SUMMARY
In order to identify and assess recent risk factors for sporadic human infections with Salmonella enterica, we conducted a case-control study in Lower Saxony, Germany. The data collection was based on standardized telephone interviews with 1017 cases and 346 controls aged >14 years. Odds ratios were calculated in single-factor and multi-factor analyses for Salmonella cases and two different control groups, i.e. population controls and controls with rotavirus infection. Multi-factor analysis revealed associations between sporadic Salmonella infections for two exposures by both sets of controls: consumption of raw ground pork [adjusted odds ratio (aOR) 2·38, 95% confidence interval (CI) 1·27–4·44] and foreign travel (aOR 2·12, 95% CI 1·00–4·52). Other exposures included consumption of food items containing eggs (aOR 1·43, 95% CI 0·80–2·54), consumption of chicken meat (aOR 1·77, 95% CI 1·26–2·50), outdoor meals/barbecues (aOR 3·96, 95% CI 1·41–11·12) and taking gastric acidity inhibitors (aOR 2·42, 95% CI 1·19–4·92), all were significantly associated with respect to one of the two control groups. The impact of consuming food items containing eggs or chicken meat was lower than expected from the literature. This might be a consequence of Salmonella control programmes as well as increased public awareness of eggs and chicken products being a risk factor for salmonellosis. Efforts to reduce Salmonella infections due to raw pork products should be intensified.
Key words: Diarrhoea, epidemiology, foodborne infections, infectious disease epidemiology, Salmonella enterica
INTRODUCTION
With 31397 reported cases, human salmonellosis was the second most common bacterial human intestinal disease reported in Germany in 2009 [1]. Understanding the source could lead to interventions to reduce the burden of the disease. Only a small proportion of cases are linked to outbreaks (fewer than 20%). Most Salmonella infections are sporadic with the source remaining unknown.
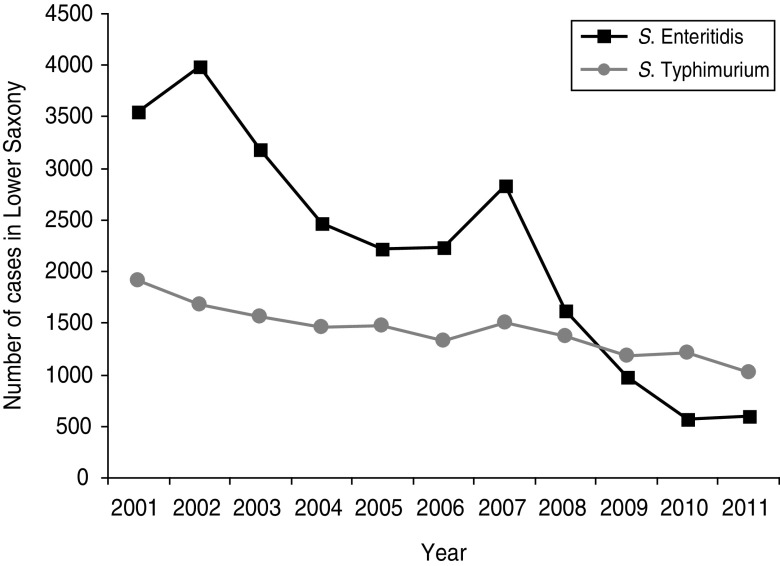
Some attempts have already been made in order to attribute sources of sporadic infections. Since salmonellae are ubiquitous in the animal population these attempts have mainly focused on relating human illness to various animal sources [2]. In the European Union, eggs, egg products and meat (especially poultry and pork) have been identified as sources of foodborne cases of salmonellosis [3]. There is evidence of S. Enteritidis infections being frequently associated with the consumption of products from raw eggs [4], while S. Typhimurium infections are seen to be associated with the consumption of pork products [5]. During the last 10 years the population's awareness of a risk for Salmonella infection from the consumption of products from raw eggs has increased. A Salmonella control programme according to Regulation (EC) No. 2160/2003 has been enforced with the aim of reducing foodborne zoonotic agents in European countries. The European countries have converted the regulation into federal laws. Distinct aims for reducing Salmonella prevalence in poultry farms have been drafted in all European countries. The decreasing number of reported S. Enteritidis infections (Fig. 1) in Germany is in accord with the reduction of S. Enteritidis detection in eggs [6].
Fig. 1.
Annual reported cases of S. Enteritidis and S. Typhimurium from 2001 to 2011 in Lower Saxony, Germany.
Thus, with the intention of deepening the knowledge about risk factors for sporadic salmonellosis, a case-control study was conducted in Lower Saxony. Lower Saxony is a federal state in the north of Germany with a rural composition and a strong agrarian infrastructure of livestock husbandry and food production as important economic sectors. The incidence of reported salmonellosis in Lower Saxony in 2009 was 36·7/100 000 inhabitants. Associations between potential risk factors and Salmonella infections were investigated. The food items focused on were those already known as sources of infection. Contact with animals and hygiene practices were also of interest. Another purpose of the study was to assess the contribution of other factors such as pre-existing conditions or use of pharmaceutical drugs to the risk of acquiring a Salmonella infection.
METHODS
Cases
Within the study, data were collected for three age groups (0–2, 3–14, >14 years). Results shown here are restricted to cases aged >14 years due to the fact that they are homogeneous concerning eating habits and other relevant conditions for Salmonella infections such as animal contact, hygiene practice and immunocompetence. Salmonella case persons (SCP) were selected between June 2008 and May 2010 from all Salmonella cases reported within the German infectious disease notification system according to the Protection against Infection Act in Lower Saxony. Local health departments (LHDs) contacted persons with laboratory-confirmed Salmonella infection and asked them to participate in the study. If a LHD's on-site investigation identified an outbreak, this information was stored in case record form and transferred to the reporting software. In addition, the study interview included a question about known diarrhoea in contact persons. Based on these two sources of information confirmed outbreak cases were excluded from the study.
Controls
In order to account for common biases (e.g. recall bias) two different control groups were considered. Population controls (PopC) were enrolled as a random sample by random digit dialling from the general population of Lower Saxony. The required phone numbers were created according to the Gabler–Häder design [7]. From each successfully contacted household the member with the most recent birthday was chosen for interview, if agreement to participate was received. At least six attempts on different days and at different times were made to contact a single person.
Rotavirus controls (RVC) were selected from persons with notified rotavirus infections, who were not associated with a reported outbreak. Rotavirus cases are notified within the same notification system as Salmonella cases.
The interview
All interviews were conducted by trained interviewers from the Institute of Public Health of Lower Saxony (Niedersächsisches Landesgesundheitsamt, NLGA) or LHDs. The interviews were based on a standardized questionnaire covering information about food items consumed, hygienic aspects of food handling in the kitchen, contact with animals and other activities during the previous 3 days before onset of the disease. For PopC the enquired time period comprised 3 days before the interview. The questionnaire also collected information on other conditions possibly associated with Salmonella infection, e.g. diabetes, immunodeficiency and use of pharmaceutical drugs. The questionnaire was tested in a pre-test of ten interviews and adapted regarding some phrases for easier comprehension over the phone. If the index person was not available the interview was conducted with another household member, who could provide adequate information about the case person.
If no successful contact could be established by the LHD, the reason for nonresponse was recorded according to the following categories:
-
•
case person could not be contacted by phone;
-
•
case person was not available for telephone interview due to language problems or mental state;
-
•
case person did not give consent for study participation.
Ethics approval
The study was exempted from ethics committee approval.
Data management
Microsoft® Access 2003 (Microsoft, USA) was used as the database system and Stata SE10® (StataCorp., USA) was used to conduct the statistical analyses. Before data entry, questionnaires were checked for plausibility and completeness. After transferring the data to the analysis program, the demographic variables were checked for plausibility and selected exposure variables were checked for interviewer bias.
Statistical analyses
From the questionnaire 47 dichotomous variables for consumed food items and 23 variables for animal contact were obtained. Four variables dealt with hygiene practice in the context of food preparation. The remaining information on potential risk factors such as medical preconditions, pharmaceutical drug use, travel behaviour, etc. was collected in 13 variables.
Because two sets of controls were recruited differently, and potential biases were expected to differ between PopC and RVC, the two control groups were considered separately.
Salmonella infections occur more frequently in summer than in winter, RVC even more frequently during winter. PopC were enrolled throughout the whole year. Food consumption and animal contact as well as foreign travel differ between winter (October–March) and summer (April–September) seasons. Therefore, seasonal adjustment by stratification of the single-factor analyses was performed for all statistical analyses.
Single risk-factor analysis was performed by Mantel–Haenszel combined odds ratios (OR) for each of the 87 variables, adjusted for season, accompanied by Wald's 95% confidence interval (CI) and two-sided P values.
For multiple logistic regression analyses a risk-factor model selection was necessary [8]. Variables which were likely to be influenced by social desirability bias were excluded, as were variables with fewer than two exposed persons. In a first selection step, variables with a P value <0·3 in the single-factor analysis were selected, as were variables with an OR > 1·5. Multicollinearity between exposures was pre-assessed via correlation analyses. In case of associations (correlation coefficient, Pearson's r > 0·2 or r < − 0·2) between exposure variables a second selection step was conducted. Either one variable was chosen as a proxy and all others were dropped from further analyses or a combined variable was constructed out of the associated variables. Starting with this set of exposure variables the associations between Salmonella status and exposures were assessed in multiple logistic regression analyses with a step-wise variable selection procedure starting with the full model. The P value cut-off for removal from the model was 0·3. Furthermore, data were adjusted for seasonal influences by including the variable ‘summer season’ in the regression analyses.
The analyses were performed separately for the two control groups to reveal the influence of presumed biases, e.g. recall bias and selection bias. Recall bias has to be considered because recently ill persons may be more likely to remember what they ate during the last days before onset of illness. However, PopC usually do not have a detailed memory of consumed food items. The results for SCP vs. PopC are interpreted as the primary results. In order to account for the recall bias, the RVC group was chosen additionally. To interpret an exposure as a risk factor for salmonellosis, statistically significant associations between exposure and salmonellosis were expected for each of the control groups (PopC and RVC).
The population-attributable risk (PAR) for the consumption of raw ground pork was estimated by using an approximation formula for case-control studies [9].
RESULTS
Study cases
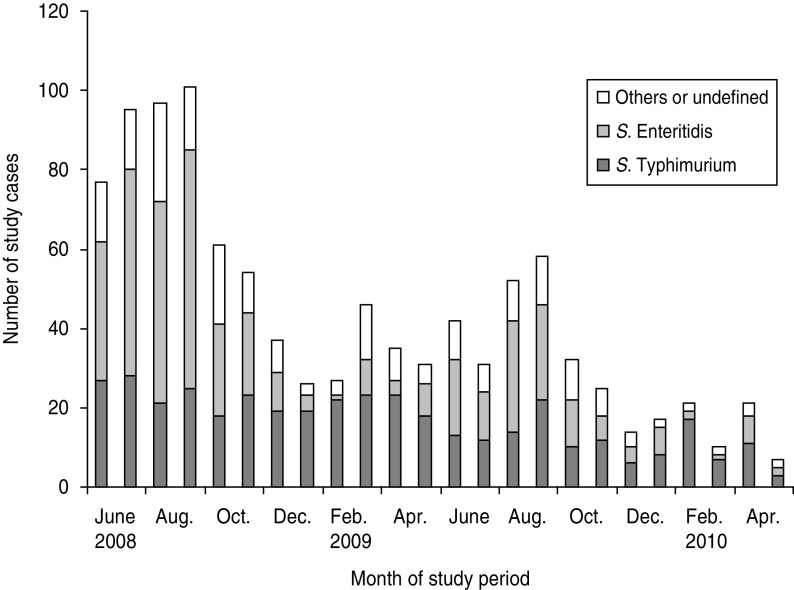
During the study period 4336 notified Salmonella cases aged >14 years were reported to the NLGA. Twenty-seven out of 46 LHDs in Lower Saxony cooperated in the study during the whole study period. A further 11 LHDs participated only for part of the study period, mainly because of the additional workload due to the 2009 swine flu pandemic. In total, these LHDs contributed 2513 cases of the required age group, of which 515 cases belonged to outbreaks. Thus, the remaining study population included 1998 eligible Salmonella cases. A successful interview was conducted with 1017 (51%) SCP. Figure 2 shows the distribution of SCP recruitment during the study period. Reasons for non-response were distributed as follows: 258 (13%) case persons could not be contacted via phone, 131 (7%) case persons were unable to participate in a telephone interview due to language problems or mental state and 592 (30%) case persons did not give their consent for study participation. The gender ratio of SCP was 47% males/53% females (average age 44 years). The corresponding values for all reported cases aged >14 years were 49% males, 51% females (average age 47 years). The period between onset of illness and interview ranged between 5 and 135 days (95% fewer than 40 days) with a mean of 20 days. The average (±s.d.) interview duration was 17 ± 7 min for all interviews conducted by NLGA.
Fig. 2.
Distribution of onset of symptoms from Salmonella cases included in the study population.
Controls
For recruitment of PopC, 1762 randomly generated telephone numbers were used, 1028 (58%) of which did not refer to private households. One hundred and forty valid telephone numbers could not be reached within at least six attempts on different days and at different times. Fourteen persons were not able to converse over the phone, and 408 (69·5%) out of 587 contacted persons refused to participate. Therefore, 176 persons aged 15–87 years (average age 48 years) participated in the complete telephone interview. The gender ratio of PopC was 53% males/47% females. The average interview duration was 13 ± 5 min for all interviews.
In addition, 170 persons were enrolled with reported rotavirus infection (RVC) from 21 LHDs. Here the average age was 47 years. The gender ratio was 49% males/51% females. The average interview duration was 16 ± 5 min for all interviews.
Variable selection procedure for multiple logistic regression analysis
Deficiencies in hygiene practice were expected to be a risk for Salmonella infections. The analyses revealed an association between good hygiene practice and salmonellosis. This result was possibly due to social desirability bias. Thus, all variables concerning hygiene practices were excluded from the analyses.
Overall, 39 exposure variables were selected in the first selection step. The seven variables for pre-existing conditions and pharmaceutical drug use, remaining after this selection step were: taking gastric acidity inhibitors, immunodeficiency, cancer, taking antibiotics, taking corticosteroids, taking other pharmaceutical drugs during the last 4 weeks, and chronic bowel disease. These variables were found to be associated with each other. The use of gastric acidity inhibitors was used as proxy with the strongest association with Salmonella infection.
Due to associations between variables referring to animal contact and owning pets or livestock, the general variables ‘animal contact in the last 3 days’ and ‘job-related animal contact of a member of the household’ were retained.
Finally, there were variables on similar food items, which were associated with each other, e.g. consumption of meat in general, consumption of chicken, and consumption of turkey. Again, the variable with the highest association with the outcome (chicken meat) was chosen for further analyses.
Consumption of raw tomatoes (fresh) and non-heated herbs (fresh or dried) and peppers were also associated with each other. This was due to, e.g. their combination in salads or the combination of tomato and mozzarella. Therefore, a combined variable for consumption of one or more of these products was used for further analyses.
After the selection procedure 12 variables remained for the multiple logistic regression analysis (Table 1).
Table 1.
Exposure frequencies in cases, population controls and rotavirus controls. Odds ratios adjusted for season from single variable analyses: cases vs. each control group for the selected variables used in multiple logistic regression analysis
| SCP (N = 1017) | PopC (N = 176) | RVC (N = 170) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | OR* | 95% CI† | n | % | OR* | 95% CI† | |
| Summer seasona | 647 | 63·6 | 95 | 54·0 | 83 | 48·8 | ||||
| Raw ground porkb | 136 | 13·4 | 12 | 6·8 | 2·22 | 1·20–4·12 | 6 | 3·5 | 4·27 | 1·88–9·70 |
| Eggsb,c | 948 | 93·2 | 158 | 89·8 | 1·45 | 0·84–2·51 | 145 | 85·3 | 2·15 | 1·32–3·52 |
| Chicken meatb | 504 | 49·6 | 61 | 34·7 | 1·03 | 0·74–1·44 | 93 | 54·7 | 0·81 | 0·58–1·12 |
| Smoked fishb | 46 | 4·5 | 5 | 2·8 | 1·59 | 0·62–4·04 | 3 | 1·8 | 2·72 | 0·82–9·02 |
| Wild gameb | 26 | 2·6 | 2 | 1·1 | 2·51 | 0·61–10·32 | 2 | 1·2 | 2·77 | 0·64–12·0 |
| Tomatoes, peppers, herbsb,d | 729 | 71·7 | 143 | 81·3 | 0·55 | 0·37–0·83 | 129 | 75·9 | 0·76 | 0·52–1·11 |
| Raw milk, raw milk cheeseb | 34 | 3·3 | 11 | 6·3 | 0·50 | 0·25–1·02 | 18 | 10·6 | 0·27 | 0·15–0·50 |
| Outdoor meals/barbecuesb,e | 92 | 9·0 | 4 | 2·3 | 3·88 | 1·40–10·79 | 12 | 7·1 | 1·11 | 0·59–2·10 |
| Animal contact (job)f | 92 | 9·0 | 16 | 9·1 | 1·00 | 0·57–1·74 | 5 | 2·9 | 3·32 | 1·32–8·33 |
| Animal contactb | 498 | 49·0 | 111 | 63·1 | 0·57 | 0·41–0·79 | 73 | 42·9 | 1·29 | 0·93–1·80 |
| Foreign travel b | 106 | 10·4 | 8 | 4·5 | 2·35 | 1·12–4·90 | 10 | 5·9 | 1·78 | 0·91–3·48 |
| Gastric acidity inhibitorsg | 120 | 11·8 | 9 | 5·1 | 2·49 | 1·24–5·02 | 28 | 16·5 | 0·67 | 0·43–1·05 |
SCP, Salmonella case persons; PopC, population controls; RVC, rotavirus controls; n, number of exposed persons; OR, odds ratio; CI, confidence interval.
Odds ratio adjusted for season for cases vs. controls.
95% CI for OR.
Bold values indicates lower limit of 95% CI above 1·0.
Onset of illness: April–September.
During the last 3 days, before onset of illness (SCP, RVC); before interview (PopC).
Or egg-containing products (e.g. cake, ice cream, pancakes, mayonnaise, etc.).
Consumption of at least one of the food items: raw tomatoes (fresh), uncooked peppers, uncooked herbs (fresh or dried).
Response to the question: ‘Did you attend a barbecue or other outdoor meal?’
Job-related animal contact of a household member.
During the last 4 weeks, before onset of illness (SCP, RVC); before interview (PopC).
Associations between exposure and outcome
Table 1 shows the ORs for associations between salmonellosis and exposures with respect to PopC and RVC adjusted only for seasonality, and Table 2 shows adjusted odds ratios (aORs) adjusted for all other variables in the model. In the multiple factor analyses (Table 2) positive statistically significant associations for both control groups were found for consumption of raw ground pork and borderline significance was found for foreign travel. Positive statistically significant associations only for PopC were found for consumption of chicken meat, outdoor meals or barbecues, and taking gastric acidity inhibitors. Consumption of eggs or egg-containing products and job-related animal contact showed positive associations only for RVC.
Table 2.
Variable adjusted odds ratios from multiple logistic regression analyses, separate for population controls and rotavirus controls
| Exposure | PopC | RVC | ||
|---|---|---|---|---|
| aOR* | 95% CI† | aOR* | 95% CI† | |
| Summer seasona | 1·45 | 1·03–2·04 | 1·78 | 1·26–2·50 |
| Raw ground porkb | 2·38 | 1·27–4·44 | 4·62 | 1·99–10·74 |
| Eggsb,c | 1·43 | 0·80–2·54 | 2·07 | 1·23–3·48 |
| Chicken meatb | 1·77 | 1·26–2·50 | 0·77 | 0·54–1·08 |
| Smoked fishb | ∼1 | P > 0·3 | 2·67 | 0·81–8·86 |
| Wild gameb | 2·46 | 0·57–10·72 | 2·32 | 0·53–10·20 |
| Tomatoes, peppers, herbsb,d | 0·52 | 0·34–0·79 | 0·75 | 0·50–1·11 |
| Raw milk, raw milk cheeseb | 0·59 | 0·28–1·23 | 0·29 | 0·15–0·54 |
| Outdoor meals/barbecuesb,e | 3·96 | 1·41–11·12 | ∼1 | P > 0·3 |
| Animal contact (job)f | ∼1 | P > 0·3 | 3·02 | 1·19–7·63 |
| Animal contactb | 0·57 | 0·41–0·81 | 1·29 | 0·92–1·82 |
| Foreign travel b | 2·12 | 1·00–4·52 | 2·13 | 1·06–4·28 |
| Gastric acidity inhibitorsg | 2·42 | 1·19–4·92 | 0·67 | 0·42–1·07 |
PopC, Population controls; RVC, rotavirus controls; aOR, adjusted odds ratio; CI, confidence interval.
Variable aORs from step-wise multiple logistic regression analysis for PopC and RVC.
95% CI for aOR.
Bold values indicates lower limit of 95% CI above 1·0.
Onset of illness: April–September.
During the last 3 days, before onset of illness (SCP, RVC); before interview (PopC).
Or egg containing products (e.g. cake, ice cream, pancakes, mayonnaise, etc.).
Consumption of at least one of the food items: raw tomatoes (fresh), uncooked peppers, uncooked herbs (fresh or dried).
Response to the question: ‘Did you attend a barbecue or other outdoor meal?’
Job-related animal contact of a household member.
During the last 4 weeks, before onset of illness (SCP, RVC); before interview (PopC).
Including age in the regression analysis did not produce any remarkable changes in the ORs. The aOR for the variable ‘age’ was 0·99 for both groups of controls.
DISCUSSION
The aim of this case-control study was to identify and to assess risk factors for sporadic salmonellosis under recent exposure conditions in Germany. The study was based on standardized interviews from cases and two groups of controls. Statistically significant associations with Salmonella infections were found for the consumption of raw ground pork, outdoor meals or barbecues, foreign travel, and taking gastric acidity inhibitors.
For consumption of raw ground pork a distinctive and statistically significant association with Salmonella infection was found for both groups of controls. This may be interpreted as strong evidence that consumption of (raw) pork is a relevant risk factor for sporadic Salmonella infections. Outbreaks due to consumption of raw pork have previously been described in Germany [13] and an association with sporadic salmonellosis was found in The Netherlands [14] while a Canadian multi-provincial case-control study failed to show this risk [15]. A PAR may be approximated for the consumption of raw ground pork, because this appears to be a popular food in Germany. For the data suggested here PAR appears to be 7% for all Salmonella cases, using PopC only as control and 13%, using both groups as one complete control. Assuming that consumption of raw ground pork during the previous 3 days in PopC is a proxy for the consumption of raw ground pork in general, this indicates an enormous burden of disease, and should therefore be taken into account for risk management action.
The consumption of eggs in any form or egg-containing products (e.g. cake, ice cream, pancakes, mayonnaise, etc.) was associated with Salmonella infection. For RVC the association was statistically significant, but not so for PopC. This leads to the conclusion that consumption or handling of eggs is probably still a moderate risk factor for Salmonella infections. This association has been described in several other studies [14, 16–18]. However, the low association between consumption or handling of eggs and Salmonella infections found in this study is in line with the assumption of the decreasing relevance of consumption of contaminated egg products for all Salmonella infections [6].
Consumption of poultry products (chicken and turkey) was associated with each other. Since the OR for consumption of chicken and salmonellosis was higher than for turkey, it was chosen for the analysis. Consumption of chicken meat showed a statistically significant association for PopC but not for RVC. This may suggest the appearance of a recall bias and may not lead to the assumption that consumption of chicken meat (or turkey) is a relevant risk factor for sporadic salmonellosis for the population under consideration.
Barbecues or outdoor meals during the 3 days prior to onset of disease were statistically significantly associated with salmonellosis for PopC. For this exposure, we would not expect recall bias, because contrary to the consumption of one distinct food item, barbecues or outdoor meals are easily recalled by everyone. Therefore, this result suggests evidence that attending a barbecue/outdoor meal is a risk factor for Salmonella infections.
Our results show a negative association for animal contact in the previous 3 days for PopC. A possible explanation for this could be some type of boost effect by continuous animal contact for immunocompetence against common zoonotic infections, which has been previously described as a possible explanation for negative associations between risk factors and illness [19]. Moreover, it is possible that the negative association is due to a different lifestyle (food consumed, activities, travel) of pet-owners compared to other people. The ORs for job-related animal contact for a household member differ substantially for the different control groups. Thus, from this data we cannot conclude that job-related animal contact could be a risk factor for salmonellosis.
Foreign travel is statistically significantly associated with salmonellosis for both control groups. This association has been previously described [4].
For the variables concerning pre-existing conditions (diabetes, use of pharmaceutical drugs, immunodeficiency, etc.) there were clear associations with salmonellosis for PopC. RVC was not an adequate group of controls for these variables because such pre-existing conditions promote diagnosis of rotavirus infections. Due to a considerable association between all these variables, we included taking gastric acidity inhibitors only in our model, which was closely related to the gastrointestinal system. Therefore, the estimate of the aOR of this category could be regarded as representative for one or more of the other associated exposures or pre-existing conditions. The adjusted OR (2·4) for PopC for taking gastric acidity inhibitors in the previous 4 weeks leads to the assumption that taking gastric acidity inhibitors carries a risk for contracting and developing salmonellosis. The patho-mechanism, a reduced gastric resistance against Salmonella due to a lack of gastric acids, is biologically plausible and has been described previously [20]. Other epidemiological studies interpreted taking gastric acidity inhibitors as a risk factor for Salmonella infection [21].
Interviews were conducted with 1017 (51%) SCP of 1998 eligible cases. We presume that the results are representative for sporadic Salmonella cases in general although the gender ratio in SCP showed slightly more women and the mean age was slightly younger than in all 4336 cases reported in Lower Saxony. However, the exclusion of outbreak-related cases worked well for large outbreaks, although some of the cases referred to as ‘sporadic’ might be related to others in an unrecognized way.
Regarding gender and mean age, PopC showed no differences to the general population in Lower Saxony [10]. Therefore, the representativeness of this control group with respect to the general population in Lower Saxony is confirmed.
As an additional control group rotavirus cases which do not belong to an outbreak were selected. The intention was to control for recall bias regarding PopC, which was expected mainly for the detailed questions about food consumption. The tendency of PopC to give quick answers without attempting to remember exactly which food was consumed was highlighted by the average interview duration, which was 4 min shorter than for the other group.
Thus, associations between consumption of different food items and outcome are suspect for being affected by recall bias with regard to PopC. Recall bias is not expected for RVC since RVC had similar symptoms as SCP and therefore were compliant, like SCP. Rotavirus infections do not belong to zoonotic diseases, foodborne infections may occur as a vehicle of human-to-human transmission but not by zoonotic transmission. Thus RVC can be assumed to be an adequate control group for most of the observed risk factors (consumed food items and animal contacts). Additionally, RVC were recruited by the same notification system as the Salmonella cases. This reduces the risk of selection bias due to selection mechanisms for access to medical care and notification. The selection bias of the case group, which is due to housing categories and socioeconomic status, was previously described for infectious intestinal diseases [11]. All of these known and unknown selection factors are assumed to be similar between RVC and SCP. However, a limitation for RVC as a control group is an expected selection due to individual pre-existing conditions which might promote infection and diagnosis of rotavirus.
The number of interviews with control persons which was obtained was lower than expected, whereas the number of case persons reached the expected number. This possibly leads to expanded CIs in the calculations and less sensitivity to detect associations. However, this does not influence the interpretation of the statistically significant associations in the study.
Regression analyses were repeated with age as an additional variable, because the average age of cases was slightly lower than that of controls. However, considerable changes in the values for aORs were not identified, thus results are presented without the inclusion of age for the regression analyses.
In order to avoid interviewer bias all interviewers were trained and a standardized questionnaire was used. Cases and controls were both interviewed by the same interviewers. Therefore, an interviewer bias was not considered.
To deal with confounding a multi-step model selection was conducted taking into account the multicollinearity of the exposures under consideration. The results of multiple logistic regressions were quite stable. Forward and backward selection procedures or scrapping of single variables did not lead to considerable changes in the calculated ORs. Some of the exposure variables which were finally selected represent the subset of variables, which were associated with each other. Including all associated variables and their product (interaction) terms would have resulted in a too complex model with such a large number of estimates that the model would not have converged. Fitting such a model would have exceeded the capability of the data [12]. Therefore, a statistically significant association of a proxy variable with salmonellosis was discussed, also considering the related group of exposures as the risk factor.
In this study from Lower Saxony, Germany, consumption of raw ground pork appears as a risk factor for sporadic salmonellosis in general. In connection with popular nutrition habits this may cause a substantial burden of disease in the target population under consideration. In addition, barbecues or outdoor meals can also be suggested as risk factors. Taking gastric acidity inhibitors appears to promote Salmonella infections.
During the last 10 years in Germany the incidence of notified S. Enteritidis cases known to be associated with the consumption of eggs [7] has constantly decreased. The incidence of S. Typhimurium, known to be associated with the consumption of raw pork [16], has remained almost constant. Combined with the findings of this study this supports evidence that the transmission of Salmonella from chicken products (and turkey products) to humans has been successfully reduced during the last years, but the transmission from pork products remains a constant problem. Therefore, keeping the successful strategy to reduce salmonellae in chickens and increasing efforts to reduce salmonellae in pigs may be suggested as important tools for risk management in Germany. Risk communication to the consumer also plays an important role. In the German population, salmonellosis is mainly assumed to be caused by (raw) eggs and chicken products. At the same time, consumption of raw ground pork is still a traditional food item in Germany. Therefore, the population's awareness of this risk factor needs to be increased.
ACKNOWLEDGEMENTS
This study is part of the FBI-Zoo Consortium financially supported by the German Federal Ministry of Education and Research (BMBF) through the German Aerospace Center (DLR), grant number 01KI07128 (FBI-Zoo).
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Robert Koch Institute. Yearbook of Infectious Disease Epidemiology 2009, 2010, pp. 168–169. [Google Scholar]
- 2.Hoelzer K, Moreno Switt AI, Wiedmann M. Animal contact as a source of human non-typhoidal salmonellosis. Veterinary Research 2011; 42: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Food Safety Authority. A quantitative microbiological risk assessment on Salmonella in meat: Source attribution for human salmonellosis from meat. EFSA Journal 2008; 2008: 1–32. [Google Scholar]
- 4.Kist MJ, Freitag S. Serovar specific risk factors and clinical features of Salmonella enterica ssp. enterica serovar Enteritidis: a study in South-West Germany. Epidemiology and Infection 2000; 124: 383–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabsch W, Tschape H, Baumler AJ. Non-typhoidal salmonellosis: emerging problems. Microbes and Infection 2001; 3: 237–247. [DOI] [PubMed] [Google Scholar]
- 6.Federal Institute for Risk Assessment (BfR). Annual report on the epidemiological situation of zoonoses in Germany 2008, 2010, p. 12. [Google Scholar]
- 7.Häder S. Telephone number sampling (http://www.gesis.org/fileadmin/upload/forschung/publikationen/gesis_reihen/howto/how-to6sh.pdf). Accessed 12 April 2012.
- 8.Greenland S. Modeling and variable selection in epidemiologic analysis. American Journal of Public Health 1989; 79: 340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor JW. Simple estimation of population attributable risk from case-control studies. American Journal of Epidemiology 1977; 106: 260. [DOI] [PubMed] [Google Scholar]
- 10.Louven N. Description and test of representativeness of a control sample from telephone sampling by Gabler–Häder (dissertation). Germany: Ostfalia, Academia for Practical Sciences, 2010. [Google Scholar]
- 11.Tam CC, Rodrigues LC, O'Brien SJ. The study of infectious intestinal disease in England: what risk factors for presentation to general practice tell us about potential for selection bias in case-control studies of reported cases of diarrhoea. International Journal of Epidemiology 2003; 32: 99–105. [DOI] [PubMed] [Google Scholar]
- 12.Rothmann K, Greenland S, Lash TL. Modern Epidemiology. Philadelphia: Lippincott Williams and Wilkins, 2008, pp. 420–421. [Google Scholar]
- 13.Jansen A, Frank C, Stark K. Pork and pork products as a source for human salmonellosis in Germany. Berliner und Muenchner Tieraerztliche Wochenschrift 2007; 120: 340–346. [PubMed] [Google Scholar]
- 14.Doorduyn Y et al. Risk factors for Salmonella Enteritidis and Typhimurium (DT104 and non-DT104) infections in The Netherlands: predominant roles for raw eggs in Enteritidis and sandboxes in Typhimurium infections. Epidemiology and Infection 2006; 134: 617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dore K et al. Risk factors for Salmonella typhimurium DT104 and non-DT104 infection: a Canadian multi-provincial case-control study. Epidemiology and Infection 2004; 132: 485–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banatvala N et al. Salmonellosis in North Thames (East), UK: associated risk factors. Epidemiology and Infection 1999; 122: 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Delarocque-Astagneau E et al. Risk factors for the occurrence of sporadic Salmonella enterica serotype typhimurium infections in children in France: a national case-control study. Clinical Infectious Diseases 2000; 31: 488–492. [DOI] [PubMed] [Google Scholar]
- 18.Molbak K, Neimann J. Risk factors for sporadic infection with Salmonella enteritidis, Denmark, 1997–1999. American Journal of Epidemiology 2002; 156: 654–661. [DOI] [PubMed] [Google Scholar]
- 19.Swift L, Hunter PR. What do negative associations between potential risk factors and illness in analytical epidemiological studies of infectious disease really mean? European Journal of Epidemiology 2004; 19: 219–223. [DOI] [PubMed] [Google Scholar]
- 20.Laine L et al. Review article: potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Alimentary Pharmacology and Therapeutics 2000; 14: 651–668. [DOI] [PubMed] [Google Scholar]
- 21.Jansen A et al. Protracted nosocomial outbreak of Salmonella Enteritidis LT 8/7. Zeitschrift für Gastroenterologie 2008; 46: 1270–1274. [DOI] [PubMed] [Google Scholar]