SUMMARY
Hypermucoviscous (HV) isolates of Klebsiella pneumoniae have been linked to virulence potential in experimental infections. We examined 33 isolates of K. pneumoniae from patients with bacteraemia for the HV phenotype on agar culture, and determined their virulence potential by screening for capsular (K) serotype by polymerase chain reaction and the presence of seven virulence factor genes. Fourteen (42·4%) isolates expressed the HV phenotype and 11 of these were serotype K1 or K2; these serotypes were not identified in HV-negative isolates. The genes rmpA, rmpA2, aerobactin, wabG and allS were significantly more frequent in HV than non-HV isolates. Multilocus sequence typing identified 21 sequence types (ST), eight of which were found in HV-positive isolates and the clonal relatedness of isolates of the most frequent types (ST23 and ST11) from different hospitals was confirmed by pulsed-field gel electrophoresis. The HV phenotype was more associated with community-acquired infection with a lower frequency of fatal underlying illness, but with significantly more focal infections, notably liver abscesses. Clinicians should be aware of such clinical impacts of the HV phenotype.
Key words: Hypermucoviscosity, Klebsiella pneumoniae
INTRODUCTION
Klebsiella pneumoniae is responsible for a variety of diseases in humans and animals but the majority of infections are associated with hospitalization. However, serious community infections due to K. pneumoniae can affect previously healthy persons and recently, K. pneumoniae serotype K1 has been identified as a major aetiological agent in liver abscesses, most prominently in Taiwan and Korea [1–4]. Typing of the capsular (K) antigen has been the classical method for characterizing K. pneumoniae strains but it is time-consuming and requires a large number of specific antisera. However, relatively few serotypes, particularly K1 and K2, appear to be associated with invasive strains. The rapid development of molecular methods available for epidemiological purposes, such as multilocus sequence typing (MLST), has given new insights into genotype-virulence relationships in several bacterial species and demonstrated genetic heterogeneity within strains of uniform serotypes [5, 6]. However, there are only a few reports on the clones of K. pneumoniae causing bacteraemia [7].
It has long been recognized that bacterial isolates expressing a mucoid phenotype on agar culture are generally considered to have more virulence, greater lethality, and increased resistance to phagocytes in animal experiments [8]. K. pneumoniae strains often form large mucoid hypermucoviscous colonies (HV phenotype) on agar culture which tend to coalesce with prolonged incubation and form a ‘string’ of growth when picked up on a loop from the agar surface.
The magA gene was reported to be a novel virulence gene related to the HV phenotype in 2004 [9] but was later found to be restricted to serotype K1 and part of the capsular polysaccharide gene cluster for this serotype [10, 11]. RmpA and rmpB genes positively control the mucoid phenotype in of K. pneumoniae [12] and both rmpA and magA are strongly associated with the HV phenotype [13]. This phenotype is now an accepted marker of virulence in clinical strains causing liver abscess and is characterized by serotype K1 and sequence type (ST) 23 [14, 15]. However, the clinical consequences of the HV phenotype in bacteraemia have remained elusive. We therefore investigated the frequency of the HV phenotype in bacteraemic K. pneumoniae isolates and compared their characteristics (virulence genes, serotypes, MLST, antimicrobial resistance, clinical manifestations) with non-HV phenotypes.
METHODS
Bacterial isolates
From June to August 2010, a total of 33 K. pneumoniae isolates were each recovered from individual patients with bacteraemia hospitalized in 13 tertiary-care hospitals located in 10 provinces of Korea: Seoul St Mary's Hospital (n = 6), Yoido St Mary's Hospital (n = 1), Bucheon St Mary's Hospital (n = 1), St Vincent Hospital (n = 5), Uijeongbu St Mary's Hospital (n = 1), Incheon St Mary's Hospital (n = 4), Chung-ang University Yongsan Hospital (n = 2), Chung-ang University Hospital (n = 2), Chungju Medical Center (n = 1), Soonchunhyang University Kumi Hospital (n = 4), Ulsan University Hospital (n = 1), Chosun University Hospital (n = 2), and Yeungnam University Medical Center (n = 3). Medical records of all the patients enrolled in the study were retrospectively reviewed to identify clinical characteristics including the underlying illness, acquisition mode of infection (community vs. hospital), source of bacteraemia, and clinical signs and symptoms.
Case definitions
Community-acquired bacteraemia was defined as a positive blood culture taken on admission or within 48 h of admission [16] and fatal underlying illness was according to the McCabe classification [17]. Patients without a clinically evident source of bacteraemia were considered to have primary bacteraemia. Liver abscess was diagnosed by evidence of an intrahepatic abscess cavity by ultrasonography or computed tomography (CT).
Microbiological tests
K. pneumoniae isolates were sent by the participating hospitals on nutrient agar slants to a central laboratory in Seoul for confirmation of species identity and susceptibility to 15 antimicrobial agents (cephalothin, cefuroxime, cefoxitin, cefotaxime, ceftazidime, cefepime, piperacillin, piperacillin-tazobactam, imipenem, meropenem, amikacin, gentamicin, ciprofloxacin, trimethoprim-sulfamethoxazole, aztreonam) by the Vitek GNI system (bioMérieux Vitek, USA). Extended spectrum β-lactamase (ESBL) production was detected by an inhibitor-potentiated disk diffusion method, as described previously [18]. The isolates were cultured on 5% sheep blood agar plate overnight at 37 °C and classified as HV or non-HV phenotype by the string test performed by two experienced technologists, using a bacterial loop to stretch a string of growth from the bacterial colony. Formation of a mucoviscous string of >5 mm was defined as a positive string test [9].
The presence of genes encoding virulence factors (rmpA, aerobactin, wabG, allS, kfu, mrkD) was determined by polymerase chain reaction (PCR) using primers documented previously [7]. The rmpA2 gene, a homologue of rmpA sharing 80% nucleotide sequence [19], was detected by PCR as described previously [20]. The virulence scores were expressed as the total number of these genes positive in each strain. Capsular serotypes (K1, K2, K20, K54, K57) were determined by multiplex PCR [21]. MLST was performed for all isolates as described by Diancourt et al. [22] and sequence types were assigned by reference to the MLST database (http://www.pasteur.fr/recherche/genopole/PF8/mlst/Kpnemoniae.html). Sequences of alleles or sequence types not registered on the database were submitted to the curator and coded as novel. Pulsed-field gel electrophoresis (PFGE) of XbaI digests of chromosomal DNA was performed on isolates of predominant sequence types [23] and DNA patterns were interpreted according to Tenover et al. [24].
Statistical analysis
Fisher's exact test was used to statistically assess the frequency of microbiological and clinical variables and the Mann–Whitney test (non-parametric) was used to compare strain virulence scores. P value <0·05 was considered to be statistically significant. The statistical software used was SPSS, release version 15.0.1 (SPSS Inc., USA).
RESULTS AND DISCUSSION
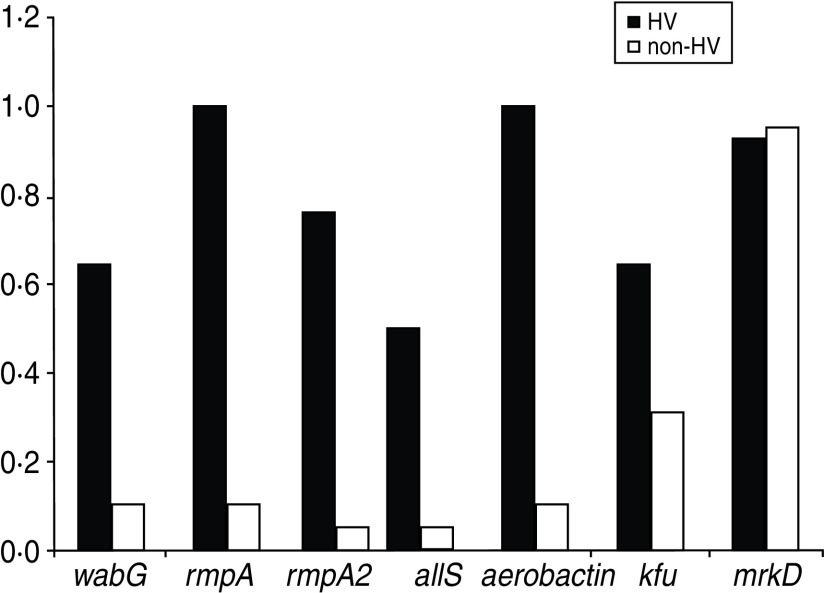
The microbiological characteristics of the 33 isolates are summarized in Table 1 and show that 14 (42·4%) were positive for the HV phenotype by the string test and all formed mucoviscous strings of >10 mm. The mean virulence score for HV-positive strains was 5·5, and for non-HV strains it was 1·6 (P < 0·001) (Fig. 1) and the distribution of virulence genes was markedly different in HV and non-HV strains. Five of the seven genes investigated, (rmpA, rmpA2, aerobactin, wabG, allS) were significantly more frequent in HV strains (100%, 78·6%, 100%, 64·3%, 50%, respectively) than in non-HV strains (5·3%, 5·3%, 10·5%, 10·5%, 5·3%, respectively). It is of note that all HV strains harboured rmpA and aerobactin. rmpA is a positive regulator of extracellular polysaccharide synthesis and its isoform, rmpA2, has also been reported to enhance the colonial mucoidity of various serotypes of K. pneumonia [19]. All isolates harbouring rmpA2 also had the rmpA gene. The aerobactin gene encodes high-affinity iron chelators and both this gene and rmpA have been associated with higher lethality in animal models [16, 25]. This coexistence of rmpA and aerobactin genes in HV strains is in agreement with previous reports that demonstrated the two genes were located simultaneously on a 180-kb plasmid [26]. The kfu gene was also more frequent in the HV phenotype, but this was not statistically significant. The mrkD gene encoding the fimbrial tip adhesin MrkD was detected in all but two isolates (Table 1). In a previous report, the mrkD gene was not detected specifically in clonal complex (CC) 82 with serotype K1 (CC82K1) [7]. In our data, not only the ST82 (CC82) isolate but also the novel clone, ST713, was negative for the mrkD gene.
Table 1.
Microbiological variables of Klebsiella pneumoniae isolates from the 33 patients with bacteraemia
| Isolate number | String test | K type | wabG | rmpA | rmpA2 | allS | aerobactin | kfu | mrkD | ESBL production | ST |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | − | n.a. | − | − | − | − | − | + | + | − | 454 |
| 2 | + | K2 | − | + | + | − | + | − | + | − | 375 |
| 6 | − | n.a. | − | − | − | − | − | + | + | − | 710 |
| 9 | + | K2 | − | + | + | − | + | − | + | − | 86 |
| 12, 38, 115, 184, 195 | − | n.a. | − | − | − | − | − | − | + | + | 11 |
| 17, 18 | − | n.a. | − | − | − | − | − | − | + | − | 36 |
| 24 | − | K54 | + | − | − | − | − | − | + | + | 711 |
| 25 | − | n.a. | − | − | − | − | − | + | + | − | 712 |
| 71 | − | n.a. | − | − | − | − | − | − | − | − | 713 |
| 100, 124, 224, 239, 253, 298, 340 | + | K1 | + | + | + | + | + | + | + | − | 23 |
| 117 | − | n.a. | + | − | − | − | − | − | + | − | 20 |
| 194 | − | n.a. | − | − | − | − | − | − | + | + | 20 |
| 146 | − | n.a. | − | − | − | − | − | + | + | − | 662 |
| 185 | − | n.a. | − | − | − | − | − | − | + | − | 70 |
| 219 | + | n.a. | − | + | − | − | + | − | + | − | 505 |
| 281 | + | K54 | + | + | + | − | + | − | + | − | 714 |
| 294 | + | K57 | − | + | + | − | + | − | + | − | 218 |
| 295 | + | K1 | + | + | − | − | + | + | − | − | 82 |
| 300 | − | n.a. | − | − | − | + | + | + | + | + | 270 |
| 315 | − | K20 | − | + | + | − | + | − | + | − | 268 |
| 336 | + | K2 | − | + | − | − | + | + | + | − | 380 |
| 730 | − | n.a. | − | − | − | − | − | + | + | + | 655 |
ESBL, Extended spectrum β-lactamase; ST, sequence type; n.a., not available, unidentified serotype.
Fig. 1.
Mean number of each virulence gene carried in hypermucoviscous (HV) and non-HV strains. HV strains carried significantly more virulence genes than non-HV strains (5·5 vs. 1·6, P < 0·001).
All but one of the 14 HV strains were grouped into specific serotypes by the multiplex PCR. K1 was the most prevalent (n = 8), followed by K2 (n = 3), K54 (n = 1) and K57 (n = 1). By contrast, only two out of 19 non-HV strains were serogrouped by PCR (K20, K54). We cannot exclude the possibility that this might be due to the fact that the PCR lacks specific primers for types K4 and K5, which are also highly virulent in experimental infection in mice and are often associated with severe infections in humans and animals [27, 28].
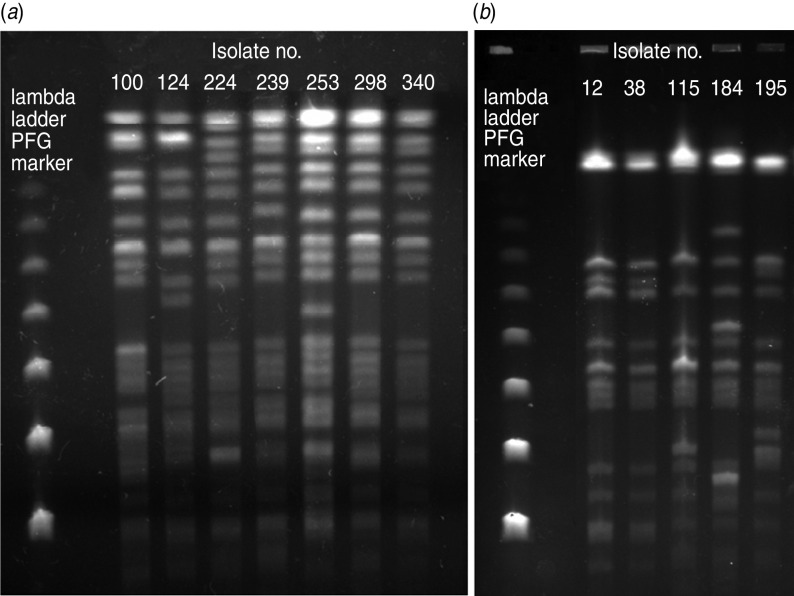
Molecular genotyping by MLST identified 21 different sequence types, including six novel alleles and seven unique sequence types (ST655, ST662, ST710, ST711, ST712, ST713, ST714; Table 1). There were two, three, and two different sequence types in K1, K2 and K54 serotypes, respectively and eight sequence types in HV strains, of which ST23 was the most frequent (7/14). Of the 13 different sequence types in non-HV strains, ST11 was the most frequent (5/19). PFGE revealed that the seven ST23 isolates from six different hospitals were closely related and of the five ST11 isolates from four different hospitals, four were closely related, and one was possibly related (Fig. 2).
Fig. 2.
Pulsed-field gel electrophoresis patterns of (a) seven ST23 and (b) five ST11 isolates. Both show clonal relationships.
All the K1 and K2 strains showed the HV phenotype. Interestingly, however, there was a difference in the distribution of virulence genes between K1 and K2 serotypes; whereas the prevalence of wabG and allS in K1 isolates was very high (100% and 87·5%, respectively), none of the K2 isolates harboured them. In addition, the kfu gene, which is known to be associated with the development of abscesses in the liver and in the brain of mice [29], was found in all of K1 isolates but in only one K2 isolate (ST380). This finding is in line with a previous report, where allS and kfu genes were present in all K1 strains tested but not in K2 strains [29]. Considering the fact that K1 strains are emerging as a pathogen capable of causing catastrophic septic ocular or central nervous system complications from liver abscesses [30], further experiments are required to validate whether the presence of additional wabG, allS and kfu genes in K1 isolates contributes to invasive complications. Interestingly, the allS gene, included in a 22-kb chromosomal region and known to be present only in the K1 serotype [29], was found in one non-HV isolate (ST270) of an unidentified serotype.
Of particular interest, in the three cases where the source of bacteraemia was a liver abscess, one case was an ST380 isolate of the K2 serotype harbouring the kfu gene. To the best of our knowledge, this is the first report of an ST380 isolate of serotype K2 causing a pyogenic liver abscess and subsequently, bacteraemia. Although K2 strains have not received as much attention as K1 strains, severe and fatal infections due to two unrelated clones (ST86 and ST380) of the K2 serotype were reported recently in France [31]. In our study, about 10% of the bacteraemic isolates had the K2 serotype, and their sequence types were ST86, ST375 and ST380. Whether these clones of K2 strains will prove to be as dominant as ST23 in the K1 strains remains to be determined.
None of the HV or non-HV strains was resistant to imipenem or meropenem. HV strains showed a lower resistance rate to all the other antimicrobial agents than non-HV strains. All HV strains were susceptible to piperacillin-tazobactam and amikacin. But in non-HV strains, the resistance rates to these antimicrobials were 31% and 21%, respectively. Of the HV strains 7% were resistant to gentamicin and ciprofloxacin and 14% to trimethoprim-sulfamethoxazole compared to non-HV strains where resistance rates to these three agents were 31%, 47% and 57%, respectively.
None of the HV strains produced ESBLs but in non-HV strains, the ESBL production rate was higher (47·4%) than that (30%) of Korean isolates of K. pneumoniae from various sources in a previous study [32]. This might be due to the predominance of ST11 in the non-HV strains, which is a dominant clone in ESBL-producing K. pneumoniae in Korea [33]. A plausible explanation for this negative association between the HV phenotype and ESBL production might be that the virulence genes were lost during the bacterial acquisition of antibiotic resistance, as it can induce phenotypic and genetic changes as a part of reduced biological fitness [34]. Or as many virulent isolates harbour a large (∼200 kb) plasmid [35], stable coexistence of another plasmid might be difficult. In addition, ST11 is a single-locus variant of ST258, which has been reported worldwide, including Korea, as the predominant clone of Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae [36–38] and therefore, it is worrisome that ST11 predominates in bacteraemic isolates.
The clinical characteristics of the patients infected by isolates with or without HV phenotype are compared in Table 2. The frequency of fatal underlying illness was significantly lower in patients infected with the HV phenotype compared to the non-HV phenotype (14·3% vs. 68·4%, P = 0·004). Similarly, the presence of focal infections was significantly more frequent in patients with the HV phenotype (78·6% vs. 26·3%, P = 0·005). Although not statistically significant, mortality was also higher in the population infected with the HV strains (28·6% vs. 10·5%, P = 0·363). Poor immune status, fatal underlying diseases of the patients infected by non-HV strains, and higher antimicrobial resistance of these strains might have influenced the risk of mortality in this group of patients.
Table 2.
Clinical chracteristics of 33 bacteraemic patients by Klebsiella pneumoniae with or without the hypermucoviscosity (HV) phenotype
| Variables | HV-positive (n = 14) | HV-negative (n = 19) | P value |
|---|---|---|---|
| Fatal underlying illness | 2/14 (14·3%) | 13/19 (68·4%) | 0·004 |
| Focal infection | 11/14 (78·6%) | 5/19 (26·3%) | 0·005 |
| Urinary tract infection | 4/14 (28·6%) | 1/19 (5·3%) | 0·138 |
| Pneumonia | 4/14 (28·6%) | 3/19 (15·8%) | 0·422 |
| Biliary tract infection | 0/14 (0%) | 1/19 (5·3%) | 0·383 |
| Liver abscess | 3/14 (21·4%) | 0/19 (0%) | 0·067 |
| Mortality by infection | 4/14 (28·6%) | 2/19 (10·5%) | 0·363 |
| Community acquisition | 12/14 (85·7%) | 8/19 (42·1%) | 0·015 |
In summary, about 40% of bacteraemic isolates of K. pneumoniae were demonstrated to be of the HV phenotype. These isolates had a higher virulence gene complement but none harboured ESBL. In contrast to the non-HV strains, most of which were of unidentified serotypes, the majority of HV strains fell into serotypes K1 and K2. The distribution of virulence genes differed between these serotypes. The isolates were in the main genetically diverse but ST23 and ST11 were the most frequent in HV and non-HV isolates, respectively. Clinicians should be aware of the increased virulence of the HV phenotype and efforts should be made to investigate the sources of infection. Finally, considering the high frequency (21·4%) of the K2 serotype in HV strains, surveillance should be extended to this serotype and its associated sequence types to determine whether severe infections due to these strains can be spread in the community.
ACKNOWLEDGEMENTS
This research was supported by a research fund (no. 2011 E4400400) of the Korean Centers for Disease Control and Prevention. We thank Dr Jung of Sungkyunkwan University for kindly donating positive strains of capsular K1 serotype K. pneumoniae.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Brook I, Frazier EH. Microbiology of liver and spleen abscesses. Journal of Medical Microbiology 1998; 47: 1075–1080. [DOI] [PubMed] [Google Scholar]
- 2.Seo TJ, et al. A clinical study on liver abscess for recent 15 years in Gwang, Cjuhonnam province. Korean Journal of Medicine 2005; 68: 26–38. [Google Scholar]
- 3.Chung DR, et al. Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea. Journal of Infection 2007; 54: 578–583. [DOI] [PubMed] [Google Scholar]
- 4.Fung CP, et al. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut 2002; 50: 420–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaureguy F, et al. Phylogenetic and genomic diversity of human bacteremic Escherichia coli strains. BMC Genomics 2008; 26: 560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sukhnanand S, et al. DNA sequence-based subtyping and evolutionary analysis of selected Salmonella enterica serotypes. Journal of Clinical Microbiology 2005; 43: 3688–3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brisse S, et al. Virulent clones of Klebsiella pneumoniae: identification and evolutionary scenario based on genomic and phenotypic characterization. PLoS One 2009; 4: e4982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moses AE, et al. Relative contributions of hyaluronic acid capsule and M protein to virulence in a mucoid strain of the group A Streptococcus. Infection and Immunity 1997; 65: 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang CT, et al. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. Journal of Experimental Medicine 2004; 199: 697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Struve C, et al. Investigation of the putative virulence gene magA in a worldwide collection of 495 Klebsiella isolates: magA is restricted to the gene cluster of Klebsiella pneumoniae capsule serotype K1. Journal of Medical Microbiology 2005; 54: 1111–1113. [DOI] [PubMed] [Google Scholar]
- 11.Yeh KM, et al. MagA is not a specific virulence gene for Klebsiella pneumoniae strains causing liver abscess but is part of the capsular polysaccharide gene cluster of K. pneumoniae serotype K1. Journal of Medical Microbiology 2006; 55: 803–804. [DOI] [PubMed] [Google Scholar]
- 12.Nassif X, et al. Positive control of colanic acid synthesis in Escherichia coli by rmpA and rmpB, two virulence-plasmid genes of Klebsiella pneumoniae. Molecular Microbiology 1989; 3: 1349–1359. [DOI] [PubMed] [Google Scholar]
- 13.Yu WL, et al. Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clinical Infectious Diseases 2006; 15: 1351–1358. [DOI] [PubMed] [Google Scholar]
- 14.Pomakova DK, et al. Clinical and phenotypic differences between classic and hypervirulent Klebsiella pneumoniae: an emerging and under-recognized pathogenic variant. European Journal of Clinical Microbiology & Infectious Diseases. Published online: 15 September 2011. doi: 10.1007/s10096-011-1396-6. [DOI] [PubMed] [Google Scholar]
- 15.Turton JF, et al. Genetically similar isolates of Klebsiella pneumoniae serotype K1 causing liver abscesses in three continents. Journal of Medical Microbiology 2007; 56: 593–597. [DOI] [PubMed] [Google Scholar]
- 16.Yu VL, et al. Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerging Infectious Diseases 2007; 13: 986–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCabe WR, Jackson GG. Gram-negative bacteremia: I. Etiology and ecology. Archives of Internal Medicine 1962; 110: 847–855. [Google Scholar]
- 18.Song W, et al. Detection of extended-spectrum beta-lactamases by using boronic acid as an AmpC beta-lactamase inhibitor in clinical isolates of Klebsiella spp. and Escherichia coli. Journal of Clinical Microbiology 2007; 45: 1180–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wacharotayankun R, et al. Enhancement of extracapsular polysaccharide synthesis in Klebsiella pneumoniae by RmpA2, which shows homology to NtrC and FixJ. Infection and Immunity 1993; 61: 3164–3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee CH, et al. Hypermucoviscosity associated with Klebsiella pneumoniae-mediated invasive syndrome: a prospective cross-sectional study in Taiwan. International Journal of Infectious Diseases 2010; 14: e688–692. [DOI] [PubMed] [Google Scholar]
- 21.Lin WH, et al. Clinical and microbiologic characteristics of Klebsiella pneumoniae isolates causing community-acquired urinary tract infections. Infection 2010; 38: 459–464. [DOI] [PubMed] [Google Scholar]
- 22.Diancourt L, et al. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. Journal of Clinical Microbiology 2005; 43: 4178–4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Böhm H, et al. DNA fingerprinting of Escherichia coli O157: H7 strains by pulsed-field gel electrophoresis. Journal of Clinical Microbiology 1992; 30: 2169–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tenover FC, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. Journal of Clinical Microbiology 1995; 33: 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nassif X, et al. Correlation of the virulence of Klebsiella pneumoniae K1 and K2 with the presence of a plasmid encoding aerobactin. Infection and Immunity 1986; 54: 603–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nassif X, et al. Mucoid phenotype of Klebsiella pneumoniae is a plasmid-encoded virulence factor. Infection and Immunity 1989; 57: 546–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Simoons-Smit AM, et al. Virulence of Klebsiella strains in experimentally induced skin lesions in the mouse. Journal of Medical Microbiology 1984; 17: 67–77. [DOI] [PubMed] [Google Scholar]
- 28.Mizuta LG, et al. Virulence for mice of Klebsiella strains belonging to the O1 group: relationship to their capsular (K) types. Infection and Immunity 1983; 40: 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu WL, et al. Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/K2 serotypes. Diagnostic Microbiology and Infectious Disease 2008; 62: 1–6. [DOI] [PubMed] [Google Scholar]
- 30.Fang CT, et al. Klebsiella pneumonia genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clincal Infectious Diseases 2007; 45: 284–293. [DOI] [PubMed] [Google Scholar]
- 31.Decré D, et al. Emerging severe and fatal infections due to Klebsiella pneumoniae in two university hospitals in France. Journal of Clinical Microbiology 2011; 49: 3012–3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeong SH, et al. Molecular characterization of extended-spectrum beta-lactamases produced by clinical isolates of Klebsiella pneumoniae and Escherichia coli from a Korean nationwide survey. Journal of Clinical Microbiology 2004; 42: 2902–2906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ko KS, et al. Predominance of an ST11 extended-spectrum beta-lactamase producing Klebsiella pneumoniae clone causing bacteraemia and urinary tract infections in Korea. Journal of Medical Microbiology 2010; 59: 822–828. [DOI] [PubMed] [Google Scholar]
- 34.Kang YS, et al. Trade-off between antibiotic resistance and biological fitness in Acinetobacter sp. strain DR1. Environmental Microbiology 2010; 12: 1304–1318. [DOI] [PubMed] [Google Scholar]
- 35.Tang HL, et al. Correlation between Klebsiella pneumoniae carrying pLVPK-derived loci and abscess formation. European Journal of Clinical Microbiology & Infectious Diseases 2010; 29: 689–698. [DOI] [PubMed] [Google Scholar]
- 36.Kitchel B, et al. Molecular epidemiology of KPC producing Klebsiella pneumoniae isolates in the United States: clonal expansion of multilocus sequence type 258. Antimicrobial Agents and Chemotherapy 2009; 53: 3365–3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rhee JY, et al. KPC-producing extreme drug-resistant Klebsiella pneumoniae isolate from a patient with diabetes mellitus and chronic renal failure on hemodialysis in South Korea. Antimicrobial Agents and Chemotherapy 2010; 54: 2278–2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qi Y, et al. ST11, the dominant clone of KPC-producing Klebsiella pneumoniae in China. Journal of Antimicrobial Chemotherapy 2011; 66: 307–312. [DOI] [PubMed] [Google Scholar]