and 95% CIs were estimated using a generalized linear model. All exposure variables found to be significant at less than the 10% level (P<0·1 by χ2 test or Fisher's exact test as appropriate) were considered in the multivariable analysis. The multivariable logistic regression model was developed hierarchically by adding variables from the univariate analysis according to proportion exposed among those ill and P value, starting with the most stringent and then gradual relaxation of these criteria. At each step, the model was simplified in a backwards stepwise procedure by removing one at a time the least significant variable (i.e. P value >0·05) which was not a substantial confounder (a substantial confounder defined as any variable whose removal caused the odds ratios of the remaining variables in the model to change by >20%). This process was repeated until all variables had been assessed in this way. To generate the final model and improve parameter estimation precision two further steps were undertaken. First, protective variables were removed one at a time on biological plausibility considerations, and this was followed by the removal of non-significant factors (at the 5% level) provided the inferences of variables remaining in the model were unchanged. Odds ratios and P values from the final model were then estimated by means of exact logistic regression. All analyses were completed in Stata version 10.
Microbiological investigation
On 17 September stool samples were collected from 10 symptomatic prisoners. Further stool samples were collected from symptomatic prisoners during the outbreak.
All stool samples were examined at St George's Hospital Microbiology Laboratory according to protocols based on UK Standards for Microbiology Investigations [18]. Specifically, stool samples were plated on the following media: XLD medium (Oxoid, UK), Campylobacter medium (Oxoid) and SMAC (Oxoid), to look for Salmonella/Shigella, Campylobacter and E. coli O157, respectively. Samples were also inoculated in mannitol selenite broth (bioMérieux, France) followed by subculture to XLD for enhanced Salmonella detection. Samples were examined for Cryptosporidium spp. by auramine staining and tested for Clostridium difficile toxins using the enzyme immunoassay (EIA) Premier Toxin A/B (Launch Diagnostics, UK).
Salmonella spp. were identified by a combination of agglutination and biochemical methods using the API system (bioMérieux). All Salmonella isolates were sent to the Health Protection Agency Salmonella Reference Unit for confirmation of identification, serotyping and phage typing [19, 20].
All stool samples were also sent to the Health Protection Agency London Regional Laboratory based at King's College Hospital for norovirus testing. This was performed using an in-house polymerase chain reaction (PCR) assay.
Symptomatic staff and all kitchen staff were asked to provide stool samples via their general practitioner.
Environmental investigation
Environmental health officers inspected the prison kitchen on 18, 21 and 22 September to assess the food-safety management system with regard to food storage, preparation and cooking, and to verify the procedures for hazard analysis and critical control point (HACCP) plan. On 18 September five environmental swabs were collected from kitchen areas (including mixing machine and bowl used in the preparation of eggs). No food remained from that served over the period 13–15 September, but food samples of eggs from the same supplier as those used during 13–15 September were collected. The source of the eggs was identified and the supplier traced.
RESULTS
Control methods
Immediate control measures included isolating all symptomatic prisoners in their cells, preventing symptomatic prisoners attending court or having visitors, advising the need for hot water, increased cleaning of cells (including in-cell sanitation) and communal areas, and initiating daily reporting of the number of cases to monitor the progression of the outbreak. The prison Command Suite was opened to assist with coordination of the outbreak. Infection control measures disrupted the movement of prisoners within the prison, transfers in and out of prison, court appearances, visitors, and religious ceremonies for 6 days. Three prisoners were hospitalized.
Epidemiological investigation
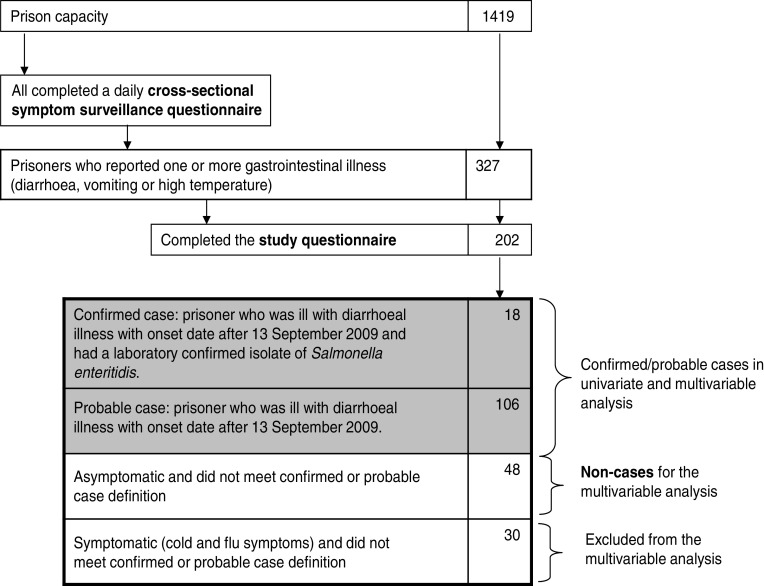
In total, 327 possible and confirmed cases were identified through the prison cross-sectional symptom surveillance questionnaire and stool sampling. Of these, 202 (61·8%) completed the study questionnaire.
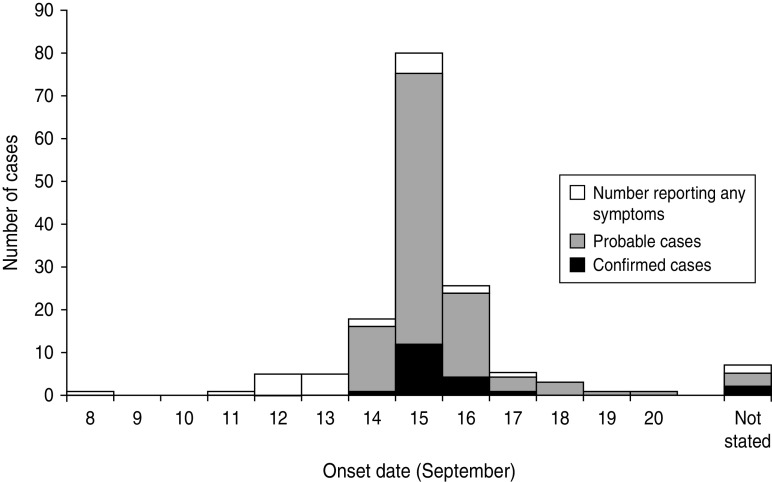
Of the 202 who completed the study questionnaire, 66·8% had diarrhoea (135/202), 62·9% headache (127/202), 61·4% abdominal pain (124/202), 56·9% fever (115/202) and 35·6% vomiting (72/202). A total of 153/202 reported any gastrointestinal symptoms (diarrhoea, vomiting, fever, abdominal pain, headache), and the dates of symptom onset ranged from 11 to 20 September (Fig. 1). The epidemic curve showed a clear peak in cases reporting onset of illness on 15 September.
Fig. 1.
The number of prisoners reporting symptoms (any of diarrhoea, vomiting, fever, abdominal pain, headache) in the study questionnaire by date of onset (n=153/202).
A total of 124 cases (18 confirmed, 106 probable) were identified (Fig. 2). Confirmed or probable cases were found in all prison wings, with an estimated attack rate ranging from 2·8% to 29·4%. Respondents were aged 21–80 years (median age 37 years). No secondary cases were identified.
Fig. 2.
Flow chart showing the method used to collect information on probable and confirmed cases in a Salmonella outbreak in a London prison, 2009.
Five probable prisoner cases reported they worked in the kitchen, three of whom prepared food. Among these three food handlers symptom onset dates were 15 or 16 September.
Cohort study
The epidemic curve suggested a point-source outbreak with likely exposure between 12 and 14 September based on the usual incubation period of Salmonella infection (12–72 h). In the univariate analysis several menu items served over this period were found to be associated with a higher risk of diarrhoeal illness at the 5% level (Table 1). The greatest risk of diarrhoeal illness was in those who consumed egg cress rolls [risk ratio (RR) 25·73, 95% CI 15·46–42·83, P<0·001]. Eighty-one percent (108/124) of all confirmed or probable cases re ported they had consumed the egg cress rolls. Other menu items that suggested an increased risk of diarrhoeal illness included a number of vegetarian choices, e.g. vegetarian flan served on 12 September (RR 5·16, 95% CI 3·56–7·48) and vegetarian nuggets on 13 September (RR 6·59, 95% CI 4·71, 9·22) (Table 1).
Table 1.
Food specific attack rates, risk ratios and 95% confidence intervals for food portions distributed across the prison according to date (cohort study)
| Food item and date served | Ate the food item | Did not eat the food item | RR | (95% CI) | P value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Ill | Total | AR | Ill | Total | AR | ||||
| Lunch, 12 Sept. | |||||||||
| Asian lamb | 22 | 241 | 0·09 | 102 | 1178 | 0·09 | 1·05 | (0·68–1·64) | 0·814 |
| Turkey lasagne | 30 | 247 | 0·12 | 94 | 1172 | 0·08 | 1·51 | (1·03–2·23) | 0·036 |
| Soya & chick pea casserole | 22 | 64 | 0·34 | 102 | 1355 | 0·08 | 4·57 | (3·10–6·92) | <0·001 |
| Vegetable flan | 23 | 60 | 0·38 | 101 | 1359 | 0·07 | 5·16 | (3·56–7·48) | <0·001 |
| Ham pasta | 38 | 142 | 0·27 | 86 | 1277 | 0·07 | 3·97 | (2·83–5·58) | <0·001 |
| Chicken leg | 52 | 470 | 0·11 | 72 | 949 | 0·08 | 1·46 | (1·04–2·05) | 0·029 |
| Turkey roll | 45 | 195 | 0·23 | 79 | 1224 | 0·06 | 3·57 | (2·56–4·99) | <0·001 |
| Fresh fruit | 43 | 338 | 0·13 | 81 | 1081 | 0·07 | 1·70 | (1·20–2·40) | 0·003 |
| Cake | 63 | 1057 | 0·06 | 61 | 362 | 0·17 | 0·35 | (0·25–0·49) | <0·001 |
| Dinner, 12 Sept. | |||||||||
| Beefburger | 49 | 549 | 0·09 | 75 | 886 | 0·08 | 1·05 | (0·75–1·49) | 0·763 |
| Beef chili | 27 | 241 | 0·11 | 97 | 1194 | 0·08 | 1·38 | (0·92–2·06) | 0·118 |
| Vegetarian sausage | 21 | 84 | 0·25 | 103 | 1351 | 0·08 | 3·27 | (2·17–4·96) | <0·001 |
| Meat ravioli | 27 | 91 | 0·30 | 97 | 1344 | 0·07 | 4·11 | (2·84–5·95) | <0·001 |
| Sausage, bacon, egg flan | 46 | 328 | 0·14 | 78 | 1107 | 0·07 | 1·99 | (1·41–2·80) | <0·001 |
| Sardine salad | 37 | 142 | 0·26 | 87 | 1293 | 0·07 | 3·87 | (2·75–5·46) | <0·001 |
| Fresh fruit | 41 | 346 | 0·12 | 83 | 1189 | 0·07 | 1·70 | (1·19–2·42) | 0·005 |
| Cake | 61 | 1019 | 0·06 | 63 | 416 | 0·15 | 0·40 | (0·29–0·56) | 0·003 |
| Lunch, 13 Sept. | |||||||||
| Curried goat | 27 | 284 | 0·10 | 97 | 1155 | 0·08 | 1·13 | (0·75–1·70) | 0·49 |
| Lamb pie | 24 | 85 | 0·28 | 100 | 1354 | 0·07 | 3·82 | (2·60–5·63) | <0·001 |
| Spiced vegetables | 20 | 64 | 0·31 | 104 | 1375 | 0·08 | 4·13 | (2·75–6·21) | <0·001 |
| Poached fish | 29 | 90 | 0·32 | 95 | 1349 | 0·07 | 4·58 | (3·20–6·53) | <0·001 |
| Roast chicken | 35 | 413 | 0·08 | 89 | 1026 | 0·09 | 0·98 | (0·67–1·42) | 0·903 |
| Beef & Yorkshire pudding | 75 | 503 | 0·15 | 49 | 936 | 0·05 | 2·85 | (2·02–4·01) | <0·001 |
| Fresh fruit | 32 | 262 | 0·12 | 92 | 1177 | 0·08 | 1·56 | (1·07–2·28) | 0·021 |
| Ice cream | 90 | 265 | 0·34 | 34 | 1133 | 0·03 | 0·71 | (0·49–1·04) | 0·078 |
| Dinner, 13 Sept. | |||||||||
| Cheese and onion | 34 | 238 | 0·14 | 90 | 1158 | 0·08 | 1·84 | (1·27–2·66) | 0·001 |
| Cheese salad | 37 | 219 | 0·17 | 87 | 1177 | 0·07 | 2·29 | (1·60–3·27) | <0·001 |
| Chicken pasta salad | 52 | 519 | 0·10 | 72 | 877 | 0·08 | 1·22 | (0·87–1·71) | 0·251 |
| Mackerel salad | 35 | 252 | 0·14 | 89 | 1144 | 0·08 | 1·79 | (1·24–2·58) | 0·002 |
| Vegetarian nuggets | 26 | 54 | 0·48 | 98 | 1342 | 0·07 | 6·59 | (4·71–9·22) | <0·001 |
| Beef bredie (no salad) | 27 | 114 | 0·24 | 97 | 1282 | 0·08 | 3·13 | (2·14–4·58) | <0·001 |
| Lunch, 14 Sept. | |||||||||
| Korean sesame chicken | 25 | 611 | 0·04 | 99 | 847 | 0·12 | 0·35 | (0·23–0·54) | <0·001 |
| Greek moussaka | 24 | 144 | 0·17 | 100 | 1314 | 0·08 | 2·19 | (1·45–3·30) | <0·001 |
| Mushroom pasta | 23 | 95 | 0·24 | 101 | 1363 | 0·07 | 3·27 | (2·19–4·89) | <0·001 |
| Potato curry | 22 | 64 | 0·34 | 102 | 1394 | 0·07 | 4·70 | (3·19–6·92) | <0·001 |
| Bulgarian pork stew | 22 | 97 | 0·23 | 102 | 1361 | 0·07 | 3·03 | (2·00–4·57) | <0·001 |
| Meat pie | 21 | 144 | 0·15 | 103 | 1314 | 0·08 | 1·86 | (1·20–2·88) | 0·004 |
| Egg cress roll | 108 | 303 | 0·36 | 16 | 1155 | 0·01 | 25·73 | (15·46–42·83) | <0·001 |
| Fresh fruit | 42 | 369 | 0·11 | 82 | 1089 | 0·08 | 1·51 | (1·06–2·15) | 0·022 |
| Cake | 64 | 1053 | 0·06 | 60 | 405 | 0·15 | 0·42 | (0·29–0·57) | <0·001 |
| Dinner, 14 Sept. | |||||||||
| Chicken burger | 63 | 637 | 0·10 | 61 | 839 | 0·07 | 1·36 | (0·97–1·90) | 0·073 |
| Greek beef stew | 24 | 194 | 0·12 | 100 | 1282 | 0·08 | 1·59 | (1·04–2·41) | 0·031 |
| Curried chickpea | 22 | 81 | 0·27 | 102 | 1395 | 0·07 | 3·71 | (2·48–5·56) | <0·001 |
| Fish | 34 | 219 | 0·16 | 90 | 1257 | 0·07 | 2·17 | (1·50–3·13) | <0·001 |
| Steak kidney pie | 36 | 201 | 0·18 | 88 | 1275 | 0·07 | 2·59 | (1·81–3·71) | <0·001 |
| Chicken salad | 32 | 92 | 0·35 | 144 | 1332 | 0·11 | 3·22 | (2·24–4·62) | <0·001 |
| Fresh fruit | 38 | 292 | 0·13 | 86 | 1184 | 0·07 | 1·79 | (1·25–2·57) | 0·001 |
| Dessert | 65 | 1024 | 0·06 | 59 | 452 | 0·13 | 0·49 | (0·35–0·68) | <0·001 |
AR, Attack rate; RR, risk ratio, CI, confidence interval.
Case/non-case analysis
In a case/non-case analysis we compared the same 124 cases to 48 non-cases who had provided individual food histories through the questionnaires distributed to prisoners (Fig. 2). Results from this analysis showed that after controlling for possible confounding, the egg cress rolls served for lunch on 14 September remained the only variable of high significance (adjusted odds ratio 41·10, 95% CI 10·28–249·74, P<0·001) (Table 2).
Table 2.
Multivariable case/non-case exact logistic regression analysis (N=172)
| Food item and date served | aOR | (95% CI) | P value |
|---|---|---|---|
| Milk (breakfast, 12 Sept.) | 2·80 | (0·11–35·36) | 0·723 |
| Ham pasta (lunch, 12 Sept.) | 10·94* | (1·10–∞) | 0·040 |
| Meat ravioli (dinner, 12 Sept.) | 3·76* | (0·38–∞) | 0·274 |
| Milk (breakfast, 13 Sept.) | 1·90 | (0·17–47·60) | 0·972 |
| Mackerel salad (dinner, 13 Sept.) | 2·66* | (0·26–∞) | 0·438 |
| Drink (dinner, 13 Sept.) | 1·62 | (0·23–10·30) | 0·835 |
| Egg cress roll (lunch, 14 Sept.) | 41·1 | (10·28–249·74) | <0·001 |
| Turkey roll (lunch, 15 Sept.) | 4·43 | (0·21–380·02) | 0·596 |
aOR, Adjusted odds ratio; CI, confidence interval.
Median unbiased estimate [26].
Microbiological investigation
On 18 September, preliminary results indicated 8/10 stool samples were positive for SE and 8/9 stool samples were negative for norovirus.
In total, SE was isolated from 33/38 stool specimens tested (32 prisoners and one member of staff). Phage typing was completed on 29 isolates, all of which were found to be phage type 4 (PT4). No pathogens were isolated from the food or environmental samples collected.
Environmental investigation
The environmental investigation revealed the kitchen staff prepared batches of shelled eggs by cracking them into large baking trays (the number of eggs per tray varied from 30 to 60) and cooking the mixture in a steam oven with inadequate temperature and time controls. The contents of all the trays were then mixed together and stored overnight in a refrigerator before being prepared as egg cress rolls. The prison HACCP stated all raw eggs should be hard-boiled or fully fried; therefore the pooled method for cooking eggs was not in line with the prison's own approved HACCP plan. The Environmental Health Officers reported the eggs used were Lion branded and sourced from a large UK catering supplier.
DISCUSSION
The results from the epidemiological, microbiological and environmental investigations demonstrated this large foodborne outbreak in a prison was most likely caused by consumption of egg cress rolls contaminated by SE PT4. SE PT4 is the most commonly reported Salmonella as documented by the Health Protection Agency [3]. In 2009, a further 11 foodborne outbreaks were reported in UK prison settings, seven caused by norovirus, one by Clostridium perfringens and one by Cryptosporidium [21].
This outbreak occurred in one of the largest prisons in Europe. Lessons were identified in the management and control of gastrointestinal disease outbreaks in a prison setting and considerations in the design of future analytical studies of outbreak investigations in prisons. These included the need to monitor sickness in staff and prisoners for early identification of outbreaks, good communication in outbreak management, regular audits to ensure local HACCP plans are fit for purpose, and to consider using routinely available data to investigate possible sources of the outbreak [22].
Management and control
The outbreak had significant implications for the management within the prison and on the wider justice system. Because of the potential person-to-person spread, control measures necessitated the isolation of symptomatic prisoners and, as a direct result, their cellmates. This meant access to showers and telephones for these prisoners were limited. The inability to speak to relatives raised concerns among family members and caused unrest among prisoners. Control measures also halted court attendances and the transfer of prisoners in and out of the prison causing an impact on the wider justice system. Limiting the movement of symptomatic prisoners and staff is the most commonly reported method used in the management of enteric outbreaks in prison settings [12].
At the time of the outbreak, there was no published national guidance document for the management and control of gastrointestinal outbreaks in prison settings. In January 2010, the multi-agency contingency plan for the management of outbreaks of communicable diseases or other health protection incidents in prisons in England and Wales was amended to include specific guidance on the management of gastrointestinal outbreaks in prisons and other custodial settings [23]. Specific learning from this outbreak which informed the national guidance included a log sheet to collate information on symptoms among prisoners and staff; the importance of accurate and consistent information for prisoners, employees, relatives and other internal and external agencies [22].
Analytical study
The cross-sectional symptom surveillance questionnaire (developed for patient management rather than as an epidemiological tool) enabled identification of the total number of prisoners who reported feeling unwell each day rather than the number of new cases arising. Prisoners may have been less likely to report symptoms as the outbreak investigation progressed and they became aware of the restrictive control measures imposed on those who were symptomatic. Therefore we cautiously interpreted the epidemic curve for the outbreak to be strongly suggestive of a point source. We wished to investigate the outbreak in a way that minimized disruption at the prison where staff were already under considerable pressure managing the outbreak. We took into consideration resource constraints, availability of routine data sources and the transient prison population. A cohort study of all prisoners, or within one wing (if representative) would have been possible, but this would have had significant resource implications in a prison of this size (over 1400 prisoners). A case-cohort study was also considered, a design where controls are randomly selected from the entire cohort thus removing the need to include all prisoners in the study. An efficient approach taken was to use the available individual prisoner reported food histories together with information relating to food items prepared and distributed across the site each day. Limitations with this approach include possible inaccuracies in the data provided by the kitchen, which may have under- or overestimated the number of portions of food items available overall. There are also limitations at an individual level as reported food consumption by cases may have been inaccurate and cases may have eaten more than one portion of a given food. This would have resulted in fewer portions being available for other prisoners. If this had occurred we would have overestimated the exposure among non-ill prisoners and potentially reduced our measure of association towards the null. There were anecdotal reports of prisoners taking the egg cress rolls to their cells and eating them later but we do not know if this was by cases or those who were not ill. These various limitations may have resulted in misclassification of exposure in controls. Misclassification may also have occurred for cases as the exposure histories provided in their questionnaires did not always match what they had indicated on their weekly menu choice. Each prisoner completed a weekly prospective menu choice form and the information was used by the prison kitchen to determine the quantity of each food item to prepare each week. There was poor agreement between the food histories as reported by cases in the study questionnaires and their menu choice selections. There is a possibility that absence of language skills in English or reduced literacy may have led to a low response rate which would affect the power of the study.
Without individual-level data for the population at risk it was not possible to complete a multivariable analysis to adjust for confounding in a conventional way. Our second analytical study in which confirmed and probable cases were compared to non-cases enabled adjustment for confounding. This second study strongly supported the conclusions from the first. We believe that in spite of the various limitations to our study we were able to identify a specific food item with a much higher risk of associated illness than any other, served on 14 September 2009, a date that from the epidemic curve looked very likely to have been the day of exposure. Furthermore more than 80% of cases could be accounted for by this exposure.
We believe the epidemiological approach is novel and potentially useful in other residential settings. It yielded a good result but did not require as many resources compared to a full cohort study.
Environmental
Environmental investigations identified a pooled method for cooking raw eggs with inadequate temperature and time controls. This method of pooling of raw eggs would have meant that just one or two eggs among several hundred would be sufficient to contaminate the mixture and result in the outbreak if not cooked sufficiently. The pooled method of cooking eggs was also identified in a Salmonella outbreak in a prison in Georgia, USA, which affected 113/640 inmates [14]. Our investigation identified a need for more training, supervision and auditing of individual prison catering managers to ensure the HACCP requirement in the Prison Service Order is correctly implemented.
The eggs used by the prison kitchen were British Lion Quality branded from a large UK catering supplier. Lion Quality eggs means the supplier must adhere to a strict code of practice to reduce/eliminate the risk of contamination. Specific measures include vaccinating hens against SE, routine Salmonella testing, hygiene monitoring, time and temperature control for storage and transportation of eggs, and satisfaction of independent audits every 18 months [24]. Despite these control methods it is not possible to guarantee eggs will be free of Salmonella and recent surveys estimate the prevalence of Salmonella in UK-sourced eggs is 0·38% (95% CI 0·14-0·82%) [25].
In conclusion, this outbreak provided a unique opportunity to perform analytical, microbiological and environmental investigations into the cause of a foodborne outbreak within a prison setting. Recommendations from the investigation have been considered at a national level [25] for the management of future outbreaks in similar settings.
ACKNOWLEDGEMENTS
The authors acknowledge the contribution made by the multi-disciplinary team during the management, control and investigation of this outbreak. Including staff at South West London Health Protection Unit, Her Majesty's Prison Wandsworth, Wandsworth Environmental Health Office, Health Protection Agency London, Health Protection Agency Centre for Infections, Department of Health, Ministry of Justice, St George's Hospital London, King's Hospital London and NHS Wandsworth. The timely resolution of the outbreak would not have been possible without the collaboration of all involved. The authors also thank all the inmates for their help and cooperation during the outbreak.
APPENDIX. Members of the Outbreak Control Team
Ruth Ruggles, Yvonne Young, Alisha Davies, Laura Shallcross, Emma Dapaah, Emma Leegood, Brian Thackeray, Louise Spencer, Keith Burgess, Chris Woods, Gordon King, Mary Piper, Velean Gilfillian, Paddy Kirwan, Peter Reddell, Helen Clark, Emily Chan, Katherine Lewis, Sheila Platt, Chris Lane, Paul Shaw, Aodhan Breathnach, Helen Maguire, Neville Verlander.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Health Protection Agency. Foodborne outbreaks reported to the Health Protection Agency, England and Wales, 1992–2010 (http://www.hpa.org.uk/web/HPAweb&Page&HPAwebAutoListName/Page/1274087663703). Accessed 18 November 2011.
- 2.Health Protection Agency. Salmonella by serotype reported to the Health Protection Agency Centre for Infections. England and Wales, 2000–2010 (http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Salmonella/EpidemiologicalData/salmDataHuman/). Accessed 18 November 2011.
- 3.Health Protection Agency. Salmonella Enteritidis phage types (PT) in humans reported to the Health Protection Agency Centre for Infections. England and Wales, 2000–2010 (http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Salmonella/EpidemiologicalData/salmDataHumanSe/). Accessed 18 November 2011.
- 4.Palmer S, et al. The role of outbreaks in developing food safety policy: population based surveillance of salmonella outbreaks in Wales 1986-98. Epidemiology and Infection 2000; 125: 467–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan O, et al. Outbreak of Salmonella Enteritidis phage type 13a: case-control investigation in Hertsmere, United Kingdom. Eurosurveillance 2007; 12: E9–10. [DOI] [PubMed] [Google Scholar]
- 6.Holtby I, et al. Two separate outbreaks of Salmonella Enteritidis phage type 14b food poisoning linked to the consumption of the same type of frozen food. Public Health 2006; 120: 817–823. [DOI] [PubMed] [Google Scholar]
- 7.Ejidokun OO, et al. Four linked outbreaks of Salmonella Enteritidis phage type 4 infection-the continuing egg threat. Communicable Disease and Public Health. 2000; 3: 95–100. [PubMed] [Google Scholar]
- 8.Anaraki S, Giraudon I, Cathcart S. Large outbreak of Salmonella Enteritidis in North East London. Eurosurveillance 2005; 17: E050317.2. [DOI] [PubMed] [Google Scholar]
- 9.Badrinath P, et al. An outbreak of Salmonella Enteritidis phage type 34a infection associated with a Chinese restaurant in Suffolk, United Kingdom. BMC Public Health 2004; 1: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowden J, et al. A national outbreak of infection with Salmonella Enteritidis phage types 5c and 6a associated with Chinese food businesses in Scotland, summer 2000. Epidemiology and Infection 2003; 130: 387–393. [PMC free article] [PubMed] [Google Scholar]
- 11.Gillespie IA, et al. Foodborne general outbreaks of Salmonella Enteritidis phage type 4 infection, England and Wales, 1992–2002: where are the risks? Epidemiology and Infection 2005; 133: 795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greig JD, et al. Review of enteric outbreaks in prisons: effective infection control interventions. Public Health 2011; 125: 222–228. [DOI] [PubMed] [Google Scholar]
- 13.Kimura T, et al. Enterotoxigenic Escherichia coli O6:H16 food poisoning outbreak in prisons. Japanese Journal of Infectious Diseases 2006; 59: 410–411. [PubMed] [Google Scholar]
- 14.Cieslak PR, et al. Preventable disease in correctional facilities: desmoteric foodborne outbreaks in the United States, 1974-1991. Archives of Internal Medicine 1996; 156: 1883–1888. [DOI] [PubMed] [Google Scholar]
- 15.Parikh AI, et al. Clostridium perfringens outbreak at a juvenile detention facility linked to a Thanksgiving holiday meal. Western Journal of Medicine 1997; 166: 417–419. [PMC free article] [PubMed] [Google Scholar]
- 16.Centres for Disease Control and Prevention. Outbreaks of Salmonella serotype Enteritidis infection associated with eating shell eggs – United States, 1999–2001. Journal of the American Medical Association 2003; 289: 540–541. [PubMed] [Google Scholar]
- 17.Directgov. Types of prisons and security categories (http://www.direct.gov.uk/en/CrimeJusticeAndTheLaw/Sentencingprisonandprobation/Goingtoprison/DG_196234). Accessed 26 April 2012.
- 18.Health Protection Agency. (http://www.hpa.org.uk/ProductsServices/InfectiousDiseases/QualityAssurance/UKStandardsForMicrobiologyInvestigations/). Accessed 3 May 2012.
- 19.Bale JA, et al. Salmonella identification: serotypes and antigenic formula. Kauffmann-White Scheme, 2007. Health Protection Agency, London, 2007. [Google Scholar]
- 20.Ward LR, et al. A phage-typing scheme for Salmonella enteritidis. Epidemiology and Infection 1987; 99: 291–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health Protection Agency. Health protection in prisons: a report to Offender Health from the Health Protection Agency, Annual Report 2009–2010. Health Protection Agency, London, 2011. [Google Scholar]
- 22.Health Protection Agency. Report on the food poisoning incident at Her Majesty's Prison Wandsworth in September 2009 (http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1267552384421). Accessed 26 April 2012.
- 23.Health Protection Agency. Appendix 9. Guidance for the management of gastrointestinal (G.I.) infection outbreaks in prisons and other custodial settings. In: Multi-Agency Contingency Plan for the Management of Outbreaks of Communicable Diseases or Other Health Protection Incidents in Prisons in England & Wales. Health Protection Agency, Offender Health (Department of Health), HM Prison Service. London, 2010. [Google Scholar]
- 24.The British Egg Information Service. Summary of Lion Quality Code of Practice (http://www.lioneggs.co.uk/files/lioneggs.co.uk/pdfs/LionCodeSummary.pdf). Accessed 12 February 2012.
- 25.Advisory Committee on the Microbiological Safety of Food. Minutes of Advisory Committee on the Microbiological Safety of Food Meeting dated 27 September 2007 (http://acmsf.food.gov.uk/acmsfmeets/acmsf2007/acmsfmeet070927/acmsfmin270907). Accessed 18 November 2011.
- 26.Hirji KF, et al. Median unbiased estimation for binary data. American Statistician 1989; 43: 7–11. [Google Scholar]